Abstract
Background
Cryptococcal meningoencephalitis (CM), is a highly fatal fungal infection of the central nervous system (CNS), affecting not only immunocompromised patients, but also apparently immunocompetent patients. CM is mainly caused by Cryptococcus neoformans (C. neoformans), while viral hepatitis B (HBV) tends to be a rare inducement. According to the literature, the most common cerebral area affected by CM was frontal lobe, while infratentorial lesions were rare, especially those complicated with cerebellar infarction.
Methods
This study capitally analyzed the clinical data of an elderly female suffering from infratentorial CM complicated with cerebellar infarction, with a history of chronic HBV.
Results
The patient suffered from the symptoms of dizziness, insanity, low-grade fever, and high cranial pressure throughout the course of the disease. Her MRI findings were hydrocephalus and infratentorial lesions, including bilateral cerebellums and meningeal enhancement. The pathogene was Cryptococcus revealed by both the cytology and ink stain of cerebrospinal fluid, and was confirmed to be C. neoformans by the Next generation sequencing (NGS). After 12 days of intravenous amphotericin B (AMB) treatment, the patient developed oliguria, and 3 days after the termination of AMB treatment, the renal function recovered. Brain MRI reexamination after the treatment showed that the diffused lesions in the cerebellum were significantly decreased, and acute infarction occurred on the left cerebellum although it was asymptomatic. The patient took fluconazole 400mg per day after discharge, without complaints during the follow-up two months later.
Conclusion
C. neoformans infection may be a possible pathogeny in chronic HBV patients with meningoencephalitis. Cerebellar infarction might be a complication of CM, therefore MRI is supposed to be re-examined during antifungal therapy. Additionally, monitoring renal function plays a vital role after AMB treatment, and renal function may recover after termination.
Keywords: Cryptococcus meningoencephalitis, Cryptococcus neoformans, Cerebral infarction, Infratentorial meningitis
Cryptococcus meningoencephalitis; Cryptococcus neoformans; Cerebral infarction; Infratentorial meningitis.
1. Introduction
Cryptococcal meningoencephalitis (CM) is a highly fatal fungal infection of the central nervous system (CNS), affecting not only immunocompromised patients, but also apparently immunocompetent patients. CM is mainly caused by Cryptococcus neoformans (C. neoformans), while viral hepatitis B (HBV) tends to be a rare inducement. According to the published literature, the most common cerebral area affected by CM was the frontal lobe [1], and infratentorial lesions were rare, especially cerebellar infarction. Herein, we reported an elderly female with a history of chronic HBV suffering from infratentorial CM complicated with cerebellar infarction.
2. Case presentation
A 83-year-old female suffered from intermittent dizziness with nausea and vomiting for 5 days, and insanity for 1 day, showing dysphoria, reticent, apastia and reduced motion. She had a previous history of chronic HBV and hyperthyroidism, but denied being infected with human immunodeficiency virus (HIV). Her admission vital signs (day-0) were normal, including temperature, blood pressure, heart rate, respiratory rate and oxygen saturation. Physical examinations were also performed on circulatory system, respiratory system and abdomen. She was confused and unable to comply with most of the neurological examination. However, her pupil light reflex and corneal reflex were confirmed normal. Spontaneous activity, normal muscular tone and tendon reflex were found on each of her limbs. The Babinski sign on both sides was negative without neck stiffness. Hematological analysis was presented in Table 1. Both magnetic resonance imaging (MRI) and enhanced MRI of her brain were shown in Figure 1. To further investigate the pathogeny, lumbar puncture (day-1) was performed with cerebral spinal fluid (CSF) pressure of 260 mmH2O. CSF tests were listed in Table 2 and Figure 2. C. neoformans appeared in the cultured CSF. Antifungal susceptibility testing revealed that the fungi was sensitive to amphotericin B (AMB), flucytosine (FC), fluconazole (FCZ), itraconazole and voriconazole. On day-3 after receipt of the CSF results, the patient started the treatment of intravenous AMB 5mg on the first day, with a successive increase of 5 more milligrams per day to reach her maintenance dose of 35 mg (0.7 mg/kg/d), combined with 5FC (100 mg/kg/d, orally in four divided doses). Additionally, she also received intravenous mannitol to reduce intracranial pressure, nasal methimazole through a gastric tube to ameliorate thyroid function, nutritional therapy to maintain the balance of the internal environment, and several symptomatic treatments. On day-5, her insanity suddenly deteriorated, manifested as delirium, therefore she failed to coordinate with the treatment. Brain MRI reexamination was shown in Figure 3. Considering that hydrocephalus was more serious than before, emergent lateral ventriculopuncture drainage was performed and the measured intracranial pressure increased to 500 mmH2O. The patient became conscious on day-9 and her dizziness was gradually relieved on day-12. Until the intracranial pressure measured by dynamic monitoring was lower than 150 mmH2O and lasted for 48 h, the ventricular drainage tube was removed on day-12. Renal function was monitored every two days, and intermittent low-grade fever occurred during the treatment. Unfortunately, her renal function got deteriorated presenting as oliguria on day-15, and returned to normal after the termination of AMB for three days. Her children refused to restart AMB even in the case of low dose and asked for discharge due to the great improvement of symptoms and the poor family economy. Before discharge, the brain MRI was shown in Figure 4, that is, the diffused lesions in the cerebellum were obviously decreased and acute infarction occurred on the left cerebellum. The patient took FCZ 400mg per day after discharge without complaints during the follow-up two months later.
Table 1.
The hematological analysis.
| Items | Results | |
|---|---|---|
| Blood routine | Leukocytes | 7.39 ∗ 10ˆ9/L |
| Neutrophil% | 83.3% ↑ | |
| Inflammatory indicators | Procalcitonin | 0.072 ng/ml |
| Interleukin-6 | 38.03 mg/L | |
| C-reactive protein | 23.98 mg/L | |
| Hepatic function | Alanine transaminase | 29 U/L |
| Total bilirubin | 11.7 umo/L | |
| Direct bilirubin | 6.5 umol/L | |
| Albumin | 36 g/L | |
| Renal function | Blood urea nitrogen | 74 umol/L |
| Creatinine | 3.2 mmol/L | |
| Electrolyte | K+ | 3.22 mmol/L↓ |
| Na+ | 140.9 mmol/L | |
| Cl− | 106 mmol/L | |
| Thyroid function | Free triiodothyronine | 2.99 pmol/L |
| Free tetraiodothyronine | 24.81 pmol/L↑ | |
| Thyrotropic hormone | 0.03 Uiu/ml↓ | |
| Tumor markers | Negative | |
| Antinuclear antibody | Negative | |
| Anti-neutrophil antibody | Negative | |
| HIV | Negative | |
| HBV-DNA | Below the lower limit line | |
∗The result of this item was normal if there was no↑ or ↓behind.
Figure 1.
(A, B, C, D) diffused lesions of cerebellum; (E) mild hydrocephalus; (F) severe stenosis of bilateral middle cerebral arteries; (G, H) T1-post gadolinium showed enhancement of the leptomeninges on bilateral cerebellums and the right temporal lobe.
Table 2.
The results of CSF test.
| Items | Results |
|---|---|
| Appearance | Colorless and transparent |
| Leukocytes | 8 ∗ 10ˆ6/L↑ |
| Neutrophil% | 81.5% |
| Lymphocyte% | 14.5% |
| Monocyte% | 3.5% |
| Red blood cell count | 0 |
| Pandy’s test | Negative |
| Glucose | 3.6 mmol/L |
| Protein | 0.36 g/L |
| Chloride | 125.2 mmol/L |
| Lactic acid | 2.7 mmol/L |
| Lactic dehydrogenase | 4 U/L |
∗The result of this item was normal if there was no↑or↓behind.
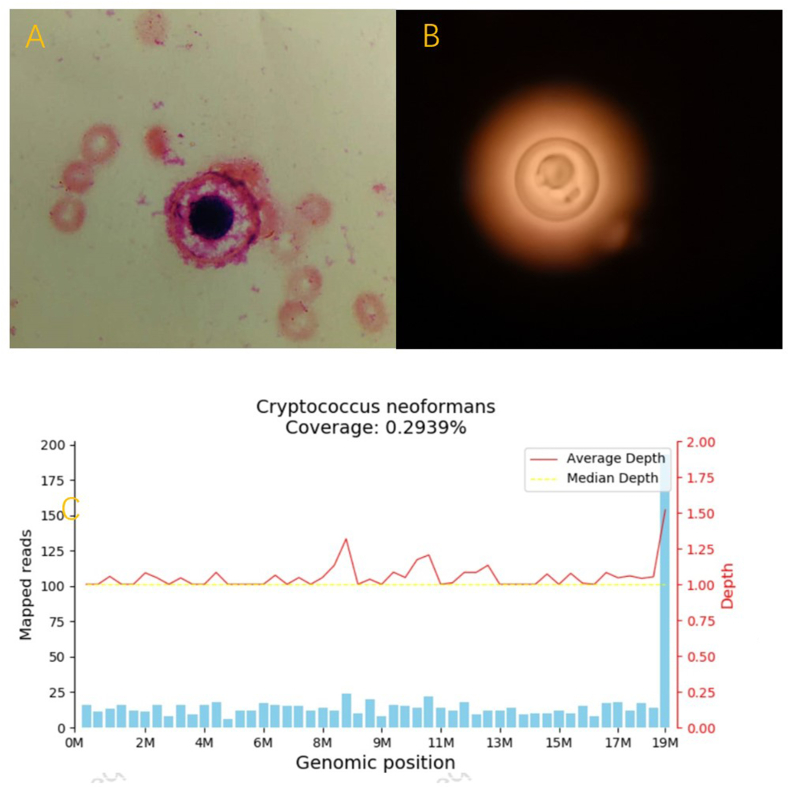
Figure 2.
(A) Both the cytology and (B) ink stain of CSF revealed Cryptococcus; (C) The Next Generation Sequencing (NGS) confirmed the infection Cryptococcus neoformans.
Figure 3.
(A, B, C, D, E) the size of lesions did not change too much compared to the previous MRI; (F) hydrocephalus was severer than before.
Figure 4.
Diffused lesions of cerebellum decreased obviously, while B, F and G showed acute cerebellum infarction.
3. Discussion
The well-known immunosuppressive factors of CM is HIV, solid organ transplantation, or after the treatment with corticosteroids [2]. Some studies also found an association between CM and viral hepatitis, especially HBV [1]. HBV infection may lead to a slew of host defense defects, including impaired cell-mediated immunity, phagocytic dysfunction, decreased antibodies and immunoglobulin concentrations, and complement deficiency. In addition, the alteration of neuroendocrine-immune system response in chronic viral hepatitis may also account for the propensity of Cryptococcus to infect the nervous system and increase the burden of fungi [3]. Therefore, the HBV history may be the potential risk of Cryptococcus infection. In terms of hyperthyroidism that the patient suffering from, there exists the relationship between CM and thyroid dysfunction in only one literature, with the pathogeny of cryptococcal thyroiditis [4]. Unfortunately, although thyroid nodules in our patient were detected by ultrasound, no further pathological examination was performed. Therefore, we have no idea whether her hyperthyroidism was associated with CM.
CM patients usually present with headache, fever, malaise, and altered mental status within several weeks. Clinical manifestations may include meningism, papilledema, cranial nerve palsies, and depressed level of consciousness [5]. According to the analysis of MRI examination results in 110 CM patients, including local lesions (24.5%), multi-site lesions (30%), abnormal meningeal enhancement (12.7%) and hydrocephalus (12.7%) and no lesions (17.3%), the most common cerebral area affected by CM was frontal lobe among different combination of these MRI features [1]. Notably, our patient manifested with dizziness, nausea and vomiting, which were not clinically common. Additionally, the lesions on MRI were located in the infratentorial regions, including bilateral cerebellums and meningeal enhancement, making the patient special from others. Interestingly, the patient suffered from asymptomatic cerebellar infarction during the treatment, while the most common infarction associated with C. neoformans was lacunar infarction primarily located in the basal ganglia [6]. We found severe stenosis of bilateral middle cerebral arteries on magnetic resonance angiography (MRA), which was arteriosclerosis, not stenosis in posterior circulation. Apart from age, there was no common risk factors for cerebral vascular disease in the patient. Why she suffered from cerebral infarction? Generally, C. neoformans tends to hematogenously spread to the brain along the surface blood, thereby inducing meningitis. When fungi reach the perivascular space through the arteries, they begin to invade the perivascular space toward the deeper parts of the brain, and there is a cerebral infarction similar to lacunar infarct as the same time [7]. Histopathologic examination and autopsy of a case suffered from cerebellar infarction with CM provided a possible mechanism. Fungi were mainly distributed in the subarachnoid space and rarely in the parenchyma, which made the arachnoid, subarachnoid spaces and pia presented seriously fibrotic. Arterioles were occluded with internal endothelial proliferation. Autopsy confirmed that the pathological alterations were predominantly localized at the surface of cerebellar hemisphere [8]. C. neoformans may directly invade the arterial walls, leading to arteritis and accelerate atherosclerosis by inducing cytokines [9]. However, whether her vascular damage was related to C. neoformans remained unclear since she has never been examined by MRA before.
According to the sequential therapeutic stages of CM antifungal treatment, including induction, consolidation, and maintenance phases, the patient was administrated a course of AMB with 5FC followed by FCZ as consolidation and maintenances, which is considered as the benchmark in antifungal therapy for CM [10]. However, AMB is associated with renal impairment, especially in the second week of induction therapy [11]. Our patient developed oliguria 12 days after intravenous AMB and her renal function recovered after the termination of AMB. Liposomal amphotericin B (L-AMB) is as effective as AMB, with favorable tolerance [12]. Unfortunately, her sons refused L-AMB because of its high price. Anyhow, our patient was clinically cured at least two months after the onset of the disease.
4. Conclusions
Cryptococcus neoformans infection may be a possible pathogeny in chronic HBV patients with meningoencephalitis. Cerebellar infarction might be a complication of CM, therefore MRI is supposed to be re-examined during antifungal therapy. Additionally, monitoring renal function plays a vital role after AMB treatment, and renal function may recover after termination.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Li Y., Zou M., Lu B., et al. Microbiological, epidemiological, and clinical characteristics of patients with Cryptococcal meningitis at a tertiary hospital in China: a 6-year retrospective analysis. Front. Microbiol. 2020;11:1837. doi: 10.3389/fmicb.2020.01837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pyrgos V., Seitz A.E., Williamson P.R., et al. Epidemiology of cryptococcal meningitis in the US: 1997-2009. PLoS One. 2013;8(2) doi: 10.1371/journal.pone.0056269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhong Y.H., Zhong X.F., Peng F.H., et al. Comparisons of presentations and outcomes of cryptococcal meningitis between patients with and without hepatitis B virus infection. Int. J. Infect. Dis. 2014;20:31–36. doi: 10.1016/j.ijid.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Avram A.M., Sturm C.A., Sisson J.C., et al. Cryptococcal thyroiditis and hyperthyroidism. Thyroid. 2004;14(6):471–474. doi: 10.1089/105072504323150822. [DOI] [PubMed] [Google Scholar]
- 5.Freitas I., Salazar T., Rodrigues P., et al. An uncommon presentation of Cryptococcal meningoencephalitis. Cureus. 2022;14(2) doi: 10.7759/cureus.21984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarkis R.A., Mays M., Isada C., et al. MRI findings in cryptococcal meningitis of the non-HIV population. Neurol. 2015;19(2):40–45. doi: 10.1097/NRL.0000000000000000. [DOI] [PubMed] [Google Scholar]
- 7.Fugate J.E., Lyons J.L., Thakur K.T., et al. Infectious causes of stroke. Lancet Infect. Dis. 2014;14(9):869–880. doi: 10.1016/S1473-3099(14)70755-8. [DOI] [PubMed] [Google Scholar]
- 8.Shimoda Y., Ohtomo S., Arai H., et al. Subarachnoid small vein occlusion due to inflammatory fibrosis-a possible mechanism for cerebellar infarction in cryptococcal meningoencephalitis: a case report. BMC Neurol. 2017;17(1):157. doi: 10.1186/s12883-017-0934-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mishra A.K., Arvind V.H., Muliyil D., et al. Cerebrovascular injury in cryptococcal meningitis. Int. J. Stroke. 2018;13(1):57–65. doi: 10.1177/1747493017706240. [DOI] [PubMed] [Google Scholar]
- 10.Williamson P.R., Jarvis J.N., Panackal A.A., et al. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat. Rev. Neurol. 2017;13(1):13–24. doi: 10.1038/nrneurol.2016.167. [DOI] [PubMed] [Google Scholar]
- 11.Bicanic T., Bottomley C., Loyse A., et al. Toxicity of amphotericin B deoxycholate-based induction therapy in patients with HIV-associated Cryptococcal meningitis. Antimicrob. Agents Chemother. 2015;59(12):7224–7231. doi: 10.1128/AAC.01698-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamill R.J., Sobel J.D., El-Sadr W., et al. Comparison of 2 doses of liposomal amphotericin B and conventional amphotericin B deoxycholate for treatment of AIDS-associated acute cryptococcal meningitis: a randomized, double-blind clinical trial of efficacy and safety. Clin. Infect. Dis. 2010;51(2):225–232. doi: 10.1086/653606. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.