Abstract
Objectives
To examine the association of shift work with and without night work with breast cancer among women in the public sector.
Methods
Using the Finnish Public Sector cohort study (N=33 359, mean age of 40.6 years at baseline), we investigated the associations of shift work and potential confounders with incident breast cancer. Exposure to permanent day work or shift work was defined from first two consecutive surveys from 2000, 2004, 2008 or 2012 and past information on exposure in a subcohort (n=20 786). Incident cases of breast cancer (n=1129) were retrieved from the National Cancer Register and the cohort members were followed to the end of 2016. HR and 95% CI from Cox proportional hazard regression models were calculated.
Results
Shift work with and without night shifts was not overall associated with breast cancer. When stratified according to age, both shift work without nights (HR 2.01, 95% CI 1.12 to 3.60) and shift work with nights (OR 2.05, 95% CI 1.04 to 4.01) were associated with an increased risk after a period of 10 years or more follow-up among women aged 50 years or older, when adjusted for age, socioeconomic status, children, smoking, alcohol and body mass index. In a subgroup with past information on exposure to shift work, the increased risk by longer exposure to shift work was not significant.
Conclusions
This study provides support for an increased risk of breast cancer among elderly shift workers. However, insufficient information on exposure and intensity of night work may attenuate the risk estimates.
Keywords: Shift Work Schedule, Occupational Health, Epidemiology, Medical Oncology
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Night shift work is probably carcinogenic to humans.
Epidemiological evidence on the association of night shift work and breast cancer is limited.
Although earlier case–control studies show positive associations between night shift work and breast cancer, majority of the cohort studies have shown weak or no associations.
WHAT THIS STUDY ADDS
In a relatively large cohort study among public sector workers in Finland, both shift work without nights and shift work with nights were associated with an increased risk of breast cancer among women aged 50 years or older after a period of 10 years or more follow-up.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Organisations need to pay attention to the possible risk of breast cancer among elderly employees with current or past exposure to shift work with or without night shifts.
Introduction
In Europe, one in five workers are doing shift work, that is, any work schedule beyond the traditional day work from 08:00 to 16:00. Further, 9.7% of women were also exposed to night shift work in 2018.1 Night work, defined as work performed during a period of not less than seven consecutive hours, including the interval from midnight to 05:00,2 is common in health and social care sector, which nowadays is one of the largest occupational sectors and where more than 30% of the employees also work during nights.
In 2019, a working group convened by the International Agency for Research on Cancer (IARC) concluded that night shift work is probably (IARC classification Group 2A) carcinogenic to humans.2 The evidence of cancer in experimental animals was sufficient and supported by strong mechanistic animal evidence. Epidemiological studies showed credible positive associations between night shift work and breast cancer, but bias could not be reasonably ruled out. Therefore, epidemiological evidence was limited.2 In general, case–control studies showed positive association between night shift work and breast cancer, but this was not the case for cohort studies, where majority have shown weak or no associations.2 3 Exceptions were two cohorts from Sweden,4 5 as well as the two Nurses Health Studies (NHS and NHS2), which showed positive associations between rotating night shift work and risk of breast cancer after 20 years (NHS2) or 30 years (NHS) of exposure to rotating night shift work.6–8
While the NHS6 7 are examples of cohort studies with large population sizes, long follow-up, regularly updated information on exposure (NHS2) and cancer diagnoses during follow-up, many other cohort studies have had methodological limitations, in combination with poor exposure information on night shift work, for example, based on baseline time only, collected retrospectively, or even after cessation of work.2 Some cohort studies have included night shift workers in the reference groups and have short follow-up, while others have not been able to control sufficiently for potential confounders or had insufficient sample size.2 9 Finally, there was a tendency for a higher risk of breast cancer in premenopausal women than in postmenopausal women.7
While exposure assessment has improved greatly in most recent case–control studies (eg, ref 10), with detailed characteristics of complete historical working time, including night shift work, although collected retrospectively, few cohort studies have been able to characterise the risk according to shift work with or without night work. An exception is the relatively small study of Knutsson et al,5 which found a doubling of the relative risk of breast cancer among shift workers with night shifts, but also a slightly increased risk among shift workers without nights assessed at baseline. A prospective cohort study of public sector female workers with exposure from payroll registers showed a negative association of night shift work with breast cancer.11 However, the follow-up time of this study was only 5 years and no baseline information on earlier exposure was available. The results of recent case–control studies show stronger associations between night work and breast cancer than observed in prospective cohort studies. Thus, there is a potential that retrospective studies are affected by recall bias, that is, that breast cancer cases and controls could report differently about previous exposure and thereby bias the results. However, the positive findings seen in case–control studies are more likely explained by obtaining complete work history, which many cohort studies have failed to capture.2
Considering the methodological limitations, and especially the inability of several earlier cohort studies to differentiate between exposure to shift work with and without night shifts, we investigated the association between shift work with and without night shifts and the incident risk of breast cancer using a large prospective cohort study with 16 years of follow-up. In order to improve the quality of exposure assessment at baseline, the assessment of shift work status was based on consistent reporting of shift work status in two consecutive surveys with 4 years between. Second, we analysed the association of shift work with risk of breast cancer in a subsample with additional information on earlier exposure to shift work.
Methods
Study design and participants
The data for this study include those of the female members of the Finnish Public Sector (FPS) study. FPS is an ongoing dynamic survey cohort initiated in 1997 including several waves of questionnaire-based surveys between the years 1997 up to the present. FPS includes two subcohorts: first, a cohort of local government employees in 10 towns (referred to as ‘the 10-town subcohort’), being a mixture of healthcare workers and employees from other municipal occupational sectors; and second, a cohort conducted within 21 large hospitals, the Finnish Hospital Personnel Study (referred to later as ‘the Hospital subcohort’). The most common occupations in the FPS cohort are those related to healthcare, social services and education. In healthcare and social services, dominated by women and shift work, the most common job titles are nurse, practical nurse, department secretary, hospital cleaner and laboratory nurse.
The survey cohort (figure 1) comprises all female participants who had responded to any of the FPS questionnaires in 2000, 2004, 2008 and 2012 (response rates 66%–68%). In order to improve exposure assessment for the long follow-up, the analysis of the whole sample was limited to participants with stable shift work status in two consecutive FPS surveys. Follow-up with respect to breast cancer started after the second survey. Those shifting between any of the three categories of shift work status (day work, shift work without nights and shift work with nights) during the two surveys were excluded. The participants entered the follow-up at different time points, depending on when they had joined the first of the two consecutive surveys. A total of 66 262 women responded to at least one of the four surveys. After excluding participants with a non-defined shift work system (irregular shift systems or missing shift work status data, n=884), women diagnosed with breast cancer before entry to the cohort (n=676), duplicates due to technical reasons from the cancer registry and employees with a change or missing information on their shift work status in the second survey (30 723), the final study population comprised 33 359 women (50.3% of the original sample). We conducted additional analyses of breast cancer according to earlier shift work exposure of the hospital subcohort, as this was the only cohort having information on exposure prior to baseline.
Figure 1.
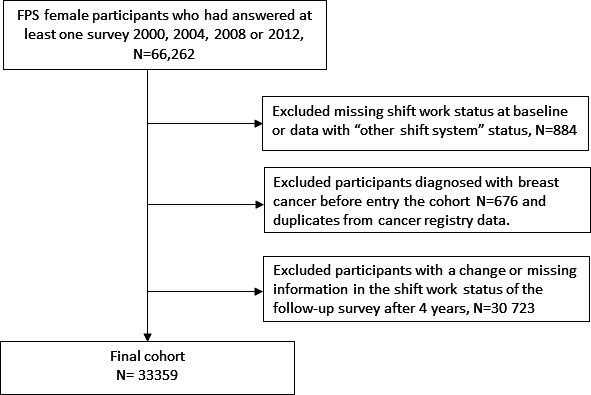
Flow chart of selection of study participants for analysis with exposure assessment based on two consecutive surveys. FPS, Finnish Public Sector study.
Shift work status
The participants were first classified as (1) day workers, (2) shift workers without night shifts, (3) shift workers with night shifts, (4) permanent night workers or (5) workers in ‘other work schedules’, based on a direct question or the presence of different work shifts. Those with ‘other work schedules’ or missing shift work status (n=884) were excluded. Shift work with night shifts and permanent night work were combined due to the low number (2%) of permanent night workers and based on the recent definition of the IARC working group for ‘night shift work’.2 This survey question has been used earlier12–14 and validated against payroll-based registry data of working hours.15 Based on the payroll data, most work schedules in shift work with or without nights were irregular, with variations in the number and in the start and end times of the shifts between weeks. In general, the intensity of night work in the rotating shift work was low, with only 10% of all employees having over 50 night shifts in a subsample of the study.16
The surveys of the hospital subcohort included an additional question of earlier shift work exposure (‘how many years in total have you worked shift work?’).
Breast cancer data
Cases of breast cancer were retrieved from the Finnish Cancer Registry using the unique personal identification applied to all residents of Finland (www.cancerregistry.fi). Cohort participants were followed up from baseline (the year after the second consecutive FPS survey in 2004, 2008 or 2012, depending on the entry year of the employee) to the end of 2016. In the additional hospital cohort analysis with information on past exposure to shift work, follow-up started from the first FPS survey (2000, 2004, 2008 or 2012) to the end of 2016. The maximum follow-up time was thus 12.5 years for the entire study population and 16.5 years in the hospital subcohort analysis, which also had working time prior to the baseline used for the ‘entire cohort’. In the Finnish Cancer Registry, the cases have been registered according to the International Classification of Diseases for Oncology, Third Revision (ICD-O-3) from 2007 onwards as well as the date of diagnosis. Cancers from 1953 to 2006 were coded by ICD-7 and have been converted to ICD-O-3. The ICD-O codes for breast cancer used in this study were C50.0–50.9.
Assessment of covariates
Covariates measured at baseline included age (years); socioeconomic status (SES; four categories: upper white collar (International Standard Classification of Occupations or ISCO=1–2), lower white collar (ISCO=3–4), skilled blue collar (ISCO=5) and other blue collar (ISCO=6–9)); having children aged 0–6 years old (three categories: no, yes and missing); having children aged 7–18 years old (three categories: no, yes and missing); current smoking status (three categories: no, yes and missing); body mass index (BMI; kg/m2), with missing values replaced by average; and alcohol consumption (continuous measure: pure alcohol g/week), with missing values replaced by average. All baseline data were obtained from the survey responses, except for SES and age which were derived from employers’ registers. Finally, we used the age of 50 years old as a proxy for menopausal status.
Statistical analysis
Associations between exposure to shift work and incident breast cancer in the survey and the payroll cohort data during follow-up were examined using Cox proportional hazard regression models. The time-dependent interactions between exposure to night shift work for all unadjusted models and the follow-up period were statistically non-significant, confirming that the proportional hazards assumption was justified. For the adjusted models of the survey data, there was some evidence of violation of the proportional hazards assumption. In order to justify the use of proportional hazards model, we stratified the analyses according to the follow-up period (<10 years and 10 years or longer). Similar stratification for shorter and longer follow-ups has also been used, for example, in the NHS.6–8
The follow-up period started from the date of the second survey and continued until the date of the first primary diagnosis of breast cancer, death or end of follow-up (31 December 2016), whichever occurred first. For all shift work exposure variables, we computed the crude and adjusted HRs and 95% CIs, controlling for age, SES, children aged 0–6 years, children aged 7–18 years, smoking, alcohol consumption and BMI. In order to account for the non-Gaussian distributions of the variables measuring alcohol consumption and BMI, these variables were entered along with their squared terms. First, we calculated the crude and adjusted associations between the dichotomised exposure variables and breast cancer in the survey cohort. Second, we did the same analyses after stratification according to age (<50 years and ≥50 years) and two follow-up periods (<10 years and ≥10 years). Statistical analyses were conducted with SAS V.9.4.
Results
Individual characteristics and exposure to night shift work
The characteristics of the cohort (N=33 359) at baseline according to shift work status are described in table 1. Upper white-collar workers represented the largest socioeconomic subgroup among day workers (36.8%), while lower white-collar workers were the largest group among shift workers with night shifts (59.6%). The mean age of shift workers with night shifts (n=5422) was lower at baseline (mean age 40.9 years, SD 9.1) compared with that of day workers (n=23 486; mean age 44.0 years, SD 8.3) and of shift workers without night shifts (n=4451; mean age 44.9 years, SD 9.0). The prevalence of women aged 50+ was lower (20.4 %) among shift workers with night shifts compared with day workers (29.8%) and shift workers without night shifts (27.7%).
Table 1.
Description of the cohorts (women) at baseline
| Variables | Shift work status | |||||||||||||||
| Day work | Shift work without nights | Shift work with nights | All | |||||||||||||
| n | % | Mean | SD | n | % | Mean | SD | n | % | Mean | SD | n | % | Mean | SD | |
| Age | ||||||||||||||||
| <50 years | 16 478 | 70.2 | 39.9 | 6.4 | 2772 | 62.3 | 39.6 | 7.0 | 4315 | 79.6 | 37.8 | 7.4 | 23 565 | 70.6 | 39.5 | 6.7 |
| 50+ years | 7008 | 29.8 | 53.6 | 2.7 | 1679 | 27.7 | 53.7 | 2.7 | 1107 | 20.4 | 53.1 | 2.3 | 9794 | 29.4 | 53.5 | 2.6 |
| All | 23 486 | 100.0 | 44.0 | 8.3 | 4451 | 100.0 | 44.9 | 9.0 | 5422 | 100.0 | 40.9 | 9.1 | 33 359 | 100.0 | 43.6 | 8.6 |
| Socioeconomic status | ||||||||||||||||
| Upper white collar | 36.8 | 10.7 | 1.8 | 28.9 | ||||||||||||
| Lower white collar | 34.0 | 28.1 | 59.6 | 37.3 | ||||||||||||
| Skilled blue collar | 18.3 | 32.8 | 36.7 | 23.3 | ||||||||||||
| Other blue collar | 9.1 | 28.5 | 1.9 | 10.5 | ||||||||||||
| Children <6 years old | ||||||||||||||||
| No | 48.7 | 48.5 | 43.7 | 47.8 | ||||||||||||
| Yes | 21.9 | 18.8 | 22.5 | 21.5 | ||||||||||||
| Missing | 29.5 | 32.8 | 33.8 | 30.6 | ||||||||||||
| Children 7–8 years old | ||||||||||||||||
| No | 33.6 | 35.6 | 35.8 | 34.5 | ||||||||||||
| Yes | 35.8 | 28.5 | 28.1 | 33.6 | ||||||||||||
| Missing | 30.6 | 22.9 | 36.1 | 31.9 | ||||||||||||
| Smoking | ||||||||||||||||
| No | 83.6 | 75.9 | 79.3 | 81.9 | ||||||||||||
| Yes | 14.1 | 21.1 | 17.7 | 15.6 | ||||||||||||
| Missing | 2.3 | 3.0 | 3.0 | 2.5 | ||||||||||||
| Body mass index (kg/m2) | 24.8 | 4.2 | 25.2 | 4.1 | 24.9 | 4.1 | 24.9 | 4.1 | ||||||||
| Alcohol consumption (g/week) | 52.5 | 81.4 | 45.3 | 79.8 | 43.1 | 73.9 | 50.0 | 80.1 | ||||||||
Association of shift work with breast cancer
We identified 1129 incident cases of first primary breast cancer after excluding the cases prior to baseline. The association between shift work status and incidence of breast cancer is shown in table 2.
Table 2.
Association of shift work with female breast cancer during follow-up: survey cohort (N=33 359). Shift work status based on first two surveys with 4 years between.
| Unadjusted | Adjusted* | |||||||||||||
| Follow-up <10 years | Follow-up ≥10 years | Follow-up <10 years | Follow-up ≥10 years | Follow-up <10 years | Follow-up ≥10 years | |||||||||
| Cases | Pyrs | Cases | Pyrs | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||
| Cases | All | Cases | All | |||||||||||
| All | ||||||||||||||
| Day work | 673 | 3356 | 60 939 | 123 | 1366 | 164 593 | Ref | Ref | Ref | Ref | ||||
| Shift work without nights | 138 | 672 | 9442 | 33 | 371 | 35 819 | 1.15 | 0.96 to 1.39 | 1.22 | 0.83 to 1.79 | 1.14 | 0.94 to 1.39 | 1.35 | 0.90 to 2.02 |
| Shift work with nights | 128 | 585 | 12 318 | 34 | 378 | 43 786 | 0.90 | 0.74 to 1.09 | 0.99 | 0.67 to 1.45 | 1.19 | 0.97 to 1.46 | 1.22 | 0.80 to 1.85 |
| <50 years | ||||||||||||||
| Day work | 362 | 1798 | 45 540 | 83 | 926 | 110 373 | Ref | Ref | Ref | Ref | ||||
| Shift work without nights | 58 | 301 | 6314 | 16 | 181 | 21 745 | 1.01 | 0.77 to 1.34 | 0.97 | 0.57 to 1.65 | 1.11 | 0.83 to 1.49 | 0.99 | 0.57 to 1.70 |
| Shift work with nights | 81 | 372 | 10 469 | 19 | 209 | 33 800 | 0.96 | 0.75 to 1.22 | 0.72 | 0.44 to 1.19 | 1.26 | 0.97 to 1.64 | 0.91 | 0.53 to 1.56 |
| 50+ years | ||||||||||||||
| Day work | 311 | 1558 | 15 398 | 40 | 440 | 54 219 | Ref | Ref | Ref | Ref | ||||
| Shift work without nights | 80 | 371 | 3128 | 17 | 191 | 14 075 | 1.14 | 0.89 to 1.45 | 1.62 | 0.92 to 2.86 | 1.18 | 0.90 to 1.53 | 2.01 | 1.12 to 3.60 |
| Shift work with nights | 47 | 213 | 1849 | 15 | 170 | 9986 | 1.11 | 0.81 to 1.51 | 1.91 | 1.04 to 3.47 | 1.17 | 0.84 to 1.63 | 2.05 | 1.04 to 4.01 |
HR and 95% CI from Cox regression models.
*Adjusted for age, SES (1–4), children 0–6 years (no/yes/missing), children 7–18 years (no/yes/missing), smoking (yes/no/missing), alc alc*alc and bmi bmi*bmi.
Pyrs, person-years; Ref, reference; SES, socioeconomic status.
For the whole group, shift work with night shifts and shift work without night shifts at baseline (based on two consecutive surveys) were associated with a modest non-significantly increased risk of breast cancer, when adjusted and compared with day work. Risk estimates were highest after the longest follow-up and in the fully adjusted models (shift work without night shifts: 33 cases, OR 1.35, 95% CI 0.90 to 2.02; shift work with night shifts: 34 cases, OR 1.22, 95% CI 0.80 to 1.85). However, among women 50 years or older, both shift work without night shifts (17 cases; HR 2.01, 95% CI 1.12 to 3.60) and shift work with night shifts (15 cases; OR 2.05, 95% CI 1.04 to 4.01) were associated with a significantly increased risk of breast cancer after a longer follow-up, when adjusted for age, SES, children, smoking, alcohol and BMI. Among the younger women, the risk of breast cancer was non-significantly increased for follow-up <10 years (shift work without night shifts: 58 cases, HR 1.11, 95% CI 0.83 to 1.49; shift work with night shifts: 81 cases, HR 1.26, 95% CI 0.97 to 1.64, in the fully adjusted models). In order to investigate the possible selection bias (healthy shift worker effect), we conducted a sensitivity analysis on the risk of breast cancer among shift workers with night shifts switching to day work (1645 women, mean age 38.0 years) compared with those who did not change (10 310 women, mean age 39.4 years) and found that there was a decreased risk among those exposed <10 years (5 cases; HR 0.23, 95% CI 0.09 to 0.58, in the fully adjusted model) but not among those exposed ≥10 years (3 cases; HR 0.94, 95% CI 0.28 to 3.17, in the fully adjusted model).
The association between shift work with night shifts and risk of breast cancer was analysed separately in the relatively small hospital subcohort because only this cohort had information on exposure prior to baseline (table 3). At baseline (the first questionnaire) and without information on past exposure, shift work including night shifts was not associated with an increased risk of breast cancer. When compared with always day workers, the crude analyses of shift workers with night shifts and followed up for <10 years showed a significantly increased risk among those who had previously worked shifts during a minimum of 15 years. After adjustment for different confounders, however, the risk estimates were attenuated and non-significantly elevated.
Table 3.
Association of night shift work with female breast cancer in the hospital subcohort according to earlier shift work exposure (based on the first survey, n=20 763)
| Unadjusted | Adjusted* | |||||||||||||
| Follow-up <10 years | Follow-up ≥10 years | Follow-up <10 years | Follow-up ≥10 years | Follow-up <10 years | Follow-up ≥10 years | |||||||||
| Cases | Pyrs | Cases | Pyrs | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||
| Cases | All | Cases | All | |||||||||||
| Day work always | 10 | 82 | 8759 | 25 | 354 | 10 653 | Ref | Ref | Ref | Ref | ||||
| Shift work with nights at baseline | 30 | 232 | 24 393 | 196 | 3112 | 91 297 | 1.22 | 0.60 to 2.50 | 0.72 | 0.48 to 1.10 | 1.36 | 0.63 to 2.97 | 0.68 | 0.41 to 1.12 |
| Day work always | 10 | 82 | 8759 | 25 | 354 | 10 653 | Ref | Ref | Ref | Ref | ||||
| Shift work with nights, 5–9 years | 4 | 30 | 10 587 | 8 | 124 | 19 056 | 0.37 | 0.12 to 1.19 | 0.18 | 0.08 to 0.40 | 0.69 | 0.20 to 2.41 | 0.37 | 0.16 to 0.88 |
| Shift work with nights, 10–14 years | 7 | 56 | 6066 | 19 | 294 | 15 228 | 1.12 | 0.43 to 2.95 | 0.44 | 0.24 to 0.79 | 1.48 | 0.52 to 4.15 | 0.60 | 0.31 to 1.17 |
| Shift work with nights, 15+ years | 19 | 146 | 7483 | 168 | 2685 | 55 167 | 2.45 | 1.14 to 5.28 | 0.90 | 0.59 to 1.37 | 1.65 | 0.72 to 3.81 | 0.72 | 0.44 to 1.19 |
| Trend: p=0.003† | Trend: p=0.006† | Trend: p=0.151† | P=0.926† | |||||||||||
HR and 95% CI from Cox regression models according to earlier shift work experience.
*Adjusted for age, SES (1–4), children 0–6 years (no/yes/missing), children 7–18 years (no/yes/missing), smoking (yes/no/missing), alc alc*alc and bmi bmi*bmi.
†P value indicates a trend test for linearity in relation to earlier exposure time.
Pyrs, person-years; Ref, reference; SES, socioeconomic status.
Discussion
In this relatively large cohort of public sector employees in Finland, shift work was not overall associated with an increased risk of breast cancer. However, after 10 years of follow-up, the risk increased twofold among women aged 50 years or older with prospective data on 4 years of exposure to shift work.
The observed risk estimates for workers 50 years and older are comparable with the risk estimates after exposure to night shift work for over 20 years, published earlier in the American Nurses’ Health Study 2 6 7 and with the Danish17 and Norwegian18 19 case–control studies of nurses.
Earlier epidemiological studies of night shift work have similarly reported higher risk of breast cancer among women over 50 years18 compared with younger women. Since our cohort included women of all ages, selection out due to left truncation, in which an ageing survivor population is included,20 cannot explain the age-related difference in the association of shift work and breast cancer. Since we do not have information on age of start of shift work in our cohort, an older age at start of shift work in our cohort compared with the pooled case–control studies could explain this observation. The observed trend of increased risk by longer exposure to night shift work is supported by earlier studies,2 but with some exceptions.7 21 Case–control studies with much more detailed exposure indicators than available in the cohort studies show generally more positive trends in the association of longer duration of night shifts and risk of breast cancer (eg, refs 19 22 23).
In the subgroup of women aged 50 years or older, we found the highest risk estimates after a longer follow-up. Long exposure time to shift work has also been found to be associated with an increased risk of breast cancer in earlier studies.4 6 7 18 The null finding of an overall association (before age stratification) between night shift work and breast cancer, when information on full earlier exposure was lacking, may basically be explained by selection in and out of night shift work, with the latter known as the healthy worker effect.24 However, the sensitivity analysis of the risk of breast cancer among those shifting from shift work to day work did not indicate any healthy shift worker effect due to the observed decreased risk among those shifting to day work, although based on very few cases.
We also found that the risk estimates of breast cancer were mostly the same among shift workers with and without night shifts, different from some previous studies which have found an increasing association between the intensity of night work and the risk of breast cancer.10 19 Many employees in this study have had a long earlier shift work experience before baseline, which is not fully captured by our data. In Finland, the occupational health services are obliged to provide free health assessment to all night shift workers. In case of any type of health-related problems linked to night work, a transfer to day work ‘whenever possible’ is recommended, as regulated by the European Union Working Time Directive. We have investigated the selection out of shift work in this population earlier.15 During a follow-up time of only 6 years, 8% of all shift workers with night shifts had switched to day work and 35% to shift work without night shifts. This indicates that especially the ‘shift work without nights’ group includes many earlier night workers. Since our own data also indicate that the risk of breast cancer tended to increase according to earlier exposure to shift work, when compared with never shift workers, it is likely that the increased risk of breast cancer among shift workers without current night work may be due to earlier exposure to night work.
Exposure to light at night during night work is the major reason for circadian disruption in shift work and an important candidate for a possible cancer pathway due to changes in melatonin patterns, including sex hormones, oxidative stress, and genetic and immunological functions.2 25 26 However, there is also evidence that shift work without night shifts—that is, alternating morning and evening work with variable and irregular shift start and end times—and insufficient resting time between shifts could be a stress factor, increasing sickness absence27 and reducing opportunities for sleep and recovery.12
The main strengths of this study include the large sample size and the long follow-up time from several survey waves with high response rates, as well as data on several potential confounders for breast cancer. The survey questionnaire enabled the separation of exposure to shift work with and without night shifts. The survey questions have been used earlier13 14 and validated against payroll-based registry data of working hours.15 The validation against registry data of working hours showed good validity for ‘shift work with nights shifts’ (sensitivity of 96% and specificity of 92% against the payroll data) and ‘permanent night work’ (sensitivity of 90% and specificity of 97%), which were combined into ‘shift work with night shifts’ in this study (due to the low number of permanent night workers, about 2%). In the hospital subcohort we had additional information on past exposure to shift work.
Limitations include the use of subjective data on exposure, lack of information on working time between the 4 years of questionnaire waves and lack of data on the intensity of night shifts. Furthermore, information on the age of the first child, family history of breast cancer, physical activity and use of sex hormones was missing. However, adjustment for these exposures in previous studies of night work and breast cancer had no or marginal influence on the risk estimates.
In summary, the results of the present study provide support for an increased risk of breast cancer among Finnish public sector employees 50 years or older. However, insufficient information on exposure and intensity of night work during the entire occupational history may attenuate the risk estimates and limit possibilities of firm conclusions.
Acknowledgments
We thank Professor Mika Kivimäki for useful comments on the study design and statistical analysis.
Footnotes
Twitter: @MikkoHaermae
Contributors: All authors have contributed to the design, writing and review of the manuscript. AO and AK analysed the data. MH acted as the guarantor of the study.
Funding: The study was supported by NordForsk, the Nordic Programme on Health and Welfare (grant 74809).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the Ethics Committee of the Hospital District of Helsinki and Uusimaa (HUS 1210/2016). Participants gave informed consent to participate in the study before taking part.
References
- 1. Eurostat . Employes persons working at nights as a percentage of the total employment, by ase, age and professional status (%) 2019. Available: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=lfsa_ewpnig&lang=en
- 2. IARC . Night shift work. IARC Monogr Identif Carcinog hazards hum, 2020: 1–371. [Google Scholar]
- 3. Sweeney MR, Sandler DP, Niehoff NM, et al. Shift work and working at night in relation to breast cancer incidence. Cancer Epidemiol Biomarkers Prev 2020;29:687–9. 10.1158/1055-9965.EPI-19-1314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Åkerstedt T, Knutsson A, Narusyte J, et al. Night work and breast cancer in women: a Swedish cohort study. BMJ Open 2015;5:e008127. 10.1136/bmjopen-2015-008127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Knutsson A, Alfredsson L, Karlsson B, et al. Breast cancer among shift workers: results of the wolf longitudinal cohort study. Scand J Work Environ Health 2013;39:170–7. 10.5271/sjweh.3323 [DOI] [PubMed] [Google Scholar]
- 6. Schernhammer ES, Kroenke CH, Laden F, et al. Night work and risk of breast cancer. Epidemiology 2006;17:108–11. 10.1097/01.ede.0000190539.03500.c1 [DOI] [PubMed] [Google Scholar]
- 7. Wegrzyn LR, Tamimi RM, Rosner BA, et al. Rotating night-shift work and the risk of breast cancer in the nurses’ health studies. Am J Epidemiol 2017;186:532–40. 10.1093/aje/kwx140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schernhammer ES, Laden F, Speizer FE, et al. Rotating night shifts and risk of breast cancer in women participating in the nurses' health study. J Natl Cancer Inst 2001;93:1563–8. 10.1093/jnci/93.20.1563 [DOI] [PubMed] [Google Scholar]
- 9. Hansen J. Night shift work and risk of breast cancer. Curr Environ Health Rep 2017;4:325–39. 10.1007/s40572-017-0155-y [DOI] [PubMed] [Google Scholar]
- 10. Cordina-Duverger E, Menegaux F, Popa A, et al. Night shift work and breast cancer: a pooled analysis of population-based case–control studies with complete work history. Eur J Epidemiol 2018;33:369–79. 10.1007/s10654-018-0368-x [DOI] [PubMed] [Google Scholar]
- 11. Vistisen HT, Garde AH, Frydenberg M, et al. Short-term effects of night shift work on breast cancer risk: a cohort study of payroll data. Scand J Work Environ Health 2017;43:59–67. 10.5271/sjweh.3603 [DOI] [PubMed] [Google Scholar]
- 12. Härmä M, Karhula K, Ropponen A, et al. Association of changes in work shifts and shift intensity with change in fatigue and disturbed sleep: a within-subject study. Scand J Work Environ Health 2018;44:394–402. 10.5271/sjweh.3730 [DOI] [PubMed] [Google Scholar]
- 13. Tucker P, Härmä M, Ojajärvi A, et al. Associations between shift work and use of prescribed medications for the treatment of hypertension, diabetes, and dyslipidemia: a prospective cohort study. Scand J Work Environ Health 2019;45:465–74. 10.5271/sjweh.3813 [DOI] [PubMed] [Google Scholar]
- 14. Tucker P, Härmä M, Ojajärvi A, et al. Association of rotating shift work schedules and the use of prescribed sleep medication: a prospective cohort study. J Sleep Res 2021;30:e13349. 10.1111/jsr.13349 [DOI] [PubMed] [Google Scholar]
- 15. Härmä M, Koskinen A, Ropponen A, et al. Validity of self-reported exposure to shift work. Occup Environ Med 2017;74:228–30. 10.1136/oemed-2016-103902 [DOI] [PubMed] [Google Scholar]
- 16. Garde AH, Harris A, Vedaa Øystein, Vedaa O, et al. Working hour characteristics and schedules among nurses in three nordic countries – a comparative study using payroll data. BMC Nurs 2019;18:12. 10.1186/s12912-019-0332-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hansen J, Stevens RG. Case–control study of shift-work and breast cancer risk in danish nurses: impact of shift systems. Eur J Cancer 2012;48:1722–9. 10.1016/j.ejca.2011.07.005 [DOI] [PubMed] [Google Scholar]
- 18. Lie J-AS, Roessink J, Kjærheim K. Breast cancer and night work among Norwegian nurses. Cancer Causes Control 2006;17:39–44. 10.1007/s10552-005-3639-2 [DOI] [PubMed] [Google Scholar]
- 19. Lie J-AS, Kjuus H, Zienolddiny S, et al. Night work and breast cancer risk among Norwegian nurses: assessment by different exposure metrics. Am J Epidemiol 2011;173:1272–9. 10.1093/aje/kwr014 [DOI] [PubMed] [Google Scholar]
- 20. Applebaum KM, Malloy EJ, Eisen EA. Left truncation, susceptibility, and bias in occupational cohort studies. Epidemiology 2011;22:599–606. 10.1097/EDE.0b013e31821d0879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Travis RC, Balkwill A, Fensom GK, et al. Night shift work and breast cancer incidence: three prospective studies and meta-analysis of published studies. J Natl Cancer Inst 2016;108. doi: 10.1093/jnci/djw169. [Epub ahead of print: 06 10 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hansen J, Lassen CF. Nested case–control study of night shift work and breast cancer risk among women in the danish military. Occup Environ Med 2012;69:551–6. 10.1136/oemed-2011-100240 [DOI] [PubMed] [Google Scholar]
- 23. Szkiela M, Kusideł E, Makowiec-Dąbrowska T, et al. How the intensity of night shift work affects breast cancer risk. Int J Environ Res Public Health 2021;18:4570. 10.3390/ijerph18094570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Baillargeon J. Characteristics of the healthy worker effect. Occup Med 2001;16:359–66. [PubMed] [Google Scholar]
- 25. Reszka E, Wieczorek E, Przybek M, et al. Circadian gene methylation in rotating-shift nurses: a cross-sectional study. Chronobiol Int 2018;35:111–21. 10.1080/07420528.2017.1388252 [DOI] [PubMed] [Google Scholar]
- 26. Gómez-Acebo I, Dierssen-Sotos T, Papantoniou K, et al. Association between exposure to rotating night shift versus day shift using levels of 6-sulfatoxymelatonin and cortisol and other sex hormones in women. Chronobiol Int 2015;32:128–35. 10.3109/07420528.2014.958494 [DOI] [PubMed] [Google Scholar]
- 27. Rosenström T, Härmä M, Kivimäki M, et al. Patterns of working hour characteristics and risk of sickness absence among shift-working hospital employees: a data-mining cohort study. Scand J Work Environ Health 2021;47:395–403. 10.5271/sjweh.3957 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


