Abstract
Background
Treatment options for pseudogynecomastia are limited, and the demand for noninvasive breast fat reduction is increasing.
Objective
We evaluated the efficacy and safety of a cold-induced lipolysis device for treating pseudogynecomastia.
Methods
In this 16-week prospective trial, a total of 15 male patients with pseudogynecomastia were treated twice with cryolipolysis. The primary endpoint was a change in the chest circumference from baseline at posttreatment week 8. Secondary endpoints were changes in body weight, fat thickness assessed using ultrasonography, independent evaluator- and patient-rated improvement, and Simon’s gynecomastia class (SGC) grading.
Results
The primary assessment, a reduction of 3.05 cm in the mean chest circumference at 8 weeks post-treatment compared to baseline, was statistically significant. The treatment effect was cumulative, with a steady decrease in chest circumference and fat thickness over the 16-week study period. The mean pain score immediately after the first session of treatment was 2.0±1.36, based on a scale of 0~10, with a score of 10 being the worst pain ever experienced. The pain decreased substantially after the end of the procedure.
Conclusion
Cryolipolysis was demonstrated to be an effective and safe option for reducing breast fat in pseudogynecomastia. Male with mild to moderate breast enlargement without skin excess can be ideal candidates.
Keywords: Adipose tissue, Diet therapy, Gynecomastia
INTRODUCTION
Gynecomastia is common abnormality of the male breasts that affects up to two-thirds of adult male1. It is defined as the benign proliferation of the mammary glandular tissue or fat tissue in male breasts, often caused by sex hormone imbalances, tumorous conditions, or numerous medications2. Excessive subareolar fat deposition without glandular proliferation is distinctively termed as pseudogynecomastia, lipomastia, or lipomatous gynecomastia3,4. Unlike true gynecomastia, pseudogynecomastia occurs mostly in obese male. Because pseudogynecomastia affects patients’ quality of life and is typically associated with psychological disturbance due to impaired body image, it is a subject of interest in the cosmetic fields5,6.
Currently, the standard treatment is surgical resection or liposuction, performed under general anesthesia7. However, many patients are wary of such invasive modalities owing to the potential for complications and extended downtime. Moreover, a recent long-term follow-up study has shown that recurrence rates after surgery are significantly higher in patients with pseudogynecomastia than in those with true gynecomastia8. Despite its effectiveness in removing large amounts of subcutaneous fat, liposuction is usually accompanied by a significant recovery time and increased risk of complications, including postprocedural pain, infection, scarring, and deep vein thrombosis9.
In light of the increasing demand for noninvasive lipoplasty, a cold-induced lipolysis technique has been newly introduced for the selective destruction of fat layers10. Both human and animal studies have demonstrated gradual thinning of the subcutaneous fat without epidermal or dermal injury11. Cryolipolysis has mainly been used for the abdomen, flank (love handle), and thighs12, and studies evaluating its efficacy and safety in male pseudogynecomastia are rare. Therefore, we conducted this clinical study to evaluate the efficacy and safety of cold-induced lipolysis for the noninvasive treatment of pseudogynecomastia.
MATERIALS AND METHODS
Study design
This single-center, single-arm, prospective clinical study was conducted at the Chung-Ang University Hospital, Seoul, Korea. The study protocol conformed to the guidelines of the Declaration of Helsinki and Korean Good Clinical Practice guidelines and was approved by the hospital’s institutional review board (IRB No. 1861-002-328).
Patients
Participants diagnosed with pseudogynecomastia, with Fitzpatrick skin types I~VI, aged 19~70 years, and with a body mass index (BMI) between 20 and 50 kg/m2 were eligible for inclusion in this study. Individuals diagnosed with true gynecomastia were excluded. Patients with a history of severe disease (cardiovascular, diabetic, thyroid, autoimmune, hepatic, or renal), coagulative disorders, endocrine disease that could induce breast enlargement (i.e., hypogonadism, breast cancer, testicular cancer, adrenal gland tumor, or pituitary gland disorder), cardiac pacemakers, and those in the high-risk group for cold-induced therapy (i.e., those with Raynaud disease, cryoglobulinemia, or cold urticaria and paroxysmal cold hemoglobulinemia) were excluded from the study. Fifteen patients agreed to participate in the study.
Measurement
Efficacy was evaluated by comparing baseline measurements with measurements taken at 4, 8, 12, and 16 weeks post-treatment. The observation period was set as the observation period in similar studies conducted previously13. The primary efficacy endpoint in our study was defined as a change in chest circumference, compared to baseline measurements, at post-treatment week 8. The primary efficacy was determined based on previous studies10. Secondary efficacy endpoint were changes in the following, compared to baseline measurements: body weight and chest circumference at 4, 12, and 16 weeks post-treatment, in addition to waist circumference, hip circumference, fat thickness assessed using ultrasonography, independent evaluator- and patient-rated improvement, and Simon’s gynecomastia class (SGC) grading. Safety factors included all adverse events recorded at all visits. Blood tests were conducted at baseline and week 16 post-treatment.
The chest circumference was measured 1 cm above the nipple line in a standing position and in a comfortably exhaled state. Waist circumference was measured near the umbilicus level at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest. Hip circumference was measured at the widest part of the hip. These measurements were recorded at all time points throughout the study period. To increase the reproducibility, the circumferences were measured using a standardized method with a tension-free tape in order to apply minimal pressure. To minimize any potential measuring bias, one researcher measured all circumferences during the entire study period.
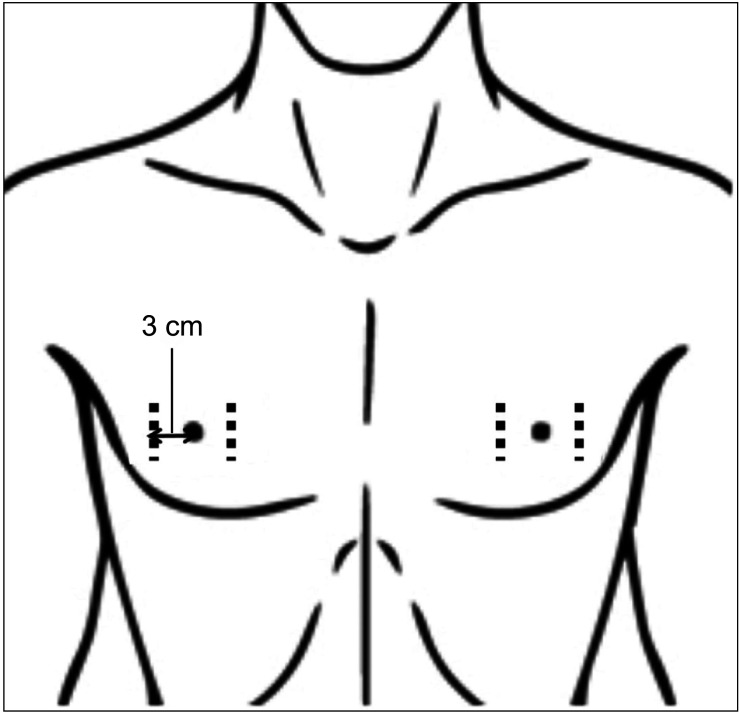
The fat thickness of the breast was measured at each visit using portable ultrasonography (ACUSON P300; Siemens, Berlin, Germany) at two points, 3 cm beside each nipple (Fig. 1). The thickness was measured twice to calculate the mean thickness. Body weights were recorded at each visit. Three independent evaluators graded the degree of improvement in pseudogynecomastia using a 5-point scale (0, no change [0%]; 1, minimal improvement [1%~25%]; 2, mild improvement [26%~50%]; 3, moderate improvement [51%~75%]; and 4, marked improvement [76%~100%]) based on photographs obtained at each time point. In addition, all patients reported their degree of improvement at each visit using a 5-point scale (0, no change; 1, minimal improvement; 2, mild improvement; 3, moderate improvement; and 4, marked improvement).
Fig. 1. Fat thickness measured area using ultrasonography.
The SGC system includes grade I (small visible breast enlargement, no skin redundancy), grade IIa (moderate breast enlargement without skin redundancy), grade IIb (moderate breast enlargement with skin redundancy), and grade III (marked breast enlargement with marked skin redundancy). At every visit, the SGC was graded by a dermatologist. Blood tests included a complete blood count (CBC), coagulation lab, serum lipid levels (triglyceride, total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol), liver function test (LFT), and renal function test (blood urea nitrogen [BUN] and creatinine). Pain was graded via a numeric rating scale.
Device description and treatment
The cold-induced lipolysis device used in the study, CLATUU™ (Classys Inc., Seoul, Korea), functions by cooling the targeted area at the selected heat extraction rate with vacuum suction to position the tissue inside the cooling panels (Fig. 2). The device consists of a control unit and two cup-shaped handpieces that directly contact the intended treatment area. The tissue is drawn into the handpiece by a moderate vacuum. This device differs from other current cryolipolysis devices, in that the entire contact area of its handpiece acts as cooling panel in order to deliver the thermal energy to a larger area spanning 360° of the targeted tissue.
Fig. 2. The cold-induced lipolysis device used in the study, CLATUU™ (Classys Inc., Seoul, Korea).

For the pretreatment preparation, the nipples were covered with bandages for protection. Topical or injected anesthesia was not necessary for any participants. Treatment areas were marked with grids. After applying a gel pad for cryolipolysis supplied by Classys Inc. onto the grid area, the handpieces were placed using moderate vacuum. The targeted cooling level was set at –7℃. The suction level was controlled between –30 kPa and –50 kPa depending on the patient’s discomfort. The cryo-energy was applied for 40 minutes per patient with subsequent manual massage for 5 minutes and warm compression for 10 minutes. Four weeks later, the treatment was repeated.
Statistics
Statistical analyses were performed using SPSS version 25.0, for Windows (IBM Corp., Armonk, NY, USA) and R version 3.53 (2019-03-11). Statistical comparisons before and after treatment were performed using a paired t-test or Wilcoxon’s signed-rank test. Values are presented as mean±standard deviation. Statistical significance was set at p<0.05.
RESULTS
Baseline demographics
A total of 15 male subjects with Fitzpatrick skin types III~IV were included in the trial. The mean age of participants was 33.0±7.98 years, mean height was 173.2±4.18 cm, mean weight was 90.57±10.53 kg, and mean BMI was 30.21±3.53 kg/m2. The BMIs of all participants were >20 kg/m2 and <50 kg/m2, which met the inclusion criteria. All participants were graded as greater than SGC grade 1, with small breast enlargement and no skin excess. Twelve subjects (80.0%) finished all procedures and follow-up study visits. Three cases of early termination occurred due to follow-up loss or consent withdrawal for personal reasons.
Efficacy
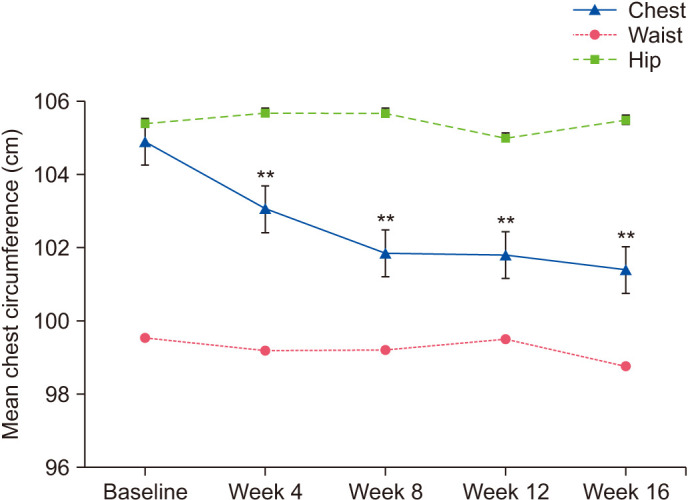
The mean reduction in the chest circumference of 3.05 cm between the baseline (104.89±6.34 cm) and week 8 (101.84±7.16 cm) measurements was statistically significant (p=0.0092), compared to the clinically meaningful threshold (1.5 cm). Moreover, a marked reduction in chest circumferences was observed at all follow-up visits over the 16-week study period (Fig. 3). The mean waist and hip circumferences measured at every visit showed no significant changes compared to the baseline measurements. In addition, the mean body weight remained stable throughout the study period.
Fig. 3. Changes in the mean chest circumference at all follow-up visit time points. **Indicates significant differences of p<0.01 compared to baseline.
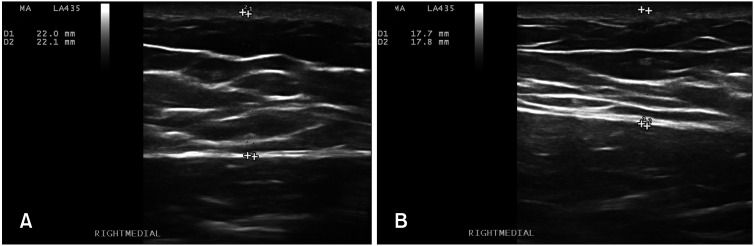
The mean subcutaneous fat thickness (mm) assessed using ultrasonography was 18.33, 16.95, 16.46, 16.18, and 15.95 mm, respectively, at baseline, 4 weeks, 8 weeks, 12 weeks, and 16 weeks (Table 1 and Fig. 4). The average thickness of the fat tissue continuously decreased to statistically significant levels of 1.38, 1.87, 2.15, and 2.38 mm after cryotherapy at 4, 8, 12, and 16 weeks, respectively (p<0.05).
Table 1. Summary of changes from baseline breast fat thickness (mm).
| Mean±SD | Median | Range | p-value* | ||
|---|---|---|---|---|---|
| ➀ Baseline | 18.33±3.48 | 17.98 | 12.53~24.70 | ||
| ② Week 4 | 16.95±3.26 | 17.08 | 10.35~21.54 | ||
| Difference (①–②) | 0.002 | ||||
| ③ Week 8 | 16.46±3.06 | 17.04 | 9.89~21.04 | ||
| Difference (①–③) | 0.002 | ||||
| ④ Week 12 | 16.18±2.77 | 16.16 | 10.36~20.56 | ||
| Difference (①–④) | 0.002 | ||||
| ⑤ Week 16 | 15.95±2.71 | 15.9 | 10.24~20.76 | ||
| Difference (①–⑤) | 0.003 | ||||
*Paired t-test or Wilcoxon signed rank test.
Fig. 4. Ultrasonography of a representative fat thickness assessment. Fat thickness at baseline (A) and at 16 weeks post-treatment (B) shows thinning of the fat layer.
At each visit, a dermatologist graded all patients using the SGC. Baseline SGC was distributed as 8.3% grade I, 33.3% grade IIa, 50.0% grade IIb, and 8.3% grade III. At week 4, the distribution changed to 16.7% grade I, 33.3% grade IIa, 50.0% grade IIb, and no grade III. At week 8, grade IIa increased to 58.3%, whereas grade IIb decreased to 25.0%. At week 16, grade I accounted for 18.2%, grade IIa 45.5%, and grade IIb 36.4%.
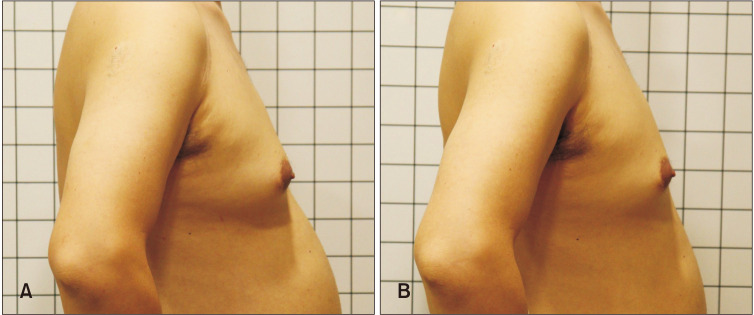
Global photographic assessment by three independent evaluators using the 5-point scale from 0 to 4 was recorded as 1.19±0.59, 1.39±0.53, 1.44±0.89, and 1.42±0.72 points of improvement at 4, 8, 12, and 16 weeks compared to baseline. Patients’ satisfaction assessed using the 5-point scale from 0 to 4 was reported as 2.33±1.07, 2.33±1.07, 2.33±1.23, and 2.82±1.08 points of improvement at 4, 8, 12, and 16 weeks compared to baseline. Fig. 5 shows the remarkable improvement in the overall contour and volume of the pseudogynecomastia, which became flatter than at baseline. Other covariates of age, baseline BMI, and body weight did not exert significant effects on the chest circumference reduction.
Fig. 5. Representative photographs of a subject. (A) Baseline and (B) post-treatment week 16.
Safety
Blood laboratory test data, including CBC, BUN/Cr, LFT, and serum lipid profile, remained stable and within normal limits throughout the study period. There were no notable clinical findings from the physical examinations. Bruising and erythema at the application sites were observed in 44.4% and 55.6% of patients, respectively, but all cases resolved within 2 weeks post-treatment. No serious or delayed adverse events were reported during the 16-week study period, and paradoxical adipose hypertrophy was not observed in this study.
The mean pain score immediately after the first treatment session was 2.0±1.36. The degree of pain decreased substantially after completion of the procedure. Furthermore, subjects reported reduced pain during the second session at week 4, with a mean score of 1.54±1.13. Although the participants had a choice to receive anesthesia, no local or injected anesthesia was used in the treatments.
DISCUSSION
Multiple options for gynecomastia, such as medication, reduction mammoplasty, and liposuction, can be considered based on the underlying cause, possible risk, costs, and expected downtime. While traditional therapeutic modalities of surgical excision or liposuction may yield dramatic effects, these methods inevitably possess inherent risks of complications. Meanwhile, cold-induced lipolysis is one of the most recent approaches to noninvasive fat reduction in the treatment areas of the abdomen14,15,16, flank14,17,18,19, and thighs20,21,22.
The cryolipolysis technique was derived from the observation of localized fatty inflammation after exposure to cold, i.e., cold-induced panniculitis, which has been described most frequently in infants. Histological analysis of the exposed area showed perivascular lymphohistiocytic infiltration, which was most intense at the dermo-subdermal junction with extension to the subcutaneous fat, starting within 24 hours after cold exposure. The change became more pronounced over 72 hours with aggregation of many more inflammatory cells in the subcutis layer and the consequent rupture and phagocytosis of adipose tissues. Within a few weeks, the progression of inflammation resolved spontaneously without residual epidermal or dermal damage23. These observations led to the conclusion that fat tissues are more susceptible and sensitive to cold injury than peripheral water-rich tissues24.
The exact mechanism governing the apoptosis and subsequent elimination of fat tissue is not yet fully understood. However, it is generally thought that caspase-3 activates the apoptotic pathway of adipose tissue10. Moreover, cryo-energy induces intracellular lipid crystallization, which leads to apoptosis of the adipocyte25. Kwon et al.26 reported that a cryolipolysis device may enhance lipid catabolism by activating endogenous lipid metabolites through the peroxisome proliferator-activated receptor pathway.
Compared to conventional mammoplasty or liposuction, cold-induced lipolysis has the overwhelming advantage of noninvasiveness. Considering that pseudogynecomastia recurs frequently after treatment8, repeated therapy is often necessary and previous surgery may impede reoperation due to fibrosis and scar formation. Moreover, no forms of anesthesia were needed in this study, and because there is no necessary downtime from work or social activity after treatment, patients can resume normal life immediately. The factors of noninvasiveness and comfort during cryolipolysis largely ease resistance to treatment in patients. The only discomfort reported by patients is a pinching pain in the treatment area caused by the suction tip, which can be controlled by decreasing the suction power. In our study, the maximum pain level of NRS after the first procedure was 4 points, and the maximum value of NRS after the second procedure was 3 points. In an article, the pain levels after operations for gynecomastia were reported as 4.13±0.78 and 6.70±1.06 scores. Therefore, pain from cryolipolysis is more tolerable than that from other invasive treatments such as liposuction27. Nonetheless, cryolipolysis is not associated with serious adverse events such as fat embolism, hematoma, necrosis, scarring, or abnormalities in the lipid profile.
Cold-induced fat reduction is also convenient for practitioners. After initially setting the appropriate cooling temperature, suctioning intensity, and procedure time, the practitioner can leave until the bell rings to signal the end of treatment. Intensive monitoring is not needed. Furthermore, this cryolipolysis system is particularly superior, in that its large handpiece with a 360° panel can cover the entirety of the breast tissue and eliminates the need for multiple procedures within a session.
In this study, noninvasive cold-induced fat reduction using a cryolipolysis device with a targeted tissue temperature of –7℃ and suction level between –30 kPa and –50 kPa significantly reduced the chest circumference compared to baseline, which was further confirmed by imaging studies using ultrasonography. The procedure improved the esthetic contour of the male breast and was well tolerated during the study period. In general, the participants reported satisfaction with the outcomes.
Unlike the abdomen or flank, the nipple and areola are highly sensitive areas that require protection. Being less abundant in fat, the breast tissue also requires a lower cooling intensity for a shorter duration than the abdomen or flank. Further studies with a larger population are needed to determine the optimal and safe treatment protocol. In addition, the use of cryolipolysis seems more appropriate for single breast enlargement in cases without excess skin. In cases with remarkable skin excess, combination treatment with high-intensity focused ultrasound may improve the clinical outcomes. For severe cases, the surgical approach should still be considered as first-line treatment.
The limitations of our study included a short follow-up period and small number of participants. Future studies will be necessary using a larger patient population and longer study period using more diverse efficacy evaluations to further assess the effect of cryolipolysis in pseudogynecomastia.
In conclusion, cryolipolysis is a safe, noninvasive modality for the treatment of pseudogynecomastia that selectively reduces breast fat tissue without severe side effects or extended downtime. Patients with mild to moderate breast enlargement without skin excess are the ideal candidates for cold-induced fat reduction.
ACKNOWLEDGMENT
The patients in this manuscript have given written informed consent to publication of their case details.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING SOURCE: None.
DATA SHARING STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Fagerlund A, Lewin R, Rufolo G, Elander A, Santanelli di Pompeo F, Selvaggi G. Gynecomastia: a systematic review. J Plast Surg Hand Surg. 2015;49:311–318. doi: 10.3109/2000656X.2015.1053398. [DOI] [PubMed] [Google Scholar]
- 2.Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clin Proc. 2009;84:1010–1015. doi: 10.1016/S0025-6196(11)60671-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bembo SA, Carlson HE. Gynecomastia: its features, and when and how to treat it. Cleve Clin J Med. 2004;71:511–517. doi: 10.3949/ccjm.71.6.511. [DOI] [PubMed] [Google Scholar]
- 4.Yazici M, Sahin M, Bolu E, Gok DE, Taslipinar A, Tapan S, et al. Evaluation of breast enlargement in young males and factors associated with gynecomastia and pseudogynecomastia. Ir J Med Sci. 2010;179:575–583. doi: 10.1007/s11845-009-0345-1. [DOI] [PubMed] [Google Scholar]
- 5.Ordaz DL, Thompson JK. Gynecomastia and psychological functioning: a review of the literature. Body Image. 2015;15:141–148. doi: 10.1016/j.bodyim.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Rew L, Young C, Harrison T, Caridi R. A systematic review of literature on psychosocial aspects of gynecomastia in adolescents and young men. J Adolesc. 2015;43:206–212. doi: 10.1016/j.adolescence.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Kim DH, Byun IH, Lee WJ, Rah DK, Kim JY, Lee DW. Surgical management of gynecomastia: subcutaneous mastectomy and liposuction. Aesthetic Plast Surg. 2016;40:877–884. doi: 10.1007/s00266-016-0705-y. [DOI] [PubMed] [Google Scholar]
- 8.Fricke A, Lehner GM, Stark GB, Penna V. Long-term follow-up of recurrence and patient satisfaction after surgical treatment of gynecomastia. Aesthetic Plast Surg. 2017;41:491–498. doi: 10.1007/s00266-017-0827-x. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy J, Verne S, Griffith R, Falto-Aizpurua L, Nouri K. Non-invasive subcutaneous fat reduction: a review. J Eur Acad Dermatol Venereol. 2015;29:1679–1688. doi: 10.1111/jdv.12994. [DOI] [PubMed] [Google Scholar]
- 10.Park JT, Kwon SH, Shin JW, Park KC, Na JI, Huh CH. The efficacy and safety of cold-induced lipolysis in the treatment of pseudogynecomastia. Lasers Surg Med. 2016;48:584–589. doi: 10.1002/lsm.22510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Avram MM, Harry RS. Cryolipolysis for subcutaneous fat layer reduction. Lasers Surg Med. 2009;41:703–708. doi: 10.1002/lsm.20864. Erratum in: Lasers Surg Med 2012;44:436. [DOI] [PubMed] [Google Scholar]
- 12.Putra IB, Jusuf NK, Dewi NK. Utilisation of cryolipolysis among Asians: a review on efficacy and safety. Open Access Maced J Med Sci. 2019;7:1548–1554. doi: 10.3889/oamjms.2019.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones IT, Vanaman Wilson MJ, Guiha I, Wu DC, Goldman MP. A split-body study evaluating the efficacy of a conformable surface cryolipolysis applicator for the treatment of male pseudogynecomastia. Lasers Surg Med. 2018 doi: 10.1002/lsm.22784. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Sasaki GH, Abelev N, Tevez-Ortiz A. Noninvasive selective cryolipolysis and reperfusion recovery for localized natural fat reduction and contouring. Aesthet Surg J. 2014;34:420–431. doi: 10.1177/1090820X13520320. [DOI] [PubMed] [Google Scholar]
- 15.Boey GE, Wasilenchuk JL. Enhanced clinical outcome with manual massage following cryolipolysis treatment: a 4-month study of safety and efficacy. Lasers Surg Med. 2014;46:20–26. doi: 10.1002/lsm.22209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shek SY, Chan NP, Chan HH. Non-invasive cryolipolysis for body contouring in Chinese--a first commercial experience. Lasers Surg Med. 2012;44:125–130. doi: 10.1002/lsm.21145. Erratum in: Lasers Surg Med 2012;44:435. [DOI] [PubMed] [Google Scholar]
- 17.Garibyan L, Sipprell WH, 3rd, Jalian HR, Sakamoto FH, Avram M, Anderson RR. Three-dimensional volumetric quantification of fat loss following cryolipolysis. Lasers Surg Med. 2014;46:75–80. doi: 10.1002/lsm.22207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernstein EF. Long-term efficacy follow-up on two cryolipolysis case studies: 6 and 9 years post-treatment. J Cosmet Dermatol. 2016;15:561–564. doi: 10.1111/jocd.12238. [DOI] [PubMed] [Google Scholar]
- 19.Few J, Gold M, Sadick N. Prospective internally controlled blind reviewed clinical evaluation of cryolipolysis combined with multipolar radiofrequency and varipulsetechnology for enhanced subject results in circumferential fat reduction and skin laxity of the flanks. J Drugs Dermatol. 2016;15:1354–1358. [PubMed] [Google Scholar]
- 20.Zelickson BD, Burns AJ, Kilmer SL. Cryolipolysis for safe and effective inner thigh fat reduction. Lasers Surg Med. 2015;47:120–127. doi: 10.1002/lsm.22320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wanitphakdeedecha R, Sathaworawong A, Manuskiatti W. The efficacy of cryolipolysis treatment on arms and inner thighs. Lasers Med Sci. 2015;30:2165–2169. doi: 10.1007/s10103-015-1781-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boey GE, Wasilenchuk JL. Fat reduction in the inner thigh using a prototype cryolipolysis applicator. Dermatol Surg. 2014;40:1004–1009. doi: 10.1097/01.DSS.0000452628.99209.4f. [DOI] [PubMed] [Google Scholar]
- 23.Rotman H. Cold panniculitis in children. Adiponecrosis E frigore of Haxthausen. Arch Dermatol. 1966;94:720–721. [PubMed] [Google Scholar]
- 24.Ingargiola MJ, Motakef S, Chung MT, Vasconez HC, Sasaki GH. Cryolipolysis for fat reduction and body contouring: safety and efficacy of current treatment paradigms. Plast Reconstr Surg. 2015;135:1581–1590. doi: 10.1097/PRS.0000000000001236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR. Selective cryolysis: a novel method of non-invasive fat removal. Lasers Surg Med. 2008;40:595–604. doi: 10.1002/lsm.20719. [DOI] [PubMed] [Google Scholar]
- 26.Kwon TR, Yoo KH, Oh CT, Shin DH, Choi EJ, Jung SJ, et al. Improved methods for selective cryolipolysis results in subcutaneous fat layer reduction in a porcine model. Skin Res Technol. 2015;21:192–200. doi: 10.1111/srt.12176. [DOI] [PubMed] [Google Scholar]
- 27.Wang Y, Wang J, Liu L, Liang W, Qin Y, Zheng Z, et al. Comparison of curative effects between mammotome-assisted minimally invasive resection (MAMIR) and traditional open surgery for gynecomastia in Chinese patients: a prospective clinical study. Breast J. 2019;25:1084–1089. doi: 10.1111/tbj.13424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.