Abstract
Mucormycosis, which is a life threatening condition, is one of the side effects experienced by post-COVID-19 patients. Early identification and timely treatment are essential to stop the dissemination of the disease, since invasive mucormycosis has a very high fatality rate and significant disease dispersion. Conventional diagnostic techniques, including clinical diagnosis, serology, histopathology and radiology, have limitations in diagnosing the disease at an early stage. This warrants the need for advanced diagnostic tools such as nucleic acid diagnostics, advanced serological tests (ELISpot), PCR (pan-Mucorale test) and multiplex PCR. These techniques have been introduced to identify this invasive fungal infection at an incipient stage, thereby helping clinicians to prevent adverse outcomes. The use of biosensors and micro-needle based diagnostic methodologies will pave the way for devising more point-of-care tests that can be employed for the detection of mucormycosis at an incipient stage. The present review discusses the current techniques available and their drawbacks, and the usefulness of advanced diagnostic tools. Furthermore, the possibility of using future diagnostic methods for the diagnosis of mucormycosis is highlighted.
Keywords: mucormycosis, diagnosis, mucorales infection, COVID-19, point-of-care diagnostics, biosensor
1. Introduction
The majority of immunocompromised individuals with uncontrolled diabetes, haematological malignancies, renal failure, chemotherapy, long-term steroid use, diabetes with post-COVID-19 infection or acquired immunodeficiency syndrome are susceptible to mucormycosis, a rare opportunistic fungal disease, which has lately become increasingly prevalent (1,2). In 1885, Paltauf (3) published the first description of mucormycosis. Since then it has been considered as the most lethal and quickly progressing form of fungal infection in humans, initiated by a fungus of the saprophytic variety such as Mucor and Rhizopus. The most common causes of fungus-related illness are rotting fruits and vegetables, although fungi spores can also spread disease when inhaled from dust or air conditioning units (4).
Rhizopus is the most frequent source of rhinocerebral mucormycosis and the genera Absidia, Mucor and Mucorale also contribute to the disease (5). Mucorale can penetrate the vascular system, preventing arterial blood flow, causing thrombosis and ischemia. Due to soft- and hard-tissue necrosis, the infection quickly spreads to adjacent tissues. Dentists and medical professionals can help with early identification and treatment of mucormycosis due to intraoral presentation being amongst the earliest clinical symptoms of cranial, rhino and ocular mucormycosis (6). The two most frequent causes of oral mucormycosis are direct wound infection and palatal mucormycosis, which are primarily disseminated by inhaling fungal spores through the nasal and paranasal sinuses (7). In the majority of cases, this progresses to a systemic fungal infection, often with a poor prognosis. Mucormycosis is difficult to identify due to its radiographic resemblance to aspergillosis, in addition to a paucity of screening methods (8). Therefore, it is essential in medicine to create diagnostic tests that are precise, quick, specific and sensitive. Despite a number of notable recent improvements, multiple fundamental diagnostic techniques employed in the initial detection of mucormycosis have remained unchanged. Serology, lateral flow devices, radiography and CT imaging, histology, microscopy and in vitro fungal culture are still employed extensively (9).
In situations where sophisticated diagnostic tools are unavailabile, several of these diagnostic procedures can be transformed into point-of-care testing. These essential processes are being supplemented by elevated biomolecule alternative technologies, such as DNA sequencing-based techniques and matrix-assisted laser desorption ionization time of flight mass spectrometry (10). Microscopy and histology are the foundational components of diagnosis. Molecular tests can also be recommended as a helpful addition to conventional diagnostic techniques for the detection and identification of mucormycosis.
2. Conventional diagnostic tools
Clinical diagnosis
Clinical diagnosis is frequently used in medical terminology, although it can be challenging for doctors to diagnose mucormycosis. The sensitivity and specificity of a clinical diagnosis are subpar. Tissue necrosis is the most suggestive clinical sign of mucormycosis. Despite this, after the disease has progressed to an advanced level, it helps to raise suspicion, start laboratory testing and reveal the clinical indicators of the condition (11). The primary manifestations of mucormycosis are dermal, respiratory and rhinocerebral mucormycosis of which the following are the clinical signs: i) Oral ulceration, which is accompanied by pain and swelling in the face; ii) black lesions on the bridge of the nose; iii) nasal discharge containing blood; iv) paranasal sinus infection, which can spread to the mouth; v) perforations in the palate; vi) paraesthesia; and vii) facial cellulitis (12).
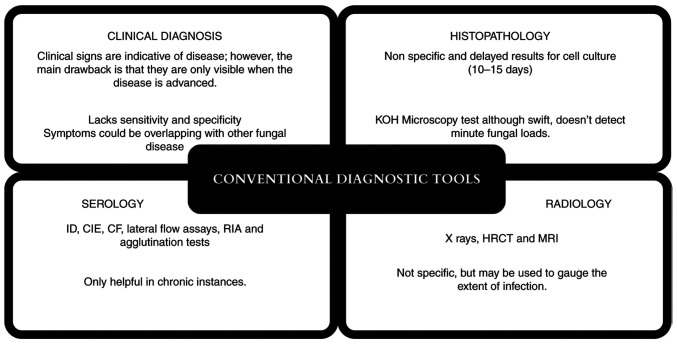
However, the symptoms listed above can overlap with those of other systemic disorders such as invasive aspergillosis, fusariosis, nocardiosis, Wegener granulomatosis and other malignancies, thus making clinical diagnosis a non-specific procedure (13). The clinical signs that are crucial in arriving at a clinical diagnosis for mucormycosis include some pertinent indicators that should not be overlooked, such as cranial nerve palsy, diplopia, sinus pain, periorbital swelling, orbital apex syndrome and palatal ulcers. These indicators are considered hallmarks for the diagnosis of mucormycosis (14). The disadvantages of conventional diagnostic tools are summarised in Fig. 1.
Figure 1.
Conventional diagnostic techniques and their disadvantages. ID, immunodiffusion; CIE, counter-immunoelectrophoresis; CF, complement fixation; RIA, radio-immunosorbent assays; HRCT, high-resolution compute tomography; MRI, magnetic resonance imaging.
Histopathology
The current gold-standard diagnostic methods for mucormycosis include microscopy, cell culture studies and histopathology (15). The foundation of microscopy is the identification and isolation of the fungus responsible for the disease. Multiple specimens may be examined for microscopy depending on the clinical symptoms and infection location; however, tissue biopsy is still the preferable method (7). Histopathological staining, including Grocott's methenamine silver (GMS) and periodic acid-Schiff (PAS) staining, offers enhanced outlines of the fungal wall. However, compared with GMS, PAS offers superior visualisation of surrounding tissues. Hence, it is more specific for mucormycosis (16).
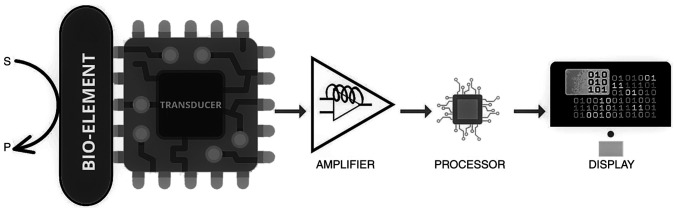
Typical histopathological images of mucormycosis comprise fungal septate or pauciseptate hyphae (Fig. 2). Histopathological diagnostics, in addition to direct microscopy, aid in the differentiation of a fungal infection from a culture contaminant. However, one significant disadvantage is that it can only provide morphological diagnosis and does not provide information regarding the specificity of the infecting organism (17).
Figure 2.
Histological image of mucormycosis (periodic acid-Schiff stain; magnification, x100). Pro-inflammatory cells are present co-existing with necrotic tissue (arrow A). Septate or pauciseptate fungal hyphae are visible all throughout the connective tissue specimen (arrow B). Sporangiophores containing spores are also seen, suggesting mucormycosis (arrow C).
Radiology
Preferred imaging techniques include contrast enhanced MRI and conventional CT. Imaging is necessary for a variety of reasons, including early diagnosis, initiation of antifungal therapy and monitoring of treatment response. Due to its improved contrast resolution in soft-tissue and marrow abnormalities, MRI is the gold standard while CT is often used in conjunction. The key symptom of black turbinate is a lack of contrast enhancement of invading mucosa due to small artery occlusion; an example of this is rhinocerebral mucormycosis. Radiography does offer signs of the type and quantity of infection, which can assist and guide biopsy sampling. However, radiography may not allow for the exact identification of the causative fungal agent or even a conclusive diagnosis of a fungal aetiology (18). The existence of major nodules (>1 cm) or perinodular halos throughout chest radiographs can show fungal infections invading blood vessels. A reverse halo accompanied by rapid tissue invasion or multiple nodules accompanied by lung effusion indicates infection by Mucorale mould. These characteristics can be indicative of fungal aetiology (19). The reverse halo sign on a CT scan is another symptom of mucormycosis and can be seen within the first week of illness in 94% of cases, as reported by Legouge et al (20) thus suggesting that CT imaging is a sensitive radiographic technique for the early diagnosis of mucormycosis.
Serology
Antibodies to fungi are identified using serology as a diagnostic tool. Serology has undergone extended use in the detection of fungal infections and is a commonly used technique. Lateral flow tests, radio-immunosorbent assays, enzyme immunoassays, immunodiffusion, counter-immunoelectrophoresis, complement fixation (CF), immunoassays using antibodies and agglutination techniques are some of the technologies used to identify antibodies in the blood or saliva (21). Future molecular technologies may be used to enhance serological techniques, but they will require direct tissue collection, standardisation, technological advancements and cost reduction (22). A monoclonal antibody (2DA6) was examined by Burnham-Marusich et al (23) using sandwich ELISA and was found to have high reactivity with purified fucomannan of the Mucor species. However, lateral flow immunoassay (LFIA) has been demonstrated to be more convenient in comparison to ELISA, as it can be used to test serum, urine and tissues more easily.
Some disadvantages of serological investigations include the technique being time intensive, such as CF, in addition to being technically challenging. Immunocompromised patients may have a lower antibody response that can also limit the utility of the test. The difficulty of serology to discriminate between current and previous infection also makes interpretation of serological tests unreliable (24).
3. Advanced diagnostic techniques
Advanced serological tests
ELISA, immunoblots and immuno-diffusion tests have all been used to diagnose mucormycosis in the past, with varying degrees of success. Serological approaches for detecting specific antigens, as well as antisera targeted at specific fungal antigens, have recently improved the specificity and sensitivity of these types of tests. For ~70 years, the precipitation in gel technique has been widely used. These tests are frequently employed with in-house antigens produced from fungal cultures to detect different forms of immunoglobulin over time. Employing an enzyme-linked immune-spot (ELISpot) assay, specific Mucorales T cells were recently observed in invasive mucormycosis (24). More research will need to be carried out to discover if these specific T cells can be employed as diagnostic surrogates (22). Burnham-Marusich et al (23) tested the monoclonocal 2DA6 antibody in the ELISA for new serological test targets and found it to be strongly reactive with distilled Mucor species.
Despite the high sensitivity of various serological tests, there are some disadvantages to be aware of such as test specificity, which has been demonstrated to be decreased by cross reactivity. Early identification of infection-induced antibody response may be challenging, since its manifestation in the peripheral blood can take 4-8 weeks. To avoid producing false-negative results, precise titre cut-off values are required. When dealing with a disease that is still in its early stages, this is especially true (25). Despite these shortcomings, serology diagnostic tests remain affordable, non-invasive and instantly offer information that can help doctors make more accurate and timely diagnoses (26).
Nucleic acid-based diagnostics
PCR methods have been improved and used in a variety of situations for the diagnosis of fungal infections. Examples of molecular assays include: i) Multiplex PCR; ii) nested PCR; iii) reverse transcription-quantitative (RT-qPCR); iv) PCR based on internal transcribed spacer regions and ribosomal DNA; v) PCR-ELISA; vi) conventional PCR; and vii) direct DNA sequencing (27). This variety of techniques offers notable benefits in terms of diagnostic specificity, as primers may be constructed to recognise specific illnesses; nevertheless, there are concerns in terms of responsiveness and reproducibility, notably in the fabrication of false-negative findings (28).
Traditional PCR is quick and can increase sensitivity; however, as there are no standardised PCR techniques that have been Food and Drug Agency approved for Mucorales detection, results might differ from lab to lab. This truth is generally acknowledged, even in advanced molecular labs where PCR methods are often used and attempts are made to standardise diverse testing components. Therefore, modified nested PCR techniques have been created for improved specificity and sensitivity (29). This is achieved by running samples through two sequential PCR reactions with two sets of primers, which enables the detection of fungal DNA with 100% specificity at a mass as low as 1 fg (24). However, this is highly dependent on sample type and concentration, and is particularly prone to contamination. MucorGenius (PathoNostics; ADT India) is a fast RT-qPCR test kit that detects fungal nucleic acid sequences to help in early identification despite low loads. It is a pan-Mucorale test, as it can detect five different species of fungus that can aid in the early and prompt detection of mucormycosis (30).
4. Future diagnostic tools
Biosensors
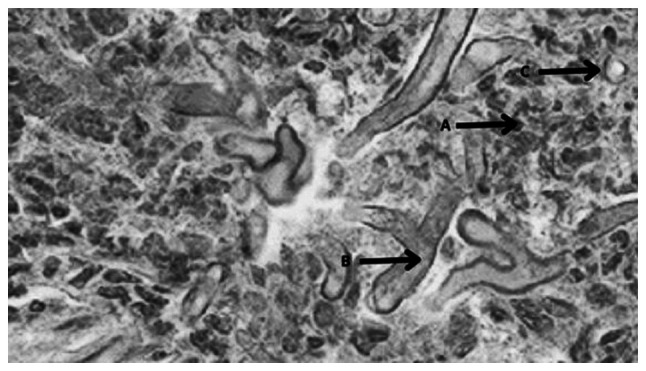
As stated by The International Union of Pure and Applied Chemistry (IUPAC), biosensors are integrated receptor-transducer systems that can offer selective quantitative or semi-quantitative analytical information utilising a biological recognition element. The three primary components of sensors and biosensors are: i) A transducer that generates an electrical signal; ii) an identification element that identifies a particular analyte or a group of analytes; and iii) a signal processor (Fig. 3). Analytical tools that can translate chemical, physical or biological data are known as sensors. In the medical field, there are 14 important types of biosensors. One such type is a wearable biosensor, which has been used to improve patient quality of life (9). Illness surveillance, aiding early detection, chronic disease therapy and, specifically, fungal identification are all essential applications of biosensors (31).
Figure 3.
Schematic illustration of a biosensor that tracks how a substrate becomes a product on the surface of a bio-element. S, substrate; P, product.
Electrochemical bio-sensors have been used to detect fungi such as Candida albicans and A. fumigatus. The relevant electrochemical biosensors for these fungi use membrane-bound impedance spectroscopy and chitosan-stabilised gold nano-particles (32). Optical biosensors to detect Candida species were developed in the study by Cai et al (33), which used Mannan on the cell surface to bind to the hydrogel Con-A. For fungal biomarker detection, optical biosensor platforms use a very flexible and ultrasensitive transducer. Whispering Gallery Mode makes use of a micro optical biosensor that can identify bacterial cell molecules and may be tweaked to detect certain fungus biomarkers (9). Fungal diagnostic research is expected to gain a lot from current and upcoming developments in bio-sensor technology, which employ a range of methodologies not yet used in medical mycology (9) .
Micro-needle-based diagnostics
Micro-needles are microscopic needles with a typical length of <1 mm and a width of 100 µm. These micro-projections can be shaped into different geometries, such as conical, pyramidal, cylindrical or even fang-like shapes, with or without a lumen, to enable effective skin penetration and bio-analysis (Fig. 4) (31). A micro-needle array is made up of hundreds of these micro-projections. As the micro-needles avoid contact with blood vessels and nerve endings, the devices produce no discomfort and are widely accepted by patients. Silicon, metals, polymers, ceramics, glass and, more recently, nanocomposite materials have all been used to create micro-needle devices (34). Historically, infectious illnesses, such as tuberculosis, were diagnosed using micro-needle based platforms (35).
Figure 4.
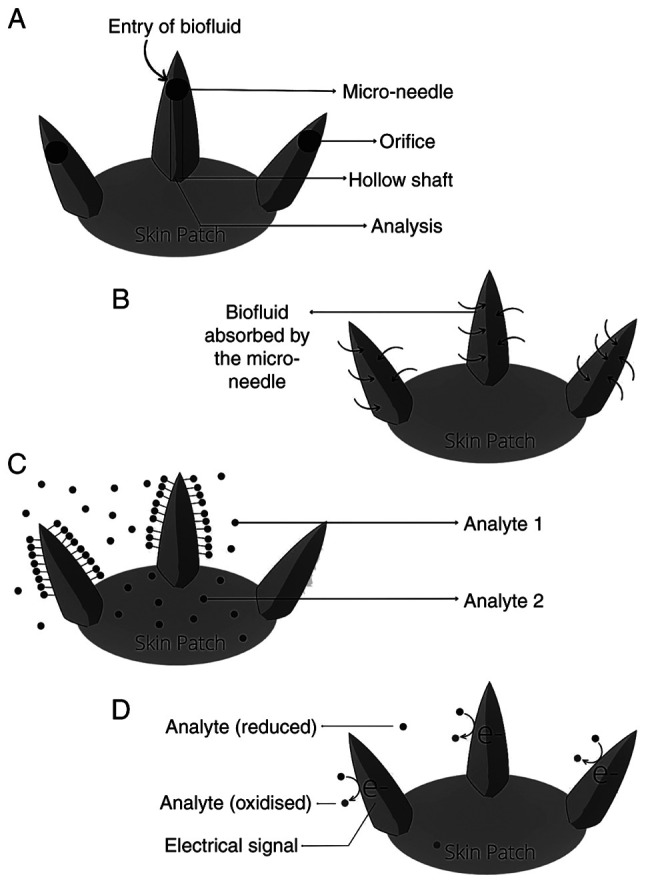
Illustration of how current micro-needle diagnostic platforms work. Micro-needle diagnostic platforms extract or detect target biofluid using (A) hollow micro-needles, (B) solid micro-needles, (C) analyte capture through specific target analyte or (D) electrochemical sensing.
There are various micro-needle based diagnostic systems that have been developed to collect or detect biomarkers in the skin. These include analyte capture micro-needles, micro-needle sensing systems, micro-needles for blood or interstitial fluid extraction, and combinations of these (34). Since the technological limitations are analogous, research into micro-needle-based diagnostics for communicable diseases can benefit from the specialized knowledge acquired via research on other diseases, even though not all techniques have been expressly proved for infectious illness detection (34). Since integrated lab-on-a-chip transdermal drug delivery devices may overcome bottlenecks and accessibility problems that afflict centralised test facilities, they have the potential to speed up a diagnosis. This makes the notion of such devices attractive to researchers. This is particularly true in the field of infectious illnesses, where there are already challenging requirements for transportation of individuals and samples, and other logistics.
5. Conclusions
The deadly fungal illness known as mucormycosis is initiated by saprophytic fungi Mucor or Rhizopus. Ingestion, inoculation or inhalation of fungus spores are all possible routes to infection. Mucormycosis is particularly common in individuals with diabetes, autoimmune illnesses, organ transplantation, haematological malignancies and weakened immune systems (14). The mortality rate of mucormycosis, particularly invasive mucormycosis, is >90% (34).
Early detection of mucormycosis is critical in preventing mortality and the spread of the disease. Clinical diagnosis, radiography and serology are all traditional diagnostic methods with limited diagnostic utility, thus making histology and microscopy key techniques in forming the majority of diagnoses.
Furthermore, depending on the observer's experience, interpretation of diagnostic results can vary, potentially leading to misdiagnosis (36). As a result, advanced serological assays such as ELISA, immunoblotting, immune-diffusion and ELISpot are required. Mucor-specific T lymphocytes are detected in the peripheral blood using the ELISpot assay. The ELISpot assay helps to reduce the percentage of patients with invasive mucormycosis who are treated with high-dose antifungal drugs only on the basis of clinical signs (27,37). Furthermore, nucleic acid diagnostics such as conventional PCR, RT-qPCR, PCR-ELISA, multiplex PCR, direct DNA sequencing and the MucorGenius rapid RT-qPCR test kit, a pan-Mucorale test, aid in the early detection of the fungus even when the fungal load is minimal (24). The most noteworthy benefit of this test is that it can detect five species of Mucor families, with blood and biopsy tissue serving as biomarker specimens (38). Biosensors and their components, as well as their functioning principles and types, have been suggested as future diagnostic tools that are species-specific and aid in the detection of specific fungal biomarkers. Biosensors enable continuous monitoring, which might be used to assess therapy effectiveness (9,39).
Future production and development of fungal biosensors for clinical use will require specific biomarkers, ideally from clinical samples, and superior immobilisation of the markers on the sensing surface. It is necessary to consider if it is possible to modify a suitable bio-fluid or biomarker for biosensor detection. Micro-needle diagnostics facilitate the detection of infectious diseases and expedite the diagnostic procedure. Micro-needles (long micro-needles) with functionalized bacterial encapsulation have been mixed with Bacillus subtilis, which is naturally present on human skin and widely used for food preparation, for effective fungal infection therapy (40). A range of antifungal medications that may specifically bind to proteins on the fungal cell are continuously produced and secreted by the encapsulated B. subtilis. Consistent production and release of different antifungal medications that can attach to molecules on the yeast cell surface-associated proteins and destroy the cell membranes may also help to prevent drug resistance (41).
Invasive fungal infections are regularly diagnosed using traditional diagnostic procedures. While the techniques used are capable of detecting fungal infections, they lack sensitivity and specificity in detecting the fungus. Newer diagnostic tests and methodologies, such as ELISA and RT-qPCR, have improved the diagnostic approaches available (25). The present study reviewed the traditional, present and future diagnostic tools for mucoromycosis, which assist in making an accurate diagnosis and initiating treatment as soon as possible to limit disease spread and mortality. To avoid fatal effects, mucormycosis must be detected as soon as possible. The diagnosis of mucormycosis is still difficult and although molecular approaches are advancing, histopathology, direct inspection and culture remain important tools. Direct culture and inspection continue to be needed as diagnostic tools, even if advanced diagnostic techniques have acquired approval for confirmation when applied to tissues. The importance of modern diagnostic procedures is at the forefront for the identification of mucormycosis at an earlier stage. The encouraging results of PCR methods based on the detection of Mucorale DNA in the blood is a promising approach for screening tests in high-risk patients (7).
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
The manuscript was written by DP and CMA. The original manuscript was proofread and revised by PSGP, RRR, GK, SRN and SS. The manuscript was referenced by RRR, GK and SRN. The figures were created by RRR. All authors read and approved the final version of the manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Rosenberg SW, Lepley JB. Mucormycosis in leukemia. Oral Surg Oral Med Oral Pathol. 1982;54:26–32. doi: 10.1016/0030-4220(82)90413-3. [DOI] [PubMed] [Google Scholar]
- 2.Abramson E, Wilson D, Arky RA. Rhinocerebral phycomycosis in association with diabetic ketoacidosis. Report of two cases and a review of clinical and experimental experience with amphotericin B therapy. Ann Intern Med. 1967;66:735–742. doi: 10.7326/0003-4819-66-4-735. [DOI] [PubMed] [Google Scholar]
- 3.Paltauf A. Mycosis mucorina. Arch für Pathol Anat und Physiol und für Klin Med. 1885;102:543–564. [Google Scholar]
- 4.Manjunatha BS, Das N, Sutariya RV, Ahmed T. Mucormycosis of the hard palate masquerading as carcinoma. Clin Pract. 2012;2(e28) doi: 10.4081/cp.2012.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: A review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004;10 (Suppl 1):S31–S47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 6.Janjua OS, Shaikh MS, Fareed MA, Qureshi SM, Khan MI, Hashem D, Zafar MS. Dental and oral manifestations of COVID-19 related mucormycosis: Diagnoses, management strategies and outcomes. J fungi (Basel) 2021;8(44) doi: 10.3390/jof8010044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: An update. J fungi (Basel) 2020;6(265) doi: 10.3390/jof6040265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pilmis B, Alanio A, Lortholary O, Lanternier F. Recent advances in the understanding and management of mucormycosis. F1000Res. 2018;7(F1000) doi: 10.12688/f1000research.15081.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hussain KK, Malavia D, Johnson EM, Littlechild J, Winlove CP, Vollmer F, Gow NAR. Biosensors and diagnostics for fungal detection. J fungi (Basel) 2020;6(349) doi: 10.3390/jof6040349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singhal N, Kumar M, Kanaujia PK, Virdi JS. MALDI-TOF mass spectrometry: An emerging technology for microbial identification and diagnosis. Front Microbiol. 2015;6(791) doi: 10.3389/fmicb.2015.00791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta MK, Kumar N, Dhameja N, Sharma A, Tilak R. Laboratory diagnosis of mucormycosis: Present perspective. J Family Med Prim Care. 2022;11:1664–1671. doi: 10.4103/jfmpc.jfmpc_1479_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54 (Suppl 1):S23–S34. doi: 10.1093/cid/cir866. [DOI] [PubMed] [Google Scholar]
- 13.Bhandari J, Thada PK, Nagalli S. Rhinocerebral Mucormycosis. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2022. [PubMed] [Google Scholar]
- 14.Corzo-León DE, Chora-Hernández LD, Rodríguez-Zulueta AP, Walsh TJ. Diabetes mellitus as the major risk factor for mucormycosis in Mexico: Epidemiology, diagnosis, and outcomes of reported cases. Med Mycol. 2018;56:29–43. doi: 10.1093/mmy/myx017. [DOI] [PubMed] [Google Scholar]
- 15.Goel A, Kini U, Shetty S. Role of histopathology as an aid to prognosis in rhino-orbito-cerebral zygomycosis. Indian J Pathol Microbiol. 2010;53:253–257. doi: 10.4103/0377-4929.64342. [DOI] [PubMed] [Google Scholar]
- 16.Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247–280. doi: 10.1128/CMR.00053-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sravani T, Uppin SG, Uppin MS, Sundaram C. Rhinocerebral mucormycosis: Pathology revisited with emphasis on perineural spread. Neurol India. 2014;62:383–386. doi: 10.4103/0028-3886.141252. [DOI] [PubMed] [Google Scholar]
- 18.Groppo ER, El-Sayed IH, Aiken AH, Glastonbury CM. Computed tomography and magnetic resonance imaging characteristics of acute invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 2011;137:1005–1010. doi: 10.1001/archoto.2011.170. [DOI] [PubMed] [Google Scholar]
- 19.Passi N, Wadhwa AC, Naik S. Radiological spectrum of invasive mucormycosis in COVID-19. BJR Case Rep. 2022;7(20210111) doi: 10.1259/bjrcr.20210111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Legouge C, Caillot D, Chrétien ML, Lafon I, Ferrant E, Audia S, Pagès PB, Roques M, Estivalet L, Martin L, et al. The reversed halo sign: Pathognomonic pattern of pulmonary mucormycosis in leukemic patients with neutropenia? Clin Infect Dis. 2014;58:672–678. doi: 10.1093/cid/cit929. [DOI] [PubMed] [Google Scholar]
- 21.Dadwal SS, Kontoyiannis DP. Recent advances in the molecular diagnosis of mucormycosis. Expert Rev Mol Diagn. 2018;18:845–854. doi: 10.1080/14737159.2018.1522250. [DOI] [PubMed] [Google Scholar]
- 22.Richardson M, Page I. Role of serological tests in the diagnosis of mold infections. Curr Fungal Infect Rep. 2018;12:127–136. doi: 10.1007/s12281-018-0321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burnham-Marusich AR, Hubbard B, Kvam AJ, Gates-Hollingsworth M, Green HR, Soukup E, Limper AH, Kozel TR. Conservation of mannan synthesis in fungi of the zygomycota and ascomycota reveals a broad diagnostic target. mSphere. 2018;3(e00094) doi: 10.1128/mSphere.00094-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lackner N, Posch W, Lass-Flörl C. Microbiological and molecular diagnosis of mucormycosis: From old to new. Microorganisms. 2021;9(1518) doi: 10.3390/microorganisms9071518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skiada A, Lass-Floerl C, Klimko N, Ibrahim A, Roilides E, Petrikkos G. Challenges in the diagnosis and treatment of mucormycosis. Med Mycol. 2018;56:93–101. doi: 10.1093/mmy/myx101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Potenza L, Vallerini D, Barozzi P, Riva G, Forghieri F, Zanetti E, Quadrelli C, Candoni A, Maertens J, Rossi G, et al. Mucorales-specific T cells emerge in the course of invasive mucormycosis and may be used as a surrogate diagnostic marker in high-risk patients. Blood. 2011;118:5416–5419. doi: 10.1182/blood-2011-07-366526. [DOI] [PubMed] [Google Scholar]
- 27.White PL. Recent advances and novel approaches in laboratory-based diagnostic mycology. Med Mycol. 2019;57:S259–S266. doi: 10.1093/mmy/myy159. [DOI] [PubMed] [Google Scholar]
- 28.Sue MJ, Yeap SK, Omar AR, Tan SW. Application of PCR-ELISA in molecular diagnosis. Biomed Res Int. 2014;2014(653014) doi: 10.1155/2014/653014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baldin C, Soliman SSM, Jeon HH, Alkhazraji S, Gebremariam T, Gu Y, Bruno VM, Cornely OA, Leather HL, Sugrue MW, et al. PCR-based approach targeting mucorales-specific gene family for diagnosis of mucormycosis. J Clin Microbiol. 2018;56(e00746) doi: 10.1128/JCM.00746-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandey M, Xess I, Sachdev J, Yadav U, Singh G, Pradhan D, Xess AB, Rana B, Dar L, Bakhshi S, et al. Development of a sensitive and specific novel qPCR assay for simultaneous detection and differentiation of mucormycosis and aspergillosis by melting curve analysis. Front Fungal Biol. 2022;2:1–11. doi: 10.3389/ffunb.2021.800898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asdaq SMB, Rajan A, Damodaran A, Kamath SR, Nair KS, Zachariah SM, Sahu RK, Fattepur S, Sreeharsha N, Nair A, et al. Identifying mucormycosis severity in indian COVID-19 patients: A nano-based diagnosis and the necessity for critical therapeutic intervention. Antibiot (Basel) 2021;10(1308) doi: 10.3390/antibiotics10111308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dutta P, Lu YJ, Hsieh HY, Lee TY, Lee YT, Cheng CM, Fan YJ. Detection of candida albicans using a manufactured electrochemical sensor. Micromachines. 2021;12(166) doi: 10.3390/mi12020166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cai D, Xiao M, Xu P, Xu YC, Du W. An integrated microfluidic device utilizing dielectrophoresis and multiplex array PCR for point-of-care detection of pathogens. Lab Chip. 2014;14:3917–3924. doi: 10.1039/c4lc00669k. [DOI] [PubMed] [Google Scholar]
- 34.Dixon RV, Skaria E, Lau WM, Manning P, Birch-Machin MA, Moghimi SM, Ng KW. Microneedle-based devices for point-of-care infectious disease diagnostics. Acta Pharm Sin B. 2021;11:2344–2361. doi: 10.1016/j.apsb.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samson R, Dharne M. COVID-19 associated mucormycosis: Evolving technologies for early and rapid diagnosis. 3 Biotech. 2022;12(6) doi: 10.1007/s13205-021-03080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu L, Zhou P, Zhao W, Hua H, Yan Z. Fluorescence staining vs. routine KOH smear for rapid diagnosis of oral candidiasis-A diagnostic test. Oral Dis. 2020;26:941–947. doi: 10.1111/odi.13293. [DOI] [PubMed] [Google Scholar]
- 37.Potenza L, Vallerini D, Barozzi P, Riva G, Gilioli A, Forghieri F, Candoni A, Cesaro S, Quadrelli C, Maertens J, et al. Mucorales-specific T cells in patients with hematologic malignancies. PLoS One. 2016;11(e0149108) doi: 10.1371/journal.pone.0149108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caramalho R, Madl L, Rosam K, Rambach G, Speth C, Pallua J, Larentis T, Araujo R, Alastruey-Izquierdo A, Lass-Flörl C, Lackner M. Evaluation of a novel mitochondrial pan-mucorales marker for the detection, identification, quantification, and growth stage determination of mucormycetes. J fungi (Basel) 2019;5(98) doi: 10.3390/jof5040098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang F, Zhang X, Chen G, Zhao Y. Living bacterial microneedles for fungal infection treatment. Res (Washington DC) 2020;2020(2760594) doi: 10.34133/2020/2760594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dannaoui E. Recent developments in the diagnosis of mucormycosis. J fungi (Basel) 2022;8(457) doi: 10.3390/jof8050457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma A, Goel A. Mucormycosis: Risk factors, diagnosis, treatments, and challenges during COVID-19 pandemic. Folia Microbiol (Praha) 2022;67:363–387. doi: 10.1007/s12223-021-00934-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.