Abstract
We examined the impact of telehealth on appointment retention among individuals with substance use disorder (SUD) by housing status. We evaluated appointment status using multivariate logistic regression with primary predictor variables of visit modality, patient’s housing status and interaction between these two variables. Between March 1 and September 30, 2020, there were 18,206 encounters among 1,626 clients with SUD. For telehealth encounters, the probability of an appointment no-show was significantly higher for persons experiencing homelessness compared to stably housed (37% versus 25%, p < 0.001). Housing status influences the effectiveness of telehealth as a modality of healthcare delivery for individuals with SUD.
Keywords: Telehealth, Substance use disorder, Persons experiencing homelessness
1. Introduction
The COVID-19 pandemic has forced healthcare systems to adapt to new methods of care delivery to avoid risk of disease transmission. A focus of this care delivery transformation has been a transition to telehealth modalities, specifically telephone and video visits (Khatri and Perrone, 2020). Behavioral health and substance use treatment programs, including Opioid Treatment Programs (OTPs), have also had to adapt to these new changes (SAMHSA, 2021). Due to the pre-pandemic practice of frequent, often daily, in-person medication dosing at OTPs and high utilization of other in-person behavioral health services, there was an increased risk of COVID-19 transmission among patients while obtaining life-saving treatment. The Substance Abuse and Mental Health Services Administration (SAMHSA) recognized this risk early and released guidance on March 16, 2020, that relaxed rules for treatment in OTPs (SAMHSA., 2020a, SAMHSA (b), 2020b). In addition to permitting a greater number of take-home doses of dispensed medication, the new guidance also allowed for greater use of telehealth for evaluating and treating patients in this setting.
Expanding telehealth services is promising for ongoing care delivery, reducing transportation and time barriers of in-person care, and may decrease the likelihood of missed appointments for some patients. However, telehealth may also pose unique challenges for other patients, such as persons experiencing homelessness (PEH), or to challenges in technological infrastructure such as a reliable phone or internet access (Ramsetty and Adams, 2020). Due to these concerns, prior to COVID-19, many health centers serving large PEH populations have steered away from using telehealth (Lin et al., 2018). We assessed the impact of the telehealth visit modality and housing status on missed appointments during the COVID-19 crisis for clients with substance use disorders (SUD). Understanding the impact of shifting from in-person care to telehealth on the continuity of care among patients with high in-person health care utilization patterns, including patients with SUDs, is critical to inform healthcare organization and insurance company decisions about the most effective visit modalities during and beyond the pandemic.
2. Methods
We conducted a retrospective analysis of encounters for individuals with SUD seeking care at an outpatient behavioral health center that is part of Denver Health between March 1, 2020 through September 30, 2020. Denver Health is a large, urban safety-net hospital that serves approximately one-third of the population in Denver County, Colorado. The behavioral health center adopted telehealth services rapidly in March 2020 following SAMSHA’s recommendations. Patients were included if they received care from the Denver Health Outpatient Behavioral Health substance use specialty services during the study time period, those with dispensed medications, prescribed medications, or therapy only clients. Patients were excluded if they were < 16 years of age, or referred to services but did not attend at least one encounter with prescriber or therapist for intake.
Encounters were included if they were visits with prescribers or therapists for medication assessment, physical examination or psychotherapy; information on encounters and sociodemographic and clinical characteristics of patients were retrieved from electronic health records.
The primary outcome was appointment status, categorized as no-show or completed, for patients with SUD. At this clinic appointments are scheduled to meet medical necessity, regulatory requirements, or as requested by clients for individual assessment. Clinic expectations appointments in first 4–6 weeks include initial medical intake and week 1 medication follow up, physical examination, counselor intake and orientation to clinic. Ongoing expected encounters include at least monthly counselor appointments, as needed medical follow up, annual medical assessment and biannual physical examination. Appointments are scheduled either in person by staff at the clinic, by phone, or client initiated medical record communication. Printed copies of appointment time are offered for every scheduled encounter. Appointment reminders are provided ahead of appointment and on day of appointment at the clinic dispensary for those who receive dispensed medication, by automated electronic reminders for clients enrolled in the electronic health record interface, and occasionally by individual phone call. If an individual is more than 10–15 min late, the clinic staff mark this client as a no show. On occasions when individuals are able to make a walk-in encounter later in the day, the no show indication is reversed. If a client cancels the appointment at least 24 h ahead of scheduled time this encounter is removed from the schedule without being marked as non-attendance.
Telehealth visit modalities included both telephone and video encounters, although the majority of telehealth appointments as the behavioral health center were via telephone. Persons were identified as experiencing homelessness through an algorithm developed by the health system. The algorithm included a multipronged approach to identify homelessness in multiple places in the electronic health record, including: a checkbox that was selected if the patient self-identified as homeless, “homeless” written in the address field for the patient, and a list of addresses associated with PEH, including homeless shelters. Retrospective address data were stored for each patient, and patients were only categorized as PEH for this study if they were flagged as homeless during the time of their index encounter. Persons were categorized as PEH or stably housed. Additional sociodemographic variables and factors that may influence appointment status were also abstracted from electronic medical records, including provider type for each visit (therapist or provider), patient age (<35 years, 35–49 years, 50–64 years, and 65 + years), sex (male or female), and race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other).
We used bivariate descriptive statistics to characterize patients and encounters. We calculated Pearson’s Chi-squared tests to examine differences in encounter and sociodemographic characteristics by housing status (PEH versus stably housed (SH) individuals). We categorized the outcome as a binary variable and modeled the likelihood of a missed appointment (1) verses a completed appointment (0) using multivariate logistic regression. Our primary predictor variables were visit modality, patient’s housing status and an interaction term of these two variables. We also controlled for provider type and patient age, sex and race/ethnicity. Since clients at the behavioral health center often have multiple encounters within the 7-month timeframe, the logistic regression model accounted for encounters clustered within patients by calculating robust standard errors. Finally, using the estimated model, we calculated average marginal effects of visit modality on appointment status by housing status. We conducted all analyses using STATA 16 (Stata Statistical Software, 2019) and SAS 9.4 software (SAS Enterprise Guide, 2014) and utilized a significance level of α = 0.05.
This project was reviewed by Denver Health’s Quality Improvement Review Committee, authorized by the Colorado Multiple Institutional Review Board at the University of Colorado, Denver, and was determined not to be human subjects’ research, thus deemed exempt from Institutional Review Board review.
3. Results
Between March 1 and September 30, 2020, there were 18,206 encounters among 1,626 patients with SUD in the outpatient behavioral health center. Overall, the prevalence of missed appointments was higher for telehealth encounters as compared to in-person encounters (34.7% versus 28.9%, p = 0.014). Almost one-quarter (23.8%; n = 387) of patients were experiencing homelessness (PEH) ( Table 1). The median age of the patient cohort was 37 years (interquartile range (IQR) = 30–47), and the majority were male (58.9%), belonged to 16–35 years age group and identified as Non-Hispanic White (54.3%). Compared to SH individuals, PEH were more likely to be male, 35–49 years in age and identify as Non-Hispanic White and less likely to be in the 65 + age group or identifying as Hispanic. When comparing encounter level characteristics, PEH were less likely to have a telehealth appointment (35.5% versus 54.8%, p < 0.001). Overall, PEH had a higher prevalence of missed appointments (no-shows) as compared to SH individuals (33.1% versus 27.2%, p < 0.001).
Table 1.
Patient (N = 1626) and encounter (N = 18,206) characteristicsa of patients, overall and by housing status (persons experiencing homelessness (PEH) or stably housed) with Substance Use Disorder seeking care at an outpatient behavioral health center at Denver Health, March – September 2020.
| Variable | All | Housing Status |
||
|---|---|---|---|---|
| PEH | Stably Housed | p-valueb | ||
| Patient-Level | N = 1626 (%) | N = 387 (%) | N = 1239 (%) | |
| Age (median = 37, IQR = 30–47) | < 0.001 | |||
| 16–35 | 42.1 | 38.2 | 43.3 | |
| 35–49 | 36.2 | 42.9 | 34.1 | |
| 50–64 | 16.9 | 17.3 | 16.7 | |
| 65 + | 4.9 | 1.6 | 5.9 | |
| Sex | < 0.001 | |||
| Male | 58.9 | 72.4 | 54.6 | |
| Female | 41.1 | 27.7 | 45.4 | |
| Race/Ethnicity | < 0.001 | |||
| Hispanic | 32.0 | 20.2 | 35.7 | |
| Non-Hispanic White | 54.3 | 67.7 | 50.1 | |
| Non-Hispanic Black | 7.1 | 7.5 | 7.0 | |
| Non-Hispanic Other or Multiracial | 6.6 | 4.7 | 7.2 | |
| Encounter-Level |
N = 18,206 (%) |
N = 4237 (%) |
N = 13,969 (%) |
|
| Visit Modality | < 0.001 | |||
| In-Person | 49.7 | 64.6 | 45.2 | |
| Telehealth | 50.3 | 35.5 | 54.8 | |
| No Show | 28.5 | 33.1 | 27.2 | < 0.001 |
| Provider Type | 0.125 | |||
| Provider | 24.5 | 25.4 | 24.3 | |
| Therapist | 75.5 | 74.6 | 75.7 | |
b p-values are based on Pearson’s Chi-Square test
Data are presented as percentages
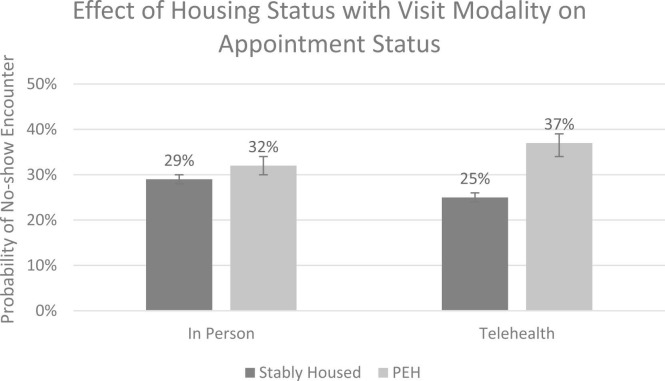
Fig. 1 shows marginal effects and 95% confidence intervals from the covariates adjusted logistic regression model for four groups: SH in-person encounters, PEH in-person encounters, SH telehealth encounters and PEH telehealth encounters. There were no significant differences in the probability of no-show for in-person encounters based on patients’ housing status (32% for PEH versus 29% for SH, ∆=3% 95% CI −0.2 to 5.7%). However, for telehealth encounters, the probability of no-show was significantly higher for PEH as compared to their SH counterparts (37% versus 25%; ∆=12%, 95% CI 6.9–16.4%). Furthermore, while comparing individuals within the same housing status, we found that SH individuals had a lower probability of missed appointment for telehealth encounters as compared to in-person encounters (25% versus 29%, ∆=−4% 95% CI −6.5% - −2.1%). On the other hand, PEH did not have a significantly different probability of missed appointment for telehealth encounters as compared to in-person encounters (37% versus 32%, ∆=5% X, 95% CI −0.1 to 9.3%).
Fig. 1.
Probabilitiesa of no-show encounter based on housing status (persons experiencing homelessness (PEH) vs. stably housed) and visit modality for patients with Substance Use Disorder seeking care at an outpatient behavioral health center of Denver Health, March - September 2020. Black lines on bars represent 95% Confidence Intervals of the Probabilities. a Probabilities are calculated as average marginal effects of visit modality on appointment status by housing status based on estimates of logistic regression model where the outcome is appointment status (no-show versus completed) and independent variables are visit modality, patient’s housing status, an interaction term of these two variables, age, sex, race/ethnicity and provider type.
4. Discussion
Our results indicate that while the overall prevalence of missed appointments was higher for telehealth encounters versus in-person encounters, housing status influences the effectiveness of telehealth as a modality of health care delivery for individuals with SUD. While PEH had a higher overall prevalence of missed appointments than persons who were SH, the differences between groups were only significant when examining telehealth appointments. PEH had a 12% higher likelihood of missing telehealth appointments compared to SH patients. Within same housing status, the probability of missing telehealth appointments as compared to in-person appointments was significantly lower for SH persons, but not significantly different for PEH.
Although telehealth was implemented at the start of the COVID-19 pandemic to reduce disease transmission and increase access to care (Wosik et al., 2020), telehealth visits may unintentionally create additional barriers for PEH. This is reflected in our findings as PEH had a higher probability of missing telehealth appointments as compared to SH patients. Access to key infrastructure components, including telephones, internet and private or safe space, is vital for use of behavioral health care through telehealth. It is plausible that PEH lack stable access to these components essential to complete appointments (Bakken, 2020). Early data from a program at Denver Health that offered cell phones to PEH to improve access to telehealth services suggested that providing phones alone did not reduce barriers to accessing care, reinforcing the importance of holistic methods to address multifaceted challenges faced by PEH and raising the possibility that PEH find benefit from clinic attendance above and beyond appointment interactions.
Despite the challenges faced by PEH in telehealth use, we found that within SH patients the likelihood of missed appointments was lower for telehealth encounters as compared to in-person encounters. This finding aligns with other evidence that shows how telehealth has improved healthcare use for clients with SUD during COVID-19 (Clark et al., 2021, Hughto et al., 2021). For individuals who have the resources, access to and an option to use telehealth has provided them with an opportunity to better manage their healthcare utilization during this pandemic.
Furthermore, telehealth has shown potential and promise in the delivery of mental healthcare for marginalized groups during COVID-19. For example, there is evidence that telehealth has been successful in promoting healthcare retention for PEH living with HIV (Brody et al., 2021),and users of youth mental health services have indicated that telehealth improved their receipt of services (Nicholas et al., 2021). Although we did not find statistically better engagement for PEH in our sample in terms of benefits of telehealth use, our findings were based on early pandemic period. It is essential to analyze data with a longer time frame to fully understand the impact of telehealth for clients with SUD.
This analysis has some limitations. First, quality data were not available for some variables that may help explain the relationship between telehealth and appointment status. For example, SUD severity could influence continuity of care. Although we explored options to include a measure for SUD severity, data were not adequate to produce confidence in our results. Additionally, it is possible that other aspects of the COVID-19 pandemic impacted care delivery and continuity in distinct ways for PEH and SH clients with SUD who are high healthcare utilizers. Despite these limitations, this analysis addressed a critical need to inform health service delivery for persons with SUDs within our healthcare system.
5. Conclusions
This analysis highlights the importance of considering housing status when evaluating telehealth services for care for SUD. For PEH, the gaps in telehealth infrastructure may eliminate the intended benefits of telehealth as a safe and efficient modality of health care delivery. Further research should explore the reasons for lower probability of completed telehealth encounters for PEH and implement and evaluate additional program supports to improve safe and continuous care delivery to this critical population.
Funding
Nothing declared.
Conflict of Interest
No conflict declared.
References
- Brody J.K., Rajabiun S., Strupp Allen H.J., Baggett T. Enhanced telehealth case management plus emergency financial assistance for homeless-experienced people living with HIV during the COVID-19 pandemic. Am. J. Public Health. 2021;111(5):835–838. doi: 10.2105/AJPH.2020.306152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark S.A., Davis C., Wightman R.S., Wunsch C., Keeler L.A.J., Reddy N., Samuels E.A. Using telehealth to improve buprenorphine access during and after COVID-19: a rapid response initiative in Rhode Island. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2021.108283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Enterprise 2014. Guide 7.1. SAS Institute Inc, Gary, NC (2014).
- Hughto J.M., Peterson L., Perry N.S., Donoyan A., Mimiaga M.J., Nelson K.M., Pantalone D.W. The provision of counseling to patients receiving medications for opioid use disorder: telehealth innovations and challenges in the age of COVID-19. J. Subst. Abus. Treat. 2021;120 doi: 10.1016/j.jsat.2020.108163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri U.G., Perrone J. Opioid use disorder and COVID-19: crashing of the crises. J. Addict. Med. 2020;14:6. doi: 10.1097/ADM.0000000000000684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C.-C.C., Dievler A., Robbins C., Sripipatana A., Quinn M., Nair S. Telehealth in health centers: key adoption factors, barriers, and opportunities. Health Aff. 2018;37(12):1967–1974. doi: 10.1377/hlthaff.2018.05125. [DOI] [PubMed] [Google Scholar]
- Nicholas J., Bell I.H., Thompson A., Valentine L., Simsir P., Sheppard H., Adams S. Implementation lessons from the transition to telehealth during COVID-19: a survey of clinicians and young people from youth mental health services. Psychiatry Res. 2021;299 doi: 10.1016/j.psychres.2021.113848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J. Am. Med. Inform. Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA 2020a. Opioid Treatment Program (OTP) Guidance . (Accessed 29 March 2021) 〈https://www.samhsa.gov/sites/default/files/otp-guidance-20200316.pdf〉.
- SAMHSA 2020b. FAQs Provision of methadone and buprenorphine for the treatment of Opioid Use Disorder in the COVID-19 emergency . (Accessed 29 March 2021) 〈https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf〉.
- SAMHSA 2021. Medication-Assisted Treatment (MAT) . (Accessed 29 March 2021) 〈https://www.samhsa.gov/medication-assisted-treatment〉.
- Stata Statistical Software: 2019. Release 16. StataCorp LLC, College Station, TX (2019).
- Suzanne Bakken Telehealth: simply a pandemic response or here to stay? J. Am. Med. Inform. Assoc. 2020;27(Issue 7):989–990. doi: 10.1093/jamia/ocaa132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J., Fudim M., Cameron B., Gellad Z.F., Cho A., Phinney D., Curtis S., Roman M., Poon E.G., Ferranti J., Katz J.N., Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]