ABSTRACT
Airborne transmission in ferrets is a key component of pandemic risk assessment. However, some emerging avian influenza viruses transmit between ferrets but do not spread in humans. Therefore, we evaluated sequential rounds of airborne transmission as an approach to enhance the predictive accuracy of the ferret model. We reasoned that infection of ferrets via the respiratory route and onward transmission would more closely model transmission in humans. We hypothesized that pandemic and seasonal viruses would transmit efficiently over two rounds of transmission, while emerging avian viruses would fail to transmit in a second round. The 2009 pandemic H1N1 (pdm09) and seasonal H3N2 viruses were compared to avian-origin H7N9 and H3N8 viruses. Depending on the virus strain, transmission efficiency varied from 50 to 100% during the first round of transmission; the efficiency for each virus did not change during the second round, and viral replication kinetics in both rounds of transmission were similar. Both the H1N1pdm09 and H7N9 viruses acquired specific mutations during sequential transmission, while the H3N2 and H3N8 viruses did not; however, a global analysis of host-adaptive mutations revealed that minimal changes were associated with transmission of H1N1 and H3N2 viruses, while a greater number of changes occurred in the avian H3N8 and H7N9 viruses. Thus, influenza viruses that transmit in ferrets maintain their transmission efficiency through serial rounds of transmission. This answers the question of whether ferrets can propagate viruses through more than one round of airborne transmission and emphasizes that transmission in ferrets is necessary but not sufficient to infer transmissibility in humans.
KEYWORDS: airborne transmission, ferret model, influenza, pandemic risk assessment
INTRODUCTION
The continued emergence of zoonotic influenza viruses (e.g., H7N9, H10N8, and H5N1 subtypes) in humans underscores the need for tools to assess their pandemic potential. A key requirement for the emergence of a pandemic influenza virus is the ability to spread from person to person via the airborne route (1–3). Ferrets are a suitable animal model to assess the transmissibility of emerging influenza viruses because they exhibit clinical signs upon influenza infection (4), they have sialic acid distribution in the respiratory tract that is similar to humans (5–7), and, importantly, pandemic and seasonal human influenza viruses transmit efficiently by the airborne route to 75 to 100% of contact ferrets (8–11). Both the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) have developed influenza risk assessment tools Infuenza Risk Assessment Tool IIRAT and Tool for Influenza Pandemic Risk Assessment, respectively that include airborne transmission between experimental animals as 1 of the 9 or 10 factors used to gauge the potential for a virus to initiate a pandemic (12, 13). In animal models, airborne or respiratory droplet transmission encompasses transmission by large particles, aerosols, and droplet nuclei (particles shrunken by evaporation), as these modes of transmission cannot be readily separated. In ferrets, airborne transmission is often evaluated in 3 or 4 pairs of ferrets (10, 14–18), and one animal in each pair is intranasally inoculated with ~106 infectious units of virus. Twenty-four hours later, the directly inoculated (DI) ferret and a naive respiratory contact (RC) ferret are introduced into a modified cage that allows air exchange but prevents physical contact between the animals. Transmission is assessed by detection of virus in nasal washes from the DI and RC animals over the course of 10 to 14 days, with or without serologic confirmation of infection.
In 2013, following the emergence in humans of avian influenza H7N9 viruses in China, the airborne transmissibility of these viruses was evaluated in ferrets. Transmission efficiency was between 33 and 50%, with one report of 100% transmission for the A/Anhui/1/2013 (H7N9) isolate (18–23); however, over five successive epidemic waves in humans from 2013 to 2017, H7N9 viruses did not spread in humans (24). In addition, avian influenza viruses of the H3N8 and H9N2 subtypes (25, 26) have been shown to transmit in ferrets but have not infected or transmitted between humans. To define the relationship between transmission in ferrets and humans, aggregate analyses have shown that experiments by a single research group are not sufficient to infer transmissibility in humans; only combined analyses of multiple studies from several research groups can be used to infer the potential for transmission in humans (27, 28).
In the ferret airborne transmission model, investigators evaluate the ability of an influenza virus to transmit to an RC from a DI ferret inoculated with a high dose of virus via intranasal inoculation under anesthesia. Recognizing that this approach does not model airborne transmission in humans, as neither the dose nor route of inoculation is physiological, we sought to determine whether ferrets infected by respiratory contact could transmit influenza viruses through the air to a naive host. We pursued these studies with the goal of enhancing the accuracy of the ferret model for predicting transmission in humans. We hypothesized that human influenza viruses would transmit efficiently over two sequential rounds of respiratory transmission in ferrets, while emerging avian influenza viruses would fail to sustain transmission. To our surprise, we found that transmission efficiency of the human and avian influenza viruses did not change over two rounds of transmission, and the viral replication kinetics over two rounds of transmission remained similar. Thus, infection by respiratory contact did not affect transmissibility in ferrets, and the additional round of transmission did not distinguish between viruses that did or did not transmit in humans. Importantly, these studies answer the fundamental question of whether ferrets infected by respiratory droplet could further propagate viruses by airborne transmission. Sequence analysis of viruses recovered from ferrets revealed that both the A/California/07/2009 (H1N1pdm09) and H7N9 viruses acquired specific mutations during sequential transmission, while the H3N2 and H3N8 viruses did not acquire mutations; however, a global analysis of host-adaptive mutations showed that minimal changes were required in the H1N1 and H3N2 viruses for transmission, while transmission of the avian H3N8 and H7N9 viruses was associated with a greater number of changes.
RESULTS
Pandemic H1N1 and avian H7N9 influenza viruses transmit over two rounds of respiratory contact in ferrets.
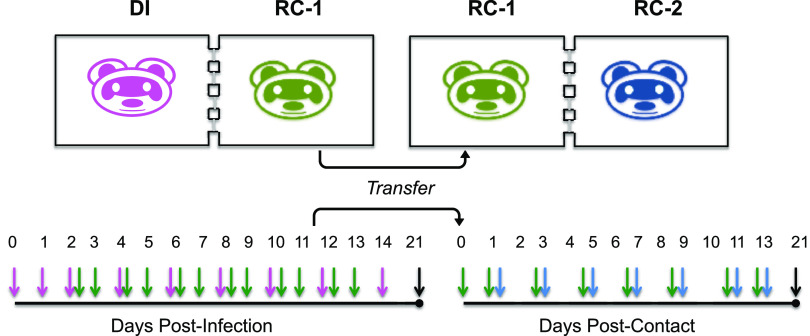
We modified our traditional experimental design (16) to evaluate whether influenza viruses were capable of two sequential respiratory transmission events in ferrets (Fig. 1). Six DI ferrets were infected with 106 50% tissue culture infective dose (TCID50) of each virus, and 24 h later, RC animals (RC1) were introduced. Nasal washes were collected daily from the RC1 ferrets, and the samples were assayed for influenza virus by antigen test strip and/or quantitative M gene reverse-transcription PCR (RT-PCR). When the RC1 ferret became infected, it was moved to a new transmission cage and became the donor ferret for a second RC (RC2) animal.
FIG 1.
Experimental design for two sequential rounds of respiratory transmission. Six ferrets were directly inoculated (DI) with 1 × 106 TCID50 of virus in a 1-mL inoculum delivered intranasally under 5% isoflurane anesthesia. Twenty-four hours later, each DI ferret was introduced into a transmission cage with a naive respiratory contact ferret (RC1). Nasal wash samples were collected daily from the RC1 ferrets and were assayed for viral antigen by test strip (FluDETECT, Zoetis) or viral RNA (M gene, quantitative reverse-transcriptase PCR [qRT-PCR], CT < 35). Once the RC1 ferret was positive by either test, this animal was moved to a new transmission cage and housed with a second naive respiratory contact (RC2). Nasal wash samples were collected from these animals on day 1 postcontact and every other day for 14 days. On day 21 postinfection for the DI ferrets and day 21 postcontact for RC1 and RC2 ferrets, terminal blood draws were performed, and the sera were assayed for antibodies via hemagglutination inhibition assay (HI) and microneutralization assay (MN). At the completion of the study, all nasal wash samples were titrated on MDCK cells. Magenta, green, and blue arrows denote the days nasal wash samples were collected from the DI, RC1, and RC2 ferrets, respectively. Black arrows denote days of terminal blood collection.
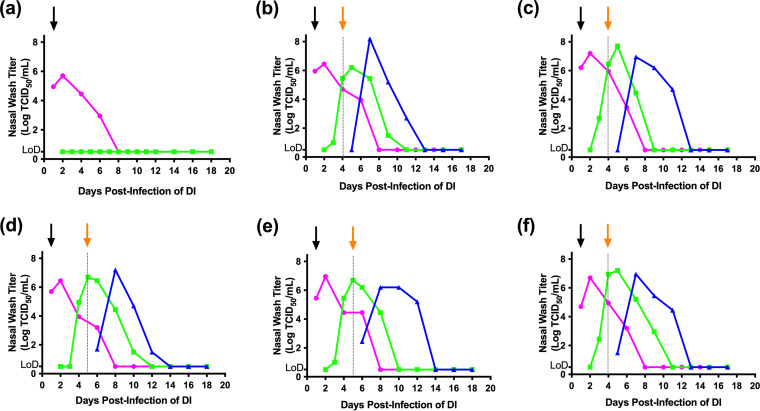
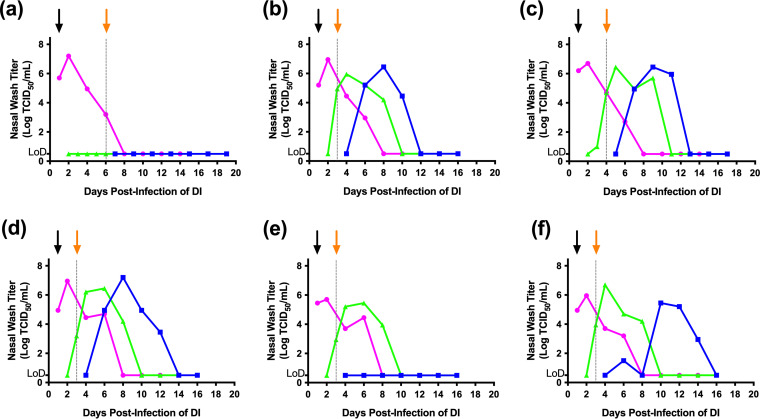
We selected a representative 2009 pandemic H1N1 virus, A/California/07/2009 (H1N1pdm09), for the initial study because this virus is highly transmissible in humans and ferrets (8, 16, 27–31). As shown in Fig. 2, H1N1pdm09 was shed at a high titer (≥106 TCID50/mL of nasal wash) from all of the DI animals and transmitted to 5 of 6 RC1 ferrets, as determined by detection of infectious virus in the nasal wash samples. When the 5 RC1 ferrets were introduced into transmission cages with RC2 ferrets, all 5 RC2 animals became infected and shed virus.
FIG 2.
Transmission of A/California/07/2009 (H1N1pdm09) over two sequential rounds of respiratory contact. Six directly inoculated (DI) ferrets were intranasally infected with 1 × 106 TCID50 of A/California/07/2009 (pH1N1) in a 1-mL volume. Twenty-four hours later, each DI animal was introduced into a transmission cage with a naive respiratory contact (RC1) ferret. Nasal wash samples were collected and assayed for evidence of viral infection, as described in Fig. 1. When the RC1 ferret became infected, it was housed with a new respiratory contact (RC2). Each panel (a to f) represents an independent replicate of DI, RC1, and RC2 (if RC1 became positive). Magenta, green, and blue lines represent the nasal wash titers for the DI, RC1, and RC2 ferrets, respectively. The black arrow denotes the day that the DI and RC1 were paired, and the orange arrow and dashed line indicate when the RC1 and RC2 ferrets were paired. Nasal wash samples were titrated on MDCK cells, and the results are expressed as log10 TCID50/mL of nasal wash. LoD denotes the limit of detection (0.5 × log [TCID50/mL]).
Virus replication was detected in 4 of the 5 RC1 animals by 2 days postcontact (dpc) and by 3 dpc in the remaining ferret; these time points correspond to day 3 or 4 postinfection of DI animals, respectively. Similarly, virus shedding was detected in 3 RC2 ferrets by 1 dpc, and all 5 RC2 ferrets shed virus by 3 dpc. Viral titers were comparable in the DI, RC1, and RC2 ferrets. All 6 of the RC1 ferrets developed hemagglutination inhibition (HI) and neutralizing antibody responses (Table 1 and Table S1 in the supplemental material), indicating that all 6 RC1 ferrets were infected during the first round of respiratory transmission, although we did not detect virus in the nasal washes from one animal. Antibody titers in this animal were greater than 8-fold lower than the other RC1 animals (Table S1), consistent with a low viral load. During the second round of transmission, all 5 of the RC2 animals developed an antibody response. Collectively, these findings demonstrated the H1N1pdm09 virus was capable of establishing an infection and transmitting onward when ferrets were infected by respiratory droplet.
TABLE 1.
Proportion of DI, RC1, and RC2 ferrets infected determined by virus isolation, hemagglutination inhibition, and neutralization assays
| Virus | No. of animals with evidence of infection/total by different assaysa,b |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DI |
RC1 |
RC2 |
||||||||||
| Viral shedding | HI assay | MN assay | Proportion of virus-positive animalsb | Viral shedding | HI assay | MN assay | Proportion of virus-positive animalsb | Viral shedding | HI assay | MN assay | Proportion of virus-positive animalsb | |
| H1N1pdm09 | 6/6 | 6/6 | 6/6 | 6/6 (100%) | 5/6 | 6/6 | 6/6 | 6/6 (100%) | 5/5 | 5/5 | 5/5 | 5/5 (100%) |
| H7N9 | 6/6 | 6/6 | 6/6 | 6/6 (100%) | 3/6 | 5/6 | 4/6 | 4/6 (66%)b | 2/3 | 2/3 | 2/3 | 2/3 (66%) |
| H3N2c | 5/5 | 5/5 | 5/5 | 5/5 (100%) | 4/5 | 4/5 | 4/5 | 4/5 (80%) | 3/4 | 3/4 | 3/4 | 3/4 (75%) |
| H3N8 | 6/6 | 6/6 | 6/6 | 6/6 (100%) | 5/6 | 5/6 | 5/6 | 5/6 (83%) | 4/5 | 4/5 | 4/5 | 4/5 (80%) |
This table excludes all RC2 animals that were introduced to RC1 animals that did not shed virus in their nasal washes.
Animals were considered positive for virus infection if they shed virus and/or were both hemagglutination inhibition (HI) and microneutralization assay (MN) positive. HI and MN positive were indicated by a reciprocal titer greater than 10 (see Table S1 in the supplemental material for results).
For the studies with A/Texas/50/2012 (H3N2), one RC1 ferret was false positive by antigen test strip. Thus, one replicate was removed from the analysis, and the proportions represent the 5 replicates.
Hemagglutination inhibition, neutralization assay, and viral shedding results for all experiments. Download Table S1, PDF file, 0.1 MB (75.6KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
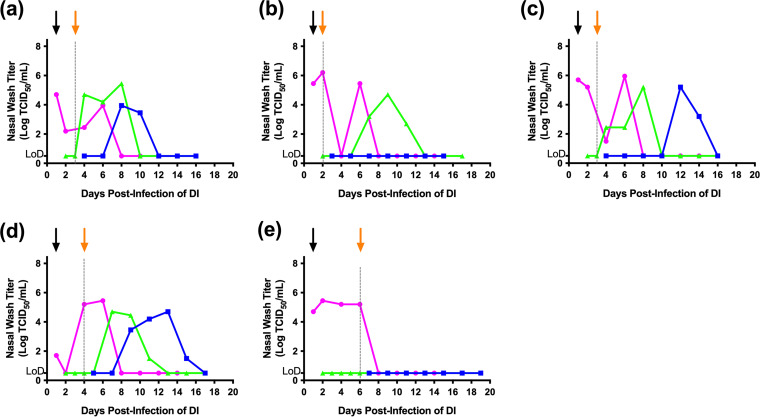
To evaluate whether an avian-origin virus could transmit over two sequential rounds of respiratory contact, we next evaluated the A/Anhui/1/2013 (H7N9) virus. The 6 DI ferrets shed virus, with peak titers between 106 and 107 TCID50/mL (Fig. 3). Three of the six RC1 ferrets shed virus, with virus detected on 2 dpc for two ferrets and on 4 dpc for the remaining animal. In the second round, virus was detected in 2 of 3 RC2 ferrets on 5 or 7 dpc (day 11 postinfection of DI for both animals). Peak titers in the RC1 and RC2 ferrets were comparable to those of the DI animals, and all of the DI ferrets had HI and neutralizing antibody responses (Table 1 and Table S1). All three of the RC1 animals that shed virus developed an antibody response (Table 1 and Table S1); however, two additional RC1 ferrets that did not shed virus had HI titers of 40, and one of them also had a neutralizing antibody titer of 25 (Table S1). Despite the absence of viral shedding, we concluded the RC1 ferret that exhibited both HI and neutralizing antibody responses had been infected bringing the total to 4 of 6 RC1 ferrets being infected. Both the RC2 ferrets that shed virus also had HI and neutralizing antibody responses, while the RC2 ferret that did not shed virus did not have a detectable antibody response. These findings indicate that 2 of 3 RC2 ferrets had been infected with H7N9 influenza and that both H1N1pdm09 and H7N9 influenza viruses were capable of at least 2 subsequent rounds of airborne transmission in ferrets.
FIG 3.
Transmission of avian influenza A/Anhui/1/2013 (H7N9) over two sequential rounds of respiratory contact. Six directly inoculated (DI) ferrets were intranasally infected with 1 × 106 TCID50 of A/Anhui/1/2013 (H7N9) in a 1-mL volume. Twenty-four hours later, each DI animal was introduced into a transmission cage with a naive respiratory contact (RC1) ferret. Nasal wash samples were collected and assayed for evidence of viral infection, as described in Fig. 1. When the RC1 ferret became infected, it was housed with a new respiratory contact (RC2). Each panel (a to f) represents an independent replicate of DI, RC1, and RC2 (if RC1 became positive). Magenta, green, and blue lines represent the nasal wash titers for the DI, RC1, and RC2 ferrets, respectively. The black arrow denotes the day that the DI and RC1 were paired, and the orange arrow and dashed line indicate when the RC1 and RC2 ferrets were paired. Nasal wash samples were titrated on MDCK cells, and the results are expressed as log10 (TCID50/mL) of nasal wash. LoD denotes the limit of detection (0.5 × log [TCID50/mL]).
Sequential respiratory transmission of seasonal human H3N2 and avian H3N8 influenza viruses in ferrets.
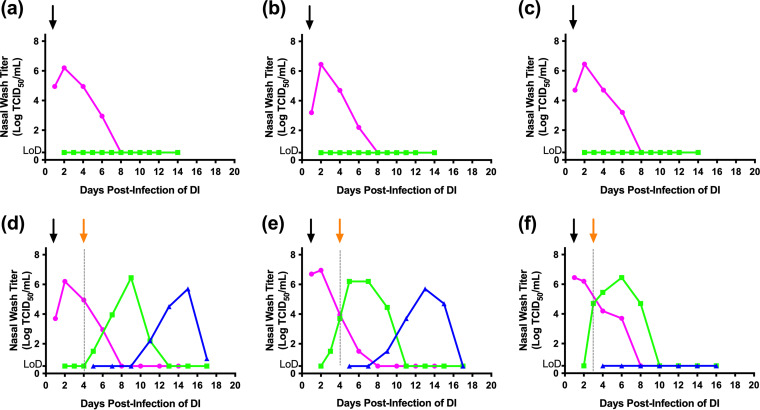
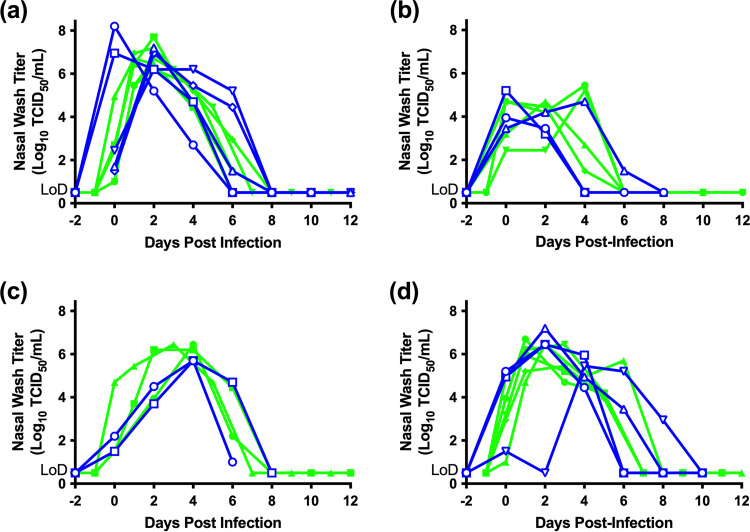
To validate our approach and determine if our findings were applicable to additional viruses, we evaluated sequential transmission of the human seasonal influenza A/Texas/50/2012 (H3N2) virus, and the avian-origin A/harbor seal/New Hampshire/179629/2011 (H3N8) virus that has not been reported to infect humans. In 2022, the first two human cases of H3N8 infections were reported in China. Importantly, both viruses had previously been shown to transmit to 3/3 and 2/3 RC ferrets, respectively (18, 25). Our experience with the H1N1pdm09 and H7N9 viruses indicated that virus was detected in nasal washes within a 2-day window, and seroconversion occurred in some animals in the absence of virus detection in nasal washes. Therefore, we modified the experimental design such that 2 days after virus was last detected in the nasal washes from RC1 ferrets, all remaining virus-negative RC1 ferrets were paired with RC2 ferrets. Transmission of A/Texas/50/2012 (H3N2) was initially evaluated (Fig. 4) in six trios; however, one trio was excluded from further analysis because the RC1 animal was housed with an RC2 animal on the basis of a positive strip test, but we could not detect viral RNA or isolate virus from the nasal wash, and the animal did not seroconvert. Thus, 5 DI ferrets were included in our analysis; all of the animals shed moderate (104 to 106 TCID50/mL) titers of virus in their nasal washes and developed HI and neutralizing antibody titers (Table 1 and Table S1). The DI animals transmitted virus to 4 of 5 RC1 ferrets, with subsequent onward transmission to 3 of 4 RC2 ferrets. Onset of viral shedding in the RC1 ferrets occurred by 3 dpc for two animals, with the remaining animals shedding virus on 6 dpc. RC1 and RC2 ferrets that shed virus had both HI and neutralizing antibody responses (Tables 1 and Table S1), while the RC1 and RC2 ferrets that did not shed virus remained seronegative, indicating that they were not infected.
FIG 4.
Transmission of seasonal influenza A/Texas/50/2012 (H3N2) over two sequential rounds of respiratory contact. Six directly inoculated (DI) ferrets were intranasally infected with 1 × 106 TCID50 of A/Texas/50/2012 (H3N2) in a 1-mL volume. Twenty-four hours later, each DI animal was introduced into a transmission cage with a naive respiratory contact (RC1) ferret. Nasal wash samples were collected and assayed for evidence of viral infection, as described in Fig. 1. When the RC1 ferret became infected, it was housed with a new respiratory contact (RC2). If an RC1 ferret remained test strip or qRT-PCR negative 2 days after the remaining RC1 ferrets became positive, this animal was introduced into a new transmission cage with an RC2 ferret. This modification to the experimental design was incorporated to determine if RC1 ferrets that became seropositive but did not shed virus in their nasal washes could transmit to naive contact animals. Each panel (a to e) represents an independent replicate of DI, RC1, and RC2. Magenta, green, and blue lines represent the nasal wash titers for the DI, RC1, and RC2 ferrets, respectively. The black arrow denotes the day that the DI and RC1 were paired, and the orange arrow and dashed line indicate when the RC1 and RC2 ferrets were paired. Nasal wash samples were titrated on MDCK cells, and the results are expressed as log10 (TCID50/mL) of nasal wash. This experiment originally had 6 replicates; however, in one pair, the nasal wash sample for one RC1 ferret was test strip positive but q-RT-PCR negative, and the ferret did not shed virus, indicating a false-positive test strip result. Thus, this pair of ferrets was excluded from the analysis. LoD denotes the limit of detection (0.5 × log [TCID50/mL]).
In the case of the avian H3N8 virus (Fig. 5), all 6 DI ferrets had high virus titers (>106 TCID50/mL) in their nasal washes and developed HI and neutralizing antibody responses. Transmission from the DI animals occurred to 5 of 6 RC1 ferrets and onward to 4 of 5 RC2 animals. All 5 of the infected RC1 ferrets began shedding virus by 2 dpc (day 3 postinfection of DI ferrets), and the infected RC2 ferrets began shedding on 3 dpc. All of the RC1 and RC2 animals that shed virus had HI and neutralizing titers, while those that did not shed virus remained seronegative (Tables 1 and Table S1). Collectively, our findings with the human H3N2 and avian H3N8 viruses are consistent with the H1N1pdm09 and H7N9 virus data and indicate that influenza viruses of different subtypes are capable of sequential airborne transmission in ferrets. We were unable to determine whether seropositive ferrets that did not shed virus were able to transmit influenza because none of the RC1 ferrets from the H3N2 and H3N8 experiments developed an antibody response in the absence of viral shedding.
FIG 5.
Transmission of avian influenza A/harbor seal/New Hampshire/179629/2011 (H3N8) over two sequential rounds of respiratory contact. Six directly inoculated (DI) ferrets were intranasally infected with 1 × 106 TCID50 of A/harbor seal/New Hampshire/179629/2011 (H3N8) in a 1-mL volume. Twenty-four hours later, each DI animal was introduced into a transmission cage with a naive respiratory contact (RC1) ferret. Nasal wash samples were collected and assayed for evidence of viral infection, as described in Fig. 1. When the RC1 ferret became infected, it was housed with a new respiratory contact (RC2). If an RC1 ferret remained test strip or qRT-PCR negative 2 days after the remaining RC1 ferrets became positive, this animal was introduced into a new transmission cage with an RC2 ferret. This modification to the experimental design was incorporated to determine if RC1 ferrets that became seropositive but did not shed virus in their nasal washes could transmit to naive contact animals. Each panel (a to f) represents an independent replicate of DI, RC1, and RC2. Magenta, green, and blue lines represent the nasal wash titers for the DI, RC1, and RC2 ferrets, respectively. The black arrow denotes the day that the DI and RC1 were paired, and the orange arrow and dashed line indicate when the RC1 and RC2 ferrets were paired. Nasal wash samples were titrated on MDCK cells, and the results are expressed as log10 (TCID50/mL) of nasal wash. LoD denotes the limit of detection (0.5 × log [TCID50/mL]).
Viral shedding patterns in RC ferrets are similar, regardless of route of infection of the donor ferret.
We compared the viral replication kinetics in the nasal washes of the RC1 and RC2 ferrets as these animals may have been infected with different virus doses. The RC1 ferrets were infected by respiratory contact with DI ferrets that had been experimentally inoculated with 106 infectious units of virus in a 1-mL volume, while the RC2 ferrets were infected from exposure to RC1 animals in whom the infectious inoculum was not known but is assumed to be much lower than the dose used to inoculate DI ferrets. As shown in Fig. 6A, the kinetics of virus shedding in the RC1 and RC2 ferrets for H1N1pdm09 were very similar, with peak titers for both of ≥106 TCID50/mL. A similar pattern was observed for the other viruses (Fig. 6B to D), although the peak titers varied among the viruses. Peak titers of the H1N1pdm09 and avian H3N8 viruses ranged from 106 to 107 TCID50/mL, while titers in ferrets infected with the avian H7N9 and H3N2 viruses ranged from 105 to 106 TCID50/mL and 104 to 105 TCID50/mL, respectively. In addition, we observed that the H1N1pdm09 and H3N8 viruses had greater than 80% transmission efficiency in the two successive rounds, while the H3N2 and H7N9 viruses displayed transmission efficiencies of 75 to 80% and 66%, respectively. Despite subtle differences in peak titers, when we compared the proportion of animals that became infected (defined by detection of infectious virus and/or an HI and neutralizing antibody titer) during each round of transmission (Table 1), the proportion of animals that became infected did not change or decrease substantially over two sequential rounds of respiratory contact.
FIG 6.
Superimposed viral shedding curves for infected RC1 and RC2 animals. Displayed are nasal wash titers from the RC1 and RC2 ferrets for a given virus. The shedding curves have been normalized such that day 0 is the first day virus was detected by culture from the animals. Each panel displays the kinetics of viral replication in nasal washes from RC1 (green) and RC2 (blue) animals that shed virus for A/California/07/2009 (H1N1 pdm09) (a), A/Texas/50/2012 (H3N2) (b), A/Anhui/1/2013 (H7N9) (c), and A/seal/New Hampshire/179629/2011 (H3N8) (d) viruses, respectively. LoD denotes the limit of detection (0.5 × log [TCID50/mL]).
Selection of viral variants during sequential transmission.
To determine if sequential rounds of respiratory transmission selected for viral variants, viruses recovered from nasal wash samples were subjected to deep sequence analysis. Tables 2 and 3 display a summary of nonsynonymous and synonymous mutations that were associated with transmission for all 4 virus strains (for a complete list of all mutations, see Tables S2 to S5). For both the 2009 pandemic H1N1 and A/Anhui/1/2013 (H7N9) viruses, nonsynonymous mutations were identified in multiple trios of ferrets, and these mutations became enriched and were maintained during transmission from the DI to RC1 and RC1 to RC2 animals. In contrast, both the A/Texas/50/2012 (H3N2) and A/harbor seal/New Hampshire/179629/2011 (H3N8) viruses did not consistently acquire nonsynonymous mutations despite sequential transmission. No synonymous mutations were associated with sequential transmission in all 4 virus strains (Table 3).
TABLE 2.
Amino acid/nonsynonymous mutations associated with at least one chain of respiratory droplet transmission
| Nucleotide frequencyd |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trio 1 |
Trio 2 |
Trio 3 |
Trio 4 |
Trio 5 |
Trio 6 |
|||||||||||||||||
| Virus straina | Protein | Nucleotide changeb | Amino acid change relative to inoculumc | Virus inoculum | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 |
| A/California/07/2009 (H1N1) | PB2 | C251A | A84D | 66 | 83 | |||||||||||||||||
| PB2 | G550A | A184T | 7 | 21 | 33 | |||||||||||||||||
| PB2 | A1684T | I562F | 24 | 39 | ||||||||||||||||||
| HA | A716G | D239 [222] (225)G | 86 | 91 | 99 | 96 | 91 | 94 | 95 | 93 | 97 | 97 | 93 | 97 | 99 | 94 | 98 | 98 | ||||
| HA | G719A | R240 [223] (226)Q | 93 | 95 | 100 | 100 | 94 | 100 | 100 | 97 | 100 | 100 | 97 | 100 | 100 | 98 | 100 | 100 | ||||
| NP | G302A | G101D | 29 | 7 | 13 | 40 | 27 | 51 | 63 | 13 | 20 | 25 | ||||||||||
| NP | G1123A | D375N | 6 | 36 | 13 | 48 | 57 | 5 | 12 | |||||||||||||
| A/Anhui/1/2013 (H7N9) | PB2 | A2132G | N711S | 15 | 100 | 99 | ||||||||||||||||
| PB2 | G2141A | S714N | 13 | 99 | 98 | |||||||||||||||||
| PB1 | C413T | P138L | 91 | 100 | ||||||||||||||||||
| PA | A1226G | N409S | 8 | 7 | 8 | 10 | 100 | 100 | 12 | 8 | ||||||||||||
| HA | A421G | N141 [123] (133)D | 47 | 43 | 52 | 55 | 42 | 98 | 99 | 50 | 100 | 100 | 47 | 5 | ||||||||
| HA | G499A | D167 [149] (158)N | 32 | 37 | 41 | 29 | 38 | 28 | 30 | 95 | ||||||||||||
| HA | T704A | L235 [217] (226)Q | 21 | 32 | 26 | 27 | 99 | 99 | 24 | 100 | 99 | 10 | ||||||||||
| NA | C29T | T10I | 99 | 100 | ||||||||||||||||||
| NA | A1379G | K460R | 99 | 100 | ||||||||||||||||||
| A/Texas/50/2012 (H3N2)e | HA | T725A | I242 (226)N | 38 | 53 | 36 | 99 | 9 | n/p | n/p | n/p | |||||||||||
| NS | A796C | S266R | 6 | 92 | 100 | 8 | 6 | 12 | n/p | n/p | n/p | |||||||||||
| A/harbor seal/New Hampshire/179629/2011 (H3N8) | HA | G433A | G145 (129)R | 100 | 100 | |||||||||||||||||
| HA | G460A | A154 (138)T | 99 | 77 | 53 | |||||||||||||||||
| HA | G668A | R223 (207)K | 29 | 15 | 13 | 9 | 4 | 98 | 98 | 11 | 99 | 11 | ||||||||||
| NA | C352T | P118S | 38 | 37 | 32 | 83 | 35 | 100 | 99 | 47 | 34 | 29 | 86 | 99 | ||||||||
| NA | G1180A | V394I | 35 | 41 | 47 | 16 | 94 | 40 | 42 | 100 | 100 | 33 | 100 | 47 | 10 | |||||||
Each group consists of 1 directly inoculated (DI) ferret and 1 or 2 respiratory contact (RC) ferrets if onward transmission occurred. The first respiratory contact is RC1. If this animal became infected, it was housed with a second respiratory contact designated RC2.
Nucleotide numbering is from the start codon of each gene.
For HA, amino acid numbering in square brackets is numbering with signal peptide removed (i.e., H1 numbering or H7 numbering); parentheses indicate H3 numbering without signal peptide.
Gray shading indicates that transmission did not occur, and underlining indicates that the mutation was associated with transmission in one or more trios of ferrets.
For A/Texas/50/2012 (H3N2), trio 6 was removed (see Results, discussion of Fig. 4); thus, a deep-sequencing analysis was not performed (n/p).
TABLE 3.
Synonymous mutations associated with at least one chain of respiratory droplet transmission
| Nucleotide frequencyd |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trio 1 |
Trio 2 |
Trio 3 |
Trio 4 |
Trio 5 |
Trio 6 |
|||||||||||||||||
| Virus straina | Protein | Nucleotide changeb | Amino acid change relative to inoculumc | Virus inoculum | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 | DI | RC1 | RC2 |
| A/California/07/2009 (H1N1) | PB2 | G120A | E40 | 95 | 96 | |||||||||||||||||
| PB2 | C1711T | L571 | 29 | 37 | 23 | 29 | 21 | 16 | 12 | 21 | 100 | 99 | ||||||||||
| PA | C169A | R57 | 35 | 16 | ||||||||||||||||||
| HA | G450A | T150 | 36 | 38 | ||||||||||||||||||
| NP | T1275C | V425 | 66 | 100 | ||||||||||||||||||
| A/Anhui/1/2013 (H7N9) | PB2 | C93T | I31 | 9 | 41 | 11 | 10 | 12 | 51 | |||||||||||||
| PB1 | C297T | H99 | 99 | 100 | ||||||||||||||||||
| PA | G879A | E293 | 99 | 99 | ||||||||||||||||||
| PA | G1812A | E604 | 95 | 97 | ||||||||||||||||||
| HA | G1326A | E396 | 79 | 87 | ||||||||||||||||||
| NA | C825T | C275 | 9 | 7 | 6 | 9 | 100 | 100 | 11 | |||||||||||||
| NS | C154T | L52 | 17 | 19 | 15 | 16 | 18 | 17 | 17 | 85 | ||||||||||||
| A/Texas/50/2012 (H3N2) | PB2 | C2067T | A689 | 74 | 100 | |||||||||||||||||
| PB1 | C2143T | L415 | 97 | 100 | ||||||||||||||||||
| HA | G795A | G265 | 97 | 100 | 5 | |||||||||||||||||
| A/harbor seal/New Hampshire/179629/2011 (H3N8) | PB1 | G414A | P138 | 100 | 100 | |||||||||||||||||
| PA | A147G | S49 | 67 | 100 | ||||||||||||||||||
| PA | A660G | P220 | 15 | 96 | ||||||||||||||||||
Each group consists of 1 directly inoculated (DI) ferret and 1 or 2 respiratory contact (RC) ferrets if onward transmission occurred. The first respiratory contact is RC1. If this animal became infected, it was housed with a second respiratory contact designated RC2.
Nucleotide numbering is from the start codon of each gene.
For HA, amino acid numbering in square brackets is numbering with signal peptide removed (i.e., H1 numbering or H7 numbering).
Gray shading indicates that transmission did not occur.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/California/07/2009 (H1N1pdm09). Download Table S2, PDF file, 0.02 MB (25.3KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
For the 2009 pandemic H1N1 virus, the HA D225G and R226Q mutations (H3 numbering) were undetected in the inoculum (i.e., below the 5% frequency cutoff threshold) but were rapidly selected and enriched to frequencies of ≥86% in the DI ferret for all 6 trios of animals. In the 5 of 6 trios in which transmission occurred to the RC1 ferret, these mutations were present at frequencies of ≥94% in the RC1 animals, and they were maintained at similar frequencies in the RC2 ferrets. Importantly, these mutations were not associated with additional mutations, indicating that no compensatory changes were required. However, the strong selection for these mutations indicates that they confer a fitness advantage in ferrets.
Analysis of the mutations that arose during sequential transmission of the A/Anhui/1/2013 (H7N9) virus (Table 2) showed that multiple mutations are associated with sequential transmission. Interestingly, in trios 4 and 5 in which transmission occurred from DI to RC1 and RC1 to RC2, the HA mutations N133/123D N123/133D and L217/226Q (H7/H3 numbering) became enriched. In these trios, both the RC1 and RC2 animals shed viruses with both mutations at frequencies of ≥98%.
The N123/133D mutation was present in the viral inoculum (47% frequency), and similar frequencies of this variant were present in the DI ferrets (i.e., 43 to 50%). In trios 4 and 5, the frequency of this mutation increased to ≥98% in the RC1 ferrets, and this frequency was maintained in viruses recovered from the RC2 ferrets; however, in trio 6 in which transmission occurred to the RC1 ferret but failed to continue to the RC2 ferret, the frequency of this mutation decreased to 5% in the RC1 animal. The HA L217/226Q mutation was not present above the cutoff threshold (5%) in the inoculum; however, it was present in all of the DI ferrets at frequencies between 10 and 32%. In trios 4 and 5, this mutation became enriched to ≥98% in the RC1, and this was maintained to the RC2 animals. In trio 6, in which the virus transmitted to the RC1 animal but failed to transmit onward, the HA L226Q mutation was present at the lowest frequency (10%) in the DI animal and was not present in the RC1 animal. This pattern in which the HA N133D and L226Q mutations become enriched during transmission from DI to RC1 and are then maintained to the RC2 in trios 4 and 5, while neither mutation became enriched in trio 6 in which the virus failed to transmit to the RC2 animal, suggests that both mutations are required for sequential airborne transmission.
Interestingly, in trios 4 and 5, sequential transmission of the H7N9 virus was associated with additional mutations that became enriched to frequencies of ≥91% (Table 2). These mutations were in the viral polymerase (i.e., PB2, PB1, and/or PA) and neuraminidase (NA) genes, and the mutations differed between the two trios of ferrets. In trio 4, the PB1 P138L, PA N409S, and NA T10I mutations were either below the 5% cutoff threshold or were detected in donor animals at a 10% frequency. Upon transmission to the RC1 animals, these mutations became enriched to ≥91% frequency and were detected in the RC2 animal at frequencies of 99 to 100%. In trio 5, the mutations PB2 N711S and S714N and NA K460R were similarly either below the detection threshold or present at frequencies between 13 and 15%, and the mutations were then detected in the RC1 and RC2 animals at frequencies between 98 and 100%. The rapid selection and enrichment of these additional mutations in each trio of ferrets strongly suggests that they contribute to or are required for transmission. Moreover, while the individual mutations differ, the selection of these mutations in association with the HA N133D and L226Q mutations indicates that compensatory mutations in the viral polymerase and NA genes may be required for multiple rounds of transmission.
Last, we performed alignments to determine if any of the mutations associated with transmission were in antigenic sites (Table S6). No mutations were identified in antigenic sites of the NA for any of the 4 subtypes. For the HA, most of the mutations in antigenic sites across all four virus subtypes were not associated with transmission; however, for the 2009 pandemic H1N1 and A/Anhui/1/2013 (H7N9) viruses, during sequential transmission, mutations at antigenic site 226 in HA (H3 numbering) became enriched to frequencies greater than 98%. Specifically, the same amino acid mutation 226Q was selected in both the H1 and H7 HAs (R226Q and L226Q, respectively), suggesting that in certain HA subtypes, transmission in ferrets may select for mutations at this site.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/Anhui/1/2013 (H7N9). Download Table S3, PDF file, 0.02 MB (26.2KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/Texas/50/2012 (H3N2). Download Table S4, PDF file, 0.02 MB (18.9KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/harbor seal/New Hampshire/179629/2011 (H3N8). Download Table S5, PDF file, 0.02 MB (21.1KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Summary of mutations in antigenic sites of HA and NA during sequential transmission. Download Table S6, PDF file, 0.02 MB (16.5KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
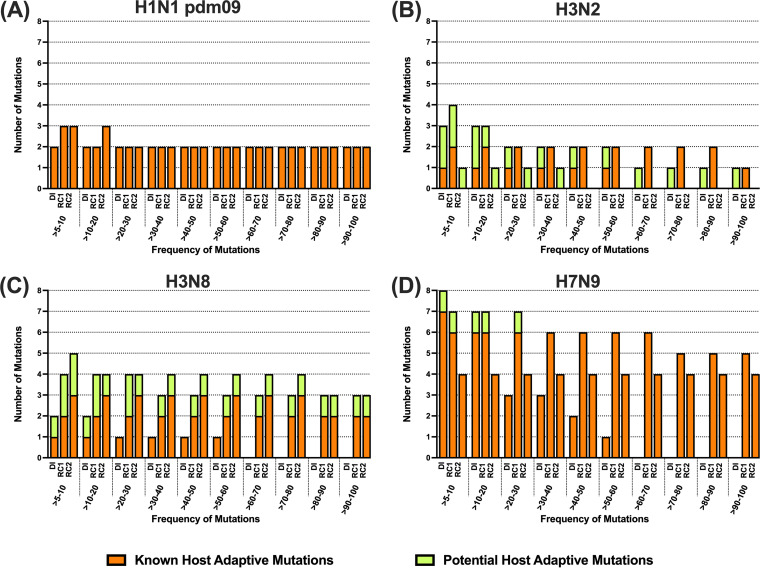
Changes in deep sequencing data are associated with host adaptation.
We next evaluated if any of the nonsynonymous changes identified in the deep-sequencing analysis were at known or potential host-adaptative sites. This analysis encompassed any mutation identified in any of the DI, RC1, or RC2 animals (Tables S2 to S5). Out of 4,454 possible sites in the 4 virus strains, 105 sites curated in FluSurver, a tool in global initiative on sharing avian flu data (GISAID), were identified by previous studies to be involved in host adaptation. Of these 105 sites, 34 are from HA, 21 are from PB2, 18 are from NP, 13 are from PA, 5 are from PB1, 5 are from M2, 5 are from NS2, 3 are from M1, and 1 is from NS2. Of the 54 nonsynonymous mutations in H1N1pdm09, 4 (PB1 P13L, HA K228R, HA D239G, and HA R240Q) were found in known host adaptation sites. Two (HA A154S and HA I242N) of 51 nonsynonymous mutations from H3N2, 4 (HA G145R, HA A154T, HA A154S, and HA Q242R) of 23 nonsynonymous mutations from H3N8, and 8 (PB2 D567N, PB2 D701N, PB2 S714N, PA N409S, HA N141D, HA G151E, HA D167N, and HA L235Q) of 23 nonsynonymous mutations from H7N9 were in known host-adaptation sites. Not surprisingly, the majority of these host-adaptive changes were enriched in the surface glycoprotein HA (13 of 40 changes in HA; odds ratio of 7.53). For the avian H7N9 virus, host-adaptive changes were also observed in the polymerase segments (PB2 and PA).
To compare the overall degree of host-adaptive changes between the 4 viral subtypes, we assessed the frequency of both known and potential host-adaptive mutations associated with transmission from the DI to RC1 and RC2. As shown in Fig. 7, this analysis indicated that the overall number of adaptive changes associated with transmission from the DI to RC1 and RC2 ferrets was between 0 and 3 for the 2009 pandemic H1N1 and A/Texas/50/2012 (H3N2) viruses, while 2 to 4 and 4 to 6 mutations were associated with transmission of the A/harbor seal/New Hampshire/179629/2011 (H3N8) and A/Anhui/1/2013 (H7N9) viruses, respectively. Next, we mapped nonsynonymous changes at nucleotide frequencies greater than or equal to 10%, 25%, and 50% from the deep-sequencing data onto the HA protein structures for all 4 subtypes grouped by the ferret types (DI, RC1, and RC2; Fig. S1 to S3). Changes that occur at sites previously known to be involved in host adaptation are colored in red, and other amino acid changes are colored in green. We observed that 18 out of 20 nonsynonymous changes in the HA occur at the receptor binding site (Fig. S3) and in its vicinity, indicating that most of these changes in HA are indeed playing a role in ferret host adaptation.
FIG 7.
Frequency of known and potential host-adaptive mutations associated with airborne transmission. To determine whether the number of host adaptive mutations was associated with sequential transmission, the frequency at which a given number of known or potential host-adaptive mutations was determined for DI, RC1, and RC2 ferrets. Panels display the findings for A/California/07/2009 (pH1N1) (A), A/Texas/50/2012 (H3N2) (B), A/seal/New Hampshire/179629/2011 (H3N8) (C), and A/Anhui/1/2013 (D) viruses, respectively.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, RC2 ferrets at nucleotide cutoff frequency of 50%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S1, PDF file, 1.9 MB (1.9MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, and RC2 ferrets at a nucleotide cutoff frequency of 25%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S2, PDF file, 1.9 MB (1.9MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, and RC2 ferrets at a nucleotide cutoff frequency of 10%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S3, PDF file, 1.9 MB (2MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
We further narrowed this analysis and counted only the number of known host-adaptive mutations in the DI/RC1 ferrets at a nucleotide cutoff frequency of 10% (Fig. S3) that were still present in the RC2 ferrets at a nucleotide cutoff frequency of 50% (Fig. S1; compare <10% to 40 to 50% in Fig. 7). This yields an estimate of the number of adaptive changes required for the virus to propagate itself successfully to subsequent hosts. In increasing order, the number of adaptive substitutions that are still retained in RC2 at a 50% nucleotide cutoff frequency are 0 for H3N2, 2 for H1N1pdm09, 3 for H3N8, and 4 for H7N9. Taken together, this indicates that the seasonal viruses H3N2 and H1N1pdm09 require none or few substitutions to propagate in ferrets, but the avian viruses H3N8 and H7N9 require more adaptive changes to transmit in ferrets. Note for the 2 viral subtypes (H1N1pdm09 and H3N8) with the highest transmission kinetics, there were mutations at 2 to 3 previously known host-adaptive sites in the RC2 ferrets, HA D239G and HA R240Q for H1N1pdm09 and HA G145R, HA A154T, and HA Q242R for H3N8. These host-adaptive changes might have contributed to the efficient transmission of the virus in the ferret host. Selection of these host-adaptive sites was also evident in the H7N9 virus. More than 50% of the viruses in the DI ferrets carried only the single HA N141D variant and fewer than 25% of the viruses carried the PB2 S714N, PA N409S, HA N141D, HA G151E, HA D167N, and HA L235Q variant; yet, the latter multisubstitution variant is selected in more than 50% of the viruses in RC1 ferrets, and 4 of these substitutions (PB2 S714N, PA N409S, HA N141D, and HA L235Q) were propagated onward to RC2 ferrets. This shows that the H7N9 virus required more adaptive changes to propagate well in ferrets compared to the other 3 viruses, and variants with more host-adaptive changes were selected during onward viral transmission.
DISCUSSION
Since the emergence of H7N9 influenza viruses in 2013, there has been limited evidence of human-to-human transmission; however, in ferrets, these viruses transmit to RC animals with efficiencies ranging from 33 to 100% (18–22). This led to debate on the merits and limitations of ferret transmission studies that was compounded by reports of avian H3N8 and H9N2 influenza viruses capable of respiratory transmission in ferrets without documented human infections (H3N8) or evidence of human-to-human transmission (H9N2) (25, 26). In fact, transmission in ferrets may more accurately represent a general level of adaptation of avian viruses to mammals rather than risk of transmissibility, and correlative analyses have shown that airborne transmission efficiency between ~50 and 75% in ferrets is suggestive of a risk of transmission in humans, but it does not infer transmissibility in humans (27). Therefore, we sought to improve the ferret model to more closely mimic transmission in humans. Specifically, we evaluated sequential transmission as an indicator of transmissibility in humans. This approach simultaneously evaluates whether ferrets can be infected by respiratory droplet with a novel virus and then transmit the virus onwards through the air. Our findings demonstrate that, like humans, ferrets can transmit influenza viruses via the airborne route over multiple rounds of transmission. Unfortunately, this approach did not distinguish between avian and human viruses, and we conclude that this modification did not enhance the model. Thus, we are still limited in our ability to assess the risk of transmission in humans posed by a virus that transmits in ferrets.
To evaluate sequential airborne transmission in ferrets as a predictor of pandemic potential, we performed sequential transmission studies with pandemic, seasonal, and emerging influenza viruses. Due to the large volume and high inoculum dose typically administered to the DI ferrets, we anticipated that the efficiency of transmission from an experimentally inoculated DI ferret would differ from transmission from an animal that acquired infection via respiratory contact. In fact, antiviral efficacy studies have demonstrated that oseltamivir-treated ferrets that were infected by contact with an infected ferret displayed greater reduction in clinical disease than oseltamivir-treated animals that were directly infected with a high dose of virus (106 infectious units) (32). We have previously demonstrated that intranasal inoculation of DI ferrets with 106 infectious units of virus in 1 mL infects the entire respiratory tract (33), but the inoculum received and the pattern of infection in the respiratory tract of RC animals are unknown. Thus, we hypothesized that seasonal and pandemic influenza viruses that are highly transmissible would transmit onward to a second RC ferret, while avian influenza viruses would not.
We found that the pandemic H1N1 and seasonal H3N2 viruses were capable of sequential transmission to at least 75% of RC1 and RC2 animals. These data support the use of the ferret model of influenza transmission because these observations agree with onward airborne spread of these viruses in humans (34–36). However, the finding that avian influenza H7N9 and H3N8 viruses were also capable of sequential transmission and the H7N9 virus transmitted to 66% of RC1 and RC2 animals disproved our hypothesis. Several research groups have performed studies evaluating chains of transmission by direct contact or cohousing in the same cage (37, 38) as well as transmission chains in which a direct contact and RC ferret are exposed simultaneously to a DI ferret (17, 39). Additionally, serial passage studies have been performed using respiratory contact as a selection pressure, where nasal wash samples from RC animals were used to directly inoculate the next donor ferret (14, 19). However, our studies clearly demonstrate a chain of onward airborne transmission from a ferret infected by respiratory contact.
The evaluation of four different virus subtypes in the same experimental system allowed us to compare viral replication kinetics in RC animals. Consistent with other reports (30, 31), peak titers of H1N1pdm09 were higher than the other viruses, and transmission to RC animals was rapid, occurring in 2 to 3 days and 1 to 2 days, respectively, in RC1 and RC2 animals. In contrast, the H3N2 virus did not replicate as efficiently in ferrets as the H1N1pdm09 virus (Fig. 4), with titers approximately 10- to 100-fold lower than H1N1pdm09, consistent with a previous report on transmission of this virus (18). Moreover, transmission to RC1 animals was delayed, with the onset of shedding from RC1 animals between 3 and 6 dpc and onward transmission to RC2 ferrets between 5 and 9 dpc. These findings were unexpected because H3N2 viruses circulate efficiently among humans and cause annual epidemics. All of the viruses used in this study were amplified in embryonated eggs, and it is possible that passage in eggs (40) affected the kinetics of replication of the H3N2 virus in ferrets. Importantly, despite these differences, A/Texas/50/2012 (H3N2) transmitted to 4 of 5 RC1 ferrets and 3 of 4 RC2 ferrets.
When we evaluated transmission of the avian influenza A/Anhui/1/2013 (H7N9) virus, a lower proportion of RC1 and RC2 ferrets became infected; this finding is consistent with the majority of previously published studies (18–21). While 3 of 6 RC1 ferrets shed virus, when serology was included, we concluded that 4 of 6 RC1 ferrets had become infected. Similarly, we observed transmission to 2 of 3 RC2 ferrets, indicating that there was no reduction in transmission efficiency over two sequential rounds of respiratory transmission. The interval of transmission from DI to RC1 ferrets was 2 to 4 days and from RC1 to RC2 was 5 to 7 days. While this is delayed relative to H1N1pdm09, it is comparable to transmission of the A/Texas/50/2012 (H3N2) virus. Finally, when transmission of the avian influenza H3N8 virus was evaluated, we observed high titers in the nasal wash samples from all the DI and RC animals. We did not observe a substantial reduction in the proportion of RC1 and RC2 animals that became infected, and the intervals, onset, and pattern of viral shedding were comparable to the H1N1pdm09 virus. All 5 RC1 animals that shed virus had onset of shedding by 2 dpc, and the RC2 animals that became infected started shedding virus 3 dpc. When we compared our findings with the previous report on transmission of this virus (25), we found that a higher proportion (5/6 or 83%) of animals became infected than that observed in the previous study (2/3 or 66%). Furthermore, transmission occurred more rapidly in our experimental system, within 2 dpc compared 5 to 7 dpc (25). The reasons for these differences are unclear but are likely due to differences in experimental systems (41). Taken together, our findings indicate that despite differences in the proportion of animals that became infected, H1N1pdm09 and H3N8 and the H3N2 and H7N9 influenza viruses exhibited similar peak titers and transmission kinetics, respectively.
When we compared the proportions of animals that became infected, we observed that 66% of the RC1 and RC2 animals became infected with the H7N9 virus. This differed from the other virus strains evaluated, which maintained efficiency of 75% or higher. While we used relatively large sample sizes of six ferrets, these groups are not large enough to draw statistically significant conclusions (42). Further, it is difficult to interpret the biological significance of a virus that transmits to 66% versus 75 or 80% of respiratory contacts. However, as shown in Fig. 6, the viral shedding patterns for a given virus were similar for infected RC1 and RC2 ferrets. Thus, infection that results from respiratory exposure to a donor ferret that was experimentally inoculated with a high dose of virus in a large volume is similar to that of an infection that results from respiratory contact with a ferret that was infected more naturally by an unknown airborne dose carried in a small volume. It is important to note that our studies do not permit evaluation of virus titers in the lungs. Collectively, we show that transmission efficiency did not change over two sequential rounds of respiratory transmission for all four virus strains evaluated and that the route of infection of the donor ferret did not influence the establishment of a secondary infection in the upper respiratory tract of an RC ferret. These findings demonstrate that ferrets infected by the airborne route can transmit influenza viruses onward; however, sequential transmission is not more informative than a single round of respiratory transmission for evaluating the transmissibility of a virus in ferrets. Furthermore, our findings indicate that the use of sequential transmission was not able to differentiate between viruses that transmit from person to person and viruses that do not.
While the sequential transmission system could not readily predict which viruses are transmissible in humans, deep sequence analysis of viruses that transmitted over multiple rounds of airborne transmission yielded insight into mutations that may support transmission. Specifically, the deep-sequencing analyses indicated that respiratory transmission exerts a selective pressure and favors specific mutations in the A/California/07/2009 (H1N1pdm09) and A/Anhui/1/2013 (H7N9) viruses. In contrast, neither the A/Texas/50/2012 (H3N2) nor the A/harbor seal/New Hampshire/179629/2011 (H3N8) viruses acquired additional mutations despite exhibiting sequential transmission. Consistent with these observations, mutations in both the H1N1pdm09 and H7N9 viruses have been reported in the literature. The D222G HA mutation in the H1N1pdm09 virus has been identified in natural isolates, and some clinical reports suggest that it is associated with increased virulence (43, 44). Experimental studies have shown the D222G mutation does not enhance virulence or alter respiratory droplet transmission in ferrets (45). The R223Q HA mutation has also been found in natural isolates (46–48) and was also identified when antigenic drift of a closely related virus, A/Tasmania/2004/2009 (H1N1), was modeled by serial contact transmission in ferrets (49). These findings suggest that both mutations may be associated with further adaptation to mammals and may not be directly linked to transmission.
For the A/Anhui/1/2013 (H7N9) virus, the HA N123D and HA L217Q mutations have previously been identified in ferret transmission studies (19). In these studies, ferrets were directly inoculated with A/Anhui/1/2013 (H7N9), and an RC animal was introduced. Nasal wash samples from infected RCs were then used to directly inoculate a second set of ferrets. Transmission to naive RCs was evaluated, and nasal wash samples from these contacts were subjected to deep sequencing. In vitro studies showed the HA N123D mutation modestly (~2- to 4-fold) increased binding to “human-like” α2,6-linked sialic acids, while the L217Q mutation promoted binding to “avian-like” α2,3-linked sialic acids. In these studies, the N123D mutation was identified in 3 of 4 RC ferrets, while the L217Q mutation was present at low frequency and was not consistently associated with transmission (19). In contrast, in our studies, these mutations occurred concurrently and were prevalent at high frequency. Given the contradictory role of these mutations, it is unclear how they contribute to transmission.
Our findings for the A/Anhui/1/2013 (H7N9) virus are consistent with other published studies, as 3 to 5 mutations were consistently associated with transmission (17, 19, 20). In both groups of ferrets that displayed sequential transmission, mutations in the viral polymerase and NA genes were also identified. None of the identified mutations resulted in the addition or loss of a glycosylation site, and several of the mutations, including PA N409S, NA T10I, and K460R, have been reported previously (50–52). PA N409S was shown to increase polymerase activity and cause a 10-fold reduction in the median mouse lethal dose (52), while NA T10I and K460R were identified in mice treated with an anti-NA monoclonal antibody but were not consistently found in treated animals (50). The NA T10I mutation was also identified in the only infected RC in an H7N9 ferret transmission study (51). Collectively, these findings suggest that this virus must acquire additional adaptive changes to balance several viral properties and support transmission.
Importantly, we also evaluated whether any of the mutations that arose during sequential transmission occurred in antigenic sites of the HA and NA. No mutations associated with transmission were identified in antigenic sites of the NA, and, with the exception of changes at position 226 (H3 numbering), there were no mutations in HA consistently associated with transmission. In both the 2009 pandemic H1N1 and A/Anhui/1/2013 (H7N9) viruses, the HA 226Q mutation was selected and became fixed during transmission. As mutations at position 226 were selected in two different subtypes in the absence of immune pressure, our results suggest that transmission in ferrets may exert a selective pressure on this site. Therefore, in the event of sustained human-to-human transmission of H7N9 viruses, changes at position 226 should be monitored, and vaccines should be formulated to match this antigenic change.
In addition to the identification of amino acid changes associated with transmission, mapping of the overall number of host-adaptive changes indicated that the pandemic H1N1 and seasonal H3N2 viruses required minimal or no mutations to transmit in ferrets, while the avian H7N9 and H3N8 viruses required a greater number of mutations (Fig. 7). This suggests that the overall mutational frequency during transmission studies may be an additional indicator of transmission potential in humans. Specifically, a low overall mutational frequency associated with transmission in ferrets may indicate that an avian virus requires minimal adaptation to become transmissible in humans.
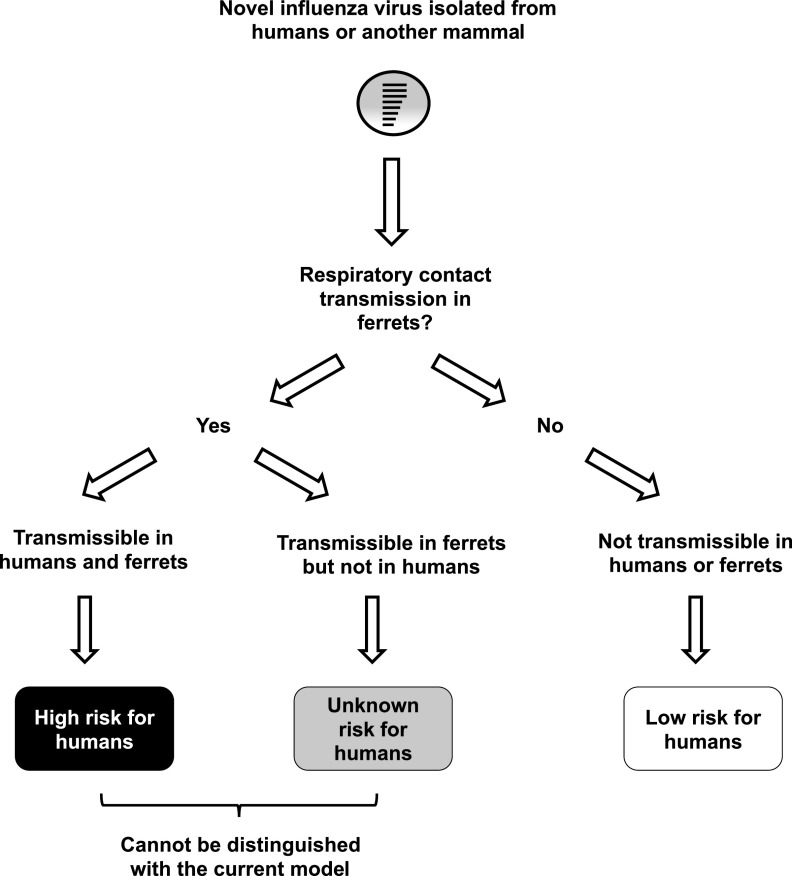
In summary, some avian influenza viruses, such as highly pathogenic H5N1 and H7N7 viruses, do not transmit in ferrets, and these viruses have not spread in humans. Therefore, the inability of a virus to transmit in ferrets is important information for risk assessment. However, when airborne transmission is detected in ferrets, the cumulative experience suggests that this phenotype is necessary but not sufficient for predicting transmissibility in humans (Fig. 8). We sought to improve on the ferret model by evaluating sequential transmission and conclude that while ferrets could sequentially transmit influenza viruses over multiple rounds of airborne transmission, this modification did not enhance the model. Thus, we are still unable to accurately assess the risk of transmission in humans posed by a virus that transmits by the respiratory route in ferrets (Fig. 8). It is important that future studies evaluate additional parameters or strategies to improve pandemic risk assessment of emerging influenza viruses.
FIG 8.
Schematic of risk assessment using airborne transmission in animal models. Airborne transmission between experimental animals is a critical component of risk assessment tools used by the CDC and WHO to assess the pandemic risk posed by an emerging influenza virus. Epidemiologically successful influenza viruses transmit by respiratory contact in ferrets, and the inability to transmit by respiratory contact in ferrets indicates a low risk of transmissibility in humans. However, some H7N9 and H3N8 influenza viruses that display the ability to transmit between ferrets have not spread between people. The risk of transmission from person to person posed by these viruses cannot be accurately assessed or distinguished with existing animal models of transmission.
MATERIALS AND METHODS
Viruses and cells.
Influenza viruses A/California/07/2009 (H1N1pdm09), A/Texas/50/2012 (H3N2), and A/Anhui/1/2013 (H7N9) were provided by the Centers for Disease Control and Prevention (Atlanta, GA). Influenza A/harbor seal/New Hampshire/179629/2011 (H3N8) virus was kindly provided by Hon Ip, US Geological Survey (Madison, WI). All viruses were propagated in specific pathogen-free 10-day-old embryonated hen’s eggs (Charles River, CT), as previously described (53). Viral titers of propagated viruses and nasal wash samples were determined on Madin-Darby canine kidney (MDCK) cells (ATCC, Manassas, VA) grown in 96-well plates and calculated using the method of Reed and Muench (54).
Ferret transmission experiments.
Equal numbers of male and female ferrets 24 to 36 weeks old (Triple F Farms, Sayre, PA) were screened by hemagglutination inhibition assay and determined to be seronegative for A/California/07/2009 (H1N1pdm09), A/Texas/50/2012 (H3N2), and A/Switzerland/9715293/2013 (H3N2) viruses. Transmission experiments were performed using large stainless steel ventilated ferret cages (Allentown, NJ) modified to permit two ferrets to be separated by an offset perforated divider, as described previously (16). To evaluate sequential transmission, groups of six ferrets were utilized as this was the maximum number of replicates that could be performed in our experimental system while allowing for evaluation of two rounds of airborne transmission. Animals were not randomized, and, due to the nature of the experimental design, the studies could not be blinded. Six ferrets were anesthetized with 5% inhalational isoflurane and inoculated intranasally with 1× 106 TCID50 of virus in a 1-mL volume of L-15 medium (Invitrogen, CA). Twenty-four hours later, these ferrets, termed directly inoculated (DI) animals, were introduced into one side of the transmission cage, and a naive respiratory contact (RC1) was housed adjacent to this animal (Fig. 1). At the time of introduction and every other day until day 14, the DI ferrets were sedated with a mixture of ketamine (20 mg/kg), xylazine (2 mg/kg), and atropine (0.05 mg/kg), and nasal wash samples were collected by instilling a 1-mL volume of phosphate-buffered saline (PBS) into the nostrils and inducing sneezing on a Petri dish. An additional 1-mL volume of PBS was used to rinse the dish, and the nasal wash samples were aliquoted and frozen at −80°C. Nasal wash samples were similarly collected from the RC1 ferrets daily, and when determined to be positive for viral antigen or RNA (see below), the RC1 ferret was moved to a new transmission cage, and a second respiratory contact (RC2) animal was introduced. Nasal washes were collected from RC1 and RC2 animals 24 h later and then every other day for 14 days. For studies with H1N1pdm09 and H7N9 influenza viruses, when an RC1 ferret did not become positive by day 14, the DI and RC1 animals were moved to conventional housing and housed separately. For the H3N2 and H3N8 viruses, 2 days after the last RC1 ferrets were determined to be virus positive, any remaining RC1 ferrets were housed with an RC2 ferret. Nasal wash samples were then collected from these animals 1 day later and then every other day for 14 days. On day 21 postinfection for the DI ferrets and 21 dpc for the RC1 and RC2 ferrets, the animals were deeply sedated, and blood was collected via cardiac puncture before euthanasia.
To detect viral antigen in the nasal wash samples of the RC1 ferrets, 100 μL of nasal wash was assayed using FluDETECT avian influenza virus antigen test strips (17) (Zoetis, NJ). As a secondary method of detection, quantitative M gene RT-PCR was incorporated for evaluation of the H3N2, H3N8, and H7N9 viruses due to reduced sensitivity of the test strips for the H7 and H3 virus strains. Viral RNA was extracted from 140 μL of nasal wash sample using a QIAamp viral RNA extraction kit (Qiagen, Hilden, Germany), and quantitative RT-PCR was performed on 5 μL of viral RNA using the Superscript III Platinum one-step q-RT-PCR system (Invitrogen, CA). RT-PCR was performed according to the CDC protocol published by the WHO (55), and a CT value of ≤35 was considered positive. RT-PCR was performed on a QuantStudio 6 Flex real-time PCR instrument (Thermo Fisher, Waltham, MA).
Evaluation of the antibody response by hemagglutination inhibition and microneutralization assays.
(i) Hemagglutination inhibition (HI). Serum samples were treated with receptor-destroying enzyme (RDE; Denken Seiken, Tokyo, Japan) overnight, followed by heat inactivation at 56°C for 30 min. Treated sera were then tested for HI according to standard protocols (56) using turkey red blood cells (0.05% suspension in normal saline).
(ii) Microneutralization assay. RDE-treated sera were subsequently evaluated in microneutralization assays as previously described (57). Serial 2-fold dilutions of sera were prepared at a starting dilution of 1:10. Diluted sera were incubated for 60 min at room temperature with 100 TCID50 of each virus. The residual infectivity was then evaluated by overlaying the sera-virus mixture on MDCK cells grown in 96-well plates (4 replicates per dilution of sera). The plates were incubated for 4 days and scored for cytopathic effect (CPE). The antibody titers were expressed as the reciprocal of the dilution that completely neutralized virus infection.
Deep sequence analysis of viral variants.
Nasal wash samples (100 μL) from the day of peak viral replication for each ferret were used to infect MDCK cells grown in 24-well plates. Once CPE was present, the supernatant was collected, and 140 μL of supernatant was subjected to a viral RNA extraction using an QIAamp viral RNA extraction kit (Qiagen) according to the manufacturer’s instructions.
cDNA was synthesized and amplified using a SuperScript III one-step RT-PCR system with Platinum Taq high-fidelity DNA polymerase (Invitrogen, Ltd., Paisley, England) following the manufacturer’s instructions and using Opti1-F1 (5′-GTTACGCGCCAGCAAAAGCAGG-3′), Opti1-F2 (5′-GTTACGCGCCAGCGAAAGCAGG-3′), and Opti1-R1 (5′-GTTACGCGCCAGTAGAAACAAGG-3′) primers. Thermal cycling conditions included reverse transcription at 55°C for 2 min and 42°C for 60 min, initial denaturation at 94°C for 2 min, 5 cycles of 94°C for 30 s, 44°C for 30 s, and 68°C for 3.5 min, 26 cycles of 94°C for 30 s, 57°C for 30 s, and 68°C for 3.5 min, and final extension of 68°C for 10 min followed by a hold at 4°C. RT-PCR products were prepared for sequencing by purifying with an Isolate II PCR and gel kit (Bioline, Inc., London, England).
PCR products (500 ng) were digested with the NEBNext dsDNA fragmentase kit (New England BioLabs, Inc., Ipswich, MA). Fragmented DNA was end repaired and ligated with the Ion P1 adaptor and unique Ion Xpress barcode adaptors (Life Technologies, Co., Carlsbad, USA) using an NEBNext fast library prep kit (New England BioLabs, Inc.). Size selection was performed with double-sided and bead-based size selection. Agencourt AMPure XP beads (Beckman Coulter, Inc., Brea, CA) were used to selectively capture DNA between 100 and 250 bp. An Experion automated electrophoresis system (Bio-Rad Laboratories, Inc., Hercules, CA) was used to confirm fragment lengths and molar concentrations. Equal molar amounts of all libraries were pooled, and libraries were sequenced by an Ion Proton system (Life Technologies, Co.), generating 200-bp reads.
Raw data, FASTQ, and BAM files were generated by the Torrent Suite software (version 5.0.4; Life Technologies, Co.). Raw Ion Torrent FASTQ data were aligned to their respective influenza A subtype references using the STAR aligner (version 2.5.3a). Duplicate reads were marked and removed from the alignment files using Picard Tools MarkDuplicates (version 2.8.2) before single-nucleotide variants were called using an in-house variant caller (available on GitHub at https://github.com/GhedinLab/timo). Variant information was pulled if the variant was present at a position with at least 200× coverage and a relative frequency of 5% or greater. Consensus sequences were generated for each sample using the major nucleotide (>50% frequency) at positions with at least 5× coverage. An “N” was called at positions with coverage lower than 5×.
Mapping of host-adaptive changes to protein structures.
To identify nonsynonymous changes found from the deep-sequencing data that could have host-adaptive effects, we made use of FluSurver (https://flusurver.bii.a-star.edu.sg), where phenotypic substitutions, such as host-adaptive changes or changes in known antigenic sites, were compiled from 150 experimental studies. Changes found in hemagglutinin at nucleotide frequencies of at least 10, 25, and 50 were mapped onto the Protein Data Bank (PDB) structures 3UBN (H1N1pdm09, A/California/07/2009), 6PDX (H3N2, A/Switzerland/9715293/2013), 4WA2 (H3N8, A/seal/New Hampshire/179629/2011), and 4BSF (H7N9, A/Anhui/1/2013). Nonsynonymous changes shown in previous studies to affect host adaptations are colored in red, and all other changes are colored in green. The PDB structures were visualized using YASARA (https://pubmed.ncbi.nlm.nih.gov/29086303/) (58). The MAFFT alignment program (einsi option) was used to align the HA and NA protein sequences for the H1N1pdm09, H3N2, H3N8, and H7N9 subtypes (https://pubmed.ncbi.nlm.nih.gov/12136088/). The corresponding antigenic sites in different HA and NA subtypes were then identified and cross referenced with the sequencing data.
Biocontainment, dual-use-research of concern (DURC), animal protocols, and statistical analysis.
For studies with A/California/07/2009 (H1N1pdm09), A/Texas/50/2012 (H3N2), and A/seal/New Hampshire/179629/2011 (H3N8) viruses, viral culture and ferret studies were performed under biosafety level 2 conditions. All experiments with the A/Anhui/1/2013 (H7N9) influenza isolate were conducted in enhanced biosafety level 3 laboratories at the NIH. All animal studies and procedures were conducted in compliance with relevant regulations and guidelines and were approved by the National Institute of Allergy and Infectious Diseases Animal Care and Use Committee and the NIH Institutional Biosafety Committee. Statistical analysis was not performed, as the number of animals utilized was only sufficient to achieve significance between viruses that had 100% and 0% transmission efficiency, and none of the influenza isolates evaluated exhibited 0% transmission efficiency (42).
Prior to performing deep sequencing of viruses, after completion of the data analysis and prior to submission of the manuscript for peer review, all of the experimental data were reviewed by the National Institutes of Allergy and Infectious Diseases (NIAID) DURC/P3CO committee as well as the NIH Intramural Institutional Review Entity (IRE) responsible for oversight of dual-use-research of concern (DURC). After completion of this review, permission was granted to publish the findings.
ACKNOWLEDGMENTS
T.C.S. and K.S. designed the experiments. T.C.S., E.W.L., and R.C. performed the experimental studies. D.R.P., K.E.E.J., and E.G. performed sequence analyses. R.T.C.L. and S.M.-S. performed mapping of host-adaptive mutations. T.C.S. and K.S. drafted and revised the manuscript.
All declare that we have no conflicts of interest.
We acknowledge Justin Bahl for performing deep sequencing of the nasal wash samples and the Comparative Medicine Branch of NIAID, NIH, for assistance and support with animal studies.
This research was supported by the Intramural Research Program of the NIH, NIAID, and by the US Department of Agriculture (USDA) National Institute of Food and Agriculture, Hatch project 4771. R.T.C.L. was supported by National Medical Research Council (NMRC) grant MOH-OFIRG19nov-0013/MOH-000565-00 to S.M.-S.
Footnotes
This article is a direct contribution from Kanta Subbarao, a Fellow of the American Academy of Microbiology, who arranged for and secured reviews by Terrence Tumpey, Centers for Disease Control and Prevention, and Veronika von Messling, Federal Ministry of Education and Research.
Contributor Information
Troy C. Sutton, Email: tcs38@psu.edu.
Kanta Subbarao, Email: kanta.subbarao@influenzacentre.org.
Xiang-Jin Meng, Virginia Polytechnic Institute and State University.
REFERENCES
- 1.Richard M, Fouchier RAM. 2016. Influenza A virus transmission via respiratory aerosols or droplets as it relates to pandemic potential. FEMS Microbiol Rev 40:68–85. doi: 10.1093/femsre/fuv039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tellier R. 2006. Review of aerosol transmission of influenza A virus. Emerg Infect Dis 12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tellier R. 2009. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface Suppl 6:S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belser JA, Eckert AM, Tumpey TM, Maines TR. 2016. Complexities in ferret influenza virus pathogenesis and transmission models. Microbiol Mol Biol Rev 80:733–744. doi: 10.1128/MMBR.00022-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu Q, Wang W, Cheng X, Zengel J, Jin H. 2010. Influenza H1N1 A/Solomon Island/3/06 virus receptor binding specificity correlates with virus pathogenicity, antigenicity, and immunogenicity in ferrets. J Virol 84:4936–4945. doi: 10.1128/JVI.02489-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Graaf M, Fouchier RA. 2014. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J 33:823–841. doi: 10.1002/embj.201387442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicholls JM, Bourne AJ, Chen H, Guan Y, Peiris JS. 2007. Sialic acid receptor detection in the human respiratory tract: evidence for widespread distribution of potential binding sites for human and avian influenza viruses. Respir Res 8:73. doi: 10.1186/1465-9921-8-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munster VJ, de Wit E, van den Brand JMA, Herfst S, Schrauwen EJA, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, Kuiken T, Osterhaus ADME, Fouchier RAM. 2009. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science 325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pappas C, Yang H, Carney PJ, Pearce MB, Katz JM, Stevens J, Tumpey TM. 2015. Assessment of transmission, pathogenesis and adaptation of H2 subtype influenza viruses in ferrets. Virology 477:61–71. doi: 10.1016/j.virol.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solórzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, García-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 11.Maines TR, Chen L-M, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcón A, Nguyen TH, Mai LQ, Sedyaningsih ER, Harun S, Tumpey TM, Donis RO, Cox NJ, Subbarao K, Katz JM. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci USA 103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO. 2020. Tool for influenza pandemic risk assessment (TIPRA). https://www.who.int/publications/i/item/tool-for-influenza-pandemic-risk-assessment-(tipra)-2nd-edition. Accessed 9 October 2022.
- 13.CDC. 2016. Influenza Risk Assessment Tool (IRAT). https://www.cdc.gov/flu/pandemic-resources/national-strategy/risk-assessment.htm. Accessed 7 July 2017.
- 14.Herfst S, Schrauwen EJA, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lakdawala SS, Lamirande EW, Suguitan AL, Wang W, Santos CP, Vogel L, Matsuoka Y, Lindsley WG, Jin H, Subbarao K. 2011. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog 7:e1002443. doi: 10.1371/journal.ppat.1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutton TC, Finch C, Shao H, Angel M, Chen H, Capua I, Cattoli G, Monne I, Perez DR. 2014. Airborne transmission of highly pathogenic H7N1 influenza virus in ferrets. J Virol 88:6623–6635. doi: 10.1128/JVI.02765-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belser JA, Gustin KM, Pearce MB, Maines TR, Zeng H, Pappas C, Sun X, Carney PJ, Villanueva JM, Stevens J, Katz JM, Tumpey TM. 2013. Pathogenesis and transmission of avian influenza A (H7N9) virus in ferrets and mice. Nature 501:556–559. doi: 10.1038/nature12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richard M, Schrauwen EJA, de Graaf M, Bestebroer TM, Spronken MIJ, van Boheemen S, de Meulder D, Lexmond P, Linster M, Herfst S, Smith DJ, van den Brand JM, Burke DF, Kuiken T, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM. 2013. Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature 501:560–563. doi: 10.1038/nature12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, Takashita E, McBride R, Noda T, Hatta M, Imai H, Zhao D, Kishida N, Shirakura M, de Vries RP, Shichinohe S, Okamatsu M, Tamura T, Tomita Y, Fujimoto N, Goto K, Katsura H, Kawakami E, Ishikawa I, Watanabe S, Ito M, Sakai-Tagawa Y, Sugita Y, Uraki R, Yamaji R, Eisfeld AJ, Zhong G, Fan S, Ping J, Maher EA, Hanson A, Uchida Y, Saito T, Ozawa M, Neumann G, Kida H, Odagiri T, Paulson JC, Hasegawa H, Tashiro M, Kawaoka Y, et al. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501:551–555. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaraket H, Baranovich T, Kaplan BS, Carter R, Song M-S, Paulson JC, Rehg JE, Bahl J, Crumpton JC, Seiler J, Edmonson M, Wu G, Karlsson E, Fabrizio T, Zhu H, Guan Y, Husain M, Schultz-Cherry S, Krauss S, McBride R, Webster RG, Govorkova EA, Zhang J, Russell CJ, Webby RJ. 2015. Mammalian adaptation of influenza A(H7N9) virus is limited by a narrow genetic bottleneck. Nat Commun 6:6553. doi: 10.1038/ncomms7553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Q, Shi J, Deng G, Guo J, Zeng X, He X, Kong H, Gu C, Li X, Liu J, Wang G, Chen Y, Liu L, Liang L, Li Y, Fan J, Wang J, Li W, Guan L, Li Q, Yang H, Chen P, Jiang L, Guan Y, Xin X, Jiang Y, Tian G, Wang X, Qiao C, Li C, Bu Z, Chen H. 2013. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science 341:410–414. doi: 10.1126/science.1240532. [DOI] [PubMed] [Google Scholar]
- 23.Zhu H, Wang D, Kelvin DJ, Li L, Zheng Z, Yoon S-W, Wong S-S, Farooqui A, Wang J, Banner D, Chen R, Zheng R, Zhou J, Zhang Y, Hong W, Dong W, Cai Q, Roehrl MHA, Huang SSH, Kelvin AA, Yao T, Zhou B, Chen X, Leung GM, Poon LLM, Webster RG, Webby RJ, Peiris JSM, Guan Y, Shu Y. 2013. Infectivity, transmission, and pathology of human-isolated H7N9 influenza virus in ferrets and pigs. Science 341:183–186. doi: 10.1126/science.1239844. [DOI] [PubMed] [Google Scholar]
- 24.Zhou L, Ren R, Yang L, Bao C, Wu J, Wang D, Li C, Xiang N, Wang Y, Li D, Sui H, Shu Y, Feng Z, Li Q, Ni D. 2017. Sudden increase in human infection with avian influenza A(H7N9) virus in China, September-December 2016. Western Pac Surveill Response J 8:6–14. doi: 10.5365/WPSAR.2017.8.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karlsson EA, Ip HS, Hall JS, Yoon SW, Johnson J, Beck MA, Webby RJ, Schultz-Cherry S. 2014. Respiratory transmission of an avian H3N8 influenza virus isolated from a harbour seal. Nat Commun 5:4791. doi: 10.1038/ncomms5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Shi J, Guo J, Deng G, Zhang Q, Wang J, He X, Wang K, Chen J, Li Y, Fan J, Kong H, Gu C, Guan Y, Suzuki Y, Kawaoka Y, Liu L, Jiang Y, Tian G, Li Y, Bu Z, Chen H. 2014. Genetics, receptor binding property, and transmissibility in mammals of naturally isolated H9N2 avian influenza viruses. PLoS Pathog 10:e1004508. doi: 10.1371/journal.ppat.1004508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buhnerkempe MG, Gostic K, Park M, Ahsan P, Belser JA, Lloyd-Smith JO. 2015. Mapping influenza transmission in the ferret model to transmission in humans. eLife 4:e07969. doi: 10.7554/eLife.07969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belser JA, Lau EHY, Barclay W, Barr IG, Chen H, Fouchier RAM, Hatta M, Herfst S, Kawaoka Y, Lakdawala SS, Lee LYY, Neumann G, Peiris M, Perez DR, Russell C, Subbarao K, Sutton TC, Webby RJ, Yang H, Yen H-L, Blanchard E, Maines TR, Choy K-T, Sia SF, Su W, Frise R, Zhou J, Hurt AC, Li C, Bestebroer T, de Meulder D, Lexmond P, Chiba S, Bhagwat A, Jones JE, Kormuth KA, Le Sage V, Caceres CJ, Carnaccini S, Ferreri LM, Geiger G, DeBeauchamp JL, Hu M, Jeevan T, Kercher LA, Patel DR, Septer KM, Sim DG, Working group on the standardization of the ferret model for influenza risk assessment. 2022. Robustness of the ferret model for influenza risk assessment studies: a cross-laboratory exercise. mBio 13:e0117422. doi: 10.1128/mbio.01174-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, Griffin J, Baggaley RF, Jenkins HE, Lyons EJ, Jombart T, Hinsley WR, Grassly NC, Balloux F, Ghani AC, Ferguson NM, Rambaut A, Pybus OG, Lopez-Gatell H, Alpuche-Aranda CM, Chapela IB, Zavala EP, Guevara DME, Checchi F, Garcia E, Hugonnet S, Roth C, The WHO Rapid Pandemic Assessment Collaboration. 2009. Pandemic potential of a strain of influenza A (H1N1): early findings. Science 324:1557–1561. doi: 10.1126/science.1176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Itoh Y, Shinya K, Kiso M, Watanabe T, Sakoda Y, Hatta M, Muramoto Y, Tamura D, Sakai-Tagawa Y, Noda T, Sakabe S, Imai M, Hatta Y, Watanabe S, Li C, Yamada S, Fujii K, Murakami S, Imai H, Kakugawa S, Ito M, Takano R, Iwatsuki-Horimoto K, Shimojima M, Horimoto T, Goto H, Takahashi K, Makino A, Ishigaki H, Nakayama M, Okamatsu M, Takahashi K, Warshauer D, Shult PA, Saito R, Suzuki H, Furuta Y, Yamashita M, Mitamura K, Nakano K, Nakamura M, Brockman-Schneider R, Mitamura H, Yamazaki M, Sugaya N, Suresh M, Ozawa M, Neumann G, Gern J, Kida H, et al. 2009. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 460:1021–1025. doi: 10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. 2009. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science 325:484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oh DY, Lowther S, McCaw JM, Sullivan SG, Leang S-K, Haining J, Arkinstall R, Kelso A, Mcvernon J, Barr IG, Middleton D, Hurt AC. 2014. Evaluation of oseltamivir prophylaxis regimens for reducing influenza virus infection, transmission and disease severity in a ferret model of household contact. J Antimicrob Chemother 69:2458–2469. doi: 10.1093/jac/dku146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore IN, Lamirande EW, Paskel M, Donahue D, Kenney H, Qin J, Subbarao K. 2014. Severity of clinical disease and pathology in ferrets experimentally infected with influenza viruses is influenced by inoculum volume. J Virol 88:13879–13891. doi: 10.1128/JVI.02341-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. 1979. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol 110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 35.Riley RL. 1974. Airborne infection. Am J Med 57:466–475. doi: 10.1016/0002-9343(74)90140-5. [DOI] [PubMed] [Google Scholar]
- 36.Salgado CD, Farr BM, Hall KK, Hayden FG. 2002. Influenza in the acute hospital setting. Lancet Infect Dis 2:145–155. doi: 10.1016/S1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 37.Herlocher ML, Elias S, Truscon R, Harrison S, Mindell D, Simon C, Monto AS. 2001. Ferrets as a transmission model for influenza: sequence changes in HA1 of type A (H3N2) virus. J Infect Dis 184:542–546. doi: 10.1086/322801. [DOI] [PubMed] [Google Scholar]
- 38.Frise R, Bradley K, van Doremalen N, Galiano M, Elderfield RA, Stilwell P, Ashcroft JW, Fernandez-Alonso M, Miah S, Lackenby A, Roberts KL, Donnelly CA, Barclay WS. 2016. Contact transmission of influenza virus between ferrets imposes a looser bottleneck than respiratory droplet transmission allowing propagation of antiviral resistance. Sci Rep 6:29793. doi: 10.1038/srep29793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sorrell EM, Wan H, Araya Y, Song H, Perez DR. 2009. Minimal molecular constraints for respiratory droplet transmission of an avian-human H9N2 influenza A virus. Proc Natl Acad Sci USA 106:7565–7570. doi: 10.1073/pnas.0900877106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gulati S, Smith DF, Cummings RD, Couch RB, Griesemer SB, St George K, Webster RG, Air GM. 2013. Human H3N2 influenza viruses isolated from 1968 to 2012 show varying preference for receptor substructures with no apparent consequences for disease or spread. PLoS One 8:e66325. doi: 10.1371/journal.pone.0066325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Belser JA, Barclay W, Barr I, Fouchier RAM, Matsuyama R, Nishiura H, Peiris M, Russell CJ, Subbarao K, Zhu H, Yen H-L. 2018. Ferrets as models for influenza virus transmission studies and pandemic risk assessments. Emerg Infect Dis 24:965–971. doi: 10.3201/eid2406.172114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nishiura H, Yen HL, Cowling BJ. 2013. Sample size considerations for one-to-one animal transmission studies of the influenza A viruses. PLoS One 8:e55358. doi: 10.1371/journal.pone.0055358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu Y, Childs RA, Matrosovich T, Wharton S, Palma AS, Chai W, Daniels R, Gregory V, Uhlendorff J, Kiso M, Klenk H-D, Hay A, Feizi T, Matrosovich M. 2010. Altered receptor specificity and cell tropism of D222G hemagglutinin mutants isolated from fatal cases of pandemic A(H1N1) 2009 influenza virus. J Virol 84:12069–12074. doi: 10.1128/JVI.01639-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mak GC, Au KW, Tai LS, Chuang KC, Cheng KC, Shiu TC, Lim W. 2010. Association of D222G substitution in haemagglutinin of 2009 pandemic influenza A (H1N1) with severe disease. Euro Surveill 15:19534. doi: 10.2807/ese.15.14.19534-en. [DOI] [PubMed] [Google Scholar]
- 45.Belser JA, Jayaraman A, Raman R, Pappas C, Zeng H, Cox NJ, Katz JM, Sasisekharan R, Tumpey TM. 2011. Effect of D222G mutation in the hemagglutinin protein on receptor binding, pathogenesis and transmissibility of the 2009 pandemic H1N1 influenza virus. PLoS One 6:e25091. doi: 10.1371/journal.pone.0025091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dakhave M, Khirwale A, Patil K, Kadam A, Potdar V. 2013. Whole-genome sequence analysis of postpandemic influenza A(H1N1)pdm09 virus isolates from India. Genome Announc 1:e00727-13. doi: 10.1128/genomeA.00727-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han Y, Sun N, Lv Q-Y, Liu D-H, Liu D-P. 2016. Molecular epidemiology and phylogenetic analysis of HA gene of influenza A(H1N1)pdm09 strain during 2010–2014 in Dalian, North China. Virus Genes 52:606–612. doi: 10.1007/s11262-016-1358-2. [DOI] [PubMed] [Google Scholar]
- 48.Nguyen HKL, Nguyen PTK, Nguyen TC, Hoang PVM, Le TT, Vuong CD, Nguyen AP, Tran LTT, Nguyen BG, Lê MQ. 2015. Virological characterization of influenza H1N1pdm09 in Vietnam, 2010–2013. Influenza Other Respir Viruses 9:216–224. doi: 10.1111/irv.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guarnaccia T, Carolan LA, Maurer-Stroh S, Lee RTC, Job E, Reading PC, Petrie S, McCaw JM, McVernon J, Hurt AC, Kelso A, Mosse J, Barr IG, Laurie KL. 2013. Antigenic drift of the pandemic 2009 A(H1N1) influenza virus in A ferret model. PLoS Pathog 9:e1003354. doi: 10.1371/journal.ppat.1003354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilson JR, Belser JA, DaSilva J, Guo Z, Sun X, Gansebom S, Bai Y, Stark TJ, Chang J, Carney P, Levine MZ, Barnes J, Stevens J, Maines TR, Tumpey TM, York IA. 2017. An influenza A virus (H7N9) anti-neuraminidase monoclonal antibody protects mice from morbidity without interfering with the development of protective immunity to subsequent homologous challenge. Virology 511:214–221. doi: 10.1016/j.virol.2017.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu L, Bao L, Deng W, Dong L, Zhu H, Chen T, Lv Q, Li F, Yuan J, Xiang Z, Gao K, Xu Y, Huang L, Li Y, Liu J, Yao Y, Yu P, Li X, Huang W, Zhao X, Lan Y, Guo J, Yong W, Wei Q, Chen H, Zhang L, Qin C. 2014. Novel avian-origin human influenza A(H7N9) can be transmitted between ferrets via respiratory droplets. J Infect Dis 209:551–556. doi: 10.1093/infdis/jit474. [DOI] [PubMed] [Google Scholar]
- 52.Yamayoshi S, Yamada S, Fukuyama S, Murakami S, Zhao D, Uraki R, Watanabe T, Tomita Y, Macken C, Neumann G, Kawaoka Y. 2014. Virulence-affecting amino acid changes in the PA protein of H7N9 influenza A viruses. J Virol 88:3127–3134. doi: 10.1128/JVI.03155-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baz M, Paskel M, Matsuoka Y, Zengel JR, Cheng X, Treanor JJ, Jin H, Subbarao K. 2015. A single dose of an avian H3N8 influenza virus vaccine is highly immunogenic and efficacious against a recently emerged seal influenza virus in mice and ferrets. J Virol 89:6907–6917. doi: 10.1128/JVI.00280-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. American J Hygiene 27:493–497. doi: 10.1093/oxfordjournals.aje.a118408. [DOI] [Google Scholar]
- 55.CDC. 2021. Influenza SARS-CoV-2 Multiplex Assay and Required Supplies. https://www.cdc.gov/coronavirus/2019-ncov/lab/multiplex.html. Accessed 9 October 2022.
- 56.WHO. 2011. Manual for the laboratory diagnosis and virological surveillance of influenza. https://www.who.int/publications/i/item/manual-for-the-laboratory-diagnosis-and-virological-surveillance-of-influenza. Accessed 18 April 2016.
- 57.Chen GL, Lamirande EW, Yang C-F, Jin H, Kemble G, Subbarao K. 2010. Evaluation of replication and cross-reactive antibody responses of H2 subtype influenza viruses in mice and ferrets. J Virol 84:7695–7702. doi: 10.1128/JVI.00511-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Land H, Humble MS. 2018. YASARA: a tool to obtain structural guidance in biocatalytic investigations. Methods Mol Biol 1685:43–67. doi: 10.1007/978-1-4939-7366-8_4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hemagglutination inhibition, neutralization assay, and viral shedding results for all experiments. Download Table S1, PDF file, 0.1 MB (75.6KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/California/07/2009 (H1N1pdm09). Download Table S2, PDF file, 0.02 MB (25.3KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/Anhui/1/2013 (H7N9). Download Table S3, PDF file, 0.02 MB (26.2KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/Texas/50/2012 (H3N2). Download Table S4, PDF file, 0.02 MB (18.9KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
List of all nonsynonymous and synonymous mutations identified during sequential transmission experiments with A/harbor seal/New Hampshire/179629/2011 (H3N8). Download Table S5, PDF file, 0.02 MB (21.1KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Summary of mutations in antigenic sites of HA and NA during sequential transmission. Download Table S6, PDF file, 0.02 MB (16.5KB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, RC2 ferrets at nucleotide cutoff frequency of 50%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S1, PDF file, 1.9 MB (1.9MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, and RC2 ferrets at a nucleotide cutoff frequency of 25%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S2, PDF file, 1.9 MB (1.9MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.
Nonsynonymous changes in the surface glycoprotein HA for all 4 viruses grouped by DI, RC1, and RC2 ferrets at a nucleotide cutoff frequency of 10%. Changes are shown in the PDB structures (3UBN for H1N1pdm09 A/California/07/2009, 6PDX for H3N2 A/Switzerland/9715293/2013, 4WA2 for H3N8 A/seal/New Hampshire/179629/2011, and 4BSF for H7N9, A/Anhui/1/2013) if they are found in any of the 6 ferret replicates in each of the DI, RC1, and RC2 ferret groups. Sialic acids are represented as magenta sticks and surfaces, host-adaptive changes that are identified in previous studies curated by FluSurver (https://flusurver.bii.a-star.edu.sg) are represented as red sticks and surfaces, and all other amino acid changes are represented as green sticks and surfaces. When host-adaptive changes are observed in some other proteins (i.e., PB2 S714N and PA N409S in H7N9 virus), they are labeled in red beside the corresponding structures. Download FIG S3, PDF file, 1.9 MB (2MB, pdf) .
This is a work of the U.S. Government and is not subject to copyright protection in the United States. Foreign copyrights may apply.