Abstract
Introduction
Global Health Security borders on prevention, detection and response to public health threats like the novel coronavirus disease 2019 (COVID-19). Global Health Security Index (GHSI) of 2019 and 2021 revealed the world remains ill-prepared to deal with future pandemics, evident in the historic impact of COVID-19 on countries. As at 7th December 2022, COVID-19 has infected over 600 million people and claimed over six million lives, mostly in countries with higher GHSI scores.
Objective
Determine whether the GHSI scores of countries have a correlation with COVID-19 cases, deaths and vaccination coverage, while adjusting for country level dynamics.
Methods
This paper utilizes GHSI database of 195 countries. Data consists of 171 questions grouped into 37 indicators across six overarching categories on health security and COVID-19. Multivariate multiple regression analysis with robust standard errors was conducted to test the hypothesis that high GHSI ratings do not guarantee better COVID-19 outcomes like cases, deaths and vaccination coverage. Also, avplots STATA command was used to check outliers with potential negative effect on outcome and predictor variables.
Results
Global average GHSI score for all 195 countries was 38.9. United States of America recorded the highest GHSI score of 75.9 but also recorded one of the highest COVID-19 cases and deaths; Somalia recorded the worst GHSI score of 16.0 and one of the lowest COVID-19 cases and deaths. High GHSI scores did not associate positively with reduction in COVID-19 cases (Coef=157133.4, p-value=0.009, [95%CI 39728.64 274538.15]) and deaths (Coef=1405.804, p-value=0.047, [95%CI 18.1 2793.508]). However, high GHSI ratings associated with increases in persons fully vaccinated per 100 population (Coef=0.572, p-value=0.000, [95%CI.272.873]).
Conclusion
It appears the world might still not be adequately prepared for the next major pandemic, if the narrative remains unchanged. Countries that recorded higher GHSI scores, counter-intuitively, recorded higher COVID-19 cases and deaths. Countries need to invest more in interventions towards attaining Universal Health Coverage (UHC) including integrated health systems and formidable primary health care to enhance preparedness and response to pandemics.
Keywords: COVID-19, Global Health Security Index, Universal Health Coverage, Primary Health Care, Pandemics, Preparedness, Health systems
Introduction
Universal health coverage (UHC) is defined by the World Health Organization (WHO) as all individuals and communities receiving health services that they need without suffering financial hardship [1]. According to the WHO, UHC includes the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course. Additionally, health workforce must have optimal skills-mix in health care facilities to achieve UHC [1]. Attaining UHC however remains elusive if Global Health Security (GHS) is challenged and countries are not pandemic ready. In effect, GHS can be said to be a panacea to attaining UHC and vice-versa because precarious GHS situation endangers efforts towards attainment of UHC, particularly in already fragile health systems. On the other hand, countries need to have robust structures for UHC so they can attain and consolidate GHS gains. UHC emphasises on access to comprehensive, appropriate, timely, and quality health services, without financial burden [2]. GHS on the other hand is centered on preventing, detecting, and responding to public health threats, particularly by protecting people and societies worldwide from infectious disease threats [3]. Erondu et al. [4] however argued that GHS guides development for the core capacities of public health but quick to add that GHS in isolation does not address primary health-care (PHC) functions such as curative services, patient management and capacity for clinical surges.
GHS and UHC are therefore complimentary concepts for resilient health systems and must be effectively managed in a balanced manner. Erondu et al. [4] and Wenham et al. [2] observed that although UHC has the capacity to empower Primary Health Care (PHC) systems and improve access to health care services, there is a propensity for mainstream UHC interventions to relegate infectious disease threats to the background in favour of health insurance and individual health services, thus compromising GHS gains in health systems.
Outbreak of the novel coronavirus disease 2019 (COVID-19) has taught the world a critical lesson of prioritizing harmonized health systems over fragmented systems that do not integrate GHS and UHC interventions within countries. For instance, albeit the United States of America (USA) is among the top-rated countries in pandemic preparedness in the 2019 and 2021 Global Health Security Index (GHSI) ratings [5], the country also ironically recorded one of the world’s highest numbers of COVID-19 cases and deaths [6], [7], [8]. This scenario demonstrates the importance of aligning health priorities in a wholistic manner through an oriented PHC system that is fully integrated with the pillars of UHC and health security in countries. This agenda can be achieved via multisectoral policy and action, and empowerment of people and communities for health [9].
Total of 195 countries participated in the 2019 and 2021 Global Health Security Index (GHSI) assessments based on six (6) benchmarked parameters namely: prevention, detection and reporting, rapid response, health system, norms and risk environment [5]. It emerged from these global assessments that the world remains dangerously unprepared to deal with future epidemic and pandemic threats. Particularly, the latest 2021 GHSI data shows a global average score of 38.9% for the 195 countries captured [5]. According to the 2021 GHSI report, none of the 195 countries placed in the top tier of the ranking. This performance signals that significant gaps exist for all countries and across all six (6) GHSI categories of assessment on global health security [5].
Since the WHO declared COVID-19 in March 2020 as a pandemic of public health concern, the virus has infected over 600 million people and claimed more than six million lives across the globe as at December, 2022 [8]. In terms of the vaccination coverage, the WHO reports that over 12 billion vaccines have so far been administered worldwide [8]; out of this number, more than66% have received at least one dose of the vaccine and approximately 8.79 billion doses are administered each day. Unfortunately, barely 17.8% of people in developing countries have received at least one dose of the vaccine [10] due to varied reasons [11], [12].
Within the WHO African region, for instance, an estimated 11.7 million cases of COVID-19 have been recorded with over 200,000 deaths as at August, 2022. Moreover, 818 million doses of the COVID-19 vaccine have been received out of which 71.4% doses have been utilized and 583.7 million doses administered to target populations, representing a fully vaccinated coverage of 17.4% [13]. Although the number of infected persons in Africa has been relatively low, the impact of COVID-19 on economies remains phenomenal, especially, in countries with already fragile economies and weaker health systems.
Available literature shows countries responded differently to the COVID-19 pandemic largely based on the existing structure of their health systems. In some cases, COVID-19 reversed gains made in UHC and public health interventions at the PHC level. Even though literature abounds on the effect of COVID-19 on health systems across the globe, there is still dearth of empirical evidence on the correlation between health security performance scores of countries and their response to COVID-19 in terms of record of case counts, deaths and vaccination coverage.
Current outlook on the GHSI performance is worrying and also begs the critical question of whether humanity is ready for a future pandemic like COVID-19 or one that is worst. Would the world’s response to COVID-19 be better if the GHSI scores were better? These questions and more informed this scientific paper. The paper analysed the latest 2021 GHSI data on 195 countries vis-à-vis the case count of COVID-19, deaths and vaccination coverage in these pertinent countries. Authors sought to test the hypothesis that high GHSI scores of countries have no significant correlation with better COVID-19 response outcomes in terms of cases, deaths and vaccination coverage.
Methods
Study design
This an empirical descriptive correlation population-based study. The paper was written based on analysed secondary data on global health security and COVID-19 outcome measures. Data was accessed from the 2021 GHSI database which is publicly available at https://www.ghsindex.org/report-model/.
Data territorial coverage
Secondary data coverage was 195 countries/territories across the globe. In terms of the regional coverage, data was accessed from countries in Africa (n = 54), Central Asia (n = 5), Eastern Asia (n = 5), Europe (n = 43), Latin America/Caribbean (n = 33), Northern America (n = 2), Oceania (n = 16), South-eastern Asia (n = 11), Southern Asia (n = 9) and Western Asia (n = 17). The population size coverage ranged from countries with less than 1 million population (n = 34) to 1–10 million (n = 81), 10–50 million (n = 600) and over 100 million (n = 13). Data on countries distribution by income levels included low-income countries (LICs) (n = 34), lower middle-income countries (LMICs) (n = 45), upper middle income (UMICs) (n = 56) and higher income countries (IHCs) (n = 60) (see Supplementary File 1).
Eligibility and exclusion criteria
Major criteria for inclusion in the data curation was all 195 countries captured in terms of completeness of data on COVID-19 cases, deaths and vaccination coverage as at 2021 and the Global Health Security Index (GHSI) scores for 2019 and 2021. Countries that did not meet these criteria were dropped from the final analysis.
GHSI methodology
GHSI data was first published in October 2019 among 195 countries across the globe [14]. These countries composed of the States Parties to the International Health Regulations [15]. GHSI is an initiative of the Nuclear Threat Initiative (NTI) and the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health, with Economist Impact. The index was based on existing knowledge and understanding on individual countries preparedness to prevent, detect, and respond to infectious disease threats. GHSI is also based on research on the 195 countries from August, 2020 through June, 2021. Data was collected through qualitative and quantitative approaches based on publicly available country level information. Details are reported in the GHSI Methodology Report [14].
GHSI Indicators
GHSI indicators are benchmarked against external factors with a potential influence on global health security. The benchmarked factors include gross domestic product (GDP) per capita, and the United Nations Development Programme’s (UNDP) Human Development Index [14]. GHSI indicators are embedded in an interactive model publicly available as an Excel workbook at www.GHSIndex.org.
Six (6) category of indicators used to measure GHSI scores are: prevention (Prevention of the emergence or release of pathogens); detection and reporting (Early detection and reporting for epidemics of potential international concern); rapid response (Rapid response to and mitigation of the spread of an epidemic); health system (Sufficient and robust health system to treat the sick and protect health workers); compliance with international norms (Commitments to improving national capacity, financing plans to address gaps, and adhering to global norms); risk environment (Overall risk environment and country vulnerability to biological threats) [14] (see Supplementary File 2).
GHSI tools and scoring criteria
GHSI consists of 171 questions grouped into 37 indicators across six (6) overarching categories, stated supra. Overall score (0−100) for each country is a weighted sum of the six categories; each category is scored on a scale of 0–100, where 100 represents the most desired health security conditions and 0 represents the least desired health security conditions. A score of 100 does not however indicate that a country has perfect national health security conditions; likewise, a score of 0 does not mean a country has no capacity. Instead, the scores of 100 and 0 represent the highest or lowest possible score, respectively, as measured by the GHSI criteria [14]. Each category is normalized based on the sum of its underlying indicators and sub-indicators, and an identical weight is then applied. Default weights used in the ranking are based on neutral (or identical) weights which are dynamic and can be adapted by users [14].
Ethical considerations
Secondary data was mainly used for the analysis and there was not contact with human subjects. As reported in the GHSI Methodology Report [14], all ethical considerations were met during the primary data collection processes by Global Health Security Index Team. Moreover, request for permission to use the secondary data was granted by the Global Health Security Index Team (see Supplementary File 3).
Data analysis
Data was accessed from the GHSI online data repository (https://www.ghsindex.org/report-model/) after receiving written permission to use the data. Some variable names and codes were however recoded, re-labeled and merged with corresponding secondary on COVID-19 outcome measures (i.e. cases, deaths and vaccination coverage) per country. Excel data was later exported to STATA statistical analysis software (version 12.0) (StataCorp, College Station, TX, USA) for further analysis. Background information on the data set was analysed descriptively highlighting the means, standard deviations for continuous variables, and frequencies and percentages for the categorical variables.
Multivariate multiple regression analysis with robust standard errors was employed to test the main hypothesis that GHSI performance of countries has no significant association with better COVID-19 outcome measures (i.e., COVID-19 case counts, deaths and vaccination coverage), holding covariates constant. All statistical tests were conducted at 95% confidence level.
Outcome variables of interest
Main outcome variables of interest were: Cumulative COVID-19 cases (numeric); Cumulative COVID-19 deaths (numeric); Persons fully vaccinated (numeric); Persons fully vaccinated per 100 population (numeric).
Predictor variables of interest
Predictor variables were cumulative GHSI score for 2021 (numeric) and change in GHSI score between 2019 and 2021 (proxy for progress made) (numeric).
Co-variates controlled
Covariates controlled for in the regression models were: WHO regions/territories (categorical), population estimates of country (categorical), and income levels of country (categorical).
Multicollinearity diagnostics were conducted on the predictor variables and co-variates through pairwise correlation test and a post-estimation test for variance inflation factors (VIFs). It was observed all variables were below the 10.0 rule thumb for exclusion as collinear predictor variables. The average VIF was 2.20. Additionally, to check for outliers we used the post-estimation avplots STATA command (added-variable plots) to check extreme values that could have a negative effect on our outcome and predictor estimators. It was found that all data points were in range and no outliers observed (see Fig. 1, Fig. 2).
Fig. 1.
Correlation between COVID-19 cumulative case count and deaths and predicter variables,
Source: Global Health Security Index Database (2021).
Fig. 2.
Correlation between cumulative vaccination coverage per 100 population and predicter variables,
Source: Global Health Security Index Database (2021).
Findings
Background information
Analysis of the secondary data show that most (28%) of the countries captured in the GHSI data were African countries, followed by Europe (22%) and Latin America/Caribbean (17%). Barely 1% of the countries were in the Northern American region. In terms of the population coverage, 42% of the countries were within the population range of 1–10million and 7% had a population of 100million+ ; most of the countries were classified as high-income countries with 17% classified as low-income countries. Table 1, Table 2 show details of the background information on the 195 countries from the GHSI data.
Table 1.
Background information.
| Indicators | Obs. | GHSI_2021 (Mean (SD) | GHSI_2019 (Mean (SD) |
Total COVID-19 cases | Total COVID-19 deaths |
|---|---|---|---|---|---|
| Region | |||||
| Africa | 54 | 29.1 (5.8) | 29.4 (6.2) | 11,239,867 | 253,772 |
| Central Asia | 5 | 37.7 (7.0) | 37.7 (6.3) | 1854,147 | 23,771 |
| Eastern Asia | 5 | 46.1 (19.4) | 46.7 (18.2) | 32,556,922 | 88,075 |
| Europe | 43 | 52.4 (10.1) | 52.4 (11.0) | 189,506,543 | 1713,031 |
| Latin America/Caribbean | 33 | 37.7 (10.3) | 37.4 (9.7) | 72,649,195 | 1735,725 |
| Northern America | 2 | 72.9 (4.3) | 71.9 (6.1) | 89,571,299 | 1046,388 |
| Oceania | 16 | 29.7 (14.9) | 28.6 (14.8) | 10,604,984 | 50,117 |
| South-eastern Asia | 11 | 45.1 (12.2) | 43.0 (13.0) | 33,973,191 | 392,082 |
| Southern Asia | 9 | 34.9 (4.4) | 35.3 (5.2) | 61,798,796 | 742,375 |
| Western Asia | 17 | 39.2 (12.1) | 39.9 (11.3) | 32,976,613 | 258,716 |
| Population | |||||
| <million | 41 | 31.4 (7.7) | 30.2 (7.7) | 6178,203 | 49,474 |
| 1–10million | 81 | 42.7 (14.0) | 42.8 (14.1) | 213,378,853 | 1778,323 |
| 10–50million | 60 | 36.9 (14.0) | 37.4 (13.6) | 103,695,057 | 1209,163 |
| 100million+ | 13 | 47.8 (12.0) | 47.3 (11.8) | 213,479,444 | 3267,092 |
| Income levels | |||||
| Low income | 34 | 27.2 (6.1) | 28.0 (5.9) | 11,345,152 | 99,619 |
| Lower middle income | 45 | 33.7 (7.1) | 33.5 (7.3) | 82,240,410 | 1164,574 |
| Upper middle income | 56 | 37.3 (12.2) | 37.0 (12.0) | 135,567,092 | 2588,930 |
| High income | 60 | 50.9 (13.0) | 50.5 (13.6) | 307,578,903 | 2450,929 |
Source: Secondary Data of Global Health Security Index 2021
Table 2.
Variable definitions.
| Variables | Statistics | |
|---|---|---|
| Outcome variables | Mean | Std. Dev. |
| Cumulative COVID-19 cases (n = 191) | 2810112.9 | 8349878.2 |
| Cumulative COVID-19 deaths (n = 191) | 33005.508 | 105171.5 |
| Persons fully vaccinated (n = 190) | 24898579 | 1.152e+ 08 |
| Persons fully vaccinated per 100 (n = 190) | 51.439 | 26.932 |
| Explanatory variables | Mean | Std. Dev. |
| GHSI_2021 score (n = 195) | 38.908 | 13.642 |
| GHSI progress proxy* (n = 195) | 0.202 | 2.507 |
| Covariates | Freq. (f) | Percent (%) |
| WHO region | ||
| Africa | 54 | 27.69 |
| Central Asia | 5 | 2.56 |
| Eastern Asia | 5 | 2.56 |
| Europe | 43 | 22.05 |
| Latin America/Caribbean | 33 | 16.92 |
| Northern America | 2 | 1.03 |
| Oceania | 16 | 8.21 |
| South-eastern Asia | 11 | 5.64 |
| Southern Asia | 9 | 4.62 |
| Western Asia | 17 | 8.72 |
| Population | ||
| <million | 41 | 21.03 |
| 1–10million | 81 | 41.54 |
| 10–50million | 60 | 30.77 |
| 100million+ | 13 | 6.67 |
| Income levels | ||
| Low income | 34 | 17.44 |
| Lower middle income | 45 | 23.08 |
| Upper middle income | 56 | 28.72 |
| High income | 60 | 30.77 |
Source: Secondary Data of Global Health Security Index 2021
*Percentage change in 2021 and 2019 GHSI scores
GHSI and COVID-19 performance scores
Average 2021 GHSI score for all 195 countries was 38.9 out of the expected optimum score of 100. United States of America (USA) recorded the highest GHSI score of 75.9 while Somalia recorded the worst GHSI score of 16; on the average, the world witnessed a marginal positive change of 0.20 between 2019 and 2021 in health security. Some specific countries nonetheless recorded negative change or retrogression (see Supplementary File 1). Data on the GHSI and COVID-19 performance scores further show countries from the Northern American region recorded the highest GHSI score of 72.9 followed by European region (mean=46.1), South-eastern Asia (mean=45.1), Central Asia (mean=37.7) and Latin America/Caribbean (mean=37.7). The least GHSI score was recorded in the African region (mean=29.1). Countries with population of 100million+ also recorded the highest GHSI mean score of 47.8; the least GHSI mean score of 31.4 was recorded in countries with a population size less than one million. Countries that fell within low-income levels also recorded the lowest average GHSI score of 27.2 compared to countries within the high-income bracket recording an average of 50.9.
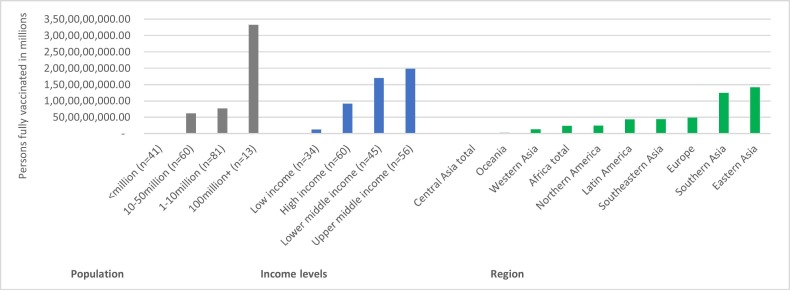
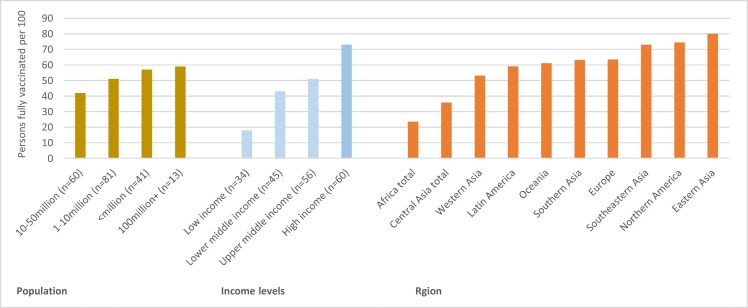
In terms of the COVID-19 performance measures, 35% of the global COVID-19 cases in 2021 were recorded in Europe while Central Asia region recorded barely 0.35% of the total global COVID-19 cases. Latin America/Caribbean region recorded 27.5% of the global COVID-19 cases followed by Europe (27.2%); the least morbidity cases were recorded in Central Asia (0.38%) and Oceania (0.79%). Countries with high population sizes also recorded high COVID-19 cases and deaths, and likewise HICs and UMICs (see Table 1). In respect of COVID-19 response, the proxy indicator of vaccination coverage shows countries with population of 100million+ ; countries within UMICs bracket and those in Eastern Asia recorded higher absolute numbers of vaccinations (see Fig. 3). Vaccination coverage per 100 population similarly show countries with population size of 100milion+ ; those within high income economies and Eastern Asia region recorded higher vaccination rate per 100 (see Fig. 4).
Fig. 3.
COVID-19 vaccinations: persons fully vaccinated,
Source: Data of Global Health Security Index database (2021).
Fig. 4.
COVID-19 vaccinations: persons fully vaccinated per 100,
Source: Data of Global Health Security Index database (2021).
Correlation between GHSI and COVID-19 outcome measures
It was discovered that (counter intuitively) an increase in GHSI scores did not translate into a reduction in the incidence of COVID-19 cases, holding other variables constant (Coef=157133.4, p-value=0.009, [95%CI 39728.64 274538.15]) (see Table 3). In effect, there appeared to be an unfavourable association between GHSI performance and incidence of COVID-19 cases in the 195 countries. Consequently, even though high GHSI scores are (intuitively) expected to translate into reduced COVID-19 cases (negative correlation), the data found the opposite (counter-intuitive) results where high GHSI scores did not translate into reduction in COVID-19 cases as expected.
Table 3.
Linear regression on correlation between COVID-19 cases and deaths and GHSI score.
| Independent variables | Model 1: COVID-19 Cases | Model 2: COVID-19 Deaths | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | p-value | [95% Conf | Interval] | Sig | Coef. | p-value | [95% Conf | Interval] | Sig | |
| GHSI_2021 score | 157133.4 | 0.009 | 39728.64 | 274538.15 | *** | 1405.804 | 0.047 | 18.1 | 2793.508 | ** |
| GHSI progress proxy* | -221634.38 | 0.254 | -603660.95 | 160392.21 | -1254.942 | 0.584 | -5770.431 | 3260.546 | ||
| Africa | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Central Asia | -829710.16 | 0.784 | -6788797 | 5129376.7 | -7614.816 | 0.831 | -78050.196 | 62820.565 | ||
| Eastern Asia | -509440.39 | 0.872 | -6748370.2 | 5729489.4 | -81988.785 | 0.030 | -155731.86 | -8245.709 | ** | |
| Europe | 639595.98 | 0.739 | -3150135.6 | 4429327.6 | 17078.562 | 0.453 | -27715.413 | 61872.537 | ||
| Latin America/Caribbean | 677069.4 | 0.697 | -2746601.6 | 4100740.4 | 36565.156 | 0.076 | -3902.046 | 77032.357 | * | |
| Northern America | 33088885 | 0.000 | 22973340 | 43204429 | *** | 380807.92 | 0.000 | 261243.93 | 500371.91 | *** |
| Oceania | 1576835.9 | 0.472 | -2741791.7 | 5895463.5 | 16770.038 | 0.518 | -34275.396 | 67815.473 | ||
| South-eastern Asia | -539668.53 | 0.817 | -5145355.6 | 4066018.6 | -13644.948 | 0.621 | -68083.376 | 40793.48 | ||
| Southern Asia | 2824337.4 | 0.243 | -1936228.5 | 7584903.4 | 10957.378 | 0.701 | -45311.691 | 67226.448 | ||
| Western Asia | 194308.13 | 0.923 | -3767774.3 | 4156390.5 | 6905.32 | 0.771 | -39925.812 | 53736.451 | ||
| <million | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| 1–10million | 1021358.7 | 0.528 | -2168808.6 | 4211525.9 | 12941.79 | 0.499 | -24765.437 | 50649.017 | ||
| 10–50million | 301054.91 | 0.860 | -3053973.4 | 3656083.2 | 8624.61 | 0.668 | -31031.246 | 48280.467 | ||
| 100million+ | 11385899 | 0.000 | 6352211.5 | 16419587 | *** | 217082.06 | 0.000 | 157584.74 | 276579.39 | *** |
| Low income | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Lower middle income | -904832.61 | 0.577 | -4097607.8 | 2287942.6 | -9949.774 | 0.603 | -47687.826 | 27788.278 | ||
| Upper middle income | -261156.01 | 0.886 | -3851811.8 | 3329499.8 | 7589.963 | 0.725 | -34850.97 | 50030.897 | ||
| High income | -395676.86 | 0.860 | -4832892.1 | 4041538.4 | -20781.056 | 0.435 | -73228.176 | 31666.063 | ||
| Constant | -4987651.2 | 0.012 | -8877826.9 | -1097475.4 | ** | -50906.817 | 0.030 | -96888.024 | -4925.61 | ** |
| Models output |
Model 1 Mean dependent var2810112.864 SD dependent var 8349878.210 R-squared 0.478 Number of obs 191.000 F-test 9.302 Prob > F 0.000 Akaike crit. (AIC)6541.256 Bayesian crit. (BIC)6599.797 |
Model 2 Mean dependent var33005.508 SD dependent var 105171.496 R-squared 0.540 Number of obs 191.000 F-test 11.942 Prob > F 0.000 Akaike crit. (AIC)4845.949 Bayesian crit. (BIC)4904.489 |
||||||||
Source: Secondary Data of Global Health Security Index 2021
* ** p < .01, * * p < .05, * p < .1
Likewise, it was observed that an increase in GHSI score did not translate into a reduction in COVID-19 deaths in the 195 countries rather increased same, holding other factors constant (Coef=1405.804, p-value=0.047, [95%CI 18.1 2793.508]) (see Table 3).
As shown in Table 4, GHSI scores had a positive association with COVID-19 vaccination coverage and persons vaccinated per 100 population. For instance, an increase in GHSI score by one point increases the percentage of persons fully vaccinated per 100 population by approximately 0.6 (Coef=0.572, p-value=0.000, [95%CI.272.873]), holding other covariates constant (see Table 4). Thus, countries that demonstrated better performance in GHSI were also more likely to witness an improvement in their response to COVID-19 in terms of persons fully vaccinated per 100 population.
Table 4.
Linear regression on correlation between COVID-19 vaccination coverage and GHSI score.
| Independent variables |
Model 1: Persons fully vaccinated |
Model 2: Persons fully vaccinated per 100 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | p-value | [95% Conf | Interval] | Sig | Coef. | p-value | [95% Conf | Interval] | Sig | |
| GHSI_2021 score | 89238.458 | 0.920 | -1660727.8 | 1839204.7 | .572 | 0.000 | .272 | .873 | * ** | |
| GHSI progress proxy* | -2880148 | 0.310 | -8464850.8 | 2704554.8 | .119 | 0.806 | -.84 | 1.079 | ||
| Africa | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Central Asia | 2858382.2 | 0.949 | -84647899 | 90364663 | 12.175 | 0.112 | -2.856 | 27.205 | ||
| Eastern Asia | 2.541e+ 08 | 0.000 | 1.488e+ 08 | 3.595e+ 08 | * ** | 24.984 | 0.007 | 6.893 | 43.075 | * ** |
| Europe | 5633530.7 | 0.844 | -50927679 | 62194741 | .09 | 0.985 | -9.626 | 9.805 | ||
| Latin America/Caribbean | -5195678.9 | 0.840 | -55760181 | 45368824 | 12.848 | 0.004 | 4.163 | 21.534 | * ** | |
| Northern America | 26787339 | 0.724 | -1.227e+ 08 | 1.763e+ 08 | -4.245 | 0.745 | -29.919 | 21.429 | ||
| Oceania | 4512196.5 | 0.887 | -58147061 | 67171454 | 21.203 | 0.000 | 10.44 | 31.966 | * ** | |
| South-eastern Asia | 10805452 | 0.755 | -57352901 | 78963805 | 30.586 | 0.000 | 18.879 | 42.294 | * ** | |
| Southern Asia | 71454430 | 0.046 | 1441427.8 | 1.415e+ 08 | * * | 32.683 | 0.000 | 20.657 | 44.709 | * ** |
| Western Asia | 2478141.9 | 0.933 | -55886282 | 60842565 | 5.803 | 0.255 | -4.222 | 15.828 | ||
| <million | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| 1–10million | 2624328 | 0.912 | -44255877 | 49504533 | -8.239 | 0.045 | -16.291 | -.186 | * * | |
| 10–50million | 11864216 | 0.636 | -37506564 | 61234997 | -5.937 | 0.169 | -14.418 | 2.543 | ||
| 100million+ | 2.006e+ 08 | 0.000 | 1.267e+ 08 | 2.745e+ 08 | * ** | -9.39 | 0.146 | -22.084 | 3.303 | |
| Low income | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||
| Lower middle income | 6897813 | 0.775 | -40567359 | 54362985 | 10.574 | 0.011 | 2.421 | 18.727 | * * | |
| Upper middle income | 26039964 | 0.335 | -27078183 | 79158110 | 20.025 | 0.000 | 10.901 | 29.149 | * ** | |
| High income | 7012143.9 | 0.833 | -58399705 | 72423993 | 38.328 | 0.000 | 27.092 | 49.563 | * ** | |
| Constant | -18475710 | 0.533 | -76787588 | 39836169 | 6.364 | 0.212 | -3.652 | 16.38 | ||
| Models output |
Model 1 Mean dependent var24898578.563 SD dependent var 115218529.283 R-squared 0.410 Number of obs 190.000 F-test 7.037 Prob > F 0.000 Akaike crit. (AIC)7527.564 Bayesian crit. (BIC)7586.010 |
Model 2 Mean dependent var51.439 SD dependent var 26.932 R-squared 0.682 Number of obs 190.000 F-test 21.651 Prob > F 0.000 Akaike crit. (AIC)1608.256 Bayesian crit. (BIC)1666.703 |
||||||||
Source: Secondary Data of Global Health Security Index 2021
* ** p < .01, * * p < .05, * p < .1
Table 5, Table 6 show a decomposition of multivariate regression output in terms of the six (6) categories of global health security indices and COVID-19 outcome measures. We also found that “prevention of emergence or release of pathogens” has significant association with vaccination coverage per 100 population (Coef = 0.307, p-value = 0.022, [95%CI 0.044 0.569]). GHSI category on “rapid response” correlated negatively with number of persons fully vaccinated (Coef = −2110977.1, p-value = 0.022, [95%CI −3919988.3 −301965.87]); similarly, improving “national financing” capacity also had a negative association with persons fully vaccinated per 100 population (Coef = −0.365, p-value = 0.003, [95%CI −.6 −.129]). However, a positive association was observed between overall “risk environment” and persons fully vaccinated per 100 population (Coef=0.835, p-value=0.000, [95%CI.538 1.132]), holding other co-variates constant (see Table 6).
Table 5.
Linear regression on categories of global health security and COVID-19 outcome measures.
| Independent variables |
Model 1: COVID-19 Cases |
Model 2: COVID-19 Deaths |
||||||
|---|---|---|---|---|---|---|---|---|
| Coef. | p-value | [95% Conf | Interval] | Coef. | p-value | [95% Conf | Interval] | |
| GHSI score category 1 | 54059.011 | 0.365 | -63424.093 | 171542.12 | 1110.895 | 0.111 | -256.72 | 2478.509 |
| GHSI score category 2 | 32520.818 | 0.534 | -70507.909 | 135549.55 | 86.631 | 0.887 | -1112.721 | 1285.983 |
| GHSI score category 3 | 32423.189 | 0.612 | -93417.898 | 158264.27 | 745.511 | 0.317 | -719.398 | 2210.421 |
| GHSI score category 4 | 47772.482 | 0.446 | -75682.406 | 171227.37 | 478.303 | 0.512 | -958.829 | 1915.435 |
| GHSI score category 5 | -29229.913 | 0.587 | -135211.93 | 76752.103 | -929.527 | 0.139 | -2163.258 | 304.204 |
| GHSI score category 6 | -21474.877 | 0.752 | -155237 | 112287.24 | -499.759 | 0.527 | -2056.877 | 1057.359 |
| Africa | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Central Asia | -575980.71 | 0.861 | -7048712.6 | 5896751.2 | -6372.041 | 0.868 | -81720.778 | 68976.695 |
| Eastern Asia | -500457.03 | 0.877 | -6887826.2 | 5886912.1 | -86462.898 | 0.023 | -160817.93 | -12107.865 |
| Europe | 485011.6 | 0.825 | -3836650.5 | 4806673.7 | 10174.111 | 0.690 | -40134.134 | 60482.355 |
| Latin America/Caribbean | 373668.96 | 0.838 | -3229024.4 | 3976362.3 | 28234.857 | 0.186 | -13703.91 | 70173.623 |
| Northern America | 32871378 | 0.000 | 22323893 | 43418864 | 373178.83 | 0.000 | 250396.1 | 495961.56 |
| Oceania | 1304242.1 | 0.558 | -3087341.7 | 5695826 | 10308.669 | 0.691 | -40813.53 | 61430.869 |
| South-eastern Asia | -1068991 | 0.655 | -5789278 | 3651296 | -17101.567 | 0.540 | -72050.183 | 37847.05 |
| Southern Asia | 2542775.2 | 0.318 | -2471370.1 | 7556920.5 | 2896.672 | 0.922 | -55472.734 | 61266.078 |
| Western Asia | -458300.16 | 0.833 | -4730676.2 | 3814075.9 | -9505.975 | 0.706 | -59240.483 | 40228.533 |
| <million | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 1–10million | 882391.75 | 0.599 | -2427222.5 | 4192006 | 8174.867 | 0.676 | -30352.18 | 46701.915 |
| 10–50million | 35357.086 | 0.984 | -3546064.7 | 3616778.9 | 2590.866 | 0.903 | -39100.28 | 44282.011 |
| 100million+ | 10990833 | 0.000 | 5682309.5 | 16299356 | 210747.06 | 0.000 | 148950.81 | 272543.3 |
| Low income | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Lower middle income | -719377.99 | 0.679 | -4139984.6 | 2701228.6 | -10160.651 | 0.615 | -49979.755 | 29658.454 |
| Upper middle income | -269480.33 | 0.895 | -4287172.6 | 3748211.9 | 3018.908 | 0.899 | -43750.839 | 49788.655 |
| High income | 154745.72 | 0.956 | -5381128.6 | 5690620 | -18099.687 | 0.580 | -82542.513 | 46343.14 |
| Constant | -1502940.4 | 0.675 | -8575465.2 | 5569584.3 | 8424.549 | 0.840 | -73906.345 | 90755.443 |
| Model 1 | Model 2 | |||||||
| Mean dependent var 2810112.864 |
SD dependent var 8349878.210 |
Mean dependent var 33005.508 |
SD dependent var 105171.496 |
|||||
| R-squared 0.480 |
Number of obs 191.000 |
R-squared 0.556 |
Number of obs 191.000 |
|||||
| F-test 7.419 |
Prob > F 0.000 |
F-test 10.060 |
Prob > F 0.000 |
|||||
| Akaike crit. (AIC) 6548.471 |
Bayesian crit. (BIC) 6620.021 |
Akaike crit. (AIC) 4847.339 |
Bayesian crit. (BIC) 4918.889 |
|||||
| * ** p < .01, * * p < .05, * p < .1 | * ** p < .01, * * p < .05, * p < .1 | |||||||
Source: GHSI Database (2021); Legend: GHSI score category 1 (Prevention of emergence or release of pathogens); GHSI score category 2 (Early detection and reporting for epidemics of potential international concern); GHSI score category 3 (Rapid response to and mitigation of the spread of an epidemic); GHSI score category 4 (Sufficient & robust health sector to treat the sick & protect health workers); GHSI score category 5 (Commitments to improving national capacity financing and adherence to norms); GHSI score category 6 (Overall risk environment and country vulnerability to biological threats)
Table 6.
Linear regression on categories of global health security and COVID-19 vaccination cov0.044 0.5erage.
| Independent variables |
Model 1: Fully vaccinated |
Model 2: full vaccination per 100 |
||||||
|---|---|---|---|---|---|---|---|---|
| Coef. | p-value | [95% Conf | Interval] | Coef. | p-value | [95% Conf | Interval] | |
| GHSI score category 1 | 196709.88 | 0.818 | -1485822.4 | 1879242.1 | .307 | 0.022 | .044 | .569 |
| GHSI score category 2 | 39479.303 | 0.958 | -1442799.6 | 1521758.2 | .048 | 0.680 | -.183 | .28 |
| GHSI score category 3 | -2110977.1 | 0.022 | -3919988.3 | -301965.87 | -.213 | 0.139 | -.495 | .07 |
| GHSI score category 4 | 1550671.2 | 0.084 | -211035.01 | 3312377.5 | .246 | 0.079 | -.029 | .52 |
| GHSI score category 5 | -1063687 | 0.166 | -2574068.2 | 446694.1 | -.365 | 0.003 | -.6 | -.129 |
| GHSI score category 6 | 1499968.1 | 0.122 | -405088.93 | 3405025.1 | .835 | 0.000 | .538 | 1.132 |
| Africa | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Central Asia | -25535837 | 0.586 | -1.180e+ 08 | 66889072 | 4.621 | 0.528 | -9.797 | 19.039 |
| Eastern Asia | 2.371e+ 08 | 0.000 | 1.327e+ 08 | 3.414e+ 08 | 18 | 0.030 | 1.722 | 34.278 |
| Europe | -24450830 | 0.438 | -86506039 | 37604380 | -6.887 | 0.162 | -16.568 | 2.793 |
| Latin America/Caribbean | -10205877 | 0.697 | -61815402 | 41403648 | 12.479 | 0.003 | 4.428 | 20.53 |
| Northern America | 565286.09 | 0.994 | -1.504e+ 08 | 1.515e+ 08 | -9.241 | 0.440 | -32.793 | 14.311 |
| Oceania | 3198243.9 | 0.919 | -58872668 | 65269156 | 19.655 | 0.000 | 9.972 | 29.338 |
| South-eastern Asia | 7551165.8 | 0.827 | -60497239 | 75599570 | 31.408 | 0.000 | 20.793 | 42.024 |
| Southern Asia | 39711570 | 0.276 | -31953497 | 1.114e+ 08 | 23.169 | 0.000 | 11.99 | 34.349 |
| Western Asia | -10927969 | 0.724 | -72033517 | 50177579 | 3.115 | 0.520 | -6.418 | 12.647 |
| <million | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 1–10million | 4913019.7 | 0.838 | -42473632 | 52299671 | -5.885 | 0.118 | -13.278 | 1.507 |
| 10–50million | 13290851 | 0.609 | -37977507 | 64559208 | -2.8 | 0.490 | -10.798 | 5.198 |
| 100million+ | 2.077e+ 08 | 0.000 | 1.319e+ 08 | 2.835e+ 08 | -2.81 | 0.640 | -14.633 | 9.013 |
| Low income | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Lower middle income | -6919197.9 | 0.783 | -56333768 | 42495372 | 3.004 | 0.443 | -4.705 | 10.713 |
| Upper middle income | 4843529.2 | 0.869 | -53009544 | 62696603 | 8.448 | 0.066 | -.577 | 17.473 |
| High income | -28165972 | 0.484 | -1.074e+ 08 | 51098243 | 18.351 | 0.004 | 5.985 | 30.716 |
| Constant | 4851185.9 | 0.925 | -96814036 | 1.065e+ 08 | 1.011 | 0.900 | -14.848 | 16.871 |
| Model 1 | Model 2 | |||||||
| Mean dependent var 24898578.563 |
SD dependent var 115218529.283 |
Mean dependent var 51.439 |
SD dependent var 26.932 |
|||||
| R-squared 0.444 |
Number of obs. 190.000 |
R-squared 0.752 |
Number of obs 190.000 |
|||||
| F-test 6.389 |
Prob > F 0.000 |
F-test 24.307 s |
Prob > F 0.000 |
|||||
| Akaike crit. (AIC) 7524.344 |
Bayesian crit. (BIC) 7595.778 | Akaike crit. (AIC) 1568.448 |
Bayesian crit. (BIC) 1639.883 |
|||||
| * ** p < .01, * * p < .05, * p < .1 | * ** p < .01, * * p < .05, * p < .1 | |||||||
Source: GHSI Database (2021); Legend: GHSI score category 1 (Prevention of emergence or release of pathogens); GHSI score category 2 (Early detection and reporting for epidemics of potential international concern); GHSI score category 3 (Rapid response to and mitigation of the spread of an epidemic); GHSI score category 4 (Sufficient & robust health sector to treat the sick & protect health workers); GHSI score category 5 (Commitments to improving national capacity financing and adherence to norms); GHSI score category 6 (Overall risk environment and country vulnerability to biological threats)
Discussion
Health security of the world remains a critical concern given the devastating impact of COVID-19 making it one of the worst pandemics in the history of mankind. Moreover, the low performance of countries in the GHSI assessments is a palpable manifestation of the vulnerability of the world to these unexpected pandemics. Per analysed GHSI data the global average score was 38.9 out of 100 [5], suggesting the world literally failed in the health security and preparedness test.
As part of efforts towards guaranteeing preparedness for future pandemics by countries, the Global Health Security Agenda (GHSA) group was set up and the framework published in 2018. According to the GHSA 2024 Framework [16], more countries by the year 2024 would have completed an evaluation of health security capacity situation in their settings [16]. The report further intimates that countries assessed with the GHSI parameters would have strengthened their capacities and demonstrated improvements in at least five technical areas to a level of ‘demonstrated capacity’ in line with the World Health Organization (WHO) International Health Regulations (IHR) Framework [15].
Indeed, the GHSA framework (2018) and GHSI assessments have been applauded as laudable steps towards independent determination of the global health security situation. Barely a few months after the first GHSI assessment, COVID-19 was declared a pandemic by the WHO with deleterious consequences. COVID-19 impact on countries vindicated the GHSI scores that the world was never ready for major pandemics. Even western countries with more robust health systems that scored higher GHSI scores did not translate into positive COVID-19 response outcomes [9], [17], [18], [19].
Analysis of the latest GHSI data, reported in this paper, particularly demonstrates the unfavourable correlation between GHSI scores and COVID-19 outcome measures. One could glean from findings of the GHSI assessments that more needs to be done to enhance resilience of health systems for future pandemics. Empirical evidence attests that even before the first case of COVID-19 was recorded in December, 2019 the world’s performance in the GHSI did not point to a world that is prepared to respond to a major pandemic like COVID-19 [20]. This observation is corroborated by findings in this current paper where higher GHSI scores did not necessarily translate into a reduction in the cumulative number of COVID-19 cases and deaths. Earlier studies [9], [17], [18], [19] arrived at similar conclusions when they analysed the 2019 GHSI data sets against similar parameters on COVID-19.
Previous studies had alluded to the fact that a lack of integrated health systems within countries compromises resilience of health systems to respond to pandemics including COVID-19 [21], [22]. Evidence from this study shows that even though many western countries scored higher on the GHSI than their Asian and African countries, the later recorded better COVID-19 outcomes in terms of case counts and deaths. Some experts attributed these dynamics to better integrated health systems in some Asian [21], [22], [23], [24] and African countries [25], [26], [27], [28], [29], [30], especially at the primary health care level. Moreover, before the outbreak of COVID-19, studies [2], [3] argued on the need to prioritise integrated health systems over fragmented ones. This approach, according to health system experts, ensures seamless integration of global security, UHC and primary health care building blocks within countries.
In lieu of the global public health paradox discovered from the GHSI data, the hypothesis has been proven that optimum GHSI performance on its own does not translate into assured preparedness of health systems to respond effectively to pandemics. Indeed, even though United States of America scored the highest 2021 GHSI score of 75.9, it also recorded the highest number of COVID-19 confirmed cases and deaths. On the contrary many countries in Africa which recorded GHSI scores below the global average of 38.9 recorded low COVID-19 cases and deaths, corroborating findings by similar studies on this subject [31], [32].
Nonetheless, higher GHSI scores corresponded positively with the percentage of persons fully vaccinated against COVID-19. This observation contradicts conclusions by Aitken et al. [20] who found that the 2019 GHSI scores had an inverse correlation with vaccination coverage. Perhaps, this could be attributed to the relatively early days of the pandemic when progress in the development and deployment of the COVID-19 vaccine were still minimal.
Evidence from the GHSI data strongly suggests a compelling need to revisit the GHSI assessment criteria to adequately account for the contextual and environmental factors that impinge on accurate determination of health system preparedness and health security situation in countries. Chang and McAleer [19] made similar recommendations having acknowledged this potential lapse in the GHSI methodology. If the GHSI is not serving its purpose as a surrogate for health system preparedness for pandemics (evident in the current GHSI data) then same must be revisited and possibly revised. It is also important to reiterate the caveat that issues of data quality, completeness and synchrony across the 195 participating countries could potentially impact negatively on the GHSI scores inadvertently. Thus, more robust and parsimonious assessment tools and strategies could help enhance the otherwise promising global health security database.
Finally, based on the available evidence, it would be more beneficial for countries to invest in integrated health systems that prioritise all building blocks of the health system. For instance, successes in health security without commensurate gains in PHC and UHC renders a country vulnerable to shocks and ravages from future pandemics. Empirical literature argues the United States of America (USA) perhaps did not fully maximise its primary health care (PHC) in response to COVID-19 hence its challenged response to COVID-19 [33]. PHC concept is typically designed to respond pragmatically to infectious disease outbreaks at the community level through effective contact tracing and mapping [34], [35]. Even though USA spends the highest per capita expenditure of US$ 10,921.01 on health in the world [36], the primary healthcare system is highly fragmented and incapacitated to deal with novel pandemics like COVID-19 [37], [38], [39], [40].
On other hand, some experts have argued that, holding exogenous factors constant, some African [25], [26], [27], [28], [29], [30], [31], [32] and Asian countries [21], [22], [23], [24] responded relatively better to COVID-19 pandemic due to a more robust PHC system in addition to leveraged experiences from earlier pandemics like Ebola (in the case of Africa). In Ghana for example, community-based health planning and services (CHPS) system was leveraged for contact tracing, isolation and case management [41], [42], [43], [44]. Unfortunately, same cannot be fully said of many western countries which appear to have consolidated on UHC and GHSI gains but seemingly demonstrated weaknesses at the PHC level [37], [38], [39], [40]. These assertions are corroborated by the evidence espoused in this paper from the GHSI data sets.
Limitations
the first, the paper is based mainly on secondary data set without the compliment of primary data. An incorporated primary data would have allowed the researchers to explore further on potential reasons for the empirical findings. Also, any existing methodological lapses already acknowledged by the GHSI team automatically apply to this study since there was no methodological review nor compliment of data with primary data.
Additionally, critics of the GHSI maintain that the index is not hinged on a theory as basis to predict countries response to pandemics like COVID-19 and thus questions whether the index is indeed adequate to measure responsiveness to national health systems. Finally, the index is criticized as not adequately accounting for health systems that do not have comprehensive UHC especially in resource-poor settings which as the potential to independently impact on countries response to pandemics.
Notwithstanding the above limitations, the GHSI promises to be important tool that is capable of gauging the global health security situation and preparedness for pandemics. Moreover, the robustness of the GHSI methodology coupled with the rigorous/validated tools makes the data fidelity unquestionable and evidence from it compelling.
Conclusion
The main question this paper attempted to addressed is why the GHSI appeared not be an indicator with the ability to predict response to the COVID-19 pandemic and whether or not this invalidates the GHSI itself. The paper also raises a vital policy dialogue issue on how GHSI can for instance be modified to account for country-specific conditions that impinged on their ability to respond effectively to the COVID-19 pandemic independent of their GHSI scores. For instance, the fact that countries with established health care capabilities like the United States might have responded poorly to the COVID-19 pandemic perhaps due to political and internal coordination problems in their health care system, as discussed in the paper.
Overall, evidence from the analysed GHSI data strongly suggests the world might still not be adequately prepared for the next major pandemic, if no drastic steps are taken to change the narrative. A global aggregate score of 38.9 out of the expected optimum score of 100is a palpable manifestation of countries unpreparedness for the next major pandemic [5]. Countries that scored higher on the GHSI assessment did not translate into optimal response to the COVID-19 pandemic. Nonetheless, the glimpse of hope is that high GHSI scores correlated positively with vaccination coverage per 100 population. Moving forward, even though the GHSI methodology has been validated and proven reliable the assessment criteria and tools might have to be revisited at the next review opportunity to reflect the contextual and environmental nuances in pertinent countries. Finally, even though the current GHSI methodology attempts to adjust for country-specific conditions there is the need to adapt the tools to account for differences in health systems in low-resource and resource rich settings. This adaption will help avert perpetual comparison of apples with oranges.
Declarations
NA.
Ethical Approval and Consent to Participate
Paper was written mainly based on analysis of publicly available secondary data; likewise, no human subjects were involved hence no Ethical Clearance required as per local ethics committees’ guidelines.
CRediT authorship contribution statement
RKA: provided conceptualization direction, literature search, synthesis and analysis and manuscript write-up; JJN AAA AA SSM EN: read and peer reviewed the manuscript based on their respective technical knowledge and expertise. All authors read and approved manuscript for publication.
Funding
There is no funding support for this work.
Consent for publication
Not applicable.
Competing interests
Authors declare that there is no conflict of interest.
Acknowledgements
The authors appreciate and acknowledge GHSI Team for granting the authors the permission to use the data.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jiph.2022.12.011.
Appendix A. Supplementary material
Supplementary material
.
Supplementary material
.
Supplementary material
.
References
- 1.Universal Health Coverage (UHC) Partnership Annual Report. Implementing a primary health care approach towards universal health coverage in the COVID-19 era. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
- 2.Wenham C., Katz R., Birungi C., et al. Global health security and universal health coverage: from a marriage of convenience to a strategic, effective partnership. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2018-001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heymann D.L., Chen L., Takemi K., et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet. 2015;385:1884–1901. doi: 10.1016/S0140-6736(15)60858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erondu N.A., Martin J., Marten R., Ooms G., Yates R., Heymann D.L. Building the case for embedding global health security into universal health coverage: a proposal for a unified health system that includes public health. Lancet. 2018;392:1482–1486. doi: 10.1016/S0140-6736(18)32332-8. [DOI] [PubMed] [Google Scholar]
- 5.Bell J.A. and Nuzzo J.B. Global Health Security Index: Advancing Collective Action and Accountability Amid Global Crisis, 2021. Accessed from www.GHSIndex.org on 20th August, 2022.
- 6.Dalglish S.L. COVID-19 gives the lie to global health expertise. Lancet. 2020;395:1189. doi: 10.1016/S0140-6736(20)30739-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tromberg B.J., Schwetz T.A., Pérez-Stable E.J., et al. Rapid scaling up of Covid-19 diagnostic testing in the United States—the NIH RADx initiative. N Engl J Med. 2020;383:1071–1077. doi: 10.1056/NEJMsr2022263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Official Website. Coronavirus disease (COVID-19) pandemic dashboard [Internet]. 2022. Accessed from: https://www.afro.who.int/news/second-covid-19-caseconfirmed-africa on 20th August, 2022.
- 9.Lal A., Erondu N.A., Heymann D.L., Gitahi G., Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397(10268):61–67. doi: 10.1016/S0140-6736(20)32228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Our World in Data. Coronavirus (COVID-19) Vaccinations. [Internet]. 2022 [cited 2022 August 20]. Available from https://ourworldindata.org/covid-vaccinations.
- 11.Alhassan R.K., Aberese-Ako M., Doegah P.T., Immurana M., Dalaba M.A., Manyeh A.K., Gyapong M. COVID-19 vaccine hesitancy among the adult population in Ghana: evidence from a pre-vaccination rollout survey. Trop Med Health. 2021;49(1):1–13. doi: 10.1186/s41182-021-00357-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alhassan R.K., Owusu-Agyei S., Ansah E.K., Gyapong M. COVID-19 vaccine uptake among health care workers in Ghana: a case for targeted vaccine deployment campaigns in the global south. Hum Resour Health. 2021;19(1):1–12. doi: 10.1186/s12960-021-00657-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.African Union (A.U.) Africa CDC, Official Website [Internet]. 2022 [cited 2022 June 17]. Available from: https://africacdc.org/covid-19/.
- 14.Global Health Security Index. GHS Index Methodology Prepared by Economist Impact [Internet] [cited 2022 August 20]. Available from: https://www.ghsindex.org/wp-content/uploads/2021/11/2021_GHSindex_Methodology_FINAL.pdf.
- 15.World Health Organization (WHO). 2005 International Health Regulations. Third Edition. 1 January 2016. ISBN: 9789241580496. [Internet] [cited 2022 August 17]. Available from https://www.who.int/publications/i/item/9789241580496.
- 16.Global Health Security Agenda (GHSA) 2024 Framework. November, 2018 [Internet] [cited 2022 August 17]. Available from https://ghsagenda.org/.
- 17.Razavi A., Erondu N., Okereke E. The Global Health Security Index: what value does it add? BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lal A., Ashworth H.C., Dada S., Hoemeke L., Tambo E. Optimizing pandemic preparedness and response systems: lessons learned from Ebola to COVID-19. Disaster Med Public Health Prep. 2020 doi: 10.1017/dmp.2020.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang C.L., McAleer M. Alternative global health security indexes for risk analysis of COVID-19. Int J Environ Res Public Health. 2020;17(9):3161. doi: 10.3390/ijerph17093161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aitken T., Chin K.L., Liew D., Ofori-Asenso R. Rethinking pandemic preparation: Global Health Security Index (GHSI) is predictive of COVID-19 burden, but in the opposite direction. J Infect. 2020;81(2):318–356. doi: 10.1016/j.jinf.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fakhruddin B.S., Blanchard K., Ragupathy D. Are we there yet? The transition from response to recovery for the COVID-19 pandemic. Prog Disaster Sci. 2020;7 doi: 10.1016/j.pdisas.2020.100102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Legido-Quigley H., Asgari N., Teo Y.Y., Leung G.M., Oshitani H., Fukuda K., Heymann D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395(10227):848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu W., Yue X.G., Tchounwou P.B. Response to the COVID-19 epidemic: the Chinese experience and implications for other countries. Int J Environ Res Public Health. 2020;17(7):2304. doi: 10.3390/ijerph17072304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang S., Wang Z., Chang R., Wang H., Xu C., Yu X., Cai Y. COVID-19 containment: China provides important lessons for global response. Front Med. 2020;14(2):215–219. doi: 10.1007/s11684-020-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osseni, I.A. COVID-19 pandemic in sub-Saharan Africa: preparedness, response, and hidden potentials. Tropical medicine and health, 48(1), 1–3. [DOI] [PMC free article] [PubMed]
- 26.Rutayisire E., Nkundimana G., Mitonga H.K., Boye A., Nikwigize S. What works and what does not work in response to COVID-19 prevention and control in Africa. Int J Infect Dis. 2020;2020(97):267–269. doi: 10.1016/j.ijid.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuguyo O., Kengne A.P., Dandara C. Singapore COVID-19 pandemic response as a successful model framework for low-resource health care settings in Africa? OMICS: A J Integr Biol. 2020;24(8):470–478. doi: 10.1089/omi.2020.0077. [DOI] [PubMed] [Google Scholar]
- 28.Dzinamarira T., Dzobo M., Chitungo I. COVID‐19: a perspective on Africa's capacity and response. J Med Virol. 2020;92(11):2465–2472. doi: 10.1002/jmv.26159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okoi O., Bwawa T. How health inequality affect responses to the COVID-19 pandemic in Sub-Saharan Africa. World Dev. 2020;135 doi: 10.1016/j.worlddev.2020.105067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tessema G.A., Kinfu Y., Dachew B.A., Tesema A.G., Assefa Y., Alene K.A., Tesfay F.H. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact and response. BMJ Glob Health. 2021;6(12) doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haider N., Yavlinsky A., Chang Y., Hasan M., Benfield C., Osman A., Kock R. The Global Health Security index and Joint External Evaluation score for health preparedness are not correlated with countries' COVID-19 detection response time and mortality outcome. Epidemiol Infect. 2020;2020(148) doi: 10.1017/S0950268820002046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leichtweis B.G., Silva L.F., da Silva F.L., Peternelli L.A. How the global health security index and environment factor influence the spread of COVID-19: a country level analysis. One Health. 2021;2 doi: 10.1016/j.onehlt.2021.100235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nowroozpoor A., Choo E.K., Faust J.S. Why the United States failed to contain COVID‐19. J Am Coll Emerg Physicians Open. 2020;1(4):686. doi: 10.1002/emp2.12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tumusiime P., Karamagi H., Titi-Ofei R., Amri M., Seydi A.B.W., Kipruto H., Cabore J. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the Fifth Health Sector Directors’ Policy and Planning Meeting for the WHO African Region. BMC Proc. 2020;14(19):1–8. doi: 10.1186/s12919-020-00203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Primary health care and health emergencies (No. WHO/HIS/SDS/2018.51). World Health Organization, 2018 [Internet] [cited August 2020]. Available from https://apo.who.int/publications/i/item/WHO-HIS-SDS-2018.52.
- 36.World Bank. Current health expenditure per capita (in US$) 2019. [Internet] [cited August 20]. Available from https://data.worldbank.org/indicator/SH.XPD.CHEX.PC.CD.
- 37.Parker R.W. Why America’s response to the COVID-19 pandemic failed: lessons from New Zealand’s success. Adm Law Rev. 2021;73:77–103. [Google Scholar]
- 38.Sauer M.A., Truelove S., Gerste A.K., Limaye R.J. A failure to communicate? How public messaging has strained the COVID-19 response in the United States. Health Secur. 2021;19(1):65–74. doi: 10.1089/hs.2020.0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schismenos S., Smith A.A., Stevens G.J., Emmanouloudis D. Failure to lead on COVID-19: what went wrong with the United States? Int J Public Leadersh. 2020 [Google Scholar]
- 40.Kettl D.F. States divided: the implications of American federalism for COVID-19. COVID-19 Read. 2020:165–181. doi: 10.1111/puar.13243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sibiri H., Prah D., Zankawah S.M. Containing the impact of COVID-19: review of Ghana's response approach. Health Policy Technol. 2021;10(1):13. doi: 10.1016/j.hlpt.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quakyi N.K., Asante N.A.A., Nartey Y.A., Bediako Y., Sam-Agudu N.A. Ghana’s COVID-19 response: the Black Star can do even better. BMJ global health. 2021;6(3) doi: 10.1136/bmjgh-2021-005569. e00556 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kenu E., Frimpong J., Koram K. Responding to the COVID-19 pandemic in Ghana. Ghana Med J. 2020;54(2):72–73. doi: 10.4314/gmj.v54i2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asiimwe N., Tabong P.T.N., Iro S.A., Noora C.L., Opoku-Mensah K., Asampong E. Stakeholders perspective of, and experience with contact tracing for COVID-19 in Ghana: a qualitative study among contact tracers, supervisors, and contacts. PloS One. 2021;16(2) doi: 10.1371/journal.pone.0247038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Supplementary material
Supplementary material