Abstract
Objectives
Laryngeal complications have been reported after endotracheal intubation and prone positioning in patients with critical coronavirus disease 2019 (COVID‐19), but their association is unclear. In this study, we investigated the rate of laryngeal complications in patients with COVID‐19 compared to an alternative condition (control group).
Methods
We retrospectively analyzed the data of 40 patients who underwent endotracheal intubation for either COVID‐19 or an alternative condition (control group). Data on age, sex, body mass index (BMI), cardiovascular disease (CVD) risk factors, use of prone therapy, duration of endotracheal intubation, and duration from extubation/tracheostomy to laryngeal evaluation were collected from medical records.
Results
There were no significant differences in BMI, frequency of CVD risk factors, duration of endotracheal intubation, or duration from extubation/tracheostomy to laryngeal evaluation between the two groups. In the COVID‐19 group, all patients adopted the prone position. In comparison, only one patient in the control group adopted the prone position. Significant differences were observed between the two groups regarding the incidence of vocal fold immobility and laryngeal granuloma.
Conclusion
Laryngeal complications were more common in the COVID‐19 group than in the control group. Prone positioning may be a risk factor for these complications.
Level of Evidence
4.
Keywords: COVID‐19, laryngeal granuloma, prone positioning, vocal cord paralysis
Laryngeal complications were more common in the COVID‐19 group compared to an alternative condition. Prone positioning may be a risk factor for these complications.
1. INTRODUCTION
At the beginning of the coronavirus disease 2019 (COVID‐19) pandemic caused by severe respiratory syndrome coronavirus 2 (SARS‐CoV‐2), approximately 5% of patients with COVID‐19 were classed as critical, requiring endotracheal intubation and mechanical ventilation. 1 , 2 Vaccination against SARS‐CoV‐2 is reported to be highly effective for COVID‐19. Severe COVID‐19 is rare among individuals who have a complete vaccination record, with a severity rate is 0.015%. 3 However, because of factors such as virus mutations, the number of infected individuals remains high, and there are still many patients at any one time with severe COVID‐19 in Japan. 4 COVID‐19 causes acute respiratory distress syndrome (ARDS) in approximately 20% of hospitalized patients. 2 Because prone positioning improves outcomes in patients with ARDS by reducing lung compression and improving lung perfusion, it has been widely used in patients with COVID‐19‐associated ARDS. 5 , 6 However, laryngeal complications, including vocal fold immobility, laryngeal/tracheal stenosis, and laryngeal granuloma after endotracheal intubation, have been reported after intubation and prone positioning in patients with COVID‐19, 7 , 8 , 9 , 10 , 11 , 12 , 13 and it has been suggested that prolonged intubation with prone positioning is associated with these laryngeal complications. 7 However, little is known about the laryngeal complications that occur after intubation and prone positioning in patients with severe COVID‐19. In this study, we investigated this issue.
2. MATERIALS AND METHODS
This retrospective study was approved by the institutional review board of Ehime University Medical Hospital (no. 2108028).
We treated 33 patients with COVID‐19 who required endotracheal intubation and mechanical ventilation at our hospital between January 2021 and July 2021. Among these patients, patients who underwent laryngeal evaluation using a flexible endoscope after extubation or tracheostomy by otolaryngologists were included.
Patients who were treated with endotracheal intubation for respiratory failure, except for respiratory failure caused by COVID‐19, in the intensive care unit between January 2018 and January 2021, and who underwent laryngeal evaluation using a flexible endoscope after extubation or tracheostomy by otolaryngologists, were included in this study as the control group. Patients who underwent lung surgery, cardiac surgery, or cranial surgery were excluded. Patients with airway burns were also excluded.
All patients were intubated by trained emergency physicians using video laryngoscopy. The endotracheal tube cuff pressure was maintained at 30–40 mmHg using cuff manometry in the control group and an automatic cuff pressure controller in the COVID‐19 group.
Patient data, including sex, age, body mass index (BMI), hypertension, hyperlipidemia, diabetes mellitus, prone therapy, duration of endotracheal intubation, duration from extubation/tracheostomy to laryngeal evaluation, and endoscopic laryngeal findings, were collected from patients' medical records.
The data are expressed as the mean ± standard error of the mean. Each parameter was compared between the two groups using the Mann–Whitney U test or Fisher's exact test with JMP software for Macintosh (SAS Institute Inc., Cary, NC). A p‐value of <.05 was considered statistically significant.
3. RESULTS
Of the 33 patients with severe COVID‐19 treated at our hospital, 16 patients who underwent laryngeal evaluation using a flexible endoscope were included in this study. Twenty‐four patients, including patients with heart failure (n = 8), respiratory failure due to pneumonia (n = 8), septic shock (n = 5), or ARDS (n = 3), comprised the control group.
The clinical characteristics of both groups are summarized in Table 1. In the COVID‐19 group, the age of the patients ranged from 36 to 82 years, with an average age of 60.4 ± 2.7 years. In the control group, the age of the patients ranged from 46 to 86 years, with an average age of 68.2 ± 2.5 years. The COVID‐19 group was significantly younger than the control group (p = .047). BMI was 24.9 ± 1.0 in the COVID‐19 group and 23.5 ± 2.0 in the control group; there was no significant difference in BMI between the two groups. All 16 patients with COVID‐19 adopted the prone position, while only 1 patient (4.2%) in the control group adopted the prone position (p < .001). The number of patients with risk factors for cardiovascular disease (CVD), including hypertension, hyperlipidemia, and diabetes mellitus, was not significantly different between the two groups (p = .19, p = .64, and p = .05, respectively). The duration of endotracheal intubation and the duration from extubation/tracheostomy to laryngeal evaluation were not significantly different between the two groups (p = .72 and p = .99, respectively). Five patients (31.3%) in the COVID‐19 group had unilateral vocal fold immobility (UVFI) (three cases on the left side and two cases on the right side), while one patient (4.2%) had left‐sided vocal fold immobility (VFI). There was a significant difference between the two groups (p = .03). Laryngeal granuloma was observed in five patients (31.3%) in the COVID‐19 group and in one patient (4.2%) in the control group (p = .03).
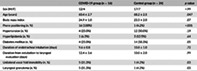
TABLE 1.
Comparison of clinical characteristics between the COVID‐19 group and the control group
| COVID‐19 group (n = 16) | Control group (n = 24) | p value | |
|---|---|---|---|
| Sex (M/F) | 12/4 | 17/7 | >.99 |
| Age (years) | 60.4 ± 2.7 | 68.2 ± 2.5 | .047 |
| Body mass index | 24.9 ± 1.0 | 23.5 ± 2.0 | .07 |
| Prone positioning (n, %) | 16 (100%) | 1 (4.2%) | <.001 |
| Hypertension (n, %) | 4 (25.0%) | 12 (50.0%) | .19 |
| Hyperlipidemia (n, %) | 1 (6.3%) | 3 (12.5%) | .64 |
| Diabetes mellitus (n, %) | 4 (25.0%) | 14 (58.3%) | .05 |
| Duration of endotracheal intubation (days) | 9.6 ± 0.8 | 10.8 ± 1.0 | .72 |
| Duration from extubation to laryngeal evaluation (days) | 12.4 ± 3.6 | 10.0 ± 2.0 | .99 |
| Unilateral vocal fold immobility (n, %) | 5 (31.3%) | 1 (4.2%) | .03 |
| Laryngeal granuloma (n, %) | 5 (31.3%) | 1 (4.2%) | .03 |
Note: M, male; F, female.
Figure 1 shows the size of the endotracheal tube. Among the male patients, 2 of 12 (16.7%) were intubated with an endotracheal tube with an internal diameter (ID) of 8.0 mm (outer diameter [OD] 11.8 mm) in the COVID‐19 group, and 7 of 17 patients (41.2%) were intubated with an endotracheal tube with an ID of 8.0 mm in the control group. Among the female patients, all four were intubated with an endotracheal tube with an ID of 7.0 mm (OD 10.4 mm) in the COVID‐19 group, and four of seven patients (57.1%) were intubated with an endotracheal tube with an ID of 7.5 mm (OD 11.2 mm) in the control group. Eight (50.0%) of 16 patients in the COVID‐19 group and 10 (41.7%) of 24 patients in the control group underwent tracheostomy. The duration from intubation to tracheostomy was 12.3 ± 0.9 days in the COVID‐19 group and 12.0 ± 1.7 days in the control group; there were no differences in the days from intubation to tracheostomy between both groups (p = .59).
FIGURE 1.
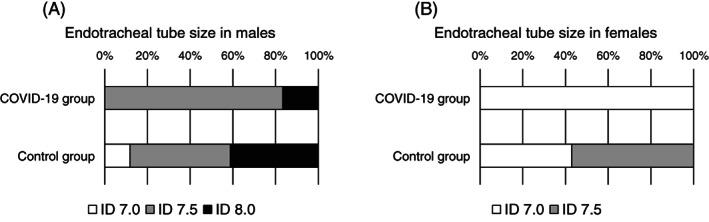
(A) Endotracheal tube size in male patients. An endotracheal tube with an internal diameter (ID) of 7.5 mm (outer diameter [OD] of 11.2 mm) was used most frequently in both groups. An endotracheal tube with an ID of 8.0 mm (OD of 11.8 mm) was less commonly used in the COVID‐19 group than in the control group. (B) Endotracheal tube size in female patients. All patients with COVID‐19 were intubated with an endotracheal tube with an ID of 7.0 mm (OD 10.4 mm), and 57.1% of patients in the control group were intubated with an endotracheal tube with an ID of 7.5 mm (OD of 11.2 mm)
Table 2 shows a comparison of clinical characteristics according to the presence or absence of UVFI among patients in the COVID‐19 group. Sex, age, BMI, duration of endotracheal intubation, duration from extubation to laryngeal evaluation, and CVD risk factors were not significantly different.
TABLE 2.
Comparison of clinical characteristics according to the presence or absence of unilateral vocal fold immobility
| Unilateral vocal fold immobility | |||
|---|---|---|---|
| Yes (n = 5) | No (n = 11) | p value | |
| Sex (M/F) | 3/2 | 9/2 | .55 |
| Age (years) | 64.6 ± 5.0 | 58.5 ± 3.3 | .46 |
| Body mass index | 23.8 ± 1.5 | 25.3 ± 1.2 | .57 |
| Duration of endotracheal intubation (days) | 9.6 ± 0.7 | 9.5 ± 1.1 | .91 |
| Duration from extubation to laryngeal evaluation (days) | 10.2 ± 6.1 | 13.5 ± 4.6 | .78 |
| Hypertension | 1 (20.0%) | 3 (27.3%) | >.99 |
| Dyslipidemia | 0 (0%) | 1 (9.1%) | >.99 |
| Diabetes mellitus | 2 (40.0%) | 2 (18.2%) | .55 |
| Endotracheal tube size | |||
| Male (n = 12) | ID 7.5: 3 | ID 7.5: 7 | |
| ID 8.0: 0 | ID 8.0: 2 | — | |
| Female (n = 4) | ID 7.0: 2 | ID 7.0: 2 | |
Note: M, male; F, female.
Table 3 shows a comparison of clinical characteristics according to the presence or absence of laryngeal granuloma among patients in the COVID‐19 group. The duration of endotracheal intubation was significantly shorter in patients with laryngeal granuloma than in patients without laryngeal granuloma (p = .03), while other factors were not significantly different between the two groups. Two patients had both UVFI and laryngeal granuloma.
TABLE 3.
Comparison of clinical characteristics according to the presence or absence of laryngeal granuloma
| Unilateral vocal fold immobility | |||
|---|---|---|---|
| Yes (n = 5) | No (n = 11) | p value | |
| Sex (M/F) | 4/1 | 8/3 | >.99 |
| Age (years) | 52.2 ± 4.4 | 64.2 ± 2.9 | .06 |
| Body mass index | 25.5 ± 0.7 | 24.6 ± 1.4 | .31 |
| Duration of endotracheal intubation (days) | 6.8 ± 1.0 | 10.8 ± 0.9 | .03 |
| Duration from extubation to laryngeal evaluation (days) | 10.6 ± 8.6 | 13.3 ± 3.8 | .23 |
| Hypertension | 1 (20.0%) | 3 (27.3%) | >.99 |
| Dyslipidemia | 0 (0%) | 1 (9.1%) | >.99 |
| Diabetes mellitus | 1 (20.0%) | 3 (27.3%) | >.99 |
| Endotracheal tube size | |||
| Male (n = 12) | ID 7.5: 4 | ID 7.5: 6 | |
| ID 8.0: 0 | ID 8.0: 2 | — | |
| Female (n = 4) | ID 7.0: 1 | ID 7.0: 3 | |
Note: M, male; F, female.
4. DISCUSSION
In this study, laryngeal complications, including UVFI and laryngeal granuloma, were observed more frequently in patients with severe COVID‐19 than in control subjects. Although the mechanism underlying these findings is unknown, prone positioning may be associated with the occurrence of laryngeal complications after endotracheal intubation.
It has been reported previously that 7.9–76% of patients with severe COVID‐19 have UVFI following endotracheal intubation. 7 , 8 , 9 Our results, which demonstrated UVFI in approximately 30% of patients, were consistent with these previous reports. The reported incidence of UVFI after prolonged intubation ranges from 7% to 41% among patients without COVID‐19. 14 , 15 , 16 , 17 However, it has not previously been reported whether there is a difference in the frequency of UVFI between COVID‐19 and other diseases requiring endotracheal intubation. In our study, the rate of UVFI after intubation was significantly higher in patients with COVID‐19 than in the control group. The duration of intubation, older age, risk factors for CVD, and the size of the endotracheal tube have been reported to be associated with VFI after endotracheal intubation. 16 , 17 , 18 , 19 In this study, patients were younger in the COVID‐19 group than in the control group. CVD risk factors, including BMI, hypertension, hyperlipidemia, and diabetes mellitus, did not differ between the two groups. The duration of intubation and the size of the endotracheal tube also did not differ between the two groups. Prone positioning was a factor that was significantly different between the two groups. It has been suggested that UVFI after endotracheal intubation is caused by recurrent laryngeal nerve paralysis (RLNP) due to compressive neural injury or arytenoid dislocation/subluxation. 14 , 20 , 21 It was difficult to differentiate between these two diseases because we did not perform laryngeal electromyography. Thus, further studies are required to investigate whether UVFI after intubation and prone therapy are caused by RLNP or arytenoid dislocation.
Laryngeal granuloma was more frequently observed in the COVID‐19 group than in the control group. It has been reported previously that the duration of intubation and the size of the endotracheal tube are risk factors for laryngeal granuloma after endotracheal intubation. 16 Similar to UVFI, these factors did not differ between the two groups. Therefore, it is suggested that prone positioning is associated with the incidence of laryngeal granuloma. In our cohort, a shorter duration of intubation was associated with the incidence of laryngeal granulation in COVID‐19 group. However, it is unclear why a shorter duration of intubation is related to laryngeal granulation. It has been reported that gastric reflux is suggested to be related to the incidence of laryngeal granulation. 22 , 23 Therefore, other factors including acid reflux might be related to the incidence of laryngeal granulation.
Prone positioning has been used to treat severe hypoxemia in patients with ARDS, 24 , 25 and it is commonly used for patients with severe COVID‐19. 6 , 7 Adverse events associated with prone positioning include pressure ulcers, endotracheal tube obstruction, facial edema, enteral feeding intolerance, accidental extubation, and hemodynamic instability, among others. 26 However, laryngeal complications due to prone positioning are not well known. The mechanism of laryngeal complications caused by prone positioning is unclear. Rotation of the neck during prone positioning may exacerbate the pressure on the larynx due to the endotracheal tube or may dislocate the endotracheal tube and cause arytenoid dislocation. In addition, disturbance of mucosal microcirculation and nerve injury because of SARS‐CoV‐2 are potential causes of UVFI. It has been reported that early intervention for patients with postintubation laryngeal injury is associated with a favorable outcome compared with late intervention. 27 Otolaryngologists should be aware of these laryngeal complications after endotracheal intubation and prone positioning and should intervene earlier.
To date, an approach to prevent laryngeal complications after intubation and prone positioning in patients with severe COVID‐19 has not been reported. However, laryngeal/tracheal stenosis was not observed in our cohort. The duration of intubation in the COVID‐19 group was similar to that in the control group, and relatively shorter than that in previous reports that reported these laryngeal complications after intubation and prone positioning in patients with severe COVID‐19. 7 , 8 , 9 , 10 , 11 , 12 , 13 It has been recommended that tracheostomy is performed at least 10 days after intubation. 28 We have performed tracheostomies within 14 days to prevent severe laryngeal complications including laryngeal or tracheal stenosis. UVFI and laryngeal granulation can be treated conservatively, while laryngeal and tracheal stenosis require surgical procedures. Therefore, timely tracheostomy is important when intubation and prone positioning are prolonged.
There are several limitations in this study that should be noted. First, this study was retrospective, and the number of included patients was small. In a power analysis comparing laryngeal complications between the COVID‐19 group and the control group, the power (1 − β) was 0.58. In addition, the number of included patients was too small in which to perform other statistical tests such as multivariate regression. A larger‐scale, prospective study will be needed to clarify our observations. Second, because we could not assess the larynx using a flexible endoscope in all patients in the COVID‐19 group, there was a risk of bias that the patients were enriched for those with laryngeal pathologies, and thus there is a possibility that the patients with COVID‐19 in our cohort were not necessarily representative of the general population. However, some patients could not be evaluated with this approach because they were transferred to another hospital or because there was a lack of testing equipment, and thus this was not related to their symptoms. We could also not assess the larynx in all patients in the control group; therefore, there was also a risk of bias in this group. However, most prolonged intubated patients underwent larynx evaluation by flexible endoscopy before oral intake. Third, we could not follow up all patients with UVFI or laryngeal granuloma. Further studies on the outcomes of UVFI and laryngeal granuloma after endotracheal intubation in patients with severe COVID‐19 are needed. In addition, laryngeal and tracheal stenosis were not observed in our cohort; however, late laryngoscopic evaluation will be needed to confirm the absence of laryngeal or tracheal stenosis in the long term. Fourth, the influence of laryngeal inflammation caused by SARS‐CoV‐2 is still unknown. In this cohort, all patients in the COVID‐19 group were treated by prone positioning therapy, while only one patient in the control group was treated using prone positioning therapy. Comparisons between the COVID‐19 group and the control group without prone positioning are required to investigate the influence of laryngeal inflammation due to SARS‐CoV‐2 infection. In addition, because the proportion that required prone positioning differed between the COVID‐19 group and control group, we should consider the possibility that systemic differences between COVID‐19 and other diseases were involved.
5. CONCLUSION
In this study, laryngeal complications, including UVFI and laryngeal granuloma, were more common in patients with COVID‐19 than in the control group. Prone positioning may be a risk factor for laryngeal complications after endotracheal intubation.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGMENT
We thank H. Nikki March, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Aibara S, Okada M, Tanaka‐Nishikubo K, et al. Laryngeal complications after endotracheal intubation and prone positioning in patients with coronavirus disease 2019. Laryngoscope Investigative Otolaryngology. 2022;7(6):1909‐1914. doi: 10.1002/lio2.874
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239‐1242. [DOI] [PubMed] [Google Scholar]
- 3. Yek C, Warner S, Wiltz JL, et al. Risk factors for severe COVID‐19 outcomes among persons aged ≥18 years who completed a primary COVID‐19 vaccination series – 465 health care facilities, United States, December 2020–October 2021. MMWR Morb Mortal Wkly Rep. 2022;71:19‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ministry of Health, Labour and Welfare, Japan. Current situation in Japan. https://www.mhlw.go.jp/stf/covid‐19/kokunainohasseijoukyou.html. Accessed April 20, 2022.
- 5. Qadri SK, Ng P, Toh TSW, et al. Critically ill patients with COVID‐19: a narrative review on prone position. Pulm Ther. 2020;6:233‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Petrone P, Brathwaite CEM, Joseph DK. Prone ventilation as treatment of acute respiratory distress syndrome related to COVID‐19. Eur J Trauma Emerg Surg. 2021;47:1017‐1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Naunheim MR, Zhou AS, Puka E, et al. Laryngeal complications of COVID‐19. Laryngosc Investig Otolaryngol. 2020;5:1117‐1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rouhani MJ, Clunie G, Thong G, et al. A prospective study of voice, swallow, and airway outcomes following tracheostomy for COVID‐19. Laryngoscope. 2021;131:E1918‐E1925. [DOI] [PubMed] [Google Scholar]
- 9. Osbeck Sandblom H, Dotevall H, Svennerholm K, Tuomi L, Finizia C. Characterization of dysphagia and laryngeal findings in COVID‐19 patients treated in the ICU—an observational clinical study. PLoS One. 2021;16:e0252347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thong G, Lorenz H, Sandhu GS, AlYaghchi C. Emergency presentation of iatrogenic airway stenosis following intubation in a patient with COVID‐19 and its management. BMJ Case Rep. 2020;13:e238508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fiacchini G, Tricò D, Ribechini A, et al. Evaluation of the incidence and potential mechanisms of tracheal complications in patients with COVID‐19. JAMA Otolaryngol Head Neck Surg. 2021;147:70‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bertone F, Robiolio E, Gervasio CF. Vocal cord ulcer following endotracheal intubation for mechanical ventilation in COVID‐19 pneumonia: a case report from Northern Italy. Am J Case Rep. 2020;21:e928126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scholfield DW, Warner E, Ahmed J, Ghufoor K. Subglottic and tracheal stenosis associated with coronavirus disease 2019. J Laryngol Otol. 2021;135:656‐658. [DOI] [PubMed] [Google Scholar]
- 14. Campbell BR, Shinn JR, Kimura KS, et al. Unilateral vocal fold immobility after prolonged endotracheal intubation. JAMA Otolaryngol Head Neck Surg. 2020;146:160‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: a prospective analysis of contributing factors. Laryngoscope. 2021;121:596‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994;111:453‐459. [DOI] [PubMed] [Google Scholar]
- 17. Brodsky MB, Levy MJ, Jedlanek E, et al. Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: a systematic review. Crit Care Med. 2018;46:2010‐2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kikura M, Suzuki K, Itagaki T, Takada T, Sato S. Age and comorbidity as risk factors for vocal cord paralysis associated with tracheal intubation. Br J Anaesth. 2007;98:524‐530. [DOI] [PubMed] [Google Scholar]
- 19. Pan DR, Jiang N. Outcomes of intubation‐induced vocal fold motion impairment. J Voice. 2020;34:250‐258. [DOI] [PubMed] [Google Scholar]
- 20. Hoffman HT, Brunberg JA, Winter P, et al. Arytenoid subluxation: diagnosis and treatment. Ann Otol Rhinol Laryngol. 1991;100:1‐9. [DOI] [PubMed] [Google Scholar]
- 21. Norris BK, Schweinfurth JM. Arytenoid dislocation: an analysis of the contemporary literature. Laryngoscope. 2011;121:142‐146. [DOI] [PubMed] [Google Scholar]
- 22. Shimazu R, Kuratomi Y, Aoki S, Inokuchi A. Laryngeal granuloma in experimental rats with gastroesophageal reflux disease and mechanically injured vocal cord mucosa. Ann Otol Rhinol Laryngol. 2014;123(4):247‐251. [DOI] [PubMed] [Google Scholar]
- 23. Ylitalo R, Ramel S. Extraesophageal reflux in patients with contact granuloma: a prospective controlled study. Ann Otol Rhinol Laryngol. 2002;111:441‐446. [DOI] [PubMed] [Google Scholar]
- 24. Gattinoni L, Tognoni G, Pesenti A, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345:568‐573. [DOI] [PubMed] [Google Scholar]
- 25. Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159‐2168. [DOI] [PubMed] [Google Scholar]
- 26. Kallet RH. A comprehensive review of prone position in ARDS. Respir Care. 2015;60:1660‐1687. [DOI] [PubMed] [Google Scholar]
- 27. Lowery AS, Malenke JA, Bolduan AJ, Shinn J, Wootten CT, Gelbard A. Early intervention for the treatment of acute laryngeal injury after intubation. JAMA Otolaryngol Head Neck Surg. 2021;147:232‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McGrath BA, Brenner MJ, Warrillow SJ, et al. Tracheostomy in the COVID‐19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717‐725. [DOI] [PMC free article] [PubMed] [Google Scholar]


