Abstract
Objectives
To analyse detailed trends in adult obesity from 2003 to 2018 in the USA, and provide the latest national estimates of adult obesity in 2017–2018.
Design, setting and participants
Analysis of data, including measured height and weight, obtained from 42 266 adults aged ≥20 years from the National Health and Nutrition Examination Survey, a cross-sectional, nationally representative sample of the US population.
Exposure
Survey period.
Primary outcome measures
The mean body mass index (BMI) and prevalence of overweight and obesity.
Results
In 2017–2018, the prevalence of overweight (including obesity, BMI ≥25 kg/m2) and obesity (BMI ≥30 kg/m2) was 73.8% (95% CI 71.1% to 76.4%) and 42.8% (95% CI 39.5% to 46.1%), respectively. From 2003 to 2018, a significant increase in the prevalence of overweight (including obesity, overall adjusted OR for 2017–2018 vs 2003–2004, 1.08 (95% CI 1.04 to 1.13) and obesity (overall adjusted OR for 2017–2018 vs 2003–2004, 1.15 (95% CI 1.10 to 1.21) was found among American adults. However, annual changes in mean BMI and the prevalence of overweight and obesity did not differ significantly before and after 2009–2010. The prevalence of overweight and obesity varied significantly by age, sex, race, education, daily total energy intake, economic conditions and physical activity status (all p<0.05).
Conclusions
Although the prevalence of adult obesity continues to rise, there have been no significant changes in the annual growth of adult obesity prevalence between 2003–2004 and 2017–2018. In 2017–2018, the prevalence of obesity was 42.8%, which equates to 76 million American adults at risk for serious and costly chronic conditions. The prevalence of obesity was higher among older adults (aged 60–69 years), females, non-Hispanic blacks, and those who did not graduate college, were physically inactive, reported lower daily total energy intake and had poor economic status.
Keywords: PUBLIC HEALTH, General endocrinology, EPIDEMIOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Our present study used a larger sample size as well as a longer time span than the previous studies.
Although National Health and Nutrition Examination Survey is designed to provide nationally representative estimates, it is a repeated cross-sectional survey, which precludes within-individual change in body mass index (BMI) or obesity.
Our study assessed annual changes in BMI and obesity, and the potential effects of the 2008–2009 global financial crisis among US adults.
Obesity was defined mainly based on measurements of BMI, which does not measure body fat directly.
Introduction
Obesity is one of the most common risk factors for chronic diseases such as diabetes mellitus, cardiovascular diseases, renal damage and cancers, which affected 670 million adults globally in 2016.1–7 In the USA, the obesity rate has been on the rise since the 1980s.8 By 2030, obesity is expected to reach a prevalence of 48.9% among American adults.9
Some studies have reported trends in obesity prevalence among American adults using data from National Health and Nutrition Examination Survey (NHANES).8 10–19 Between 1976–1980 and 1988–1994, the prevalence of obesity among American adults increased from 14.5% to 22.5%.10 The prevalence of obesity increased from 22.9% to 30.5% from 1988–1994 to 1999–2000, maintaining similar growth rates of approximately 8%.11 Over the period from 1999–2000 to 2017–2018, there was a larger increase in the prevalence of obesity among males (from 27.5% to 43.0%) than seen previously and a similar growth in the prevalence among females (from 33.4% to 41.9%).14 The majority of previous studies have focused on differences in the prevalence of obesity by age, sex and race. Differences in the prevalence of obesity by other covariates such as educational level, economic status, daily total energy intake and physical activity status have been scarcely studied. The effects of the 2008–2009 global financial crisis on economic status, physical activity status and daily total energy intake are still unknown. How changes in economic status, physical activity status and daily total energy intake may impact the prevalence of overweight and obesity is less well understood.
In this study, our primary aim was to provide the latest national estimates of adult obesity and evaluate trends in mean body mass index (BMI) and adult obesity from 2003 to 2018. The secondary aims of our study were as follows: (1) To explore the changes in mean BMI and adult obesity before and after 2009–2010 (ie, before and after the 2008–2009 global financial crisis taken place) and (2) To assess how these trends might vary by age, sex, race, educational level, economic status, daily total energy intake and physical activity status.
Materials and methods
Database and participants
The NHANES is a nationally representative sample of the US population, which collects data from survey participants through household interviews, standardised physical examinations and laboratory tests in mobile examination centres.20 The survey is unique in that it combines data from interviews and physical examinations. The NHANES released data every 2 years to ensure an adequate sample size for analyses and to protect confidentiality. The survey examines a nationally representative sample of approximately 5000 people each year. The NHANES interview includes demographic, socioeconomic, dietary and health-related questions. The examination component consists of medical, dental and physiological measurements, as well as laboratory tests administered by highly trained medical personnel. Detailed information on the NHANES procedures is available in the literature.21
The present study used NHANES data from adults aged ≥20 years (N=44 790) collected from eight survey cycles from 2003 to 2018. Among the 44 790 participants (21 668 males and 23 122 females), 42 266 had complete data on BMI and were included in the final analysis.
Data collection
Information about anthropometric measurements (including height and weight) and BMI was obtained from examination data. Information about age, sex, race, education and poverty income ratio (PIR) was obtained from demographic data. Data on total energy intake were obtained from the total nutrient intake file from the second-day dietary interview, which contains a summary of the individual’s nutrition from all foods and beverages provided on the dietary recall. Total energy intake was categorised into tertiles. PIR was a ratio of family income to the poverty threshold, which was calculated by dividing family income by the poverty guidelines for the year the survey was completed. PIR was categorised into two groups: <130% and ≥130%. This classification of PIR has been used in a previous study.22 Data on physical activity were obtained from the physical activity questionnaire. Based on the 2018 Physical Activity Guidelines for Americans, respondents who engaged in moderate-intensity aerobic activity for 150 min/week, vigorous-intensity aerobic activity for 75 min/week or an equivalent combination of both (1 min of vigorous-intensity physical activity is equivalent to 2 min of moderate-intensity physical activity) were defined as meeting the guidelines.23 In our analysis, physical activity was categorised into three levels: sufficiently active, insufficiently active and inactive. Sufficiently active was defined as moderate-intensity aerobic activity for 150 min/week, vigorous-intensity aerobic activity for 75 min/week or an equivalent combination of both. Insufficiently active was defined as some aerobic activity for 10–149 min/week, but not enough to meet the guidelines. Inactive was defined as some physical activity (<10 min/week) or no reported physical activity.23 This classification of physical activity has been used in previous studies.24
Statistical analysis
According to the WHO classification, we defined overweight, including obesity, as BMI ≥25 kg/m2 and obesity as ≥30 kg/m2. Overall, the mean BMI and prevalence of overweight and obesity in each survey cycle were calculated by incorporating sample weights and adjusting for clusters and strata of the complex sample design of the NHANES. Individuals with missing demographic information on height or weight measurements were excluded from the analyses.
In table 1, continuous variables are presented as weighted means and SEs, while categorical variables are presented as unweighted counts and weighted proportions. Comparisons between survey cycles were made using the Wald test (categorical variables) or Kruskal-Wallis rank-sum test (skewed distribution).
Table 1.
Baseline characteristics of participants*
| Characteristics | National Health and Nutrition Examination Survey cycles† | ||||||||
| Total (n=42 266) |
2003/2004 (n=4647) |
2005/2006 (n=4680) |
2007/2008 (n=5607) |
2009/2010 (n=5994) |
2011/2012 (n=5237) |
2013/2014 (n=5520) |
2015/2016 (n=5406) |
2017/2018 (n=5175) |
|
| Age, years | 47.11±0.20 | 46.02±0.52 | 46.42±0.74 | 46.55±0.44 | 46.92±0.49 | 47.21±0.82 | 47.45±0.38 | 47.92±0.58 | 48.14±0.53 |
| Age, years (group) | |||||||||
| 20–30 | 8033 (20.5) | 940 (21.0) | 1101 (20.5) | 928 (20.5) | 1134 (21.1) | 1043 (20.6) | 1025 (20.6) | 1016 (20.2) | 846 (19.7) |
| 30–39 | 7175 (18.4) | 759 (20.3) | 823 (19.8) | 997 (19.1) | 1010 (18.1) | 916 (17.5) | 951 (17.4) | 921 (17.4) | 798 (19.0) |
| 40–49 | 7035 (19.4) | 742 (21.6) | 782 (21.2) | 920 (21.2) | 1063 (19.8) | 869 (19.4) | 991 (18.9) | 896 (17.7) | 772 (16.3) |
| 50–59 | 6714 (18.1) | 596 (16.6) | 622 (16.9) | 902 (17.8) | 956 (18.2) | 877 (18.9) | 914 (18.1) | 917 (18.8) | 930 (19.3) |
| 60–69 | 6629 (12.8) | 695 (10.2) | 631 (11.0) | 894 (11.0) | 876 (12.0) | 820 (13.5) | 866 (14.1) | 863 (14.5) | 984 (15.1) |
| ≥70 | 6680 (10.8) | 915 (10.5) | 721 (10.3) | 966 (10.5) | 955 (10.8) | 712 (10.1) | 773 (11.0) | 793 (11.4) | 845 (11.6) |
| Sex, n (%) | |||||||||
| Male, n (%) | 20 408 (48.0) | 2237 (48.1) | 2237 (48.2) | 2746 (48.0) | 2889 (48.1) | 2585 (48.1) | 2638 (48.0) | 2638 (47.6) | 2493 (47.7) |
| Female, n (%) | 21 858 (52.0) | 2410 (51.9) | 2443 (51.8) | 2.861 (52.0) | 3105 (51.9) | 4652 (51.9) | 2882 (52.0) | 2882 (52.4) | 2682 (52.3) |
| Race | |||||||||
| Mexican American | 6805 (8.4) | 931 (8.0) | 944 (8.0) | 967 (8.3) | 1096 (8.6) | 509 (7.7) | 737 (9.1) | 936 (8.8) | 685 (8.7) |
| Other Hispanic | 3755 (5.3) | 139 (3.5) | 148 (3.4) | 629 (4.9) | 610 (5.0) | 538 (6.5) | 488 (5.6) | 720 (6.4) | 483 (6.9) |
| Non-Hispanic white | 18 120 (67.4) | 2464 (72.0) | 2338 (71.9) | 2625 (69.6) | 2865 (67.9) | 1917 (66.5) | 2366 (65.9) | 1767 (64.0) | 1778 (62.4) |
| Non-Hispanic black | 9094 (11.4) | 910 (11.2) | 1064 (11.4) | 1155 (11.2) | 1087 (11.4) | 1382 (11.5) | 1135 (11.5) | 1142 (11.4) | 1219 (11.5) |
| Other race | 4492 (7.5) | 203 (5.4) | 186 (5.2) | 231 (6.1) | 336 (7.2) | 891 (7.7) | 794 (7.9) | 841 (9.4) | 1010 (10.5) |
| Education, n (%) | |||||||||
| Less than high school | 10 814 (16.4) | 1362 (18.1) | 1290 (17.4) | 1728 (20.3) | 1710 (18.9) | 1235 (16.4) | 1191 (15.2) | 1277 (14.3) | 1021 (11.0) |
| High school graduate | 9787 (23.6) | 1167 (27.1) | 1119 (25.0) | 1392 (25.4) | 1376 (22.9) | 1098 (19.8) | 1232 (21.6) | 1172 (20.8) | 1231 (27.0) |
| Some college or AA degree | 12 266 (31.4) | 1263 (31.5) | 1334 (31.3) | 1440 (29.0) | 1679 (30.3) | 1576 (32.4) | 1704 (32.9) | 1602 (32.5) | 1668 (30.8) |
| College graduate or above | 9345 (28.6) | 847 (23.2) | 931 (26.1) | 1041 (25.3) | 1216 (27.7) | 1324 (31.3) | 1389 (30.3) | 1352 (32.4) | 1245 (31.1) |
| Poverty income ratio, n (%) | |||||||||
| <130% | 12 129 (21.3) | 1264 (20.5) | 1167 (17.1) | 1552 (20.4) | 1817 (21.7) | 1724 (24.6) | 1762 (24.7) | 1568 (20.9) | 1275 (20.1) |
| ≥130% | 26 450 (78.7) | 3119 (79.5) | 3294 (82.9) | 3536 (79.6) | 3592 (78.3) | 3078 (75.4) | 3335 (75.3) | 3280 (79.1) | 3216 (79.9) |
| BMI, kg/m2 | 28.93±0.07 | 28.24±0.15 | 28.57±0.23 | 28.54±0.16 | 28.75±0.13 | 28.73±0.21 | 29.17±0.17 | 29.42±0.25 | 29.86±0.26 |
| BMI, kg/m2 (group) | |||||||||
| <25 | 12 522 (30.7) | 1480 (33.7) | 1432 (32.9) | 1628 (32.0) | 1684 (30.9) | 1714 (31.7) | 1700 (30.0) | 1517 (28.7) | 1367 (26.9) |
| 25–30 | 14 046 (32.9) | 1632 (34.1) | 1608 (32.9) | 1934 (34.3) | 2030 (33.4) | 1677 (33.8) | 1767 (32.6) | 1731 (31.9) | 1667 (30.8) |
| ≥30 | 15 698 (36.4) | 1535 (32.2) | 1640 (34.2) | 2045 (33.7) | 2280 (35.8) | 1846 (34.6) | 2053 (37.4) | 2158 (39.4) | 2141 (42.3) |
| Total energy intake, kcal/d | 2027.31±7.96 | 2113.90±13.81 | 2051.01±25.07 | 2016.62±20.87 | 2061.43±27.10 | 2014.61±18.59 | 2017.22±23.24 | 1970.20±23.28 | 1980.34±23.18 |
| Physical activity, n (%) | |||||||||
| Inactive | 8504 (18.1) | 150 (5.6) | 142 (4.4) | 1656 (23.1) | 1711 (23.7) | 355 (6.8) | 1562 (26.3) | 1565 (23.0) | 1363 (21.2) |
| Insufficiently active | 6649 (17.5) | 1380 (50.2) | 1403 (47.5) | 734 (13.0) | 817 (13.7) | 536 (10.3) | 568 (9.7) | 567 (9.9) | 644 (11.3) |
| Sufficiently active | 23 320 (64.4) | 1156 (44.2) | 1303 (48.2) | 3217 (63.8) | 3466 (62.7) | 4346 (82.9) | 3390 (64.0) | 3274 (67.1) | 3168 (67.5) |
*Data are presented incorporating sample weights and adjusted for clusters and strata of the complex sample design of the National Health and Nutrition Examination Survey (2003–2018).
†Values are presented as mean±SE for continuous variables and unweighted numbers (weighted %) for categorical variables.
AA, associate of arts; BMI, body mass index.
We used survey-weighted generalised linear regression models to evaluate the trends in BMI and the prevalence of overweight and obesity by survey period. Multivariate survey-weighted generalised linear regression models were adjusted for age, sex, race, education, PIR, total energy intake and physical activity status. A p value for the trends was obtained by entering the median value of each category of BMI, the prevalence of overweight and obesity as a continuous variable and rerunning the corresponding survey-weighted generalised linear regression models.
We used a previously described method to compare trends in mean BMI and prevalence of overweight and obesity before and after 2009–2010 to explore the potential impact of the 2008–2009 global financial crisis.25 We calculated annual mean BMI changes as the absolute value of the difference in mean BMI between the start and end years divided by the total number of years covered. We also calculated the annual relative changes in overweight and obesity prevalence as the absolute value of the difference in prevalence between the start and end years divided by the prevalence in the start year annualised by accounting for compounding. Welch’s t-tests were used to compare trends in mean BMI and prevalence of overweight and obesity before and after 2009–2010.
All simulations and analyses were performed using R software (R Foundation for Statistical Computing, Vienna, Austria, V.3.6.3) and the ‘survey’ package (eg, svymean and svyglm), which considers sampling weights (16-year exam weight), clustering and stratification of the complex survey design.26 A two-sided p<0.05 was considered to be statistically significant.
Patient and public involvement
The public was not involved in the design, conduct, reporting, or dissemination plans of our study.
Results
The demographic characteristics of all participants according to the eight survey cycles are listed in table 1. In total, 42 266 participants (20 408 males and 21 858 females) were included in our final analysis. The weighted mean (SE) age of the population was 47.11 (0.20) years, 47.97% of the population were male and the weighted mean (SE) BMI was 28.93 (0.07) kg/m2. Approximately two-thirds (67.36%) were non-Hispanic white, 11.41% were non-Hispanic black, 8.38% were Mexican American, 5.33% were Hispanic and 7.51% were categorised as ‘other race’. More than 80% had a minimum of a high school education and approximately 80% reported good economic status (PIR ≥130%). The average (SE) daily total energy intake was 2027.31 (7.96) kcal. Approximately 65% reported meeting physical activity guidelines. The prevalence of overweight and obesity increased over time, whereas the inverse was true for normal weight (p=0.002). The prevalence of overweight and obesity varied significantly by age, sex, race, education, daily total energy intake, economic conditions and physical activity status (online supplemental table S1).
bmjopen-2022-065425supp001.pdf (748.5KB, pdf)
The mean (SE) BMI levels increased from 28.24 (0.07) kg/m2 in 2003–2004 to 29.86 (0.26) kg/m2 in 2017–2018 (online supplemental table S2). In 2017–2018, the obesity prevalence was 42.8% (95% CI 39.5% to 46.1%), increasing more than 10% from 32.3% in 2003–2004 (95% CI 29.9% to 34.6%) (online supplemental table S3). Consistent with the increase in mean BMI and obesity prevalence, we found that the prevalence of overweight (including obesity) increased from 66.3% (95% CI 64.4% to 68.3%) in 2003–2004 to 73.8% (95% CI 71.1% to 76.4%) in 2017–2018 (online supplemental table S4). We used survey-weighted generalised linear regression models to evaluate the trends in BMI and prevalence of overweight and obesity by survey period (table 2). Compared with 2003–2004, the mean (SE) BMI increased by 1.96 kg/m2 (95% CI 1.34 to 2.57, p<0.001) in 2017–2018 after adjusting for age, sex, race, education, PIR and physical activity status (table 2, online supplemental table S5). The findings were similar for the prevalence of overweight and obesity. Compared with 2003–2004, the adjusted ORs for the prevalence of overweight (including obesity) and obesity were 1.08 (95% CI 1.04 to 1.13, p<0.001) and 1.15 (95% CI 1.10 to 1.21, p<0.001), respectively (table 2, online supplemental table S6, S7). However, we found no significant effect of the survey cycle on the prevalence of overweight among males after adjusting for potential confounding variables (adjusted OR 1.05, 95% CI 1.00 to 1.11, p=0.050) (online supplemental table S7).
Table 2.
Change in BMI, overweight and obesity over time among adults in the USA, 2003–2018
| Years | Mean BMI | Prevalence of overweight | Prevalence of obesity | |||
| Adjusted β* (95% CI) | P value | Adjusted OR* (95% CI) | P value | Adjusted OR* (95% CI) | P value | |
| 2003–2004 | Reference | Reference | Reference | |||
| 2005–2006 | 0.38 (−0.23 to 0.99) | 0.215 | 1.01 (0.97 to 1.05) | 0.598 | 1.03 (0.99 to 1.07) | 0.184 |
| 2007–2008 | 0.48 (0.04 to 0.93) | 0.035 | 1.02 (0.98 to 1.05) | 0.281 | 1.03 (1.00 to 1.06) | 0.084 |
| 2009–2010 | 0.70 (0.26 to 1.15) | 0.002 | 1.03 (0.99 to 1.07) | 0.178 | 1.06 (1.03 to 1.09) | <0.001 |
| 2011–2012 | 1.08 (0.55 to 1.61) | <0.001 | 1.05 (1.00 to 1.09) | 0.034 | 1.07 (1.03 to 1.11) | <0.001 |
| 2013–2014 | 1.18 (0.66 to 1.70) | <0.001 | 1.05 (1.01 to 1.08) | 0.012 | 1.08 (1.04 to 1.11) | <0.001 |
| 2015–2016 | 1.59 (1.03 to 2.20) | <0.001 | 1.06 (1.02 to 1.10) | 0.005 | 1.11 (1.07 to 1.16) | <0.001 |
| 2017–2018 | 1.96 (1.34 to 2.57) | <0.001 | 1.08 (1.04 to 1.13) | <0.001 | 1.15 (1.10 to 1.21) | <0.001 |
| P for trend | <0.001 | <0.001 | <0.001 | |||
*Models adjusted for age, sex, race, education, family poverty income ratio, daily total energy intake and physical activity status.
BMI, body mass index.;
Table 3 shows the annual change in mean BMI as well as overweight and obesity prevalence from 2003–2004 to 2009–2010 and from 2011–2012 to 2017–2018. The increase in mean BMI was somewhat larger after 2009–2010 (0.12 kg/m2 annual relative increase, 95% CI 0.06 to 0.19) than before 2009–2010 (0.07 kg/m2 annual relative increase, 95% CI 0.02 to 0.13). However, this difference was not statistically significant (p=0.848). Annual changes in the prevalence of overweight and obesity were similar. The acceleration in the rise of obesity prevalence was mainly due to an increase in the prevalence of obesity among those who were in a better economic status (0.40% annual relative increase, 95% CI −1.11% to 1.93% vs 2.97% annual relative increase, 95% CI 1.75% to 4.20%). Again, this difference was not significantly different (p=0.985). Likewise, for the prevalence of overweight (including obesity), the annual increase was numerically faster after 2009–2010 than before 2009–2010 (0.6%, 95% CI −0.08% to 1.27% vs 0.72%, 95% CI 0.15% to 1.29%; p=0·584). Remarkably, the prevalence of overweight (including obesity) was nearly unchanged among those with poor economic conditions after 2009–2010 (0.00% annual relative increase, 95% CI −0.96% to 0.97%) compared with before 2009–2010 (1.82% annual relative increase, 95% CI 0.55% to 3.10%, p=0.037). Meanwhile, both males and females with poor economic conditions had a slower increase in BMI and the prevalence of overweight and obesity after 2009–2010 compared with before 2009–2010. In contrast, a larger increase was found among those with good economic conditions after 2009–2010, although without statistical significance (p>0.05).
Table 3.
Annual change in BMI, overweight, obesity and economic status during 2003–2010 and 2011–2018
| Characteristic | Male | Female | Both | ||||||
| 2003/2004–2009/2010 | 2011/2012–2017/2018 | P value | 2003/2004–2009/2010 | 2011/2012–2017/2018 | P value | 2003/2004–2009/2010 | 2011/2012–2017/2018 | P value | |
| Change (95% CI) in mean BMI (kg/m2) | |||||||||
| Overall | 0.07 (0.02 to 0.13) | 0.12 (0.06 to 0.19) | 0.848 | 0.65 (−0.01 to 0.14) | 0.13 (−0.39 to 2.76) | 0.846 | 0.07 (0.02 to 0.13) | 0.12 (0.06 to 0.19) | 0.848 |
| PIR <130% | 0.17 (0.02 to 0.32) | 0.08 (−0.06 to 0.22) | 0.245 | 0.17 (0.04 to 0.30) | 0.06 (−0.09 to 0.21) | 0.186 | 0.17 (0.05 to 0.28) | 0.07 (−0.04 to 0.18) | 0.170 |
| PIR ≥130% | 0.07 (−0.01 to 0.14) | 0.11 (0.04 to 0.17) | 0.716 | 0.15 (−0.04 to 0.13) | 0.16 (0.07 to 0.25) | 0.943 | 0.06 (0.00 to 0.11) | 0.13 (0.07 to 0.20) | 0.922 |
| Percentage change (95% CI) in overweight prevalence | |||||||||
| Overall | 0.69 (−0.18 to 1.56) | 0.50 (−0.24 to 1.24) | 0.393 | 0.50 (−0.45 to 1.47) | 0.95 (0.30 to 1.60) | 0.746 | 0.60 (−0.08 to 1.27) | 0.72 (0.15 to 1.29) | 0.584 |
| PIR <130% | 2.64 (−0.52 to 4.82) | −0.06 (−1.60 to 1.50) | 0.050 | 1.33 (0.10 to 2.56) | 0.03 (−0.97 to 1.04) | 0.096 | 1.82 (0.55 to 3.10) | 0.00 (−0.96 to 0.97) | 0.037 |
| PIR ≥130% | 0.36 (−0.59 to 1.31) | 0.64 (−0.03 to 1.33) | 0.646 | 0.28 (−0.81 to 1.40) | 1.31 (0.55 to 2.08) | 0.900 | 0.30 (−0.50 to 1.10) | 0.95 (0.34 to 1.56) | 0.844 |
| Percentage change (95% CI) in obesity prevalence | |||||||||
| Overall | 1.93 (0.10 to 3.76) | 2.29 (0.54 to 4.02) | 0.589 | 1.15 (−0.39 to 2.76) | 1.71 (0.56 to 2.84) | 0.699 | 1.51 (0.24 to 2.81) | 1.99 (0.93 to 3.04) | 0.689 |
| PIR <130% | 3.16 (0.12 to 6.19) | 2.38 (−0.48 to 5.25) | 0.378 | 2.38 (0.34 to 4.46) | 0.95 (−0.77 to 2.67) | 0.192 | 2.56 (0.81 to 4.31) | 1.47 (0.00 to 2.95) | 0.223 |
| PIR ≥130% | 1.93 (−0.03 to 3.85) | 2.08 (−0.38 to 3.77) | 0.536 | 0.97 (−1.00 to 3.00) | 2.21 (0.62 to 3.78) | 0.796 | 0.40 (−1.11 to 1.93) | 2.97 (1.75 to 4.20) | 0.985 |
P value for difference in annual changes for 2004–2010 vs 2011–2018.
BMI, body mass index; PIR, poverty income ratio.
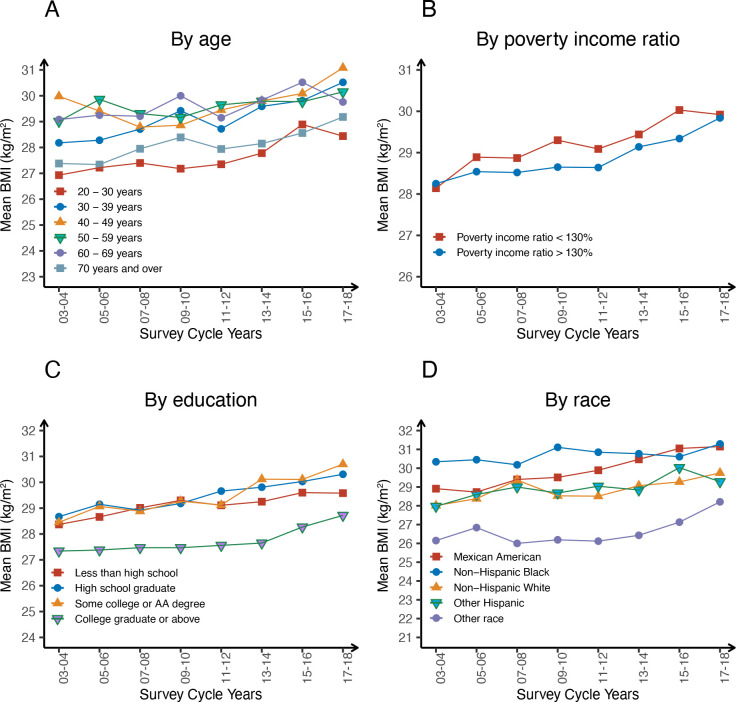
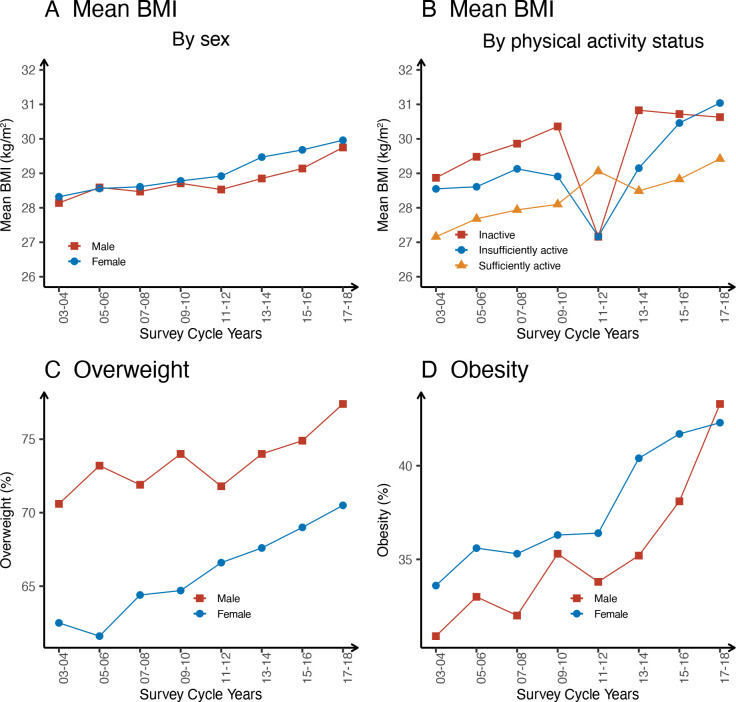
Graphical representations of the changes in the distribution of mean BMI and overweight and obesity prevalence are shown in figures 1 and 2. Figure 1 shows the changes in mean BMI across years stratified by age, PIR, education and race. Similar trends in mean BMI were found across subgroups of age, PIR, education, race, sex and physical activity status. Overall, the mean BMI generally increased over time among all participants. In the age subgroup, the lowest mean BMI was found in those aged 20–30 years, followed by those aged >70 years (online supplemental table S2, figure 1). Compared with good economic conditions, BMI was higher for those with poor economic conditions since 2005–2006. In 2017–2018, participants with poor economic conditions had a mean BMI 1.68 kg/m2 lower than those with good economic conditions. Between 2003–2004 and 2017–2018, a lower mean BMI was found among participants with a higher educational level than among those with a lower educational level. A similar trend was found in the subgroup stratified by race. In 2017–2018, the mean (SE) BMI for all participants was 29.86±0.26 kg/m2, with the highest mean BMI in non-Hispanic blacks (31.29±0.29 kg/m2) and the lowest BMI in other racial populations (28.21±0.39 kg/m2) (table 1, figure 1). Figure 2 shows the changes in mean BMI across years stratified by sex and activity status. Changes in overweight and obesity prevalence across years stratified by sex are also shown in figure 2. From 2003–2004 to 2017–2018, the mean BMI increased similarly in both sexes, by approximately 1.61 kg/m2 for males and 1.64 kg/m2 for females (online supplemental table S2, figure 2). Meanwhile, males had a lower BMI than females. In the physical activity status subgroup, there was a more complex pattern, with a decrease in mean BMI in 2011–2012 among those who were inactive and insufficiently active. Although there was an acceleration in the increase of mean BMI among those who were sufficiently active, their mean BMI was the lowest.
Figure 1.
Mean BMI by age (A), poverty income ratio (B), education (C) and race (D) group from 2003 through 2018.
Figure 2.
Mean BMI by sex (A), physical activity status (B)group and prevalence of overweight (C) and obesity (D) from 2003 through 2018.
The trends in increasing obesity prevalence over time were largely consistent for males and females. In 2003–2004, males had a lower mean BMI and a lower prevalence of obesity than females, but the opposite pattern was seen in 2017–2018. In 2017–2018, males had a higher prevalence of obesity than females (43.3%, 95% CI 38.2% to 48.4% vs 42.3%, 95% CI 38.6% to 46.0%) (online supplemental table S3, figure 2).
The trends in increasing overweight prevalence over time were similar for both sexes. Overall, the overweight prevalence in males was higher than that in females. Between 2003–2004 and 2017–2018, the overweight (including obesity) increased similarly in both sexes, by approximately 1.61 kg/m2 for males and 1.64 kg/m2 for females. For overweight (including obesity) prevalence trends, there was an increasing prevalence among males from 70.6% (95% CI 68.0% to 73.0%) in 2003–2004 to 77.4% (95% CI 73.9% to 80.9%) in 2017–2018, and among females from 62.5% (95% CI 59.9% to 65.9%) to 70.5% (95% CI 67.3% to 73.6%) (online supplemental table S4, figure 2).
Discussion
Our present study showed that the prevalence of obesity among American adults increased from 32.3% in 2003–2004 to 42.8% in 2017–2018. These results are broadly consistent with the results reported by the NCHS. In 2017–2018, the prevalence of obesity was 42.3% among males and 43.3% among females. Compared with 2003–2004, the mean BMI increased by 1.94 kg/m2, obesity prevalence increased by 15% and overweight prevalence increased by 8% in 2017–2018 after adjusting for age, sex, race, education, PIR and physical activity status. The increases in mean BMI and the prevalence of both overweight and obesity were somewhat larger after 2009–2010 than before 2009–2010. However, the difference was not statistically significant.
The levels and changes in trends of mean BMI and obesity prevalence among American adults have been covered by numerous studies.9 15 27–29 The NCHS reported that the age-adjusted obesity prevalence among adults was 42.4% in 2017–2018, and obesity prevalence increased among adults from 1999–2000 to 2017–2018.15 Another study using data from the 2005–2014 NHANES also showed that a statistically significant positive linear trend in obesity prevalence was present in females but not in males.28 One recent study suggested that the prevalence of obesity among US adults increased from 35.4% in 2011–2012 to 43.4% in 2017–2018. From 2011–2012 to 2017–2018, the mean BMI increased from 28.7 kg/m2 to 29.8 kg/m2.29 Our results were broadly consistent with the results of the above studies at each time point. However, our present study used a larger sample size as well as a longer time span than the above studies.
To the best of our knowledge, few studies have assessed annual changes in BMI and obesity prevalence and the potential effects of the 2008–2009 global financial crisis among US adults. A previous study conducted using NHANES data from 1999 to 2008 showed that the increases in the prevalence of obesity do not appear to be continuing at the same rate from 1999–2000 to 2007–2008. When they adjusted for age and race with survey period as a categorical variable, there were no significant differences in the prevalence of obesity between 2003–2004 and 2007–2008 for males.27 This is broadly consistent with our findings. In our study, statistically significant differences in mean BMI and obesity prevalence for both sexes were found since 2009–2010 (table 2). Furthermore, a previous study evaluated the effects of the economic crisis on dietary quality and obesity rates.30 They found that economic changes can modify diet quality and increase the risk of having a poor diet or being obese, which was mainly due to the changes in economic and work conditions. In our study, the impact of economic conditions on BMI was complex. A significant increase in mean BMI was found among both the poor and the rich. The overall BMI was higher for those with poor economic conditions since 2005–2006 than for those with good economic conditions (figure 1). However, the acceleration in the increase of obesity prevalence was mainly due to an increase in the prevalence of obesity among those who are in a better economic status (table 3). Interestingly, there was no significant difference in the annual change in obesity prevalence before and after the financial crisis. This may be mainly due to the increase in the proportion of the poor after the financial crisis. The proportion of the poor increased from 21.68% in 2009–2010 to 24.6% in 2011–2012. This trend continued until 2015. In our present study, although the differences were not statistically significant, numerical larger increases in mean BMI and the prevalence of both overweight and obesity were found after 2009–2010 than before 2009–2010.
Interestingly, participants in the highest daily total energy intake tertile had the lowest BMIs compared with those in the lowest daily total energy intake tertile (28.97 kg/m2 vs 29.30 kg/m2). The findings were similar for the prevalence of obesity (36.7% vs 39.9%) and overweight (69.8% vs 70.9%). Thus, we analysed the characteristics of the participants according to tertiles of daily total energy intake (online supplemental table S8). Compared with those in the lowest daily total energy intake tertile, participants in the highest daily total energy intake tertile had higher proportions of non-Hispanic whites and individuals who were college educated (college degree or higher), sufficiently physically active and had good economic status. This might in part be related to the lower BMI and prevalence of obesity.
In addition, although the mean BMI and the prevalence of overweight and obesity increased over time, the mean daily total energy intake decreased from 2003–2004 to 2017–2018 (2113.90±7.96 kcal/day vs 1980.34±7.96 kcal/day, p<0.001). Several mechanisms may explain this phenomenon: (1) The reduction in energy intake may lead to hunger increases and energy expenditure declines, leading to physiological adaptations that tend to push body weight back up31; and (2) In the USA, carbohydrate intake has increased markedly, resulting in major increases in the proportion of calories from carbohydrates.32 A high-carbohydrate diet could produce postprandial hyperinsulinaemia, which promotes energy storage and causes an increase in body weight.33
In our study, a lower mean BMI was found among participants with a higher educational level than among those with a lower educational level. A previous study showed that a higher educational level is related to a lower BMI level among middle-aged females, mainly on account of selection.34 Theories of selection note that low-BMI children tend to have higher grades and test scores, and better chances of completing secondary and tertiary education. It has also been reported that young overweight or obese females are more likely to have a lower educational level.34 This might be explained by the following reasons: (1) Children with a lower BMI tend to come from socioeconomically advantaged families, and have better chances of completing their studies34; (2) Children with a lower BMI may benefit from physical activity, which may have a positive influence on academic performance35; and (3) Negative views on high-BMI children may impair their academic performance.36 Our results also show that females had a higher prevalence of obesity than males. This may be due to oestrogen-reducing postprandial fatty acid oxidation, leading to an increase in body fat among females.37 Meanwhile, it was less likely for females to be physically active than for males.
In our study, approximately 67.4% of participants reported meeting physical activity guidelines in 2017–2018. As reported by the NCHS, 53.3% of adults aged ≥18 years met the 2018 Physical Activity Guidelines for Americans for aerobic physical activity. However, the NCHS estimates were limited to leisure-time physical activity only. Our estimates were based on the Global Physical Activity Questionnaire, including both daily activities (work activities) and leisure time activities. For this reason, our estimates were larger than those reported by NCHS reports.
Although NHANES is designed to provide nationally representative estimates, it is a repeated cross-sectional survey, which precludes within-individual change in BMI or obesity. Meanwhile, obesity was defined mainly based on measurements of BMI, which does not measure body fat directly. Although BMI is highly correlated with overall body fat,38 the relationship between BMI and body fat varies by sex, age and race-ethnicity.39 In addition, the study used a large nationally representative sample of adults from the USA. Thus, our results are only generalisable to the US population. Therefore, there are certain limitations in the extrapolation of the study results.
The COVID-19 global pandemic has changed the lifestyle of most Americans. It has been reported that approaches designed to contain the spread of COVID-19, such as lockdowns, might exacerbate the prevalence of obesity.40 The effects of the COVID-19 global pandemic on BMI and the prevalence of obesity have yet to be examined. Regrettably, information about anthropometric measurements in NHANES after 2018 has not been released. Additional follow-up studies are required to answer these questions.
Conclusions
Although the prevalence of adult obesity continues to rise, there have been no significant changes in the annual growth of adult obesity prevalence between 2003–2004 and 2017–2018. In 2017–2018, the prevalence of obesity was 42.8%, which equates to 76 million Americans at risk for serious and costly chronic conditions. The prevalence of obesity was higher among older adults (aged 60–69 years), females, non-Hispanic blacks and participants who did not graduate college, were physically inactive, reported lower daily total energy intake and had poor economic status.
Supplementary Material
Footnotes
Contributors: WG and ZL: designed the research; ZL and ML: analysed the data; ZL: wrote the paper; ZL: had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; WG, ZL, ML and SW: assisted with interpretation of the results and critically reviewed the manuscript; and all authors: read and approved the final manuscript. ZL is the guarantor. The authors report no conflicts of interest.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Data described in the article are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Approval was obtained from the National Center for Health Statistics Research Ethics Review Board, and all participants provided written informed consent (Approval number: Protocol#98-12, #2005-06, #11-17, #18-01, https://www.cdc.gov/nchs/nhanes/irba98.htm). Participants gave informed consent to participate in the study before taking part.
References
- 1.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American heart association scientific statement on obesity and heart disease from the obesity Committee of the Council on nutrition, physical activity, and metabolism. Circulation 2006;113:898–918. 10.1161/CIRCULATIONAHA.106.171016 [DOI] [PubMed] [Google Scholar]
- 2.Petrelli F, Cortellini A, Indini A, et al. Association of obesity with survival outcomes in patients with cancer: a systematic review and meta-analysis. JAMA Netw Open 2021;4:e213520. 10.1001/jamanetworkopen.2021.3520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Islami F, Goding Sauer A, Gapstur SM, et al. Proportion of cancer cases attributable to excess body weight by US state, 2011-2015. JAMA Oncol 2019;5:384–92. 10.1001/jamaoncol.2018.5639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piché M-E, Tchernof A, Després J-P. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res 2020;126:1477–500. 10.1161/CIRCRESAHA.120.316101 [DOI] [PubMed] [Google Scholar]
- 5.Emerging Risk Factors Collaboration, Wormser D, Kaptoge S, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet 2011;377:1085–95. 10.1016/S0140-6736(11)60105-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut 2013;62:933–47. 10.1136/gutjnl-2013-304701 [DOI] [PubMed] [Google Scholar]
- 7.NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–42. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hales CM, Fryar CD, Carroll MD, et al. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA 2018;319:1723–5. 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. State-Level prevalence of adult obesity and severe obesity. N Engl J Med 2019;381:2440–50. 10.1056/NEJMsa1909301 [DOI] [PubMed] [Google Scholar]
- 10.Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998;22:39–47. 10.1038/sj.ijo.0800541 [DOI] [PubMed] [Google Scholar]
- 11.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999-2000. JAMA 2002;288:1723–7. 10.1001/jama.288.14.1723 [DOI] [PubMed] [Google Scholar]
- 12.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7. 10.1001/jama.2012.39 [DOI] [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14. 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic Origin-1999-2000 to 2017-2018. JAMA 2020;324:1208–10. 10.1001/jama.2020.14590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hales CM, Carroll MD, Fryar CD. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief 2020:1–8. [PubMed] [Google Scholar]
- 16.Ellison-Barnes A, Johnson S, Gudzune K. Trends in obesity prevalence among adults aged 18 through 25 years, 1976-2018. JAMA 2021;326:2073–4. 10.1001/jama.2021.16685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baskin ML, Ard J, Franklin F, et al. Prevalence of obesity in the United States. Obes Rev 2005;6:5–7. 10.1111/j.1467-789X.2005.00165.x [DOI] [PubMed] [Google Scholar]
- 18.Ogden CL, Carroll MD, Kit BK. NCHS Data Brief. In: Prevalence of obesity in the United States, 2009-2010, 2012: 1–8. [PubMed] [Google Scholar]
- 19.Kwak YE, McMillan R, McDonald EK. Trends in overweight and obesity Self-awareness among adults with overweight or obesity in the United States, 1999 to 2016. Ann Intern Med 2021;174:721–3. 10.7326/M20-3882 [DOI] [PubMed] [Google Scholar]
- 20.Zipf G, Chiappa M, Porter KS, et al. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1 2013;1:1–37. [PubMed] [Google Scholar]
- 21.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: Analytic guidelines, 1999-2010. Vital Health Stat 2 2013;2:1–24. [PubMed] [Google Scholar]
- 22.Fadeyev K, Nagao-Sato S, Reicks M. Nutrient and food group intakes among U.S. children (2-5 years) differ by family income to poverty ratio, NHANES 2011-2018. Int J Environ Res Public Health 2021;18. doi: 10.3390/ijerph182211938. [Epub ahead of print: 13 Nov 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020–8. 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim D, Konyn P, Cholankeril G, et al. Physical activity is associated with nonalcoholic fatty liver disease and significant fibrosis measured by FibroScan. Clin Gastroenterol Hepatol 2022;20:e1438–55. 10.1016/j.cgh.2021.06.029 [DOI] [PubMed] [Google Scholar]
- 25.Wang L, Zhou B, Zhao Z, et al. Body-Mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet 2021;398:53–63. 10.1016/S0140-6736(21)00798-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Curtin LR, Mohadjer LK, Dohrmann SM, et al. The National health and nutrition examination survey: sample design, 1999-2006. Vital Health Stat 2 2012;2:1–39. [PubMed] [Google Scholar]
- 27.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–41. 10.1001/jama.2009.2014 [DOI] [PubMed] [Google Scholar]
- 28.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–91. 10.1001/jama.2016.6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu B, Du Y, Wu Y, et al. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ 2021;372:n365. 10.1136/bmj.n365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norte A, Sospedra I, Ortíz-Moncada R. Influence of economic crisis on dietary quality and obesity rates. Int J Food Sci Nutr 2019;70:232–9. 10.1080/09637486.2018.1492523 [DOI] [PubMed] [Google Scholar]
- 31.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995;332:621–8. 10.1056/NEJM199503093321001 [DOI] [PubMed] [Google Scholar]
- 32.Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr 2013;97:848–53. 10.3945/ajcn.112.052662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludwig DS, Ebbeling CB. The Carbohydrate-Insulin Model of Obesity: Beyond "Calories In, Calories Out". JAMA Intern Med 2018;178:1098–103. 10.1001/jamainternmed.2018.2933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benson R, von Hippel PT, Lynch JL. Does more education cause lower BMI, or do lower-BMI individuals become more educated? Evidence from the National longitudinal survey of youth 1979. Soc Sci Med 2018;211:370–7. 10.1016/j.socscimed.2017.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castelli DM, Hillman CH, Buck SM, et al. Physical fitness and academic achievement in third- and fifth-grade students. J Sport Exerc Psychol 2007;29:239–52. 10.1123/jsep.29.2.239 [DOI] [PubMed] [Google Scholar]
- 36.Crosnoe R. Gender, obesity, and education. Sociol Educ 2007;80:241–60. 10.1177/003804070708000303 [DOI] [Google Scholar]
- 37.O'Sullivan AJ. Does oestrogen allow women to store fat more efficiently? a biological advantage for fertility and gestation. Obes Rev 2009;10:168–77. 10.1111/j.1467-789X.2008.00539.x [DOI] [PubMed] [Google Scholar]
- 38.Flegal KM, Shepherd JA, Looker AC, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr 2009;89:500–8. 10.3945/ajcn.2008.26847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gallagher D, Visser M, Sepúlveda D, et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996;143:228–39. 10.1093/oxfordjournals.aje.a008733 [DOI] [PubMed] [Google Scholar]
- 40.Clemmensen C, Petersen MB, Sørensen TIA. Will the COVID-19 pandemic worsen the obesity epidemic? Nat Rev Endocrinol 2020;16:469–70. 10.1038/s41574-020-0387-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065425supp001.pdf (748.5KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data described in the article are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm