Abstract
Hurricane evacuations during a pandemic require a revised understanding of vulnerabilities within communities and the development of different strategies and policies to accommodate the needs of populations vulnerable to the combined hurricane-pandemic threat. The prolonged COVID-19 pandemic has added economic, psychological, social, health, and workforce stressors to communities across the United States. Using original research data from workshops held in May 2020 involving emergency management, public health, and related experts to support planning efforts for hurricane evacuation and sheltering, we analyze two key issues: (1) shifting sources of vulnerability in a COVID-19 environment and (2) solutions proposed during the post-lockdown/pre-vaccine time frame. We discuss findings in the context of policy integration options to solidify and expand protections for populations in need of evacuation and sheltering assistance. Findings show that vulnerabilities associated with underlying health conditions and socio-economic disparities were of increased concern to evacuation and shelter planners. Non-congregate options were of interest but were not expected to accommodate all populations in need of public assistance. Registries used in some states offer means with which to evaluate vulnerabilities and align individuals and families with appropriate resources and facilities. There remains a need to expand and standardize existing policies based on COVID-19 operating protocols to ensure inclusivity of socio-economically disadvantaged and disabled individuals in hurricane preparation efforts.
Keywords: Vulnerability, Hurricane + pandemic event, Sheltering, Evacuation
1. Introduction and background
On March 11, 2020 the World Health Organization declared the COVID-19 outbreak a pandemic. By summer, the COVID-19 pandemic was entrenched in the U.S., taxing healthcare and medical infrastructure while restricting social and economic activity. However, “The pandemic's disruption of daily lives, health systems, and economies is unprecedented, and reverberations will continue long after the first wave of infection ebbs and a vaccine is developed” [1]; p. 586). The pandemic is occurring against a backdrop of natural hazards such as hurricanes, wildfires, and tornadoes. As the coronavirus outbreak continues, governments will need to develop and adjust policies and practices that address not only the pandemic itself, but also potential collisions and intersections with other hazards.
Vulnerable populations have an increased risk of negative outcomes (e.g., economic hardships, health effects, social isolation) from hazards due to political, economic, or social inequities experienced at the household, community, state, and national levels [2]. Capacity to withstand hazards vary from one community to another depending on institutional, infrastructural, and community characteristics and can be assessed at a variety of scales [3]. As such, the vulnerability of individuals and groups are unique to a given geographic area and hazard. People living in coastal areas, for example, may be more vulnerable to hurricanes and coastal flooding, while those in mountainous areas or the northern plains may be vulnerable to snowstorms and extreme wind events. Furthermore, people and groups are differentially vulnerable given where they are situated within the natural and built environments, economic structure, and the social and institutional fabric of a community.
Conducting evacuation and sheltering operations during a widespread pandemic is an unprecedented task. This article specifically addresses the following research questions: (1) To what extent has the pandemic added to or exacerbated pre-existing socioeconomic and health inequities of vulnerable populations, especially when the pandemic compounds vulnerability to other hazards? (2) What policy options can be leveraged to solidify and expand the strategies that emerged to meet the needs of vulnerable populations facing the threat of a hurricane during a pandemic? We answer these questions for the specific case of social vulnerability to a compound hurricane-pandemic threat. We analyze how the COVID-19 pandemic is expected to expand groups vulnerable to hurricane hazards and how evacuation and sheltering operations may develop new accommodations for the additional populations. Our analysis uses qualitative data collected in May and June 2020 from practitioners and experts in emergency management and related fields from the Gulf coast and eastern seaboard of the United States. Our findings emphasize how COVID-19 related economic and health inequalities expanded the working definition of vulnerable populations in hazardous settings. We tie our findings together to offer implications for policy and practice that solidify and expand protections for vulnerable populations and meet their needs by incorporating vulnerability explicitly into emergency management planning and operations. This study may inform emergency management for compound hazards requiring evacuation and sheltering of vulnerable populations that may not be traditionally considered vulnerable to one of the hazards or with increased vulnerability due to experiencing vulnerability from both hazards simultaneously.
2. The COVID-19 pandemic and compounding hurricane threats
For coastal communities along the Atlantic and Gulf coasts of the U.S., concerns about virus transmission complicated efforts to prepare for and respond to the 2020 hurricane season, which was forecasted to be above normal [4]. Hurricane preparedness and response under normal conditions, including evacuation and mass sheltering, are generally at odds with virus containment and contagion management strategies such as social or physical distancing, self-isolation and quarantining, and cleaning and hygiene activities [5,6]. Pei et al.’s [7] simulations show that virus transmission may be increased by hurricane evacuation unless minimization measures are implemented by the counties receiving evacuees.
The COVID-19 pandemic has changed local, state, and federal agencies’ preparedness and response strategies for hurricanes, especially in terms of evacuation strategies and mass sheltering. For example, the Federal Emergency Management Agency [8] released the COVID-19 Pandemic Operational Guidance for the 2020 Hurricane Season that contained considerations specific to hurricane response during the COVID-19 pandemic. Recommended changes included reviewing clearance times and decision timelines for mass care and sheltering given COVID-19 infection concerns, modifying evacuation plans to account for limited travel options and increased time needed for evacuation of healthcare facilities, leveraging non-congregate sheltering options, conducting COVID-19 screenings of staff and evacuees entering shelter locations, and targeting evacuation orders and communication to reduce voluntary evacuation from areas outside a declared evacuation area [8].
The prolonged nature of the COVID-19 pandemic, including the sustained efforts for infection control and virus containment as well as the economic impacts, can have significant implications for at-risk coastal communities and people within these communities. While there is significant literature on vulnerability to hurricane evacuation and sheltering behavior (see for example [[9], [10], [11], [12], [13], [14], [15]], additional research is needed regarding how individuals and communities react when faced with the threat of a hurricane during a pandemic and how emergency management policies and practices may be adapted to improve outcomes.
Fears about the virus and financial strain during the pandemic make evacuation behavior difficult to predict [6]. A pandemic scenario may affect the propensity of vulnerable populations to either evacuate or shelter in a congregate venue. Survey results from communities in coastal Virginia, for example, show that fear of virus transmission will not deter populations traditionally in need from going to shelters [16]. Furthermore, while Pei et al.’s [7] simulations show that virus transmission may be increased by hurricane evacuation, financial strain associated with COVID-19 reduced evacuation intentions for populations experiencing financial impacts of the pandemic [16]. This finding highlights how income and economic insecurity resulting from the pandemic might introduce additional vulnerabilities to different individuals and groups.
3. Vulnerability
The risk of a disaster is the product of the potentially damaging hazard, such as a hurricane, wildfire, or pandemic, and the vulnerability of the people, infrastructure, political system, economy, and environment experiencing the hazard [2,[17], [18], [19], [20], [21], [67]]. The starting point for reducing disaster risk and enhancing resilience is understanding how both hazards and vulnerabilities uniquely affect specific segments of society [22]. Understanding vulnerability and how it changes, particularly when considering a post-COVID world, is critical for managing future events.
Three themes or perspectives underpin the conceptualization of vulnerability [19]. The first hinges on the association between vulnerability and risk, where vulnerability is a pre-existing condition [2]. In the context of a hazard such as a hurricane, this perspective considers the distribution of hurricane risk such as from storm surge or strong winds, occupancy within the hazard zone, and potential damage. Second, vulnerability reflects social or tempered response to hazards where not all individuals and groups are equally vulnerable and the differential vulnerability depends on their coping ability [19,20]. This perspective emphasizes the social vulnerability of individuals and communities, and highlights vulnerability as socially constructed, “rooted in historical, cultural, social, and economic processes” [19]; p. 533). Finally, a third theme combines elements of the first two, focusing on vulnerability as hazardousness and vulnerability of place [19,23,24]. This conceptualization treats vulnerability as both a biophysical threat and social capacity within a specific geographic context.
Vulnerability has policy implications for disaster risk reduction efforts [25]. Specifically, for whom or for what should policies be targeted? In analyzing how the composition of vulnerable populations are changing and to identify public policy implications of those changes during a simultaneous hurricane and pandemic, we utilize the social vulnerability lens. We consider social vulnerability a forward-looking concept that lends itself to policy making by linking factors that place people at risk relative to each other and the conditions of their socio-economic and physical environments [[26], [27], [28]]. This also allows us to determine how social, economic, and environmental changes may create “windows of vulnerability” [20]. Understanding social vulnerability and the changing nature and scope of vulnerability relative to the economic, health, and social effects of the COVID-19 pandemic is critical for understanding how emergency management policies and programs can be adaptive [66].
4. Social vulnerability and hurricane evacuation and sheltering
The roots of social vulnerability are generally found within the underlying social conditions that may be temporally remote or distant from the actual hazard event [29]. Vink, Takeuchi, and Kibler [30] identified four characteristics of social vulnerability: (1) lack of material and/or financial resources; (2) having physical or mental disability; (3) lack of access to information; and (4) having specific commitments that restrict the ability to cope. These characteristics explain the vulnerability of six main groups: children, older adults, ethnic minorities, people with disabilities, people living in poverty, and women. We use these four characteristics to organize our analysis of how the COVID-19 pandemic has affected vulnerable populations, the extent to which the pandemic has added to or exacerbated economic and health inequalities, and the existing policies in place to ensure equity for vulnerable populations during hurricane evacuation and sheltering operations.
4.1. Lack of material and/or financial resources
Economic status of individuals has long been identified as an indicator of vulnerability. Household income is a common measure of the resource base available to draw upon in coping with hazards [31], and liquid assets that can easily be converted into income are key facets of the resource base [[68], [69]]. Lower income individuals often bear a disproportionate impact of a disaster, as they tend to be concentrated in areas at higher risk or reside in housing that is less able to provide protection. More importantly, they often do not have access to resources needed to prepare for, respond to, and recover from a disaster. For example, Mcleod and Kessler [31] find that low-income individuals and households have higher risk exposure, and their vulnerability is not only determined by their low-income status but also on how their income influences access to education and subsequent occupational choice. Evacuation can involve significant financial resources to cover transportation, lodging, meals, and other living costs [12], that may disproportionately challenge those with limited resources. Lack of transportation is a major barrier to evacuation for socially vulnerable populations [2,12].
The provision of emergency shelters is an emergency response strategy to meet the needs of those with limited resources to evacuate and who lack safe residences within which they can shelter in place. Other emergency management responses to target these vulnerable populations include free transportation services to evacuate lower-income residents to safer locations and distribution of preparedness kits for residents who are unemployed, underemployed, or receiving public assistance [32].
4.2. Physical and mental disabilities
Studies have shown that physical and mental conditions have a significant impact on vulnerability of individuals with disabilities [[33], [34], [35]]. For example, in terms of coping response, research has shown that medically fragile populations have lower propensity to evacuate compared to those without medical challenges [14,36]. Evacuation plans are often based on the assumption that people have the physical and mental capabilities to, for instance, successfully travel to safe zones or to access emergency shelters [30].
To develop inclusive emergency preparedness and response plans, the Centers for Disease Control and Prevention (CDC) recommends state agencies include information on persons with disabilities as part of agencies’ priorities for addressing vulnerable populations [37]. States have incorporated information on persons with disabilities through public health data such as those collected from national and state-based surveys, as well as through voluntary registries such as those maintained by the National Center on Birth Defects and Developmental Disabilities, and the CDC.
4.3. Limited access to information due to lack of knowledge and experience
Evacuation and related emergency management policies and practices often assume that at-risk populations have access to certain evacuation resources, information, and experiences [30]. This assumption can be detrimental to individuals and groups without such access. Limited language proficiencies, for example, may prevent some people from obtaining knowledge needed to effectively cope with the threat such as by evacuating or going to an emergency shelter. Transient or migrant populations may also lack knowledge or understanding of the local context which can increase their vulnerability.
Studies have shown that individuals with limited access to information and evacuation experiences require communication and information platforms that can improve their knowledge and safety [35]. Continuous and sustained communication about shelter availability and transparent information about local government and stakeholder responsibilities are among evacuation best practices that can address some of the needs of those with limited information access [35]. These practices ensure the provision and effective dissemination of information on evacuation, especially for the evacuation of vulnerable groups that are more likely to have limited access to evacuation information or lack previous experiences from which to draw on [30,35,37].
4.4. Restricted by commitments
Some individuals are disproportionately vulnerable because they have commitments that restrict their ability to cope with a hazard event. For example, some individuals are restricted in their ability to evacuate because they must care for dependents or pets, or because they are worried about loss of possessions during an event. Ng, Behr, and Diaz [14] found that people were less willing to evacuate due to increased perceptions that burglary will happen while their residences are vacant. Emergency management professionals also perceive this concern especially in low- and moderate-income neighborhoods [32]. In this case, social vulnerability stems from an attachment or a sense of duty which influences decision making and ability to cope during an evacuation.
Individuals who are caretakers of children or dependent adults, such as those who require specialized medical equipment or have transportation needs, are also vulnerable because their commitment and duty to these dependents limit their mobility to evacuate. Access to specialized shelters such as those with medical equipment or that offer power for electricity-dependent equipment make it easier for vulnerable individuals, and those they care for, to find safe shelter.
In investigating evacuation failure during disasters, Heath et al. [38] found that pet-owning households without children are less likely to evacuate compared to other households. This finding underscores the need for evacuation procedures that take into consideration the evacuation needs of specific households such as those with pets. Planning guidance from the U.S. Department of Homeland Security [39]; for example, states that evacuation procedures need to accommodate people with pets or service animals, since previous experience has demonstrated that individuals would refuse to evacuate if they had to leave their pets behind.
5. Conceptual model
To answer the research questions, we developed a conceptual model adapted from the framework by Vink et al. [30] that focuses on social vulnerability to flooding. The Vink et al. framework had the core aim of examining relevant policies to reduce vulnerability, and as such, was particularly relevant for understanding how policies should be targeted at different characteristics of vulnerability and socially vulnerable populations to equitably ameliorate disaster risks at multiple levels for the different groups of people. We adapt this framework to apply to the context of simultaneous risk of hurricanes and pandemic, and the associated evacuation and sheltering response to compound hurricane-pandemic risks.
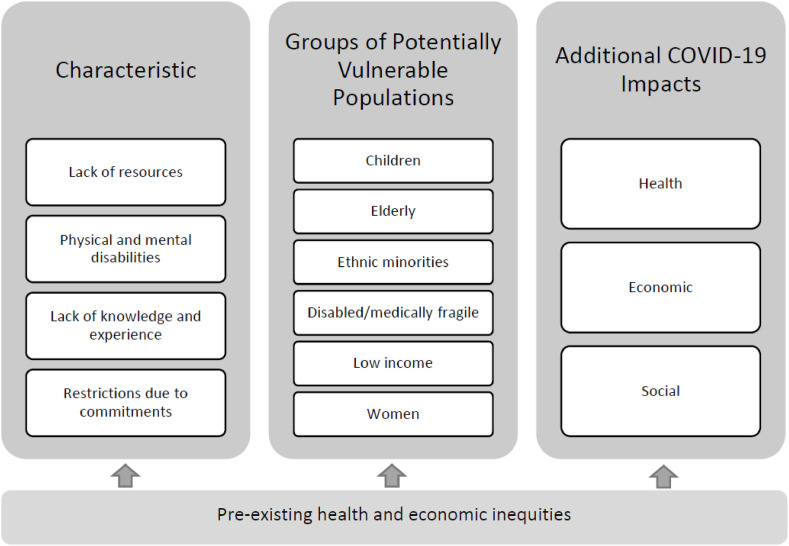
The first two components of the conceptual model shown in Fig. 1 reflect the four characteristics of social vulnerability and groups of potentially vulnerable populations from the Vink et al. framework. We then include the additional impacts of the COVID-19 pandemic on vulnerable populations. Finally, the conceptual model recognizes that social vulnerability is intertwined with pre-existing health and economic inequities, and these inequities may exacerbate social vulnerability for some individuals and groups. Endemic inequities, as they relate to vulnerability, are inherent in factors such as income, education, nutrition, transportation, housing, jobs, environment, psychosocial stresses, and health care [34].
Fig. 1.
Conceptual model of social vulnerability to a simultaneous hurricane and pandemic threat, adapted by authors from Vink et al. [30].
The COVID-19 pandemic shares commonalities with other disasters, including that vulnerabilities and impacts are disproportionately distributed and some groups are more socially vulnerable than others. “In the COVID-19 pandemic everyone is susceptible to the virus, but not everyone is vulnerable in the same way or to the same degree. Some aspects of susceptibility in the pandemic can be exacerbated by socially constructed conditions such as malnutrition, addiction, and poverty which are dimensions of vulnerability rooted in processes such as corruption, inequality, lack of access to services such as healthcare, sanitation, and education” [40]; p. 2).
However, Yusuf et al. [41] note that while there is overlap between populations vulnerable to the coronavirus and to a hurricane, “the [COVID-19] pandemic presents new vulnerable populations” and that in “recognizing individuals at higher risk of contracting COVID-19 – the elderly and medically-fragile – and those who lack the ability to evacuate, the definition of a vulnerable population during the hurricane-pandemic is being expanded” (p. 164). Research has found that the disproportionate burden of a pandemic among socially vulnerable people and groups can be partly explained by economic, health, and social factors, and exacerbated by inequities faced by these populations [40,[42], [43], [44]].
Economic impacts of the pandemic may contribute to greater vulnerability as more people experience reduction in or complete loss of employment. These impacts challenge not only how individuals and families meet their day-to-day needs, but also reduces their coping ability to evacuate during a hurricane. Dasgupta et al. [45] found that counties with housing characteristics of low-to moderate-income households (e.g., high-density housing and crowded housing) and with a larger percentage of residents lacking access to vehicles, had higher risk ratios for being a COVID-19 hotspot. This is in line with findings where low-income groups and racial minorities have been identified as more vulnerable to the pandemic [[46], [47], [48]]. Low-income individuals are more likely to keep working in in-person environments during the COVID-19 pandemic because they do not have enough savings to live on which gives them less flexibility in deciding to stay at home [49].
Medical evidence also indicates that the elderly and the medically fragile are particularly vulnerable during the pandemic. For example, those with cancer are more vulnerable to infections [50]. Specific populations, such as African Americans, Latinos, and Native Americans have also experienced a disproportionate burden of COVID-19 infections and deaths [48,51]. Analysis by Correa-Agudelo et al. [48] of COVID-19 mortality rates in the early stage of the pandemic found that the top ten most populous counties in terms of COVID-19 mortality risks had higher proportions of African American and other minority races compared to the national average.
Some of the root causes of social vulnerability such as physical and mental disabilities and other underlying health and physical conditions or challenges have been exacerbated by the COVID-19 pandemic. Stay-at-home and physical distancing approaches to managing COVID-19 contagion have also led to social impacts, especially in terms of vulnerabilities due to social isolation. Individuals with mental health and substance abuse problems, along with those subject to domestic abuse, become further isolated and their symptoms and victimization may worsen.
Economic and health inequalities may perpetuate and exacerbate vulnerabilities. For example, individuals with low socio-economic status likely also live in housing that is overcrowded and/or in poor condition. Such residences, where physical distancing cannot be maintained, make them more susceptible to coronavirus exposure and to physical damage from a hurricane. Hamilton [52] notes that people experience scarcity differently according to their socio-economic status, and that the scarcity of products such as toilet paper, cleaning supplies, and protective equipment during the COVID-19 pandemic exacerbates economic inequalities because of hoarding behavior by those with greater financial resources. Furthermore, she argues that coping responses and other risks may be affected by previous and chronic experiences with resource scarcity (e.g., people living in poverty or those with lower incomes).
From a health disparities or inequities perspective, upstream and midstream social determinants of health and health outcomes are also important in recognizing how economic, health, and social effects of COVID-19 amplify vulnerability of certain individuals and groups [53,54]. For example, lack of health insurance and limited access to COVID-19 testing and quality health care contribute to medically underserved individuals and make them disproportionately more vulnerable [53,55]. The extant research also identifies how racial inequality reinforces health inequities [56] and that healthcare may bias certain racial and minority groups leading to disparate quality of care and health outcomes [57].
6. Methods
A team of researchers from Old Dominion University and the University of South Florida conducted online workshops through Zoom as well as through Zeetings, a web-based platform that allowed participants to access the same set of questions through asynchronous collaboration, in May and June 2020. A series of six workshops engaged professionals and subject matter experts involved in evacuation and sheltering vulnerable populations in gathering information on planning, resource needs, and concerns during the COVID-19 pandemic. Participants were identified through existing researcher networks from both Universities, and potential participants were asked to send the invitation to anyone they thought should be included. A convenience snowball sample was used to recruit participants to the workshops. These workshops were held during the post-lockdown/pre-vaccination time frame of the COVID-19 response phase that simultaneously took place with the 2020 Atlantic hurricane preparedness phase. Old Dominion University's Institutional Review Board rendered the decision, Reference # 20–099, of outside the definition of human subjects research for this study, Package # 1606408-1, on May 12, 2020.
The online workshops included discussion about which populations are considered vulnerable and protocols to accommodate the needs of additional populations during the anticipated 2020 Atlantic hurricane season in the midst of the COVID-19 pandemic. Each of the six workshops focused on a specific theme: (1) vulnerable populations, (2) health and infection control, (3) evacuation and sheltering workforce, (4) psychological well-being, (5) logistics, and (6) communication and messaging. Each workshop included three to four semi-structured questions identifying areas of concern, capacities to accommodate emergent issues, and resource needs to implement best practices related to the theme. For example, the workshop on vulnerable populations included the following discussion questions: (1) What changes to hurricane evacuation and sheltering planning are being considered or underway? (2) What populations are most vulnerable and why? (3) What issues are/will be impacting vulnerable populations?
Professionals from federal, state, and local agencies, nonprofit and volunteer organizations, businesses, and universities with expertise including emergency management, public health and administration, social services and science were recruited. Participants held positions such as Emergency Managers, Emergency Coordinators, Public Health Professionals, among others. Two hundred sixty-five individuals from 20 states, mostly from the Atlantic and Gulf Coasts, participated across the six workshops. Participants represented the following types of agencies at the federal, state, and local levels: emergency management, public health, human services, mass care, and transportation. Participating nonprofit and volunteer organizations include those focusing on disaster response and recovery, serving specific vulnerable populations such as pregnant women and children, addressing social equity issues, and research associations focusing on issues such as environmental health, public health, and marine sciences.
Workshop participation ranged from 74 attendees (for the workshop on psychological well-being) to 198 attendees (for the workshop on vulnerable populations). Workshop attendance was opt-in. Participants could attend a single workshop or multiple workshops and many attended more than one workshop. Identifying information was not associated with workshop participation to ensure participant confidentiality. Moderated concurrent breakout groups consisting of 12–18 participants were used to collect responses to the same semi-structured questionnaire. Transcripts of each recorded session were qualitatively analyzed by individual team members and then validated in pairs to ensure consistent outcomes were identified. More specifically, the process included researchers independently reviewing the transcripts to identify emergent themes and key issues. The researchers then paired up to discuss and arrive at consensus on the identified themes. The analysis and interpretation of themes were done with examples of emergency management policies from the Gulf coast and eastern seaboard as well as COVID-19 and disaster response literature related to economic, health, and social impact. Descriptive quotes were selected to illustrate participants’ perspectives related to major themes but to maintain confidentiality these quotes are not associated with any participant information.
7. Results and discussion
This section presents the key issues raised by workshop participants. First, we explore emergent themes from the workshops associated with: (1) which vulnerable populations should be considered in evacuation and shelter planning during the 2020 hurricane season and concurrent COVID-19 pandemic, and (2) what strategies are being considered to adapt evacuation and shelter operations to meet the potentially altered demand. The changes expressed by participants are contextualized using relationships shown in Fig. 1 between the vulnerability literature and emergent research on COVID-19. Second, we discuss the implications of and capacity for pursuing the participant's recommendations for expanding vulnerability assessment prior to evacuation and sheltering in the context of emergency management policies from federal, state, and local governments. Findings indicate that pre-pandemic disaster preparation and response strategies to address traditional characteristics and groups of vulnerable populations can be adapted to accommodate populations with additional vulnerabilities associated with COVID-19 during an evacuation and sheltering situation.
7.1. Revising perspectives on vulnerability to accommodate COVID-19
Workshop participants anticipated serving populations with traditional vulnerabilities to hurricane impacts and vulnerabilities exacerbated by COVID-19 during evacuation and sheltering operations for the 2020 Atlantic hurricane season. Subpopulations considered at the start of hurricane season to be vulnerable to COVID-19 complications included evacuees and shelter staff and volunteers that are immunocompromised, elderly, pregnant, infants, or have chronic health conditions. Further, participants expected populations with financial insecurities, mental health concerns, substance abuse, and domestic violence experiences to have increased in number and severity because of COVID-19 lockdowns. Populations with COVID-19 symptoms, exposure, or positivity were a newly vulnerable population whose various characteristics of vulnerability must be addressed to protect their own health and others.
Participants noted that the role of vulnerability in decision-making varies across populations and geographic locations. Participants were concerned that individual financial strain associated with COVID-19, experiences with other recent disasters, or virus transmission fears would change behavior. Those with underlying health conditions may not go to emergency shelters. The general public may be afraid to travel outside of their community for a required evacuation and choose to go to a local public shelter instead. Populations with pets, who are disabled, or live in insecure or unsafe housing in evacuation zones would still be in need of public options despite fears of virus transmission.
These changes in vulnerability have ripple effects on evacuation and sheltering during a hurricane-pandemic. Additional resources are needed to manage the health of these vulnerable individuals and to shield other evacuees, shelter staff, and shelter volunteers from being infected. Populations with underlying medical conditions that may not pose challenges for evacuation and sheltering during typical hurricane conditions may have increased risk to the virus, which may change their overall perceptions of risk and affect how they respond to a hurricane in the midst of a pandemic.
In terms of vulnerabilities associated with economic or financial impacts of COVID-19, participants noted the increase in individuals who experience reduced work hours or job loss because of business and operational restrictions associated with efforts to manage virus contagion. These individuals will have fewer resources to cope with a hurricane, may not be able to evacuate, and thus more likely to shelter at home, which puts them at physical risk, or go to an emergency shelter which may expose them to the virus.
Healthcare availability as a whole, and disproportionate access to healthcare more specifically, were areas of concern. Factors such as socioeconomic status and location affect one's ability to access and maintain care during the pandemic. Many individuals faced financial strain prior to the pandemic, and for many at the lower income range, this strain has increased with the COVID-19 pandemic, and without health insurance they may be unable to afford healthcare. This could result in persons not receiving critical care or being tested or treated for COVID-19. Additionally, location is an ongoing issue that may be exacerbated by the pandemic. Participants stated that it can be difficult to communicate with those in rural communities prior to any hazard event. Access to healthcare is also limited in rural areas regardless of the presence of a pandemic. Those without transportation in impoverished communities may also regularly have difficulty accessing care. Due to the pandemic, many medical providers have limited their care to emergencies and participants expressed concern that the encouragement for social distancing may deter people from seeking care for fear of contracting COVID-19, thus potentially having a negative impact on community health.
7.2. Strategies considered to address shifting vulnerabilities
Enhanced communication strategies would improve evacuee understanding of how evacuation and sheltering processes are being planned to account for shifting inequities in health and economic resources during a compound hurricane-pandemic event. Participants proposed a stronger approach to overall outreach. States with existing registries were encouraged to notify participating populations early to ensure evacuation plans are communicated prior to an evacuation event occurring. Resiliency hubs1 in churches and community centers like those available throughout the City of Baltimore, Maryland, were suggested as locations where information could be disseminated to marginalized groups, especially those experiencing social stigma related to the pandemic, such as Asian American populations.
Emergency managers reported planning to accommodate the same population as projected with existing models. Participants raised the concern that, given the compound threat of the COVID-19 pandemic and an impending hurricane, additional time and resources would be needed to ensure the well-being of staff and evacuees. Public shelter options and consequently the ability to socially distance become more limited as the hurricane risk increases. One participant stated that emergency managers faced the dilemma that they “Have to be prepared to make a decision for overall safety of evacuee while protecting from illness. Anything less than a Category 3, we can probably social distance, but anything larger, I don't think we have the structural stability to maintain social distancing.” A participant suggested two plans depending on the strength of the storm: (1) following Red Cross and CDC social distancing guidelines, or (2) following existing sheltering plans with social distancing to the extent possible. A triage system was also proposed by another participant who noted that resource limitations “actually overwhelms the system because we can't triage correctly ...we have to become more strategic in our thinking.” To reduce uncertainty for a specific vulnerable population, one participant suggested making sure nursing homes and adult living facilities update their emergency plans to account for COVID-19. Outside of evacuation zones, participants emphasized the importance of recommending residents in less physically vulnerable locations shelter in place, thereby reducing shadow evacuation2 that might clog non-congregate shelter options and roadways.
Congregate transportation, meals, bathrooms, and other spaces present risks that motivated participants to re-evaluate options to reduce risk for all populations. Suggested strategies included providing gift cards to support evacuation of residents with limited resources and using hotel rooms as shelters, similar to those used by the Red Cross in past evacuations and by localities to house the homeless during the pandemic. It was understood that non-congregate options would not work for everyone though, so reduced capacity transportation options and larger or better ventilated public shelters would be required for those with disabilities, pets, or in need of specialized care.
Evacuee support options were also being re-evaluated to accommodate potential increases in demand from vulnerable and sick populations. Functional Assessment Service Teams3 that are available would need to be deployed and the number of teams expanded to meet increased shelter capacity and greater access and functionality requirements. Additional personnel with medical or sanitation expertise were identified as a critical need to conduct vulnerability and illness assessments, and maintain facility hygiene. Regarding the need to address children's mental health during a hurricane-pandemic, a participant questioned “Children don't know how to cope […] where is it that we put some type of plan in place to deal with that type of stress with kids, with young people?”
The potentially expanded set of support staff was expected to benefit from practice drills as available. Given the concerns about exposure, telehealth options were being explored, but with potential hurricane-induced lapses in power and internet access, this option may fall short. Partnerships with the Medical Reserve Corps and the American Association of Retired Persons (AARP) were discussed and considered. However, recruiting retired doctors and nurses as volunteers was not advisable due to their own age-related vulnerability to the virus.
Participants called for increased information sharing to identify and accommodate virus-related vulnerabilities. However, supply chain issues and government funding reductions brought into question the capacity to store, provide, and replenish supplies to prevent the spread of COVID-19 while accommodating needs of medically fragile populations, such as personal protective equipment, oxygen tanks, and NARCAN and other medications.
One participant suggested using the Social Vulnerability Index (SoVI, see Ref. [19] to estimate demand by populations with exacerbated vulnerabilities. SoVI and other social vulnerability indices could be used to estimate expected demand and paired with other modeling tools to provide updated information for shelter planning and operation.
Pre-registration for evacuation shelters for those with underlying conditions or existing infections as well as onsite screenings for vulnerabilities to COVID-19 complications, exposure, and symptoms were other complementary strategies identified by participants. Models for special needs shelters that already use special registries could be expanded within states or adopted in other states. One participant provided an example of how registries facilitate resource allocation: “Prescreening is critical to understanding. So, the medically vulnerable may use Oxygen or nebulizers. There [is] a potential for aerosol virus particles. Using structural barriers within our regional shelters as a physical barrier plus privacy screens.” Registries and individualized care plans were also thought to facilitate the transition from shelters back to homes and the community through contact tracing and transition teams.
Participants also questioned not only how to assess shelter intake to account for resource needs and availability, but also which vulnerabilities, if any, to prioritize. Actions to isolate the populations with increased risk of complications from COVID-19 were under consideration; however, the potential for negative effects upon mental health concerned some participants. Separate shelters for individuals that tested positive for the virus was another suggestion, but this could create issues for families and caregivers. If assessment of underlying health conditions and virus testing are not possible, participants suggested that the assumption may have to be made that everyone presenting is a spreader of and at increased vulnerability to complications from the virus. Without documentation and assessment of illness and underlying conditions, all shelters would need to comply with social distancing and sanitation protocols and more shelters may need to incorporate special needs protocols, including the potential expansion of existing community registries to capture populations with underlying medical conditions.
7.3. Special registries as policy tools to support evacuation and sheltering adaptation
The Stafford Act (1988) and the Post-Katrina Emergency Management Reform Act (2006) mandate that people with disabilities should be given equal opportunity to be integrated in general population shelters. Similarly, the American Disabilities Act of 1990, the Rehabilitation Act of 1973, and the Fair Housing Act (FHA) of 1968 outline specifications for suitable sheltering sites including how to select locations that are compliant and to confirm the sites are hardened to withstand the needed environmental hazards. The Acts also describe appropriate measures that should be taken to retrofit existing locations to ensure they meet accessibility requirements [58]. These requirements for inclusion and integration are not waived during emergency evacuations and sheltering.
A special needs registry is a “list of individuals within a jurisdiction who require assistance before, during, or after an emergency” [59]; p. 1). Information in such special needs registries are voluntarily provided by residents and include contact information and any access or functional needs. Registry information can be used to help appropriately plan for and respond to emergencies, including evacuations and sheltering. While “special needs registry” is the most commonly used terminology for these registries, they have also been titled “emergency evacuation assistance registry”, “vulnerable populations registry”, and “medical needs registry” [59]. Some states such as Florida, Utah, and New Jersey have developed state-based registries that are accompanied by a consolidated set of resources dedicated to the overall sustainability of the registries, such as through maintenance and updates [60,61]. Other states (e.g., Pennsylvania, Louisiana, Virginia, North Carolina) have more localized registries administered by individual cities or counties.
Needs registries assist emergency managers in understanding their community in a more precise manner. Information in the registries may provide planners with specific and minimal resource requirements in response to an emergency. This allows planners to improve their preparedness planning and anticipate the needs of the community during an emergency. The registries provide details that planners can use to create specific community emergency plans that include information such as what durable medical equipment, consumable medical supplies, and other personal assistance may be required at general, special, or medical needs shelters, or what types of transportation will be needed to assist those without a way to evacuate on their own.
Registries may be used to inform planning. Some registries are used to provide additional benefits to those who sign up by providing additional check-ups prior to and following an emergency, thus providing assistance to individuals with no support network in the local area. Some jurisdictions use the registry to coordinate transportation assistance as well as placement into shelters based on an individual's needs and the care a shelter is able to provide. Registries are even being expanded to tie into 9-1-1 systems to provide first responders with critical information about an individual's needs before even arriving on scene of an emergency (see for example [62]. It is critical to note though, that registries require robust management and maintenance and generally do not guarantee individual assistance during a disaster or emergency. The capabilities of each jurisdiction and the participation of residents drive how the registry information is applied.
An understanding of expanded definitions of vulnerable populations can feed into identification of data needs and development of data systems that can inform planning processes and disaster response. Special needs registries can serve as a data system that can help fill this need. However, the availability of certain population-specific data, such as those included in special needs registries, vary by state, county, and even individual jurisdictions. These registries can provide a mechanism to gather voluntary information from residents directly to help inform preparedness and response planning processes, but there are limitations and obstacles that need to be overcome with the registries before they can be used to support at-risk or vulnerable populations within communities.
8. Conclusions and implications
Our findings suggest that vulnerabilities associated with underlying health conditions and socio-economic disparities are of increased concern for evacuation and sheltering during a hurricane-pandemic event. The health, economic, and social impacts of the COVID-19 pandemic add a layer of vulnerability on top of traditional hurricane vulnerability, thus broadening the definition of individuals and groups considered vulnerable. Simultaneously, the pandemic exacerbated pre-existing socioeconomic and health inequities that underpin social vulnerability (Fig. 1), making some groups much more vulnerable than others, and affecting their ability to effectively cope with the threat of a hurricane during the pandemic. For example, while low-to-moderate income households have generally been considered vulnerable because they are under-resourced in terms of being able to evacuate, the negative financial and economic impacts of the pandemic have exacerbated their vulnerability. Furthermore, certain segments of the population such as those over the age of 65, with chronic health conditions or comorbidities, and others requiring specific care during a pandemic have added complications to the definition of vulnerable populations.
Our analysis also identified the need for specific data on vulnerable populations for use in assessing vulnerability and informing planning and operations through updated data and models. Workshop participants identified special registries as a way to collect data needed to evaluate vulnerabilities and align individuals and families with appropriate resources and facilities. Our review of registries used in different states found that registries can serve as a data system to collect information that can be used to inform planning processes. These registries can serve as policy tools for supporting adaptations in evacuation and sheltering responses.
Our findings indicate that new and interdependent foci within an expanded definition of vulnerable populations regarding health and physical risk during a hurricane-pandemic scenario is needed for emergency managers, evacuation staff, and residents. Evacuation projections can then be adjusted, guidance sought for accommodating vulnerable populations from public health departments and other relevant social services organizations, and recommendations condensed into staff training materials and operations plans. Without a clear way to balance and accommodate competing needs, workshop participants had more questions than answers regarding how to address vulnerable populations going into the 2020 hurricane season.
Having now completed the 2020 hurricane season, which consistent with the forecast predictions earlier in the year proved to be an above-normal hurricane season, we can turn to planning and preparedness for other compounding events by building on knowledge learned from the previous hurricane season. For example, how do we reconcile conflicting protocols for specific hazards, like a hurricane, and pandemic management and adjust our messaging and outreach to facilitate effective response? Building connections between long-term care facility administrators and emergency management has improved the evacuation process for those who would otherwise hesitate to do so due to medical fragility and informed shelter in place protocols through combined practice drills [63,64]. These connections can be nurtured and others put in place to more effectively meet the needs of populations vulnerable to the combined risk of a pandemic and other hazards. Taking action sooner rather than later will allow an opportunity to alter emergency management plans in a way that will effectively mitigate risk for the socially vulnerable, such as those in nursing homes or long-term care facilities [65], while modifying perceived risk for vulnerable populations and, thus, encouraging those who are hesitant.
9. Limitations and future research
The workshops to support this research took place from May to June 2020. The sentiments expressed by participants reflect knowledge pre-vaccine and early on in the 2020 compound hurricane-pandemic season. Research and updates related to COVID-19 are constantly evolving and while there have been many “lessons learned” since June 2020, there is still much we do not know regarding long-term impacts and effects from the virus and how individuals will be able to cope with continued restrictions on their lives and daily movements. Our research discusses pre-existing conditions and socio-economic status and inequities but does not address the uncertainties that exist within a prolonged pandemic event and how those conditions may continue to deteriorate as we approach the next hurricane season while still under a pandemic event with potentially even more contagious new strains within our communities.
Additional research is needed to better understand the longer-term consequences of the expanded vulnerabilities brought on by the COVID-19 pandemic. For example, children are likely to suffer mental health consequences of the pandemic, the extent of these consequences have yet to be explored. The compounded mental health impacts of the pandemic on top of the fear of an impending hurricane also warrant further research. Similarly, pregnant women are disproportionately affected due to increased risk of complications from COVID-19 and the lack of research regarding the effects of COVID-19 on expecting mothers and unborn babies. How might the additional threat of a hurricane further increase the risk to pregnant women and increase their vulnerability? Finally, while most groups identified as socially vulnerable to a hurricane event will continue to be vulnerable in a situation marked by a pandemic, participants expected additional groups to be vulnerable. (i.e. substance abuse problems, experiencing domestic violence, or discrimination) and have increased numbers and severity of their vulnerabilities due to COVID-19 lockdowns and social isolation. Future research should focus on how specific policies and programs to meet the unique needs of these populations, such as domestic abuse shelters and substance abuse programs, can evolve to incorporate adaptations that address the specific hurricane evacuation needs of these populations given their enhanced vulnerabilities.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research was supported by the National Science Foundation-funded Social Science Extreme Events Research (SSEER) Network and the CONVERGE facility at the Natural Hazards Center at the University of Colorado Boulder (NSF Award #1841338). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF, SSEER, or CONVERGE.
Footnotes
Resiliency hubs are locations that are well-known to the community's residents and provide a spot for distributing supplies and other resources during an emergency event.
Shadow evacuations are voluntary evacuations of people outside of a designated evacuation zone.
A Functional Assessment Service Team (FAST) is a team of trained members that provide assistance in evaluating the access or functional needs of individuals and how their needs can be supported.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijdrr.2021.102386.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Phillips C.A., Caldas A., Cleetus R., Dahl K.A., Declet-Barreto J., Licker R.…Carlson C.J. Compound climate risks in the COVID-19 pandemic. Nat. Clim. Change. 2020;10:586–588. [Google Scholar]
- 2.Blaikie P., Cannon T., Davis I., Wisner B. Routledge; 2014. At Risk: Natural Hazards, People's Vulnerability and Disasters. [Google Scholar]
- 3.Cutter S.L., Burton C.G., Emrich C.T. Disaster resilience indicators for benchmarking baseline conditions. J. Homel. Secur. Emerg. Manag. 2010;7(1):51. [Google Scholar]
- 4.National Oceanic and Atmospheric Administration . 2020, May 21. Busy Atlantic Hurricane Season Predicted for 2020.https://www.noaa.gov/media-release/busy-atlantic-hurricane-season-predicted-for-2020 [Press release] [Google Scholar]
- 5.Shultz J.M., Fugate C., Galea S. Cascading risks of COVID-19 resurgence during an active 2020 Atlantic hurricane season. J. Am. Med. Assoc. 2020;324(10):935–936. doi: 10.1001/jama.2020.15398. [DOI] [PubMed] [Google Scholar]
- 6.Shultz J.M., Kossin J.P., Hertelendy A., Burkle F., Fugate C., Sherman R., Galea S. Mitigating the twin threats of climate-driven Atlantic hurricanes and COVID-19 transmission. Disaster Med. Public Health Prep. 2020;14(4):494–503. doi: 10.1017/dmp.2020.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pei S., Dahl K.A., Yamana T.K., Licker R., Shaman J. Compound risks of hurricane evacuation amid the COVID-19 pandemic in the United States. GeoHealth. 2020;4(12) doi: 10.1029/2020GH000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Federal Emergency Management Agency (FEMA) 2020. COVID-19 Pandemic Operational Guidance for the 2020 Hurricane Season.https://www.fema.gov/media-collection/covid-19-pandemic-operational-guidance-2020-hurricane-season [Google Scholar]
- 9.Bian R., Wilmot C.G. Measuring the vulnerability of disadvantaged populations during hurricane evacuation. Nat. Hazards. 2017;85(2):691–707. [Google Scholar]
- 10.Bowser G.C., Cutter S.L. Stay or go? Examining decision making and behavior in hurricane evacuations. Environment. 2015;57(6):28–41. [Google Scholar]
- 11.Dash N., Gladwin H. Evacuation decision making and behavioral responses: individual and household. Nat. Hazards Rev. 2007;8(3):69–77. [Google Scholar]
- 12.Huang S.-K., Lindell M.K., Prater C.S. Who leaves and who stays? A review and statistical meta-analysis of hurricane evacuation studies. Environ. Behav. 2016;48(8):991–1029. [Google Scholar]
- 13.Huang S.-K., Lindell M.K., Prater C.S., Wu H.-C., Siebeneck L.K. Household evacuation decision making in response to Hurricane Ike. Nat. Hazards Rev. 2012;13(4):283–296. [Google Scholar]
- 14.Ng M., Behr J., Diaz R. Unraveling the evacuation behavior of the medically fragile population: findings from hurricane Irene. Transport. Res. Pol. Pract. 2014;64:122–134. [Google Scholar]
- 15.Vásquez W.F., Murray T.J., Mozumder P. Understanding hurricane evacuation planning in the Northeastern and Mid-Atlantic United States. Nat. Hazards Rev. 2015;17(1) [Google Scholar]
- 16.Old Dominion University Social Science Research Center (ODU SSRC) Life in hampton roads survey: hurricanes and COVID-19. 2020. https://www.odu.edu/news/2020/8/lihr_hurricanes_and_
- 17.Birkmann J. In: Measuring Vulnerability to Natural Hazards: towards Disaster Resilient Societies. Birkmann J., editor. United Nations University Press; 2006. Measuring vulnerability to promote disaster-resilient societies: conceptual frameworks and definitions. [Google Scholar]
- 18.Chambers R. Vulnerability, coping and policy (editorial introduction) IDS Bull. 2006;37:33–40. [Google Scholar]
- 19.Cutter S.L. Vulnerability to environmental hazards. Prog. Hum. Geogr. 1996;20(4):529–539. [Google Scholar]
- 20.Dow K. Exploring differences in our common future(s): the meaning of vulnerability to global environmental change. Geoforum. 1992;23(3):417–436. [Google Scholar]
- 21.Weichselgartner J., Bertens J. Natural disasters: acts of God, nature or society? On the social relation to natural hazards. WIT Trans. Ecol. Environ. 2000;45:3–12. [Google Scholar]
- 22.United Nations . Paper Presented at the World Conference on Disaster Reduction, Kobe, Hyogo. 2005. Hyogo Framework for Action 2005-2015: building the resilience of nations and communities to disasters. [Google Scholar]
- 23.Cutter S.L., Mitchell J.T., Scott M.S. Revealing the vulnerability of people and places: a case study of Georgetown County, South Carolina. Ann. Assoc. Am. Geogr. 2000;90(4):713–737. [Google Scholar]
- 24.Wu S.-Y., Yarnal B., Fisher A. Vulnerability of coastal communities to sea-level rise: a case study of Cape May County, New Jersey, USA. Clim. Res. 2002;22(3):255–270. [Google Scholar]
- 25.Birkmann J. Risk and vulnerability indicators at different scales: applicability, usefulness and policy implications. Environ. Hazards. 2007;7(1):20–31. [Google Scholar]
- 26.Benson C. In: Mapping Vulnerability: Disasters, Development and People. Bankoff G., Frerks G., Hilhorst D., editors. Routledge; 2004. Macro-economic concepts of vulnerability: dynamics, complexity and public policy. [Google Scholar]
- 27.Hilhorst D., Bankoff G. In: Mapping Vulnerability: Disasters, Development and People. Bankoff G., Frerks G., Hilhorst D., editors. Routledge; 2004. Introduction: mapping vulnerability. [Google Scholar]
- 28.Cutter S.L., Boruff B.J., Shirley W.L. Social vulnerability to environmental hazards. Soc. Sci. Q. 2003;84(2):242–261. [Google Scholar]
- 29.Weichselgartner J. Disaster mitigation: the concept of vulnerability revisited. Disaster Prev. Manag. 2001;10(2):85–95. [Google Scholar]
- 30.Vink K., Takeuchi K., Kibler K.M. A quantitative estimate of vulnerable people and evaluation of flood evacuation policy. J. Disaster Res. 2014;9(5):887–900. [Google Scholar]
- 31.McLeod J.D., Kessler R.C. Socioeconomic status differences in vulnerability to undesirable life events. J. Health Soc. Behav. 1990;31(2):162–172. [PubMed] [Google Scholar]
- 32.Smith N., Fraser M. Straining the system: novel coronavirus (COVID-19) and preparedness for concomitant disasters. Am. J. Publ. Health. 2020;110(5):648–649. doi: 10.2105/AJPH.2020.305618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Comfort L., Wisner B., Cutter S., Pulwarty R., Hewitt K., Oliver-Smith A., Krimgold F. Reframing disaster policy: the global evolution of vulnerable communities. Environ. Hazards. 1999;1(1):39–44. [Google Scholar]
- 34.Karaye I.M., Thompson C., Horney J.A. Evacuation shelter deficits for socially vulnerable Texas residents during Hurricane Harvey. Health Services Research and Managerial Epidemiology. 2019;6 doi: 10.1177/2333392819848885. 2333392819848885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kako M., Steenkamp M., Ryan B., Arbon P., Takada Y. Best practice for evacuation centres accommodating vulnerable populations: a literature review. International Journal of Disaster Risk Reduction. 2020;46:101497. [Google Scholar]
- 36.Ng M., Diaz R., Behr J. Departure time choice behavior for hurricane evacuation planning: the case of the understudied medically fragile population. Transport. Res. E Logist. Transport. Rev. 2015;77:215–226. [Google Scholar]
- 37.Alexander D., Gaillard J.C., Wisner B. In: The Routledge Handbook of Hazards and Disaster Risk Reduction. first ed. Wisner B., Gaillard J.C., Kelman I., editors. Routledge; New York: 2012. Disability and disaster. [Google Scholar]
- 38.Heath S.E., Kass P.H., Beck A.M., Glickman L.T. Human and pet-related risk factors for household evacuation failure during a natural disaster. Am. J. Epidemiol. 2001;153(7):659–665. doi: 10.1093/aje/153.7.659. [DOI] [PubMed] [Google Scholar]
- 39.U.S. Department of Homeland Security Planning considerations: evacuation and shelter in place. guidance for state, local, tribal and territorial partners. 2019. https://www.fema.gov/sites/default/files/2020-07/planning-considerations-evacuation-and-shelter-in-place.pdf
- 40.Alcántara-Ayala I., Burton I., Lavell A., Mansilla E., Maskrey A., Oliver-Smith A., Ramírez-Gómez F. Editorial: root causes and policy dilemmas of the COVID-19 pandemic global disaster. International Journal of Disaster Risk Reduction. 2021;52:101892. doi: 10.1016/j.ijdrr.2020.101892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yusuf J., Hill S., Feo E.L., Whytlaw J.L., Richardson T. The compound threat of COVID-19 and hazards: public management and policy issues from a stakeholder perspective. International Journal of Policy Studies. 2020;11(2):149–181. [Google Scholar]
- 42.Blumenshine P., Reingold A., Egerter S., Mockenhaupt R., Braveman P., Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg. Infect. Dis. 2008;14(5):709–715. doi: 10.3201/eid1405.071301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bouye K., Truman B.I., Hutchins S., Richard R., Brown C., Guillory J.A., Rashid J. Pandemic influenza preparedness and response among public-housing residents, single-parent families, and low-income populations. Am. J. Publ. Health. 2009;99(S2):S287–S293. doi: 10.2105/AJPH.2009.165134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deslatte A., Hatch M.E., Stokan E. How can local governments address pandemic inequities? Publ. Adm. Rev. 2020;80(5):827–831. doi: 10.1111/puar.13257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dasgupta S., Bowen V.B., Leidner A., Fletcher K., Musial T., Rose C., Oster A.M. Association between social vulnerability and a county's risk for becoming a COVID-19 Hotspot - United States, June 1-July 25, 2020. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69(42):1535–1541. doi: 10.15585/mmwr.mm6942a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with covid-19. N. Engl. J. Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C., Sullivan P.S. Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Correa-Agudelo E., Mersha T.B., Branscum A.J., MacKinnon N.J., Cuadros D.F. Identification of vulnerable populations and areas at higher risk of COVID-19-related mortality during the early stage of the epidemic in the United States. Int. J. Environ. Res. Publ. Health. 2021;18(8) doi: 10.3390/ijerph18084021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.CDC . 2020. Health Equity Considerations and Racial and Ethnic Minority Groups.https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html#fn19 July 24, 2020. [Google Scholar]
- 50.Dai M., Liu D., Liu M., Zhou F., Li G., Chen Z., Zhang Z., You H., Wu M., Zheng Q. Patients with cancer appear more vulnerable to SARS-COV-2: a multicenter study during the COVID-19 outbreak. Canc. Discov. 2020;10(6):783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. J. Am. Med. Assoc. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hamilton R. Scarcity and coronavirus. J. Publ. Pol. Market. 2020;40(1):99–100. [Google Scholar]
- 53.Gray D.M., II, Anyane-Yeboa A., Balzora S., Issaka R.B., May F.P. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat. Rev. Gastroenterol. Hepatol. 2020;17(9):520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Snyder B.F., Parks V. Spatial variation in socio-ecological vulnerability to Covid-19 in the contiguous United States. Health Place. 2020;66:102471. doi: 10.1016/j.healthplace.2020.102471. [DOI] [PubMed] [Google Scholar]
- 55.Woolhandler S., Himmelstein D.U. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann. Intern. Med. 2020;173(1):63–64. doi: 10.7326/M20-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015;41:311–330. [Google Scholar]
- 57.Sabin D.J.A., Nosek D.B.A., Greenwald D.A.G., Rivara D.F.P. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J. Health Care Poor Underserved. 2009;20(3):896. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.United States Department of Health and Human Services (USDHHS) FEMA's functional needs support services guidance. 2020. https://www.phe.gov/Preparedness/planning/abc/Pages/functional-needs.aspx
- 59.Federal Emergency Management Agency (FEMA) Best practice: special needs registries - overview of registry issues. Lessons learned information sharing (LLIS) 2011. https://www.hsdl.org/?view&did=765518
- 60.Utah Special Needs Registry Welcome to Utah's special needs registry. 2020. https://specialneedsutah.org/
- 61.NJ Register Ready Register Ready – New Jersey's special needs registry for disasters. 2019. https://www13.state.nj.us/SpecialNeeds/
- 62.City of Danville Heads up! Special needs registry. 2020. https://www.danville-va.gov/390/Heads-Up-Special-Needs-Registry
- 63.Hyer K. For long-term care, readiness gaps abound. Health Prog. 2013;94(6):43–49. [PubMed] [Google Scholar]
- 64.Whytlaw J.L. Regional planning efforts encourage coordination between senior care facilities and emergency managers in New Jersey. Journal of Emergency Management. 2020;18(5):373–382. doi: 10.5055/jem.2020.0486. [DOI] [PubMed] [Google Scholar]
- 65.Hutton N.S., Allen M.J. Challenges in upgrading emergency power in Florida nursing homes following Hurricane Irma. Weather, Climate, and Society. 2020;12(4):805–814. [Google Scholar]
- 66.Turner B.L., II, Kasperson R.E., Matson P.A., McCarthy J.J., Corell R.W., Christensen C., Schiller A. A framework for vulnerability analysis in sustainability science. Proc. Natl. Acad. Sci. U.S.A. 2003;100(14):8074–8079. doi: 10.1073/pnas.1231335100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liverman Diane, R.E. Kasperson . In: Understanding Global Environmental Change. Kasperson Roger., E, editor. Vol. 26. Clark University; 1990. Vulnerability to Global environmental change; pp. 27–44. [Google Scholar]
- 68.Allinovia Luca, Mane Erdgin, Romano Donato. Measuring household resilience to food insecurity: application to Palestinian households. EC-FAO Food Security Programme Rom. 2009:1–39. [Google Scholar]
- 69.2003. https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/4011
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.