Abstract
Objectives
To characterize trends in pediatric mental health visit counts, including visits for prolonged length of stay (LOS), in a sample of emergency departments (EDs) from 29 states during COVID‐19.
Methods
We performed a secondary analysis of the Clinical Emergency Data Registry from January 2020 through December 2021. We reported trends in pediatric mental health visit counts overall and for those with prolonged ED LOS. We reported incident rate ratios (IRRs) for monthly counts compared to January 2020. Among visits with LOS >24 hours, we reported on the most common diagnostic categories.
Results
There were 107 EDs from 29 states with available complete data in 2020 and 2021. Pediatric mental health visit counts resulting in a LOS greater than 6, 12, and 24 hours were higher for much of 2021. At their peak, there were 604 visits with LOS >12 hours (IRR, 2.14; 95% confidence interval [CI], 1.86–2.47) and 262 visits (IRR, 2.46; 95% CI, 1.97–3.09) with LOS >24 hours in April 2021. Pediatric mental health visits with LOS >12 hours and >24 hours made up 20.9% and 7.3% of pediatric mental health visits overall, respectively. For visits with ED LOS >24 hours, the most common diagnostic categories were suicide or self‐injury, depressive disorders, and mental health syndrome.
Conclusions
In this sample of 107 EDs in 29 states, visit counts with prolonged LOS >24 hours more than doubled in some months since the arrival of COVID‐19. These findings are indicative of an increasingly strained emergency and mental health system.
Keywords: emergency department crowding, length of stay, mental health, pediatrics
1. INTRODUCTION
1.1. Background
The COVID‐19 pandemic has had an extraordinary impact on the mental health of children, either as a direct result of trauma related to the pandemic, reduced access to outpatient mental health care, or by social stressors related to caregiving disruptions or social isolation. 1 Data from the National Syndromic Surveillance Program have demonstrated growth in emergency department (ED) visits for mental health conditions, most significantly among girls ages 12–17 years through January 2022. 2 Although pediatric ED visits overall fell early in the pandemic, by as much as 45.7% in 1 large study, multiple studies demonstrate the greater burden of mental health visits extend through December 2020. 4 , 5 , 6 Greater demand for ED‐based pediatric mental healthcare may portend worsening boarding and crowding. Previous work from before COVID‐19 has documented a decade‐long trend toward increasingly prolonged ED length of stay (LOS) for pediatric patients with mental health conditions. 7 This problem may have been further exacerbated by shifting ED, hospital, and behavioral health facility operational practices early in the pandemic. 8 Understanding trends in LOS during COVID‐19 is essential for policymakers seeking to better match mental health care resources to the needs of children.
1.2. Importance
Although limited survey data suggest mental health boarding has worsened during COVID‐19, 9 there is a paucity of literature addressing prolonged LOS for children with mental health needs in community EDs, the site of the vast majority of pediatric ED visits nationally. 10 For these patients, the ED is a place for diagnosis, triage, and potentially brief intervention. Prolonged LOS may represent a delay in the transition to definitive care. A more complete understanding of prolonged ED LOS for children with mental health conditions, inclusive of community EDs, is essential to inform policymaking around pediatric mental health services.
1.3. Goals of this investigation
We aimed to characterize pediatric mental health visit counts, including for prolonged ED LOS, in a sample of community EDs across 29 states, from January 2020 to December 2021. We hypothesized that increased mental health stressors and health system capacity constrains would result in an increase in visits with prolonged ED LOS for children with mental health conditions.
2. MATERIALS AND METHODS
2.1. Study design and setting
We performed a secondary analysis of pediatric (≤17 years of age) ED visits in a sample of 107 EDs that had complete data in the Clinical Emergency Data Registry (CEDR). 11 CEDR is a Centers for Medicare & Medicaid Services Qualified Clinical Data Registry that includes data provided by a large sample of voluntarily participating EDs across the United States. CEDR is primarily composed of smaller community‐based emergency medicine groups seeking efficient quality reporting in the CMS merit‐based incentive payment system. For the subset of EDs with complete visit‐level data in 2020 and 2021, EDs associated with hospitals were linked to the 2020 American Hospital Association Annual Survey to identify hospital characteristics. We described EDs in the analysis sample according to their visit volume, urban–rural designations, US census region, ownership status, and teaching status.
We identified pediatric mental health visits according to International Classification of Disease‐10 (ICD‐10) codes consistent with the Child and Adolescent Mental Health Disorder Classification System (CAMHD‐CA), which classifies pediatric mental health disorders across ICD‐10 and aligns with the Diagnostic and Statistical Manual of Mental Health Disorders, Fifth Edition and Clinical Classifications Software. 12 This definition included diagnoses of autism spectrum disorder, developmental delay, and injury codes related to suicide attempt and intentional self‐harm. We reported on ED visits with any of these mental health diagnosis codes and separately for all other non‐mental health‐related ED visits.
2.2. Outcomes
The primary outcomes were monthly ED visit counts for mental health‐related visits, count of visits resulting in either of admit or transfer to another facility, and count for visits with prolonged ED LOS. We reported monthly count of pediatric ED visits with prolonged ED LOS consistent with prior studies: >6, 12, and 24 h. 7
The Bottom Line
In this secondary analysis of administrative data from 107 emergency departments (EDs) in the Clinical Emergency Department Registry, the authors found that pediatric mental health ED visits with prolonged lengths‐of‐stay increased significantly during the COVID‐19 pandemic despite an overall decrease in pediatric ED visits, suggesting mental health resources were not able to meet demand.
2.3. Analysis
We reported on monthly counts across all sample EDs during different pandemic periods as compared to January 2020. We calculated incident rate ratios (IRRs) for the monthly count of visits, as compared to the January 2020 level, with 95% confidence intervals (CIs) adjusted for clustering at the ED‐level. We plotted counts for weekly overall visits, visits resulting in admit/transfer, and visits with >6, >12, and >24 h LOS. Overall visits and those resulting in admit/transfer were plotted with overlaid nonparametric smoothed curves, generated with a locally weighted scatter smoothing method and 95% confidence regions (locally estimated scatterplot smoother (LOESS)). LOESS bandwidth in each plot was identified by minimizing the associated bias‐corrected Akaike information criterion. 12 For visits resulting in LOS >12 h and >24 h, we reported on their proportion relative to overall pediatric mental health visits. We tested for the difference in proportion with prolonged LOS, for mental health versus non‐mental health pediatric visits, using unadjusted logistic regression model with standard errors corrected for clustering at the ED level. We also reported pooled visit counts across EDs by their US census region. Due to the limitation that we do not have pre‐pandemic data for all sample EDs, we performed a secondary analysis of visit counts in a subset of 33 EDs with complete data available in 2019, 2020, and 2021, and reported monthly IRRs for each month in 2020 and 2021, in that case as compared to the same month in 2019.
To further characterize the population of patients with prolonged LOS, we performed a post‐hoc frequency tabulation of CAMHD‐CA diagnostic categories for ED visits with LOS >24 h among pediatric mental health ED visits during the study period. Analyses were performed with R (version 4.1.2). This work was classified as exempt by the institutional review board at Yale University, and all results reporting adhered to Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
3. RESULTS
3.1. Site and patient characteristics
3.1.1. Sample characteristics
Our sample included 107 community EDs that had complete data in 2020 and 2021, found in 29 states. Median ED visit volume in 2020 was 29,662 (interquartile range [IQR], 17,696–40,503). All sites met American Hospital Association criteria for community hospital designation: nonfederal, short‐term hospitals whose facilities and services are available to the public. The sample of EDs spanned all census regions, including 13 in the Northeast, 22 in the Midwest, 38 in the South, 34 in the West. A total of 92 EDs (86%) were in urban areas whereas 15 (14%) sites were in micropolitan/rural areas. Sample EDs had a median proportion of pediatric visits, calculated from the CEDR data, of 11.1% (IQR, 8.7%–14.1%). Our sample period from January 2020 to December 2021 included 6,984,624 total (adult and pediatric) ED visits. A total of 997,209 (14.3%) of these visits were pediatric (age ≤17 years old) visits, and 43,301 visits (4.3% of overall pediatric visits) included a diagnosis code for a mental health condition. Across the sample of pediatric mental health visits, the median age was 15 years old (IQR, 13–16).
3.1.2. Pediatric mental health visits
Counts
The monthly counts of pediatric ED visits for mental health conditions across all EDs in March and April 2020 were below the January 2020 level, 1435 and 829, across sites (IRR, 0.76; 95% CI, 0.71–0.81 and IRR, 0.44; 95% CI, 0.41–0.48, respectively). Visit counts rose to a high of 2455 in September 2021 (IRR, 1.30; 95% CI, 1.23–1.38) (Table A1). Visit counts for non‐mental health conditions remained below levels seen in January 2020 throughout the study period (Figure 1). Overall visit counts were above levels seen in January 2020 for much of 2021, with greater visit counts in the Spring and Fall, consistent with seasonal patterns noted in prior literature. 13 The increase in visit counts for pediatric mental health visits contrasted with counts for non‐mental health visits, which were decreased relative to January 2020 throughout the study period.
FIGURE 1.
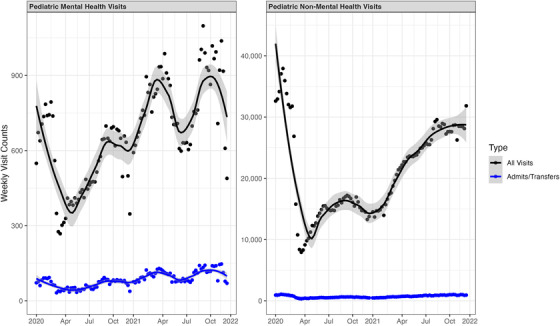
Pooled visit counts for pediatric visits in the analysis sample. Figure reports pooled weekly visit counts for mental health and non‐mental health as well as those resulting in admit or transfer. Sample includes pediatric visits across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021.
Admit/transfer counts
Early in the COVID‐19 pandemic, the count of pediatric mental health visits resulting in admit/transfer fell to 137 in April 2020 (IRR, 0.57; 95% CI, 0.46–0.70), before rising at or above January 2020 levels through much of 2021 (Figure 1). At their peak, there were 404 pediatric mental health visits resulting in admit/transfer in September 2021 (IRR, 1.68; 95% CI, 1.43–1.97) (Table A2).
Prolonged length of stay
Pediatric mental health visit counts resulting in LOS >6, >12, and >24 hours were higher for much of 2021 (Figure 2). At their peak relative to the January 2020 level, there were 975 such visits with LOS >6 hours (IRR, 1.92; 95% CI, 1.72–2.13) in November 2021. For visits with LOS >12 hours and 24 hours, counts were highest relative to January 2020 in April 2021 at 604 (IRR, 2.14; 95% CI, 1.86–2.47) and 262 (IRR, 2.46; 95% CI, 1.97–3.09), respectively (Tables A3, A4, and A5). Pediatric mental health visits with LOS >12 hours and >24 hours made up 20.9% and 7.3% of pediatric mental health visits overall, respectively, throughout the study period. In contrast, non‐mental health visits resulted in LOS >12 hours and >24 hours for only 1.8% and 0.2% of visits in our sample (P < 0.001 for differences in proportion).
FIGURE 2.
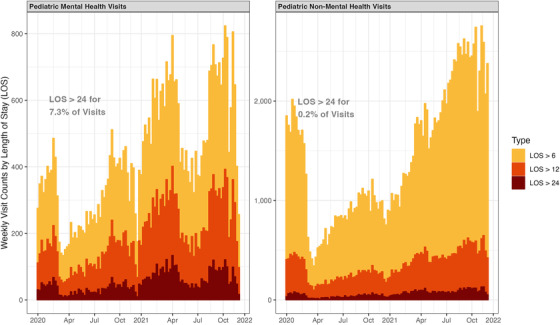
Pooled visit counts for pediatric visits with prolonged length of stay in the analysis sample. Figure reports pooled weekly visit counts for pediatric visits resulting in length of stay (LOS) greater than 6, 12, and 24 hours, for mental health and non‐mental health visits. Across all pediatric mental health visits in the study period, 7.3% resulted in an LOS >24 hours. In contrast, across all pediatric non‐mental health visits, 0.2% resulted in an LOS >24 hours. Sample includes pediatric visits across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021.
Distribution by US census region
Although overall visit counts for pediatric mental health visits exhibited similar patterns over time across US census region, visits with prolonged LOS among analyzed CEDR EDs were clustered in the Northeast and the South (Figure 3; Table A6.)
FIGURE 3.
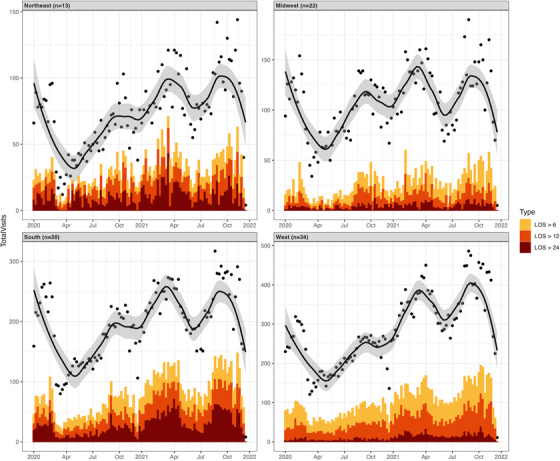
Pooled visit counts for pediatric visits with prolonged length of stay by US census region. Figure reports pooled weekly visit counts for pediatric visits resulting in length of stay (LOS) greater than 6, 12, and 24 h, for mental health visits. The sample included 13 emergency departments in the Northeast, 22 in the Midwest, 38 in the South, and 34 in the West. Sample includes pediatric visits across a total of 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021.
Secondary analysis
In a secondary analysis of 33 EDs with complete data reporting in 2019, 2020, and 2021 (Table A7), we found that overall pediatric mental health visit counts and counts for visits resulting in admit/transfer were below their 2019 baseline for much of 2020 and below or near their baseline for much of 2021 (Tables A8 and A9). In contrast, counts for visits with prolonged LOS were above their 2019 baseline for much of 2020 and 2021 (Tables A10, A11, and A12). Visits with LOS prolonged beyond 24 h were rare in the 2019 data, with only 12 such cases found across all 33 EDs, rising to 117 cases in 2021, and precluding stable point estimates for monthly incident rate ratios.
Diagnoses
Among pediatric patients with a mental health diagnosis and prolonged ED LOS >24 h in our analysis sample, the most common CAMHD‐CA diagnostic categories were suicide or self‐injury (2064 [66.3%]), depressive disorders (1325 [42.5%]), and mental health syndrome (868 [27.9%]) (Table 1).
TABLE 1.
Most common diagnostic categories among pediatric patients with mental health conditions and prolonged ED length of stay (>24 h) in 2020 and 2021
| Category | Count | Percent |
|---|---|---|
| Suicide or self‐injury | 2064 | 66.3 |
| Depressive disorders | 1325 | 42.5 |
| Mental health symptom | 868 | 27.9 |
| Disruptive, impulse control, and conduct disorders | 494 | 15.9 |
| Anxiety disorders | 439 | 14.1 |
| ADHD | 356 | 11.4 |
| Trauma and stressor‐related disorders | 343 | 11.0 |
| Miscellaneous | 232 | 7.4 |
| Autism spectrum disorder | 219 | 7.0 |
| Bipolar and related disorders | 144 | 4.6 |
Note: Percent is reported out of total ED visits. Column sums to greater than 100 because each ED visit can have multiple associated diagnosis codes. Categories of diagnostic codes are drawn from the Child and Adolescent Mental Health Disorder Classification System.
Abbreviations: ADHD, attention‐deficit/hyperactivity disorder; ED, emergency department.
4. LIMITATIONS
There are several important limitations of our work. Although these data include a sample of community EDs across the United States, this sample is likely not representative of community emergency medicine generally. Enrollment in the Clinical Emergency Data Registry is voluntary and more common for smaller hospital‐based EDs than larger sites. Although our secondary analysis of 33 EDs did show increased monthly visit counts with prolonged LOS in 2020 and 2021 as compared to the same months in 2019, our broader data reporting is limited to 2020 and 2021. Furthermore, we are not able to distinguish the subset of visits where a mental health condition is listed, but where the ED visit is for a primarily medical concern, as CEDR lacks a delineator for the “primary” diagnosis on the chart. This limitation is mitigated given that visits for primarily medical concerns can be expected to have lower LOS, and, therefore, this likely attenuates the severity of prolonged LOS for our analysis sample. Reporting of common diagnosis groups (Table 1) was an unplanned subgroup analysis. CEDR also lacks standardized data fields on race, ethnicity, and insurance status. Characterizing variable impact of prolonged LOS and linkage to downstream care across EDs must be a focus of future work, as these may be important mechanisms driving outcomes disparities. 9 Unfortunately, given the nature of this convenience sample of EDs and limitations for allowed data reporting of individual sites in CEDR, we were unable to report site‐level factors associated with prolonged LOS. Furthermore, our study dataset lacked the necessary timestamps and details to specifically describe time spent “boarding” in the ED (ie, a decision has been made to admit or transfer a child to an inpatient setting, but they continue to wait for definitive care). Future work should address to what extent prolonged LOS represents downstream capacity constraints, at other acute care facilities or at psychiatric facilities, versus time‐to‐admit decision by emergency physicians, psychiatrists, or social workers in the ED.
5. DISCUSSION
In a registry sample of 107 community EDs across 29 states in the United States, visit counts for mental health conditions with prolonged LOS have grown throughout the pandemic. This contrasts with non‐mental health visits, which have been below their January 2020 level throughout the pandemic era. This suggests inpatient or outpatient capacity for mental health services may not be meeting ongoing demands. In our sample of EDs, 1 in 5 children (20.9%) presenting to sample EDs with mental health conditions experienced prolonged ED stays exceeding 12 h in 2020 and 2021. This was higher than the peak identified in previous work with nationally representative data (12.7% in a nationally representative sample of pediatric mental health ED visits), 7 and many patients with extreme ED LOS exceeded 24 h.
This growth in ED LOS for pediatric mental health visits may be related to changes in the underlying epidemiology of children's mental health. First, the incidence of pediatric mental health problems may have worsened during COVID, due to increased psychosocial stressors, social isolation, 1 or loss of a caregiver. 14 Second, as community‐based transmission of SARS‐COV‐2 variants has persisted, patients in need of mental health care may have concomitant infectious symptoms and/or confirmed COVID infection. This may result in delays for outpatient mental health treatment, or greater referrals to the ED for diagnosis, risk stratification, and disposition due to COVID restrictions in other settings.
Broader system stressors outside the ED setting are likely to play a role in the capacity of the mental health system to provide timely definitive care for patients who present to the ED. To prevent community transmission of COVID‐19, some inpatient and outpatient mental health programs limited capacity early in the pandemic thereby decreasing available beds and delaying both transfers and discharges from EDs to a site of definitive care. In addition to limited isolation bed availability within the mental healthcare system, there may be outbreaks or staffing shortages in psychiatric facilities leading to closures or reduced services. Decreased access to outpatient services or school‐based care may have also resulted in more complex ED presentations and fewer options for ongoing care. ED‐based care can adapt to the need for prolonged boarding, for example, by implementing dedicated pediatric mental health liaison programs. 15 To the extent that these solutions are less viable for smaller and community EDs, telepsychiatry and partnerships with larger systems may be beneficial.
Future work on pediatric mental health readiness among community EDs should conceptualize ED LOS as a system indicator for access and quality. Rapid measurement and dissemination of ED presentations, admissions, and LOS can be used to monitor the impact of interventions targeting population mental health and as a proxy for broader system functioning, with the goal of a fully accessible, flexible, and integrated mental health system.
AUTHOR CONTRIBUTIONS
Alexander T. Janke and Arjun K. Venkatesh conceived the study and obtained the data. Alexander T. Janke performed the data analysis and drafted the manuscript. All authors contributed to the critical revision. Alexander T. Janke had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICTS OF INTEREST
Alexander T. Janke reports support from the VA Office of Academic Affiliation as part of the National Clinician Scholars Program at the VA Ann Arbor/University of Michigan. The views expressed here do not represent the US Government. Arjun K. Venkatesh reports receiving grants from the Centers for Medicare & Medicaid Services and the American College of Emergency Physicians outside the submitted work; receiving funding from an Emerging Infectious Diseases and Disaster Preparedness grant from the Society for Academic Emergency Medicine Foundation; and having committee leadership roles with the American College of Emergency Physicians and the Society for Academic Emergency Medicine. The other authors made no disclosures.
Biography
Alexander T. Janke, MD, MHS, is a Clinical Instructor in Emergency Medicine at the University of Michigan in Ann Arbor, Michigan. His interests are health policy and emergency care quality and value.

1.
TABLE A1.
Pooled monthly visit counts and incident rate ratios, all pediatric mental health visits
| ALL PEDIATRIC MENTAL HEALTH VISITS | 2020 | 2021 | ||
|---|---|---|---|---|
| Count | IRR (95% CI) | Count | IRR (95% CI) | |
| January | 1886 | (reference) | 1687 | 0.89 (0.84–0.96) |
| February | 2018 | 1.07 (1.00–1.14) | 1910 | 1.01 (0.95–1.08) |
| March | 1435 | 0.76 (0.71–0.81) | 2228 | 1.18 (1.11–1.26) |
| April | 829 | 0.44 (0.41–0.48) | 2332 | 1.24 (1.16–1.31) |
| May | 1181 | 0.63 (0.58–0.67) | 2343 | 1.24 (1.17–1.32) |
| June | 1204 | 0.64 (0.59–0.69) | 1835 | 0.97 (0.91–1.04) |
| July | 1342 | 0.71 (0.66–0.76) | 1659 | 0.88 (0.82–0.94) |
| August | 1455 | 0.77 (0.72–0.83) | 1850 | 0.98 (0.92–1.05) |
| September | 1831 | 0.97 (0.91–1.04) | 2455 | 1.30 (1.23–1.38) |
| October | 1887 | 1.00 (0.94–1.07) | 2334 | 1.24 (1.16–1.31) |
| November | 1770 | 0.94 (0.88–1.00) | 2295 | 1.22 (1.14–1.29) |
| December | 1546 | 0.82 (0.77–0.88) | 1955 | 1.04 (0.97–1.10) |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021. IRRs are reported against January 2020 reference. CIs are adjusted for clustering within EDs.
Abbreviations: CEDR, Clinical Emergency Data Registry; CI, confidence interval; ED, emergency department; IRRs, incident rate ratios; LOS, length of stay.
TABLE A2.
Pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting in admit/transfer
| VISITS RESULTING IN ADMIT/TRANSFER | 2020 | 2021 | ||
|---|---|---|---|---|
| Count | IRR (95% CI) | Count | IRR (95% CI) | |
| January | 241 | (reference) | 243 | 1.01 (0.84–1.21) |
| February | 262 | 1.09 (0.91–1.29) | 273 | 1.13 (0.95–1.35) |
| March | 179 | 0.74 (0.61–0.90) | 316 | 1.31 (1.11–1.55) |
| April | 137 | 0.57 (0.46–0.70) | 366 | 1.52 (1.29–1.79) |
| May | 149 | 0.62 (0.51–0.76) | 288 | 1.20 (1.01–1.42) |
| June | 126 | 0.52 (0.42–0.65) | 232 | 0.96 (0.81–1.15) |
| July | 175 | 0.73 (0.60–0.88) | 237 | 0.98 (0.82–1.18) |
| August | 156 | 0.65 (0.53–0.79) | 273 | 1.13 (0.95–1.35) |
| September | 242 | 1.01 (0.84–1.20) | 404 | 1.68 (1.43–1.97) |
| October | 213 | 0.89 (0.74–1.06) | 377 | 1.57 (1.33–1.84) |
| November | 240 | 1.00 (0.83–1.19) | 379 | 1.57 (1.34–1.85) |
| December | 173 | 0.72 (0.59–0.87) | 310 | 1.29 (1.09–1.52) |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021, for pediatric mental health visits resulting in admit or transfer. IRRs are reported against January 2020 reference. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio.
TABLE A3.
Pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting length of stay >6 h
| VISITS RESULTING IN LOS >6 h | 2020 | 2021 | ||
|---|---|---|---|---|
| Count | IRR (95% CI) | Count | IRR (95% CI) | |
| January | 509 | (reference) | 618 | 1.21 (1.08–1.37) |
| February | 571 | 1.12 (1.00–1.26) | 728 | 1.43 (1.28–1.60) |
| March | 447 | 0.88 (0.77–1.00) | 864 | 1.70 (1.52–1.89) |
| April | 256 | 0.50 (0.43–0.58) | 911 | 1.79 (1.61–1.99) |
| May | 339 | 0.67 (0.58–0.76) | 892 | 1.75 (1.57–1.95) |
| June | 373 | 0.73 (0.64–0.84) | 629 | 1.24 (1.10–1.39) |
| July | 415 | 0.82 (0.72–0.93) | 591 | 1.16 (1.03–1.31) |
| August | 471 | 0.93 (0.82–1.05) | 673 | 1.32 (1.18–1.48) |
| September | 640 | 1.26 (1.12–1.41) | 891 | 1.75 (1.57–1.95) |
| October | 655 | 1.29 (1.15–1.44) | 940 | 1.85 (1.66–2.06) |
| November | 647 | 1.27 (1.13–1.43) | 975 | 1.92 (1.72–2.13) |
| December | 545 | 1.07 (0.95–1.21) | 759 | 1.49 (1.33–1.67) |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021, for pediatric mental health visits resulting in length of stay >6 h. IRRs are reported against January 2020 reference. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A4.
Pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting length of stay >12 h
| VISITS RESULTING IN LOS >12 h | 2020 | 2021 | ||
|---|---|---|---|---|
| Count | IRR (95% CI) | Count | IRR (95% CI) | |
| January | 282 | (reference) | 360 | 1.28 (1.09–1.49) |
| February | 307 | 1.09 (0.93–1.28) | 436 | 1.55 (1.33–1.80) |
| March | 260 | 0.92 (0.78–1.09) | 560 | 1.99 (1.72–2.29) |
| April | 131 | 0.46 (0.38–0.57) | 604 | 2.14 (1.86–2.47) |
| May | 189 | 0.67 (0.56–0.81) | 566 | 2.01 (1.74–2.32) |
| June | 206 | 0.73 (0.61–0.87) | 350 | 1.24 (1.06–1.45) |
| July | 224 | 0.79 (0.67–0.95) | 327 | 1.16 (0.99–1.36) |
| August | 270 | 0.96 (0.81–1.13) | 402 | 1.43 (1.23–1.66) |
| September | 373 | 1.32 (1.13–1.54) | 552 | 1.96 (1.70–2.26) |
| October | 362 | 1.28 (1.10–1.50) | 578 | 2.05 (1.78–2.36) |
| November | 377 | 1.34 (1.15–1.56) | 574 | 2.04 (1.77–2.35) |
| December | 303 | 1.07 (0.91–1.26) | 449 | 1.59 (1.37–1.85) |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021, for pediatric mental health visits resulting in length of stay >12 h. IRRs are reported against January 2020 reference. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A5.
Pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting length of stay >24 h
| VISITS RESULTING IN LOS >24 H | 2020 | 2021 | ||
|---|---|---|---|---|
| Count | IRR (95% CI) | Count | IRR (95% CI) | |
| January | 107 | (reference) | 115 | 1.08 (0.83–1.41) |
| February | 106 | 1.00 (0.76–1.30) | 142 | 1.34 (1.04–1.72) |
| March | 93 | 0.87 (0.66–1.16) | 235 | 2.21 (1.76–2.78) |
| April | 24 | 0.23 (0.14–0.35) | 244 | 2.29 (1.83–2.88) |
| May | 75 | 0.71 (0.53–0.95) | 262 | 2.46 (1.97–3.09) |
| June | 68 | 0.64 (0.47–0.87) | 133 | 1.25 (0.97–1.61) |
| July | 70 | 0.66 (0.49–0.89) | 110 | 1.03 (0.79–1.35) |
| August | 69 | 0.65 (0.48–0.88) | 129 | 1.21 (0.94–1.57) |
| September | 95 | 0.89 (0.68–1.18) | 216 | 2.03 (1.61–2.56) |
| October | 105 | 0.99 (0.75–1.29) | 199 | 1.87 (1.48–2.37) |
| November | 112 | 1.05 (0.81–1.37) | 207 | 1.95 (1.54–2.46) |
| December | 66 | 0.62 (0.46–0.84) | 133 | 1.25 (0.97–1.61) |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021, for pediatric mental health visits resulting in length of stay >24 h. IRRs are reported against January 2020 reference. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments, IRRs, incident rate ratios; LOS, length of stay.
TABLE A6.
Visit counts by year and US census region
| US census region | VISIT COUNT | LOS >6 H | LOS >12 H | LOS >24 H |
|---|---|---|---|---|
| Northeast (n = 13) | ||||
| 2020 | 1678 | 817 | 692 | 394 |
| 2021 | 2793 | 1359 | 1094 | 660 |
| Midwest (n = 22) | ||||
| 2020 | 4653 | 908 | 406 | 32 |
| 2021 | 5552 | 1275 | 571 | 67 |
| South (n = 38) | ||||
| 2020 | 4,823 | 1,554 | 923 | 455 |
| 2021 | 6758 | 2982 | 2073 | 1131 |
| West (n = 34) | ||||
| 2020 | 7140 | 2557 | 1248 | 107 |
| 2021 | 9780 | 3855 | 2020 | 267 |
Note: Table reports pooled visit counts across 107 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021, for overall visits, and for visits with prolonged LOS.
Abbreviations: LOS, length of stay; US, United States.
TABLE A7.
Characteristics of ED sites in the subset analysis with pre‐pandemic (2019) comparison data
| Site Characteristic | Value |
|---|---|
| States represented (n) | 16 |
| Visit volume (median, IQR) | 22,966 (12,404–35,257) |
| Census region (n) | |
| Northeast | 3 |
| Midwest | 10 |
| South | 6 |
| West | 14 |
| Urban–rural designation (n) | |
| Metro | 29 |
| Micro/rural | 4 |
| Percent pediatric visits (median, IQR) | 12.5 (9.4–16.7) |
| Total visits (n) | 2,849,775 |
| Total pediatric visits (n, %) | 320,739 (11.3) |
| Total pediatric mental health visits (N, %) | 21,012 (6.6) |
| Age for pediatric mental health visits (median, IQR) | 15 (13–16) |
Note: Of the 107 EDs in the analysis sample, 33 had continuous data reporting from January 2019 through December 2021. Characteristics of these 33 EDs are reported here.
Abbreviation: ED, emergency department; IQR, interquartile range.
TABLE A8.
Subset analysis of 33 EDs, pooled monthly visit counts, and incident rate ratios of all pediatric mental health visits
| 2019 | 2020 | IRR (95% CI) | 2021 | IRR (95% CI) | |
|---|---|---|---|---|---|
| January | 615 | 658 | 1.07 (0.96–1.19) | 523 | 0.85 (0.76–0.96) |
| February | 610 | 687 | 1.13 (1.01–1.26) | 534 | 0.88 (0.78–0.98) |
| March | 738 | 528 | 0.72 (0.64–0.80) | 638 | 0.86 (0.78–0.96) |
| April | 711 | 300 | 0.42 (0.37–0.48) | 642 | 0.90 (0.81–1.00) |
| May | 703 | 405 | 0.58 (0.51–0.65) | 649 | 0.92 (0.83–1.03) |
| June | 493 | 374 | 0.76 (0.66–0.87) | 507 | 1.03 (0.91–1.16) |
| July | 517 | 498 | 0.96 (0.85–1.09) | 405 | 0.78 (0.69–0.89) |
| August | 590 | 471 | 0.80 (0.71–0.90) | 463 | 0.78 (0.70–0.89) |
| September | 754 | 622 | 0.82 (0.74–0.92) | 716 | 0.95 (0.86–1.05) |
| October | 769 | 666 | 0.87 (0.78–0.96) | 605 | 0.79 (0.71–0.87) |
| November | 700 | 570 | 0.81 (0.73–0.91) | 657 | 0.94 (0.84–1.04) |
| December | 587 | 534 | 0.91 (0.81–1.02) | 560 | 0.95 (0.85–1.07) |
Note: Table reports pooled visit counts across 33 EDs in the Clinical Emergency Data Registry in 2020 and 2021. IRRs are reported against 2019 reference for the corresponding month. For example, the incident rate of pediatric mental health visits in February 2020 was 1.13 (687 visits) as compared to February 2019 (610 visits). CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A9.
Subset analysis of 33 EDs, pooled monthly visit counts and incident rate ratios, and pediatric mental health visits resulting in admit/transfer
| 2019 | 2020 | IRR (95% CI) | 2021 | IRR (95% CI) | |
|---|---|---|---|---|---|
| January | 95 | 129 | 1.36 (1.04–1.77) | 96 | 1.01 (0.76–1.34) |
| February | 117 | 125 | 1.07 (0.83–1.37) | 89 | 0.76 (0.58–1.00) |
| March | 154 | 96 | 0.62 (0.48–0.80) | 130 | 0.84 (0.67–1.07) |
| April | 157 | 75 | 0.48 (0.36–0.63) | 124 | 0.79 (0.62–1.00) |
| May | 103 | 82 | 0.80 (0.60–1.06) | 109 | 1.06 (0.81–1.39) |
| June | 73 | 61 | 0.84 (0.59–1.17) | 74 | 1.01 (0.73–1.40) |
| July | 89 | 100 | 1.12 (0.84–1.50) | 65 | 0.73 (0.53–1.01) |
| August | 120 | 94 | 0.78 (0.60–1.03) | 80 | 0.67 (0.50–0.88) |
| September | 152 | 132 | 0.87 (0.69–1.10) | 130 | 0.86 (0.68–1.08) |
| October | 149 | 119 | 0.80 (0.63–1.02) | 113 | 0.76 (0.59–0.97) |
| November | 136 | 115 | 0.85 (0.66–1.08) | 135 | 0.99 (0.78–1.26) |
| December | 101 | 90 | 0.89 (0.67–1.18) | 104 | 1.03 (0.78–1.35) |
Note: Table reports pooled pediatric mental health visit counts resulting in admit/transfer across 33 EDs in the Clinical Emergency Data Registry in 2020 and 2021. IRRs are reported against 2019 reference for the corresponding month. For example, the incident rate of pediatric mental health visits resulting in admit/transfer in February 2020 was 1.07 (125 visits) as compared to February 2019 (117 visits). CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A10.
Subset analysis of 33 EDs, pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting in length of stay >6 h
| 2019 | 2020 | IRR (95% CI) | 2021 | IRR (95% CI) | |
|---|---|---|---|---|---|
| January | 152 | 135 | 0.89 (0.71–1.12) | 155 | 1.02 (0.82–1.27) |
| February | 168 | 170 | 1.01 (0.82–1.25) | 168 | 1.00 (0.81–1.24) |
| March | 180 | 131 | 0.73 (0.58–0.91) | 181 | 1.01 (0.82–1.23) |
| April | 177 | 71 | 0.40 (0.31–0.53) | 193 | 1.09 (0.89–1.33) |
| May | 166 | 76 | 0.46 (0.35–0.60) | 200 | 1.20 (0.98–1.48) |
| June | 71 | 85 | 1.20 (0.88–1.63) | 160 | 2.25 (1.71–2.97) |
| July | 88 | 114 | 1.30 (0.99–1.70) | 115 | 1.31 (0.99–1.72) |
| August | 96 | 120 | 1.25 (0.96–1.63) | 131 | 1.36 (1.05–1.77) |
| September | 154 | 198 | 1.29 (1.04–1.58) | 242 | 1.57 (1.29–1.92) |
| October | 174 | 207 | 1.19 (0.97–1.45) | 182 | 1.05 (0.85–1.28) |
| November | 150 | 177 | 1.18 (0.95–1.46) | 221 | 1.47 (1.20–1.81) |
| December | 129 | 153 | 1.19 (0.94–1.49) | 184 | 1.43 (1.14–1.78) |
Note: Table reports pooled pediatric mental health visit counts resulting in length of stay >6 h across 33 EDs in the Clinical Emergency Data Registry in 2020 and 2021. IRRs are reported against 2019 reference for the corresponding month. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A11.
Subset analysis of 33 EDs, pooled monthly visit counts and incident rate ratios, and pediatric mental health visits resulting in length of stay >12 h
| 2019 | 2020 | IRR (95% CI) | 2021 | IRR (95% CI) | |
|---|---|---|---|---|---|
| January | 62 | 60 | 0.97 (0.68–1.38) | 74 | 1.19 (0.85–1.67) |
| February | 67 | 75 | 1.12 (0.81–1.56) | 89 | 1.33 (0.97–1.82) |
| March | 62 | 58 | 0.94 (0.93–0.94) | 90 | 1.45 (1.45–1.46) |
| April | 75 | 24 | 0.32 (0.20–0.51) | 111 | 1.48 (1.10–1.98) |
| May | 49 | 35 | 0.71 (0.46–1.10) | 95 | 1.94 (1.37–2.74) |
| June | 27 | 35 | 1.30 (0.78–2.14) | 61 | 2.26 (1.44–3.55) |
| July | 26 | 43 | 1.65 (1.02–2.69) | 51 | 1.96 (1.22–3.15) |
| August | 35 | 54 | 1.54 (1.01–2.36) | 65 | 1.86 (1.23–2.80) |
| September | 72 | 87 | 1.21 (1.20–1.21) | 126 | 1.75 (1.75–1.76) |
| October | 69 | 104 | 1.51 (1.50–1.51) | 102 | 1.48 (1.47–1.48) |
| November | 65 | 86 | 1.32 (1.32–1.33) | 99 | 1.52 (1.52–1.53) |
| December | 53 | 73 | 1.38 (0.97–1.96) | 84 | 1.58 (1.12–2.24) |
Note: Table reports pooled pediatric mental health visit counts resulting in length of stay >12 h across 33 EDs in the Clinical Emergency Data Registry in 2020 and 2021. IRRs are reported against 2019 reference for the corresponding month. CIs are adjusted for clustering within EDs.
Abbreviations: CI, confidence interval; EDs, emergency departments; IRR, incident rate ratio; LOS, length of stay.
TABLE A12.
Subset analysis of 33 EDs, pooled monthly visit counts and incident rate ratios, pediatric mental health visits resulting in length of stay >24 h
| 2019 | 2020 | 2021 | |
|---|---|---|---|
| January | 1 | 6 | 11 |
| February | 1 | 8 | 12 |
| March | 1 | 0 | 7 |
| April | 2 | 2 | 7 |
| May | 1 | 1 | 13 |
| June | 1 | 10 | 8 |
| July | 4 | 9 | 15 |
| August | 1 | 8 | 8 |
| September | 0 | 5 | 7 |
| October | 0 | 4 | 13 |
| November | 0 | 3 | 9 |
| December | 0 | 4 | 7 |
Note: Table reports pooled pediatric mental health visit counts resulting in length of stay >24 h across 33 emergency departments in the Clinical Emergency Data Registry in 2020 and 2021. Low counts in 2019 precluded stable point estimates for incident rate ratios by month.
Abbreviation: ED, emergency department.
Janke AT, Nash KA, Goyal P, Auerbach M, Venkatesh AK. Pediatric mental health visits with prolonged length of stay in community emergency departments during COVID‐19. JACEP Open. 2022;3:e12869. 10.1002/emp2.12869
Supervising Editor: Matthew Hansen, MD, MCR.
REFERENCES
- 1. Abramson A, Children's mental health is in crisis. In: American Psychological Association [Internet]. 1 Jan 2022 [cited 9 Aug 2022]. Available: https://www.apa.org/monitor/2022/01/special–childrens–mental–health
- 2. Radhakrishnan L, Leeb RT, Bitsko RH, et al. Pediatric emergency department visits associated with mental health conditions before and during the COVID–19 pandemic – United States, January 2019–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71:319‐324. [DOI] [PubMed] [Google Scholar]
- 3. Chadi N, Spinoso–Di Piano C, Osmanlliu E, Gravel J, Drouin O. Mental health–related emergency department visits in adolescents before and during the COVID–19 pandemic: a multicentric retrospective study. J Adolesc Health. 2021;69:847‐850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID–19. Pediatrics. 2021;147:e2020029280. doi: 10.1542/peds.2020-029280 [DOI] [PubMed] [Google Scholar]
- 5. Ibeziako P, Kaufman K, Scheer KN, Sideridis G. Pediatric mental health presentations and boarding: first year of the COVID–19 pandemic. Hosp Pediatr. 2022;12:751‐760. [DOI] [PubMed] [Google Scholar]
- 6. Nash KA, Zima BT, Rothenberg C, et al. Prolonged emergency department length of stay for US pediatric mental health visits (2005–2015). Pediatrics. 2021;147:e2020030692. doi: 10.1542/peds.2020-030692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pinals DA, Hepburn B, Parks J, Stephenson AH. The behavioral health system and its response to COVID–19: a snapshot perspective. Psychiatr Serv. 2020;71:1070‐1074. [DOI] [PubMed] [Google Scholar]
- 8. Leyenaar JK, Freyleue SD, Bordogna A, Wong C, Penwill N, Bode R. Frequency and duration of boarding for pediatric mental health conditions at acute care hospitals in the US. JAMA. 2021;326:2326‐2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Whitfill T, Auerbach M, Scherzer DJ, Shi J, Xiang H, Stanley RM. Emergency care for children in the united states: epidemiology and trends over time. J Emerg Med. 2018;55:423‐434. [DOI] [PubMed] [Google Scholar]
- 10. Clinical Emergency Department Registry. In: American College of Emergency Physicians [Internet]. [cited 2 Jul 2021]. Available: https://www.acep.org/cedr/
- 11. Biel MG, Tang MH, Zuckerman B. Pediatric mental health care must be family mental health care. JAMA Pediatr. 2020;174:519‐520. [DOI] [PubMed] [Google Scholar]
- 12. Wang X, Nonparametric Analysis of Covariance [R package fANCOVA version 0.6–1]. 2020. [cited 14 Nov 2022]. Available: https://CRAN.R–project.org/package=fANCOVA [Google Scholar]
- 13. Marshall R, Ribbers A, Sheridan D, Johnson KP. Mental health diagnoses and seasonal trends at a pediatric emergency department and hospital, 2015–2019. Hosp Pediatr. 2021;11:199‐206. [DOI] [PubMed] [Google Scholar]
- 14. Hillis SD, Blenkinsop A, Villaveces A, et al. COVID–19–associated orphanhood and caregiver death in the United States. Pediatrics. 2021;148(6):e2021053760. doi: 10.1542/peds.2021-053760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sheridan DC, Sheridan J, Johnson KP, et al. The effect of a dedicated psychiatric team to pediatric emergency mental health care. J Emerg Med. 2016;50:e121‐e128. [DOI] [PubMed] [Google Scholar]


