A 29-year-old housewife presented with acute onset bilateral lower limb weakness and urinary retention for 2 days. She had a history of fever and running nose 2 days before the weakness. She had no other significant past medical history. Examination showed grade 4/5 power in lower limbs with normal power in upper limbs, exaggerated deep tendon jerks bilaterally over lower limbs, bilateral extensor plantar, and dissociated sensory loss below T6 (loss of pain and temperature with preserved dorsal column sensations). Fundoscopy was normal. The rest of the systemic examination was unremarkable.
Biochemical parameters including electrolytes, renal function tests, liver function tests, and blood counts were normal. Magnetic resonance imaging of the spine showed bilateral round high signal intensity lesions involving anterior horn cells on axial T2-weighted images (T2-WIs). Sagittal T2-WIs showed thin T2 high signal intensity lesions involving the T2-T10 segments without contrast enhancement Figure 1. Brain imaging was normal. Cerebrospinal fluid analysis showed elevated protein (126 mg/dL), the cell count was normal, and the oligoclonal bands were negative. Serum anti-aquaporin 4 antibody was negative and anti-myelin oligodendrocyte glycoprotein immunoglobulin G (anti-MOG IgG) antibody was positive in the serum and cerebrospinal fluid. Autoimmune and infective workups were negative. She was diagnosed to have MOG antibody-positive myelitis and was managed with high-dose steroids (methylprednisolone 1 g daily intravenously) for 5 days with which she improved clinically. She did not have any recurrence of the disease during a follow-up of 1 year. Isolated involvement of the spinal cord in anti-MOG syndrome can mimic spinal cord infarction. Owl-eye appearance in axial T2-WI of the spine can be due to cord infarction, cord contusion, compressive myelopathy, and infectious (poliomyelitis or enterovirus) or inflammatory conditions. Spinal cord gray matter T2 hyperintensity in anti-MOG syndrome may be due to the presence of oligodendrocytes containing MOG in the spinal cord gray matter. MOG myelitis can involve both gray matter and central white matter. It can cause either longitudinally extensive spinal cord lesions or T2-hyperintense short lesions. “H” sign on axial view and sagittal line hyperintensity surrounded by a cloudier T2-hyperintense signal on sagittal view is due to the involvement of gray matter. Leptomeningeal enhancement in MOG myelitis can help differentiate it from neuromyelitis optica spectrum disorder (NMOSD) and multiple sclerosis. This case reminds the readers to be aware of the anti-MOG syndrome in the differential diagnosis of spinal cord infarction.
Figure 1.
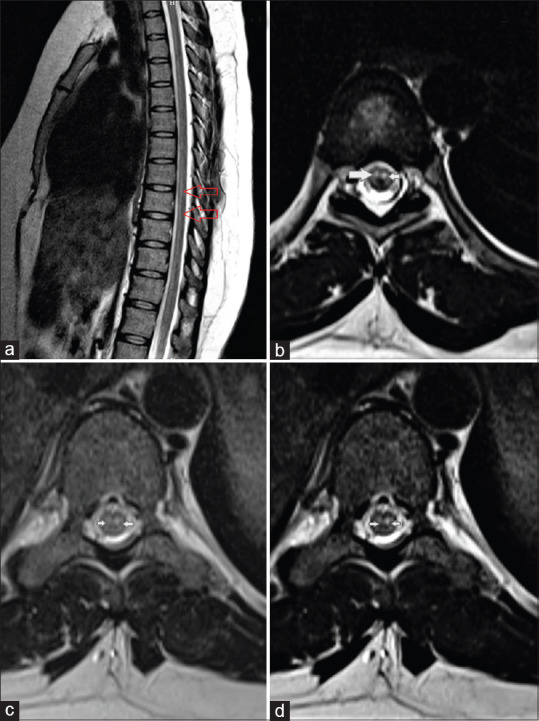
Magnetic resonance imaging of the spine showing “owl-eye appearance” (bilateral round high signal intensity lesions involving anterior horn cells on axial T2-weighted images) (b-d). Sagittal T2-weighted images showing thin T2 high signal intensity lesions involving the T2-T10 segments (a)
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.


