Abstract
Background
The purpose of the study was to compare the clinical presentation, management, and outcomes of surgical revascularization for acute limb ischemia (ALI) in 2 groups of patients–with and without SARS-CoV-2 infection.
Methods
During the 2 years (01.01.2020–31.12.2021) all consecutive patients diagnosed with ALI and treated with urgent revascularization were prospectively enrolled. Based on the results of polymerase chain reaction swab for SARS-CoV-2 infection patients were allocated to group A–infected or group B–noninfected. Demographic characteristics, clinical, imaging, laboratory data, and details of treatment were collected prospectively. The composite endpoint of major amputation and/or death at 30 days after surgery was defined as main study outcome. The postoperative ankle-brachial index value, reinterventions, complications, and length of hospital stay were considered as secondary outcomes.
Results
Overall, 130 patients (139 limbs with ALI) were analyzed–21 patients (23 limbs) in group A and 109 patients (116 limbs) in group B. The anatomical site of arterial occlusion, duration, and severity of ischemia did not differ significantly between the groups. Patients with COVID-19 had significantly shorter time from ALI onset till administration of the first dose of anticoagulant: 8 (2.5–24) hr vs. 15.7 (6–72) hr in group B, P = 0.02. Vascular imaging was performed before intervention only in 5 (23.8%) infected patients compared to 78 (71.5%) patients in group B, P < 0.001. The main outcome was registered in 38 (29.2%) patients, significantly more frequent in infected cohort: 12 (57.1%) patients in group A versus 26 (23.8%) in group B, P = 0.003. Difference was preponderantly caused by high mortality in group A–9 (42.8%) patients, compared to 17 (15.5%) patients in group B, P = 0.01. The difference in the rate of limb loss was not statistically significant: 4 (17.3%) limbs were amputated in COVID-19 patients and 12 (10.3%) limbs–in noninfected patients (P = 0.3). Combination of ALI and COVID-19 resulted in increased 30-day mortality–risk ratio (RR) 2.7 (95% confidence interval [CI]: 1.42–5.31), P = 0.002, but did not lead to significantly higher amputation rate–RR 1.6 (95% CI: 0.59–4.75), P = 0.32. In group A initial admission of the patient in the intensive care unit was an independent risk factor for amputation/death. Excepting systemic complications which were more frequently registered among COVID-19 patients: 7 (33%) cases vs. 14 (12.8%) in group B, P = 0.04; no differences in other secondary outcomes were observed between the groups.
Conclusions
Study demonstrates the significant negative impact of COVID-19 upon the 30-day amputation-free survival in patients undergoing urgent surgical revascularization for ALI. The difference in outcome is influenced by higher rate of mortality among infected patients, rather than by the rate of limb loss. Severity of COVID-19, namely requirement of intensive care, mostly determines the outcome of ALI treatment.
Introduction
Acute limb ischemia (ALI) is a major vascular emergency associated with high rates of mortality, limb loss, and permanent disability. Despite significant progresses achieved in many fields of vascular surgery during the last decades the outcomes of ALI treatment generally remain unchanged.1 Mortality and major amputation rates reported in contemporary series both exceed 10% within 30 days of follow-up.2 , 3 Challenges in management of ALI could be explained by significant variability of causes and underlying vascular conditions, versatility of curative approaches, short time available for limb salvage, frailty, and polymorbidity of most patients.
Global pandemic of severe acute respiratory syndrome caused by coronavirus type 2 (SARS-CoV-2) has dramatically affected the health care system worldwide. Association of coronavirus infection disease (COVID-19) with acute thrombotic events, in particular with ALI, was observed from the beginning of the “first wave” of pandemic.4 , 5 Early experience in the management of patients with ALI and COVID-19 uncovered dismal results of treatment with unusually high rates of reintervention (around 13%), amputation (>30%) and death (>35%).5, 6, 7 Amid the pandemic, the European Society for Vascular Surgery published an update of clinical practice guideline on the management of ALI in patients with COVID-19, based on the analysis of limited number of publications: 89 case reports and nine cohort studies reporting on 13–49 patients. The majority of studies were observational with high heterogeneity and risk of bias.8 Although several important recommendations were formulated, the authors of the guideline highlighted very low level of evidence and called for continuous efforts in data collection and collaboration in research initiatives.9 Thus, the current study aimed to compare the clinical presentation, management, and outcomes of surgical revascularization for ALI in 2 groups of patients–with and without SARS-CoV-2 infection treated in a single center during the same time period.
Material and Methods
It was a single-center observational prospective cohort study. The study protocol was elaborated according to the principles of Declaration of Helsinki and approved by the university's ethical committee. Written informed consent was obtained from all enrolled patients.
Patients
During 2 years (01.01.2020–31.12.2021) all consecutive patients presenting in 24/7 vascular service of the Institute of Emergency Medicine (Chisinau, Moldova), diagnosed with ALI and treated with urgent (<24 hr from admission) revascularization were prospectively enrolled. The ALI was defined as suddenly developed perfusion deficit of upper or lower limb threatening its viability and lasting no more than 14 days.10 Patients with acute occlusion of native arteries, vascular reconstructions (autologous conduit, synthetic bypass, stent, or stent graft) and peripheral aneurysm were included. Patients were excluded if they met any of the following criteria: (1) ALI caused by trauma (including iatrogenic injuries); (2) ALI associated with aortic dissection; (3) ALI as a complication of vascular interventions developed in the early postoperative period (during the same hospitalization); (4) acute onset of intermittent claudication. Since the first COVID-19 cases were confirmed in the Republic of Moldova in March 2020, all hospitalized patients were tested with a polymerase chain reaction swab for SARS-CoV-2 infection. Based on the results of the test, patients were allocated to one of the two groups: group A–infected and group B–noninfected. Demographic characteristics and comorbidities; clinical, imaging, and laboratory data relevant to the diagnosis and severity of ALI (in both groups), and COVID-19 (in group A); details of revascularization procedure, antithrombotic treatment and complications were collected prospectively and registered in a dedicated database.
Diagnosis and Treatment
Diagnosis of ALI was made clinically by a qualified vascular surgeon and severity of ischemia was classified according to the Rutherford categories: grade I–rest pain without sensory loss and motor deficit; grade IIA–sensory loss without motor deficit, and grade IIB–any motor deficit.10 Duplex ultrasound (DUS), computed tomography angiography and digital subtraction angiography were used on discretion of specialist and depending on availability. Direct pressure measurement in leg compartments was performed in patients with clinically suspected compartment syndrome. Chest radiography was performed in all patients and Brixia score was used for semiquantitative assessment of pulmonary involvement in group A.11 Surgical risk was stratified according to the definitions of the American Society of Anesthesiologists classification.
Open surgical procedures (thrombo-embolectomy, thrombo-endarterectomy, and bypass) were mostly used for limb revascularization. Completion imaging was not performed routinely. The percutaneous techniques (thrombo-aspiration, balloon angioplasty, and stenting) were used only occasionally due to its limited availability in emergency settings. A four-compartment fasciotomy was performed if clinical signs of compartment syndrome were present or compartment pressure exceeds 30 mm Hg. All patients received antithrombotic treatment perioperatively, while selection of drugs, dose, and duration of therapy was done individually. Internal medicine specialists and intensivists were responsible for treatment of COVID-19 in group A according to the protocols available at that time.
Definitions
Hypertension was defined as systolic blood pressure >140 mm Hg or diastolic pressure >90 mm Hg, documented diagnosis or ongoing use of antihypertensive medication. Ischemic heart disease was defined as the presence of angina pectoris, history of myocardial infarction, or any coronary artery revascularization. Atrial fibrillation was defined as a documented history or characteristic electrocardiographic pattern. Diabetes mellitus was defined by history, treatment with insulin, or with antidiabetic drugs. Anemia was defined as hemoglobin <130 g/L for men and <120 g/L for women, and impaired renal function–as serum creatinine >105 μmol/L.
Presumed embolic nature of acute arterial occlusion was determined by operating surgeon based on history (arterial fibrillation and previous embolic events); vascular imaging (absence of significant atheroma/calcification) and distinct embolus removed during surgery. Popliteal artery aneurysm was diagnosed if popliteal artery diameter exceeded 15 mm.
Study Outcomes
The results of revascularization were assessed clinically, hemodynamically–by determination of ankle-brachial index (ABI) and anatomically–using postoperative DUS (group B only). The composite endpoint of major amputation and/or death at 30 days after surgery was defined as the main study outcome. The postoperative ABI value, reinterventions, complications, and length of hospital stay were considered as secondary outcomes.
Statistical Analysis
Categorical variables are presented as absolute numbers with percentage, and continuous variables as medians with 25–75% interquartile range or means ± standard deviation. Difference of medians was assessed by Mann-Whitney test, difference of means–by two-tailed t-test, and difference between proportions–by Fisher’s exact test. The risk ratio (RR) is reported to compare the probability of main outcomes between groups. Association of variables with outcome was tested in univariable and multivariable models. Binary logistic regression with calculation of odds ratios (OR) was used to analyze association of variables with dichotomous outcomes. A P-value <0.05 was considered statistically significant. Statistical analysis was conducted using “GraphPad Prism” (v. 8.0.1, GraphPad Software, San Diego, California, USA) and SPSS 22.0 (SPSS Inc., Chicago, IL, USA) software.
Results
Patient Characteristics
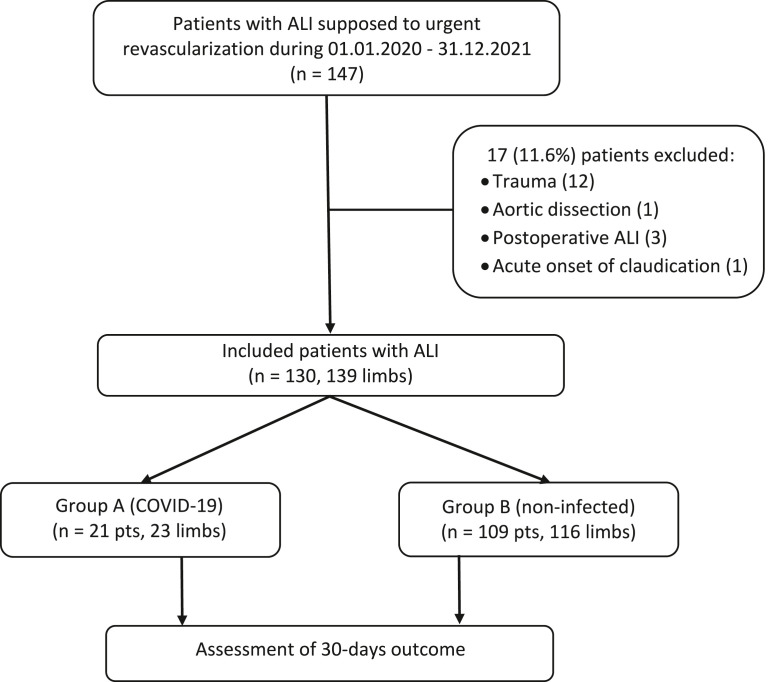
Overall, 147 patients were treated with urgent revascularization during the study period. After exclusion of 17 cases, 130 patients (139 limbs with ALI) were analyzed–21 patients (23 limbs) in group A and 109 patients (116 limbs) in group B (Fig. 1 ). The baseline characteristics of the patients are presented in Table I . Patients in the group A had a higher prevalence of diabetes mellitus (57.1% in group A vs. 24.7% in group B, P = 0.007) than those in group B, while atrial fibrillation was diagnosed more frequently among noninfected patients (33.3% in group A vs. 74.3% in group B, P < 0.001). Embolism was considered as a cause of acute arterial occlusion in the majority of noninfected patients (47.8% in group A vs. 74.1% in group B, P = 0.02) and, vice versa, thrombosis was more characteristic for patients with COVID-19 (52.1% in group A vs. 21.5% in group B, P = 0.004). There were no significant differences in demographic characteristics and other comorbidities between the 2 groups, nor did the anatomical site of arterial occlusion, duration, and severity of ischemia differ significantly between the group A and group B.
Fig. 1.
Flow-chart demonstrating the inclusion of 130 patients (139 limbs) with ALI.
Table I.
Demographic, clinic, and laboratory data of study participants
| Variable | Total (130 pts, 139 limbs) | Group A (21 pts, 23 limbs) | Group B (109 pts, 116 limbs) | P valuea |
|---|---|---|---|---|
| Age (years) | 71 (65–77) | 66 (63–74) | 71 (65–77) | 0.11 |
| Female | 44 (33.8%) | 7 (33.3%) | 37 (33.9%) | 1.0 |
| Hypertension | 117 (90%) | 19 (90.4%) | 98 (89.9%) | 1.0 |
| Ischemic heart disease | 106 (81.5%) | 17 (80.9%) | 89 (81.6%) | 1.0 |
| Atrial fibrillation | 88 (67.6%) | 7 (33.3%) | 81 (74.3%) | <0.001 |
| Diabetes mellitus | 39 (30%) | 12 (57.1%) | 27 (24.7%) | 0.007 |
| Renal impairment | 54 (41.5%) | 10 (47.6%) | 44 (40.3%) | 0.63 |
| Anemia | 19 (14.6%) | 1 (4.7%) | 18 (16.5%) | 0.3 |
| ASA 2 | 10 (7.6%) | 0 | 10 (9.1%) | 0.36 |
| ASA 3 | 86 (66.1%) | 15 (71.4%) | 71 (65.1%) | 0.62 |
| ASA 4 | 34 (26.1%) | 6 (28.5%) | 28 (25.6%) | 0.78 |
| Upper limb ALI | 32 (23%) | 6 (26%) | 26 (22.4%) | 0.78 |
| Lower limb ALI | 107 (76.9%) | 17 (73.9) | 90 (77.5%) | 0.78 |
|
20 (18.6%) | 4 (23.5%) | 16 (17.7%) | 0.51 |
|
87 (81.3%) | 13 (76.4%) | 74 (82.2%) | 0.51 |
| Native artery occlusion | 135 (97.1%) | 23 (100%) | 112 (96.5%) | 1.0 |
| Stent/bypass occlusion | 4 (2.8%) | 0 | 4 (2.8%) | 1.0 |
| Embolism | 97 (69.7%) | 11 (47.8%) | 86 (74.1%) | 0.02 |
| Thrombosis | 37 (26.6%) | 12 (52.1%) | 25 (21.5%) | 0.004 |
| Popliteal artery aneurysm | 5 (3.5%) | 0 | 5 (4.3%) | 0.59 |
| Duration of ALI (hr) | 20 (6–96) | 16 (6.5–24) | 22.5 (5–96) | 0.47 |
| Rutherford I | 8 (5.7%) | 1 (4.3%) | 7 (6%) | 1.0 |
| Rutherford IIA | 43 (30.9%) | 6 (26%) | 37 (31.8%) | 0.8 |
| Rutherford IIB | 88 (63.3%) | 16 (69.5%) | 72 (62%) | 0.6 |
| Mean ABI | 0.04 ± 0.13 | 0.05 ± 0.19 | 0.03 ± 0.12 | 0.5 |
| NLR | 6.8 (3.4–12) | 11.1 (5.3–24.5) | 6.3 (3.4–11) | 0.01 |
| D-dimer (ng/mL) | 1,070 (420–3,265) | 2,600 (660–7,400) | 925 (325–2,755) | 0.08 |
| Myoglobin (ng/mL) | 157 (73–391) | 181 (31–653) | 155 (77–325) | 0.77 |
| C reactive protein (mg/L) | 30 (9–72) | 57 (34–119) | 25 (6–48) | 0.001 |
| Cardiac troponin I (ng/ml) | 0.43 ± 1.18 | 0.68 ± 1.96 | 0.4 ± 1.05 | 0.59 |
| Serum lactate (mmol/L) | 2.0 (1.8–2.3) | 2.1 (2.0–2.4) | 2.0 (1.8–2.2) | 0.15 |
Continuous variables presented as median (25–75 IQR) or mean (±SD) values.
Categorical variables are calculated per patient or per limb as appropriate.
A P values of less than 0.05 are marked with bold (statistically significant differences).
ASA, American Society of Anesthesiologists; IQR, interquartile range and SD, standard deviation.
Group A versus group B.
The laboratory data reflected marked systemic inflammatory reaction among patients with COVID-19. Median values of neutrophil to lymphocytes ratio (NLR) and C-reactive protein were significantly higher in group A compared to group B: 11.1 (5.3–24.5) vs. 6.3 (3.4–11), P = 0.01 and 57 (34–119) mg/L vs. 25 (6–48) mg/L, P = 0.001, respectively. No difference between groups was found comparing the level of D-dimers and biomarkers of ischemia: myoglobin, cardiac troponin I, and serum lactate.
The median time from the debut of COVID-19 to the clinical manifestations of ALI was 13 (10–17) days. Twelve patients (57.1%) in group A developed ALI during the in-hospital treatment for COVID-19 and were transferred from other institutions. At the moment of presentation to the vascular service 11 (52.3%) patients had symptomatic COVID-19 status, and 12 (57.1%) patients were considered in severe condition and admitted to the dedicated intensive care unit (ICU). Pulmonary involvement characteristic for SARS-CoV-2 infection was diagnosed on radiography in 15 (71.4%) cases with median Brixia score of 7 (3–11) points. It should be mentioned that 20 (95.2%) patients in group A were not vaccinated against COVID-19, and 1 patient had an incomplete vaccination scheme.
Treatment of ALI
Data regarding management of ALI are summarized in Table II . Patients with COVID-19 had significantly shorter time from ALI onset till administration of the first dose of anticoagulant: 8 (2.5–24) hr vs. 15.7 (6–72) hr in group B, P = 0.02. Vascular imaging was performed before intervention only in 5 (23.8%) infected patients compared to 78 (71.5%) patients in group B, P < 0.001. There were no significant differences in characteristics of surgical procedures, anesthesia, and postoperative management with exception of more frequent use of unfractionated heparin in group A.
Table II.
Management of acute limb ischemia
| Variable | Total |
Group A |
Group B |
P valuea |
|---|---|---|---|---|
| (130 pts, 139 limbs) | (21 pts, 23 limbs) | (109 pts, 116 limbs) | ||
| Time from symptoms to anticoagulation (hr) | 14 (6–62) | 8 (2.5–24) | 15.7 (6–72) | 0.02 |
| Time from presentation to intervention (hr) | 3 (2–7) | 2 (2–5) | 3 (2–8) | 0.42 |
| Vascular imaging (any) | 83 (63.8%) | 5 (23.8%) | 78 (71.5%) | <0.001 |
|
53 (40.7%) | 2 (9.5%) | 51 (46.7%) | 0.001 |
|
51 (39.2%) | 4 (19%) | 47 (43.1%) | 0.05 |
| Local anesthesia | 54 (41.5%) | 10 (47.6%) | 44 (40.3%) | 0.63 |
| Spinal anesthesia | 68 (52.3%) | 10 (47.6%) | 58 (53.2%) | 0.81 |
| General anesthesia | 8 (6.1%) | 1 (4.7%) | 7 (6.4%) | 1.0 |
| Thromb (embol) ectomy | 122 (87.7%) | 23 (100%) | 99 (85.3%) | 0.07 |
| Bypass/endarterectomy | 12 (8.6%) | 0 | 12 (10.3%) | 0.21 |
| Percutaneous revascularization | 5 (3.5%) | 0 | 5 (4.3%) | 0.59 |
| Fasciotomy | 22 (15.8%) | 2 (8.6%) | 20 (17.2%) | 0.53 |
| Duration of surgery (min) | 70 (60–100) | 80 (70–90) | 70 (60–108) | 0.39 |
| Postoperative anticoagulation | ||||
|
45 (34.6%) | 12 (57.1%) | 33 (30.2%) | 0.02 |
|
85 (65.3%) | 9 (42.8%) | 76 (69.7%) | 0.02 |
| Antithrombotic drug at dischargeb | ||||
|
14/104 | 0/12 | 14/92 | 0.35 |
|
85/104 | 12/12 | 73/92 | 0.66 |
|
5/104 | 0/12 | 5/92 | 1.0 |
Continuous variables presented as medians (25–75 IQR). IQR, interquartile range
Categorical variables are calculated per patient or per limb as appropriate.
A P values of less than 0.05 are marked with bold (statistically significant differences).
CTA, computed tomography angiography; LMWH, low molecular weight heparin; SAPT, single antiplatelet therapy; DAPT, double antiplatelet therapy; OAK, oral anticoagulants (warfarin or rivaroxaban); DPI, dual pathway inhibition (rivaroxaban + aspirin).
Group A versus group B.
Denominator is a number of survivors.
Primary Outcome
Overall, the composite endpoint of major amputation and/or death at 30 days after surgery was registered in 38 (29.2%) patients, significantly more frequent in infected cohort: 12 (57.1%) patients in group A versus 26 (23.8%) patients in group B, RR 2.3 (95% confidence interval [CI]: 1.45–3.94), P < 0.001. Difference in composite outcome was preponderantly caused by extremely high mortality in group A–9 (42.8%) patients, compared to 17 (15.5%) patients in group B, P = 0.01. The difference in rate of limb loss was not statistically significant: 4 (17.3%) limbs were amputated in COVID-19 patients and 12 (10.3%) limbs–in noninfected patients (P = 0.3). Thus, among patients undergoing open revascularization combination of ALI and COVID-19 resulted in increased 30-day mortality–RR: 2.7 (95% CI: 1.42–5.31), P = 0.002, but did not lead to significantly higher amputation rate–RR: 1.6 (95% CI: 0.59–4.75), P = 0.32.
In the entire study cohort, 4 variables demonstrated statistically significant association with composite primary outcome in univariable analysis and were subsequently included in multivariable model (Table III ). Results of logistic regression analysis demonstrated significant association of COVID-19 and NLR value on admission of >5.4 with negative outcome of ALI treatment. In group A initial admission of the patient in the ICU was an independent risk factor for amputation or/and death.
Table III.
Factors significantly associated with 30-days composite outcome of major amputation and/or death (general cohort and patients with COVID-19)
| General cohort (groups A and B) | ||||||
|---|---|---|---|---|---|---|
| Variable | Univariate analysis |
Multivariate analysisa |
||||
| OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Atrial fibrillationb | 0.37 | 0.17–0.81 | 0.01 | - | - | - |
| Embolism | 0.31 | 0.14–0.69 | 0.02 | 0.51 | 0.21–1.25 | 0.14 |
| COVID-19 | 4.25 | 1.61–11.22 | 0.002 | 3.17 | 1.13–8.91 | 0.02 |
| NLR >5.4 | 23.4 | 8.59–63.6 | <0.0001 | 2.46 | 1.0–6.03 | 0.04 |
| COVID-19 patients (group A) | ||||||
| Brixia score ≥8 | 25.9 | 1.2–546.6 | 0.03 | 45.8 | 0.001–798 | 0.99 |
| ICU admission | 16.5 | 1.76–154 | 0.01 | 32 | 1.56–656 | 0.02 |
A P values of less than 0.05 are marked with bold (statistically significant differences).
Binary logistic regression.
Variable was not included in multivariate analysis due to high correlation with embolism (risk of multicollinearity).
Secondary Outcomes
Excepting systemic complications which were more frequently registered among COVID-19 patients: 7 (33%) cases vs. 14 (12.8%) in group B, P = 0.04; no differences in other secondary outcomes were observed between groups. The median value of postoperative ABI in group A was 1.0 (0.3–1.0) vs. 0.94 (0.58–1.0) in group B, P = 0.89; local complications rate–33.3% vs. 21 (19.2%), P = 0.15; reintervention rate–2 (8.6%) vs. 11 (9.4%), P = 1.0; and length of hospitalization – 6 (3–12) vs. 6 (4–9) days, P = 0.76, respectively.
Discussion
Three systematic reviews regarding management of ALI in COVID-19 patients were published during 2021–2022 summarizing the results of 36, 9, and 11 studies, respectively.11, 12, 13 Single metanalysis performed by Jain et al., included 11 articles that reported data on 196 patients with ALI and SARS-CoV-2 infection.13 At the moment only 4 published studies have directly compared outcomes of ALI treatment (amputation, rethrombosis, and mortality) in COVID-19 positive and COVID-19 negative patients.14, 15, 16, 17 Thus, our prospective study with a sample size of 21 infected and 109 noninfected patients undergoing urgent revascularization procedure in a single tertiary institution can provide some additional data to this important issue.
Clinical and demographic characteristics of the patients with ALI and COVID-19 in our study were similar to those reported by others.11 , 12 , 18 The majority of patients were male in a seventh decade of their life and with multiple comorbidities. Diabetes mellitus, hypertension, ischemic heart disease, and chronic renal disease were diagnosed more frequently compared to the data provided by Bellosta et al.19 We found that COVID-19 positive patients had lower rate of atrial fibrillation and, respectively, of embolic cause of ALI compared to the noninfected group. This observation may reflect the dominant role of endothelial injury and hypercoagulability in development of SARS-CoV-2 associated thrombosis.
Acute arterial occlusion mostly involved infra-inguinal segment, leading to immediately threatened limb ischemia (Rutherford IIB category) in almost 70% of the cases. Upper limb ischemia was diagnosed approximately in one-quarter of observations. Other authors11 , 17 provide similar results with exception of the study published by Sekar et al., where only 29% of cases were categorized as Rutherford IIB.18 It is worth to mention that in our study anatomic location of arterial occlusion, severity, and duration of ischemia were similar in infected and noninfected patients as well as mean preoperative ABI value. In contrast, Soares et al., reported mean preoperative ABI of 0.35 in noninfected patients (39% of cases with viable limb–category Rutherford I) compared to mean ABI of 0.05 in patients with COVID-19.17
The pandemic of SARS-CoV-2 profoundly affected the logistics of medical care, mostly during the first waves–until wide implementation of testing and vaccination. Some authors reported significant delay in ALI treatment among infected patients.18 Vice versa, in our study patients from group A arrived in emergency vascular service nearly 2 times faster compared to noninfected cohort. This difference could be explained by the fact that 57% of the patients with SARS-CoV-2 infection developed ALI during in-hospital treatment for COVID-19. Vascular imaging was performed preoperatively in significantly smaller proportion of the patients in group A, especially DUS. However, there was no significant association of skipped vascular imaging and amputation-free survival at 30 days: OR: 1.2 (95% CI: 0.56–2.66), P = 0.61. Positive COVID-19 status influenced the type and volume of surgical revascularizations. As it’s shown in Table II, infected patients were not treated with percutaneous techniques, and no surgical bypasses were performed in this group. This fact theoretically can be explained by several issues: limited access to the endovascular suite, attempts of operating surgeon to minimize the volume of intervention in a critically ill patient, technical difficulty of complex arterial reconstruction performed using personal protective equipment, awareness about reduced success rate of revascularization in this category of patients, and so on.
Reported outcomes of ALI treatment in patients with COVID-19 are not uniform. While many studies6 , 19, 20, 21, 22 highlight excessive rate of major amputations (around 60–70%) and mortality (nearly 40–50%), especially in early stage of pandemic, other authors provide more optimistic results.14 , 16 , 23 The 30-day mortality rate of 42.8% observed in our study in group A was close to the upper limit of 95% CI, determined for overall mortality in the metanalysis by Jain et al.,—0.33 (95% CI: 0.25–0.42); while the rate of major amputations was lower—17.3% in our study versus 43% according to pooled results.13 However, this data should be interpreted with caution due to high grade of heterogeneity characteristic for studies included in metanalysis. The mortality rate in COVID-19 patients could be hardly influenced by comorbidities, grade of pulmonary involvement, types of SARS-CoV-2 and vaccination status, rather than by direct consequences of ALI. Furthermore, rate of amputations depends on the following: proportion of upper and lower limbs in study cohort, severity of ischemia, type of treatment (revascularization versus conservative), duration of follow-up and other. Thus, direct comparison of the outcomes between studies usually is not possible.
Comparative studies that include both infected and noninfected patients with ALI provide the opportunity for determination of factors associated with treatment outcomes. Our results generally are in consonance with those reported by other investigators. Positive COVID-19 status was significantly associated with mortality in current study (OR: 4.0, 95% CI: 1.48–11.1), in the comparison study of Soares et al., (hazard ratio: 1.8, 95% CI: 1.0–4.0)17 and according to the results of the single metanalysis available at the moment (pooled OR: 4.71, 95% CI: 1.1–19.9).13 While in some studies COVID-19 was an independent predictor of limb loss,17 our data (OR: 1.8, 95% CI: 0.5–6.2) and results of the metanalysis (OR: 0.26, 95% CI: 0.02–3.0) have not demonstrated significant association between these variables.
In study of Soares et al., the D-dimers level >1,000 md/dL was independently associated with mortality and limb loss in multivariable analysis.17 Our data did not demonstrate a statistically significant impact of D-dimers level upon probability of the composite outcome. However, we found that NLR of more than 5.4 was an important predictor of unfavorable results of ALI treatment in general cohort of the patients: OR: 2.4 (95% CI: 1.0–6.0). Subgroup analysis in patients with COVID-19 and ALI provided the statistically insignificant result (OR: 8.8, P = 0.07), probably due to small sample size. During the last years, several studies have demonstrated good prognostic role of NLR in patients with ALI, with minimal difference in reported optimal cut-off values.24, 25, 26 Thus, in study of Taurino et al., the rate of amputation and mortality at 30 days among patients with NLR >5 was nearly 10 times higher compared to “low-NLR” group.24 In other study, based on the retrospective analysis of 345 patients with ALI, the NLR ≥5.4 had a 90.5% sensitivity and 73.6% specificity for composite endpoint of a 30-day death or amputation, as well as significant negative association with amputation-free survival at 6 months and 1 year.25 Recently, Pasqui et al., reported similar results using the cut-off NLR value of ≥ 5.57.26 At the moment, existing evidence confirms the important role of this simple and universally available biomarker of inflammation in decision-making process in patients with ALI.
Finally, it is important to note, that at the moment nearly all ALI cases associated with COVID-19 were reported among nonvaccinated patients and our study is not an exception.18 , 27 Based on this data and relying on high efficiency of current vaccines in prophylaxis of severe forms of COVID-19, the wide-scale vaccination seems to be an important measure in prevention of cases with dangerous combination of ALI and SARS-CoV-2 infection.
Strengths and Limitations
There are several weak points in the current study. The most important limitation is the small sample size with a very limited number of observations in the study group A (ALI and COVID-19). However, it is a common problem since majority of published studies in this field are based on comparable number of included patients. It should be mentioned that during the pandemic our institution was designated at the national level as a referral center for all emergency surgical patients infected with COVID-19. Thus, presented data potentially reflects nationwide experience from the Republic of Moldova. There is a chance that large international multicentric prospective registries (i.e., “Vascular Surgery COVID-19 Collaborative”) will provide significantly higher grade of evidence in the near future. The other limitation is a short-term follow-up and scarce data regarding the rate of re-thrombosis in group A due to limited access to postoperative imaging. Despite these limitations several strengths of present study could be mentioned: homogenous cohort of the patients (all cases were treated with urgent revascularization, while patients treated conservatively or with primary amputation were excluded) and prospective design of data collection.
Conclusions
Results of our study demonstrate the significant negative impact of positive COVID-19 status upon the 30-day amputation-free survival in patients undergoing urgent surgical revascularization for ALI. The difference in composite outcome of amputation and/or death is influenced by the higher rate of mortality among infected patients, rather than by the rate of limb loss, that in current study was not different from noninfected cohort. Since severity of COVID-19, namely requirement of critical care, mostly determines the outcome of ALI treatment, the prevention of severe forms of SARS-CoV-2 infection by vaccination could potentially improve the amputation-free survival in these patients.
Footnotes
Declaration of interest: None.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions: AP, DC, and VC researched literature, planned the study and elaborated the study protocol. AP and VC were involved in data acquisition and data analysis. AP and DC performed statistical analysis and wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval for research: Study protocol was approved by the Research Ethics Committee of State University of Medicine and Pharmacy “Nicolae Testemitanu”, Chisinau, Moldova.
References
- 1.Baril D.T., Ghosh K., Rosen A.B. Trends in the incidence, treatment, and outcomes of acute lower extremity ischemia in the United States Medicare population. J Vasc Surg. 2014;60:669–677. doi: 10.1016/j.jvs.2014.03.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poursina O., Elizondo-Adamchik H., Montero-Baker M., et al. Safety and efficacy of an endovascular-first approach to acute limb ischemia. J Vasc Surg. 2021;73:1741–1749. doi: 10.1016/j.jvs.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Yang P.K., Su C.C., Hsu C.H. Clinical outcomes of surgical embolectomy versus catheter-directed thrombolysis for acute limb ischemia: a nationwide cohort study. J Thromb Thrombolysis. 2022;53:517–522. doi: 10.1007/s11239-021-02532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warrior K., Chung P.A., Ahmed N., et al. Acute limb ischemia due to arterial thrombosis associated with coronavirus disease 2019. Crit Care Explor. 2020;2:e0140. doi: 10.1097/CCE.0000000000000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellosta R., Luzzani L., Natalini G., et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020;72:1864–1872. doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topcu A.C., Ozturk-Altunyurt G., Akman D., et al. Acute limb ischemia in hospitalized COVID-19 patients. Ann Vasc Surg. 2021;74:88–94. doi: 10.1016/j.avsg.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Attisani L., Pucci A., Luoni G., et al. COVID-19 and acute limb ischemia: a systematic review. J Cardiovasc Surg (Torino) 2021;62:542–547. doi: 10.23736/S0021-9509.21.12017-8. [DOI] [PubMed] [Google Scholar]
- 8.Jongkind V., Earnshaw J.J., Bastos Gonçalves F., et al. Editor's choice - update of the European society for vascular surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia in light of the COVID-19 pandemic, based on a scoping review of the literature. Eur J Vasc Endovasc Surg. 2022;63:80–89. doi: 10.1016/j.ejvs.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Björck M., Boyle J.R., Dick F. The need of research initiatives amidst and after the covid-19 pandemic: a message from the editors of the EJVES. Eur J Vasc Endovasc Surg. 2020;59:695–696. doi: 10.1016/j.ejvs.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Björck M., Earnshaw J.J., Acosta S., et al. European society for vascular surgery (ESVS) 2020 clinical practice guidelines on the management of acute limb ischaemia. Eur J Vasc Endovasc Surg. 2020;59:173–218. doi: 10.1016/j.ejvs.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Borghesi A., Maroldi R. COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med. 2020;125:509–513. doi: 10.1007/s11547-020-01200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanders I., Stather P., Sivagangan P., et al. The mysterious risk of arterial thrombosis with COVID-19: a case series and systematic review of acute limb ischaemia. Cureus. 2022;14:e25080. doi: 10.7759/cureus.25080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain A., Reddy A., Murugesan R., et al. Outcomes of patients with acute limb ischemia in patients with COVID-19: a systemic review and meta-analysis. Cureus. 2022;14:e27370. doi: 10.7759/cureus.27370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mascia D., Kahlberg A., Melloni A., et al. Single-center vascular hub experience after 7 weeks of COVID-19 pandemic in lombardy (Italy) Ann Vasc Surg. 2020;69:90–99. doi: 10.1016/j.avsg.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldman I.A., Ye K., Scheinfeld M.H. Lower-extremity arterial thrombosis associated with COVID-19 is characterized by greater thrombus burden and increased rate of amputation and death. Radiology. 2020;297:E263–E269. doi: 10.1148/radiol.2020202348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yesilkaya N., Tellioglu T.M., Unay F.C., et al. Histopathologic evaluation of COVID-19 patients with peripheral arterial thromboembolism: does clot composition make any sense? Ann Vasc Surg. 2021;74:80–87. doi: 10.1016/j.avsg.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Athayde Soares R., Futigami A.Y., Barbosa A.G., et al. Acute arterial occlusions in COVID-19 times: a comparison study among patients with acute limb ischemia with or without COVID-19 infection. Ann Vasc Surg. 2022;83:80–86. doi: 10.1016/j.avsg.2022.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sekar N., Jagan J., Viruthagiri A., et al. Management of acute limb ischaemia due to COVID-19 induced arterial thrombosis: a multi-centre Indian experience. Ann Vasc Dis. 2022;15:113–120. doi: 10.3400/avd.oa.22-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellosta R., Piffaretti G., Bonardelli S., et al. Regional survey in lombardy, northern Italy, on vascular surgery intervention outcomes during the COVID-19 pandemic. Eur J Vasc Endovasc Surg. 2021;61:688–697. doi: 10.1016/j.ejvs.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Indes J.E., Koleilat I., Hatch A.N., et al. Early experience with arterial thromboembolic complications in patients with COVID-19. J Vasc Surg. 2021;73:381–389.e1. doi: 10.1016/j.jvs.2020.07.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Zoubi N., Shatnawi N., Jarbo H. Acute lower limb ischemia in patients infected with COVID-19. Int J Gen Med. 2021;14:833–839. doi: 10.2147/IJGM.S301462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Etkin Y., Conway A.M., Silpe J., et al. Acute arterial thromboembolism in patients with COVID-19 in the New York city area. Ann Vasc Surg. 2021;70:290–294. doi: 10.1016/j.avsg.2020.08.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barac S., Onofrei R.R., Neagoe P.V., et al. An observational study on patients with acute limb ischemia and SARS-CoV-2 infection: early and late results in limb salvage rate. J Clin Med. 2021;10:5083. doi: 10.3390/jcm10215083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taurino M., Aloisi F., Del Porto F., et al. Neutrophil-to-Lymphocyte ratio could predict outcome in patients presenting with acute limb ischemia. J Clin Med. 2021;10:4343. doi: 10.3390/jcm10194343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coelho N.H., Coelho A., Augusto R., et al. Pre-operative neutrophil to lymphocyte ratio is associated with 30 Day death or amputation after revascularisation for acute limb ischaemia. Eur J Vasc Endovasc Surg. 2021;62:74–80. doi: 10.1016/j.ejvs.2021.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Pasqui E., de Donato G., Giannace G., et al. The relation between neutrophil/lymphocyte and platelet/lymphocyte ratios with mortality and limb amputation after acute limb ischaemia. Vascular. 2022;30:267–275. doi: 10.1177/17085381211010012. [DOI] [PubMed] [Google Scholar]
- 27.Xie B., Semaan D.B., Binko M., et al. COVID-19–Associated acute limb ischemia during the delta surge and effect of vaccines. J Vasc Surg. 2022;75:e128–e129. doi: 10.1016/j.jvs.2022.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]