Abstract
Background
The mental health of the UK population declined at the onset of the COVID-19 pandemic. Convenience sample surveys indicate that recovery began soon after. Using a probability sample, we tracked mental health during the pandemic to characterise mental health trajectories and identify predictors of deterioration.
Methods
This study was a secondary analysis of five waves of the UK Household Longitudinal Study (a large, national, probability-based survey that has been collecting data continuously since January, 2009) from late April to early October, 2020 and pre-pandemic data taken from 2018–19. Mental health was assessed using the 12-item General Health Questionnaire (GHQ-12). We used latent class mixed models to identify discrete mental health trajectories and fixed-effects regression to identify predictors of change in mental health.
Findings
Mental health was assessed in 19 763 adults (≥16 years; 11 477 [58·1%] women and 8287 [41·9%] men; 3453 [17·5%] participants from minority ethnic groups). Mean population mental health deteriorated with the onset of the pandemic and did not begin improving until July, 2020. Latent class analysis identified five distinct mental health trajectories up to October 2020. Most individuals in the population had either consistently good (7437 [39·3%] participants) or consistently very good (7623 [37·5%] participants) mental health across the first 6 months of the pandemic. A recovering group (1727 [12·0%] participants) showed worsened mental health during the initial shock of the pandemic and then returned to around pre-pandemic levels of mental health by October, 2020. The two remaining groups were characterised by poor mental health throughout the observation period; for one group, (523 [4·1%] participants) there was an initial worsening in mental health that was sustained with highly elevated scores. The other group (1011 [7·0%] participants) had little initial acute deterioration in their mental health, but reported a steady and sustained decline in mental health over time. These last two groups were more likely to have pre-existing mental or physical ill-health, to live in deprived neighbourhoods, and be of Asian, Black or mixed ethnicity. Infection with SARS-CoV-2, local lockdown, and financial difficulties all predicted a subsequent deterioration in mental health.
Interpretation
Between April and October 2020, the mental health of most UK adults remained resilient or returned to pre-pandemic levels. Around one in nine individuals had deteriorating or consistently poor mental health. People living in areas affected by lockdown, struggling financially, with pre-existing conditions, or infection with SARS-CoV-2 might benefit most from early intervention.
Funding
None.
Introduction
Marked declines in population mental health were observed in several countries after the onset of the COVID-19 pandemic. In eight countries (China, Spain, Italy, Iran, USA, Turkey, Nepal, and Denmark), relatively high rates of anxiety disorder, depression, post-traumatic stress disorder, psychological distress, and stress have been reported since the start of the pandemic.1 Using a random sample with pre-pandemic data, we previously reported that the prevalence of clinically significant levels of mental distress was 50% higher than before the pandemic a month after lockdown measures were introduced in the UK (April, 2020).2
As the pandemic develops, interest is turning to how changing circumstances have affected people's mental health and whether early indicators herald persistently poor mental health and subsequent increasing unmet clinical need. Studies assessing mental health trends since the beginning of the pandemic have reported symptoms of anxiety disorder, depression, and loneliness steadily improving since May, 2020.3, 4, 5 However, these studies have methodological problems relating to sampling, adjustment, and mental health measures. First, these studies used convenience samples, which means they cannot be adjusted properly for sampling bias and are thus considered poor tools for estimating population statistics.6, 7 Second, many studies have considerable attrition over time, and individuals with poor mental health are more susceptible to dropout,8 resulting in an overoptimistic assessment of mental health trends. Third, many studies used mental health indicators that were limited to symptoms occurring only in the past week.9 A clinical diagnosis of anxiety disorder or a depressive episode require symptoms to be consistently present for at least the past 2 weeks—otherwise, fluctuation in psychological distress commonly seen in healthy populations might become overstated as clinical illness. Most studies do not have comparable pre-pandemic data,10 which is important to understand whether the acute increases in mental distress in the population returned to pre-pandemic levels after the initial shock of its onset. Furthermore, the average trajectory for the whole population could mask varied responses to the pandemic—some groups might have remained or become increasingly vulnerable.
Research in context.
Evidence before this study
We searched Embase, PsychINFO, and MEDLINE for articles published in English between Jan 1 2020, and Jan 31, 2021, using search terms relating to mental health (‘psychiatr*' or ‘mental' or ‘distress’ or ‘depression’ or ‘anxiety’), COVID (‘covid’ or ‘coronavirus’ or ‘sars-cov-2), and longitudinal analysis (‘trajector*’ or ‘longitudinal’ or ‘latent curve’). Of 496 studies retrieved, only 13 conducted a trend analysis. Studies with a pre-pandemic baseline showed that population mental health deteriorated with the onset of the pandemic in the UK, USA, China, and European countries. Most studies were drawn from convenience samples, where participants are recruited according to ease of access. UK studies on trends since the beginning of the pandemic indicated a pattern of immediate recovery in the population overall and in all subgroups (regardless of gender, age, employment status, and other deprivation measures). However, studies that rely on follow-up from convenience samples might be biased towards a positive trend in mental health because study attrition is more likely among those with poor or deteriorating mental health.
Added value of this study
Using a longitudinal, probability sample survey to map mental health in the first 6 months of the COVID-10 pandemic in the UK, we found the elevated rates of poor mental health immediately after the onset of the pandemic (April 24–30, 2020) were sustained, with significant improvements occurring only from July, 2020 (when UK schools reopened, infection rates fell, and substantial relaxation of lockdown measures occurred). This study revealed that, although most of the population either remained resilient or reacted and recovered within the first 6 months of the pandemic, there are two groups of individuals of continuing concern. In one group, individuals' mental health deteriorated rapidly at the onset of the pandemic and showed no sign of recovery; the other group comprised people whose mental health progressively worsened month on month during the pandemic. Infection with SARS-CoV-2, previous physical or mental health conditions, and financial difficulties predicted subsequent deterioration in mental health during the pandemic.
Implications of all the available evidence
Socioeconomic pressures—both area-level deprivation and individual financial struggles—emerged as risk factors for deteriorating mental health during the pandemic, highlighting the need for policies aimed at socioeconomic inequalities in the recovery response. Confirmed infection with SARS-CoV-2 also strongly predicted a subsequent decline in mental health. These findings provide valuable information for policy makers and planners about the likelihood of changing needs for mental health services because of the pandemic.
There are crucial questions for public mental health concerning whether new disparities have emerged in population mental health and, if so, whose mental health has been poor during the pandemic. Understanding these questions is key to delivering preventive interventions for those at the highest risk, identifying where unmet clinical need might lie, and anticipating additional referrals for services. Common risk factors for mental health deterioration in the initial phase of the pandemic have been reported, including being a woman, being younger (≤40 years), having a chronic physical or mental illness, being unemployed, and having frequent exposure to social media or news coverage of COVID-19.1 Most of these risk factors were associated with poor mental health before COVID-19. In the early phases of the pandemic, young people, women, and parents living with preschool children saw greater than average decreases in mental health (measured by the 12-item General Health Questionnaire [GHQ-12]) compared with results of pre-pandemic studies.2 Whether these groups and characteristics are associated with sustained psychological distress as the pandemic has continued remains unclear. Additionally, although some of the determinants of worsening mental health might have receded after the early shock of pandemic onset and initial easing of national lockdown, some might have persisted, for example, infection with SARS-CoV-2,11 localised containment measures, and financial insecurity.12
We used a large, longitudinal panel sample, which was representative of the adult UK general population, with the overall aim of describing population trends in mental health during the first 6 months of the pandemic, overall and by age and gender.
We aimed to identify distinct trajectories in mental health over this period, describe the characteristics of individuals within each distinct mental health trajectory, and identify adversities that predict worsening mental health during the pandemic.
Methods
Study design and participants
Understanding Society, the UK Household Longitudinal Study (UKHLS) is a large, national, probability-based survey that has been collecting data continuously since January, 2009.13 The sample is representative of the UK population, comprising clustered, stratified samples of households in England, Scotland, and Wales and a non-clustered, systematic random sample in Northern Ireland. Areas with proportionately large migrant and ethnic minority populations were oversampled. The questionnaires were available in English and Welsh.
Before March, 2020, around half of data collection was done face-to-face and data were collected annually. With the onset of the COVID-19 pandemic, the survey transitioned online,14 with monthly, and then bi-monthly data collections from July, 2020. Panel members who took part in waves 8 or 9 (between Jan 1, 2016, and May 21, 2019) were invited to complete a series of web-based data collections in the last week of each month: April 24 to 30, May 27 to June 2, June 25 to July 1, July 24 to 31, and Sept 24 to Oct 1, 2020.
All household members aged 16 years or older were invited to participate, except for those unable to make an informed decision, because of incapacity, and those with unknown postal addresses or addresses abroad. Those aged 16 years in April, 2020, were not eligible to complete the UKHLS at previous waves, but participated in the COVID-19 survey if they were from eligible households (ie, those with at least one participant in the two most recent waves of the main survey).
Invitations were sent to 42 330 panel members. 17 761 participated in April (a 42·0% response rate), 14 811 (35·0%) in May, 14 123 (33·4%) in June, and 13 754 (32·5%) in July. For the September, 2020, survey only panel members who had completed at least one COVID web survey were invited (66·4% of the issued sample; 30·4% of the total eligible panel). Responses were linked to pre-pandemic data from Understanding Society's main survey wave 10 (most participants surveyed between January, 2018, and December, 2019). Analyses used longitudinal non-response weights as calculated and described in detail by the data custodians15 and provided with the September wave. Unweighted and weighted statistics for each wave and patterns of non-response to the COVID-19 web surveys are provided in the appendix (pp 1–5).
Individuals gave oral informed consent for participation in the study. Ethics approval was granted by the University of Essex Ethics Committee for the COVID-19 web and telephone surveys (ETH1920-1271).
Procedures
We calculated a composite score from summing items in the GHQ-12, which is validated as a unidimensional measure of psychological distress in the past 2 weeks in non-clinical populations.16 The GHQ-12 was administered by self-completion in wave 10 and in each of the five COVID-19 web survey waves. The items refer to difficulties with sleep, concentration, problems in decision making, strain, feeling overwhelmed, and other indicators of distress. GHQ-12 items were scored as follows: 0, not at all; 1, no more than usual; 2, rather more than usual; or 3, much more than usual. A total score was derived for each wave (0–36). In addition to the total score, used when generating a mean score, a binary measure was derived identifying those reporting distress in at least four of the 12 items. A score of 4 or more is used to indicate a level of mental distress that is clinically relevant.
Sociodemographic variables included gender (women vs men), age (16–24 years, 25–34 years, 35–44 years, 45–54 years, 55–69 years, and ≥70 years) and ethnicity (White British, White other, mixed, Asian, Black, or other). Household structure captured indicators of whether the participant lived with a partner (yes vs no) and the age of the youngest child living in the household (no children, 0–5 years, or 6–15 years). Area-level context was captured with geography (Wales, Scotland, Northern Ireland, and English region) and quintiles based on ranked Index of Multiple Deprivation (IMD) scores, an area-level deprivation measure mapped to lower layer super output areas (median population size of 1500) that was only available for England. Thus, analyses by IMD quintile were done in the sample of residents in England only.
Presence of a pre-existing mental condition was identified using previous UKHLS waves by the question: “has a doctor or other health professional diagnosed you with a psychiatric illness?” Indicator variables were constructed to identify individuals who had been asked by the UK National Health Service to shield during the pandemic because of an underlying physical illness or health condition and those who identified as keyworkers, who were obliged to continue working in certain sectors during lockdowns. COVID-related adversities were captured with three indicators. The first was SARS-CoV-2 infection status, drawing on responses to questions about the results of any coronavirus test a participant had had, whether they suspected but had not confirmed that they had contracted the virus, and whether they had had symptoms. Responses were categorised as follows: no suspected case, suspected but unconfirmed case, and confirmed case. Second, we created a binary variable to indicate whether participants had problems with paying bills during the pandemic. This variable was only available from three of the five COVID related waves. Finally, whether the participant lived in an area with local lockdown measures was determined (for England only) using local authority code. This variable was mapped to dates when participants had been mandated to be under partial or full reimposition of measures to control the spread of SARS-CoV-2, or the deferring of planned easing of restrictions, in response to a localised spike in infections.17 A list of local authorities that had local lockdown restrictions, their implementation dates, and a description of lockdown measures in the UK are provided in the appendix (p 6).
Statistical analysis
Population-level changes in mean GHQ-12 score and the proportion of individuals with clinically significant levels of mental distress during the pandemic were examined graphically and compared with means from wave 10 (2018 to 2019). We constructed latent class mixed models to identify typical distinct trajectories of mental health over the pandemic using the Stata program GLLAMM.18 These models included fixed effects for time (parameterised as time since first COVID-19 data collection) and discrete random variables for the latent classes. A four-latent class model was initially fitted to determine whether a squared term for time and a random intercept and slope were a good fit for the data (as indicated by a likelihood ratio test). Once the functional form of the model was determined, models were fitted with one to seven latent classes. Each model with two or more classes used random starting values from the model with one fewer class and a grid-search technique was used (with 50 iterations) to avoid the model identifying local maxima.
Model fit was determined using the Bayesian information criterion, the sample size-adjusted Bayesian information criterion, the adjusted Vuong-Lo-Mendell-Rubin likelihood ratio test, and a measure of entropy. The Bayesian information criterion measures used a correction for the sample size to account for the correlated nature of the data19 and the entropy statistic value was normalised.20 In addition to these fit statistics, models were compared graphically to examine whether a larger number of latent classes provided a clearer theoretical interpretation of the data.
After selection of the best model, participants were classified according to their most likely group and group membership was cross tabulated with baseline covariates. To test for association between covariates and latent class membership, it was necessary to account for the uncertainty in individuals' group membership. This was done using Wang and colleagues three step procedure,21 which involved creating 10 imputed datasets with class membership determined using a random variable created from the posterior probabilities from the mixed model. Next, a univariable multinomial logistic regression model was fitted to each imputed dataset, with class membership as the dependent variable. The p-value for the association between covariates and class membership was determined using Rubin's rules to combine the f-test from each model. The latent class trajectory analysis was reported in line with the Guidelines for Reporting on Latent Trajectory Studies checklist (appendix p 7).
1442 (7·3%) of 19 763 participants had missing GHQ-12 score data for all their COVID-19 waves and were excluded. Those with missing GHQ-12 data had similar gender distribution and previous mental health prevalence to the analysis sample but were younger and more likely to be from the lowest area-level deprivation quintile (appendix p 5). Sociodemographic variables were cross tabulated with group membership. No covariate had more than 5% of data missing; all missing data were excluded from cross-tabulations.
Fixed-effect models were fitted to individuals' repeated GHQ-12 scores to ascertain which of three COVID-19 adversity variables were associated with a change in GHQ-12 score. These were confirmed or suspected infection with SARS-CoV-2 infection; local lockdown measures; and reported problems paying bills. These models included parameters for time since first wave of data collection (as a continuous variable and its square, both with p<0·01 from Wald test), subject-specific effects that captured all time-invariant confounders, and time-dependent adversity variables.
In a sensitivity analysis, the GHQ-12 total for each participant was recalculated removing the question “have you recently been able to enjoy your normal day-to-day activities?,” which was considered potentially to be indicative of pandemic-related restrictions rather than mental health. Population trends and fixed-effects models were then refitted on this adapted version of the GHQ-12.
All analyses accounted for sampling probability weights. Cross-tabulations and calculations of means also accounted for clustered and stratified sampling using the svy suite of commands in Stata. Analyses were done using Stata (version 14) and graphs were produced using R package ggplot2.
Role of the funding source
There was no funding source for this study.
Results
19 763 participants contributed data to at least one of the COVID-19 web surveys (11 477 [58·1%] women and 8287 [41·9%] men; median follow-up 153 days, IQR 62–153). 10 541 (53%) participants completed all COVID-19 web surveys and 3787 (19%) completed only one (2794 [14%] completed just the first survey; appendix p 4). A further 1442 (7·3%) participants did not complete the GHQ-12 questions at least once and were excluded. A detailed description of respondents, patterns of web-survey non-response, and characteristics of those with missing GHQ-12 data are provided in the appendix (pp 1, 4–5).
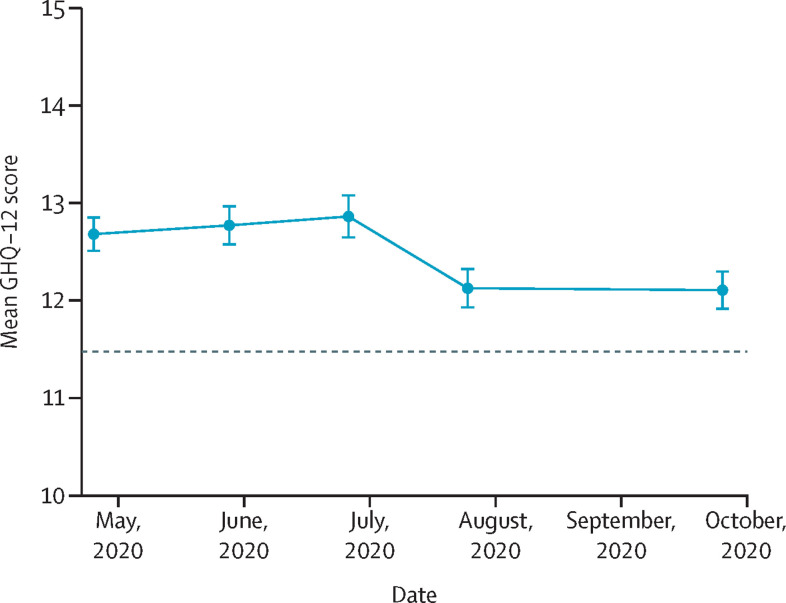
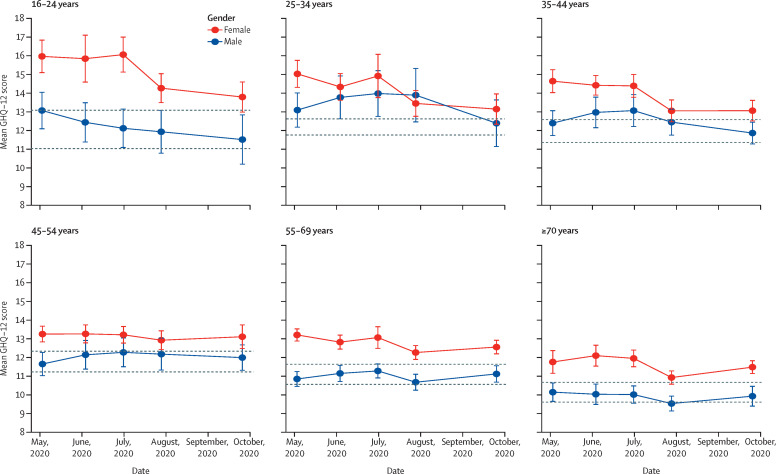
During the first five waves of the COVID-19 web survey, the mean GHQ-12 score for the whole population peaked at 12·9 at the end of June, 2020, before improving, although not to pre-pandemic levels (figure 1 ). The temporal trend varied by gender and age group (figure 2 ), with the initial peak most pronounced among those aged 16–24 years. Participants aged 45 years and older had relatively little variation in mean GHQ-12 score over time up to October, 2020. A similar pattern in temporal trends was evident in the prevalence of clinically significant levels of mental distress (appendix p 12).
Figure 1.
Overall mean GHQ-12 score by month of data collection
The dashed horizontal line represents the pre-pandemic mean (from 2018–19). Error bars represent 95% CIs. GHQ-12=General Health Questionnaire.
Figure 2.
Mean GHQ-12 score by month of data collection, by age group and gender
The dashed horizontal lines represent the pre-pandemic mean (from 2018–19). Error bars represent 95% CIs. GHQ-12=General Health Questionnaire.
When examining temporal trends for individual GHQ-12 items, we found greater temporal variation for some items than others (appendix p 13). Enjoyment in day-to-day activities showed the strongest effect of the pandemic, at least initially. Other items indicative of a sustained effect of the pandemic were loss of sleep, feeling under strain, and feeling unhappy and depressed. Sensitivity analysis revealed that these trends persisted when the question “Have you recently been able to enjoy your day-to-day activities?” was removed from the GHQ-12 total (appendix p 14).
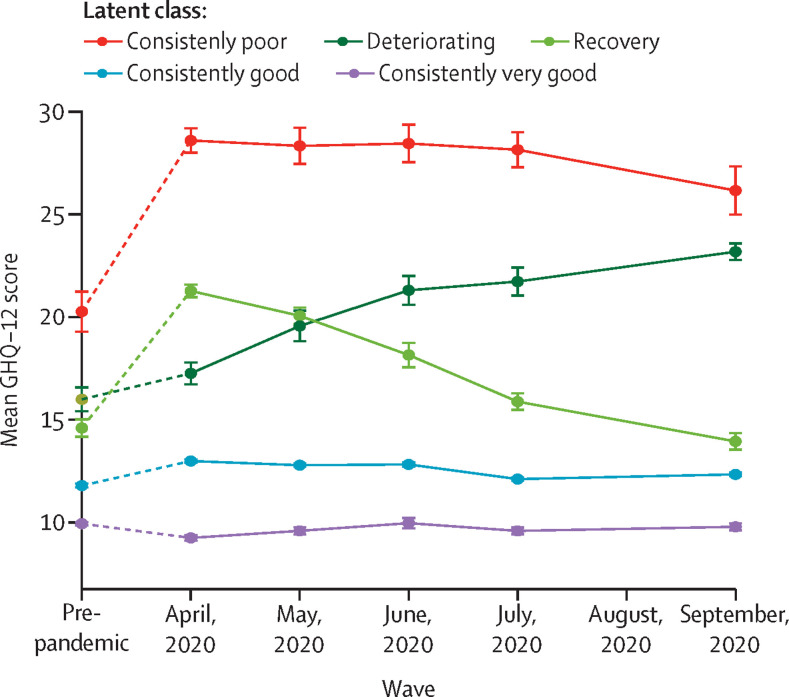
After fitting models with one to seven latent classes, the five-class model was considered the best fit (appendix pp 8–9). Even though models with a greater number of latent classes were associated with lower Bayesian information criterion values, the drop in Bayesian information criterion plateaued after five classes. Additionally, models with a greater number of classes were associated with considerably poorer entropy (a measure of information) and contained low-prevalence subclasses of the smaller model. Therefore, we opted for the more parsimonious five-class model.
From this model, five distinct mental health trajectories emerged (figure 3 ). Most individuals in the population had either consistently good (7437 [39·3%] participants) or consistently very good (7623 [37·5%] participants) mental health across the first 6 months of the pandemic to October, 2020, with little divergence from their pre-pandemic scores. A recovering group (1727 [12·0%] participants) showed worsened mental health during the initial shock of the pandemic and then returned to around pre-pandemic levels of mental health by October, 2020. The two remaining groups were characterised by poor mental health throughout the observation period; for one group, (523 [4·1%] participants) there was an initial worsening in mental health that was sustained with highly elevated scores. The other group (1011 [7·0%] participants) had little initial acute deterioration in their mental health, but reported a steady and sustained decline in mental health over time.
Figure 3.
Observed mean GHQ-12 score from five class-specific trajectories across five waves of data collection during the pandemic
The dashed line indicates the change from the pre-pandemic score. Error bars represent 95% CIs. GHQ-12=General Health Questionnaire.
Characteristics of people following the five trajectories are shown in table 1 . People with consistently very good mental health were more likely than those with good mental health, as well as more likely than the rest of the general population, to be men, older (aged ≥45 years), partnered, without previous health conditions, and to live in the most affluent neighbourhoods. By contrast, those in the deteriorating mental health group were more likely to be women, Asian, younger (aged 16–35 years), without a partner, and have a previous mental illness. Participants in the consistently very poor mental health group were more likely than the general population to be of mixed ethnicity, women, shielding, living in deprived neighbourhoods, without a partner, and have previous mental illness. People in the recovering category, characterised by initial reaction followed by recovery, were more likely to be women, young adults, or have children living in the household. People from the mixed ethnic group were overrepresented in the very poor group, and Asian people were more likely to have followed a deteriorating trajectory (appendix p 10).
Table 1.
Membership in each latent class group according to key demographics
| Total (n=18 321) | Consistently very good (n=7623; 37·5%) | Consistently good (n=7437; 39·3%) | Recovery (n=1727; 12·0%) | Deteriorating (n=1011; 7·0%) | Consistently very poor (n= 523; 4·1%) | p value* | ||
|---|---|---|---|---|---|---|---|---|
| Gender | .. | .. | .. | .. | .. | .. | <0·0001 | |
| Female | 7665 (51·6%) | 3574 (43·0%) | 2969 (54·3%) | 573 (61·8%) | 355 (57·4%) | 194 (63·1%) | .. | |
| Male | 10 655 (48·5%) | 4048 (57·0%) | 4468 (45·7%) | 1154 (38·2%) | 656 (42·6%) | 329 (36·9%) | .. | |
| Age (years) | .. | .. | .. | .. | .. | .. | <0·0001 | |
| 16–24 | 1474 (11·8%) | 532 (7·9%) | 627 (13·2%) | 164 (15·0%) | 99 (16·2%) | 52 (15·6%) | .. | |
| 25–34 | 1968 (15·7%) | 661 (11·2%) | 872 (15·8%) | 239 (24·8%) | 123 (21·6%) | 73 (20·4%) | .. | |
| 35–44 | 2788 (15·1%) | 1071 (12·9%) | 1135 (15·7%) | 312 (19·0%) | 173 (15·0%) | 97 (18·5%) | .. | |
| 45–54 | 3687 (17·9%) | 1462 (18·7%) | 1562 (17·4%) | 359 (15·2%) | 208 (18·2%) | 96 (22·5%) | .. | |
| 55–69 | 5419 (23·9%) | 2388 (27·8%) | 2139 (23·6%) | 443 (16·5%) | 295 (21·0%) | 154 (18·7%) | .. | |
| ≥70 | 2985 (15·6%) | 1509 (21·6%) | 1102 (14·3%) | 210 (9·5%) | 113 (8·1%) | 51 (4·3%) | .. | |
| Ethnicity | .. | .. | .. | .. | .. | .. | <0·0001 | |
| White British | 14 979 (86·9%) | 6269 (87·9%) | 6081 (88·0%) | 1381 (84·8%) | 820 (85·1%) | 428 (77·3%) | .. | |
| White other | 732 (3·5%) | 297 (3·7%) | 312 (3·9%) | 61 (2·7%) | 47 (2·1%) | 15 (2·7%) | .. | |
| Mixed | 318 (2·1%) | 118 (1·3%) | 131 (1·8%) | 41 (2·7%) | 12 (1·7%) | 16 (10·2%) | .. | |
| Asian | 1397 (5·1%) | 550 (4·0%) | 557 (4·7%) | 161 (7·3%) | 85 (8·9%) | 44 (5·2%) | .. | |
| Black | 449 (1·9%) | 198 (2·7%) | 173 (1·3%) | 45 (1·0%) | 21 (1·6%) | 12 (4·4%) | .. | |
| Other | 93 (0·5%) | 32 (0·5%) | 38 (0·3%) | 15 (1·5%) | 7 (0·6%) | 1 (0·2%) | .. | |
| Age of youngest child in household, years | .. | .. | .. | .. | .. | .. | 0·092 | |
| No children | 13 232 (73·8%) | 5609 (75·8%) | 5353 (74·5%) | 1176 (67·9%) | 711 (70·2%) | 383 (71·7%) | .. | |
| <6 | 1610 (4·3%) | 625 (3·6%) | 658 (4·6%) | 175 (5·9%) | 107 (3·9%) | 45 (3·7%) | .. | |
| 6–15 | 3479 (18·3%) | 1389 (17·4%) | 1426 (17·6%) | 376 (20·6%) | 193 (20·7%) | 95 (21·9%) | .. | |
| Lives with partner | .. | .. | .. | .. | .. | .. | <0·0001 | |
| Yes | 12 573 (59·8%) | 5455 (68·3%) | 5106 (60·8%) | 1097 (47·5%) | 627 (45·0%) | 288 (34·4%) | .. | |
| No | 5748 (40·2%) | 2168 (31·7%) | 2331 (39·3%) | 630 (52·5%) | 384 (55·0%) | 235 (65·6%) | .. | |
| Keyworker | .. | .. | .. | .. | .. | .. | 0·056 | |
| Yes | 5815 (31·1%) | 2250 (28·9%) | 2527 (34·2%) | 559 (28·7%) | 339 (30·9%) | 140 (29·3%) | .. | |
| No | 12 504 (68·9%) | 5375 (71·1%) | 4908 (65·9%) | 1168 (71·3%) | 672 (69·1%) | 383 (70·7%) | .. | |
| NHS shielding letter received | .. | .. | .. | .. | .. | .. | 0·027 | |
| Yes | 1136 (7·2%) | 453 (6·1%) | 448 (6·4%) | 112 (9·1%) | 61 (10·1%) | 62 (15·2%) | .. | |
| No | 17 181 (92·8%) | 7167 (93·9%) | 6988 (93·6%) | 1615 (90·9%) | 950 (89·9%) | 461 (84·8%) | .. | |
| Index of Multiple Deprivation quintile | .. | .. | .. | .. | .. | .. | <0·0001 | |
| Most deprived | 2215 (17·9%) | 889 (14·4%) | 850 (17·0%) | 241 (22·5%) | 137 (23·3%) | 98 (37·0%) | .. | |
| Second | 2670 (18·9%) | 1089 (18·5%) | 1087 (18·4%) | 258 (19·4%) | 162 (21·6%) | 74 (21·5%) | .. | |
| Third | 2940 (19·8%) | 1214 (19·5%) | 1213 (21·1%) | 289 (21·6%) | 137 (14·3%) | 87 (15·7%) | .. | |
| Fourth | 3427 (22·5%) | 1464 (24·6%) | 1394 (21·1%) | 312 (22·5%) | 173 (23·5%) | 84 (15·5%) | .. | |
| Least deprived | 3526 (20·8%) | 1515 (23·1%) | 1441 (22·4%) | 309 (14·0%) | 191 (17·4%) | 70 (10·3%) | .. | |
| Previous mental illness | .. | .. | .. | .. | .. | .. | <0·0001 | |
| Yes | 1189 (6·6%) | 321 (2·6%) | 496 (6·6%) | 178 (12·4%) | 101 (11·0%) | 93 (18·0%) | .. | |
| No | 16 815 (93·4%) | 7158 (97·4%) | 6812 (93·4%) | 1529 (87·6%) | 892 (89·0%) | 424 (82·0%) | .. | |
Numbers relate to the absolute frequency and percentages relate to the proportion after weighting. NHS=UK National Health Service.
p values from multinomial logistic model following multiple imputation. Relative rate ratios from multinomial logistic regression comparing likelihood of class membership with very good class are provided in the appendix (p 10).
Results from fixed-effects regression showed that reporting a confirmed or suspected SARS-CoV-2 infection was associated with a subsequent increase in GHQ-12 score, which was more pronounced among confirmed cases (mean change in GHQ-12 score 2·08, 95% CI 1·06–3·10) than for suspected cases (0·23, 0·04–0·41; table 2 ). Living in an area under local lockdown measures (0·24, 0·01–0·46) and having problems paying bills (0·59, 0·12–1·06) were also linked to subsequent worsening in mental health. In sensitivity analysis, these inferences were consistent when an adapted version of the GHQ-12 was used (appendix p 11).
Table 2.
Fixed-effect model of effect of dynamic time-dependent variables on within-subject change in GHQ-12
| Change in GHQ-12*(95% CI) | ||
|---|---|---|
| Local lockdown | 0·24 (0·01–0·46) | |
| SARS-CoV-2 infection status | ||
| No suspected symptoms | 1 (ref) | |
| Suspected case | 0·23 (0·04–0·41) | |
| Confirmed case | 2·08 (1·06–3·10) | |
| Problems paying bills | 0·59 (0·12–1·06) | |
Wave-specific frequencies for each covariate are in the appendix (pp 1–3). GHQ-12=General Health Questionnaire.
β coefficients from fixed effects model.
Discussion
In this study, we found that in a random probability sample of UK participants across the first 6 months of the COVID-19 pandemic up to October, 2020, overall mental health only began to recover in July, 2020 (later than previously reported3). Mental health continued to improve through to October, 2020, although not to pre-pandemic levels. This overall view masks the very different experiences encountered by people as the pandemic progressed, which we identified using latent class analysis. Five distinct trajectories emerged. Around three quarters of participants had either consistently very good or good mental health throughout the pandemic; a substantial minority of participants reported a very different experience, with very poor or steadily worsening mental health and, by October, 2020, had far more mental health symptoms than before the pandemic. These trajectories were not equally distributed within the population. Living in a deprived neighbourhood, shielding for health reasons, and self-reporting a previous mental illness were all significantly more common in individuals whose mental health worsened between April and October, 2020. Men, older age groups, and those living in affluent areas were most likely to have maintained good mental health throughout the pandemic.
For women, the picture was complex. They were more likely than men to have deteriorating or very poor mental health trajectories. However, compared with our previous report, in which women were reported as being more affected than men at the start of the pandemic,2 in this update, women were over-represented in the recovered group. Notably, this was also the case for parents of young children and for young people, many of whom suffered precipitous decline in their mental health at the beginning of the pandemic,2 but who appear to have better mental health by October, 2020. Several factors might play a part in the improving mental health of these individuals over this period. For example, easing of national containment measures, school re-openings, summer holidays, and falling infection and death rates. Although socioeconomic context was not a predictor of larger increases in distress initially, over the course of the pandemic this factor gained predictive power. Similarly, Asian, Black and mixed ethnicity individuals did not have elevated levels of distress early in the pandemic, but in this analysis Asian and mixed ethnicity individuals were overly represented in the very poor or deteriorating groups, indicating that minority ethnic groups might need ongoing support during the pandemic.
Our findings support the results of registry studies that reported a diagnosis of COVID-19 is associated with a subsequent decline in mental health.11 Longer-term follow-up of patients with confirmed SARS-CoV-2 infection is required to assess who is most affected and whether this translates into long-term clinical need for mental health services. Also, for the first time to our knowledge, we observed that local lockdown measures were negatively affecting mental health.
The overall positive message in the UK about the mental health of the general population during the pandemic appears to mirror findings from earlier convenience surveys, which reported a rapid decline in mental health to the lowest level at the beginning of the pandemic, followed by a bounce back.3 Our results are also consistent with most reports from the USA22 and across Europe,3, 5 showing improvement in mental health in populations since the initial deterioration at the beginning of the pandemic. However, whereas these reports find that improvements in mental health occurred almost immediately after the start of the pandemic, we found that recovery in overall population mental health did not occur in the UK until July, 2020, coinciding with lifting of the national lockdown measures. Other studies might have overstated the pace of recovery for three reasons. First, surveys using convenience samples are unrepresentative, even after demographic adjustments;7 second, high-frequency online data collection, with no supplementary telephone interviews, can lead to particular loss of participants with poor or declining mental health, resulting in assessment of trends which are biased towards better mental health;8 and third, use of wellbeing and measures relating to short periods (such as yesterday or the past week) are likely to show more volatility (and less clinical relevance) than measures relating to the past 2 weeks.
Our findings provide important new signals of deteriorating mental health in particular groups of people as the pandemic developed through to the autumn of 2020. Most studies have defined groups by social or economic characteristics and described the mental health trajectory of these. By contrast, we identified varying mental health trajectories and then described the social and economic characteristics associated with each distinct trajectory. This approach led to a focus on those with deteriorating or consistently poor mental health and allowed us to identify individuals with the greatest clinical relevance and isolate predictors of deterioration. Such information might be especially relevant given Chandola and colleagues12 report of deteriorating mental health in those with financial stressors using the same COVID-19 Understanding Society dataset up to July, 2020. However, this study12 did not find an effect of having problems paying bills, which might result from the lower statistical power of shorter follow-up and a dichotomised outcome measure. The five distinct trajectories that we identified are strikingly similar to those reported across six years of data collection in the UK, albeit using a different measure (the 12-item Short Form).23 We might conclude from this comparison that the pandemic has resulted in an acceleration of the rate of change of mental health among UK adults. The fact that those in the lowest income areas were more likely to have mental health declines suggests that existing mental health inequalities are being accentuated.
Our analysis has several important strengths. First, the sample was identified using random probability sampling. This methodology is greatly preferable compared with surveys that use convenience sampling, which lack a theoretical basis for correcting sampling bias or for statistical inference.6 Second, as well as including multiple timepoints after the onset of the COVID-19 pandemic in the UK, unlike many other mental health surveys during the pandemic, our sample includes pre-pandemic data, allowing us to understand whether individuals' mental health recovered to pre-pandemic levels. The longitudinal nature of the data enabled discrete trajectories of change to be discerned. Lastly, the large sample size and rich set of covariates provide sufficient statistical power to identify latent class trajectories and characteristics that were associated with them.
This study has some limitations. We lacked longitudinal data on some factors that might have given a more complete picture of the determinants of mental health during the pandemic, such as exposure to violence and abuse, or health behaviours. Heterogeneity revealed by the latent class models could indicate other time-dependent effects not captured by the model, or might explain the associations identified by the fixed-effect regression. For example, local lockdowns were enforced when there were localised spikes in infections; therefore, increases in the GHQ-12 score might have been better explained by factors associated with infectious disease outbreaks rather than local lockdowns. Additionally, fixed-effects models affect generalisability because individuals who do not have change in the independent variable are excluded.24 However, drawbacks associated with the fixed-effects model are outweighed by the fact that all time-invariant confounders are accounted for.25 Although the GHQ-12 score is a validated measure of mental health,16, 26 it is not equivalent to a clinical diagnosis. A previous mental illness diagnosis was ascertained from self-report, and the estimated prevalence (6·6%) was lower than expected, indicating underreporting. This might be because of socially desirable responding or could indicate non-response bias that was not accounted for in the sample weights, potentially leading to underestimation of the prevalence of deteriorating or consistently poor mental health. These data might normally be ascertained from routinely collected clinical contacts; however, there has been a decrease in visits to primary care for mental illness,27 even though individuals' mental health was apparently worsening. We have not adjusted for seasonal variation in population mental health.28 Using data from the same survey, we and others29 have previously found that any effects of seasonal and year-to-year variation on mental health were minimal and unlikely to account for changes in population mental health during the pandemic. Finally, our study only includes data up to the beginning of October, 2020, before the second and third waves of COVID-19 restrictions in the UK. National survey data reported that post-pandemic anxiety was at its lowest in July, 2020, and increased again up to January, 2021.30
Compared with previous rapid convenience surveys, which suggested the mental health of individuals in the UK adjusted quickly to the social changes surrounding the pandemic, our results imply that a more prolonged deterioration in mental health occurred, with relatively little psychological adjustment or habituation, until July, 2020, coinciding with the revocation of national lockdown measures. We also found an effect of localised lockdowns on levels of mental distress. We might anticipate similar effects to have occurred during subsequent national lockdowns in November, 2020, and January, 2021.
Our findings have important implications for mental health policy makers and service planners. Many individuals with deteriorating mental health might be existing service users whose symptoms have been worsening over time. As the pandemic has progressed, socioeconomic effects have emerged as strongly associated with declining mental health, suggesting that mental health might continue to deteriorate with the double dip recession anticipated for the UK post-Brexit and post-pandemic.31 Therefore, socioeconomic policies should be central to post-pandemic recovery programmes to address the mental health effects seen in low-income communities and the further likely effects of school closures, financial hardship, job insecurity, and local restrictions. Mental health services might also expect to see increased referrals from the around 10% of individuals recovering from COVID-1932 who develop features of so-called long COVID, including psychiatric illness.11
Preventive interventions might usefully be targeted at the vulnerable groups of people whom we have identified. In advance of further lockdowns or future pandemics, public mental health should be a priority and support should be focussed on deprived communities, while local authority public health measures and social welfare should target deprived families and individuals.
Data sharing
The main cohort data are publicly available via UK Data Service repository (study numbers 6614 and 8644), and do not require ethical assessment for academic research purposes. The use of area-level information (SN 7248) is provided under a UK Data Service special license. Our statistical code is available on request to the corresponding author.
Declaration of interests
MH reports grants from Innovative Medicines Initiative, outside the submitted work. SLH reports grants from the National Institute for Health Research, grants from the Economic and Social Research Council (ESRC), grants from Wellcome Trust, grants from the Medical Research Council, and grants from Guy's and St Thomas' Charity, outside the submitted work; is a member of the following advisory groups: ethnic inequalities in health care among people with multiple conditions (University of Sussex), Advisory Board NHS Race and Health Observatory, Co-Chair Academic Reference Group and Board Member The Royal Foundation, Mental Health Research Group NHS England and NHS Improvement, The Mental Health Equalities Data Quality and Research Subgroup NHS England and NHS Improvement, Patient and Carers Race Equalities Framework Steering Group NHS England and NHS Improvement, Advancing Mental Health Equalities Taskforce Health Education England, Mental Health Workforce Equalities Subgroup Maudsley Learning, Maudsley Learning Advisory Board South London and Maudsley NHS Foundation Trust (SLaM), Independent Advisory Groups, the SLaM Partnership Group, Lambeth Public Health, Serious Youth Violence Public Health Task and Finish Group Thrive London, Thrive London Advisory Board Black Thrive, Black Thrive Advisory Board NHS England and NHS Improvement, The Mental Health Workforce Equalities Subgroup Commissions: Welsh Government's Race Equality Plan; and contributed to the evidence review for Health and Social Care and Employment and Income policy areas. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
The Understanding Society COVID-19 Study is funded by the ESRC and the Health Foundation Ipsos. Fieldwork for the study is carried out by MORI and Kantar. Understanding Society is an initiative funded by the ESRC and various UK Government departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex. The research data are distributed by the UK Data Service.
Contributors
MP, KMA, and SM devised the study concept. MP wrote the initial analysis plan with input from KMA, SM, and MH. MP did the data analysis and produced the figures. KMA, MP, and SM wrote the first draft of the manuscript and all authors contributed to editing and commenting on the final version. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19: longitudinal analyses of 36,520 adults in England. Lancet Psychiatry. 2020;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varga TV, Bu F, Dissing AS, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200 000 Western and Northern Europeans. Lancet Reg Health Eur. 2021;2 doi: 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierce M, McManus S, Jessop C, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benzeval M, Burton J, Crossley TF, et al. High frequency online data collection in an annual household panel study: some evidence on bias prevention and bias adjustment. March 5, 2021. https://www.iser.essex.ac.uk/research/publications/working-papers/understanding-society/2021-03
- 8.Czeisler MÉ, Wiley JF, Czeisler CA, Rajaratnam SMW, Howard ME. Uncovering survivorship bias in longitudinal mental health surveys. medRxiv. 2021 doi: 10.1101/2021.01.28.21250694. published online Feb 17. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saunders R, Buckman JEJ, Fonagy P, Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol Med. 2021 doi: 10.1017/S0033291721000957. published online March 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thombs BD, Bonardi O, Rice DB, et al. Curating evidence on mental health during COVID-19: a living systematic review. J Psychosom Res. 2020;133 doi: 10.1016/j.jpsychores.2020.110113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandola T, Kumari M, Booker CL, Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med. 2020 doi: 10.1017/S0033291720005048. published online Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.University of Essex. Institute for Social and Economic Research. NatCen Social Research. Kantar Public . 12th edition. UK Data Service; 2019. Understanding society: waves 1-9, 2009–2018 and Harmonised BHPS: waves 1–18, 1991–2009 [data collection] [DOI] [Google Scholar]
- 14.Burton J, Lynn P, Benzeval M. How Understanding Society: The UK Household longitudinal study adapted to the COVID-19 pandemic. Surv Res Methods. 2020;14:235–239. [Google Scholar]
- 15.Institute of Social and Economic Research . University of Essex; Colchester: 2020. Understanding society COVID-19 user guide. Version 5.0. [Google Scholar]
- 16.Pevalin DJ. Multiple applications of the GHQ-12 in a general population sample: an investigation of long-term retest effects. Soc Psychiatry Psychiatr Epidemiol. 2000;35:508–512. doi: 10.1007/s001270050272. [DOI] [PubMed] [Google Scholar]
- 17.Institute for Government Coronavirus: local lockdowns. 2021. https://www.instituteforgovernment.org.uk/explainers/coronavirus-local-lockdowns
- 18.Rabe-Hesketh S, Skrondal A, Pickles A. GLLAMM Manual. Oct 25, 2004. https://econpapers.repec.org/paper/bepucbbio/1160.htm
- 19.Jones RH. Bayesian information criterion for longitudinal and clustered data. Stat Med. 2011;30:3050–3056. doi: 10.1002/sim.4323. [DOI] [PubMed] [Google Scholar]
- 20.Asparouhov T, Muthén B. Variable-specific entropy contribution. June 19, 2018. https://www.statmodel.com/download/UnivariateEntropy.pdf
- 21.Wang C, Brown CH, Bandeen-roche K, Ang CW, Rown CHB, Oche KBA. Residual diagnostics for growth mixture models: examining the impact of a preventive intervention on multiple trajectories of aggressive behavior. J Am Stat Assoc. 2012;471:1054–1076. [Google Scholar]
- 22.Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res. 2020 doi: 10.1016/j.jpsychires.2020.10.035. published online Oct 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Curtis S, Cunningham N, Pearce J, Congdon P, Cherrie M, Atkinson S. Trajectories in mental health and socio-spatial conditions in a time of economic recovery and austerity: a longitudinal study in England 2011–17. Soc Sci Med. 2021;270 doi: 10.1016/j.socscimed.2020.113654. [DOI] [PubMed] [Google Scholar]
- 24.Collischon M, Eberl A. Let's talk about fixed effects: let's talk about all the good things and the bad things. Kolner Z Soz Sozpsychol. 2020;72:289–299. [Google Scholar]
- 25.Gunasekara FI, Richardson K, Carter K, Blakely T. Fixed effects analysis of repeated measures data. Int J Epidemiol. 2014;43:264–269. doi: 10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–197. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 27.Carr MJ, Steeg S, Webb RT, et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021;6:e124–e135. doi: 10.1016/S2468-2667(20)30288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Graaf R, van Dorsselaer S, ten Have M, Schoemaker C, Vollebergh WAM. Seasonal variations in mental disorders in the general population of a country with a maritime climate: findings from the Netherlands mental health survey and incidence study. Am J Epidemiol. 2005;162:654–661. doi: 10.1093/aje/kwi264. [DOI] [PubMed] [Google Scholar]
- 29.Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. 2020 doi: 10.1017/S0033291720004432. published online Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Office for National Statistics Coronavirus and the social impacts on Great Britain. 15 January 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/15january2021
- 31.Romei V. UK at risk of double-dip recession as economy shrinks in November. Jan 15, 2021. https://www.ft.com/content/98d2c130-ac89-4eea-97a3-dc4636adc95d
- 32.Office for National Statistics The prevalence of long COVID symptoms and COVID-19 complications. Dec 16, 2020. https://www.ons.gov.uk/news/statementsandletters/theprevalenceoflongcovidsymptomsandcovid19complications
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The main cohort data are publicly available via UK Data Service repository (study numbers 6614 and 8644), and do not require ethical assessment for academic research purposes. The use of area-level information (SN 7248) is provided under a UK Data Service special license. Our statistical code is available on request to the corresponding author.