Abstract
Background:
In physiotherapists, biomechanical overload risk assessment (RA) is particularly complex due to the tasks’ variability. The present study aims to propose a new methodology, named Whole Body RA Musculoskeletal Biomechanical Overload (WB-RAMBO), to assess the risk in the activities performed by physiotherapists.
Methods:
Each type of intervention was broken down into elementary operations. The risk factors (force, repetitiveness, and incongruous postures) were recorded and evaluated for each of these. For each task, the risk level was obtained by integrating the results of multiple ergonomic methods among those proposed by the international literature. To verify and validate the obtained results, we reviewed the medical records of health surveillance carried out on physiotherapists.
Results:
From the ergonomic point of view, RA shows a situation of acceptability. The observed slight dysergonomies are diluted in the work shift and allow an optimal functional recovery of the musculoskeletal system.
Conclusions:
This method proposes a RA for each operation performed. A work plan subjected to such a peculiar RA can be redesigned and adapted to the company’s and the hypersusceptible worker’s organizational needs.
Keywords: Functional rehabilitation technicians, work-related musculoskeletal disorders, dysergonomies, health surveillance
1. Introduction
Numerous literature studies show that functional rehabilitation technicians [1-6], more commonly known as physiotherapists, are potentially exposed to the risk of biomechanical overload to the musculoskeletal system. RA from biomechanical overload to which these operators are exposed is particularly complex due to the extreme variability of the tasks. The related overload depends not only on organizational and structural aspects but also mainly on the level of impairment and the residual functional ability of the patient, so it is difficult to propose a standardized methodology for RA.
Many methods proposed in the international literature (e.g., REBA [7], HAL ACGIH [8], OCRA [9], STRAIN INDEX [10]) assess single risk factors or body segments. MAPO (Assisted Handling of Hospitalized Patients) is another method extensively used in health care (HC) facilities [11, 12], but its primary outcome is not focused on RA but on risk management by organizational and structural preventive measures. The HOARA (Holistic Approach RA method) [13] can allow the RA for head/neck, spine, and upper and lower limbs resulting from activities performed by health care workers (HCWs) in the work shift. HOARA is a new tool developed for both RA and risk management.
Our study was carried out with the primary objective of developing an innovative methodology, named Whole Body RA Muskuloskeletal Biomechanical Overload (WB-RAMBO), to assess the risk of biomechanical overload to the musculoskeletal system in the activities performed in outpatient clinics and inpatient wards by physiotherapists employed in a large university hospital.
2. Methods
The study was carried out at the Spedali Civili Hospital of Brescia, Brescia, Italy, with the support of the Coordinator of the Physiotherapy Unit, who provided accurate information about the type, frequency, and duration of the different rehabilitation interventions (tasks) carried out by physiotherapists both in the inpatient wards and the outpatient clinic (Table 1).
Table 1.
Operations for rehabilitation purposes performed in inpatient wards. A: Orthopaedic patient (simple or multiple trauma); B: Multi-pathologic/Complex patients; C: Neurological/Neurosurgical patients; D: Critical Care Area patients; E: Outpatient clinic.
| Operations | A | B | C | D | E |
|---|---|---|---|---|---|
| Patient identification, consultation, and review of medical records (in particular to rule out relative or absolute contraindications to treatment) by ward staff | x | x | x | x | x |
| Assessment of the patient’s condition and vital signs | x | x | |||
| Evaluation and adjustment of the rehabilitation setting in which to carry out the treatment (evaluating and adjusting the presence of a catheter, nasogastric tube, or other devices and monitoring systems) | x | x | x | x | x |
| Positioning the patient in a correct posture | x | x | x | x | x |
| Passive or active-assisted mobilization at the bedside of the affected body district (usually mobilization of at least three joint districts bilaterally) | x | x | x | - | x |
| Passive or active-assisted bedside mobilization of upper and lower limbs and, if possible, of the neck and head (approximately 10 to 20 repetitions for all joint areas) | x | x | |||
| Sensory-motor stimulation and reactivation of the affected body districts | x | x | x | ||
| Active mobilization and muscle strengthening of the affected area (usually reactivation of at least three joint areas bilaterally) | x | x / with breathing exercises | x | x | |
| Reaching and maintaining a sitting position (with the possible simultaneous addition of exercises to realign the trunk muscles) | x | x | x | x | |
| Reaching and maintaining a sitting position (with exercises for reaching and maintaining the midline, axial loading, and reactivation of the trunk) | x | x / at least two physiotrp | x | ||
| Achieving and maintaining a standing position | x | x / help of 1-2 physiotrp | x / help of 1-2 physiotrp | x | |
| Walking with help or supervision of a physiotherapist (with or without aid) | x | x | x | x | |
| Wheelchair with correct postural alignment in bed or chair and orthotic positioning | x | x | x | x | x |
For the interventions carried out on the wards, since these are difficult to standardize, as they are strictly dependent on the level of impairment of the inpatients, the work plans and activity diaries for all the interventions carried out by each physiotherapist for a month were analyzed.
The outpatient interventions are, on the contrary, more standardized; we evaluated all the types of intervention carried out by the physiotherapist in the outpatient clinic, defining each of their frequency and duration in the work shift.
Each intervention was broken down into elementary operations, recording every dysergonomy regarding force commitment, repetitive movements, and maintenance of incongruous postures. The duration of each observed dysergonomy was summed, resulting in the overall biomechanical overload per work shift as a basis for RA by the multi-method methodology.
Such work was followed by direct observation and video filming of some rehabilitation interventions both on the wards and in outpatient clinics.
Each physiotherapist was observed for a half-shift during ward activity, as videotaping patients was impossible. The interventions carried out on seven patients (out of the 14 assigned to a single physiotherapist per shift) in the departments of Orthopedics and Traumatology, Internal Medicine, and Neurology were evaluated. The times of incongruous posture of the various articular districts of the upper limb (shoulder, elbow, wrist-hand), spine, and lower limbs and the number and duration of actions in force for each operation performed during the intervention on each patient were recorded.
Regarding the outpatient interventions, the activities of physiotherapists with more seniority in the department were videotaped, showing the rehabilitation interventions carried out on colleagues who acted as actors, with subsequent ergonomic evaluation.
For each task, the risk was calculated by integrating the results of multiple assessment methods from those proposed by the international literature.
As in our previous contributions [14-17], the RA followed the methodology indicated in the SIML Guidelines [18] on work-related musculoskeletal disorders and pathologies and according to the technical standard ISO 11228-3 [19]. The preliminary assessment consisted of verifying the existence of specific “items” proposed by the Washington State Assessment Standard (Caution Zone Checklist Washington, CZCW) [20]. The Standard’s more complex analytical level checklist (Hazard Zone Checklist Washington, HZCW) was applied to all investigated operations [20]. We chose this RA method because it guarantees the possibility of performing a holistic assessment of the biomechanical overload for the entire musculoskeletal system: spine, upper and lower limbs. The posture was assessed according to the technical standard ISO 11226:2000 [21]. This standard allows the analysis of static postures of the spine necessary for rehabilitation activities performed by physiotherapists.
For the assessment of manual handling tasks in lifting and pulling-pushing, the NIOSH equation for calculating the compound lifting index (ISC) [22] and the Snook and Ciriello tables [23] were used, respectively. The ACGIH-HAL methods [8] and the Italian version of the OREGE method developed by the French INRS [24, 25] were used to assess the risk of biomechanical overload of the upper limb. Among the various methods proposed in the international literature, the manual activity index offers the possibility of having an estimate of the risk focused on the hand-wrist district, which is mainly involved in some peculiar rehabilitation activities such as manipulations and bandages. The OREGE method thoroughly evaluates all anatomical districts of the upper limb and cervical spine.
Figure 1 shows the step-by-step evaluation phases to explain better and visualize the calculations performed to define the risk.
Figure 1.
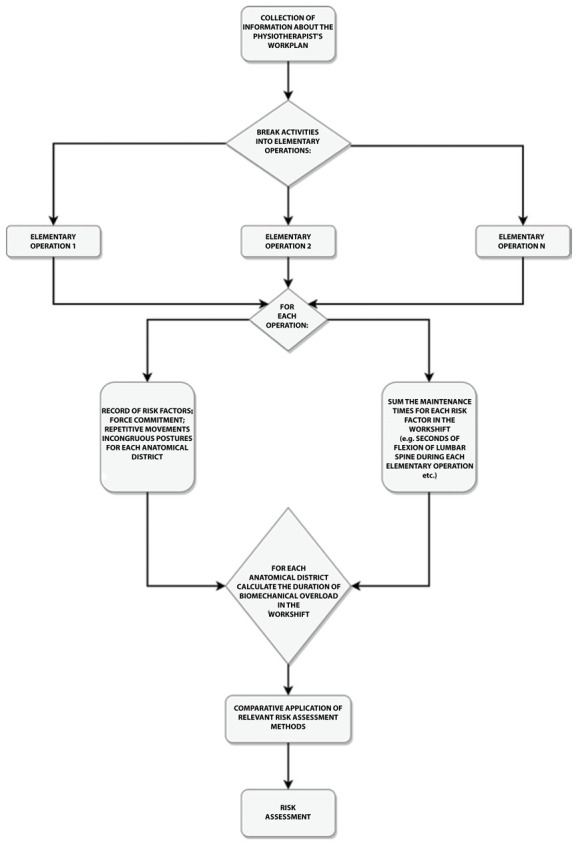
Diagram of the calculation performed to define the risk.
To verify/validate the risk assessment, we retrieved the results of the health surveillance carried out according to Italian Legislative Decree 81/08 over the last five years, aggregating them according to the occurrence of musculoskeletal pathologies and stratifying them by gender and age. Overall, we evaluated 221 medical records of 160 workers and calculated the incidence and prevalence of musculoskeletal diseases and disorders during the considered period.
3. Results
The information obtained by the coordinators by breaking down the work plans into tasks (rehabilitation interventions) and elementary operations resulted in the sequences of activities highlighted in Table 1 for interventions in the wards.
Table 2 shows the results of the RA for the different rehabilitation interventions. Only for the activities in Orthopedics and Medicine departments (Comprehensive Rehabilitation), the preliminary risk assessments, according to Caution Zone Checklist of State of Washington (CZCW) [20], showed the need for in-depth assessment of the risk of manual handling of patients with methods of higher analytical level such as the Hazard Zone Checklist of State of Washington (HZCSW) [20], as well as the assessment according to the technical standard ISO 11226:2000 [21] that did not show critical issues worthy of note.
Table 2.
Results of the biomechanical overload RA of the spine and upper limb in different rehabilitation interventions.
| Department / Intervention | Caution Zone Checklist W | Hazard Zone Checklist W | ISO 11226:2000 | NIOSH | Snook - Ciriello | HAL ACGIH | OREGE |
|---|---|---|---|---|---|---|---|
| Orthopedics and Traumatology1 | + MMC > 34 Kg 1 die |
0 | A | ||||
| Medicine (comprehensive rehabilitation) | + MMC > 34 Kg 1 die |
0 | A | ||||
| Neurosurgery1 | 0 | 0 | A | ||||
| Outpatient clinics1 | 0 | 0 | A | ||||
| US immersion activities | 0 | 0 | A | A ISC | Low risk | ||
| M 18-45 yy. : 0,41 |
I.S.R. F.I. Thrust (M): 0.02 | ||||||
| M <18 yy. >45 yy. : 0,51 |
I.S.R. F. M (M):0.02 | ||||||
| F 18-45 yy. : 0,51 |
I.S.R. F.I. Thrust (F): 0.04 | ||||||
| F <18 yrs and >45 yrs 0,68 | I.S.R. F. M (F): 0.03 | ||||||
| US massage activities | 0 | 0 | A | Low risk | |||
| I.S.R. F.I. Thrust (M): 0.19 | |||||||
| I.S.R. F. M (M):0.17 | |||||||
| I.S.R. F.I. Thrust (F): 0.26 | |||||||
| I.S.R. F. M (F): 0.29 | |||||||
| Lower limb adhesive-elastic bandage | 0 | 0 | A | A(6) | |||
| Lower limb rehabilitation | 0 | 0 | A | A | A(6) | ||
| Locked shoulder | 0 | 0 | A | ||||
| Dystrophic patient | 0 | 0 | A | ||||
| Pediatric clubfoot | 0 | 0 | A | ||||
| Pediatric Myogenic Torticollis | 0 | 0 | A |
Legend: A: acceptable; 0: no item present; ISC: complex lifting index; I.S.R. F.I.: Risk index for the initial force in thrust; I.S.R. F.M.: Risk index for thrust holding force; MMC: manual handling of loads.
For all the other workstations investigated, there were no critical points relating to the manual handling of loads. The dysergonomies observed at the upper limb, spine, and knee level are noted in Table 3, with an indication of their duration and entity. In any case, these do not configure a significant risk. They are diluted in the work shift, allowing an optimal functional recovery of the musculoskeletal system. However, a few suggestions for preventive interventions are presented at the end of the same table.
Table 3.
Duration of dysergonomies observed in the working shift for different musculoskeletal segments.
| Interventions | Upper limb | Spine | Inf. limb | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Side* | Shoulder | Elbow | Wrist | Force Pinch | Force commitment | C | L | Knee | |
| Orthopedics and Traumatology | R | 16'03" | 3'02" | 15'50" | 2'06" | 5'55" | 22'12" | 25'31" | 28'9" |
| L | 12'10" | 3'47" | 7'41" | 4'3" | 6'7" | ||||
| Medicine (comprehensive re-education)1 | R | 10'05" | - | - | - | 6' 7" | 22'12" | 3'30" | 5' |
| L | 10'05" | - | - | - | 6' 7" | ||||
| Neurosurgery | R | 10" | 3'02" | 14' | - | 3'max/5' moderate | 2' | 10' | 2' |
| L | - | - | - | - | - | ||||
| Outpatient clinics | R | 12" | - | 26'30'' | 62' | 12' | 29' | - | |
| L | - | - | - | - | - | ||||
| Ultrasound massage | R | - | - | - | - | - | - | 4" | - |
| L | - | - | - | - | - | ||||
| Lower limb adhesive-elastic bandage2 | R | - | - | 10'6'' | - | - | - | - | - |
| L | - | - | - | - | - | ||||
| Lower limb | R | 5' nc | - | - | 4'10'' (minimum force) |
- | 5' nc | 5' nc | - |
| L | - | - | 5'nc | - | - | - | |||
| Locked shoulder | R | - | - | 86'35'' nc | - | - | 25'40'' nc |
7' nc | - |
| L | - | - | - | - | - | - | |||
| Dystrophic patient3 | R | - | - | 32'nc | - | - | 19'50'' nc |
10'25'' nc | - |
| L | - | - | - | - | - | - | |||
Legend: nc: non-continuous.
1 Squatting for 5’ with the first patient is not necessary. It would be appropriate to eliminate this dysergonomy by replacing this posture with sitting on a chair.
2 Need to keep the bandages taut when applying them to the affected limb. Consequently, it is essential to have a height-adjustable table to avoid elevation of the shoulders or flexion of the cervical spine, or incongruous postures of the lumbar spine.
3 Fully uncooperative patient, positioned for treatment on two juxtaposed couches. Consequently, to treat a hemisoma, the operator must kneel on the couch to perform the treatment.
* R: Right, L: Left
The pooled results of the health surveillance carried out in 2016-2021 show 21 physiotherapists out of 160 (13%) affected by at least one musculoskeletal pathology and five (3%) by more than one. Table 4 shows the main characteristics of the analyzed population.
Table 4.
Characteristics of workers.
| Number of physiotherapists | Mean Age (years) | Length of service (years) | Physiotherapists with symptoms | WRMSDs | Not WRMSDs |
|---|---|---|---|---|---|
| 160 | 47,5 | 19,46 | 21* (13%) | 1*° | 25* |
| 32 Male 128 Female |
0 (0%) Male 21 (100%) Female |
* More than one MSD affected the same physiotheraphist.
° Pathology diagnosis before employment in the physiotherapy department.
The 26 musculoskeletal pathologies found are distributed as follows: 12 (46%) cervical discopathies, 7 (27%) shoulder tendinopathies, 3 (11%) coxarthrosis, 1 (4%) spondylolisthesis, 1 (4%) rhizarthrosis, 1 (4%) dorsal discopathy and 1 (4%) lumbosacral discopathy (Figure 2).
Figure 2.
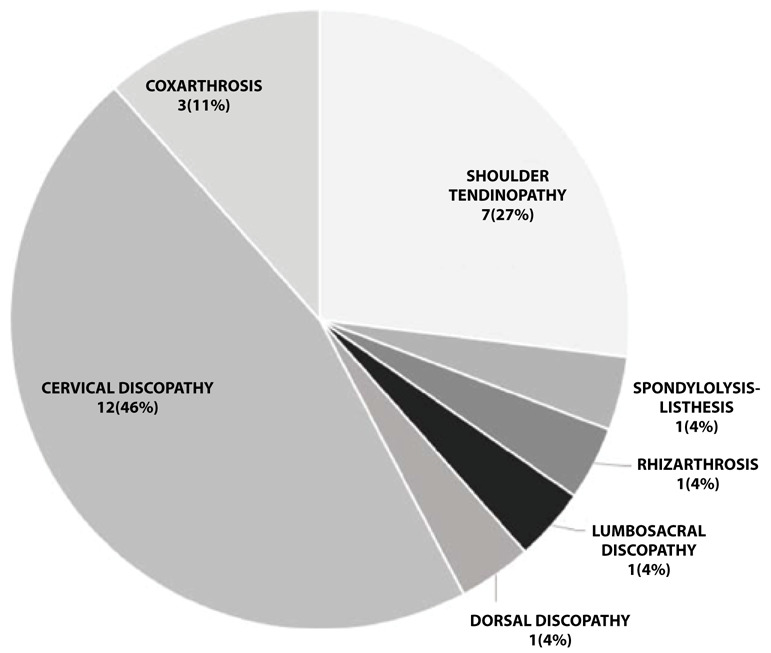
MSDs distribution in physiotherapists from 2016 to 2021.
The diagnosis of these pathologies was always supported by the reports of instrumental examinations such as muscle-tendon ultrasound and magnetic resonance imaging (MRI) for shoulder and radiography (RX) and MRI for lumbosacral discopathy. The pathologies’ onset is before the period considered, the most recent one dating back to 2010. None of the pathologies presents characteristics of technopathy. Local trauma and subacromial impingement played a significant role in the onset of the tendinopathies observed in 7 of the 8 musculoskeletal pathologies analyzed. The only case of lumbosacral discopathy was recognized as an occupational disease for other work performed before employment in the physiotherapy department before 2016.
4. Discussion
Although numerous literature studies have investigated biomechanical risk factors for functional rehabilitation technicians [1-3, 26-29], there are relatively few studies assessing the magnitude of these risks and comparing the results of RA with the prevalence of musculoskeletal disorders in employees diagnosed by imaging techniques. Studies using surface electromyography (sEMG) combined with questionnaires have been conducted to assess the risk of biomechanical overload of the upper limb in physiotherapists [4]; sEMG combined with 3D camera recording and load cells has been exploited experimentally to quantify biomechanical overload of the spine and lower limb during manual mobilization of patients [30]. The European report (Assessing Arm Elevation at Work with Technical Systems, PEROSH Joint Research Project Recommendations for procedures to measure occupational, physical activity and workload, 2018) [31] recommends instrumental and observational RA methods a best practice, especially where the observational method can help the interpretation of experimental data.
Aims of future studies will be the objectification of risk analysis performed using observational methods with objective RA tools (surface electromyography, load cells, kinematic sensors, and optoelectronic systems).
Furthermore, the proposed method could be extended to other healthcare workers engaged in highly demanding biomechanical tasks in medical and surgical wards.
The main aim of our study was to set up a methodology (WB-RAMBO) for a holistic RA of biomechanical overload to all musculoskeletal segments, including upper and lower limbs and spine for all the activities performed by physiotherapists during the work shift, according to information drawn from work plans and activity diaries.
As already extensively described in the “Methods” section of this contribution, the choice of the methods used to carry out the RA was directed towards methods allowing the analysis of the entire musculoskeletal apparatus (upper limbs, lower limbs, and spine). We also chose methods that allowed a deepening of the biomechanical overload for certain anatomical districts considered more stressed in this activity. Since the starting basis of WB-RAMBO is the operators’ work plan, the multi-methodological comparative approach proposed here may, in the future, be modified by choice of other methods more focused on the analysis of the districts most overloaded by the performed tasks. However, the objective of WB-RAMBO remains the multi-methodological RA of the tasks identified in the work plans of healthcare workers (HCWs) employed in outpatient and ward activities.
With the WB-RAMBO method, we performed a biomechanical overload RA for all tasks carried out by rehabilitation technicians based on field observation and videotaping of both outpatient and inpatient activities. As previously highlighted, the daily activities performed by physiotherapists cannot be standardized due to the variability of the patients treated. We tried to overcome such bias by following the same operator in a half-day or an entire 8-hour shift to represent the workload better. Where not possible, activities were simulated by experienced staff. The diaries of the activities carried out in a month of work were also examined to verify whether the observed shift could be defined as “standard” and, therefore, whether all the types of rehabilitation intervention carried out had been subject to evaluation.
The results of our RA method show a situation of acceptability from the ergonomic point of view, both for outpatient and ward activities. The comparative multi-methodological analysis has shown the absence of significant dysergonomies in terms of extent and duration in the shift. The observed ones, although of slight entity, are diluted in the work shift and allow an optimal functional recovery of the musculoskeletal apparatus.
The results were compared with the evidence from worker health surveillance to verify their accuracy. In this specific hospital, such a comparison confirmed RA results with little evidence of physiotherapists’ musculoskeletal pathologies (Figure 1). Although with wide variability in prevalence among the different data available in the literature, physiotherapists have the highest prevalence of musculoskeletal disorders in the lumbar spine district (32-80% of reported disorders) [1, 2, 26, 32-34]. In the analyzed sample, the highest percentages are found for cervical discopathy (46%).
A prevalence of 27% emerges for shoulder tendinopathy. Such a prevalence is consistent with only some literature data [33, 34], whereas lumbosacral discopathies account for only 4%, values lower than those reported in the literature for this district [1, 2, 26, 32-34].
5. Conclusions
In conclusion, our study demonstrates that the evaluated physiotherapist tasks can be considered “safe” from an ergonomic point of view. There are no dysergonomies of such duration and entity as to configure an overload for the musculoskeletal system of workers.
The analysis of health data confirms the results of the risk assessment, the prevalence of MSDs is, in fact, lower in our population than in the literature data. WB-RAMBO method allows us to sound out the work plans and analyze each elementary task in biomechanical overload, which is particularly useful for defining prevention measures and better managing the fitness of hypersusceptible workers. The point is particularly useful for occupational physicians in managing hypersusceptible workers whose professionalism does not make them easily relocatable to other operating units. Such subjects can be adequately protected, excluding them from most overloading sub-tasks while maintaining the rest of other activities. Weighing up the duration and frequency of each sub-task makes it easier to draw up a personalized work plan for a worker suffering from a musculoskeletal disease or disorder.
From the management point of view, such a detailed analysis of the work plan allows for intervention by reorganizing the plan itself, where necessary, through a congruous distribution among workers and in the shift of sub-tasks with a more significant biomechanical load. This tool is handy to the Coordinator in drawing up the work plan because it is thus able to distribute the operations with more significant overload better and alternate them with a less biomechanical load. Our study proposes a holistic assessment of biomechanical overload to the musculoskeletal apparatus for each activity performed by the physical therapist through a multimethodological assessment approach with few precedents in the literature [13]. The starting point for identifying the activities under evaluation is the physical therapist’s work plans and activity diaries. The assessment of risk from biomechanical overload to the musculoskeletal system must be based on official technical-organizational data by providing for the collaboration of all the professional figures involved: occupational physician, company management, coordinators, workers. A work plan subject to such a peculiar analysis can be redesigned and adapted to the organizational needs of the company but also to the hypersusceptible worker to ensure constant worker-environment-work compatibility [35].
Acknowledgements:
We would like to thank the management, the Coordinator, and the Spedali Civili Hospital of Brescia workers for their collaboration.
Funding:
This research received no external funding.
Institutional Review Board Statement:
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this study, as it was performed in the context of risk assessment in the occupational context, that is compulsory according to the Italian Decree 81/2008.
Informed Consent Statement:
Patient consent was waived due to the reasons above explained. Data were treated according to the Italian Legislative Decree 196/2003 and the EU Regulation 2016/679.
Declaration of Interest:
The authors declare no conflict of interest.
References
- 1.Rozenfeld V, Ribak J, Danziger J, Tsamir J, Carmeli E. Prevalence, risk factors and preventive strategies in work-related musculoskeletal disorders among Israeli physical therapists. Physiother Res Int. 2010;15(3):176–184. doi: 10.1002/pri.440. Doi:10.1002/pri.440. [DOI] [PubMed] [Google Scholar]
- 2.Grooten WJ, Wernstedt P, Campo M. Work-related musculoskeletal disorders in female Swedish physical therapists with more than 15 years of job experience: prevalence and associations with work exposures. Physiother Theory Pract. 2011;27(3):213–222. doi: 10.3109/09593985.2010.481323. Doi:10.3109/09593985.2010.481323. [DOI] [PubMed] [Google Scholar]
- 3.Petracca M, Bongiorni M, Bartoletti R, Villa L, Candura SM. Movimentazione manuale, idoneità alla mansione e disturbi muscolo-scheletrici negli operatori sanitari dell’Ospedale di Sondrio [Manual handling, job fitness, and musculoskeletal disorders in the Sondrio hospital (Italy) healthcare workers.] G Ital Med Lav Ergon. 2018;40(4):203–207. [PubMed] [Google Scholar]
- 4.Lupi A, Martinelli R, Tobia L, Paoletti A. Valutazione del rischio da sovraccarico biomeccanico dell’art superiore nei tecnici di fisiokinesiterapia [Evaluation of risks of biomechanical overload of the upper limb in physical kinesis therapists] G Ital Med Lav Ergon. 2005;27(2):235–236. [PubMed] [Google Scholar]
- 5.Gerbaudo L, Violante B. Correlazione tra disturbi muscolo-scheletrici e posture disergonomiche in un gruppo di operatori sanitari di un’azienda ospedaliera [Relationship between musculoskeletal disorders and work-related awkward postures among a group of health care workers in a hospital] Med Lav. 2008;99(1):29–39. [PubMed] [Google Scholar]
- 6.Passier L, McPhail S. Work related musculoskeletal disorders amongst therapists in physically demanding roles: qualitative analysis of risk factors and strategies for prevention. BMC Musculoskelet Disord. 2011;12:24. doi: 10.1186/1471-2474-12-24. Published 2011 Jan 25. Doi:10.1186/1471-2474-12-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hignett S, McAtamney L. Rapid entire body assessment (REBA) Appl Ergon. 2000;31(2):201–205. doi: 10.1016/s0003-6870(99)00039-3. Doi:10.1016/s0003-6870(99)00039-3. [DOI] [PubMed] [Google Scholar]
- 8.ACGIH. American Conference of Governmental Industrial Hygienists (ACGIH) TLVs and BEIs. Cincinnati: American Conference of Governmental Industrial Hygienists; 2000. [Google Scholar]
- 9.Occhipinti E, Colombini D, Occhipinti M. Metodo Ocra: messa a punto di una nuova procedura per l’analisi di compiti multipli con rotazioni infrequenti [Ocra Method: development of a new procedure for analysis of multiple tasks subject to infrequent rotation] Med Lav. 2008;99(3):234–241. [PubMed] [Google Scholar]
- 10.Moore JS, Garg A. The Strain Index: a proposed method to analyze jobs for risk of distal upper extremity disorders. Am Ind Hyg Assoc J. 1995;56(5):443–458. doi: 10.1080/15428119591016863. Doi:10.1080/15428119591016863. [DOI] [PubMed] [Google Scholar]
- 11.Battevi N, Menoni O, Ricci MG, Cairoli S. MAPO index for risk assessment of patient manual handling in hospital wards: a validation study. Ergonomics. 2006;49(7):671–687. doi: 10.1080/00140130600581041. Doi:10.1080/00140130600581041. [DOI] [PubMed] [Google Scholar]
- 12.Menoni O, Ricci MG, Panciera D, Occhipinti E. Valutazione dell’esposizione ad attività di movimentazione manuale dei pazienti nei reparti di degenza: metodi, procedure, indice di esposizione (MAPO) e criteri di classificazione [The assessment of exposure to and the activity of the manual lifting of patients in wards: methods, procedures, the exposure index (MAPO) and classification criteria. Movimientazione e Assistenza Pazienti Ospedalizzati (Lifting and Assistance to Hospitalized Patients)] Med Lav. 1999;90(2):152–172. [PubMed] [Google Scholar]
- 13.Baracco A, Coggiola M, Bosio D, et al. Whole body biomechanical burden of healthcare workers: proposal for a complementary risk assessment and management tool (HOARA) Med Lav. 2019;110(5):372–388. doi: 10.23749/mdl.v110i5.7624. Published 2019 Oct 29. Doi:10.23749/mdl.v110i5.7624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sala E, Torri D, Apostoli P. Esperienze di applicazione della valutazione del rischio dalle Linee Guida SIMLII sul rischio biomeccanico per l’arto superiore [The risk assessment procedures from SIMLII guidelines on upper extremity musculoskeletal disorders: discussion on results about a casistic from different working conditions] G Ital Med Lav Ergon. 2008;30(3 Suppl):20–25. [PubMed] [Google Scholar]
- 15.Sala E, Torri D, Tomasi C, Apostoli P. Stima del rischio da sovraccarico biomeccanico all’arto superiore condotta, con l’impiego di più metodi di analisi, in diversi settori manifatturieri [Risk assessment for upper extremity work related muscoloskeletal disorders in different manufactures by applying six methods of ergonomic analysis] G Ital Med Lav Ergon. 2010;32(2):162–173. [PubMed] [Google Scholar]
- 16.Sala E, Bonfiglioli R, Fostinellil J, et al. Metodi di valutazione del rischio da sovraccarico biomeccanico all’apparato muscolo scheletrico a confronto: esperienza applicativa di dieci anni [Risk assessment comparison of biomechanical overloading of the musculoskeletal system: 10 years’ applied experience] G Ital Med Lav Ergon. 2014;36(4):260–266. [PubMed] [Google Scholar]
- 17.Apostoli P, Sala E, Curti S, Cooke RM, Violante FS, Mattioli S. Loads of housework? Biomechanical assessments of the upper limbs in women performing common household tasks. Int Arch Occup Environ Health. 2012;85(4):421–425. doi: 10.1007/s00420-011-0690-z. Doi:10.1007/s00420-011-0690-z. [DOI] [PubMed] [Google Scholar]
- 18.Apostoli P, Occhipinti M, Romano C, et al. Pavia Pime Editrice; 2006. Linee guida per la prevenzione dei disturbi e delle patologie muscolo scheletriche dell’arto superiore correlati con il lavoro. [Google Scholar]
- 19.British Standards Institute. BS ISO 11228-3:2007 Ergonomics - Manual handling - Part 3: Handling of low loads at high frequency. 2015;3(August) Avaiable on line at: https://www.iso.org/standard/26522.html. (last accessed 02-09-2022) [Google Scholar]
- 20.Washington State Department of Labor and Industries. Ergonomics. Olympia (WA): Washington State Department of Labor and Industries, 2000. WAC 296-62-051. Available at http://www.lni.wa.gov/Safety/Topics/Ergonomics/ServicesResources/Tools/default.asp . (last accessed 01-06-2022) [Google Scholar]
- 21.ISO 11226. ISO 11226:2000(en), Ergonomics - Evaluation of static working postures. 2000. Avaiable on line at: https://www.iso.org/standard/25573.html (last accessed 01-09-2022) [Google Scholar]
- 22.Waters TR, Putz-Anderson V, Garg A, Fine LJ. Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. 1993;36(7):749–776. doi: 10.1080/00140139308967940. Doi:10.1080/00140139308967940. [DOI] [PubMed] [Google Scholar]
- 23.Snook SH, Ciriello VM. The design of manual handling tasks: Revised tables of maximum acceptable weights and forces. Ergonomics. 1991;34(9):1197–1213. doi: 10.1080/00140139108964855. Doi:10.1080/00140139108964855. [DOI] [PubMed] [Google Scholar]
- 24.Apostoli P, Bazzini G, Sala E, Imbriani M. La versione italiana “OREGE” (Outil de Repérage et d’Evaluation des Gestes) dell’INRS (Institut national de recherche et de sécurité) per la valutazione dei disturbi muscolo-scheletrici dell’arto superiore [The Italian version of “OREGE” (Outil de Repérage et d’Evaluation des Gestes) of the INRS (Institut national de recherche et de sécurité) for the assessment of musculoskeletal disorders of the upper limb] G Ital Med Lav Ergon. 2002;24(1):3–25. [PubMed] [Google Scholar]
- 25.Apostoli P, Sala E, Gullino A, Romano C. Analisi comparata dell’applicazione di quattro metodi per la valutazione del rischio biomeccanico per l’arto superiore [Comparative analysis of the use of 4 methods in the evaluation of the biomechanical risk to the upper limb] G Ital Med Lav Ergon. 2004;26(3):223–241. [PubMed] [Google Scholar]
- 26.Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 2000;80(4):336–351. doi: 10.1093/ptj/80.4.336. Doi:10.1093/ptj/80.4.336. [DOI] [PubMed] [Google Scholar]
- 27.Vieira ER, Schneider P, Guidera C, Gadotti IC, Brunt D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J Back Musculoskelet Rehabil. 2016;29(3):417–428. doi: 10.3233/BMR-150649. Doi:10.3233/BMR-150649. [DOI] [PubMed] [Google Scholar]
- 28.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57(11):649–655. doi: 10.1136/ard.57.11.649. Doi:10.1136/ard.57.11.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ostör AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology. 2005;44:800–805. doi: 10.1093/rheumatology/keh598. doi:10.1093/rheumatology/keh598. [DOI] [PubMed] [Google Scholar]
- 30.Brinkmann A, Fifelski C, Lau S, et al. Quantification of Lower Limb and Spine Muscle Activity in Manual Patient Handling - A Case Study. Stud Health Technol Inform. 2020;272:249–252. doi: 10.3233/SHTI200541. doi:10.3233/SHTI200541. [DOI] [PubMed] [Google Scholar]
- 31.Weber B, Douwes M, Forsman M, Könemann R, Heinrich K, Enquist H, Pinder A, Punakallio A, Uusitalo A, Ditchen D, et al. Assessing Arm Elevation at Work with Technical Systems; Partnership for European Research in Occupational Safety and Health: Sydney, NSW, Australia, 2018. DOI: 10.23775/20181201. [Google Scholar]
- 32.Holder NL, Clark HA, DiBlasio JM, et al. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys Ther. 1999;79(7):642–652. doi: 10.1093/ptj/79.7.642. doi:10.1093/ptj/79.7.642. [DOI] [PubMed] [Google Scholar]
- 33.Carta A, Parmigiani F, Parrinello G, Porru S. Fisioterapisti e disturbi muscoloscheletrici: analisi di una casistica [A survey on musculoskeletal disorders in physiotherapists] G Ital Med Lav Ergon. 2007;29(3 Suppl):583–584. [PubMed] [Google Scholar]
- 34.Alrowayeh HN, Alshatti TA, Aljadi SH, Fares M, Alshamire MM, Alwazan SS. Prevalence, characteristics, and impacts of work-related musculoskeletal disorders: a survey among physical therapists in the State of Kuwait. BMC Musculoskelet Disord. 2010;11:116. doi: 10.1186/1471-2474-11-116. Published 2010 Jun 11. doi:10.1186/1471-2474-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Apostoli P, Cristaudo A, Violante FS. SIML 2017. Nuova Editrice Berti; 2017. Linee guida per la Sorveglianza Sanitaria. [Google Scholar]


