Abstract
Background
There is a growing awareness of the heterogeneity of obstructive sleep apnoea (OSA). Clinical trials of CPAP treatment on cardiovascular protection have been mostly negative. We aimed to assess the association between polysomnographic parameters and incident major adverse cardiovascular events (MACEs), and to investigate if the CPAP effect could be better delineated among clinical subgroups.
Methods
This sleep cohort study was conducted using a clinical database and territory-wide electronic health administration data in Hong Kong. Cox regressions were used to calculate HRs. Latent class analysis was used to cluster patients with OSA according to clinical and polysomnographic features.
Results
Of 1860 eligible Chinese subjects who underwent polysomnography (2006–2013), 1544 (83%) had OSA. Over median follow-up of 8.3 years, 278 (14.9%) experienced MACEs. Apnoea–hypopnoea index (AHI) did not predict MACEs (HR: 0.95; 95% CI 0.76 to 1.17), whereas sleep time with oxygen saturation <90% (TST90) (HR: 1.41; 95% CI 1.10 to 1.81) was an independent predictor of MACEs, as were wake and nocturnal heart rate. In moderate–severe OSA (n=1108) who were indicated for CPAP treatment, regular CPAP was not associated with reduction of incident MACEs. Further cluster analysis identified a subgroup (n=333) who was younger, more obese, had more severe OSA (higher AHI and TST90) and more cardiovascular risks, in whom regular CPAP was associated with a lower risk of MACEs (HR:0.49, 95% CI 0.25 to 0.95).
Conclusions
OSA-related TST90 and mean heart rate, but not AHI, were robust predictors of MACEs. A clinical phenotype subgroup who demonstrated beneficial effect of CPAP treatment was identified.
Keywords: sleep apnoea
Key messages.
What is the key question?
Can routine polysomnographic (PSG) data independently predict cardiovascular endpoints, and would long-term CPAP treatment of obstructive sleep apnoea (OSA) according to widely used PSG and/or other clinical parameters be associated with lower risk of adverse cardiovascular events?
What is the bottom line?
Sleep-apnoea related hypoxia and mean heart rate, but not apnoea–hypopnoea index (AHI) are likely to be dominant predictors of adverse cardiovascular outcomes. Not all patients with moderate–severe OSA according to AHI criteria benefited uniformly from regular CPAP therapy, but those who were younger with greater nocturnal hypoxaemia, higher AHI and other concurrent cardiovascular risk factors demonstrated a lower incidence of cardiovascular events with regular CPAP treatment.
Why read on?
Data from clinical trials has been controversial and largely negative regarding cardiovascular protection, and this study addresses the prognostication ability of different sleep indices as well as differential patient cluster response to CPAP therapy in terms of incident major cardiovascular events using a sleep clinic population.
Introduction
Untreated obstructive sleep apnoea (OSA) is believed to lead to a cluster of serious adverse health sequelae, particularly in the context of cardiovascular morbidity and mortality.1 Many OSA cohorts studying cardiovascular endpoints have drawn positive conclusions or at least in some OSA subgroups.2–6 However, the modifying effect of CPAP treatment of OSA on cardiovascular outcomes is highly controversial. Several large randomised controlled trials (RCTs) have reported negative results, in terms of either primary or secondary cardiovascular prevention by treatment of OSA with CPAP.7–10
To date, the apnoea–hypopnoea index (AHI) remains the key parameter on which severity of OSA is categorised, in turn guiding physician prescription for CPAP therapy. However, it has long been observed that the pathophysiology downstream of sleep disordered breathing resulting in adverse health outcomes may not be adequately reflected by AHI on polysomnograms (PSG).11 Furthermore, due to the heterogeneity among OSA subjects, it is increasingly recognised that the effect of CPAP on health outcomes may not be uniform across the entire spectrum of OSA population. The aims of the current study were to determine the association between various polysomnographic measures of OSA and incident major adverse cardiovascular events (MACEs) in a sleep clinic cohort, and to evaluate the impact of CPAP therapy which has been prescribed per usual criteria in consensus recommendations, based on consideration of AHI, symptoms and background cardiovascular disease (CVD) risks.12
Methods
Study design and subjects
This was a clinic-based retrospective cohort study. The target cohort was drawn from those seen at the Department of Medicine, and received first diagnostic sleep studies between 1 January 2006 and 31 December 2013 at the Ho Ting Sik Sleep Disorders Centre, Queen Mary Hospital. Subjects were excluded if they had non-Chinese ethnicity; sleep disorders other than OSA; invalid or incomplete record; treatment other than CPAP; or conditions with known effect on OSA.
Data sources
Baseline clinical data were derived from protocolised questionnaires implemented as part of clinical routine to all subjects undergoing sleep studies (see online supplemental materials for details of variables).
thoraxjnl-2021-217714supp001.pdf (347.6KB, pdf)
Follow-up data were drawn from the Hong Kong Hospital Authority (HA) Clinical Management System up to the day of data entry. This territory-wide system covers all electronic patient records (ePR) of those who attend HA healthcare facilities (hospitals and clinics). CPAP adherence data were extracted from both the ePR and paper records which would contain periodic objective data from CPAP device and protocolised nurse evaluation of CPAP usage. The details of data acquisition regarding this historical cohort have been published previously.13
Overnight PSG data have been stored on electronic files and were manually scored or rescored according to American Academy of Sleep Medicine 2012 criteria.14
CPAP compliance
For this study, CPAP compliance was dichotomised into regular use or not. Regular use was defined as average use ≥4 hours/night for >70% of the follow-up period, or on average of >4 hours per night (for CPAP devices which only provided cumulative hours of use), and these patients were classified as ‘treated’. Others with no or less than regular use, or defaulted CPAP clinic follow-up, were classified as ‘untreated’.
Study outcome
The primary outcome was time from the baseline diagnostic PSG to the first confirmed (adjudicated) event of the MACE composite endpoint. Fatal MACEs were deaths from CVDs. Non-fatal MACEs were defined as the first hospitalisation due to acute coronary syndrome (acute myocardial infarction and unstable angina), revascularisation procedures (percutaneous coronary intervention and coronary artery bypass grafting), stroke or exacerbation of congestive heart failure. Censoring occurred on the day of data entry for those who did not develop the outcome of interest, or last clinical visit for those lost to follow-up or the date of death whichever occurred first.
Statistical analysis
Sleep and other measures were summarised using summary statistics. Bonferroni adjustment for multiple tests was applied for comparison within cluster groups. Multiple imputation was conducted to handle missing data. Cox regression models were constructed to assess the association between OSA and MACEs in the entire dataset and the untreated subgroup. Multivariable models were estimated with adjustment for known cardiovascular risk factors captured in the study (see table 1 and online supplemental material).
Table 1.
Characteristics of study patients in total and by incident major adverse cardiovascular events (MACEs) (n=1860)
| Variables | Total (n=1860) |
Incident case (n=278) |
Event free (n=1582) |
P for difference |
| Demographics | ||||
| Male, n (%) | 1236 (66.5%) | 200 (71.9%) | 1036 (65.5%) | 0.042 |
| Age, year | 52.4 (12.2) | 59.0 (12.2) | 51.2 (11.9) | <0.001 |
| Symptom and measures | ||||
| BMI, kg/m2 | 27.7 (5.3) | 28.0 (5.0) | 27.7 (5.4) | 0.367 |
| Neck circumference, cm | 38.4 (4.0) | 39.3 (4.7) | 38.3 (3.9) | 0.001 |
| Waist circumference, cm | 93.1 (12.4) | 95.2 (11.2) | 92.7 (12.6) | <0.001 |
| Hip circumference, cm | 99.3 (9.8) | 98.5 (9.1) | 99.4 (9.9) | 0.130 |
| Epworth Sleepiness Scale | 8.7 (5.4) | 8.4 (5.5) | 8.7 (5.3) | 0.307 |
| Polysomnogram | ||||
| TST, min | 422.0 (371.5–458.5) | 407.5 (356.0–455.0) | 423.0 (373.6–459.0) | 0.039 |
| AHI, /hour | 21.7 (8.0–46.9) | 28.3 (10.3–52.9) | 20.5 (7.5–45.8) | 0.003 |
| REM-AHI, /hour | 30.9 (11.2–54.3) | 36.9 (15.0–57.2) | 30.0 (10.8–54.0) | 0.052 |
| 3% ODI, /hour | 16.4 (4.8–41.0) | 22.9 (8.5–49.3) | 15.6 (4.4–39.0) | <0.001 |
| Mean SpO2, % | 95.0 (93.7–96.0) | 94.7 (93.1–96.0) | 95.0 (93.8–96.1) | <0.001 |
| Min SpO2, % | 81.0 (71.0–87.0) | 79.0 (68.0–86.0) | 81.0 (72.0–87.0) | 0.005 |
| TST90, min | 6.8 (0.7–36.4) | 17.1 (1.9–56.9) | 5.8 (0.6–30.7) | <0.001 |
| Arousal Index, /hour | 19.0 (11.8–31.0) | 21.8 (14.0–36.2) | 18.4 (11.3–30.2) | <0.001 |
| Mean AHD, s | 22.5 (18.9–26.8) | 22.2 (18.8–26.4) | 22.5 (18.9–26.8) | 0.553 |
| Nocturnal MHR, /min | 63.8 (58.5–70.1) | 65.7 (58.3–71.9) | 63.8 (58.5–69.8) | 0.048 |
| Wake MHR, /min | 69.2 (63.0–75.7) | 71.0 (62.9–79.1) | 68.9 (63.0–75.3) | 0.016 |
| History | ||||
| Prior hypertension, n (%) | 1187 (63.8%) | 229 (63.8%) | 958 (60.6%) | <0.001 |
| Prior diabetes, n (%) | 586 (31.5%) | 138 (31.5%) | 447 (28.3%) | <0.001 |
| Fasting glucose, mmol/L | 5.4 (4.9–6.5) | 5.9 (5.0–7.7) | 5.4 (4.9–6.4) | <0.001 |
| Prior hyperlipidaemia, n (%) | 614 (33.0%) | 116 (33.0%) | 498 (31.5%) | 0.001 |
| Total cholesterol, mmol/L | 4.9 (4.2–5.6) | 4.8 (4.1–5.5) | 4.9 (4.3–5.6) | 0.262 |
| Triglycerides, mmol/L | 1.6 (1.1–2.2) | 1.6 (1.2–2.3) | 1.6 (1.1–2.2) | 0.110 |
| Prior CVDs, n (%) | 232 (12.5%) | 77 (27.7%) | 155 (9.8%) | <0.001 |
| Statin use, n (%) | 442 (23.8%) | 92 (33.1%) | 350 (22.1%) | <0.001 |
| Beta blocker use, n (%) | 442 (23.8%) | 118 (42.4%) | 324 (20.5%) | <0.001 |
| Family history of CVD, n (%) | 466 (25.1%) | 75 (25.1%) | 391 (24.7%) | 0.467 |
| Cigarette smoking, n (%) | <0.001 | |||
| No | 1262 (67.8%) | 161 (57.9%) | 1101 (69.6%) | |
| Former | 263 (14.1%) | 47 (16.9%) | 216 (13.7%) | |
| Current | 332 (17.8%) | 69 (24.8%) | 263 (16.6%) | |
| Alcohol use, n (%) | 0.014 | |||
| No | 1411 (75.8%) | 198 (71.2%) | 1213 (76.7%) | |
| Former | 314 (16.9%) | 49 (17.6%) | 265 (16.8%) | |
| Current | 127 (6.8%) | 30 (10.8%) | 97 (6.1%) | |
| Physical activity, n (%) | 0.028 | |||
| Low | 1199 (64.5%) | 198 (71.2%) | 1001 (63.3%) | |
| Medium | 542 (29.1%) | 63 (22.7%) | 479 (30.3%) | |
| High | 101 (5.4%) | 14 (5.0%) | 87 (5.5%) | |
| Education level, n (%) | <0.001 | |||
| Primary or below | 501 (26.9%) | 109 (39.2 %) | 392 (24.8%) | |
| Secondary | 827 (44.5%) | 111 (39.9%) | 716 (45.3%) | |
| Tertiary | 529 (28.4%) | 57 (20.5%) | 472 (29.8%) | |
| Body weight change*, kg | 1.4 (6.4) | 0.8 (6.2) | 1.5 (6.5) | 0.127 |
| Regular CPAP use, n (%) | 293 (15.8%) | 42 (15.1%) | 251 (15.9%) | 0.818 |
| Follow-up time, months | 99.5 (70.6–122.9) | 53.9 (26.0–75.7) | 104.2 (80.3–125.6) | <0.001 |
Data are given as mean (SD), median (IQR) or n (%).
Numbers may not add to total because of missing values.
*Body weight change was defined as body weight at endpoint or censoring minus baseline body weight.
AHD, apnoea–hypopnoea duration; AHI, apnoea–hypopnoea index; BMI, body mass index; CVDs, cardiovascular diseases; MACEs, major adverse cardiovascular events; MHR, mean heart rate; ODI, oxygen desaturation index; OSA, obstructive sleep apnoea; REM-AHI, apnoea–hypopnoea index during rapid eye movement sleep; SpO2, peripheral capillary oxygen saturation; TST90, sleep time with oxygen saturation below 90; TST, total sleep time.
To investigate the effect of CPAP therapy on MACEs, Cox regression on CPAP compliance, with and without adjustment of potential confounders was conducted. We further used the latent class analysis (LCA)15 to cluster the patients with moderate–severe OSA into subgroups based on the most informative indicators which were selected from least absolute shrinkage and selection operator (LASSO) regression.16
Sensitivity analyses included the following: Fine and Gray regressions were processed to treat 96 competing deaths rather than censoring; landmark analyses were performed at half year and 1 year (landmark time) to avoid the potential immortal time bias introduced by CPAP compliance; the associations between PSG parameters and MACEs was evaluated in the subgroup of non-obese OSA subjects and the outcome of non-fatal MACEs; for a unified presentation of the results, the findings were shown by a single imputed dataset. Analyses in different multiple-imputed datasets or complete-data analysis were also conducted.
Results from Cox regression were presented as HR with 95% CI. All statistical analyses were conducted using R (V.3.4.3). Details of statistical analysis are provided in the online supplemental file.
Results
Sample characteristics
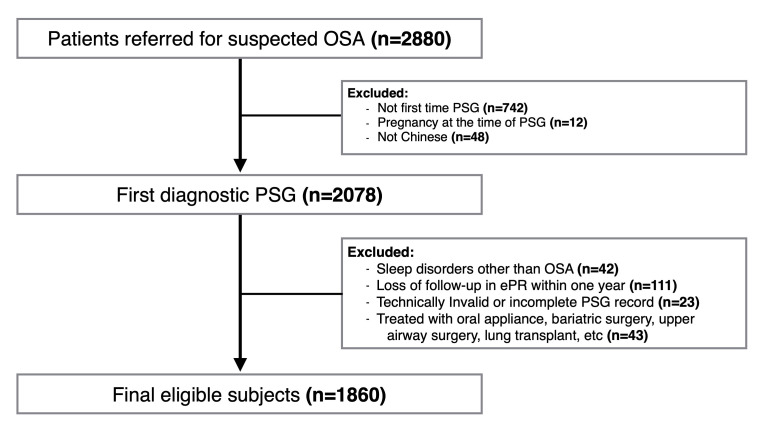
From 2006 to 2013, 2880 cases underwent PSG at our sleep clinic, and 1860 subjects meeting the criteria were included in the analysis (figure 1). Clinical characteristics of the sample are summarised in table 1. A total of 1236 (66.5%) were men, with a mean age of 52.4±12.2 years, mean BMI of 27.7±5.3 kg/m2 (obesity is defined as BMI ≥25 kg/m2 for subjects in Hong Kong), and median AHI of 21.7/hour. The amount of missing PSG data ranged from 0.16% (Min SpO2) to 3.8% (AHI during rapid eye movement sleep (REM-AHI)). Over a median follow-up of 100 months (IQR, 71–123 months), 278 (14.9%) subjects developed fatal and non-fatal MACEs, giving an incidence rate of 1.95 (95% CI 1.73 to 2.19) per 100 person years.
Figure 1.
Flow chart of the study cohort. ePR, electronic patient record; OSA, obstructive sleep apnoea; PSG, polysomnography.
Of these 278 cases who developed incident MACEs, 56 (20.1%) had acute coronary syndrome, 87 (31.3%) had revascularisation procedure, 54 (19.4%) had stroke, 54 (19.4%) had congestive heart failure and 27 (9.7%) died due to cardiovascular-related cause. Besides, 96 subjects died due to other reasons.
AHI as a predictor of MACEs
The incidence rates of MACEs per 100 person years with (95% CI) in patients with no, mild, moderate or severe OSA were 1.19 (0.82 to 1.66), 1.83 (1.42 to 2.33), 1.93 (1.47 to 2.50) and 2.40 (2.01 to 2.84), respectively, but the risk of MACEs in severe OSA by category was no longer different from no OSA after adjustment. AHI as a continuous variable was significantly associated with incident outcomes in the univariable Cox model (table 2), but the magnitude was reduced after adjustment for age (HR: 1.22, 95% CI 1.23 to 1.46) and was not significant after adjustment for gender, BMI and other cardiovascular confounders (HR: 0.95, 95% CI 0.76 to 1.17).
Table 2.
Cox regression analysis: associations of polysomnographic parameters and incident MACEs
| PSG parameters | Univariable model | Multivariable model* |
| HR (95% CI) | HR (95% CI) | |
| Total dataset (n=1860) | ||
| AHI (46.9 vs 8.0) | 1.24 (1.05 to 1.45) | 0.95 (0.76 to 1.17) |
| REM-AHI (54.4 vs 11.1) | 1.19 (0.98 to 1.44) | 1.03 (0.80 to 1.31) |
| 3% ODI (41.3 vs 4.9) | 1.24 (1.07 to 1.44) | 1 (0.82 to 1.22) |
| Mean AHD (26.8 vs 18.9) | 1.02 (0.88 to 1.18) | 0.96 (0.82 to 1.13) |
| TST90† (36.4 vs 0.7) | 1.10 (1.05 to 1.16) | 1.41 (1.10 to 1.81) |
| Mean SpO2 (96.0 vs 93.7) | 0.89 (0.83 to 0.96) | 0.99 (0.89 to 1.10) |
| Min SpO2 (87.0 vs 71.0) | 0.86 (0.75 to 0.97) | 0.99 (0.85 to 1.15) |
| Arousal index (30.9 vs 11.8) | 1.18 (1.06 to 1.32) | 1.03 (0.90 to 1.17) |
| Nocturnal MHR (70.2 vs 58.5) | 1.21 (1.05 to 1.40) | 1.27 (1.10 to 1.46) |
| Wake MHR (75.7 vs 63.1) | 1.24 (1.07 to 1.42) | 1.30 (1.12 to 1.50) |
| Untreated subset (n=1567) | ||
| AHI (39.4 vs 6.3) | 1.31 (1.12 to 1.52) | 0.99 (0.81 to 1.22) |
| REM-AHI (51.0 vs 8.9) | 1.27 (1.04 to 1.56) | 1.06 (0.82 to 1.38) |
| 3% ODI (34.0 vs 3.8) | 1.29 (1.12 to 1.47) | 1.03 (0.86 to 1.24) |
| Mean AHD (26.5 vs 18.7) | 0.97 (0.83 to 1.14) | 0.93 (0.78 to 1.11) |
| TST90† (25.4 vs 0.3) | 1.09 (1.05 to 1.13) | 1.46 (1.14 to 1.86) |
| Mean SpO2 (96.2 vs 9.0) | 0.89 (0.82 to 0.95) | 0.99 (0.89 to 1.11) |
| Min SpO2 (88.0 vs 74.0) | 0.82 (0.73 to 0.92) | 0.96 (0.83 to 1.10) |
| Arousal index (27.4 vs 11.0) | 1.23 (1.11 to 1.37) | 1.08 (0.95 to 1.22) |
| Nocturnal MHR (70.0 vs 58.6) | 1.29 (1.12 to 1.49) | 1.33 (1.15 to 1.54) |
| Wake MHR (75.7 vs 63.0) | 1.33 (1.15 to 1.54) | 1.38 (1.19 to 1.61) |
These PSG parameters were modelled separately. The PSG variables are compared by 75th versus 25th percentiles.
Bold font indicates statistical significance.
*Multivariable models adjusted for age, gender, body mass index, neck circumference, waist circumference, body weight change, Epworth sleepiness scale, total sleep time, cigarette smoking, alcohol use, physical activity, prior hypertension, prior cardiovascular disease, prior hyperlipidaemia and prior diabetes.
†TST90 with non-linearity was transformed using restricted cubic spline transformation with three knots at default 0.1, 0.5 and 0.9 quantiles.
AHD, apnoea–hypopnoea duration; AHI, apnoea–hypopnoea index; BMI, body mass index; HR, hazard ratio; MACEs, major adverse cardiovascular events; MHR, mean heart rate; ODI, oxygen desaturation index; OSA, obstructive sleep apnoea; PSG, polysomnography; REM-AHI, apnoea–hypopnoea index during rapid eye movement sleep; SpO2, peripheral capillary oxygen saturation; TST90, sleep time with oxygen saturation below 90%; TST, total sleep time.
Other PSG parameters as predictors of MACEs
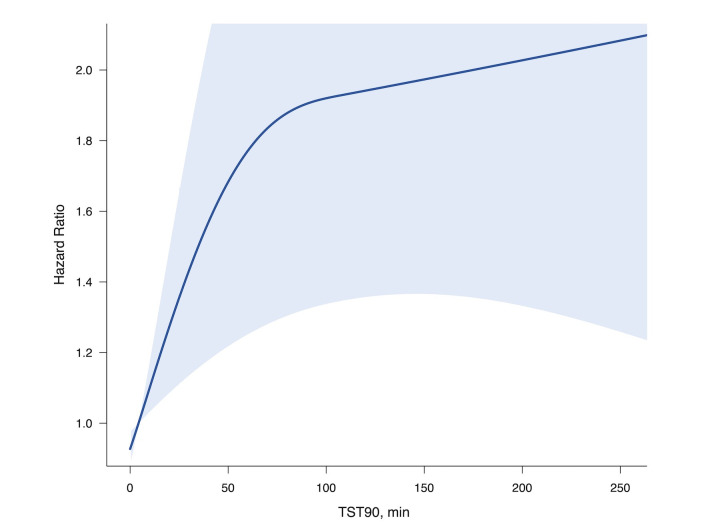
Sleep time with oxygen saturation below 90% (TST90), mean heart rate (MHR), oxygen desaturation index (ODI), REM-AHI and arousal index were significant predictors of MACEs in the univariable Cox models. To allow for the non-linear association between TST90 and its HR of MACEs (figure 2). Cubic spline transformations were conducted. TST90, wake MHR and nocturnal MHR remained as independent predictors in the fully adjusted multivariable models, with HR of 1.41 (95% CI 1.10 to 1.81), 1.30 (95% CI 1.12 to 1.50) and 1.27 (95% CI 1.10 to 1.46), respectively (table 2). With additional adjustment in the final model for hip circumference, family history of CVD, educational level, beta blocker and statin use, the risk from TST90 was only marginally attenuated (HR: 1.40, 95% CI 1.09 to 1.80). TST90 did not show any significant interactions with gender and age (p=0.104 and 0.537, respectively), as were MHRs.
Figure 2.
TST90 and its HR with incident MACEs. The model was derived from the fully adjusted Cox regression including a restricted cubic spline term with three knots, restricted to untreated subgroup. The blue shaded curve represents 95% CI. MACEs, major adverse cardiovascular events; TST90, sleep time with oxygen saturation below 90%.
To further investigate the impact of PSG parameters on non-fatal MACEs, we performed additional analyses in the entire dataset and CPAP untreated subset (online supplemental table E1). TST90 was a robust significant predictor for non-fatal MACEs (HR: 1.43, 95% CI 1.11 to 1.85). Similar to wake MHR, nocturnal MHR during the PSG study was also predictive of MACEs after full adjustment (HR: 1.25, 95% CI 1.08 to 1.45). The effects of TST90 and MHR in competing risk models had similar HRs to those from the Cox regressions (online supplemental table E2); TST90 and wake MHR were significant predictors for incident MACEs when restricted to non-obese subjects (BMI <25 kg/m2) (online supplemental table E3).
Association between TST90 and AHI
AHI showed a higher density between 0 and 25/hour with a wide range of TST90 values. On the other hand, TST90 values close to zero were often seen in combination with a wide range of AHI values (online supplemental figure E1). Further Pearson correlation analysis showed only a mild association between TST90 and AHI (r=0.65, 95% CI 0.62 to 0.68). In multivariable Cox model, entering both TST90 and AHI simultaneously, TST90 was still a robust predictor of MACEs with a HR of 1.89 (95% CI 1.39 to 2.57), while the HR of AHI was not significant.
Role of CPAP in the incidence of MACEs
Among 1544 patients with AHI≥5/hour, 293 patients had regular long-term CPAP compliance (CPAP-treated group), of which 252 were evaluated for primary prevention, and 41 for secondary prevention. A total of 265 out of 1108 patients with moderate–severe OSA (AHI≥15/hour) were classified as CPAP-treated group. Subjects with regular long-term CPAP compliance were more likely to have higher baseline AHI and more prior diabetes, other baseline characteristics were balanced between CPAP treated and untreated groups (online supplemental table E4).
Compared with the no-OSA (AHI <5/hr) group, a lower hazard risk was observed in patients with moderate–severe OSA who were adherent to CPAP treatment. However, the difference was attenuated after adjustments, with HR of 0.93 (95% CI 0.56 to 1.56) in treated group versus HR of 1.02 (95% CI 0.67 to 1.55) in untreated group (Log-rank test, p=0.20) (table 3). The model was refitted with exclusion of those who defaulted sleep clinic follow-up (n=134) and those with irregular CPAP use (n=164), and results did not change significantly.
Table 3.
Cox regression analysis: the effect of CPAP on fatal and non-fatal MACEs (n=1860)
| No OSA | Mild OSA | Untreated moderate–severe OSA |
Treated moderate–severe OSA |
|
| Incident MACEs | ||||
| No. of subjects | 316 | 436 | 843 | 265 |
| Incident MACEs, n (%) | 31 (9.8%) | 63 (14.4%) | 146 (17.3%) | 38 (14.3%) |
| Unadjusted HR | Ref | 1.48 (0.97 to 2.28) | 1.90 (1.29 to 2.80) | 1.52 (0.95 to 2.45) |
| Partially adjusted HR* | Ref | 1.10 (0.71 to 1.69) | 1.06 (0.70 to 1.60) | 0.88 (0.53 to 1.45) |
| Fully adjusted HR† | Ref | 1.10 (0.71 to 1.70) | 1.02 (0.67 to 1.55) | 0.93 (0.56 to 1.56) |
| Incident non-fatal MACEs | ||||
| No. of subjects | 316 | 436 | 843 | 265 |
| Incident MACEs, n (%) | 29 (9.2%) | 60 (13.8%) | 138 (16.4%) | 38 (14.3%) |
| Unadjusted HR | Ref | 1.51 (0.97 to 2.35) | 1.92 (1.28 to 2.86) | 1.63 (1.01 to 2.64) |
| Partially adjusted HR* | Ref | 1.13 (0.72 to 1.76) | 1.09 (0.71 to 1.67) | 0.96 (0.58 to 1.60) |
| Fully adjusted HR† | Ref | 1.13 (0.72 to 1.77) | 1.05 (0.68 to 1.63) | 1.03 (0.61 to 1.75) |
*Partially adjusted for age, gender, body mass index.
†Fully adjusted for age, gender, body mass index, waist circumference, body weight change, Epworth sleepiness scale, total sleep time, cigarette smoking, alcohol use, physical activity, prior hypertension, prior cardiovascular disease, prior hyperlipidaemia and prior diabetes.
CPAP, continuous positive airway pressure; HR, hazard ratio; MACEs, major adverse cardiovascular events; OSA, obstructive sleep apnoea.
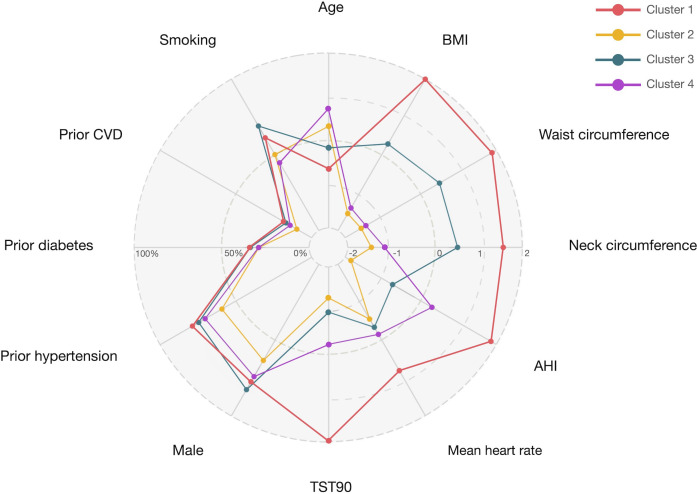
Secondary analysis by a two-stage LASSO-LCA algorithm was conducted for cluster profile identification, which followed by Cox regression to interrogate the response of CPAP treatment on different clusters for the outcome of MACEs. The first stage LASSO using all patients’ characteristics identified nine robust indicators (online supplemental figure E2). Three additional cardiovascular risk factors (AHI, BMI and waist circumference) were considered based on published literature, thus finalising on 12 indicators for further clustering analysis. LCA revealed that models with four distinct clusters had the best fit (BIC=116 995.2). These subgroups were distinguished notably by age, gender, obesity, OSA severity and comorbidities. The radar chart graphically showed that cluster 1 (n=333, 30% of the moderate–severe OSA cohort) was characterised by significantly younger patients with obesity, with the highest severity of OSA and more comorbidities (table 4 and figure 3). In this cluster, compared with the untreated group, the CPAP-treated group was significantly associated with reduced risk of incident MACEs (HR: 0.49, 95% CI 0.25 to 0.95) in the univariable Cox model. The effect was tenable after adjustments, with the HR of 0.45 (95% CI 0.23 to 0.90) and the statistical power of 87% (table 5). The finding of differential response to CPAP also had been validated in view of fully adjusted model with interactions between CPAP and by OSA subphenotype (p=0.01). The other three clusters with relatively lower risks did not demonstrate any significant benefit from CPAP treatment. To avoid immortal time bias, landmark analyses were conducted by excluding patients who developed incident MACEs or censored within 6 months and 12 months, similar results were observed (online supplemental table E5).
Table 4.
Characteristics of patients in moderate–severe OSA by clusters (n=1108)
| Variables | Cluster 1 (n=333, 30%) |
Cluster 2 (n=265, 24%) |
Cluster 3 (n=271, 24%) |
Cluster 4 (n=239, 22%) |
P for difference* |
| Demographics | |||||
| Male, n (%) | 258 (77.5%) | 168 (63.4%) | 224 (82.7%) | 177 (74.1%) | <0.001 |
| Age, year | 49.6 (12.2) | 55.6 (11.5) | 52.5 (12.0) | 58.0 (11.2) | <0.001 |
| Symptom and measurements | |||||
| BMI, kg/m2 | 34.7 (5.4) | 25.1 (2.8) | 30.0 (2.3) | 25.5 (2.3) | <0.001 |
| Neck circumference, cm | 42.8 (4.2) | 36.9 (2.7) | 40.8 (2.3) | 37.5 (2.3) | <0.001 |
| Waist circumference, cm | 108.7 (12.0) | 87.4 (6.8) | 100.1 (5.4) | 88.2 (5.7) | <0.001 |
| Polysomnogram | |||||
| AHI, /hour | 68.2 (53.7–82.3) | 23.1 (18.8–28.4) | 35.3 (25.4–46.5) | 49.2 (37.8–61.0) | <0.001 |
| TST90, min | 111.3 (50.3–200.6) | 3.8 (1.4–8.0) | 15.6 (6.8–27.5) | 40.4 (21.7–68.0) | <0.001 |
| Mean heart rate, /min | 69.0 (63.1–75.0) | 62.5 (57.5–68.3) | 63.6 (57.5–70.5) | 64.0 (58.9–70.7) | <0.001 |
| History | |||||
| Prior hypertension, n (%) | 262 (78.7%) | 157 (59.2%) | 202 (74.5%) | 168 (70.3%) | <0.001 |
| Prior diabetes, n (%) | 113 (33.9%) | 76 (28.7%) | 91 (33.6%) | 69 (28.9%) | 0.362 |
| Prior CVDs*, n (%) | 62 (18.6%) | 26 (9.8%) | 46 (17.0%) | 34 (14.2%) | 0.020 |
| Cigarette smoking, n (%) | <0.001 | ||||
| No | 229 (73.4%) | 200 (74.3%) | 160 (74.1%) | 241 (59.4%) | |
| Former | 41 (13.1%) | 26 (9.7%) | 23 (10.6%) | 77 (19.0%) | |
| Current | 42 (17.1%) | 43 (14.3%) | 33 (17.0%) | 88 (18.0%) | |
| Regular CPAP use, n (%) | 100 (30.0%) | 43 (16.2%) | 54 (19.9%) | 68 (28.5%) | 0.083 |
| Incident MACEs, n (%) | 57 (17.1%) | 38 (14.3%) | 46 (17.0%) | 43 (18.0%) | <0.001 |
| Follow-up time, months | 93.9 (66.4–117.1) | 100.4 (73.3–123.4) | 97.7 (69.3–118.0) | 94.0 (67.6–119.2) | 0.705 |
Data are given as mean (SD), median (IQR) or n (%).
Characteristics among clusters were compared by analysis of variance or Kruskal-Wallis test for continuous variables and χ2 test for categorical variables.
*Bonferroni corrected for multiple comparisons (p ≤ (0.05/12)=p ≤ 0.004).
AHI, apnoea–hypopnoea index; BMI, body mass index; CPAP, continuous positive airway pressure; CVDs, cardiovascular diseases; MACEs, major adverse cardiovascular events; OSA, obstructive sleep apnoea; TST90, sleep time with oxygen saturation below 90%.
Figure 3.
Radar chart comparing 12 characteristics of patients with moderate–severe OSA in each of the four clusters. Since these 12 indicators have different ranges, z-standardised scores were plotted for quantitative variables and proportions for categorical variables to simplify the interpretation of the chart. AHI, apnoea–hypopnoea index; BMI, body mass index; CVDs, cardiovascular diseases; OSA, obstructive sleep apnoea; TST90, sleep time with oxygen saturation below 90%.
Table 5.
Cox regression analysis: the effect of CPAP on MACEs in patients with moderate–severe OSA by clusters (n=1108)
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | |
| No. of subjects | 333 | 265 | 271 | 239 |
| Incident MACEs, n (%) | 57 (17.1%) | 38 (14.3%) | 46 (17.0%) | 43 (18.0%) |
| Crude HR | 0.49 (0.25 to 0.95) | 0.85 (0.33 to 2.19) | 0.94 (0.45 to 1.95) | 1.18 (0.62 to 2.27) |
| Adjusted HR* | 0.44 (0.22 to 0.85) | 0.85 (0.33 to 2.19) | 0.85 (0.41 to 1.77) | 1.57 (0.79 to 3.13) |
| Adjusted HR† | 0.45 (0.23 to 0.90) | 0.79 (0.30 to 2.12) | 0.68 (0.31 to 1.45) | 1.40 (0.67 to 2.91) |
*Adjusted for age, gender and body mass index.
†Adjusted for age, gender, body mass index, waist circumference, neck circumference, AHI, TST90 and mean heart rate.
AHI, apnoea–hypopnoea index; MACEs, major adverse cardiovascular events; OSA, obstructive sleep apnoea; TST90, sleep time with oxygen saturation below 90%.
Finally, statistical models in other multiple-imputed datasets or complete-case analysis did not change the results significantly. The Cox regression models all satisfied the proportional hazards assumption.
Discussion
In a clinic-based cohort of middle-aged OSA subjects, AHI was not significantly associated with incident MACEs after adjustment for potential confounders. In contrast, TST90 and MHR were independent and significant predictors of the occurrence of fatal and non-fatal MACEs. Regular CPAP treatment was not associated with a lower rate of MACEs, but cluster analysis based on baseline clinical and PSG features identified a high-risk subgroup who could benefit from regular CPAP treatment. The prognostication ability of different sleep indices as well as potential differential patient benefit from CPAP therapy on long-term cardiovascular burden should be elaborated in future OSA studies and clinical practice.
The severity of oxygen desaturation and event duration may vary widely among patients with similar AHI and influence outcomes. In our study, for a TST90 from 0 to 1 min, the AHI ranged from 0 to 76/hour. This broad range and weak correlation represent the diversity of OSA characterisation. TST90 measures the depth and the duration of event-related hypoxia that may not be captured by AHI or ODI. One study suggested that nocturnal desaturation, but not the frequency of apnoea, corresponded with the haemodynamic stress in patients with heart failure and had a bearing on cardiovascular outcomes.17 Similar evidence came from a large clinic cohort in Canada, where the findings endorsed a relationship between the TST90 (but not AHI) and composite cardiovascular events.18 The ‘hypoxic burden’ of OSA with the innovative measurement of sleep-event-related area under the oxygen desaturation curve predicted stroke and cardiovascular morbidity more consistently than AHI and ODI.19–21 On the other hand, a low prognostic value of both AHI and ODI for cardiovascular events was reported in a post-hoc analysis of the SAVE study.22
AHI is subject to a number of measurement challenges. The choice of oxygen desaturation cut-offs (set at ≥4% or≥3%) to identify hypopnoea could influence the association analyses with clinical outcomes. The Sleep Heart Health Study (SHHS) found that only ≥4%, but not ≥3% desaturation-defined hypopnoea index were associated with hypertension and CVD.23 Another Spanish cohort found that AHI by either ≥4% or≥3% hypopnoea criterion was appropriate to identify cardiovascular mortality risk in women and elderly, but the AHI definition with ≥3% oxyhaemoglobin desaturation or event-related arousal failed to predict increased risk in the elderly.24
The incidence rate of MACEs was 1.95 per 100 person years in our cohort, which is close to the rates from other clinic-based studies with similar cardiovascular outcomes.2 18 The source of patients, especially the selection of the reference group, might account for the negative associations with AHI in clinic studies. Compared with community cohorts,4 6 25–28 the control group in clinic cohorts usually have a greater prevalence of concomitant chronic medical conditions and this could attenuate the estimation of exposure-disease association. Furthermore, health literacy and intention to seek medical care of clinic cohort controls tend to be higher than that of community ones, which would render a narrower gap of hospitalisation between severe OSA group and no-OSA controls.
Multiple studies have demonstrated that resting heart rate, one of the simplest measurements, is associated with CVD in the general population.29 30 Daytime heart rate is susceptible to fluctuations of emotion and activity, whereas nocturnal heart rate has been found to be more related to MACEs,31 32 which might reflect sympathetic activation and a loss of cardiac reserve in patients with OSA. Sleep-related heart rate variability predicted incident stroke in a French cohort.21 An increased night-time heart rate through increased sympathetic tone may injure the vascular endothelium and predispose to cardiac arrhythmias.33 34 In this study, nocturnal hypoxia (TST90) and MHR derived from PSG were the only two significant predictors of long-term risk of MACEs. Our finding has been observed previously in the SHHS, in which the subgroup of patients with OSA with higher sleep apnoea-specific heart rate response had higher cardiovascular morbidity and mortality, and the hypoxic burden was also particularly high in this subgroup.35
The effect of CPAP therapy may provide a viable surrogate for the adverse impact of OSA on cardiovascular endpoint, but results of studies have been limited and inconsistent. The Spanish Zaragoza cohort in men with ten years’ follow-up suggested a dramatic modifying effect from CPAP treatment of OSA on CVDs.2 In contrast, large RCTs of CPAP intervention did not demonstrate a significant cardiovascular risk prevention.7–10 This discrepancy has stimulated scrutiny of the current understanding of OSA and its health sequelae. It is progressively recognised that OSA is a heterogenous disease and the OSA population even more so with highly variable symptom presentations or comorbidities36–38; hence, the adverse health impacts and their prevention by treating OSA may not be uniform across the entire patient spectrum despite the same OSA severity categorised by AHI.
This clinical cohort was prescribed CPAP therapy per consensus recommendations along with international guidelines, thus heavily biased towards those with AHI≥15/hour. As a group, no beneficial effect of regular CPAP treatment on incident MACEs could be demonstrated. However, based on 24 clinical and PSG parameters, further cluster analysis helped to identify one subtyped group of patients with moderate–severe OSA who were clinically indicated for CPAP, and who had a significantly lower incident risk of MACEs over a median of 8 years’ CPAP use. Among four clusters of subjects, this group was comparatively younger, more obese, had higher AHI and greater oxygen desaturation (TST90), and had more background comorbidities such as CVD and hypertension. Our findings may reflect that severe OSA with hypoxaemia would be of greater detriment to those with prior cardiovascular comorbidities who would thus also derive more benefit from treatment.39 40 OSA is a disease of insidious onset, and there is no information regarding prior incubation period. It is plausible that the adverse impact in older subjects is not as well reversed through CPAP use compared with younger counterparts. Much research is needed to delineate the mechanisms of potential adverse cardiovascular impact in the heterogenous OSA population.
Phenotypic characterisation of patients with OSA may identify treatment-responsive clusters, allowing refinement of the therapeutic approach. Our findings of the protective CPAP effect on CVD outcomes in only a phenotypic subgroup of patients resonate with that of the few studies along the same theme. In the SHHS cohort, the excessively sleepy subtype was significantly associated with increased risk of coronary heart disease or heart failure compared with other subtypes, and compared with individuals without OSA (AHI <5/hour), the sleepy subtype had a significantly increased risk for both prevalent and incident cardiovascular events.41 The SAVE study did not find a beneficial effect of CPAP therapy in secondary prevention of MACEs over a 3.7 years follow-up,8 while the post-hoc analyses of the dataset classified four phenotypes based on patients’ clinical characteristics, and the subgroups with comorbid diabetes had better response to CPAP compared with those without.42 In the US veteran cohort study, seven clusters were identified on baseline polysomnographic data, with the ‘periodic limb movement in sleep’, ‘hypopnoea and hypoxia’, and ‘combined severe’ subgroups showing significantly increased risk of adverse cardiovascular outcomes,43 and the risk of adverse events for regular versus non-regular CPAP use was significantly lower among the first two subgroups.
A single centre for sleep apnoea related data has the benefit of meticulous protocolised collection of demographic, anthropometric and clinical history at first presentation to the sleep clinic and which were all available for the study analysis. We have body weight measurements at both baseline and endpoint (or very close to endpoint) as the surrogate measure of on lifestyle behaviour changes during the follow-up period. In addition, our sample consisted of a considerable number of non-obese OSA subjects, with 34% of subjects (n=624) having BMI <25 kg/m2, the threshold for defining obesity in this study population. Although adjustments for obesity (BMI) and central obesity (waist circumference) removed much of the OSA signal, nocturnal hypoxia still emerged as an independent predictor for incident MACEs. Further exploration of TST90 by the continuous spectrum showed a non-linear dose–response curve with incident MACEs. This finding could help clinicians for better clinical decision-making according to risk-targeted management.
This study has the limitation of using historical data. The retrospective nature is compensated by abundance of data captured by the comprehensive electronic healthcare record system. In particular, MACEs have the unique advantage of being significant and clearly defined healthcare events and thus very well captured and accurately coded in this territory-wide healthcare administration system. Through the ePR, we have also been able to collect data about beta blocker and statin use, fasting glucose, and lipid profile that may affect the incidence of MACEs. Treatment was non-randomised as expected of a clinical cohort follow-up study, we addressed this issue by fully adjusting our models and further cluster analysis. CPAP usage data were collected with protocolised assessment at clinic follow-up, and given the long course of years of nightly treatment, CPAP adherence was defined by simple dichotomization of an average of greater or less than 4 hours/per night while one should not take this as a rigid cut-off number. Although we have 133 untreated patients with OSA with TST90 >100 min, the limited amount of cases at the tail end resulted in a wide CI of the non-linear dose–response curve.
In conclusion, in a clinic cohort presenting for suspected OSA, AHI in the baseline PSG was not significantly associated with incident MACEs over the median of 8 years follow-up. On the other hand, nocturnal hypoxaemia and mean heart rate documented on the sleep study were better measures regarding the subsequent risk of CVD consequences in this OSA cohort. CPAP treatment of OSA was not associated with risk reduction of incident major cardiovascular events in all those who were treated, but only in a subgroup of moderate–severe OSA characterised by younger age, higher obesity, higher AHI and greater oxygen desaturation, and more baseline CVD risks. The findings further support that awareness of the heterogeneity of OSA would allow for better identification of those at risk of specific adverse health outcomes and those who are most likely to benefit from CPAP treatment.44
Acknowledgments
The authors are grateful to the contributions from the following staff of the University of Hong Kong: Peony Chong in project coordination and data acquisition, Michelle Cheong and Kelvin Lau in manual scoring of polysomnogram and overall data entry, Yan Liu and Christopher Hui in data acquisition, and Terence Tam, Herbert Kwok and sleep nurses in patient care. The authors thank Xiao Dong Zhuang of the Department of Cardiology, the First Affiliated Hospital of Sun Yat-Sen University for his valuable suggestions.
Footnotes
Contributors: Study design: MSMI, PHX. Data acquisition: PHX, MMSL, DCLL and MSMI. Data analysis and interpretation: PHX, DYTF and MSMI. Manuscript preparation: PHX, DYTF, MMSL, DCLL and MSMI. All authors approved the final version to be submitted. The corresponding author (MSMI) is responsible for the overall content as guarantor. She has full access to all the data in the study and has final responsibility for the decision to submission.
Funding: This study was supported by the Ho Ting Sek Donation Fund for Sleep Research.
Disclaimer: The Ho Ting Sek Donation Fund had no role in the study design and analysis, as well as no input into the results and manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request, to be made to the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was obtained from the Institutional Review Board (IRB) of the University of Hong Kong/Hospital Authority of Hong Kong West Cluster (UW16-340). This was a retrospective study based on clinical data and electronic healthcare records.
References
- 1. Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 2017;69:841–58. 10.1016/j.jacc.2016.11.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marin JM, Carrizo SJ, Vicente E, et al. Long-Term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005;365:1046–53. 10.1016/S0140-6736(05)71141-7 [DOI] [PubMed] [Google Scholar]
- 3. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41. 10.1056/NEJMoa043104 [DOI] [PubMed] [Google Scholar]
- 4. Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation 2010;122:352–60. 10.1161/CIRCULATIONAHA.109.901801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Campos-Rodriguez F, Martinez-Garcia MA, Reyes-Nuñez N, et al. Role of sleep apnea and continuous positive airway pressure therapy in the incidence of stroke or coronary heart disease in women. Am J Respir Crit Care Med 2014;189:1544–50. 10.1164/rccm.201311-2012OC [DOI] [PubMed] [Google Scholar]
- 6. Hla KM, Young T, Hagen EW, et al. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin sleep cohort study. Sleep 2015;38:677–84. 10.5665/sleep.4654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barbé F, Durán-Cantolla J, Sánchez-de-la-Torre M, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA 2012;307:2161–8. 10.1001/jama.2012.4366 [DOI] [PubMed] [Google Scholar]
- 8. McEvoy RD, Antic NA, Heeley E, et al. Cpap for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 2016;375:919–31. 10.1056/NEJMoa1606599 [DOI] [PubMed] [Google Scholar]
- 9. Peker Y, Glantz H, Eulenburg C, et al. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with Nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med 2016;194:613–20. 10.1164/rccm.201601-0088OC [DOI] [PubMed] [Google Scholar]
- 10. Sánchez-de-la-Torre M, Sánchez-de-la-Torre A, Bertran S, et al. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med 2020;8:359–67. 10.1016/S2213-2600(19)30271-1 [DOI] [PubMed] [Google Scholar]
- 11. Punjabi NM. Counterpoint: is the apnea-hypopnea index the best way to quantify the severity of sleep-disordered breathing? no. Chest 2016;149:16–19. 10.1378/chest.14-2261 [DOI] [PubMed] [Google Scholar]
- 12. Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 2006;29:375–80. 10.1093/sleep/29.3.375 [DOI] [PubMed] [Google Scholar]
- 13. PH X, CKM H, MMS L. Incident type 2 diabetes in obstructive sleep apnea and effect of continuous positive airway pressure treatment: a retrospective clinic cohort study. Chest 2019;156:743–53. 10.1016/j.chest.2019.04.130 [DOI] [PubMed] [Google Scholar]
- 14. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. deliberations of the sleep apnea definitions Task force of the American Academy of sleep medicine. J Clin Sleep Med 2012;8:597–619. 10.5664/jcsm.2172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. John Wiley & Sons Inc, 2009. [Google Scholar]
- 16. Tibshirani R. The LASSO method for variable selection in the COX model. Stat Med 1997;16:385–95. [DOI] [PubMed] [Google Scholar]
- 17. Gottlieb JD, Schwartz AR, Marshall J, et al. Hypoxia, not the frequency of sleep apnea, induces acute hemodynamic stress in patients with chronic heart failure. J Am Coll Cardiol 2009;54:1706–12. 10.1016/j.jacc.2009.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kendzerska T, Gershon AS, Hawker G, et al. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med 2014;11:e1001599. 10.1371/journal.pmed.1001599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Azarbarzin A, Sands SA, Stone KL, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the osteoporotic fractures in men study and the sleep heart health study. Eur Heart J 2019;40:1149–57. 10.1093/eurheartj/ehy624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Azarbarzin A, Sands SA, Taranto-Montemurro L, et al. The sleep apnea-specific hypoxic burden predicts incident heart failure. Chest 2020;158:739–50. 10.1016/j.chest.2020.03.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blanchard M, Gervès-Pinquié C, Feuilloy M, et al. Hypoxic burden and heart rate variability predict stroke incidence in sleep apnoea. Eur Respir J 2021;57:2004022. 10.1183/13993003.04022-2020 [DOI] [PubMed] [Google Scholar]
- 22. Linz D, Loffler KA, Sanders P, et al. Low prognostic value of novel nocturnal metrics in patients with OSA and high cardiovascular event risk: post hoc analyses of the save study. Chest 2020;158:2621–31. 10.1016/j.chest.2020.06.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Punjabi NM, Newman AB, Young TB, et al. Sleep-Disordered breathing and cardiovascular disease: an outcome-based definition of hypopneas. Am J Respir Crit Care Med 2008;177:1150–5. 10.1164/rccm.200712-1884OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Campos-Rodriguez F, Martínez-García MA, Reyes-Nuñez N, et al. Impact of different hypopnea definitions on obstructive sleep apnea severity and cardiovascular mortality risk in women and elderly individuals. Sleep Med 2016;27-28:54–8. 10.1016/j.sleep.2016.05.020 [DOI] [PubMed] [Google Scholar]
- 25. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 26. Marshall NS, Wong KKH, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton health study. Sleep 2008;31:1079–85. [PMC free article] [PubMed] [Google Scholar]
- 27. Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-Disordered breathing and mortality: a prospective cohort study. PLoS Med 2009;6:e1000132. 10.1371/journal.pmed.1000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med 2010;182:269–77. 10.1164/rccm.200911-1746OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cook S, Togni M, Schaub MC, et al. High heart rate: a cardiovascular risk factor? Eur Heart J 2006;27:2387–93. 10.1093/eurheartj/ehl259 [DOI] [PubMed] [Google Scholar]
- 30. Zhang D, Shen X, Qi X. Resting heart rate and all-cause and cardiovascular mortality in the general population: a meta-analysis. CMAJ 2016;188:E53–63. 10.1503/cmaj.150535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Palatini P, Reboldi G, Beilin LJ, et al. Predictive value of night-time heart rate for cardiovascular events in hypertension. The ABP-International study. Int J Cardiol 2013;168:1490–5. 10.1016/j.ijcard.2012.12.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Johansen CD, Olsen RH, Pedersen LR, et al. Resting, night-time, and 24 H heart rate as markers of cardiovascular risk in middle-aged and elderly men and women with no apparent heart disease. Eur Heart J 2013;34:1732–9. 10.1093/eurheartj/ehs449 [DOI] [PubMed] [Google Scholar]
- 33. Thorin E, Thorin-Trescases N. Vascular endothelial ageing, heartbeat after heartbeat. Cardiovasc Res 2009;84:24–32. 10.1093/cvr/cvp236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Verrier RL, Josephson ME. Impact of sleep on arrhythmogenesis. Circ Arrhythm Electrophysiol 2009;2:450–9. 10.1161/CIRCEP.109.867028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Azarbarzin A, Sands SA, Younes M, et al. The sleep Apnea-Specific Pulse-Rate response predicts cardiovascular morbidity and mortality. Am J Respir Crit Care Med 2021;203:1546–55. 10.1164/rccm.202010-3900OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bailly S, Destors M, Grillet Y, et al. Obstructive sleep apnea: a cluster analysis at time of diagnosis. PLoS One 2016;11:e0157318. 10.1371/journal.pone.0157318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Keenan BT, Kim J, Singh B, et al. Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep 2018;41:zsx214. 10.1093/sleep/zsx214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pien GW, Ye L, Keenan BT, et al. Changing faces of obstructive sleep apnea: treatment effects by cluster designation in the Icelandic sleep apnea cohort. Sleep 2018;41:zsx201. 10.1093/sleep/zsx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lee C-H, Sethi R, Li R, et al. Obstructive sleep apnea and cardiovascular events after percutaneous coronary intervention. Circulation 2016;133:2008–17. 10.1161/CIRCULATIONAHA.115.019392 [DOI] [PubMed] [Google Scholar]
- 40. Peker Y, Thunström E, Glantz H, et al. Effect of obstructive sleep apnea and CPAP treatment on cardiovascular outcomes in acute coronary syndrome in the RICCADSA trial. J Clin Med 2020;9:4051. 10.3390/jcm9124051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mazzotti DR, Keenan BT, Lim DC, et al. Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med 2019;200:493–506. 10.1164/rccm.201808-1509OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Quan W, Zheng D, Douglas McEvoy R, et al. High risk characteristics for recurrent cardiovascular events among patients with obstructive sleep apnoea in the save study. EClinicalMedicine 2018;2-3:59–65. 10.1016/j.eclinm.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zinchuk AV, Jeon S, Koo BB, et al. Polysomnographic phenotypes and their cardiovascular implications in obstructive sleep apnoea. Thorax 2018;73:472–80. 10.1136/thoraxjnl-2017-210431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ryan S, Cummins EP, Farre R, et al. Understanding the pathophysiological mechanisms of cardiometabolic complications in obstructive sleep apnoea: towards personalised treatment approaches. Eur Respir J 2020;56:1902295. 10.1183/13993003.02295-2019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2021-217714supp001.pdf (347.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request, to be made to the corresponding author.