There has understandably been widespread concern about the impact of the COVID-19 pandemic and associated restrictions on the mental health of children and young people, with evidence of recent increases in the prevalence of mental health problems.1 Yet there has been relatively little evaluation of how mental health has changed over the pandemic and varied for children and young people living in a range of circumstances. One exception is the Co-SPACE study, a UK-based longitudinal online survey of parents and carers of children and adolescents aged 4–16 years, and adolescents aged 11–16 years, who have been invited to participate monthly since the fifth day of the UK's first national lockdown in March, 2020. Co-SPACE has now run for over a year, and more than 8700 families have provided data using the well validated Strengths and Difficulties Questionnaire (SDQ).2 As the study uses convenience sampling and does not have pre-pandemic data, it cannot answer how the pandemic affected the prevalence of mental health problems. Nevertheless, the collection of monthly data from a population with diverse social and demographic backgrounds provides a unique opportunity to examine how things have changed over time throughout the pandemic, and, crucially, for whom.
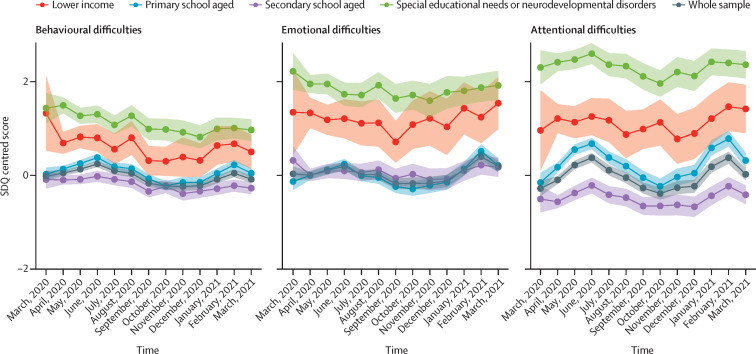
Between March, 2020, and March, 2021, we have seen clear increases in parent-reported symptoms of SDQ behavioural and attentional difficulties at times of peak restrictions, when most children were not physically attending school (figure ).3 These symptoms increased throughout the first national lockdown (March–June, 2020), decreased and stabilised as restrictions eased, increased again from January, 2021, when a further national lockdown was introduced, and then decreased again when most children returned to school in March, 2021. Average adolescent self-reported SDQ symptoms across all examined domains (behavioural, attentional, and emotional), and parent-reported emotional symptoms, were fairly stable over time; however, the highest levels of both parent-reported and adolescent-reported symptoms were when high levels of restrictions were in place and schools were closed to most children.3
Figure.
Changes in parent-reported child mental health difficulties (using the SDQ) in the UK Co-SPACE sample, from March, 2020, to March, 2021
Each SDQ subscale score is grand mean centred. The overall Co-SPACE sample consists of 8752 families (905 [10·3%] on lower income, 5443 [62·2%] with primary school aged (4–10 years) children, 3309 [37·8%] with secondary school aged (11–16 years) children, and 1547 [17·7%] with children with special educational needs or neurodevelopmental disorders). SDQ=Strengths and Difficulties Questionnaire.
Strikingly, we have seen greater changes in parent-reported SDQ mental health symptoms (in line with pandemic-related restrictions) among pre-adolescent children (aged 4–10 years), but a more stable pattern among adolescents (11–16 years).3 This finding needs further exploring; however, two potential contributing factors are isolation from peers and family stress. Notably, the majority of pre-adolescents (but not adolescents) were reported by parents to be cut off from their peers at times of peak restrictions.4 Stress (assessed with the Depression Anxiety and Stress Scale—21 items5) has also been particularly high among parents of pre-adolescents when restrictions have been high.6 At these times, many parents were juggling home schooling with work demands and domestic commitments, and more than 60% of parents in the Co-SPACE study reported that they did not feel able to meet the needs of both their child and their work.6 Notably, but unsurprisingly, parental stress was particularly high among single-adult households, among low-income families, and where children had special educational needs or neurodevelopmental disorders.6 These findings are certainly a cause for concern given the known associations between parental stress, negative family environments, and adverse child outcomes.7
Other clear patterns include the very high levels of parent-reported SDQ mental health symptoms among children and young people with special educational needs or neurodevelopmental disorders and those living on low family incomes throughout the pandemic. The strong association between these factors and poor mental health was evident well before the pandemic8, 9 so the elevated symptoms might not be surprising. However, it is particularly concerning that, although we saw overall improvements in parent-reported SDQ mental health symptoms in March, 2021, as restrictions eased, parents of children with special educational needs or neurodevelopmental disorders and in low-income families continued to report high levels of symptoms.
The Co-SPACE findings complement others, such as the UK National Health Service digital survey, which reported an increased prevalence in mental health problems in July, 2020, compared with 2017, particularly for attentional difficulties among younger boys (aged 5–10 years), and with high rates among families that were struggling financially.1 The fairly stable pattern that we found for parent-reported and adolescent-reported emotional symptoms was also consistent with a school-based longitudinal study10 that assessed self-reported anxiety and wellbeing among children and adolescents aged 6–18 years in England between May and November, 2020. Although notably, in that study, average youth self-reported wellbeing was highest during the first national lockdown when most children were not in school, highlighting the need to now examine what accounts for variability in individuals' mental health experiences during the pandemic.
Ultimately, the learnings from the Co-SPACE study are mostly not new. Economic hardship, special educational needs and neurodevelopmental disorders, parental stress, and child and adolescent mental health are closely related. However, the disruption caused by the pandemic has put these risks for child and adolescent mental health in stark relief. Our findings that some groups of children appear to be less likely to bounce back as restrictions have eased brings further cause for concern. The ongoing effects of the pandemic, particularly for the most disadvantaged, underscore the importance of recognising and meeting the support needs of children and families to ensure that inequalities are not widened further and children are given the opportunity to reach their full potential.
This research was funded by the UK Research and Innovation and the Westminster Foundation. PW is funded by a UK National Institute for Health Research (NIHR) Postdoctoral Research Fellowship (PDF-2016-09-092). CC is supported by the NIHR Oxford and Thames Valley Applied Research Collaboration. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care.
References
- 1.Vizard T, Sadler K, Ford T, et al. Mental health of children and young people in England 2020. Wave 1 follow-up to the 2017 survey. Oct 22, 2020. https://files.digital.nhs.uk/AF/AECD6B/mhcyp_2020_rep_v2.pdf
- 2.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psycho Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 3.Shum A, Skripkauskaite S, Pearcey S, Waite P, Creswell C. Report 10: children and adolescents' mental health: one year in the pandemic. May 5, 2021. https://cospaceoxford.org/findings/report-10-changes-in-childrens-mental-health-throughout-one-year-of-the-covid-19-pandemic/
- 4.Pearcey S, Raw J, Shum A, Waite P, Creswell C. Supplementary report 07: regular communication with friends outside the household during full lockdown and in the following months when restrictions were eased. Sept 23, 2020. http://cospaceoxford.org/wp-content/uploads/2020/10/Co-SPACE-supplementary-report-07-DfE.pdf
- 5.Lovibond SH, Lovibond PF. 2nd edn. Psychology Foundation; Sydney: 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- 6.Shum A, Skripkauskaite S, Pearcey S, Waite P, Creswell C. Report 09: update on children's & parents/carers' mental health; Changes in parents/carers' ability to balance childcare and work: March 2020 to February 2021. March 8, 2021. https://cospaceoxford.org/findings/changes-in-parents-carers-ability-to-balance-childcare-and-work-march-2020-to-february-2021/
- 7.Stith SM, Liu T, Davies LC, et al. Risk factors in child maltreatment: a meta-analytic review of the literature. Aggress Violent Behav. 2009;14:13–29. [Google Scholar]
- 8.Wickham S, Whitehead M, Taylor-Robinson D, Barr B. The effect of a transition into poverty on child and maternal mental health: a longitudinal analysis of the UK Millennium Cohort Study. Lancet Public Health. 2017;2:e141–e148. doi: 10.1016/S2468-2667(17)30011-7. [DOI] [PubMed] [Google Scholar]
- 9.Gadeyne E, Ghesquière P, Onghena P. Psychosocial functioning of young children with learning problems. J Child Psychol Psychiatry. 2004;45:510–521. doi: 10.1111/j.1469-7610.2004.00241.x. [DOI] [PubMed] [Google Scholar]
- 10.ImpactEd Lockdown lessons: pupil learning and wellbeing during the Covid-19 pandemic. February, 2021. https://impacted.org.uk/covid-19