Abstract
Introduction:
The co-occurrence of posttraumatic stress disorder (PTSD) and alcohol misuse presents a significant clinical concern among military veterans. Fear of self-compassion, the active resistance to thinking and behaving compassionately toward oneself, may be an important consideration that underlies this relation.
Objective:
The current investigation examined whether self-compassion and fear of self-compassion, separately, mediated the association between PTSD symptoms and alcohol misuse among a sample of military veterans.
Method:
Data were collected from 203 military veterans (M age = 35.08 years, 77.70% male, 72.2% White) who responded to an online survey.
Results:
The findings indicated that both self-compassion and fear of self-compassion significantly explained the association between PTSD symptoms and alcohol misuse. Furthermore, fear of self-compassion explained this relation after adjusting for levels of self-compassion.
Conclusions:
These results suggest that both self-compassion and a fear of self-compassion may be important considerations in the PTSD-alcohol misuse relation; future work should extend these findings in longitudinal and intervention frameworks.
Keywords: posttraumatic stress disorder symptoms, self-compassion, fear of self-compassion, alcohol misuse, military
The co-occurrence of posttraumatic stress disorder (PTSD) and problematic alcohol use is common (Debell et al., 2014; Jacobsen, Southwick, & Kosten, 2001; Lai, Cleary, Sitharthan, & Hunt, 2015) and affects a disproportionate number of military veterans (Seal et al., 2011). Prevalence rates suggest that military veterans are significantly more likely than the general population to be diagnosed with PTSD (23% and 8%, respectively; Fulton et al., 2015; Kilpatrick et al., 2013) and to screen positive for lifetime alcohol abuse/dependence (42.4% and 30.3%, respectively; Fuehrlein et al., 2016; Grant et al., 2015; Hasin, Stinson, Ogburn, & Grant, 2007). Notably, treatment-seeking veterans diagnosed with PTSD are approximately 4 times as likely to also be diagnosed with an alcohol use disorder (Seal et al., 2011). Veterans with comorbid PTSD and alcohol misuse experience significantly greater impairment, including greater disorder severity, social and occupational dysfunction, and suicidality, as compared with those who experience either disorder alone (Bowe & Rosenheck, 2015; Fuehrlein et al., 2016; Norman, Haller, Hamblen, Southwick, & Pietrzak, 2018). The above findings suggest that there is a need to identify mechanisms that underlie this PTSD-alcohol misuse relation, particularly to understand factors that increase alcohol use risk among veterans with PTSD symptoms. Self-compassion, and the fear of self-compassion, are worth considering in this regard because both refer to how someone treats themselves during difficult times. Thus, the goal of the current study is to examine whether self-compassion and fear of self-compassion explain the PTSD-alcohol misuse relation among military veterans.
Self-compassion refers to an adaptive tendency to approach oneself and emotional experiences with nonjudgmental understanding and acceptance as well as the ability to recognize that hardship and personal setbacks are a shared part of the common human experience (Neff, 2003). Accordingly, self-compassion is comprised of three interrelated positive qualities (self-kindness, mindfulness, and common humanity), and the absence of three negative counterparts (self-judgment, overidentification, and isolation). The positive responses are considered adaptive because they reflect compassionate ways of relating to oneself in the context of difficult life situations, including treating oneself with warmth and kindness, taking a balanced emotional perspective, and acknowledging the shared human experience. Self-compassion has been theoretically and empirically linked with a wide range of mental health benefits (Neff, Kirkpatrick, & Rude, 2007; Trompetter, de Kleine, & Bohlmeijer, 2017) and has been identified as an important therapeutic target (Galili-Weinstock et al., 2018; Germer & Neff, 2013; MacBeth & Gumley, 2012). A growing body of work has demonstrated the protective capacity of self-compassion following traumatic exposure (Thompson & Waltz, 2008; Zeller, Yuval, Nitzan-Assayag, & Bernstein, 2015); conceptually, self-compassion may soothe the threat response, offset the formation of self-critical or shame-based assumptions, and promote a greater willingness to approach painful or distressing trauma-related emotions (Germer & Neff, 2015). Consistent with this proposition, self-compassion has been found to be associated with lower PTSD symptom severity (Hiraoka et al., 2015; Kearney et al., 2013), and interventions aimed at increasing self-compassion and reducing PTSD symptoms have shown efficacy among military veterans (Kearney et al., 2013).
Although the benefits of self-compassion are clear, not everyone engages in these adaptive ways of self-relating, and some individuals tend to respond to difficult situations in ways that reflect the negative counterparts of self-compassionate responding. Specifically, these individuals respond to hardship with judgmental and harsh self-criticism, interpret the experience as isolating, and overidentify with negative emotions. Indeed, this way of responding has been found to be associated with negative mental health outcomes (Gilbert, McEwan, Matos, & Rivis, 2011; López et al., 2015; Muris & Petrocchi, 2017) and has been implicated in the maintenance of PTSD (Hoffart, Øktedalen, & Langkaas, 2015).
This uncompassionate way of responding may not be due to an inability to be self-compassionate but instead may reflect a fear of self-compassion. Fear of self-compassion involves the active resistance to thinking and behaving compassionately toward oneself and includes fears associated with feeling undeserving, viewing compassion as a weakness, lack of familiarity/consideration for the importance of compassion, and/or concern for the potential implications of being too compassionate toward oneself (e.g., lowering personal standard, exposing flaws; Gilbert et al., 2011). Fear of self-compassion and self-compassion are overlapping yet distinct constructs. For instance, individuals may have low levels of self-compassion and not fear being self-compassionate. Thus, fear of self-compassion is an important consideration in mental health because compassion has been proposed to deactivate psychological and biological threat systems, and stimulate the self-soothing system (associated with safety and security; Gilbert & Irons, 2005), which is one explanation for the emotion-regulating capacity of self-compassion (Finlay-Jones, Rees, & Kane, 2015; Neff, 2003). Empirically, self-compassion has been found to be inversely related to emotion dysregulation, and emotion dysregulation has been found to mediate the relation between self-compassion and mental health outcomes (Inwood & Ferrari, 2018), including PTSD symptom severity (Scoglio et al., 2018). Thus, individuals who are fearful of self-compassion, and actively resist behaving compassionately, may find it difficult to regulate emotions. Consistent with this proposition, fear of self-compassion has been associated with various negative mental health outcomes (Gilbert, McEwan, Catarino, Baião, & Palmeira, 2014; Joeng & Turner, 2015; Joeng et al., 2017; Xavier, Gouveia, & Cunha, 2016), including PTSD symptom severity (Miron, Sherrill, & Orcutt, 2015; Miron, Seligowski, Boykin, & Orcutt, 2016).
Fear of Self-Compassion and PTSD
Conceptually, fear of self-compassion and PTSD symptoms may relate to one another in two important ways. First, fear of self-compassion may be caused by trauma-induced changes to schematic belief systems (consistent with social-cognitive models; Janoff-Bulman, 1992; Ehlers & Clark, 2000; Park, Mills, & Edmondson, 2012), resulting in a set of beliefs that are inconsistent with a self-compassionate perspective. Specifically, trauma exposes individuals to unprecedented life events, and as a result they undergo processes of assimilation and/or accommodation (Joseph & Linley, 2005; Payne, Joseph, & Tudway, 2007). During these processes, individuals may adopt extreme beliefs about the self, such as an extremely negative and/or critical self-views, including the belief that they are undeserving of kindness (i.e., an overaccommodated belief). These individuals may then perceive aspects of self-compassion to be incompatible with their new belief system and therefore may actively resist self-compassion because behaving compassionately would be in direct conflict with their schematic sense of self (as described by Miron et al., 2016).
Alternatively, deficits in the ability to self-soothe (a potential benefit of self-compassion; Gilbert & Irons, 2005) may motivate extreme posttraumatic reactions. Self-compassion has been posited to activate the self-soothing system, which may reduce the overwhelming negative emotions that can arise following difficult experiences (Gilbert & Irons, 2005). In the context of trauma, individuals who fear self-compassion may experience a greater challenge moderating these trauma-related emotions. Inability to regulate these emotions may result in more severe posttraumatic reactions, potentially motivating maladaptive ways of responding (e.g., alcohol use). Importantly, fear of self-compassion may be particularly pronounced in military veterans. The military culture socializes service members to value qualities that can be incompatible with self-compassion such as emotional control, stoicism, and invulnerability (McAllister, Callaghan, & Fellin, 2019). Thus, military members may find it more difficult to respond compassionately to oneself when faced with hardship and may actively resist this behavior because it may be viewed as inconsistent with expectations of military culture.
Fear of Self-Compassion and Alcohol Misuse
Regarding the relation between fear of self-compassion and alcohol use, alcohol use may function to suppress aversive experiential states that arise via failures to self-soothe, which is consistent with the tension-reduction theory (Conger, 1956). Specifically, internal tension may arise from fear of self-compassion, coupled with PTSD symptomology. The tension-reduction theory suggests that people drink to reduce tension, and this pattern of use may be negatively reinforcing because it may help a person avoid unwanted experiences, leading to repeated use (Conger, 1956). Furthermore, according to the self-awareness model of the causes and effects of alcohol consumption, drinking may be utilized to reduce access to self-relevant information (Hull, 1981). Specifically, alcohol’s interference with higher-order cognitive processes, such as those that are involved in processing self-relevant information, can, in turn, reduce awareness of self, and associated critical self-thoughts and associated distress. Therefore, alcohol consumption may be motivated, and reinforced, by the desire to avoid self-critical thoughts and feelings associated with fear of self-compassion. Consistent with theory, empirical research has indicated that self-compassion appears to prevent/reduce problematic alcohol use because self-compassion has been found to be associated with lower rates of alcohol misuse among college students (Miron, Orcutt, Hannan, & Thompson, 2014) and trauma-exposed individuals (Miron et al., 2014; Tanaka, Wekerle, Schmuck, Paglia-Boak, & MAP Research Team, 2011) and is inversely related to disorder severity among individuals seeking treatment for substance use (Vettese, Dyer, Li, & Wekerle, 2011), thus suggesting a protective role of self-compassion in relation to patterns of alcohol misuse. Therefore, presumably, individuals who fear self-compassion will not have the protective benefits of self-compassion.
The Present Study
There is a well-known link between PTSD and alcohol misuse, and the co-occurrence of these conditions has been associated with more severe posttraumatic outcomes (Dass-Brailsford & Myrick, 2010; Jacobsen et al., 2001; Norman, Tate, Anderson, & Brown, 2007; Ouimette, Goodwin, & Brown, 2006; Read, Brown, & Kahler, 2004), especially among military veterans (Bowe et al., 2015; Norman et al., 2018), emphasizing the need for research focused on mechanisms that underlie this relationship among military samples. Given the relation between fear of self-compassion to PTSD symptoms (Miron et al., 2015; Miron et al., 2016), and the inverse relation between self-compassion and alcohol use (Miron et al., 2014; Tanaka et al., 2011), we tested two hypotheses. First, we hypothesized that at the bivariate level, fear of self-compassion would significantly and positively relate to both PTSD symptoms and alcohol misuse, self-compassion would negatively relate to both PTSD symptoms and alcohol misuse, and self-compassion and fear of self-compassion would be significantly negatively related but reflect distinct constructs in our sample. Consistent with the theoretical benefits of self-compassion, our second hypothesis was that self-compassion would explain the PTSD symptom-alcohol misuse relation, such that higher PTSD symptoms would be related to lower self-compassion, which, in turn, would be associated with greater alcohol misuse. Extending this work, our last hypothesis was that fear of self-compassion would explain the PTSD-alcohol misuse relation after adjusting for self-compassion, such that PTSD would be associated with higher fear of self-compassion, which would relate to greater alcohol misuse.
Method
Participants and Procedures
We collected data on 203 military veterans via an online survey. The survey was advertised on Amazon’s Mechanical Turk (MTurk) platform, which is an Internet marketplace capable of generating reliable data (Mishra & Carleton, 2017). The study was advertised as a survey about military combat experiences and moral, emotional, and psychological well-being. Interested participants clicked on the advertisement to learn more about the study. A link was provided to direct participants to an external survey, in which they were asked to read through the informed consent. Interested individuals that self-identified as military veterans (as indicated in the consent form), were then instructed to click the next button indicating that they agreed to participate. Participants were then directed to a prescreen questionnaire. Participants had to be at least 18 years old, proficient in the English language, served in the United States military, and deployed to either Afghanistan or Iraq in support of recent operations. Military status was verified using a series of validations measures. Specifically, participants were asked to respond to basic questions about their military service, including their branch of service, time in service, and number of deployments. Individuals that indicated that they had no prior military service or selected 0 for the number of deployments were not eligible to participate. Participants then responded to questions that are generally not common knowledge to civilians (e.g., “What is the acronym for the locations where final physicals are taken prior to shipping off for basic training?”), which have been used in previous MTurk studies with military veterans (Lynn & Morgan, 2016). To further ensure the quality of data, attention checks were included throughout the survey to ensure participants were attentively reading and responding to the questions being asked (e.g., “Please select the color red from the options given”). Participants who failed to correctly respond to these attention checks were excluded from the study. Participants were compensated $2.00 for their participation.
Following data collection, we carefully evaluated the data. In total, 696 people accessed the survey. Based on the prescreen questions, 431 were ineligible for the study (n = 265), and 62 failed attention checks (n = 203). The final sample included 203 Iraq and Afghanistan veterans, with ages ranging from 21 to 63 years (M = 35.05, SD = 8.09). The majority of the sample reported being male (n = 157, 77.70%) and White (n = 143, 72.20%). Most reported serving in the Army (n = 106, 52.20%), with the majority of the sample indicating that they were active duty (n = 173, 85.20%). These study procedures were approved by the author’s institutional review board.
Measures
PTSD symptoms.
The PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (PCL-5; Weathers et al., 2013) is a 20-item self-report measure used to assess PTSD symptoms. Participants responded to a series of questions that correspond to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, criteria for PTSD. Participants were asked to indicate how often they have been bothered by each of the symptoms over the past month, in reference to a deployment-related traumatic event. Responses are given on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). A total score was calculated by summing all the items, with higher scores indicating greater PTSD symptom severity. The PCL-5 has shown good internal consistency and convergent and discriminant validity (Blevins, Weathers, Davis, Witte, & Domino, 2015). In the current study, the PCL-5 demonstrated excellent reliability (α = .97).
Alcohol misuse.
The Alcohol Use Disorders Identification Test (AUDIT; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998) is a 10-item self-report measure used to assesses alcohol consumption, behaviors, and problems, with responses scored between 0 and 4. A total score is calculated by summing all the items, with higher scores indicating greater alcohol misuse. The AUDIT has demonstrated good test-retest reliability and internal consistency (Searle et al., 2015), including in the current study (α = .91).
Fear of self-compassion.
Fear of self-compassion is measured using a 15-item self-report scale assessing fears related to the expression of kindness and compassion towards oneself (Gilbert et al., 2011). Responses are given on a 5-point scale ranging from 0 (do not agree at all) to 4 (completely agree). A total score is obtained by summing all items. Higher scores represent a greater fear of being self-compassionate. This scale has demonstrated excellent internal consistency, with a Cronbach’s alpha of α = .97.
Self-Compassion.
The Self-Compassion Scale (Neff, 2003) is a 26-item self-report measure assessing individuals across positive (self-kindness, mindfulness, and common humanity) and negative qualities (self-judgment, overidentification, and isolation). Responses are given on a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always). For the purpose of this study, a total score was computed by summing all the items. Higher scores indicate greater self-compassion. Reliability in the current study was excellent (α = .90).
Data Analysis
Preliminary analyses were conducted to examine for covariates to be included in the analysis and obtain descriptive and demographic information and intercorrelations among the primary study variables.
For the primary analyses, multiple mediation models were tested. The first model examined the direct and indirect associations among PTSD symptoms, self-compassion, and alcohol misuse. The second model examined the direct and indirect associations among PTSD symptoms, fear of self-compassion, and alcohol misuse. The third model examined the direct and indirect associations among PTSD symptoms, fear of self-compassion, and alcohol misuse after adjusting for self-compassion. Self-compassion was included as a covariate in this third mediation model to ensure that the relations were specific to fear of self-compassion rather than simply reflecting levels of self-compassion.
In these models, PTSD symptoms were included as the predictor (X), alcohol misuse as the outcome (Y), and self-compassion and fear of self-compassion, separately, were entered as the mediating variables (M). In these models, the a path represents the association between the predictor (PTSD symptoms) and the mediators (self-compassion or fear of self-compassion). The b path represents the associations between the mediator variable and the outcome variable (alcohol misuse). The c′ path represent the direct path from the predictor to the outcome while controlling for the indirect relations in the model.
This mediation model was examined using the SPSS macro PROCESS (Model 4; Hayes, 2012). Bootstrapping was done with 5,000 random samples generated from the observed covariance matrix to estimate 95% confidence intervals and significance values. Mediation is considered to be significant if the upper and lower bounds of the 95% confidence interval does not contain zero (Preacher & Hayes, 2004).
Results
Descriptive Data
Intercorrelations among the primary variables are presented in Table 1. Fear of self-compassion was significantly and positively associated with both PTSD symptoms and alcohol misuse. Self-compassion was significantly and negatively associated with PTSD symptoms, alcohol misuse, and fear of self-compassion. PTSD symptoms were significantly and positively associated with alcohol misuse.
Table 1.
Intercorrelations Among Primary Variables
| Variables | 1 | 2 | 3 | 4 | M (SD) |
|---|---|---|---|---|---|
|
| |||||
| 1. PCL-5, PTSD symptoms | — | — | — | — | 28.47 (22.27) |
| 2. AUDIT, alcohol misuse | .490*** | — | — | — | 10.39 (9.14) |
| 3. Fear of self-compassion | .603*** | .567*** | — | — | 19.29 (16.72) |
| 4. Self-compassion | −.288*** | −.267*** | −.535*** | — | 80.23 (19.50) |
Note. PCL-5 = PTSD Checklist DSM-5; AUDIT = Alcohol Use Disorder Identification Test.
p < .001.
The first mediation model (see Figure 1 and Table 2) revealed that PTSD symptoms were significantly associated with self-compassion (a path), self-compassion was significantly associated with alcohol misuse (b path), and PTSD symptoms were significantly associated with alcohol misuse (c path). Furthermore, the indirect association was significant. However, the direct association (c′ path) remained significant after controlling for the indirect relations in the model; this suggests partial mediation.
Figure 1.
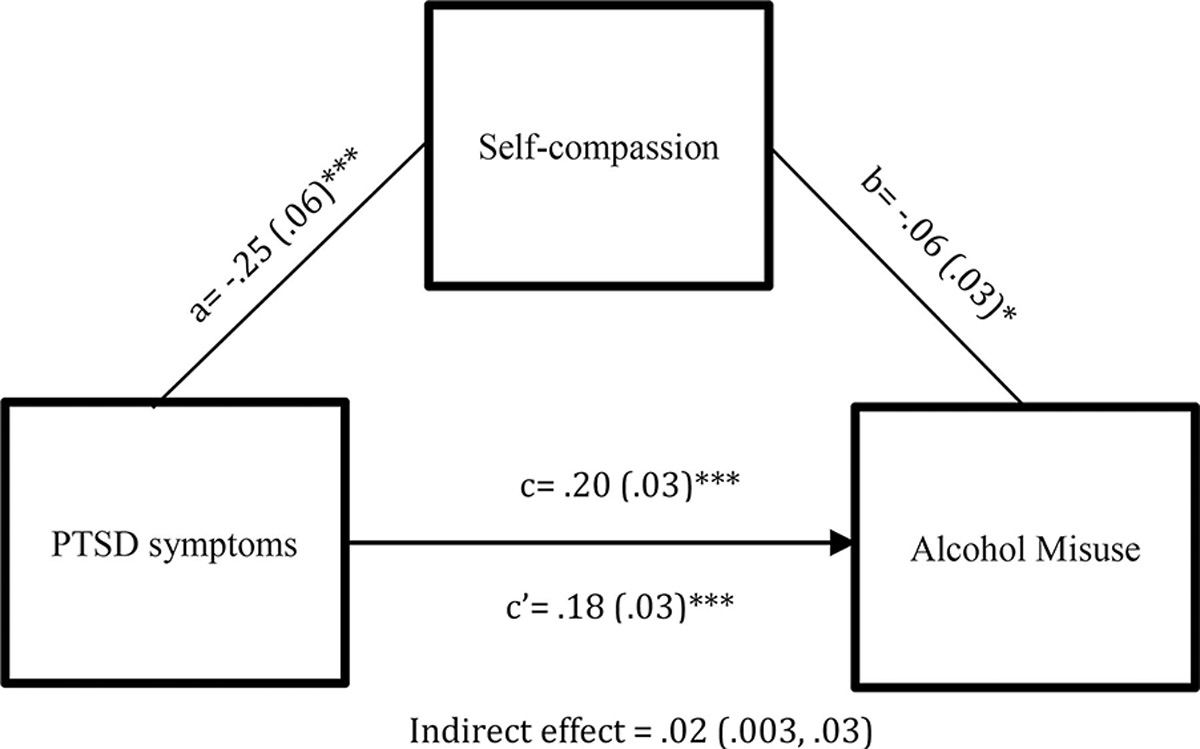
PTSD symptoms on alcohol misuse through self-compassion. PTSD = posttraumatic stress symptoms. * p < .05. *** p < .001.
Table 2.
Summary of Mediational Analyses
| Paths | Unstandardized coefficient (B) | SE | t | p value |
|
| ||||
| Model 1 | ||||
| PTSD symptoms → self-compassion (a) | −.2545 | .0596 | −4.2378 | <.0001 |
| Self-compassion → alcohol misuse (b) | −.0648 | .0300 | −2.1599 | .0320 |
| PTSD symptoms → alcohol misuse (c′) | .1835 | .0263 | 6.9764 | <.0001 |
| Model 3 | ||||
| PTSD symptoms → fear of self-compassion (a) | .3654 | .0400 | 9.1267 | <.0001 |
| Fear of self-compassion → alcohol misuse (b) | .2336 | .0441 | 5.2944 | <.0001 |
| PTSD symptoms → alcohol misuse (c′) | .1011 | .0293 | 3.4487 | .0007 |
|
| ||||
| Indirect paths | Unstandardized coefficient (B) | SE | BootLLCI | BootULCI |
|
| ||||
| Model 1 | ||||
| Self-compassion (a × b) | .0164 | .0074 | .0025 | .0320 |
| Model 3 | ||||
| Fear of self-compassion (a × b) | .0854 | .0189 | .0519 | .1250 |
Note. PTSD = posttraumatic stress disorder symptoms; BootLLCI = Bootstrapping lower limit confidence interval; BootULCI = Bootstrapping upper limit confidence interval. Model 3 is adjusted for self-compassion.
The second and third mediation models revealed that PTSD symptoms were significantly associated with fear of self-compassion (a path), fear of self-compassion was significantly associated with alcohol misuse (b path), and PTSD symptoms were significantly associated with alcohol misuse (c path). Furthermore, the indirect association was significant. However, the direct association (c′ path) remained significant after controlling for the indirect relations in the model; this suggests partial mediation. These findings remained the same after adjusting for levels of self-compassion. We present the third model (see Figure 2 and Table 2).
Figure 2.
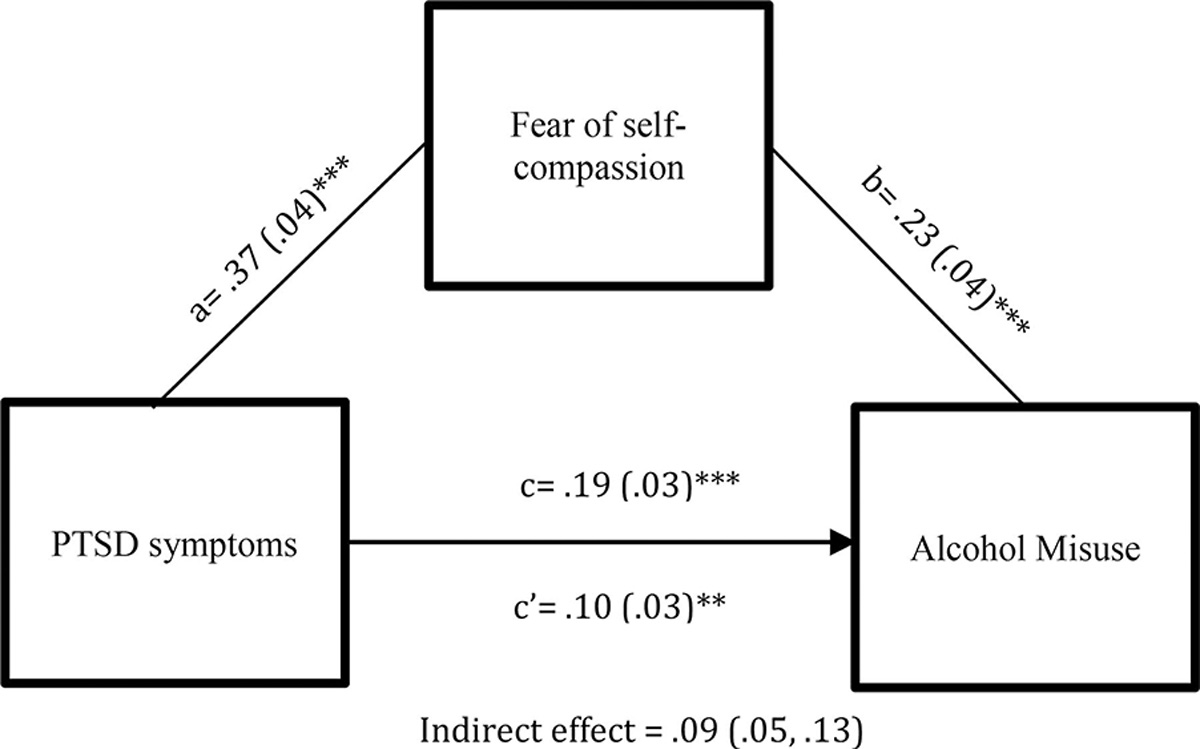
PTSD symptoms on alcohol misuse through fear of self-compassion. Results are adjusted for self-compassion. PTSD = posttraumatic stress symptoms. ** p < .01. *** p <.001.
Discussion
The goal of this study was to examine the relations among PTSD symptoms, self-compassion, fear of self-compassion, and alcohol misuse among a sample of military veterans. Our results suggest that both self-compassion and fear of self-compassion, separately, mediated the association between PTSD symptoms and alcohol misuse. However, fear of self-compassion explained the PTSD-alcohol misuse, even when controlling for levels of self-compassion, suggesting that fear of self-compassion’s role in this relation is distinct and does not simply reflect levels of self-compassion. These findings offer preliminary support for the clinical relevance of both self-compassion and fear of self-compassion in the co-occurrence of PTSD and alcohol misuse. Furthermore, our findings suggest that self-compassion may be an important target for preventing or treating alcohol misuse among military veterans experiencing PTSD symptoms, although additional research would be needed to further examine these relations using intervention and longitudinal investigations.
Consistent with our hypothesis, both self-compassion and fear of self-compassion significantly explained the association between PTSD symptoms and alcohol misuse. This finding is consistent with cognitive models of PTSD that suggest trauma can result in the formation of more critical self-appraisals because individuals may experience shifts in beliefs about oneself following a traumatic event and the development of PTSD (Foa, Ehlers, Clark, Tolin, & Orsillo, 1999; Ehlers et al., 2000), and these compromised perceptions of self can lead to a current sense of threat, which can exacerbate and maintain posttraumatic symptomology (Ehlers et al., 2000). Both low levels of self-compassion and a fear of self-compassion can be conceptualized as reflecting a type of self-criticism because low levels of self-compassion can involve treating oneself with critical self-judgment, and fear of self-compassion can involve resisting self-kindness following difficult experiences (Gilbert et al., 2011; López et al., 2015; Neff, 2003). Our mediational framework suggests that the association between PTSD, self-compassion, and fear of self-compassion extends to greater alcohol misuse. This finding is consistent with the self-awareness model of the causes and effects of alcohol consumption (Hull, 1981), which suggests that attempts to reduce self-relevant information (such as critical self-evaluations that are inherent to fear of self-compassion) may motivate and reinforce alcohol use. Furthermore, this lack of self-compassionate responding or fear of self-compassion in the context of PTSD symptoms may make self-soothing difficult, thus exacerbating aversive experiential states and the use of alcohol to reduce the tension associated with these experiences (Conger, 1956).
Overall, our findings suggest that both self-compassion and fear of self-compassion are associated with PTSD symptoms and greater alcohol misuse, underscoring the potential clinical utility of assessing both levels of self-compassion and attitudes toward self-compassion in military veterans. Such information could help identify trauma-exposed individuals at heightened risk for both PTSD and alcohol misuse. Furthermore, fear of self-compassion corresponds with different forms of self-critical tendencies (e.g., feeling undeserving of compassion, fearing implications of being compassionate), which may be important targets for treatment. Reductions in certain forms of self-critical assumptions (e.g., blame) have been associated with reductions in posttrauma symptoms (Holliday, Holder, & Surís, 2018), and this finding may extend to these other forms of self-criticism. Cognitive-processing therapy (Resick & Schnicke, 1992), a treatment for PTSD that targets dysfunction cognitions regarding the trauma (Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick et al., 2008), may be especially useful for individuals who are higher in self-critical tendencies related to fear of self-compassion. Future research would benefit from examining whether cognitive-processing therapy results in reductions of these specific tendencies and whether these reductions result in consequent improvements in PTSD and alcohol misuse symptoms from pre to posttreatment.
Although reducing self-critical tendencies that accompany fear of self-compassion could be an important therapeutic target, it may be useful to not only decrease these negative qualities, but also increase positive qualities of being self-compassionate, and specifically to increase the degree to which people feel comfortable (rather than fearful) about expressing self-compassion. Self-compassion is an important target for research because it has been found to be modifiable (Beaumont, Jenkins, & Galpin, 2012; Kearney et al., 2013; Neff & Germer, 2013). Prior research has indicated that self-compassion is an adaptive strategy (Neff, 2003) that has important implications for mental health and well-being (MacBeth & Gumley, 2012) and has shown relevance among trauma-exposed population (Hoffart et al., 2015; Zeller et al., 2015). Self-compassion interventions have shown to be efficacious in increasing levels of self-compassion (Neff & Germer, 2013) and reducing mental health symptoms (Wilson, Mackintosh, Power, & Chan, 2018), including PTSD symptoms among military veterans (Kearney et al., 2013). Current interventions utilize aspects of self-compassion (i.e., increasing mindfulness and acceptance), such as acceptance and commitment therapy (ACT; Hayes, Strosahl, & Wilson, 2012), and newer treatments are more compassion oriented, such as compassion-focused therapy (Gilbert, 2010) and mindful self-compassion (Neff & Germer, 2013). To our knowledge, compassion-focused therapy and mindful self-compassion have yet to be studied in relation to PTSD and alcohol misuse, and more research is needed to determine whether these are plausible treatment options. Recent studies have shown that ACT has been effective at increasing levels of self-compassion (Yadavaia, Hayes, & Vilardaga, 2014), and there has been some research on using ACT for both PTSD and alcohol use separately (e.g., Boals & Murrell, 2016; Lang et al., 2017; Thekiso et al., 2015); however, research has recommended that integrated treatments for PTSD and alcohol use disorders (AUDs) are preferred when co-occurrence is present (Management of Post-Traumatic Stress Working Group, 2010) because they share common features (Jacobsen et al., 2001). Recently a pilot study using ACT to treat PTSD-AUD among military veterans successfully reduced both PTSD and alcohol symptoms (Meyer et al., 2018).
ACT, which utilizes aspects of self-compassion (Neff & Tirch, 2013) may provide peripheral support for the utility of self-compassion in treating PTSD-AUD among military veterans. However, more research is needed on teaching individuals with PTSD and AUD how to behave self-compassionately and testing whether this specific skill results in increases in self-compassion and reductions in fear of self-compassion as well as subsequent reductions in PTSD and alcohol misuse symptoms. Skill training focused on self-compassion for these populations may offset the formation of self-critical appraisals that can maintain PTSD (Ehlers et al., 2000) but also teach individuals with PTSD how to develop a self-compassionate orientation, which may be able to help them improve the ability to self-soothe, cope with future adversity, and manage distress in more adaptive ways (vs. using alcohol).
Several limitations should be considered when interpreting the study findings. The use of a cross-sectional design precludes the ability to make claims of causality. Thus, our findings suggest only associations among PTSD symptoms, self-compassion, fear of self-compassion, and alcohol misuse. Future work should incorporate prospective and longitudinal assessment to gain insight into the direction of these associations. An additional limitation is the data were collected using self-report assessments, and therefore, the responses may be subject to response biases (e.g., socially desirable responding). Furthermore, the use of self-report may be limited by the insight and/or willingness of the participants to respond accurately. Future research should incorporate additional methods of assessment to reduce the limitations of self-report assessments and add to the validity of the findings. Our use of MTurk further limits our findings because the sample was restricted to individuals who have knowledge of, and access to, the MTurk platform. Additionally, considering this was a volunteer-based study, individuals had to self-select to participate; thus, there may be characteristics that systematically differ between the individuals that chose to participate versus those who did not. This volunteer bias can influence the generalizability of research findings; thus, more research is needed to replicate these findings using diverse recruitment strategies. Furthermore, our use of a military sample using MTurk makes it difficult to generalize the findings to other military samples (e.g., treatment seeking, active duty). Future studies should replicate and extend these findings using other military samples (e.g., treatment seeking) and more diverse trauma-exposed populations to extend the generalizability of current study findings.
Despite these limitations, our findings contribute to the larger literature on self-compassion and mental health, specifically on PTSD and alcohol misuse among military veterans. This is the first study to examine self-compassion and fear of self-compassion in relation to both PTSD and alcohol misuse in a sample of military veterans. Examining these associations lends support to the potential use of incorporating self-compassion into treatments for veterans experiencing PTSD and alcohol misuse symptoms, pending further research. Overall, our findings suggest that fear of self-compassion is associated with both PTSD and alcohol misuse and appears to play a role in the PTSD-alcohol misuse relation. As such, our findings underscore the importance of more research on the clinical utility of self-compassion in military mental health.
Clinical Impact Statement.
Individuals that experience both posttraumatic stress disorder (PTSD) and alcohol misuse have been shown to experience more negative mental health consequences. This study examined whether fear of self-compassion (the active resistance to treating oneself compassionately) explained the relation between PTSD and alcohol misuse. Self-compassion is considered to be protective against negative mental health consequences; thus, resisting self-compassion could partially explain the relation between PTSD and alcohol misuse. We found that greater PTSD symptoms were associated with greater fears of self-compassion, which was associated with greater alcohol misuse. This study highlights the importance of addressing fear of self-compassion in this relation.
Acknowledgments
Work on this paper by Nicole H. Weiss was supported by National Institute on Drug Abuse Grants K23DA039327.
References
- Beaumont EA, Jenkins P, & Galpin AJ (2012). ‘Being kinder to myself’: A prospective comparative study, exploring post-trauma therapy outcome measures, for two groups of clients, receiving either cognitive behaviour therapy or cognitive behaviour therapy and compassionate mind training. Counselling Psychology Review, 27, 31–43. [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Boals A, & Murrell AR (2016). I am > trauma: Experimentally reducing event centrality and PTSD symptoms in a clinical trial. Journal of Loss and Trauma, 21, 471–483. 10.1080/15325024.2015.1117930 [DOI] [Google Scholar]
- Bowe A, & Rosenheck R (2015). PTSD and substance use disorder among veterans: Characteristics, service utilization and pharmacotherapy. Journal of Dual Diagnosis, 11, 22–32. 10.1080/15504263.2014.989653 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine, 158, 1789–1795. [DOI] [PubMed] [Google Scholar]
- Conger JJ (1956). Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol, 17, 296–305. [PubMed] [Google Scholar]
- Dass-Brailsford P, & Myrick AC (2010). Psychological trauma and substance abuse: The need for an integrated approach. Trauma, Violence, & Abuse, 11, 202–213. [DOI] [PubMed] [Google Scholar]
- Debell F, Fear NT, Head M, Batt-Rawden S, Greenberg N, Wessely S, & Goodwin L (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49, 1401–1425. 10.1007/s00127-014-0855-7 [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Finlay-Jones AL, Rees CS, & Kane RT (2015). Self-compassion, emotion regulation and stress among Australian psychologists: Testing an emotion regulation model of self-compassion using structural equation modeling. PLoS ONE, 10, e0133481. 10.1371/journal.pone.0133481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. [Google Scholar]
- Fuehrlein BS, Mota N, Arias AJ, Trevisan LA, Kachadourian LK, Krystal JH, . . . Pietrzak RH (2016). The burden of alcohol use disorders in U.S. military veterans: Results from the National Health and Resilience in Veterans Study. Addiction, 111, 1786–1794. 10.1111/add.13423 [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, . . . Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Galili-Weinstock L, Chen R, Atzil-Slonim D, Bar-Kalifa E, Peri T, & Rafaeli E (2018). The association between self-compassion and treatment outcomes: Session-level and treatment-level effects. Journal of Clinical Psychology, 74, 849–866. 10.1002/jclp.22569 [DOI] [PubMed] [Google Scholar]
- Germer CK, & Neff KD (2013). Self-compassion in clinical practice. Journal of Clinical Psychology, 69(8), 856–867. [DOI] [PubMed] [Google Scholar]
- Germer CK, & Neff KD (2015). Cultivating self-compassion in trauma survivors. In Follette VM, Briere J, Rozelle D, Hopper JW, & Rome DI (Eds.), Mindfulness-oriented interventions for trauma: Integrating contemplative practices (pp. 43–58). New York, NY: The Guilford Press. [Google Scholar]
- Gilbert P (2010). The CBT distinctive features series. Compassion focused therapy: Distinctive features. New York, NY: Routledge/Taylor & Francis Group. [Google Scholar]
- Gilbert P, & Irons C (2005). Focused therapies and compassionate mind training for shame and self-attacking. In Gilbert P (Ed.), Compassion: Conceptualisations, research and use in psychotherapy (pp. 263–325). New York, NY: Routledge. [Google Scholar]
- Gilbert P, McEwan K, Catarino F, Baião R, & Palmeira L (2014). Fears of happiness and compassion in relationship with depression, alexithymia, and attachment security in a depressed sample. British Journal of Clinical Psychology, 53, 228–244. 10.1111/bjc.12037 [DOI] [PubMed] [Google Scholar]
- Gilbert P, McEwan K, Matos M, & Rivis A (2011). Fears of compassion: Development of three self-report measures. Psychology and Psychotherapy: Theory, Research and Practice, 84, 239–255. 10.1348/147608310X526511 [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, . . . Hasin DS (2015). Epidemiology of DSM–5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. Journal of the American Medical Association Psychiatry, 72, 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, & Grant BF (2007). Prevalence, correlates, disability, and comorbidity of DSM–IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64, 830–842. 10.1001/archpsyc.64.7.830 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf
- Hayes SC, Strosahl KD, & Wilson KG (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Hiraoka R, Meyer EC, Kimbrel NA, DeBeer BB, Gulliver SB, & Morissette SB (2015). Self-compassion as a prospective predictor of PTSD symptom severity among trauma-exposed US Iraq and Afghanistan war veterans. Journal of Traumatic Stress, 28(2), 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffart A, Øktedalen T, & Langkaas TF (2015). Self-compassion influences PTSD symptoms in the process of change in trauma-focused cognitive-behavioral therapies: A study of within-person processes. Frontiers in Psychology, 6, 1273. 10.3389/fpsyg.2015.01273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holliday R, Holder N, & Surís A (2018). Reductions in self-blame cognitions predict PTSD improvements with cognitive processing therapy for military sexual trauma-related PTSD. Psychiatry Research, 263, 181–184. [DOI] [PubMed] [Google Scholar]
- Hull JG (1981). A self-awareness model of the causes and effects of alcohol consumption. Journal of Abnormal Psychology, 90, 586–600. 10.1037/0021-843X.90.6.586 [DOI] [PubMed] [Google Scholar]
- Inwood E, & Ferrari M (2018). Mechanisms of change in the relationship between self-compassion, emotion regulation, and mental health: A systematic review. Applied Psychology: Health and Well-Being, 10, 215–235. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, & Kosten TR (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry, 158, 1184–1190. 10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R (1992). Shattered assumptions: Towards a new psychology of trauma. New York, NY: The Free Press. [Google Scholar]
- Joeng JR, & Turner SL (2015). Mediators between self-criticism and depression: Fear of compassion, self-compassion, and importance to others. Journal of Counseling Psychology, 62, 453–463. 10.1037/cou0000071 [DOI] [PubMed] [Google Scholar]
- Joeng JR, Turner SL, Kim EY, Choi SA, Lee YJ, & Kim JK (2017). Insecure attachment and emotional distress: Fear of self-compassion and self-compassion as mediators. Personality and Individual Differences, 112, 6–11. 10.1016/j.paid.2017.02.048 [DOI] [Google Scholar]
- Joseph S, & Linley PA (2005). Positive adjustment to threatening events: An organismic valuing theory of growth through adversity. Review of General Psychology, 9, 262–280. 10.1037/1089-2680.9.3.262 [DOI] [Google Scholar]
- Kearney DJ, Malte CA, McManus C, Martinez ME, Felleman B, & Simpson TL (2013). Loving-kindness meditation for posttraumatic stress disorder: A pilot study. Journal of Traumatic Stress, 26, 426–434. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM–IV and DSM–5 criteria. Journal of Traumatic Stress, 26, 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai HMX, Cleary M, Sitharthan T, & Hunt GE (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Lang AJ, Schnurr PP, Jain S, He F, Walser RD, Bolton E, . . . Chard KM (2017). Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 9(Suppl. 1), 74–84. 10.1037/tra0000127 [DOI] [PubMed] [Google Scholar]
- López A, Sanderman R, Smink A, Zhang Y, van Sonderen E, Ranchor A, & Schroevers MJ (2015). A reconsideration of the Self-Compassion Scale’s total score: Self-compassion versus self-criticism. PLoS ONE, 10, e0132940. 10.1371/journal.pone.0132940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn B, & Morgan J (2016). Using Amazon’s Mechanical Turk (MTurk) to recruit military Veterans: Issues and suggestions. The Military Psychologist, 31, 8–14. [Google Scholar]
- MacBeth A, & Gumley A (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32, 545–552. [DOI] [PubMed] [Google Scholar]
- Management of Post-Traumatic Stress Working Group. (2010). VA/DoD clinical practice guideline for management of post-traumatic stress (pp. 1–251). Washington, DC: Veterans Health Administration, Department of Defense. [Google Scholar]
- McAllister L, Callaghan JE, & Fellin LC (2019). Masculinities and emotional expression in UK servicemen: ‘Big boys don’t cry’? Journal of Gender Studies, 28, 257–270. [Google Scholar]
- Meyer EC, Walser R, Hermann BLA, Bash H, DeBeer BB, Morissette SB, . . . Schnurr PP (2018). Acceptance and commitment therapy for co-occurring posttraumatic stress disorder and alcohol use disorders in veterans: Pilot treatment outcomes. Journal of Traumatic Stress, 31, 781–789. 10.1002/jts.22322 [DOI] [PubMed] [Google Scholar]
- Miron LR, Orcutt HK, Hannan SM, & Thompson KL (2014). Childhood abuse and problematic alcohol use in college females: The role of self-compassion. Self and Identity, 13, 364–379. [Google Scholar]
- Miron LR, Seligowski AV, Boykin DM, & Orcutt HK (2016). The potential indirect effect of childhood abuse on posttrauma pathology through self-compassion and fear of self-compassion. Mindfulness, 7, 596–605. 10.1007/s12671-016-0493-0 [DOI] [Google Scholar]
- Miron LR, Sherrill AM, & Orcutt HK (2015). Fear of self-compassion and psychological inflexibility interact to predict PTSD symptom severity. Journal of Contextual Behavioral Science, 4, 37–41. 10.1016/j.jcbs.2014.10.003 [DOI] [Google Scholar]
- Mishra S, & Carleton RN (2017). Use of online crowdsourcing platforms for gambling research. International Gambling Studies, 17, 125–143. [Google Scholar]
- Muris P, & Petrocchi N (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology & Psychotherapy, 24, 373–383. 10.1002/cpp.2005 [DOI] [PubMed] [Google Scholar]
- Neff K (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–101. [Google Scholar]
- Neff KD, & Germer CK (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69, 28–44. [DOI] [PubMed] [Google Scholar]
- Neff KD, Kirkpatrick KL, & Rude SS (2007). Self-compassion and adaptive psychological functioning. Journal of Research in Personality, 41, 139–154. 10.1016/j.jrp.2006.03.004 [DOI] [Google Scholar]
- Neff K, & Tirch D (2013). Self-compassion and ACT. In Kashdan TB & Ciarrochi J (Eds.), Mindfulness, acceptance, and positive psychology: The seven foundations of well-being (pp. 78–106). Oakland, CA: New Harbinger Publications. [Google Scholar]
- Norman SB, Haller M, Hamblen JL, Southwick SM, & Pietrzak RH (2018). The burden of co-occurring alcohol use disorder and PTSD in U.S. Military veterans: Comorbidities, functioning, and suicidality. Psychology of Addictive Behaviors, 32, 224–229. 10.1037/adb0000348 [DOI] [PubMed] [Google Scholar]
- Norman SB, Tate SR, Anderson KG, & Brown SA (2007). Do trauma history and PTSD symptoms influence addiction relapse context? Drug and Alcohol Dependence, 90, 89–96. 10.1016/j.drugalcdep.2007.03.002 [DOI] [PubMed] [Google Scholar]
- Ouimette P, Goodwin E, & Brown PJ (2006). Health and well being of substance use disorder patients with and without posttraumatic stress disorder. Addictive Behaviors, 31, 1415–1423. [DOI] [PubMed] [Google Scholar]
- Park CL, Mills MA, & Edmondson D (2012). PTSD as meaning violation: Testing a cognitive worldview perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 66–73. 10.1037/a0018792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne AJ, Joseph S, & Tudway J (2007). Assimilation and accommodation processes following traumatic experiences. Journal of Loss and Trauma, 12, 75–91. 10.1080/15325020600788206 [DOI] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Read JP, Brown PJ, & Kahler CW (2004). Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors, 29, 1665–1672. 10.1016/j.addbeh.2004.02.061 [DOI] [PubMed] [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MOB, Scher CD, Clum GA, & Young-Xu Y (2008). A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76, 243–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, & Feuer CA (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, & Schnicke MK (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60, 748–756. [DOI] [PubMed] [Google Scholar]
- Scoglio AA, Rudat DA, Garvert D, Jarmolowski M, Jackson C, & Herman JL (2018). Self-compassion and responses to trauma: The role of emotion regulation. Journal of Interpersonal Violence, 33, 2016–2036. [DOI] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, & Ren L (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116, 93–101. [DOI] [PubMed] [Google Scholar]
- Searle AK, Van Hooff M, McFarlane AC, Davies CE, Fairweather-Schmidt AK, Hodson SE, . . . Steele N (2015). The validity of military screening for mental health problems: diagnostic accuracy of the PCL, K10 and AUDIT scales in an entire military population. International Journal of Methods in Psychiatric Research, 24, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, Wekerle C, Schmuck ML, Paglia-Boak A, & MAP Research Team. (2011). The linkages among childhood maltreatment, adolescent mental health, and self-compassion in child welfare adolescents. Child Abuse & Neglect, 35, 887–898. [DOI] [PubMed] [Google Scholar]
- Thekiso TB, Murphy P, Milnes J, Lambe K, Curtin A, & Farren CK (2015). Acceptance and commitment therapy in the treatment of alcohol use disorder and comorbid affective disorder: A pilot matched control trial. Behavior Therapy, 46, 717–728. 10.1016/j.beth.2015.05.005 [DOI] [PubMed] [Google Scholar]
- Thompson BL, & Waltz J (2008). Self-compassion and PTSD symptom severity. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 21, 556–558. 10.1002/jts.20374 [DOI] [PubMed] [Google Scholar]
- Trompetter HR, de Kleine E, & Bohlmeijer ET (2017). Why does positive mental health buffer against psychopathology? An exploratory study on self-compassion as a resilience mechanism and adaptive emotion regulation strategy. Cognitive Therapy and Research, 41, 459–468. 10.1007/s10608-016-9774-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vettese LC, Dyer CE, Li WL, & Wekerle C (2011). Does self-compassion mitigate the association between childhood maltreatment and later emotion regulation difficulties? A preliminary investigation. International Journal of Mental Health and Addiction, 9, 480–491. [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). Clinician-Administered PTSD Scale for DSM–5 (CAPS-5). Boston, MA: National Center for PTSD. [Google Scholar]
- Wilson AC, Mackintosh K, Power K, & Chan SW (2018). Effectiveness of Self-Compassion Related Therapies: A Systematic Review and Meta-analysis. Mindfulness, 10, 1–17. [Google Scholar]
- Xavier A, Gouveia JP, & Cunha M (2016, August). Non-suicidal self-injury in adolescence: The role of shame, self-criticism and fear of self-compassion [Springer U.S.]. Child and Youth Care Forum, 45, 571–586. 10.1007/s10566-016-9346-1 [DOI] [Google Scholar]
- Yadavaia JE, Hayes SC, & Vilardaga R (2014). Using acceptance and commitment therapy to increase self-compassion: A randomized controlled trial. Journal of Contextual Behavioral Science, 3, 248–257. 10.1016/j.jcbs.2014.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M, Yuval K, Nitzan-Assayag Y, & Bernstein A (2015). Self-compassion in recovery following potentially traumatic stress: Longitudinal study of at-risk youth. Journal of Abnormal Child Psychology, 43, 645–653. 10.1007/s10802-014-9937-y [DOI] [PubMed] [Google Scholar]


