Abstract
Purpose
The COVID-19 pandemic has had a profound impact on American life. However, the burden of the pandemic has not been distributed equally. The purpose of this study was to investigate whether racial and economic residential segregation were associated with COVID-19 related factors in the nation's capital, Washington D.C., during the first year of the pandemic.
Methods
Racial, economic, and racialized economic segregation were assessed using the Index of Concentration at the Extremes measure and data from the 2014–2018 American Community Survey. COVID-19 related factors (i.e., incidence, testing rate, and percent positivity) were assessed using data from the Washington D.C. government. Spearman rank correlation was used to assess the relationship between each segregation measure and each COVID-19 related factor.
Results
Washington D.C. neighborhoods with a higher concentration of African Americans, lower income residents, and African Americans with low income had a higher incidence of COVID-19 and greater percent positivity, but lower testing rates compared to their counterparts.
Conclusions
There is a geographic mismatch between neighborhoods most vulnerable to COVID-19 and the neighborhoods where the testing resources are being used. More resources should be allocated to the most vulnerable neighborhoods to address the COVID-19 pandemic in an equitable manner.
Introduction
With the death of over half a million Americans, the emergence and persistence of COVID-19 in the United States has undoubtedly altered American life [1]. As an airborne, infectious disease, COVID-19 has been touted by some in mainstream media as “a great equalizer” where social standing would not impact vulnerability [2]. In reality, vulnerability to COVID-19 is not uniform in American society as data consistently identifies stark racial disparities [3,4]. For example, in the nation's capital, Washington D.C., African Americans represent ~46% of the population but make up 75% of COVID-19 related deaths [5]. COVID-19 disparities have mostly been explained by two reasons: 1) African Americans are disproportionately affected by pre-existing health conditions (e.g., heart disease, diabetes, and kidney disease) that are risk factors for COVID-19 and 2) African Americans are more likely to have front line occupations that offer less protection (e.g., contact with the public, no paid sick leave) against the virus [6], [7], [8]. However, the failure to contextualize these explanations leaves lost opportunity to adequately address the disparities and reduce the spread of the virus.
We draw on fundamental cause theory, which posits that racism and socioeconomic inequality are root causes of health disparities, to explain the disproportionate effect of COVID-19 on African Americans [9,10]. These root causes operate largely via racial residential segregation, an institutional mechanism of racism that represents the physical separation of residences by race and is tied to economic opportunity [11], [12], [13]. Despite the passing of the Fair Housing Act of 1968 which made explicit discriminatory housing practices illegal, segregation is still maintained in contemporary American society [14]. Decades of research have highlighted the importance of neighborhood level resources on the health of residents [15]. The neighborhood environment provides access to resources such as education, occupational opportunities, healthy food availability, engagement in physical activity, clean air and water, social capital, healthcare, and safety. These resources in turn are associated with disease vulnerability [16], [17], [18], [19]. Segregation has been associated with a myriad of chronic and infectious health outcomes such as incident cardiovascular disease [20], systolic blood pressure [21], obesity [22], and tuberculosis [23,24]. The risk of disease associated with segregation is not inherently due to residing next to individuals of a specific race or economic status. Rather, the associations are the result of the concentration of social disadvantage and systematic disinvestment in marginalized communities [25].
Based on the extant literature demonstrating that residential segregation is a significant predictor of many health outcomes, we hypothesize that it will also associate with COVID-19 related factors. In the present study, we first map the neighborhood level geographic distribution of COVID-19 related factors (i.e., incidence, number of tests administered, and percent positivity rate) in Washington D.C. We then assess whether racial and economic segregation, measured both independently and jointly, are associated with COVID-19 related factors.
Material and methods
Study population
Washington D.C. is the capital city of the United States and is home to approximately 705,000 residents [26]. Based on data from the 2014–2018 American Community Survey, most of the population identify as either Black or African American (47.2%) or white (45.1%). Economically, Washington D.C. leads the country in median household income ($82,604). However, there are stark racial and economic segregation patterns in the city. Data from the University of Michigan's Census Scope indicate that 66% of one race would have to move to a different neighborhood for African Americans and whites to be equally distributed geographically [27]. Washington D.C. has greater income inequality than any state in the nation, and economic status differs greatly along racial lines [28]. The median household income for African Americans is $43,564 while it is $132,040 for white households, and the poverty rate is 25.7% for African Americans and 6.9% for whites [26].
Measures
Segregation
We obtained the population level estimates for race and median household income using data from the 2014–2018 American Community Survey at the census tract level and aggregated the estimates to be consistent with the neighborhood boundaries utilized by the Washington D.C. government. Using the Index of Concentration at the Extreme (ICE) measure, we assessed three types of segregation in Washington D.C.: racial (African American/white), economic (high income/low income), and racialized economic (low income & African American/high income & white). We used income cutoffs consistent with the literature where “high income” was considered a median household income of $100,000 or greater and $25,000 or less was considered “low income [29].” The ICE measure has been used in previous public health studies as a measure of local segregation patterns because it can be meaningfully employed at lower levels of geography (e.g., neighborhoods) and permits joint measurement of racial and economic segregation [30,31]. The general formula is given by:
where for a given neighborhood i:
Ai= number of persons in Category A (e.g., high income)
Bi= number of persons in Category B (e.g., low income)
Ti= total count of persons belonging to population categorized in relation to the measure (e.g., high+ low income)
Possible ICE values range from +1 to −1 where +1 represents everyone being in Category A and −1 represents everyone being in Category B. In the analyses, white, high income, and high income & white were coded as Category A, and African American, low income, and low income & African Americans were coded as Category B.
COVID-19 outcomes
Three COVID-19 related factors were assessed in this study: incidence, number of tests administered, and percent positivity rate. Neighborhood level COVID −19 data were retrieved from the Government of District of Columbia's coronavirus website (https://coronavirus.dc.gov/). The coronavirus website is updated daily to track the status of the ongoing coronavirus pandemic, and we use data for the first six and second six months since the first reported case of COVID-19 in Washington D.C. (March 7, 2020- September 7, 2020 & September 8, 2020-March 6, 2021). The neighborhoods are groups of one to seven contiguous census tracts, enabling comparisons with the U.S. Census data. We calculated the population-standardized number of cases and tests per 1000 residents for each Washington D.C. neighborhood. Percent positivity was calculated as the number of cases divided by the number of tests.
Statistical analyses
Bivariate associations using Spearman rank correlations were employed to assess the associations between segregation measures and COVID outcomes. The Spearman method was used because it is a nonparametric test that does not assume a linear relationship between two variables. Maps were created using QGIS 3.12.3, and analyses were conducted using R 4.0.1.
Results
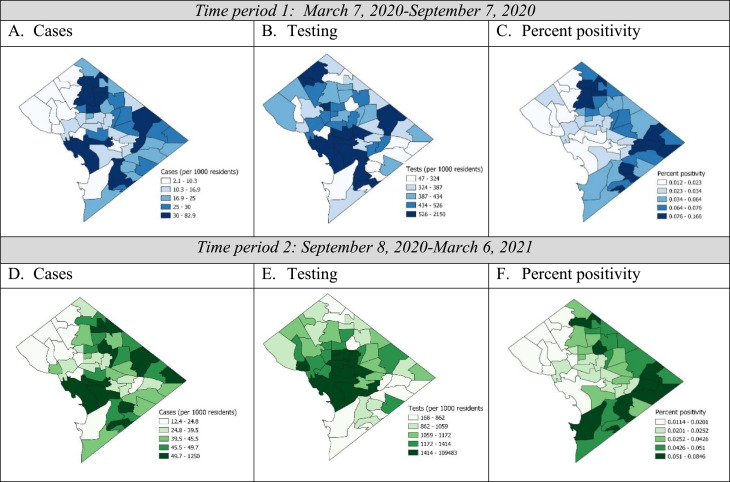
In the first six months, there were a total of 14,102 reported COVID-19 cases and 298,793 tests that were mapped to neighborhoods in Washington D.C. (Fig. 1 ). This corresponds to an overall percent positivity of 4.7%. In the second six months, there were an additional 27,317 cases and 962,570 tests. The percent positivity for the second six months equates to 2.8%.
Fig. 1.
Geographical distribution of COVID-19 related factors.
Overall, there were similar patterns in the correlations between each of the segregation measures with the COVID-19 related factors (Table 1 ). There were inverse correlations for cases and percent positivity, and positive correlations for testing. This indicates that neighborhoods with a greater concentration of African Americans (vs. whites), low income (vs. high income) residents, and African Americans of low income (vs. whites of high income) have higher rates of COVID-19 incidence despite lower testing rates (Table 1). There were no significant differences in the correlations between the first six months and second six months for any of the segregation-COVID factor relationships (data not shown).
Table 1.
Spearman correlations between segregation and COVID-19 related factors
| First 6 months |
Second 6 months |
|||||
|---|---|---|---|---|---|---|
| Cases | Testing | Percent positivity | Cases | Testing | Percent positivity | |
| Racial segregation | −0.59⁎⁎⁎ | 0.30* | −0.81⁎⁎⁎ | −0.53⁎⁎⁎ | 0.54* | −0.80⁎⁎⁎ |
| Economic segregation | −0.46⁎⁎⁎ | 0.33* | −0.64⁎⁎⁎ | −0.56⁎⁎⁎ | 0.38⁎⁎ | −0.77⁎⁎⁎ |
| Racialized economic segregation | −0.53⁎⁎⁎ | 0.32* | −0.72⁎⁎⁎ | −0.61⁎⁎⁎ | 0.45⁎⁎ | −0.84⁎⁎⁎ |
P < .05,.
P < .01,.
p < .001.
Discussion
In this study, we found inverse associations between segregation (racial, economic, and racialized economic) and COVID-19 cases and percent positivity, but positive associations between the segregation measures with COVID-19 testing in Washington D.C. These associations did not significantly change between the first and second six months of the pandemic. As COVID-19 is an ongoing pandemic, this study highlights the increased need for adequate resources for vulnerable populations in the nation's capital. The findings are consistent with fundamental cause theory in that it highlights that marginalized races (i.e. African Americans in the United States) and economically disadvantaged populations are more likely to be burdened by new diseases (e.g. COVID-19) and less likely to have access to sufficient health preserving resources (e.g. testing) needed to mitigate its impact [9,12,32].
Our findings that segregation patterns are associated with COVID-19 incidence and percent positivity are consistent with emerging studies [33,34]. For example, a study by Yu et al. of 100 metropolitan areas in the United States found that higher racial segregation was associated with COVID incidence and deaths, and this association was most pronounced for racially segregated cities that also had high income inequality [35]. An analysis in Massachusetts using the same Index of Concentration segregation measure used in the present study found that the joint measure of racialized economic segregation was associated with COVID-19 related deaths. In the study, residents in neighborhoods with a high concentration of low-income people of color were dying from COVID 1.66 times the rate of residents of neighborhoods with a high concentration of high income non-Hispanic whites [36]. Overall, the emerging literature suggests that racial and economic segregation are important upstream determinants of inequities of COVID-19 outcomes.
Since COVID-19 can be spread by both symptomatic and asymptomatic individuals, testing is a critical component of curbing the community spread of the virus. In the present study, we find that African American and economically disadvantaged neighborhoods received less tests per 1000 residents compared to white and economically advantaged neighborhoods. Extant investigations of the association between segregation and testing have yielded mixed findings. A study using early COVID data (through April 12, 2020) from NYC found no association between zip code level racial composition and testing but a significant inverse association between income and testing rate [37]. Findings from a study by Bilal et al. using data from New York City, Philadelphia, and Chicago suggests that temporality may play a role. This study found that socioeconomically disadvantaged neighborhoods received less testing than advantaged neighborhoods in the early weeks of the pandemic, but no association as the pandemic progressed [38]. However, findings from the present study show no change in trends over time in Washington D.C.
In this study, we did not account for potential confounders or mediators due to sample size restrictions. The smallest unit of geography of publicly available COVID-19 statistics for Washington D.C. is the neighborhood level. There are 51 D.C. neighborhoods, and analyses would be underpowered for regression techniques. Having more granular publicly data, such as the census tract level, would more than triple the sample size and statistical power would be increased. It would also facilitate more precise identification of the most vulnerable areas of the city. The publicly available data also does not permit analyses of whether COVID-19 data matches onto residents’ home neighborhood. Washington D.C. is part of a larger metropolitan area with a lot of intrastate and interstate commuting, and it is possible that people seek resources where they work or travel. The data also does not permit assessment of how many people have been tested. It is likely that some segments of the population (e.g., healthcare workers, correctional officers) have received multiple tests while others have not been tested at all. Lastly, we used income cutoffs ($100,000 for high income and $25,000) that were consistent with the literature. However, since D.C. leads the nation in both median household income and income inequality, the cutoffs may not capture segregation in the same way as other geographic regions.
Conclusion
As COVID-19 is an ongoing threat, there will be a continuous need for analyses such as the present one to monitor equitable distribution of life preserving resources for combating the virus. From an equity standpoint, the finding that segregation was associated with COVID-19 incidence and percent positivity but the testing association was in the opposite direction suggests that there is a geographic mismatch between neighborhoods most vulnerable to COVID-19 and the neighborhoods where the testing resources are being allocated. It is possible that vulnerable neighborhoods are being undertested, and the corresponding incidence rates are an underestimate of the true occurrence of COVID-19 in these areas. More resources should be allocated to the most vulnerable neighborhoods to address the COVID-19 pandemic in an equitable manner.
Acknowledgments
Research supported by the National Human Genome Research Institute Intramural Research Program of the National Institutes of Health.
References
- 1.CDC COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#cases_casesinlast7days (2020).
- 2.Mein S.A. COVID-19 and health disparities: the reality of “the great equalizer. J Gen Intern Med. 2020 doi: 10.1007/s11606-020-05880-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chowkwanyun M., Reed A.L. Racial health disparities and Covid-19 — caution and context. N Engl J Med. 2020 doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 4.Laurencin C.T., McClinton A. The COVID-19 Pandemic: a call to action to identify and address racial and ethnic disparities. J. Racial Ethn. Heal. Disparities. 2020 doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of the District of Columbia. Coronavirus Data. 2020 https://coronavirus.dc.gov/data Coronavirus Data. [Google Scholar]
- 6.Hooper, Monica Webb, Nápoles, Anna Maria, Pérez-Stable, E.J. COVID-19 and racial/ethnic disparities. J. Am. Med. Assoc.
- 7.Dorn A.van, Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020 doi: 10.1016/s0140-6736(20)30893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am. J. Ind. Med. 2020 doi: 10.1002/ajim.23145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Link B.G., Phelan J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995:80–94. Spec No. [PubMed] [Google Scholar]
- 10.Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015;41:311–330. [Google Scholar]
- 11.Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laster Pirtle W.N. Racial capitalism: a fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Heal. Educ. Behav. 2020 doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zalla L.C., Martin C.L., Edwards J.K., Gartner D.R., Noppert G.A. A geography of risk: structural racism and COVID-19 mortality in the United States. Am. J. Epidemiol. 2021 doi: 10.1093/aje/kwab059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faber J.W. Segregation and the geography of creditworthiness: racial inequality in a recovered mortgage market. Hous. Policy Debate. 2018 doi: 10.1080/10511482.2017.1341944. [DOI] [Google Scholar]
- 15.Diez Roux A.V., Mair C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010 doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 16.Hirsch J.A., Moore K., Clarke P. Changes in the built environment and changes in the amount of walking over time: longitudinalresults from the multi-ethnic study of atherosclerosis. Am. J. 2014;180(8):799–809. doi: 10.1093/aje/kwu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christine P.J., et al. Longitudinal associations between neighborhood physical and social environments and incident type 2 Diabetes Mellitus. JAMA Intern. Med. 2015;175:1311. doi: 10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mujahid M.S., Diez Roux A.V., Cooper R.C., Shea S., Williams D.R. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis) Am. J. Hypertens. 2011;24:187–193. doi: 10.1038/ajh.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hajat A., et al. Air pollution and individual and neighborhood socioeconomic status: evidence from the multi-ethnic study of atherosclerosis (MESA) Environ. Health Perspect. 2013 doi: 10.1289/ehp.1206337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kershaw K.N., Osypuk T.L., Do D.P., De Chavez P.J., Roux A.V.D. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease the multi-ethnic study of atherosclerosis. Circulation. 2015 doi: 10.1161/CIRCULATIONAHA.114.011345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kershaw K.N., et al. Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among black adults: the CARDIA study. JAMA Intern. Med. 2017 doi: 10.1001/jamainternmed.2017.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bower K.M., et al. Racial residential segregation and disparities in obesity among women. J. Urban Heal. 2015 doi: 10.1007/s11524-015-9974-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Soc. Sci. Med. 2000 doi: 10.1016/S0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- 24.Acevedo-Garcia D. Zip code-level risk factors for tuberculosis: neighborhood environment and residential segregation in New Jersey, 1985-1992. Am. J. Public Health. 2001 doi: 10.2105/AJPH.91.5.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams D.R., Cooper L.A. COVID-19 and health equity - a new kind of ‘herd Immunity. JAMA. 2020 doi: 10.1001/jama.2020.8051. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Census Bureau. data.census.gov.
- 27.Segregation: Dissimilarity Index. Census Scope. http://www.censusscope.org/us/m8840/chart_dissimilarity.html.
- 28.2014-2018 American Community Survey. Gini Index of Income Inequality. https://data.census.gov/cedsci/table?q=ginicoefficient&g=0100000US.04000.001&tid=ACSDT5Y2018.B19083&hidePreview=true.
- 29.Krieger N., et al. Local residential segregation matters: stronger association of census tract compared to conventional city-level measures with fatal and non-fatal assaults (total and firearm related), using the index of concentration at the extremes (ICE) for racial. Econ. J. Urban Heal. 2017 doi: 10.1007/s11524-016-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feldman J.M., Waterman P.D., Coull B.A., Krieger N. Spatial social polarisation: using the Index of Concentration at the Extremes jointly for income and race/ethnicity to analyse risk of hypertension. J. Epidemiol. Community Health. 2015 doi: 10.1136/jech-2015-205728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N., Kim R., Feldman J., Waterman P.D. Using the index of concentration at the extremes at multiple geographical levels to monitor health inequities in an era of growing spatial social polarization: massachusetts, USA (2010–14) Int J Epidemiol. 2018 doi: 10.1093/ije/dyy004. [DOI] [PubMed] [Google Scholar]
- 32.Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015 doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- 33.Hendryx M., Luo J. COVID-19 prevalence and mortality rates in association with black race and segregation in the United States April 1 to April 15, 2020. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3582857. [DOI] [Google Scholar]
- 34.Millett G.A., et al. Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 2020 doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu, Qinggang, et al. The lethal spiral: racial segregation and economic disparity jointly exacerbate the COVID-19 fatality in large American cities. PsyArXiv. [DOI] [PMC free article] [PubMed]
- 36.Chen J.T., Waterman P.D., Krieger N. COVID-19 and the unequal surge in mortality rates in Massachusetts, by city/town and ZIP Code measures of poverty, household crowding, race/ethnicity,and racialized economic segregation. HCPDS Work. Pap. 2020 [Google Scholar]
- 37.Cordes J., Castro M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat. Spatiotemporal. Epidemiol. 2020 doi: 10.1016/j.sste.2020.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bilal U., Barber S., Diez-Roux A.V. medRxiv. 2020. Spatial Inequities in COVID-19 outcomes in Three US Cities. [DOI] [Google Scholar]