Abstract
Severe cases of COVID-19 often require orotracheal intubation (OTI) and mechanical ventilation, and post-intubation laryngeal injury (PI-LI) is one of the important complications of OTI. Some studies have claimed that the frequency of PI-LI may be higher in COVID-19 patients as compared with that in non-COVID-19 patients, because of the larger size of endotracheal tube used, the longer OTI time, use of prone positioning of the patients, etc. Herein, we describe six cases of PI-LI who presented with dyspnea after recovering from COVID-19. Five of the patients were male and the median OTI period was 9 days. All the patients showed abnormal endoscopic findings, including posterior glottic synechiae/stenosis or subglottic/posterior glottic granulomas. Four patients required surgical intervention, including tracheostomy, laryngomicrosurgery, or laterofixation of the vocal cord. Many post-COVID-19 patients experience persistent symptoms (post-COVID-19 syndrome), including dyspnea. Two of our patients with dyspnea had been treated by internists as cases of post-COVID-19 syndrome. Therefore, we wish to underscore the need for every healthcare professional to be aware of the possibility of PI-LI after OTI, especially during the ongoing COVID-19 pandemic. Otolaryngologists should undertake endoscopic assessment of the larynx in patients presenting with dyspnea after recovering from COVID-19.
Keywords: SARS-CoV-2, Laryngeal stenosis, Subglottic stenosis, Laryngeal granuloma, ACE2
Abbreviations: OTI, orotracheal intubation; PI-LI, post-intubation laryngeal injury; ETT, endotracheal tube
1. Introduction
Since December 2019, there has been an explosion of cases of COVID-19 caused by SARS-CoV-2 around the world. An estimated 4%-5% of cases with severe COVID-19 needed intubation and mechanical ventilatory support during the illness [1,2].
There have been numerous reports of laryngeal injury, including glottic erosions, edema, granulomas, vocal fold immobility, and posterior glottic or subglottic stenosis following orotracheal intubation (OTI) in COVID-19 patients [3], [4], [5], [6]. Some studies have concluded that the incidence of OTI-induced laryngeal and tracheal injuries is higher in COVID-19 patients that in patients with other diseases than COVID-19 (non-COVID-19 patients), because of the longer OTI period, larger sizes of endotracheal tubes (ETTs) used, prone positioning of the patients, etc. [3,7]. In this report, we describe six cases of post-intubation laryngeal injury (PI-LI) who presented with dyspnea after recovering from COVID-19.
2. Case Presentation
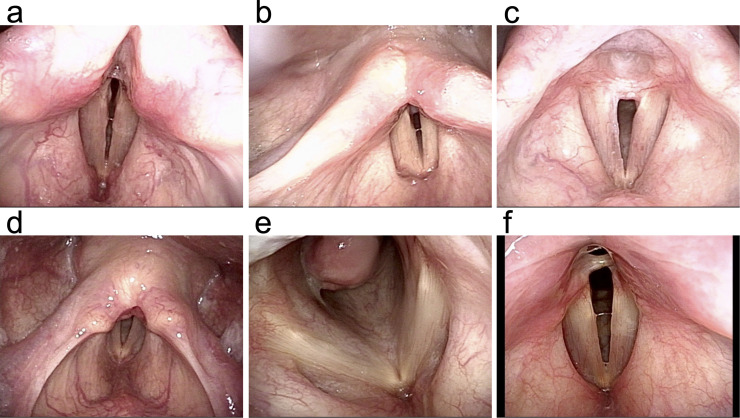
Five patients were male and one was female. The median interval from extubation to consultation at our department was 2 months. Four of the six patients had received treatment for COVID-19 in the emergency care unit of our hospital. All the patients presented with dyspnea. Two patients had dyspnea only on exertion, and were treated conservatively, while the remaining 4 patients required surgical intervention. The endoscopic findings and patient characteristics are summarized in Fig. 1 , supplementary Fig. 1 and Table 1 . The detailed medical histories of three representative cases are described below; those of the remaining 3 cases are described in the supplementary case presentation.
Fig. 1.
Endoscopic findings of the patients. (a) Case 1. Post-glottic stenosis. (b) Case 2. Subglottic granulation tissue and defective abduction of the vocal cords. (c) Case 3. Posterior glottic stenosis caused by vocal cord synechiae. (d) Case 4. Posterior glottic stenosis. (e) Case 5. Subglottic granuloma. (f) Case 6. Posterior glottic synechiae.
Table 1.
Characteristics of the patients.
| Case | Age | Sex | Comorbidities | Smoking | OTI time (day) | ETT size (mm) | Tracheostomy | Prone positioning | Viral variant | Time (month) | Symptoms | Endoscopic findings | Surgical intervention | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 51 | M | - | + | 11 | 8 | + | - | - | 8 | Wheezing, dyspnea | Posterior glottic stenosis | Tracheostomy, LMS, laterofixation | Tracheal-stoma close |
| 2 | 65 | F | HTN, DM | - | 16 | N.A. | + | - | - | 2 | Wheezing, dyspnea | Posterior glottic synechia/stenosis | Tracheostomy, TLM | Tracheal-stoma close |
| 3 | 75 | M | HTN, DM | - | 5 | 8.5 | +* | - | - | 5 | Wheezing, dyspnea | Posterior glottic stenosis, subglottic granuloma | Tracheostomy | Depending on tracheal stoma |
| 4 | 52 | M | HTN, DM | - | 14 | 8 | + | + | L452R | 2 | Dyspnea on exertion | Posterior glottic stenosis | - | Follow-up |
| 5 | 46 | M | HTN | - | 3 | 8 | - | - | N.A. | 1 | Wheezing, dyspnea | Subglottic granuloma | Tracheostomy, LMS | Tracheal-stoma close |
| 6 | 46 | M | DM | + | 7 | 8 | - | + | L452R | 0 (5 days) | Dyspnea on exertion | Posterior glottic granuloma, posterior glottic synechia/stenosis | - | Follow-up |
| Median | 51.5 | 9 | 2 |
DM, diabetes mellitus; HTN, hypertension; LMS, laryngomicrosurgery; N.A., not available; Time, interval from extubation to consultation at our department; TLM, transoral laser microsurgery
In case 3, the patient developed prolonged respiratory failure after extubation, yet re-intubation was difficult; therefore, we performed cricothyrotomy followed by tracheostomy.
2.1. Case 1
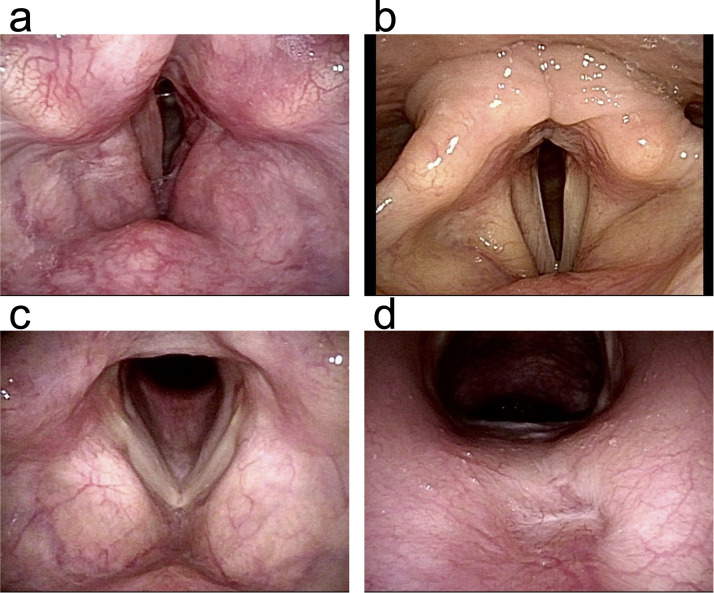
A 51-year-old man with COVID-19: Underwent tracheostomy after OTI for 11 days. Eight months after extubation, he presented to our outpatient clinic with wheezing and worsening of dyspnea, which had been treated during the previous 3 months as a manifestation of peripheral airway obstruction, but without any improvement. Endoscopy revealed posterior glottic stenosis and restricted opening of the glottis (Fig. 1a). Tracheotomy was performed, and in the subsequent surgery performed under general anesthesia, the adhesions were cut, which resulted in minimal improvement. Then, he underwent laterofixation of the left vocal cord (Fig. 2 a).
Fig. 2.
Post-surgical endoscopy. (a) Case 1. Laterofixation of the left vocal cord was performed to widen the airway. (b) Case 2. The posterior glottic synechiae were ablated with a CO2 laser. (c, d) Case 5. The subglottic granuloma was resected transorally. Views from above (c) and below (d) are shown. The base of the lesion was on the subglottic posterior wall.
2.2. Case 2
A 65-year-old woman with COVID-19: The patient underwent tracheostomy after 16 days of OTI. Two months after the extubation, she visited our hospital complaining of dyspnea and wheezing, and was diagnosed as having posterior glottic stenosis. Endoscopic examination revealed a thick posterior glottic web and restricted glottic abduction (Fig. 1b). After tracheotomy, the web was removed with CO2 laser under general anesthesia (Fig. 2b). Postoperatively, the airway diameter increased and the dyspnea disappeared, so that the tracheal stoma could be closed.
2.3. Case 5
A 46-year-old man with COVID-19: The patient underwent OTI for three days. One month after extubation, he began to experience wheezing and was treated as a case of asthma. Since one month of conservative treatment at an internal medicine clinic led to no improvement, the patient consulted an otolaryngologist and was diagnosed as having subglottic granuloma. Despite two months of treatment, the granuloma grew, with worsening of the dyspnea; therefore, the patient consulted our department. Endoscopy revealed subglottic granulomas filling the airway (Fig. 1e). Tracheostomy was performed, and laryngomicrosurgery was performed subsequently to resect the granuloma. The tracheal stoma was closed after confirming the absence of any evidence of granuloma regrowth (Fig. 2c, d).
3. Discussion
We report 6 cases of laryngeal injury caused by OTI performed for the treatment of COVID-19. All of the patients presented with dyspnea. All the four patients who needed surgical interventions had wheezing in addition to dyspnea. In our case series, especially in Case 1, although there was a risk of sacrificing the voice quality, we prioritized securing of the airway. The treatment strategy should be discussed well in advance with the patients in order to improve their quality of life.
It has been reported that post-intubation laryngeal and tracheal complications are more common in COVID-19 patients than in non-COVID-19 patients [3,7]. Laryngeal injuries long after intubation have been reported in 40% of COVID-19 and 11% of non-COVID-19 patients, and serious laryngeal injuries have also been found to be about twice as common in COVID-19 patients (6.3% vs. 2.9%) [3,8]. However, because of limited prospective studies, it remains unclear if COVID-19 is actually causally related to the increased incidence of laryngeal injury. In our cases reported herein, four of the six patients were treated for COVID-19 at our hospital and the remaining two had been treated at other hospitals. Until May 2022, 200 COVID-19 patients underwent OTI at our hospital, and 41 of these patients died during the treatment; thus, at least 2% (4/200) of all the intubated patients [2.5% (4/159) of the surviving cases] suffered from PI-LI with dyspnea according to current data. Retrospective/prospective comprehensive surveillance might reveal a higher incidence of PI-LI. The larger sizes of ETTs used and longer OTI times (i.e., delayed tracheostomy), which are reported as risk factors for PI-LI, are sometimes suggested as contributing to protecting the healthcare professionals engaged in COVID-19 treatment [9], [10], [11], [12]. Of our cases, 3 underwent tracheostomy during OTI, and the median OTI period was 14 [range: 11-16] days in these patients. On the other hand, early tracheostomy (within 7 days) is reportedly correlated with better overall outcomes [13]. Earlier tracheostomy may be suggested in COVID-19 patients as well, with the hope of decreasing the incidence of PI-LI, although it is also important to secure the safety of the treating healthcare professionals. Prone positioning in patients undergoing OTI has also been reported as a risk factor for laryngeal injury. We adopted prone positioning in two of our patients during the initial treatment for COVID-19. Although a small number of cases of PI-LI may be inevitable, every effort should be made to minimize the incidence. It is necessary to take every available opportunity to discuss with anesthesiologists and emergency physicians about the methods of OTI to prevent PI-LI.
Another possible risk factor specific to COVID-19 is pre-existing laryngitis; SARS-CoV-2 enters human cells via angiotensin-converting enzyme 2 (ACE2) receptors, which are expressed in vascular endothelial cells, renal tubular cells, alveolar epithelial cells, etc. [14]. In the head and neck region, ACE2 receptors have been reported to be expressed in the epithelial cells, particularly in the nasal and oral mucosa, laryngeal glottic area, including the vocal cords, and salivary glands [14]. Pre-existing laryngeal inflammation might increase the risk of PI-LI.
Comorbidities that serve as risk factors for PI-LI include type 2 diabetes mellitus, obesity, hypertension, cardiovascular disease, and smoking, which likely impair the wound healing ability of mucosa damaged by ETTs [4]. At the same time, these factors are also associated with increased severity of COVID-19, which is associated with a higher likelihood of intubation and subsequent PI-LI. All of our patients had at least one of these risk factors.
Persistent symptoms after COVID-19 (post-COVID-19 syndrome) might cause PI-LI to be overlooked. Many patients experience various symptoms after recovery from acute COVID-19. The major reported symptoms are fatigue, sleep disorder, dyspnea, and cough [15]. In our series, two patients with dyspnea were treated as cases of post-COVID-19 syndrome by internists. Patients presenting with dyspnea after recovering from COVID-19 should be evaluated by otorhinolaryngologists. Every effort needs to be made to inform healthcare professionals about the possible development of laryngeal injury after OTI, especially during this COVID-19 pandemic.
4. Conclusion
We report six cases of PI-LI who presented with dyspnea. The COVID-19 pandemic has increased the need for OTI, and every healthcare professional should be aware of possible laryngeal injury after OTI. Otolaryngologists should perform endoscopic evaluation of the larynx when encountering previously intubated patients presenting with complaints pertaining to the airways or voice.
Disclosure statement
The authors have no conflict of interest to declare in relation to submission of this article.
Ethical Statement
This manuscript was written in accordance with the Code of Ethics of the World Medical Association (Helsinki Declaration). We confirmed a patient's anonymity. We have obtained informed consent from the participant presented in the study.
This material has not been published in completely or in part elsewhere.
The authors declare that they have no conflict of interest or financial disclosures.
Footnotes
Disclosure of Potential Conflicts of Interest: No potential conflicts of interest were disclosed.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.anl.2022.12.007.
Appendix. Supplementary materials
References
- 1.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Félix L, Tavares TL, Almeida VPB, Tiago RSL. Incidence of Laryngotracheal Lesions After Orotracheal Intubation in Coronavirus Disease Patients. Laryngoscope. 2022;132:1075–1081. doi: 10.1002/lary.29862. [DOI] [PubMed] [Google Scholar]
- 4.Naunheim MR, Zhou AS, Puka E, Franco RA, Jr., Carroll TL, Teng SE, et al. Laryngeal complications of COVID-19. Laryngoscope Investig Otolaryngol. 2020;5:1117–1124. doi: 10.1002/lio2.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neevel AJ, Smith JD, Morrison RJ, Hogikyan ND, Kupfer RA, Stein AP. Postacute COVID-19 Laryngeal Injury and Dysfunction. OTO Open. 2021;5 doi: 10.1177/2473974X211041040. 2473974x211041040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watson NA, Karagama Y, Burnay V, Boztepe S, Warner S, Chevretton EB. Effects of coronavirus disease-2019 on voice: our experience of laryngeal complications following mechanical ventilation in severe coronavirus disease-2019 pneumonitis and review of current literature. Curr Opin Otolaryngol Head Neck Surg. 2021;29:437–444. doi: 10.1097/MOO.0000000000000768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fiacchini G, Tricò D, Ribechini A, Forfori F, Brogi E, Lucchi M, et al. Evaluation of the Incidence and Potential Mechanisms of Tracheal Complications in Patients With COVID-19. JAMA Otolaryngol Head Neck Surg. 2021;147:70–76. doi: 10.1001/jamaoto.2020.4148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esteller-Moré E, Ibañez J, Matiñó E, Ademà JM, Nolla M, Quer IM. Prognostic factors in laryngotracheal injury following intubation and/or tracheotomy in ICU patients. Eur Arch Otorhinolaryngol. 2005;262:880–883. doi: 10.1007/s00405-005-0929-y. [DOI] [PubMed] [Google Scholar]
- 9.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020;75:785–799. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishio N, Hiramatsu M, Goto Y, Shindo Y, Yamamoto T, Jingushi N, et al. Surgical strategy and optimal timing of tracheostomy in patients with COVID-19: Early experiences in Japan. Auris Nasus Larynx. 2021;48:518–524. doi: 10.1016/j.anl.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020;277:2173–2184. doi: 10.1007/s00405-020-05993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275:679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 14.Descamps G, Verset L, Trelcat A, Hopkins C, Lechien JR, Journe F, et al. ACE2 Protein Landscape in the Head and Neck Region: The Conundrum of SARS-CoV-2 Infection. Biology (Basel) 2020;9 doi: 10.3390/biology9080235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114:428–442. doi: 10.1177/01410768211032850. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.