Abstract
Background
The WHO Comprehensive Mental Health Action Plan 2013–2030 encourages routine collection and reporting of a set of essential mental health indicators, including the availability of psychotropic medicines. The global monitoring of country-level psychotropic medicine consumption trends can provide information on the extent of the availability of psychotropic medicines. The primary objective of this study was to investigate global trends in psychotropic medicines consumption from 2008 to 2019 across 65 countries and regions according to country income level and geographical region.
Methods
In this longitudinal trends study, we used pharmaceutical sales data from the IQVIA-Multinational Integrated Data Analysis System (IQVIA-MIDAS). We analysed monthly sales data of psychotropic medicines between Jan 1, 2008, and Dec 31, 2019. Total psychotropic medicine consumption included sales of antidepressants, antipsychotics, tranquilisers, sedatives or hypnotics, and mood stabilisers. Population estimates of each country or region (eight lower-middle-income countries, 19 upper-middle-income countries, and 38 high-income countries) were based on the UN World Population Prospects 2019 report. Average annual sales trends of psychotropic medicines, expressed as defined daily dose (DDD) per 1000 inhabitants per day, were estimated using a random-effects model adjusted for income level and region. Relative changes in the annual consumption of psychotropic medicines by income, expressed as DDD per 1000 inhabitants per day, were assessed as percentage change for each medicine class.
Findings
Psychotropic medicine sales increased from 28·54 DDD per 1000 inhabitants per day in 2008 to 34·77 DDD per 1000 inhabitants per day in 2019, corresponding to a 4·08% (95% CI 2·96–5·21) relative average increase annually. The absolute annual increase was greater in high-income countries (3·31 DDD per 1000 inhabitants per day, 95% CI 3·01–3·61) compared with upper-middle-income countries (1·94 DDD per 1000 inhabitants per day, 1·45–2·44) and low-middle-income countries (0·88 DDD per 1000 inhabitants per day, 0·62–1·13; p<0·0001). The relative average annual increase in psychotropic medicine sales from 2008 to 2019 was greater in upper-middle-income countries (7·88%, 95% CI 6·99–8·77) than in lower-middle-income countries (2·90%, 2·40–3·39) and high-income countries (1·02%, 0·80–1·24). In 2019, the regional consumption of psychotropic medicines varied greatly, with the highest sales of all psychotropic medicine classes reported in northern America (167·54 DDD per 1000 inhabitants per day) and lowest sales reported in Asia (5·59 DDD per 1000 inhabitants per day). 17 countries had very low consumption of psychotropic medicines in 2019, including high-income countries and countries with a high prevalence of mental disorders.
Interpretation
The consumption of psychotropic medicines has increased over a 12-year period, and although the absolute growth rate was highest in high-income countries, the relative growth is highest in middle-income countries and especially upper-middle-income countries. Disparities in psychotropic medicine consumption of countries can only partly be explained by geographical location and income. Greater efforts are needed to increase the availability of psychotropic medicines in countries with very low consumption, which is probably due to financial or cultural reasons as well as scarcity of trained health-care professionals to prescribe psychotropic medicines.
Funding
None.
Introduction
Globally, mental disorders such as depression and anxiety are among the top ten causes of years lived with disability in people aged 10–49 years.1, 2, 3 Pharmacological treatment of mental disorders is effective and often used as first-line treatment in countries where psychological interventions are difficult to access.3 WHO has recognised that the health systems of individual countries across the world have not yet adequately responded to the burden of mental disorders and that there is often a substantial gap between the need for mental health treatment and its availability, especially in low-income and middle-income countries.4 As part of the WHO Comprehensive Mental Health Action Plan 2013–2030, targets have been set to increase the output of global research on mental health and to encourage routine collection and reporting of a core set of mental health indicators.4, 5 Routine monitoring of the availability of psychotropic medicines in individual countries is specifically mentioned as a mental health indicator of health and social system actions.4 The global monitoring of country-level psychotropic consumption trends can provide information on the extent of pharmacological interventions for mental disorders and the availability of psychotropic medicines. Moreover, psychotropic medicine consumption data can be used to inform future policy evaluation, especially in middle-income countries, where these data are scarce.4 To our knowledge, there are no global surveillance studies to track and compare country-level use of psychotropic medicines. The few published international comparison studies on the consumption of psychotropic medicines are limited to one type of psychotropic drug.6, 7, 8
Research in context.
Evidence before this study
We searched PubMed for studies written in English published between Jan 1, 1990, and Jan 19, 2021, with the following terms: (((((treatment) OR (medication)) AND (sales)) OR (MIDAS)) AND (trend)) AND (mental health disorder). The search yielded 299 articles. We excluded articles deemed not to be relevant on the basis of their titles. We reviewed abstracts of the remaining articles to identify potentially relevant articles and scanned reference lists of relevant articles. The primary criterion was that the study reported trends in psychotropic sales or consumption. Most previous studies were from Europe, with a few studies comparing psychotropic medicine consumption in 27 countries. However, psychotropic medicine consumption in these multinational studies was often based on self-reported use or individual-level prescription data. Most studies reported trends in the consumption of antidepressants, with only two studies comparing the consumption of tranquilisers in multiple countries. Although a general increase in psychotropic medicine sales was observed in most studies, the consumption of hypnotics decreased.
Added value of this study
This is the largest and most up-to-date assessment of consumption trends of all major classes of psychotropic medicines for 65 countries and regions from 2008 to 2019, grouped according to country income level (lower-middle, upper-middle, and high) and geographical region. This comprehensive description of the epidemiology of psychotropic medicine consumption identified countries with very low consumption of psychotropic medicines; provided baseline consumption rates that can be used as a benchmark to measure and monitor future global, regional, and national use of psychotropic medicines; and assessed the relationship between psychotropic medicine consumption and the prevalence of mental disorders, life expectancy, and health expenditure at the country level. We identified 17 countries with very low consumption of psychotropic medicines in 2019. These countries are unlikely to provide sufficient access to psychotropic medicines for patients. The reasons for such low consumption are multifactorial, with both the direction and the strength of the association between psychotropic medicine consumption and the prevalence of mental disorders, life expectancy, and health expenditure varying according to country income level.
Implications of all the available evidence
The consumption of antidepressants, mood stabilisers, and antipsychotics has increased from 2008 to 2019, suggesting improved overall access to these medicines, but consumption rates of individual countries varied substantially. Disparities in access to psychotropic medicines remain a challenge across most of the world, especially in middle-income countries. Strategies to improve access to psychotropic medicines that should be considered include training health-care workers who can prescribe cost-effective, essential, psychotropic medicines; public education; and involving community leaders to promote appropriate understanding of psychotropic medicine use. Our study findings can be used as a foundation to evaluate future interventions designed to improve appropriate use of psychotropic medicines.
To improve our understanding of global trends in medication treatment for mental health conditions in high-income countries, lower-middle-income countries, and upper-middle-income countries, we aimed to describe the consumption of psychotropic medicines in 65 countries and regions from 2008 to 2019. Additionally, we set out to capture any changes in consumption over time by geographical location and in relation to the prevalence of mental disorders, life expectancy, and health expenditure. Last, we identified countries that have very low consumption of psychotropic medicines, which suggests poor access to psychotropic medicine therapy.
Methods
Data sources
Psychotropic medicine sales data (based on European Pharmaceutical Marketing Research Association [EphMRA] Anatomical Classification of Pharmaceutical Products listed in the appendix p 2) were obtained from the IQVIA Multinational Integrated Data Analysis System (IQVIA-MIDAS) database up to Sept 30, 2020. MIDAS captures global data on the volume of specific pharmaceutical products sold to retail and hospital pharmacies, and enables comparisons of national-level sales audits by providing international standardisation of sales value and volumes, and medical prescription data.9 Data sources differ by country and data type, but are usually a combination of sales data from manufacturers (direct sales) and wholesalers; in some countries, sales data are also acquired from hospital and retail pharmacies (appendix pp 3–5). The average coverage has been shown to be 88%,10 with adjustments made to estimate the total sales volume based on knowledge of market share of the contributing retail or hospital pharmacies and wholesalers.11 Data from IQVIA-MIDAS have been internally validated from alternative sources of sales data and are used for the evaluation of global medicine consumption patterns.12 Consumption of both generic and brand products is included. The database does not contain patient-level data; thus, no information on indications and patient demographics was available. Hence, institutional review board approval was not required.
We categorised psychotropic medicines into five major medicine classes: antidepressants, mood stabilisers, antipsychotics, tranquilisers, and sedatives or hypnotics. We excluded ADHD medications as they are mainly used in children and adolescents, which make direct comparisons with other psychotropic medicines inappropriate. Antidepressants were subdivided, mainly according to mode of action, into the following groups:13 non-selective monoamine reuptake inhibitors (tricyclic), SSRIs, SNRIs, monoamine oxidase inhibitors, and antidepressants not otherwise categorised (other; appendix p 6). Antipsychotics were divided into typical (N5A9) and atypical (N5A1) agents.
Prevalence of mental disorders and life expectancy was derived from the Global Burden of Diseases, Injuries, and Risk Factors Study 2019.14 Income level and country health-care expenditure (defined as percentage of the gross domestic product) estimates for each country were obtained from the World Bank.15 Data from low-income countries were not available. Data from 2019 were tabulated according to UN geographical regions (Africa, Asia, Europe, Latin America and the Caribbean, northern America, and Oceania), and subregion (western Asia).16
Data analysis
The sales data of selected medicine classes were stratified on the basis of country income level (ie, lower-middle income, upper-middle income, and high income) to investigate how consumption trends vary with country income level. We calculated both the standard units per person and the defined daily dose (DDD) per 1000 inhabitants per day for each year using the sales volume data and national population data.17 The DDD is the assumed average maintenance dose per day for a drug used for its main indication in adults and is only available for single-molecule products. As such, combination products and herbal products were excluded from these analyses. Population estimates of each country were obtained from the UN World Population Prospects 2019 report.16 Of the 65 countries and regions, 27 were classified as middle-income countries (eight lower-middle-income countries and 19 upper-middle-income countries), and 38 as high-income countries. For each medicine class, we calculated the absolute changes in sales for each year throughout the study period using a random-effects model adjusted for income level and region. Annual relative changes in the DDD per 1000 inhabitants per day were assessed as percentage change for each medicine class.
Psychotropic medicine sales from 2019 were compared with the prevalence of mental disorders, with life expectancy, and with health expenditure using fixed-effects panel regression analysis. We also identified countries that had very low consumption of psychotropic medicines, defined as 25th percentile of DDD per 1000 inhabitants per day in 2019. Data were analysed using Stata (version 16).
Role of the funding source
There was no funding source for this study.
Results
Globally, the total consumption of psychotropic medicines increased from 28·54 DDD per 1000 inhabitants per day in 2008 to 34·77 DDD per 1000 inhabitants per day in 2019 (table 1 ), corresponding to a relative average increase of 4·08% (95% CI 2·96 to 5·21) annually. The greatest increase in DDD per 1000 inhabitants per day over time was seen for antidepressants (table 2 ), corresponding to a relative average increase per year of 3·50% (95% CI 3·23 to 3·76), followed by antipsychotics (relative average increase per year of 2·49%, 2·22 to 2·75). A relative average decrease per year was seen for tranquilisers (–0·99%, 95% CI −1·41 to 0·57) and sedatives or hypnotics (–0·91%, −1·41 to 0·41). Consumption of SSRIs was 8·79 DDD per 1000 inhabitants per day in 2008 and remained high during the study period, with an average annual increase of 0·26 DDD per 1000 inhabitants per day (95% CI 0·22 to 0·31). An increase in consumption was observed for SNRIs, antidepressants not otherwise categorised, and antipsychotics (table 1). The consumption of tricyclic antidepressants, mood stabilisers, tranquilisers, sedatives, and hypnotics decreased during the study period.
Table 1.
Global trends of psychotropic medicine consumption by medicine class in 65 middle-income and high-income countries and regions, 2008–19
|
Consumption (DDD per 1000 inhabitants per day) |
Average annual change in DDD per 1000 inhabitants per day (95% CI) | p value for income level | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||||
| All psychotropics | 28·54 | 9·61 | 30·05 | 31·31 | 30·87 | 31·81 | 32·00 | 32·62 | 33·05 | 33·54 | 34·12 | 34·77 | 2·61 (2·37 to 2·85) | <0·0001 | |
| Lower-middle income | 4·97 | 5·24 | 5·43 | 5·89 | 5·83 | 6·03 | 5·98 | 6·25 | 6·53 | 6·59 | 6·97 | 6·77 | 0·88 (0·62 to 1·13) | .. | |
| Upper-middle income | 5·81 | 6·24 | 6·79 | 7·96 | 8·78 | 9·28 | 9·85 | 10·55 | 10·94 | 11·70 | 12·50 | 13·52 | 1·94 (1·45 to 2·44) | .. | |
| High income | 108·42 | 112·21 | 114·57 | 116·92 | 113·73 | 117·11 | 117·33 | 118·80 | 119·94 | 121·04 | 121·91 | 123·61 | 3·31 (3·01 to 3·61) | .. | |
| All antidepressants | 13·20 | 13·87 | 14·38 | 15·16 | 14·98 | 15·68 | 16·12 | 16·83 | 17·39 | 17·99 | 18·77 | 19·76 | 1·33 (1·22 to 1·44) | 0·0003 | |
| Lower-middle income | 1·38 | 1·53 | 1·65 | 1·84 | 1·95 | 2·07 | 2·19 | 2·34 | 2·49 | 2·62 | 2·86 | 2·95 | 0·43 (0·33 to 0·52) | .. | |
| Upper-middle income | 2·45 | 2·69 | 3·03 | 3·56 | 3·95 | 4·26 | 4·62 | 5·08 | 5·40 | 5·94 | 6·44 | 7·09 | 0·70 (0·58 to 0·82) | .. | |
| High income | 51·98 | 54·42 | 56·71 | 58·72 | 57·18 | 59·77 | 61·07 | 63·29 | 65·22 | 66·97 | 69·43 | 72·93 | 1·84 (1·68 to 2·00) | .. | |
| SSRI antidepressants | 8·79 | 9·26 | 9·61 | 10·15 | 9·94 | 10·34 | 10·62 | 11·06 | 11·40 | 11·72 | 12·19 | 12·82 | 0·26 (0·22 to 0·31) | 0·0008 | |
| Lower-middle income | 0·87 | 0·97 | 1·05 | 1·18 | 1·26 | 1·33 | 1·41 | 1·50 | 1·60 | 1·69 | 1·84 | 1·93 | 0·13 (0·09 to 0·17) | .. | |
| Upper-middle income | 1·82 | 2·00 | 2·26 | 2·67 | 2·92 | 3·15 | 3·39 | 3·75 | 3·95 | 4·31 | 4·59 | 5·00 | 0·15 (0·10 to 0·20) | .. | |
| High income | 34·31 | 36·00 | 37·52 | 38·84 | 37·40 | 38·80 | 39·61 | 40·85 | 41·96 | 42·77 | 44·31 | 46·47 | 0·35 (0·28 to 0·42) | .. | |
| SNRI antidepressants | 1·80 | 1·92 | 2·01 | 2·13 | 2·19 | 2·33 | 2·44 | 2·62 | 2·74 | 2·90 | 3·08 | 3·32 | 0·09 (0·08 to 0·11) | 0·0048 | |
| Lower-middle income | 0·09 | 0·12 | 0·14 | 0·17 | 0·19 | 0·21 | 0·23 | 0·24 | 0·26 | 0·29 | 0·32 | 0·34 | 0·02 (0·01 to 0·03) | .. | |
| Upper-middle income | 0·19 | 0·23 | 0·27 | 0·33 | 0·39 | 0·46 | 0·55 | 0·64 | 0·71 | 0·82 | 0·98 | 1·16 | 0·05 (0·03 to 0·06) | .. | |
| High income | 7·50 | 7·96 | 8·37 | 8·75 | 8·86 | 9·39 | 9·74 | 10·35 | 10·77 | 11·29 | 11·78 | 12·58 | 0·13 (0·12 to 0·15) | .. | |
| Tricyclic antidepressants | 1·23 | 1·22 | 1·20 | 1·22 | 1·20 | 1·22 | 1·20 | 1·19 | 1·19 | 1·17 | 1·15 | 1·12 | −0·02 (−0·02 to 0·02) | 0·058 | |
| Lower-middle income | 0·35 | 0·37 | 0·37 | 0·39 | 0·40 | 0·41 | 0·42 | 0·47 | 0·50 | 0·50 | 0·53 | 0·51 | 0·00 (−0·00 to 0·01) | .. | |
| Upper-middle income | 0·31 | 0·30 | 0·32 | 0·35 | 0·37 | 0·36 | 0·37 | 0·37 | 0·37 | 0·39 | 0·38 | 0·37 | −0·00 (−0·01 to 0·00) | .. | |
| High income | 4·35 | 4·30 | 4·25 | 4·24 | 4·07 | 4·20 | 4·10 | 3·96 | 3·93 | 3·82 | 3·71 | 3·66 | −0·03 (−0·04 to 0·03) | .. | |
| Monoamine oxidase inhibitors | 0·04 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·02 | 0·02 | −0·00 (−0·00 to 0·00) | 0·14 | |
| Lower-middle income | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 (0·00 to 0·01) | .. | |
| Upper-middle income | 0·01 | 0·01 | 0·01 | 0·01 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | 0·00 | −0·00 (−0·00 to 0·00) | .. | |
| High income | 0·16 | 0·14 | 0·14 | 0·13 | 0·13 | 0·13 | 0·12 | 0·12 | 0·11 | 0·11 | 0·11 | 0·10 | −0·00 (−0·01 to 0·00) | .. | |
| Antidepressants not otherwise specified | 1·35 | 1·44 | 1·52 | 1·62 | 1·63 | 1·76 | 1·82 | 1·94 | 2·04 | 2·17 | 2·31 | 2·47 | 0·10 (0·9 to 0·11) | 0·0004 | |
| Lower-middle income | 0·06 | 0·07 | 0·08 | 0·09 | 0·10 | 0·12 | 0·13 | 0·14 | 0·14 | 0·14 | 0·16 | 0·16 | 0·03 (0·01 to 0·05) | .. | |
| Upper-middle income | 0·14 | 0·15 | 0·18 | 0·21 | 0·26 | 0·28 | 0·31 | 0·33 | 0·37 | 0·41 | 0·48 | 0·56 | 0·03 (0·02 to 0·03) | .. | |
| High income | 5·67 | 6·03 | 6·44 | 6·75 | 6·72 | 7·25 | 7·50 | 8·01 | 8·44 | 8·98 | 9·52 | 10·12 | 0·16 (0·14 to 0·18) | .. | |
| Mood stabilisers | 0·06 | 0·06 | 0·06 | 0·06 | 0·06 | 0·07 | 0·06 | 0·07 | 0·07 | 0·07 | 0·07 | 0·07 | −0·001 (−0·001 to 0·00) | 0·98 | |
| Lower-middle income | 0·01 | 0·01 | 0·01 | 0·01 | 0·02 | 0·02 | 0·02 | 0·02 | 0·02 | 0·02 | 0·02 | 0·02 | 0·0001 (−0·00 to 0·0003) | .. | |
| Upper-middle income | 0·02 | 0·02 | 0·02 | 0·02 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·03 | 0·04 | −0·000 (−0·001 to 0·000) | .. | |
| High income | 0·22 | 0·22 | 0·22 | 0·23 | 0·22 | 0·23 | 0·22 | 0·22 | 0·22 | 0·22 | 0·21 | 0·21 | −0·001 (−0·001 to 0·001) | .. | |
| Tranquilisers | 7·13 | 7·27 | 7·14 | 7·36 | 7·09 | 7·22 | 7·07 | 7·01 | 6·90 | 6·72 | 6·56 | 6·40 | −0·09 (−0·13 to 0·05) | 0·16 | |
| Lower-middle income | 2·45 | 2·48 | 2·45 | 2·59 | 2·34 | 2·38 | 2·21 | 2·16 | 2·19 | 2·14 | 2·21 | 2·10 | −0·02 (−0·05 to 0·01) | .. | |
| Upper-middle income | 1·90 | 1·96 | 1·99 | 2·38 | 2·49 | 2·50 | 2·52 | 2·62 | 2·63 | 2·70 | 2·77 | 2·84 | 0·14 (0·04 to 0·24) | .. | |
| High income | 24·40 | 24·89 | 24·68 | 24·62 | 23·62 | 24·24 | 23·84 | 23·43 | 22·95 | 22·16 | 21·21 | 20·63 | −0·22 (−0·26 to 0·18) | .. | |
| Sedatives or hypnotics | 5·33 | 5·49 | 5·46 | 5·59 | 5·53 | 5·53 | 5·36 | 5·26 | 5·19 | 5·21 | 5·07 | 4·84 | −0·09 (−0·12 to 0·06) | <0·0001 | |
| Lower-middle income | 0·50 | 0·55 | 0·57 | 0·63 | 0·64 | 0·65 | 0·63 | 0·60 | 0·62 | 0·58 | 0·57 | 0·56 | 0·004 (−0·01 to 0·02) | .. | |
| Upper-middle income | 0·69 | 0·75 | 0·78 | 0·85 | 0·95 | 1·00 | 1·02 | 1·09 | 1·12 | 1·21 | 1·31 | 1·47 | 0·04 (0·02 to 0·06) | .. | |
| High income | 21·65 | 22·24 | 22·36 | 22·67 | 22·25 | 22·21 | 21·49 | 21·00 | 20·64 | 20·72 | 19·96 | 18·66 | −0·17 (−0·22 to 0·11) | .. | |
| All antipsychotics | 2·82 | 2·92 | 3·01 | 3·14 | 3·20 | 3·31 | 3·39 | 3·46 | 3·51 | 3·56 | 3·66 | 3·70 | 0·22 (0·20 to 0·24) | 0·0002 | |
| Lower-middle income | 0·62 | 0·68 | 0·75 | 0·81 | 0·87 | 0·91 | 0·95 | 0·95 | 1·03 | 1·06 | 1·12 | 1·15 | 0·19 (0·13 to 0·25) | .. | |
| Upper-middle income | 0·75 | 0·82 | 0·96 | 1·14 | 1·37 | 1·49 | 1·66 | 1·72 | 1·76 | 1·86 | 1·99 | 2·08 | 0·20 (0·16 to 0·23) | .. | |
| High income | 10·17 | 10·44 | 10·60 | 10·69 | 10·45 | 10·67 | 10·71 | 10·87 | 10·92 | 10·98 | 11·10 | 11·17 | 0·24 (0·21 to 0·27) | .. | |
| Typical antipsychotics | 0·90 | 0·88 | 0·89 | 0·91 | 0·89 | 0·88 | 0·89 | 0·84 | 0·80 | 0·78 | 0·76 | 0·71 | −0·02 (−0·03 to 0·01) | 0·15 | |
| Lower-middle income | 0·22 | 0·23 | 0·25 | 0·23 | 0·24 | 0·23 | 0·22 | 0·19 | 0·18 | 0·18 | 0·19 | 0·18 | 0·02 (−0·02 to 0·07) | .. | |
| Upper-middle income | 0·34 | 0·33 | 0·40 | 0·48 | 0·52 | 0·52 | 0·58 | 0·55 | 0·54 | 0·53 | 0·54 | 0·53 | 0·05 (0·03 to 0·07) | .. | |
| High income | 3·01 | 2·94 | 2·89 | 2·82 | 2·65 | 2·61 | 2·55 | 2·44 | 2·32 | 2·25 | 2·15 | 1·94 | −0·06 (−0·07 to 0·04) | .. | |
| Atypical antipsychotics | 1·89 | 2·01 | 2·08 | 2·19 | 2·27 | 2·40 | 2·47 | 2·59 | 2·67 | 2·74 | 2·87 | 2·96 | 0·24 (0·22 to 0·25) | 0·0001 | |
| Lower-middle income | 0·39 | 0·43 | 0·49 | 0·56 | 0·62 | 0·66 | 0·71 | 0·74 | 0·83 | 0·86 | 0·92 | 0·95 | 0·16 (0·13 to 0·20) | .. | |
| Upper-middle income | 0·40 | 0·47 | 0·55 | 0·64 | 0·84 | 0·96 | 1·06 | 1·15 | 1·21 | 1·31 | 1·44 | 1·53 | 0·15 (0·13 to 0·17) | .. | |
| High income | 7·05 | 7·38 | 7·60 | 7·77 | 7·69 | 7·96 | 8·07 | 8·34 | 8·51 | 8·65 | 8·87 | 9·15 | 0·30 (0·28 to 0·32) | .. | |
DDD=defined daily dose.
Table 2.
Annual DDD per 1000 inhabitants per day and percentage change in psychotropic medication use by drug class
|
Antidepressants |
Antipsychotics |
Tranquilisers |
Sedatives or hypnotics |
|||||
|---|---|---|---|---|---|---|---|---|
| DDD per 1000 inhabitants per day | Percentage change | DDD per 1000 inhabitants per day | Percentage change | DDD per 1000 inhabitants per day | Percentage change | DDD per 1000 inhabitants per day | Percentage change | |
| 2008 | 13·20 | .. | 2·82 | .. | 7·13 | .. | 5·33 | .. |
| 2009 | 13·87 | 5·08% | 2·92 | 3·55% | 7·27 | 1·96% | 5·49 | 3·00% |
| 2010 | 14·38 | 3·68% | 3·01 | 3·08% | 7·14 | −1·79% | 5·46 | −0·55% |
| 2011 | 15·16 | 5·42% | 3·14 | 4·32% | 7·36 | 3·08% | 5·59 | 2·38% |
| 2012 | 14·98 | −1·19% | 3·2 | 1·91% | 7·09 | −3·67% | 5·53 | −1·07% |
| 2013 | 15·68 | 4·67% | 3·31 | 3·44% | 7·22 | 1·83% | 5·53 | 0·00% |
| 2014 | 16·12 | 2·81% | 3·39 | 2·42% | 7·07 | −2·08% | 5·36 | −3·07% |
| 2015 | 16·83 | 4·40% | 3·46 | 2·06% | 7·01 | −0·85% | 5·26 | −1·87% |
| 2016 | 17·39 | 3·33% | 3·51 | 1·45% | 6·90 | −1·57% | 5·19 | −1·33% |
| 2017 | 17·99 | 3·45% | 3·56 | 1·42% | 6·72 | −2·61% | 5·21 | 0·39% |
| 2018 | 18·77 | 4·34% | 3·66 | 2·81% | 6·56 | −2·38% | 5·07 | −2·69% |
| 2019 | 19·76 | 5·27% | 3·70 | 1·09% | 6·40 | −2·44% | 4·84 | −4·54% |
DDD=defined daily dose.
In 2019, the total consumption of psychotropic medicines was 123·61 DDD per 1000 inhabitants per day in high-income countries, 13·52 DDD per 1000 inhabitants per day in upper-middle-income countries and 6·77 DDD per 1000 inhabitants per day in lower-middle-income countries (table 1). The greatest absolute increase in sales from 2008 to 2019 was reported in high-income countries (3·31 DDD per 1000 inhabitants per day, 95% CI 3·01–3·61). The average annual change in sales was statistically different between high-income countries compared with upper-middle-income countries (1·94 DDD per 1000 inhabitants per day, 1·45–2·44) and lower-middle-income countries (0·88 DDD per 1000 inhabitants per day, 0·62–1·13; p<0·0001; table 1). By contrast, the relative average annual increase in psychotropic medicine sales from 2008 to 2019 was greater in upper-middle-income countries (7·88%, 95% CI 6·99–8·77) than in lower-middle-income countries (2·90%, 2·40–3·39) and high-income countries (1·02%, 0·80–1·24; appendix p 7). The average percentage change per year, measured as standard units per person per year, was greatest in lower-middle-income countries (1·99%, 95% CI 1·67–2·30; appendix p 7). In lower-middle-income countries, there was an increase in sales of all psychotropic medicine classes, except for tranquilisers (table 1). The sales of tricyclic antidepressants, typical antipsychotics, tranquilisers, and sedatives or hypnotics decreased in high-income countries. Trends in antidepressant consumption in upper-middle-income countries largely followed those of high-income countries, with steeper growth in high-income countries for SSRIs, SNRIs, and antidepressants not otherwise defined. In contrast to high-income countries and lower-middle-income countries, the sales of tranquilisers (0·14 DDD per 1000 inhabitants per day, 95% CI 0·04–0·24) and sedatives or hypnotics (0·04 DDD per 1000 inhabitants per day, 0·02–0·06) increased in upper-middle-income countries.
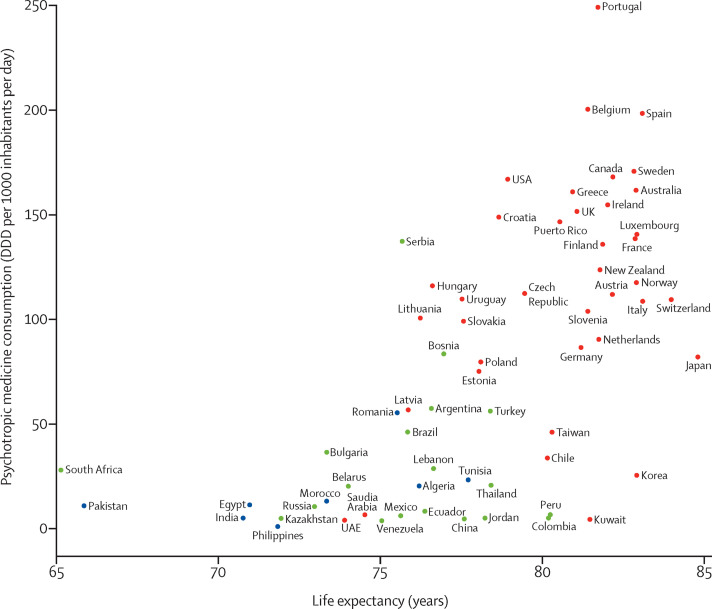
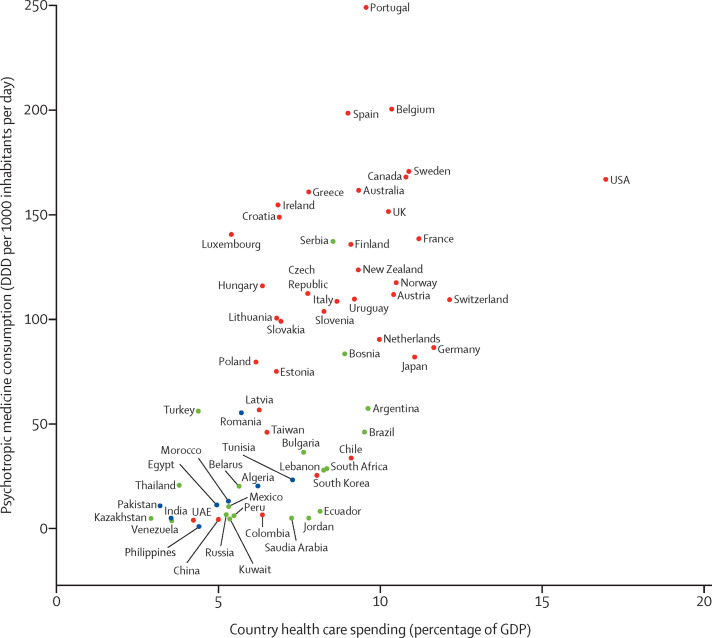
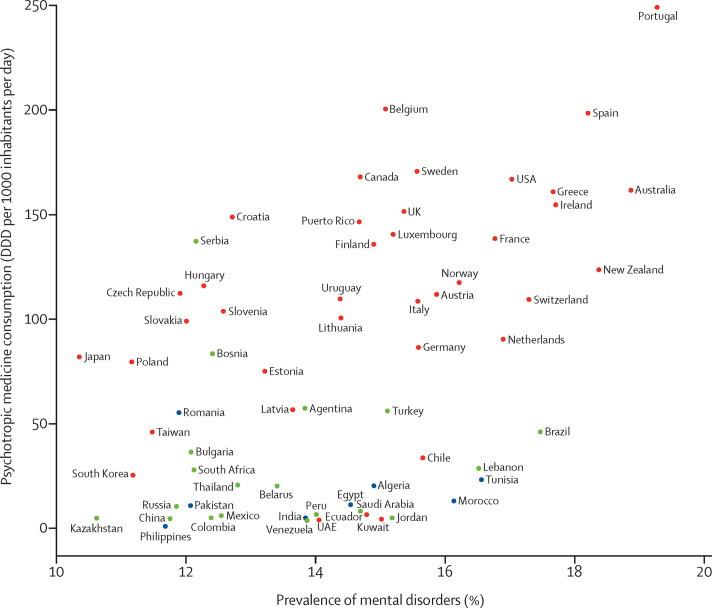
Although we found positive associations between changes in the psychotropic consumption of a country and the average life expectancy of the people of a country (p<0·0001, figure 1 ) and health expenditures (p=0·050, figure 2 ), these associations were largely driven by upper-middle-income countries. For high-income countries and lower-middle-income countries only, there was no evidence of a statistical association between changes in psychotropic medicine consumption and prevalence of mental illness (p=0·083 and p=0·15, respectively; figure 3 ). Lower-middle-income countries such as Morocco and India had relatively low consumption of psychotropic medicines, but a high prevalence of mental disorders. The association between changes in consumption of psychotropic medication and life expectancy was strong for countries of all income levels (p<0·0001; appendix p 10). For lower-middle-income countries and upper-middle-income countries, there was an association between changes in psychotropic medicine consumption and health expenditures (percentage of the gross domestic product; p=0·041 and p=0·038, respectively; figure 2).
Figure 1.
Correlation between psychotropic medicine consumption and life expectancy in 65 countries in 2019 by income
High-income countries are labelled in red, upper-middle-income countries in green, and lower-middle-income countries in blue. DDD=defined daily dose. UAE=United Arab Emirates.
Figure 2.
Correlation between psychotropic medicine consumption and health-care spending in 64 countries and regions in 2018 by income
High-income countries are labelled in red, upper-middle-income countries in green, and lower-middle-income countries in blue. Data on health-care spending in Puerto Rico were not available. DDD=defined daily dose. GDP=gross domestic product. UAE=United Arab Emirates.
Figure 3.
Correlation between psychotropic medicine consumption and prevalence of mental disorders in 65 countries and regions in 2019 by income
High-income countries are labelled in red, upper-middle-income countries in green, and lower-middle-income countries in blue. DDD=defined daily dose. UAE=United Arab Emirates.
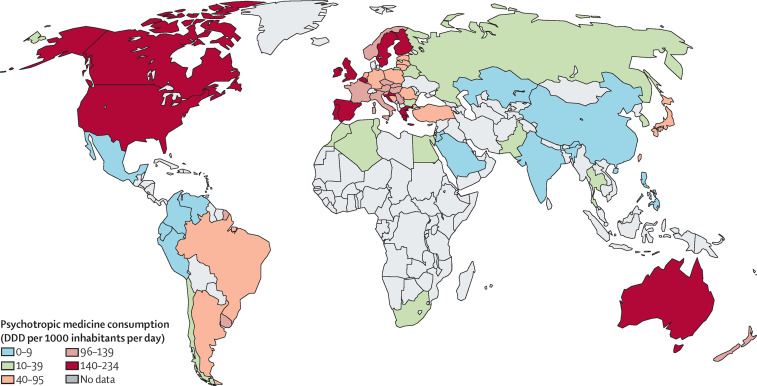
After adjusting for income level, overall psychotropic sales were highest in northern America (167·54 DDD per 1000 inhabitants per day), but higher levels of consumption were found in some individual European countries (appendix pp 8–9). The lowest levels of consumption were found in Asia (5·59 DDD per 1000 inhabitants per day). In 2019, the country with the highest psychotropic sales volume was Portugal (249·08 DDD per 1000 inha-bitants per day), followed by Belgium (200·46 DDD per 1000 inhabitants per day), Spain (198·48 DDD per 1000 inhabitants per day), Sweden (170·77 DDD per 1000 inhabitants per day), Canada (168·10 DDD per 1000 inhabitants per day), and the USA (166·99 DDD per 1000 inhabitants per day; figure 4 ). Despite the overall global increase in psychotropic consumption, countries such as Finland, France, Luxembourg, and Norway, with high volume of psychotropic sales in 2008, reduced their psychotropic consumption over the study period (appendix pp 8–9). Switzerland and Japan, both with mid-range consumption, as well as Jordan (low consumption), also reduced their consumption of psychotropic medicine. Countries with the lowest consumption in 2019 were the Philippines (0·93 DDD per 1000 inhabitants per day), Venezuela (3·69 DDD per 1000 inhabitants per day), United Arab Emirates (3·97 DDD per 1000 inhabitants per day), Kuwait (4·34 DDD per 1000 inhabitants per day), China (4·57 DDD per 1000 inhabitants per day), and Kazakhstan (4·84 DDD per 1000 inhabitants per day). Except for Venezuela, the same countries also had the lowest psychotropic medicine consumption in 2008.
Figure 4.
Consumption of psychotropic medicines in 65 countries and regions, 2019
DDD=defined daily dose.
For antidepressants and antipsychotic agents, regional trends were similar to those of psychotropic agents overall. Greece had the highest level of antipsychotic consumption among all the included countries and regions (26·02 DDD per 1000 inhabitants per day), and the consumption of sedatives or hypnotics was highest in Belgium (46·93 DDD per 1000 inhabitants per day; appendix pp 8–9). The sales of tranquilisers ranged from 2·22 DDD per 1000 inhabitants per day in Asia to 14·92 DDD per 1000 inhabitants per day in Europe. Within Europe, the consumption of tranquilisers was highest in Serbia (94·50 DDD per 1000 inhabitants per day), followed by Portugal (90·86 DDD per 1000 inhabitants per day). Most countries reported low sales of mood stabilisers (<0·05 DDD per 1000 inha-bitants per day). The highest consumption was recorded in Belgium (0·75 DDD per 1000 inhabitants per day), followed by the Netherlands (0·37 DDD per 1000 inhabitants per day) and Luxembourg (0·43 DDD per 1000 inha-bitants per day).
17 countries were in the 25th percentile of consumption as measured by DDD per 1000 inhabitants per day in 2019. Beside the previously mentioned six countries with the lowest DDD per 1000 inhabitants per day (the Philippines, Venezuela, United Arab Emirates, Kuwait, China, and Kazakhstan), Jordan, Colombia, India, Mexico, Saudi Arabia, Peru, Ecuador, Russia, Pakistan, Egypt, and Morocco had consumption ranging from 4·97 to 13·07 DDD per 1000 inhabitants per day (appendix pp 8–9).
Discussion
This study reported the consumption of psychotropic medicines in 65 countries and regions disaggregated by country income level and geographical region. It serves two important purposes: first, to identify countries and regions with relatively low consumption of psychotropic medicines, and, second, to serve as the baseline to monitor future change. We compared global trends of psychotropic medicine sales data and found that the consumption of psychotropic medicines has increased with a relative average annual increase of 4% over a 12-year period. The global increase in the use of psychotropic medicine has been linked to more awareness of mental health as a pivotal part of overall health,18 behavioural changes leading to a greater willingness to seek treatment,19 and drug treatment lasting longer.20 In addition, polypharmacy with psychotropic medicines is now more prevalent.21, 22 The growth of psychotropic medicine consumption is not uniform. Notably, high-income countries such as Finland, France, Luxembourg, and Norway, as well as Venezuela (a lower-middle-income country), have seen a decrease in the consumption of psychotropic medicine. Our study suggests that the increase in sales of psychotropic medicines in upper-middle-income countries can partly be explained by the country level burden of mental illness, life expectancy, and health expenditure.
Throughout the study period, the consumption of psychotropic medicines in lower-middle-income countries and upper-middle-income countries was lower than in high-income countries, but the average annual increase in sales of psychotropic medicine from 2008 to 2019 was 7·9% in upper-middle-income countries compared with 1·02% in high-income countries. According to the Global Burden of Diseases, Injuries, and Risk Factors Study 2019, prevalences of mental health disorders in upper-middle-income countries and lower-middle-income countries have remained stable at 13%.14 Although a high prevalence of mental health disorders, such as schizophrenia, is reported in southeast and east Asia,23 most Asian countries in our study had very low rates of antipsychotics consumption. The Philippines (0·93 DDD per 1000 inhabitants per day), China (4·57 DDD per 1000 inhabitants per day), and India (4·98 DDD per 1000 inhabitants per day) were among the countries with the lowest consumption of psychotropics in 2019. Our results support WHO findings that between 76% and 85% of people with severe mental disorders receive no treatment with medicines for their disorder in middle-income countries.4
In addition to country income level, we found geographical differences in the consumption of psychotropic medicines. In 2019, the total consumption of psychotropic medicines, controlled for income, in Asia (5·59 DDD per 1000 inhabitants per day) was about 3% of that of northern American countries (167·54 DDD per 1000 inhabitants per day). Within regions, not all drug classes have high consumption rates despite there being a high level of total psychotropic medicine consumption. For example, certain high-income countries appear to preferentially consume sedatives or hypnotics, or tranquilisers, and only a few countries have high consumption rates of both. In 2019, consumption rates of antidepressant and antipsychotic medicines in the USA and Canada were similar, but the consumption of tranquilisers was higher in the USA than in Canada, where the consumption of sedatives or hypnotics was lower. In some cases, countries that are similar in terms of geographical location—eg, the neighbouring countries of Finland, Norway, and Sweden—have different patterns of psychotropic consumption rates. These differences might be explained by variations in health-care policy.24, 25 Similar observations are made for the UK and France and different Asian regions such as Taiwan and China. Overall, regional differences in medicine consumption are probably due to multiple factors. Previous research has suggested variations in the role of health technology assessment, service organisation and delivery, and medicine reimbursement policies. Each of these factors probably plays a part in explaining international variation in medicines use, but their relative importance will vary depending on the disease area in question and the system context.26
Results for analyses by psychotropic medicine class show that the overall consumption of antidepressants is rising in all 65 countries and regions, with the relative rate of increase higher in lower-middle-income countries and upper-middle-income countries than in high-income countries. The increase in the consumption of antidepressants in this study is in line with a rising trend shown in a previous study on antidepressants consumption in 25 high-income countries.6 There is substantial overlap in the high-income countries included in both studies, and when we compared the results from 2008 to 2013, the results were, unsurprisingly, very similar, which supports the validity of our results. Our study shows that the increase in consumption of antidepressants in high-income countries continued after 2013. More importantly, our study shows that the relative increase in antidepressant sales is even more pronounced in lower-middle-income countries and upper-middle-income countries. Despite the rise in overall sales of antidepressants, a recent WHO study suggested that there is considerable evidence of undertreatment.27 In 2019, the global sales of SSRIs were twice as high as the consumption of all other antidepressants combined. A few studies from individual countries have reported trends of antidepressant use as well as other psychotropic medicine use that are similar to the findings of this study.28, 29 This trend aligns with the main clinical practice guidelines in children and adults, which recommend that people with moderate-to-severe depression receive medication treatment.30 SSRIs are recommended as a first-line antidepressant and have replaced benzodiazepines as first-line treatment of generalised anxiety disorders, panic attacks, and post-traumatic stress disorder owing to their favourable risk–benefit ratio.31 In all countries, SSRIs, SNRIs, and other antidepressants are being favoured over tricyclic antidepressants and monoamine oxidase inhibitors, but in lower-middle-income countries the consumption of older, and potentially more affordable, antidepressants is still growing. Tricyclic antidepressants are prescribed for indications other than depression or anxiety, particularly in chronic pain and sleep disorders.
Our study found a decreasing trend in the sales of typical antipsychotics, largely driven by high-income countries. The sales of both typical and atypical antipsychotic medicines are rising in upper-middle-income countries. The broad use of antipsychotics can be linked to expanded regulatory approval for indications outside psychosis and an increase in their off-label use, notably their more common use for mood disorders.32 A previous cross-sectional electronic health record study on the consumption of antipsychotics in Australia, New Zealand and 14 American, Asian, and European countries showed that the use of atypical antipsychotics from 2005 to 2014 was growing in all 16 countries.7 In our study, for the same 16 countries, this growth continued after 2014 until our last recorded data point in December, 2019.
Over the study period, there was a modest decrease in the average annual change in tranquiliser and sedative or hypnotic consumption in high-income countries, which might partly be explained by the increasing prescriber and patient awareness of the addictive nature, dependence, and withdrawal symptoms of drugs such as benzodiazepines and Z drugs.33, 34 To our knowledge, only two studies have compared the consumption of tranquilisers in multiple countries.11 Both studies found higher rates of consumption in France, Spain, and the USA compared with Germany and the UK. Individual European country studies on the use of anxiolytics confirm a north–south divide, with southern European countries reporting an increase in the use of anxiolytics from 2006 onwards,35 whereas northern European countries have reported a decrease, particularly in younger age groups (18–25 years).36, 37 Our study found high rates of consumption of tranquilisers in Serbia (94·50 DDD per 1000 inhabitants per day) and Croatia (80·26 DDD per 1000 inhabitants per day), which was similar to rates reported in a 2018 study on the impact of socioeconomic instability on benzodiazepine exposure in three Balkan countries.38 Although socioeconomic instability could explain the difference seen between three eastern European countries in that study,38 our results suggest that, on a global level, socioeconomic unrest can only partly explain the variation in the consumption of tranquilisers. For example, Algeria and Egypt, countries that have experienced considerable political and economic disruption in the past decade, have relatively low rates of consumption of tranquilisers (5·48 and 0·96 DDD per 1000 inhabitants per day, respectively).
One study described and compared the change in consumption of sedatives and hypnotics, based on pharmacy dispensing data, in France, Italy, Portugal, and Spain between 2003 and 2010.39 Although our study covered a different period, we also found a decrease in the consumption of sedatives in France and Italy, and an increase in Spain, from 2008 to 2019. For countries such as France and Italy, this decrease might be because of the social attitudes, governmental initiatives, and concerns about stimulant misuse.40 The decrease in overall psychotropic consumption in high-income countries, such as Finland, France, and Luxembourg, was largely driven by a steep decrease in sedative or hypnotic consumption. Further studies from individual countries confirm the decreasing trend in the consumption of sedatives.28, 41 Of note is the high level of sedative sales found in Belgium (46·93 DDD per 1000 inhabitants per day) and Japan (44·50 DDD per 1000 inhabitants per day) in 2019. According to the UN International Narcotics Control Board, Japan and Belgium ranked second and third, respectively, for sedative or hypnotic consumption worldwide in 2015.42 The high levels of sedative or hypnotic consumption in Japan and Belgium might be related to the high use of these medicines as a treatment for insomnia.43
Among the 17 countries with the lowest consumption in 2019, the Philippines and Morocco are the lowest (0·93 DDD per 1000 inhabitants per day) and highest (13·07 DDD per 1000 inhabitants per day). Such low DDD per 1000 inhabitants per day means that, on average, the consumption of psychotropic medicine is only sufficient for one patient per 1000 inhabitants per day in the Philippines and 13 patients per 1000 inhabitants per day in Morocco, assuming there is no polypharmacy. Clearly, this is well below our current understanding of the epidemiology of mental health disorders. Urgent improvement in the access to psychotropic medication for patients is needed. 14 of these countries are middle-income countries, in which financial factors might contribute to such low consumption. However, three countries, namely Kuwait, Saudi Arabia, and the United Arab Emirates, are high-income countries, and thus a country's economic status does not fully explain the low consumption. Previous studies reported that patients with mental disorders in Arab countries tend to express their psychological problems in terms of physical symptoms, thereby avoiding the stigma attached to mental illness.44 Furthermore, reliance upon a deity and religious leaders as a means of coping with mental health issues is another prevalent theme in the Arab world.44 All these factors might partly explain the low consumption in these countries.
China has one of the lowest consumptions of psychotropic medications (one of the bottom five) in contrast to Taiwan, which has a consumption around ten times that of China (4·57 DDD per 1000 inhabitants per day for China vs 46·04 DDD per 1000 inhabitants per day for Taiwan). Previous studies also suggested that the Taiwanese population had higher endorsement of psychotropic medications than other Chinese communities, especially for antidepressants and tranquillisers.45 Moreover, studies suggest the Taiwanese population also has a better recognition of depression than other Chinese communities.45 Despite the similar Chinese ethnicity, religion, and cultural traditions between China and Taiwan, this finding suggests that other social factors might still have an important role in affecting psychotropic medication consumption.
The use of international pharmaceutical sales data enables a unique global comparison of trends in psychotropic medicine consumption despite differences in health-care systems. However, there were some limitations to this study. Our data only reflect the country-level supply side of psychotropic medication. Factors such as costs, access, and quality assurance have a large effect on the demand side. Pharmaceutical sales data do not reflect individual-level treatment for mental health problems. For this reason, we could not measure trends by age, gender, and indications or appropriateness of prescribing. Individual-level data are needed to inform us about potential overuse, underuse, misuse, unnecessarily expensive use, and access to psychotropic medicine.46 Particularly, in some of the lower-middle-income countries included in our study, current regulatory capacity and enforcement might not be sufficient to ensure affordable access to quality medication for people living in those countries.47 International studies of medicine use usually present data in DDDs to allow comparisons between population groups. However, DDD is not a measure of therapeutic use; hence, our study cannot address quality of prescribing. We did not measure societal differences and attitudes towards mental health. Studies have suggested that higher country spending on health care and positive cultural attitudes towards mental illness are associated with regular use of psychotropic medicines.19 Psychosocial interventions are effective in treating some mental disorders with or without concurrent pharmacological treatment, such as depression or anxiety.48, 49 However, for other conditions, such as schizophrenia and bipolar disorder, psychosocial interventions are commonly considered adjuctive to medication. We were unable to investigate the availability of these other interventions; however, there is evidence to suggest that the access to psychosocial interventions in many lower-middle-income countries is lower than psychotropic medication access.50 Last, as our study included data from 65 countries and regions, the findings are only applicable to these countries and regions. To provide a full picture, data from all other countries are urgently needed to further our understanding of how to improve our global mental health.
Each cultural and geopolitical region presents its own set of factors that affect treatment referral and prescribing behaviours. We identified 17 countries with very low consumption of psychotropic medicines. Countries with low consumption rates for psychotropic medicines are unlikely to provide sufficient access to psychotropic drugs, and the reasons for this should be identified.4 Poor access to health care in general, and affordability could prevent many individuals who might benefit from psychotropic medication from receiving treatment, especially in countries where the use of psychotropic medicines is further restricted because of the lack of qualified health workers with the appropriate authority to prescribe medications.46, 51 These governments should focus on training health-care workers who can prescribe cost-effective psychotropic medicines in the WHO model list of essential medicines.52 However, countries such as Kuwait, Saudi Arabia, and the United Arab Emirates, which are high-income countries, have low consumption rates of psychotropic medicine; hence, the barriers to access were not fully due to economic reasons. There is some evidence that stigma and cultural considerations contribute to low consumption of psychotropics.19 Therefore, it is important for governments to address this issue with public education and consider involving community and religious leaders to promote appropriate understanding of psychotropic medicine use. Our study findings can be used as the baseline to evaluate future interventions to improve access.
The consumption of psychotropic medicines has increased over a 12-year period, and, although the absolute growth rate is highest in high-income countries, the relative growth is highest in lower-middle-income countries and upper-middle-income countries. Disparities in psychotropic medicine consumption of countries can only partly be explained by geographical location and income level. Efforts need to be made to improve the availability of psychotropic medicines in countries with a low consumption of psychotropic medicines, but high prevalence of mental disorders.
Data sharing
The underlying MIDAS data were provided by IQVIA under licence. The terms of our agreement do not permit disclosure, sublicensing, or sharing of IQVIA MIDAS data. IQVIA will honour legitimate requests for MIDAS data from qualified researchers. Please contact IQVIA to seek approval for data access; a licence fee might be applied.
Declaration of interests
JEB is supported by the Hong Kong Research Grants Council as a recipient of the Hong Kong PhD Fellowship Scheme. JFH is supported by the Wellcome Trust (211085/Z/18/Z), the University College London Hospitals National Institute for Health Research (NIHR) Biomedical Research Centre (London, UK), and the NIHR North Thames Applied Research Collaboration. KKCM is the recipient of the CW Maplethorpe Fellowship, reports grants from the NIHR and the Hong Kong Research Grant Council, and reports personal fees from IQVIA, unrelated to the submitted work. EWC has received an honorarium from the Hong Kong Hospital Authority, and research grants from the Hong Kong Research Grants Council, the Hong Kong Research Fund Secretariat of the Food and Health Bureau, the National Natural Science Fund of China, the Australian National Health and Medical Research Council, the Wellcome Trust, Bayer, Bristol Myers Squibb, Pfizer, Janssen, Amgen, Takeda, and the Hong Kong Narcotics Division of the Security Bureau, outside the submitted work. CSLC has received grants from the Food and Health Bureau of the Hong Kong Government, the Hong Kong Research Grant Council, the Hong Kong Innovation and Technology Commission, Pfizer, IQVIA, and Amgen, and personal fees from Primevigilance, outside the submitted work. ICKW reports research funding outside the submitted work from Amgen, Bristol Myers Squibb, Pfizer, Janssen, Bayer, GSK, Novartis, the Hong Kong Research Grants Council, the Hong Kong Health and Medical Research Fund, the NIHR, the European Commission, and the Australian National Health and Medical Research Council, and has also received expert testimony payment from the Hong Kong Court of Final Appeal and speaker's fees from Janssen and Medice in the previous 3 years. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
We thank IQVIA for their assistance and information regarding the use of IQVIA-MIDAS data.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contributors
RB, JEB, EWC, VKCY, and ICKW conceptualised and designed the study. BA, RB, EWC, LW, and ICKW acquired data. RB, LW, KKCM, and WCYL did the statistical analysis. All authors contributed to data interpretation. ZW and MYB contributed to literature review. RB and LW drafted the manuscript. RB and CSLC made the figures. All authors were involved in critical revision of the manuscript for important intellectual content. ICKW and LW accessed and verified the underlying data.
Supplementary Material
References
- 1.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391:1357–1366. doi: 10.1016/S0140-6736(17)32802-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Mental health action plan 2013–2020. 2013. http://apps.who.int/iris/bitstream/10665/89966/1/9789241506021_eng.pdf
- 5.WHO Mental health action plan 2013–2020 (extended to 2030) 2019. http://www.emro.who.int/mnh/mental-health-action-plan/index.html
- 6.Chalabi M. Antidepressants: global trends. 2013. https://www.theguardian.com/news/2013/nov/20/mental-health-antidepressants-global-trends
- 7.Hálfdánarson Ó, Zoëga H, Aagaard L, et al. International trends in antipsychotic use: a study in 16 countries, 2005–2014. Eur Neuropsychopharmacol. 2017;27:1064–1076. doi: 10.1016/j.euroneuro.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Raman SR, Man KKC, Bahmanyar S, et al. Trends in attention-deficit hyperactivity disorder medication use: a retrospective observational study using population-based databases. Lancet Psychiatry. 2018;5:824–835. doi: 10.1016/S2215-0366(18)30293-1. [DOI] [PubMed] [Google Scholar]
- 9.Cook MN. Estimating national drug consumption using data at different points in the pharmaceutical supply chain. Pharmacoepidemiol Drug Saf. 2006;15:754–757. doi: 10.1002/pds.1309. [DOI] [PubMed] [Google Scholar]
- 10.Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14:742–750. doi: 10.1016/S1473-3099(14)70780-7. [DOI] [PubMed] [Google Scholar]
- 11.Khong TP, de Vries F, Goldenberg JS, et al. Potential impact of benzodiazepine use on the rate of hip fractures in five large European countries and the United States. Calcif Tissue Int. 2012;91:24–31. doi: 10.1007/s00223-012-9603-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsia Y, Sharland M, Jackson C, Wong ICK, Magrini N, Bielicki JA. Consumption of oral antibiotic formulations for young children according to the WHO Access, Watch, Reserve (AWaRe) antibiotic groups: an analysis of sales data from 70 middle-income and high-income countries. Lancet Infect Dis. 2019;19:67–75. doi: 10.1016/S1473-3099(18)30547-4. [DOI] [PubMed] [Google Scholar]
- 13.WHO ATC/DDD index. Nervous system. 2019. https://www.whocc.no/atc_ddd_index/?code=N06A
- 14.Global Burden of Disease Collaborative Network Global Burden of Disease Study 2017 (GBD 2017) results. 2018. http://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Booklet.pdf
- 15.WHO Global health expenditure database. 2020. https://apps.who.int/nha/database
- 16.UN World population prospects 2019. 2019. https://population.un.org/wpp/
- 17.WHO Collaborating Centre for Drug Statistics Methodology ATC/DDD Index 2021. 2021. https://www.whocc.no/atc_ddd_index/
- 18.Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 19.Lewer D, O'Reilly C, Mojtabai R, Evans-Lacko S. Antidepressant use in 27 European countries: associations with sociodemographic, cultural and economic factors. Br J Psychiatry. 2015;207:221–226. doi: 10.1192/bjp.bp.114.156786. [DOI] [PubMed] [Google Scholar]
- 20.WHO Duration of antidepressant treatment. 2012. https://www.who.int/mental_health/mhgap/evidence/resource/depression_q2.pdf?ua=1
- 21.Brett J, Daniels B, Karanges EA, et al. Psychotropic polypharmacy in Australia, 2006 to 2015: a descriptive cohort study. Br J Clin Pharmacol. 2017;83:2581–2588. doi: 10.1111/bcp.13369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loggia G, Attoh-Mensah E, Pothier K, et al. Psychotropic polypharmacy in adults 55 years or older: a risk for impaired global cognition, executive function, and mobility. Front Pharmacol. 2020;10 doi: 10.3389/fphar.2019.01659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naveed S, Waqas A, Chaudhary AMD, et al. Prevalence of common mental disorders in South Asia: a systematic review and meta-regression analysis. Front Psychiatry. 2020;11:899. doi: 10.3389/fpsyt.2020.573150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vallgårda S. Addressing individual behaviours and living conditions: four Nordic public health policies. Scand J Public Health. 2011;39(suppl):6–10. doi: 10.1177/1403494810378922. [DOI] [PubMed] [Google Scholar]
- 25.Vilhelmsson A. Depression and antidepressants: a Nordic perspective. Front Public Health. 2013;1:30. doi: 10.3389/fpubh.2013.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nolte E, Corbett J. International variation in drug usage: an exploratory analysis of the “causes” of variation. Rand Health Q. 2015;4:1. [PMC free article] [PubMed] [Google Scholar]
- 27.Thornicroft G, Chatterji S, Evans-Lacko S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. 2017;210:119–124. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stephenson CP, Karanges E, McGregor IS. Trends in the utilisation of psychotropic medications in Australia from 2000 to 2011. Aust N Z J Psychiatry. 2013;47:74–87. doi: 10.1177/0004867412466595. [DOI] [PubMed] [Google Scholar]
- 29.Wu CS, Shau WY, Chan HY, Lee YC, Lai YJ, Lai MS. Utilization of antidepressants in Taiwan: a nationwide population-based survey from 2000 to 2009. Pharmacoepidemiol Drug Saf. 2012;21:980–988. doi: 10.1002/pds.3255. [DOI] [PubMed] [Google Scholar]
- 30.American Psychological Association APA clinical practice guideline for the treatment of depression across three age cohorts. Feb. 16, 2019. https://www.apa.org/depression-guideline/guideline.pdf
- 31.National Institute for Health and Care Excellence Depression in adults: treatment and management. NICE guideline: short version (update NICE guideline CG90) May, 2018. https://www.nice.org.uk/guidance/GID-CGWAVE0725/documents/short-version-of-draft-guideline
- 32.Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS. Increasing off-label use of antipsychotic medications in the United States, 1995–2008. Pharmacoepidemiol Drug Saf. 2011;20:177–184. doi: 10.1002/pds.2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ilyas S, Moncrieff J. Trends in prescriptions and costs of drugs for mental disorders in England, 1998-2010. Br J Psychiatry. 2012;200:393–398. doi: 10.1192/bjp.bp.111.104257. [DOI] [PubMed] [Google Scholar]
- 34.Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. 2009;23:19–34. doi: 10.2165/0023210-200923010-00002. [DOI] [PubMed] [Google Scholar]
- 35.Carrasco-Garrido P, Hernández-Barrera V, Jiménez-Trujillo I, et al. Time trend in psychotropic medication use in Spain: a nationwide population-based study. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13121177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurko T, Saastamoinen LK, Tuulio-Henriksson A, et al. Trends in the long-term use of benzodiazepine anxiolytics and hypnotics: a national register study for 2006 to 2014. Pharmacoepidemiol Drug Saf. 2018;27:674–682. doi: 10.1002/pds.4551. [DOI] [PubMed] [Google Scholar]
- 37.Tähkäpää SM, Saastamoinen L, Airaksinen M, Tuulio-Henriksson A, Aalto-Setälä T, Kurko T. Decreasing trend in the use and long-term use of benzodiazepines among young adults. J Child Adolesc Psychopharmacol. 2018;28:279–284. doi: 10.1089/cap.2017.0140. [DOI] [PubMed] [Google Scholar]
- 38.Marković SZ, Dimitrijević Jovanović NI, Sedić B, et al. Impact of differences in economic development and socioeconomic stability on benzodiazepine exposure between the three Balkans countries. Psychiatr Danub. 2019;31(suppl 5):750–760. [PubMed] [Google Scholar]
- 39.Vicente Sánchez MP, Macías Saint-Gerons D, de la Fuente Honrubia C, González Bermejo D, Montero Corominas D, Catalá-López F. [Trends of use of anxiolytics and hypnotics in Spain from 2000 to 2011] Rev Esp Salud Pública. 2013;87:247–255. doi: 10.4321/S1135-57272013000300004. [DOI] [PubMed] [Google Scholar]
- 40.Zito JM, Safer DJ, de Jong-van den Berg LT, et al. A three-country comparison of psychotropic medication prevalence in youth. Child Adolesc Psychiatry Ment Health. 2008;2:26. doi: 10.1186/1753-2000-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barczyk ZA, Rucklidge JJ, Eggleston M, Mulder RT. Psychotropic medication prescription rates and trends for New Zealand children and adolescents 2008–2016. J Child Adolesc Psychopharmacol. 2020;30:87–96. doi: 10.1089/cap.2019.0032. [DOI] [PubMed] [Google Scholar]
- 42.International Narcotics Control Board Psychotropic substances. 2016. https://www.incb.org/documents/Psychotropics/technical-publications/2016/Technical_Publication_2016.pdf
- 43.Doi Y, Minowa M, Okawa M, Uchiyama M. Prevalence of sleep disturbance and hypnotic medication use in relation to sociodemographic factors in the general Japanese adult population. J Epidemiol. 2000;10:79–86. doi: 10.2188/jea.10.79. [DOI] [PubMed] [Google Scholar]
- 44.Al-Krenawi A. Mental health practice in Arab countries. Curr Opin Psychiatry. 2005;18:560–564. doi: 10.1097/01.yco.0000179498.46182.8b. [DOI] [PubMed] [Google Scholar]
- 45.Wong DFK, Cheng C-W, Zhuang XY, et al. Comparing the mental health literacy of Chinese people in Australia, China, Hong Kong and Taiwan: implications for mental health promotion. Psychiatry Res. 2017;256:258–266. doi: 10.1016/j.psychres.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 46.Wirtz VJ, Hogerzeil HV, Gray AL, et al. Essential medicines for universal health coverage. Lancet. 2017;389:403–476. doi: 10.1016/S0140-6736(16)31599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.WHO Improving access to and appropriate use of medicines for mental disorders. 2017. https://apps.who.int/iris/bitstream/handle/10665/254794/9789241511421-eng.pdf
- 48.National institute for Health and Care Excellence Depression in adults: recognition and management. 2009. https://www.nice.org.uk/guidance/cg90/chapter/Context [PubMed]
- 49.National institute for Health and Care Excellence Anxiety disorders, quality statement 2: psychological interventions. 2014. https://www.nice.org.uk/guidance/qs53/chapter/quality-statement-2-psychological-interventions
- 50.Rathod S, Pinninti N, Irfan M, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights. 2017;10 doi: 10.1177/1178632917694350. 1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103:777–780. doi: 10.2105/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO WHO model lists of essential medicines. 2019. https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The underlying MIDAS data were provided by IQVIA under licence. The terms of our agreement do not permit disclosure, sublicensing, or sharing of IQVIA MIDAS data. IQVIA will honour legitimate requests for MIDAS data from qualified researchers. Please contact IQVIA to seek approval for data access; a licence fee might be applied.