ABSTRACT
While influenza cases in Arizona have nearly tripled since 2018, vaccination rates continue to lag. Statewide, Hispanics and African Americans had the lowest vaccination rates despite having higher influenza infection rates than Whites. Given Arizona’s racial influenza vaccination disparity and the general increase in vaccination hesitancy due to COVID-19, the purpose of this study was to better understand the influences of seasonal influenza vaccination in Arizona during the COVID-19 pandemic using qualitative methods. Findings from this study revealed that many participants were motivated to get the influenza vaccine to protect their family and close friends. The heightened concern for COVID-19 prompted some Hispanic/Latino focus group discussion participants to consider getting vaccinated. However, many Hispanic/Latino participants also expressed that they stopped getting influenza vaccine due to negative vaccination experiences or concern about sickness following immunization. African American participants primarily discussed receiving the vaccine as part of their routine health visit. Compared to other races, more White participants believed that vaccination was unimportant because they were healthy, and the people they interacted with never got sick. Distinct factors influence risk perception and vaccination intention across different racial/ethnic groups. Effective interventions can account for these factors and be tailored to the target population to maximize vaccination uptake.
KEYWORDS: Influenza, vaccination intention, COVID-19, qualitative research, Arizona
Background
Seasonal influenza is a significant threat to global public health.1 Despite the availability of vaccines, there are over 3 million severe cases and nearly 650,000 deaths annually from influenza worldwide.2 With the onset of the 2019 novel coronavirus disease (COVID-19), the World Health Organization (WHO) reported that global influenza surveillance declined or was suspended to prioritize the COVID-19 response.3 The Centers for Disease Control and Prevention (CDC) reported substantially lower levels of influenza incidence and associated illnesses and hospitalizations during the 2020–2021 flu season compared with previous influenza seasons, attributing the change in part to COVID-19 mitigation strategies.4 Prevention and control strategies for influenza and COVID-19 are similar and include handwashing, coughing and sneezing etiquette, and social distancing/isolation.5–9
The World Health Organization (WHO) reported vaccination hesitancy as a leading threat to global health.1 The delay, reluctance, and refusal to vaccinate hinder the ability to eradicate vaccine-preventable diseases permanently.10,11 Influenza vaccination hesitancy is nuanced, with various documented micro, macro, and contextual factors.12 Influenza vaccination hesitancy was a challenge before the COVID-19 pandemic, and the pandemic only further complicates it.13 Understanding influenza vaccination hesitancy in the context of COVID-19 is imperative to improving influenza vaccination rates.
In Arizona, influenza incidence nearly tripled between the 2018–2019 and 2019–2020 influenza season.14 Additionally, between these two influenza seasons, Arizona’s adult vaccination rate increased by less than one percentage point (from 42.6% to 43.2%), whereas the national adult vaccination increased by 3.1% points (from 45.3% to 48.4%).15,16 Statewide, Hispanics and African Americans had the lowest vaccination rates despite having higher influenza infection rates than Whites (43.8%, 38.3%, and 49.6%, respectively).17 Despite the challenges with vaccination, influenza vaccines are available throughout the state at local clinics, mobile clinics, public health department and community organizations.
Several theoretical frameworks have been used to understand influenza vaccination behavior. Some of the most prevalent ones in the literature are the Health Belief Model, Theory of Planned Behavior, and Theory of Reasoned Action.18–21 One of the key criticisms of these theories is that they primarily center on individual attitudes and beliefs while overlooking the influence of social factors and social processes.22,23 Receiving a vaccine protects the health of the individual vaccinated and the health of others around them by minimizing viral spread and ultimately increasing herd immunity. Because of the broader social implications for not getting vaccinated against infectious diseases, vaccination can be perceived as a form of “social contract,” in which everyone has the moral obligation to get vaccinated and collective responsibility to protect one another.24 To account for the influence of social factors on vaccination behavior, the Increasing Vaccination Model (IVM) was used for this research. This model was proposed by Noel Brewer and posited that four domains influence vaccination behavior, namely, psychological processes, social processes, motivation, and practical issues.25 The IVM was adopted by the World Health Organization in 2018 to guide its vaccination efforts.26 To date, only one study has used the IVM, conducting a qualitative evaluation of COVID vaccination hesitancy.26 This study will be the first to use the IVM to understand influenza vaccination behavior.
Given Arizona’s racial influenza vaccination disparity and general increase in vaccination hesitancy due to COVID-19, the purpose of this qualitative study was to identify factors that influence the decision to get the seasonal influenza vaccine and explore racial/ethnic differences in vaccination attitudes that influence decision-making during the COVID-19 pandemic.
Methods
Participants and recruitment
This study took place in Pima County, Arizona, the second-most populous county in Arizona located on the US-Mexico border. The seasonal influenza vaccine coverage rate in Pima County was 32.3% during the 2018–2019 influenza season and 41.5% during the 2019–2020 influenza season, the highest in the state for both seasons.27 As of 2019, it is estimated that 38% of Pima County residents were of Hispanic or Latino origin, 4.2% Black/African American, 4.4% Native American and 3.3% Asian.28 While the county-level data for the racial distribution of vaccinations is unavailable, it is presumed that the racial disparity in influenza vaccination at the state level persists at the county level.
The Institutional Review Board at the University of Arizona reviewed and approved the study. Due to restrictions of in-person data collection, this study employed online strategies for recruitment and data collection. All study procedures were conducted virtually. Participants were recruited between August 2020 and November 2020. Eligible individuals included Spanish and English-speaking adults over the age of 18 who lived in Pima County for at least six months. Out of 124 individuals who expressed interest in the study through an online intake form, 64 were invited to participate in the focus group discussions (FGD). Some invited FGD participants recruited others to participate in their assigned FGD resulting in 21 additional participants. In total, 56 participants completed the study (Table 1).
Table 1.
Descriptive characteristics of participants.
| Participants N = 56 (%) |
|
|---|---|
| Gender | |
| Male | 16 (29) |
| Female | 19 (34) |
| Race/Ethnicity1 | |
| African American | 5 (9) |
| Asian | 2 (4) |
| Hispanic/Latino | 15 (27) |
| White | 14 (25) |
| Preferred Language | |
| English | 24 (43) |
| Spanish | 11 (20) |
| Unavailable Information | 21 (38) |
1Participants could select more than one options.
Data collection
FGDs were conducted to investigate influenza risk perception and influenza vaccination intention, stratified by race, gender, and language (Table 2). Trained facilitators were race and gender-matched to participants to conduct the discussions. The 15-item FGD guide was developed based on the IVM constructs, assessing vaccine-related attitudes, perceptions, and behavior. FGDs were conducted virtually using conferencing software and participants provided verbal informed consent for participation. All participants were compensated $25 for their time.
Table 2.
Descriptive characteristics of focus groups.
| Focus Group | Race | Gender | Language | # Participants |
|---|---|---|---|---|
| 1 | African American | Combined Gender | English | 9 |
| 2 | African American | Combined Gender | English | 4 |
| 3 | African American | Male | English | 3 |
| 4 | White | Male | English | 7 |
| 5 | White | Female | English | 5 |
| 6 | Combined Race | Male | English | 4 |
| 7 | White | Female | English | 4 |
| 8 | Hispanic/Latino | Female | Spanish | 6 |
| 9 | Hispanic/Latino | Female | Spanish | 7 |
| 10 | Hispanic/Latino | Male | Spanish | 2 |
| 11 | Hispanic/Latino | Male | Spanish | 5 |
Data analysis
Eleven FGDs were conducted between September and December 2020 (Table 2). Each session was audio and video recorded on Zoom and transcribed verbatim. The audio recordings for the Spanish-speaking focus groups were first transcribed into Spanish and then translated into English. All transcripts were reviewed and cleaned for clarity and readability.
The transcripts were organized and coded in Dedoose software version 8.3.43. The data were thematically analyzed according to Braun and Clark’s methodological process.29 Five team members familiarized themselves with the data and took notes on our impressions; subsequent discussions formed the basis of a preliminary codebook. We then deductively and inductively coded a single transcript through an iterative process until no new codes emerged. The final codebook consisted of 28 codes. With the finalized codebook, all transcripts were independently coded by two team members, and any discrepancies were reconciled by discussion of the coders. Once coding was completed, we defined themes that emerged from the data.
Positionality statement
Regarding positionality and methodological rigor, the research team comprised of public health practitioners, physicians, administrative staff, undergraduate students, and graduate students. These individuals were from White, African American/Black, Asian, and Latino/a backgrounds. Positionality challenges related to sex, gender, race/ethnicity, power, health, SES, and privilege were intentionally addressed throughout the research design and data collection processes through reflection and training, which focused on how these issues might impact the interviewing process and data analysis. Through practice, teaching, or study, all team members have experience and knowledge in health behavior and vaccinations.
Results
The thematic findings are categorized by the domains of the IVM and summarized in Figure 1. While we present the themes as belonging to distinct domains, we recognize the interconnectedness between the domains. Additionally, we also detail the racial/ethnic differences among the themes presented.
Figure 1.
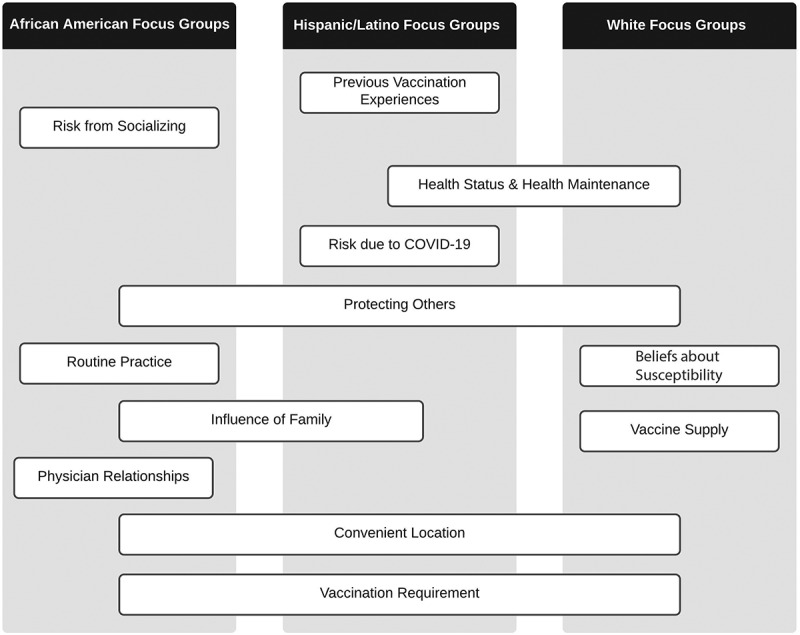
Summary of themes across focus groups.
Domain 1: psychological processes
Previous vaccination experiences
Compared to other groups, more participants in the Hispanic/Latino FGDs recounted negative experiences that influenced their decision not to get vaccinated. Whether it was getting sick after getting the influenza shot, hearing of someone who got sick after getting vaccinated, or a negative experience with the process, these factors were sufficient to deter vaccination.
I’m not against vaccines, but I always got them because I believe that the immune system creates antibodies. But like 8 years ago, they gave me the flu shot, and my blood pressure dropped a lot. The person that gave me the shot left me there. I told them to help me, and they didn’t.[…]Since then, I haven’t gotten the shot, and I don’t think I’m going to get it because I’m more scared that my blood pressure will drop and I’ll have a heart attack. (P2, Hispanic/Latino/Female FG)
Honestly, I think I had a very, very bad [experience]. When I started [got the vaccine], I didn’t have symptoms. Then I started having flu-like symptoms. They lasted like 4 days. Honestly, I haven’t gotten it again. I do think about it – if I give them to my kids. But there are times that I question myself because I think, what are they getting? Or in the future, is it going to affect them? For them, they always get it when the pediatrician tells me. But I haven’t gotten them. I haven’t gotten the flu shot again because of the bad experience that I had when I started to feel very bad. (P37, Spanish-speaking/Hispanic/Latino/Female FG)
Health status and health maintenance
Many participants expressed that their positive health status – being healthy or never getting sick – was why they did not get the influenza shot. This perspective was most prevalent among White participants and some Hispanic/Latino participants.
In the circle of people that I know, very few people get vaccinated. Here, for example, in my house they used to get it, they haven’t got it for about two years now because they would get really sick. I tell you, it’s the effects that make people react differently. They used to get the flu vaccine, and they always got sick, and they would tell me,” you don’t get sick, and you don’t get it.” No, well, that is why I haven’t gotten it, do you understand me? Because I feel like, no, it is not that I don’t need it but that I don’t get sick. (P50, Hispanic/Latino/Male FG)
I’m healthy. I take care of myself. I’ve been doing the things like coughing and all that; I’ve been doing that for most of my life. Most of you guys were talking about getting the flu shot. I haven’t had a flu shot in 40–30 years and haven’t been around people with the flu and all that. I don’t get it. I can’t even tell you the last time I’ve had a cold. (P23, White/Male FG)
Hispanic/Latino participants also talked about their health status in the context of the body being a natural defense against influenza. Participants believed that for as long as they are taking care of their bodies, they were not at risk for influenza.
I think that how you eat if you eat healthy, I think you are not at risk for getting the flu. If you eat a lot of things that have vitamin C like they say, and natural food, I don’t think you should be scared. […]But I know that I am taking care of myself. I wouldn’t be too scared if there is a flu outbreak. Well, that’s my opinion. (P40: Hispanic/Latino/Female FG)
I don’t know. I’ve, I’ve had the flu before, and I’ve been treated with the medicine when I got flu, and I think that just made me think that I’m I don’t need a vaccine. I can just get treatment after I get sick. And then I think I was more like focusing on building up the immune system or taking care of my body rather than okay I’m gonna get vaccinated. So I don’t get flu for this reason (P14, Combined Race/Male FG)
Risk from socializing
The risk of getting influenza from socializing was most prominently discussed among African American participants. While many believed the influenza shot minimized their risk of getting influenza, there was still a concern that interactions with other people may increase their risk of infection.
Our family has gotten the flu vaccine believing that our risk would be lower.[…]If one of my friends told me that he or she has gotten the flu, I wouldn’t even be around them. I will drop some chicken noodle soup off at your doorstep and keep it moving in the right direction. So, I am going to say my risk would be fairly low because of getting the vaccine. And I don’t plan on being around anybody with the flu. (P43, African American/Combined Gender FG)
Yeah, I just feel high concern even if I did get a flu shot. I would still be on alert for like my loved ones and friends, and family. […]But yeah, at work would be like the main risk. And which, luckily, I’m not in a living situation right now where I’m with a ton of family members. […]I’d say my risk is more minimal. But, I’d say about a moderate because I still am in a high socializing place. (46, African American/Combined Gender FG)
Risk due to COVID-19
Many participants believed that if they got infected with both influenza and COVID-19, their sickness would be worse. For this reason, some participants who normally never get vaccinated against influenza were considering it.
And as I said, this is the first year that I got the flu shot because I didn’t want to have that problem on top of COVID. But if it were just the flu, I wouldn’t have taken it because I’m not afraid of the flu (P51, Hispanic/Latino/Male FG)
Keeping the immunity or the immune system is really important, and I’ve never gotten the flu shot. But I do think I am going to get it this year because I see the risk of getting weaker. Having the flu normally doesn’t affect me a lot. I haven’t really had it. But this year, everything with COVID I think it’s worth getting it. (P42, Hispanic/Latino/Female FG)
Domain 2: social processes
Protecting others
Across all FGDs, many participants shared that they get vaccinated or consider getting vaccinated to protect the family, friends, and other people that they know and interact with. Even among participants not afraid of the influenza, there was concern for getting other people sick.
I do things to protect myself, and I have to think about. I have a new grandson, and I do some babysitting for my family, so I don’t want to get something to pass on to them. I don’t have the kind of fear that some people express about getting the disease. I don’t want to get it, but I don’t fear it either. […]I pay attention to the people around me and who I would put at risk if I had the disease, but I’m not afraid of it. I do what I need to do to protect myself just like I would be for any disease. (P27, African American/Combined Gender FG)
The last time I, well I have been getting the flu vaccine for years now, and at first, I had little fear about it because as a child I got vaccines and suffered from it. But, since my son has asthma, the whole family decided to get vaccinated against influenza. We already have a few years, and this year was no exception. (P48, Hispanic/Latino/Male FG)
Beliefs about susceptibility
Many participants felt that they were not susceptible to influenza infections because they had not been previously infected, knew others who never received the influenza vaccine and never had an influenza infection, or they interacted with people who were perceived to not be susceptible to illness.
I don’t take a shot and like my father has cancer and he’s recovering from it. And my mother has some health issues. They haven’t had the flu shot in 10 years, and they’ve not had the flu in any of those years.[…]I’m around people, and I don’t ask, and for some reason, I don’t get it. And so I don’t take the shot. (P23, White/Male FG)
I don’t really oppose getting the influenza vaccine. It just never seemed like something that was important because I didn’t feel very susceptible, and the people I interacted with didn’t appear susceptible. (P13, Combined Race/Male FG)
Routine practice
African American participants frequently discussed the “routine” of getting their influenza shot. Getting vaccinated was an activity they did as a child and is now a practice they continued into adulthood.
I got the flu shot. I think a couple weeks ago at my doctor’s appointment, and I’ve always just gotten it because, I mean, it was just a routine from being a child that it’s something that you have to get (P44, African American/Combined Gender FG)
Just has become a part of what you have to do, you know, you go to the dentist, you go to the doctor for your annual checkup. And you just got to get a flu shot. I mean, there is, at least for our family, no ifs, ands, or buts about it. So it’s not really anything we think about it’s just something like I said, we automatically do. (P43, African American/Combined Gender FG)
I had quite an exceptional a doctor, and I retained him until he retired after 20 years, and most recently, this past Sunday, I took a flu shot. And I just do that as a matter of caution, and it’s just a routine I’m into now, and just follow up and follow through. And that’s – that’s basically what I go through when I have to deal with vaccines. (P35, African American/Combined Gender FG)
Influence of family
When our African American participants discussed vaccination behaviors within their families, there was a sense of agreement that the vaccination decision is something everyone would follow. However, among our Hispanic/Latino participants, there seemed to be more differences of opinion about vaccinations within families, influencing some to get vaccinated or others not to. Children were also influential in vaccine decision making, conveying information that would either convince, dissuade, or introduce doubt about getting vaccinated.
Well, like I said for my age, I am 44 years old. I think that maybe that’s why I get the shot too, because of what my daughter tells me. “You have to get it mom because you are 55 years old, and we have to well, you know – you have to get the shot so that when you get the flu, it isn’t as strong. (P40, Hispanic/Latino/Female FG)
But I’m remembering that my husband […] when the moment came that we had our small children. He always said to take them to get their vaccines and, of course, his favorite: the flu shot. But when I would talk with him, thank God, he would say: okay I agree with your point of view, do what you want. And now I’m happy that I didn’t give my kids the vaccines (P4, Hispanic/Latino/Female FG)
Physician relationships
More African American participants talked about getting their influenza shot from their doctor’s office. Participants spoke about the relationship with their physician and getting a influenza shot at their physician’s prompting.
And so every time I go to the doctors, and they say, Do you want the flu shot?. I just say Yeah. Sometimes I forget that I even forget I say yes, I just get there, they just give me the shot and I’m like oh! You know, cause it’s just something that needs to be done. (P44, African American/Combined Gender FG)
My situation is with the doctor; I’ve had him for 25 years he’s an exceptional doctor, so he kind of kept a reminder of things that I need to be looking for and be mindful as you age (P35, African American/Combined Gender FG)
Domain 3: motivation
The domain of motivation functions as a mediating variable in the IVM. Our study found that participants expressed their intention or willingness to get vaccinated in the context of the other domains. Participants explicitly expressed their intention not to get vaccinated with statements such as “I’m not getting the flu shot” and “I don’t get the shot”. Willingness to get vaccinated was reflected in sentiments such as “I think it’s worth getting” and “It has to be a requirement for me to get it.” Overall, motivation varied across participants and FGDs. Whether motivation was positive or negative on vaccination uptake depended on the factors perceived to be salient to individual participants.
Domain 4: practical issues
Vaccination requirement
Being required to get vaccinated was expressed across the different FGDs with participants sharing they got vaccinated because their place of employment or education required them to. Among participants who do not get the influenza shot, some expressed only doing so if required.
When I worked for the state – they have clinics, and we all had to line up, and we’d all get a flu shot because I was working for the Division of Developmental Disabilities, and we’re going into homes with people that have some … too often have compromised immune systems. (P16, White/Female FG)
It has to be a requirement for me to get it like for work or whatever, for school or something like that, and I’ll be convinced to get vaccinated for flu. (P14, Combined Race/Male FG)
Convenient location
Locations such as local pharmacies provided convenient access to get vaccinated. Additionally, some participants discussed getting it at their place of employment, which helped streamline getting vaccinated.
The last vaccine. I got was the flu shot as well. And it was administered through where I worked at, and they came in, and it was pretty, pretty easy to set an appointment. I walked in and walked out within a matter of minutes. (P25, White/Male FG)
They make it easy in my doctor’s office that I can go in there. I would go get a flu shot this year they’re doing drive-through flu shots at my doctor’s office. […]I’ve got my appointment set up, and they will do it right there in my car (P30, African American/Combined Gender FG)
Vaccine supply
White participants discussed vaccine supply issues more than other groups – several recounted experiences of attempting to get vaccinated but locations running out of supply. Concerned about shortages, some participants were prompted to get vaccinated earlier in the season to beat demand.
Okay, so I just wanted to say that I brought my daughter to get her flu shot at the same place I got mine. And I think it was only slightly a couple of weeks after and my doctor’s office had already run out a flu shot […]I had even called our local Walgreens and CVS, and I think CVS was the only one who had the flu shot still that late in the season. In hindsight, I think we didn’t even go and get it at that point, I think. We ended up maybe by that point – things were already falling apart with the cruise planning. We’re just like, alright, we’re just gonna hunker down and no one’s catching anything for a while. So anyway, but we had the same experience of all like running out of flu vaccines. (P19, White/Female FG)
Discussion
This study revealed similarities and differences among the factors influencing vaccination uptake among diverse populations. Twelve key themes emerged from our data: previous vaccination experiences, health status and health maintenance, risk from socializing, risk due to COVID-19, protecting others, beliefs about susceptibility, routine practice, influence of family, physician relationships, vaccination requirement, convenient location, and vaccine supply. Some were shared across all FGDs while other themes were more isolated to specific groups. Some shared themes had different meanings or implications depending on the FGD context. For example, White FGD participants spoke about their health status in the context of never getting sick and therefore not needing the influenza shot, whereas Hispanic/Latino participants talked about their health status as the body/immune system being a natural defense against the influenza, reducing the need to get vaccinated. Overall, our findings underscore the importance of accounting for different factors and their nuanced value when promoting vaccination uptake among diverse populations.
While FGDs for this study were stratified by gender and race/ethnicity, the results focused on were racial/ethnic differences. Many of the same themes emerged for gender as they did for race/ethnicity; differences by gender were not as pronounced. One notable difference was the discussion of children and vaccination – specifically whether participants vaccinate their children – which was more prominent among female participants.
Some results from this study are consistent with findings from previous qualitative research, while other results offer new insights. The theme of convenient location and health maintenance as factors of vaccination uptake are supported by other qualitative studies.23 However, the health maintenance theme in our study was predominant among our Hispanic/Latino participants, contrasting previous research where it was prevalent among the African American participants.23 The previous vaccination experiences’ theme that emerged among our Hispanic/Latino participants was consistent with other findings for this same demographic.30 Furthermore, our study’s findings related to the social processes’ domain of the IVM were consistent with previous research, corroborating the idea that social networks and social norms influence vaccination uptake.31 Surprisingly, cost and financial concerns did not emerge as a prevalent theme in our study despite findings in the literature.23,30
Many African American participants expressed receiving their influenza vaccine from their doctor’s office and were responsive to reminders and encouragement from their physician to get vaccinated. While provider recommendations are positively associated with vaccination uptake,32 our findings seem to contradict what has been established in the literature about the African American community and medical mistrust; given historical injustices, racial discrimination, and divergent cultural experiences, African Americans are more likely to have higher levels of distrust in health care systems and medical professionals than their racial counterparts.33,34 Our findings suggest that trusting physician-patient relationships may exist for some community members and warrant further investigation into why our results are divergent from previous literature. Several participants noted the longevity of the relationship with their provider. Medical mistrust may lead people to search and stick with a provider long-term when trust is demonstrated and established; however, more research is needed to investigate conditions that promote doctor-patient trust among racial/ethnic minorities. Nevertheless, our data illustrate that trusting physician-patient relationships can help address the disparities in vaccination uptake among African Americans and other racial/ethnic groups.
The novelty and uncertainty of COVID-19 increased perceived risk and perceived susceptibility to influenza. Surprisingly, the consideration of COVID-19 as a factor for vaccination was not shared across by all participants but was most notable only among our Hispanic/Latino participants. The potential severe sickness from getting infected with both influenza and COVID-19 caused some vaccine-refusing participants to reconsider getting the influenza vaccine. More research should be conducted to explore if the influence of COVID-19 on influenza vaccine uptake is unique to Hispanic/Latino populations. Our study was conducted before the availability of COVID-19 vaccines. With COVID-19 vaccines now available, future research should be conducted to assess how COVID-19 vaccination uptake may affect influenza vaccination uptake across all population demographics.
This study is the first to utilize the Increasing Vaccination Model to understand influenza vaccination behavior. While traditional theoretical frameworks, such as the Health Belief Model or the Theory of Reasoned Action, used in vaccination research primarily address individual-level determinants, the IVM’s inclusion of social processes and practical issues allows us to better identify opportunities for intervention in other ecological realms such as interpersonal, institutional, and policy areas that impact vaccination behavior.35 Various factors were identified across the four domains of the IVM. Future research should explore the interconnectedness of factors within the individual domains and across domains. For instance, some participants evaluated vaccination risk and benefits to their health against the risk and benefits of others in their social network when deciding to get vaccinated. Research has shown that how risks are assessed and evaluated in relation to one another can influence behavioral outcomes.36 Some participants in our study expressed that they previously never got vaccinated until it was discovered their child had asthma; influenza shots then became necessary to them. Here we see the participants’ personal perceived risk of getting the influenza being weighed against the perceived risk of their child with asthma getting the influenza. Recognizing that competing factors may be at play in the vaccination decision.
The findings of this research also support the case for implementing vaccination mandates and providing vaccines in accessible locations. Participants in our study spoke about getting vaccinated from local pharmacies or at their work. Influenza vaccination drives at schools and employment places have been shown to increase vaccination rates.37,38 As suggested by the IVM, practical issues may make the difference between intention versus actual vaccination uptake. Therefore, providing easier access to vaccines helps increase vaccination rates. Research has shown that vaccine mandates also increase vaccination rates.39,40 However, while mandates may be effective, care and caution should be taken, particularly for marginalized populations with historical trauma of forced medical practices.41,42 To mandate vaccination without provisions that mitigate access barriers or acknowledge historical medical failings would only exacerbate vaccination inequity.
This research has several limitations. There is no representation of indigenous populations in our sample despite Arizona having 22 federally recognized Sovereign Nations.43 When this research was conducted, approval was not obtained to conduct research with Native populations. Additionally, conducting virtual FGDs facilitated broader accessibility and convenience for participants to engage in our study and allowed us to comply with the COVID-19 safety regulations. However, the virtual setting may have impeded the organic flow of conversation typical of FGDs. While additional layers of anonymity were available to participants (joining by phone or having their camera off), it limited the ability to read body language and social cues. Despite the challenges, the virtual format facilitated data collection during a challenging time and allowed important research activities to continue while protecting everyone’s safety.
Conclusion
There are distinct factors that influence risk perception and vaccination intention across different racial/ethnic groups. Health communication strategies and intervention development should be tailored to sub-population differences to maximize vaccination uptake. Utilizing frameworks such as the IVM provide guidance and reveal opportunities for nuanced intervention development that account for different ecological domain influences in promoting influenza vaccination uptake.
Acknowledgments
We would like to acknowledge the following groups and organizations for supporting this research: the Pima County Health Department of Arizona, Paisano Unidos, and The University of Arizona Evaluation Group for Analysis of Data and The University of Arizona College of Linguistics. Special thanks to Mary Kinkade at the Pima County Health Department and the members of The University of Arizona Alliance for Vaccine Literacy – Jacob Marczak, Veena Raghuraman, and Ava Neddermeyer for their work on this project.
Funding Statement
This work was supported by the University of Arizona Mel and Enid Zuckerman College of Public Health Dean’s Fund; the Western Region Public Health Training Center, Tucson, AZ; the Pima County Health Department, Tucson, AZ; and the University of Arizona Graduate Professional Student Committee. PM is partially supported by the GHES training grant from NIH/FIC under Award Number D43 TW010540 and NIH/NIA R03AG069796-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author contributions
CMPV, PM, MK, KK, BK, and MBN conceptualized and developed the study. NMM, MBN, KJ, SV, KK, BK and PM were involved in data collection. NMM, PM, PM, LBG, MBN, SV, KJ contributed to data analysis and interpretation. NMM drafted the manuscript. All authors critically reviewed the draft of the manuscript and approved the final version.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- 1.World Health Organization . Ten threats to global health in 2019. 2019. [accessed 2021 Jul 18]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 2.World Health Organization . Up to 650 000 people die of respiratory diseases linked to seasonal flu each year. 2017. [accessed 2021 Jul 18]. https://www.who.int/news/item/13-12-2017-up-to-650-000-people-die-of-respiratory-diseases-linked-to-seasonal-flu-each-year.
- 3.Owen J. WHO warns that averting flu pandemic may be harder as surveillance switches to covid-19. BMJ. 2020;369:m2441. doi: 10.1136/bmj.m2441. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention . 2020-2021 flu season summary | CDC. 2021. [accessed 2021 Nov 3]. https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm.
- 5.Itaya T, Furuse Y, Jindai K. Does COVID-19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int J Infect Dis. 2020;97:78–8. doi: 10.1016/J.IJID.2020.05.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conlon A, Ashur C, Washer L, Eagle KA, Bowman MAH. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am J Infect Control. 2021;49(6):694–700. doi: 10.1016/j.ajic.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatt H. Improving influenza vaccination rates during COVID-19 pandemic– the need of the hour. J Glob Health. 2021;11:1–3. doi: 10.7189/jogh.11.03042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Candelli M, Pignataro G, Torelli E, Gullì A, Nista EC, Petrucci M, Saviano A, Marchesini D, Covino M, Ojetti V, et al. Effect of influenza vaccine on COVID-19 mortality: a retrospective study. Intern Emerg Med. 2021;16(7):1849–55. doi: 10.1007/s11739-021-02702-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang MJ, Rooks BJ, Le TTT, Santiago IO, Diamond J, Dorsey NL, Mainous AG. Influenza vaccination and hospitalizations among COVID-19 infected adults. J Am Board Fam Med. 2021;34:S179–82. doi: 10.3122/JABFM.2021.S1.200528. [DOI] [PubMed] [Google Scholar]
- 10.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Wei Z, Liu Y, Zhang L, Sun X, Jiang Q, Li Z, Wu Y, Fu C. Stages of HPV vaccine hesitancy among guardians of female secondary school students in China. J Adolesc Health. 2022. doi: 10.1016/j.jadohealth.2022.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005-2016. PLoS One. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Pumpo M, Vetrugno G, Pascucci D, Carini E, Beccia V, Sguera A, Zega M, Pani M, Cambieri A, Nurchis MC, et al. Is covid-19 a real incentive for flu vaccination? Let the numbers speak for themselves. Vaccines (Basel). 2021;9(3):276. doi: 10.3390/vaccines9030276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minnick C. ADHS reports influenza cases are three times higher in 2019 than previous season with more than half the cases reported in children, health officials urge public to get vaccinated. 2019. [accessed 2021 Jul 18]. https://www.azdhs.gov/director/public-information-office/index.php#news-release-112219.
- 15.Centers for Disease Control and Prevention . Flu vaccination coverage, United States, 2018–19 influenza season | FluVaxview | seasonal influenza (Flu) | CDC. 2019. [accessed 2021 Jul 18]. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm.
- 16.Centers for Disease Control and Prevention . Flu vaccination coverage, United States, 2019–20 influenza season | FluVaxview | seasonal influenza (Flu) | CDC. 2020. [accessed 2021 Jul 18]. https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm?web=1&wdLOR=cEDDACEB2-A2FF-4FD3-B6BA-35F2D09FAC46.
- 17.Centers for Disease Control and Prevention . Influenza vaccination coverage for persons 6 months and older | FluVaxview | seasonal influenza (Flu) | CDC. 2021. [accessed 2021 Jul 18]. https://www.cdc.gov/flu/fluvaxview/interactive-general-population.htm.
- 18.Kan T, Zhang J. Factors influencing seasonal influenza vaccination behaviour among elderly people: a systematic review. Public Health. 2018;156:67–78. doi: 10.1016/j.puhe.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.AMS W, Lau JTF, Ling MY, Cheng KM, Lau MMC. A longitudinal study using parental cognitions based on the theory of planned behavior to predict childhood influenza vaccination. J Infect Public Health. 2020;13(7):970–79. doi: 10.1016/j.jiph.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–80. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.PKH M, Lau JTF. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: the application of the health belief model. Health Educ Res. 2014;30(5):706–18. doi: 10.1093/her/cyv038. [DOI] [PubMed] [Google Scholar]
- 22.VanLandingham MJ, Suprasert S, Grandjean N, Sittitrai W. Two views of risky sexual practices among northern Thai males: the health belief model and the theory of reasoned action. J Health Soc Behav. 1995;36(2):195–212. doi: 10.2307/2137225. [DOI] [PubMed] [Google Scholar]
- 23.Quinn S, Jamison A, Musa D, Hilyard K, Freimuth V. Exploring the continuum of vaccine hesitancy between African American and white adults: results of a qualitative study. PLoS Curr. 2016:8. doi: 10.1371/currents.outbreaks.3e4a5ea39d8620494e2a2c874a3c4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Korn L, Böhm R, Meier NW, Betsch C. Vaccination as a social contract. Proc Natl Acad Sci USA. 2020;117(26):14890–99. doi: 10.1073/pnas.1919666117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest Suppl. 2017;18(3):149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- 26.Gayle H, Foege W, Brown L, Kahn B. Framework for equitable allocation of COVID-19 vaccine. Framework Equitable Allocation COVID-19 Vaccine. 2020:1–252. 10.17226/25917. [DOI] [Google Scholar]
- 27.Centers for Disease Control and Prevention . Influenza vaccination coverage for persons 6 months and older | FluVaxview | seasonal influenza (Flu) | CDC. 2021. [accessed 2021 Oct 12]. https://www.cdc.gov/flu/fluvaxview/interactive-general-population.htm/.
- 28.US Census Bureau . U.S. Census Bureau quickFacts: Pima County, Arizona. 2019. [accessed 2021 Sep 29]. https://www.census.gov/quickfacts/fact/table/pimacountyarizona/PST045219.
- 29.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 30.Daniels NA, Juarbe T, Rangel-Lugo M, Moreno-John G, Pérez-Stable EJ. Focus group interviews on racial and ethnic attitudes regarding adult vaccinations. J Natl Med Assoc. 2004;96:1455. [PMC free article] [PubMed] [Google Scholar]
- 31.Quinn SC, Hilyard KM, Jamison AM, An J, Hancock GR, Musa D, Freimuth VS. The influence of social norms on flu vaccination among African American and White adults. Health Educ Res. 2017;32(6):473–86. doi: 10.1093/her/cyx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jun LP, Srivastav A, Amaya A, Dever JA, Roycroft J, Kurtz MS, O’Halloran A, Williams WW. Association of provider recommendation and offer and influenza vaccination among adults aged ≥18 years – United States. Vaccine. 2018;36(6):890–98. doi: 10.1016/J.VACCINE.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 33.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–65. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97(7):951–56. doi: 10.13016/lfd2-l89x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Edu Behav. 2012;39(2):229–43. doi: 10.1177/1090198111415105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nichter M. Global health: why cultural perceptions, social representations, and biopolitics matter. Tucson (AZ): University of Arizona Press; 2008. [Google Scholar]
- 37.Szilagyi PG, Schaffer S, Rand CM, Goldstein NPN, Hightower AD, Younge M, Albertin CS, DiBitetto K, Yoo B, Humiston SG. School‐located influenza vaccination: do vaccine clinics at school raise vaccination rates? J Sch Health. 2019;89(12):1004–12. doi: 10.1111/josh.12840. [DOI] [PubMed] [Google Scholar]
- 38.Nowalk MP, Lin CJ, Toback SL, Rousculp MD, Eby C, Raymund M, Zimmerman RK. Improving influenza vaccination rates in the workplace: a randomized trial. Am J Prev Med. 2010;38(3):237–46. doi: 10.1016/j.amepre.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 39.Lytras T, Kopsachilis F, Mouratidou E, Papamichail D, Bonovas S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: a systematic review and meta-regression analysis. Hum Vaccin Immunother. 2016;12(3):671–81. doi: 10.1080/21645515.2015.1106656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rakita RM, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol. 2010;31(9):881–88. doi: 10.1086/656210. [DOI] [PubMed] [Google Scholar]
- 41.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87(11):1773–78. doi: 10.2105/AJPH.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pearson JD. Lewis Cass and the politics of disease: the Indian vaccination act of 1832. Wicazo Sa Rev. 2003;18(2):9–35. doi: 10.1353/wic.2003.0017. [DOI] [Google Scholar]
- 43.US Department of the Interior Indian Affairs . Tribal leaders directory | Indian affairs. [accessed 2021 Nov 4]. https://www.bia.gov/bia/ois/tribal-leaders-directory/.


