Abstract
Background
Academic teaching institutions perform approximately one third of all orthopedic procedures in the United States. Revision total knee arthroplasty (rTKA) is a complex and challenging procedure that requires expertise and extensive planning, however the impact of resident involvement on outcomes is poorly understood. The aim of the study was to investigate whether resident involvement in rTKA impacts postoperative complication rates, operative time, and length of hospital stay (LOS).
Methods
The American College of Surgeons National Surgical Quality Improvement Program registry was queried to identify patients who underwent rTKA procedures from 2006-2012 using CPT codes 27486 and 27487. Cases were classified as resident involved or attending only. Demographics, comorbidities, and 30-day postoperative complications were analyzed. Multiple logistic regression analysis was performed to identify independent risk factors for increased 30-day postoperative complications. Wilcoxon rank sum tests were performed to determine the impact of resident involvement on operative time and LOS with significance defined as p<0.05.
Results
In total, 2,396 cases of rTKA were identified, of which 972 (40.6%) involved residents. The two study groups were similar, however the resident involved cohort had more patients with hypertension and ASA class 3 (p=0.02, p=0.04). There was no difference in complications between the cohorts (No Resident vs Resident-involved: 7.0% vs 6.7%, p=0.80). Multivariate analysis identified obesity (OR: 1.81, 95% CI: 1.18-2.79, p=0.01), morbid obesity (OR: 1.66, 95% CI: 1.09-2.57, p=0.02), congestive heart failure (OR: 5.97, 95% CI: 1.19-24.7, p=0.02), and chronic prosthetic joint infection (OR: 3.16, 95% CI: 2.184.56, p<0.01), as independent risk factors for 30-day complications after rTKA. However, resident involvement was not associated with complications within 30-days following rTKA (OR: 0.91, 95% CI: 0.65-1.26, p=0.57). Resident involvement was associated with increased operative time (p<0.001) and LOS (P<0.001).
Conclusion
Resident involvement in rTKA cases is not associated with an increased risk of 30-day postoperative complications. However, resident operative involvement was associated with longer operative time and length of hospital stay.
Level of Evidence: III
Keywords: resident education, revision total knee arthroplasty, TKA
Introduction
Total knee arthroplasty (TKA) is an effective procedure that provides pain relief and improvement of function. Amid the increase in volume of primary TKA and continued expansion of indication criteria and patient selection, the volume of revision TKA (rTKA) has increased. With increasing incidence of rTKA, it is imperative that future surgeons develop an appropriate framework for preoperative planning, postoperative management, and necessary technical skills to successfully care for patients that require rTKA.1
Academic teaching institutions perform approximately one third of all orthopedic procedures in the United States. Therefore, operative participation of residents in various settings including rTKA are a fundamental aspect of resident education. However, resident participation in surgical specialties, like orthopedic surgery, is a potential source of patient apprehension.2 In addition to patient concern, training residents can significantly increase operative time especially while training junior orthopedic residents.3 While in some procedures, operative time may have minimal impacts, multiple studies have demonstrated that increased operative time increases the risk of postoperative complications in the setting of total joint arthroplasty procedures.4-7 As a result, academic surgeons have to balance training residents while minimizing adverse events and providing efficient care, especially while performing challenging procedures that require extensive planning and skill.
Prior studies have demonstrated that resident participation does not have a significant impact on postoperative complications after various primary orthopedic procedures including primary TKA.8-16 However, the impact of resident involvement in complex revision cases on intraoperative and postoperative outcomes is poorly understood. The aim of the study was to investigate whether resident involvement in rTKA impacts postoperative complication rates, operative time, and length of hospital stay (LOS). We hypothesize that resident participation during rTKA would not have a significant impact on postoperative complications, LOS, or operative time.
Methods
Data Source
Patients undergoing rTKA were identified utilizing the American College of Surgeons National Surgical Quality Improvement Program database (ACS-NSQIP). The NSQIP database prospectively collects perioperative patient variables from private and academic hospitals across the United States.16 The data is collected by expert clinical reviewers and includes information up to 30 days following the procedure. Information collected includes patient demographics, medical comorbidities, preoperative laboratory values, operative time, length of hospital stay (LOS), and postoperative complications within 30 days of surgery. The last year that NSQIP database collected resident involvement information was 2012; therefore, data of patients who underwent rTKA from 2006 to 2012 was obtained and analyzed for this study. Patient records were retrieved and analyzed using Current Procedural Terminology (CPT) and International Classification of Diseases Ninth Revision (ICD 9) codes. Cases are de-identified and selected based on a systematic sampling process with a reported inter-observer disagreement rate of 2%.16,17 Due to the de-identified nature of the data, this study was granted exemption from the local institutional review board (IRB).
Patient Selection, Demographics, and Comorbidities
A total of 4,309 rTKA cases were identified during the study period using CPT codes 27486 and 27487. Patients with incomplete/incongruent information regarding resident participation (n=1,781) and those with revision due to periprosthetic malignancy (n=32) were excluded from the study. After exclusion, 2,396 cases were included, of which 972 (40.6%) consisted of at least one resident involved. (Figure 1)
Figure 1.
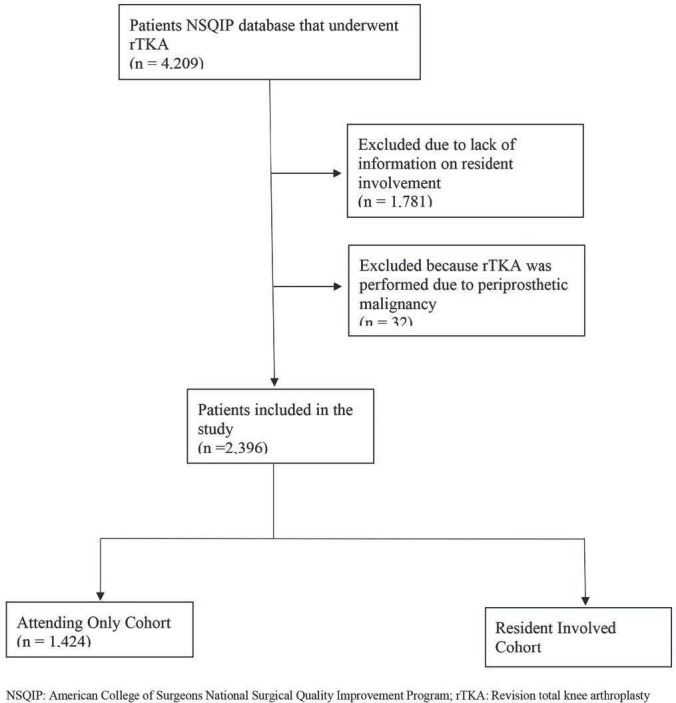
Flowchart of Inclusion and Exclusion Criteria.
Basic patient demographics including age and sex are recorded in the database and were compared between resident involved and non-resident procedures. Age was stratified by 10-year increments with patients identified as <50 years, 50-59.9years, 60-69.9 years, 70-79.9 years, and >80 years. Body mass index (BMI) was calculated from each patients’ height and weight and was defined as normal for BMI 18 to 29.9 kg/m2, obese for BMI 30 to 39.9 kg/m2, and morbidly obese as BMI > 40 kg/m2. Other preoperative conditions including diabetes mellitus, smoking history, chronic obstructive pulmonary disease, congestive heart failure, hypertension, and American Society of Anesthesiologist class (ASA) were compared between the two cohorts. Diabetes mellitus is categorized as insulin-dependent, non-insulin dependent, or no diabetes in the database; however, for the purposes of this study patients were categorized as having diabetes mellitus (insulin-dependent or non-insulin dependent) or not. The indication for rTKA was determined using ICD 9 codes and were categorized as component failure, prosthetic joint infection (PJI), aseptic necrosis, periprosthetic fracture, or dislocation. (Table 1).
Table 1.
Comparison of Comorbidities Between Resident Involved and Attending Only Cohorts Undergoing Revision Total Knee Arthroplasty
| Comorbidities | Attending Only (n= 1,424) | Resident Involved (n= 972) | P-Value |
|---|---|---|---|
| Age, years | |||
| < 50 years | 123 (8.6) | 90 (9.3) | 0.60 |
| 50 - 59.9 years | 308 (21.6) | 238 (24.5) | 0.10 |
| 60 – 69.9 years | 451 (31.7) | 312 (32.1) | 0.83 |
| 70 – 79.9 years | 386 (27.1) | 243 (25) | 0.25 |
| >80 years | 156 (11) | 89 (9.2) | 0.15 |
| Male Sex | 568 (39.9) | 419 943.1) | 0.16 |
| Body Mass Index, m/kg2 | |||
| Normal | 536 (37.6) | 383 (39.4) | 0.38 |
| Obese | 408 (28.7) | 278 (28.6) | 0.98 |
| Morbid Obesity | 480 (33.7) | 311 (32.0) | 0.38 |
| Diabetes Mellitus | 324 (22.8) | 191 (19.7) | 0.07 |
| Smoke | 168 (11.8) | 113 (11.6) | 0.90 |
| Chronic Obstructive Pulmo- nary Disease | 63 (4.4) | 38 (3.9) | 0.54 |
| Congestive Heart Failure | 5 (0.4) | 4 (0.41) | 0.81 |
| Hypertension | 991 (69.6) | 633 (65.1) | 0.02* |
| ASA Classification | |||
| 1-No Disturb | 18 (1.3) | 14 (1.4) | 0.71 |
| 2- Mild Disturb | 589 (41.4) | 427 (43.9) | 0.21 |
| 3- Severe Disturb | 784 (55.1) | 493 (50.7) | 0.04* |
| 4- Life Threat | 42 (2.9) | 37 (3.8) | 0.25 |
| 5- Moribund | 0 (0) | 1 (0.1) | 0.23 |
| Reason for Revision TKA | |||
| Component Failure | 1087 (76.3) | 725 (74.6) | 0.33 |
| Prosthetic Joint Infection | 197 (13.8) | 163 (16.8) | 0.04* |
| Aseptic Necrosis/ Oste- olysis | 27 (1.9) | 12 (1.2) | 0.21 |
| Peri-prosthetic Fracture | 110 (7.7) | 67 (6.9) | 0.44 |
| Stiffness | 3 (0.2) | 5 (0.51) | 0.21 |
Bold*: significant finding (P<0.05); ‘-’: not calculable
Outcomes
The NSQIP database tracks patients for any occurrence of various adverse events for 30 days postoperatively. Therefore, only 30-day postoperative complications were compared between the cohorts. The primary outcomes evaluated were overall complications, surgical complications, medical complications, operative time, and LOS. Overall complications were defined as any occurrence of medical or surgical complications. In this study, surgical complications were defined as any occurrence of superficial surgical site infection (SSI), deep SSI, wound dehiscence, wound infections, and neurologic deficits. Medical complications were defined as any occurrence of pulmonary embolism (PE), deep vein thrombosis (DVT), urinary tract infection (UTI), renal insufficiency, pneumonia, or sepsis.
Statistical Analysis
Pearson Chi-square tests and Fischer exact tests were performed for univariate analysis to compare patient demographics, preoperative comorbidities, indication for rTKA, and postoperative complications after rTKA between the resident involved and non-resident cohorts. A multiple binomial regression analysis was performed to control for potential confounding variables and identify independent risk factors for increased complication rates within 30-days following rTKA. Additionally, Wilcoxon rank sum test was performed to compare operative time and LOS between the cohorts. All statistical analyses were performed using R version 4.0, with statistical significance defined as p<0.05.
Results
Patient Characteristics
Overall, 2,396 cases of rTKA were included in the study, with 40.6% of the revision cases involving a resident. Patients in the resident involved cohort had a significantly higher incidence of patients with ASA class 3 and hypertension (p=0.04; p=0.02; Table 1). In regard to the indication for rTKA, the resident involved cohort had a higher incidence of PJI (16.8% vs 13.8%, p=0.04; Table 1).
Postoperative Complications
On univariate analysis, there was no significant difference in overall complication rate (6.7% vs 7.0%, p=0.80), surgical complication rate (3.1% vs 3.9%, p=0.27), or medical complication rate (4.8 vs 4.5%, p=0.70) between the resident involved and non-resident cohorts (Table 2).
Table 2.
Comparison of Complication Rates Between Resident Involved and Attending Only Cohorts following Revision Total Knee Arthroplasty
| Adverse Events | Attending Only | Resident Involved | Unadjusted |
|---|---|---|---|
| (n= 1,424) | (n= 972) | P-Value | |
| Overall Complication Rate | 99 (7.0) | 65 (6.7) | 0.80 |
| Medical Complication Rate | 64 (4.5) | 47 (4.8) | 0.70 |
| Pulmonary Embolism | 8 (0.56) | 1 (0.1) | 0.07 |
| Deep Vein Thrombosis | 9 (0.63) | 11 (1.1) | 0.19 |
| Urinary Infection | 23 (1.6) | 15 (1.5) | 0.89 |
| Renal Insufficiency | 4 (0.28) | 1 (0.1) | 0.65 |
| Pneumonia | 9 (0.63) | 5 (0.51) | 0.71 |
| Systemic Infection (Sepsis, Septic Shock) | 11 (0.77) | 14 (1.4) | 0.11 |
| Surgical Complication Rate | 56 (3.9) | 30 (3.1) | 0.27 |
| Wound Infection | 15 (1.1) | 4 (0.4) | 0.08 |
| Wound Dehiscence | 9 (0.63) | 7 (0.72) | 0.79 |
| Superficial SSI | 10 (0.7) | 8 (0.82) | 0.74 |
| Deep SSI | 18 (1.3) | 11 (1.1) | 0.77 |
| Neurologic Injury | 4 (0.28) | 0 (0) | 0.15 |
Bold*: significant finding (P<0.05); ‘-’: not calculable
Multivariate analysis identified obesity (OR: 1.81, 95% CI: 1.18-2.79, p=0.01), morbid obesity (OR: 1.66, 95% CI: 1.09-2.57, p=0.02), congestive heart failure (OR: 5.97, 95% CI: 1.19-24.7, p=0.02), and chronic prosthetic joint infection (OR: 3.16, 95% CI: 2.18-4.56, p<0.01), as independent risk factors for 30-day complications after rTKA (Table 3). However, resident involvement was not associated with complications within 30-days following rTKA (OR: 0.91, 95% CI: 0.65-1.26, p=0.57). (Figure 2)
Table 3.
Independent Risk Factors for Complications Within 30-days After Revision Total Knee Arthroplasty
| Age, (Reference: <50 years) | ||
| 50 - 59.9 years | 1.36 [0.67-2.99] | 0.42 |
| 60 – 69.9 years | 1.56 [0.79-3.39] | 0.23 |
| 70 – 79.9 years | 1.40 [0.68-3.13] | 0.38 |
| > 80 years | 2.10 [0.94-4.99] | 0.08 |
| Male Sex | 1.19 [0.85-1.66] | 0.32 |
| Body Mass Index (Reference: 18.5 to 30 m/kg2) | ||
| Obese (30 to 34.9 m/kg2) | 1.81 [1.18-2.79] | 0.01* |
| Morbid Obesity (>34.9 m/kg2) | 1.66 [1.09-2.57] | 0.02* |
| Diabetes Mellitus | 1.10 [0.73-1.66] | 0.64 |
| Smoking History | 1.44 [0.86-2.34] | 0.15 |
| Chronic Obstructive Pulmonary Disease | 1.37 [0.67-2.61] | 0.36 |
| Congestive Heart Failure | 5.97 [1.19-24.7] | 0.02* |
| Hypertension | 0.80 [0.55-1.17] | 0.24 |
| ASA (reference: 1- No Disturb) | ||
| 2- Mild Disturb | 5.58 [0.45-23.5] | 0.97 |
| 3- Severe Disturb | 7.28 [0.19-94.1] | 0.97 |
| 4- Life Threat | 12.3 [0.22-31.2] | 0.97 |
| Reason for Revision TKA (reference: Component failure) | ||
| Infected Implant | 3.16 [2.18-4.56] | <0.001* |
| Aseptic Necrosis/ osteolysis | 0.42 [0.02-2.11] | 0.41 |
| Peri-prosthetic Fracture | 1.14 [0.56-2.10] | 0.69 |
| Stiffness | - | 0.99 |
| Resident Involvement | 0.91 [0.65-1.26] | 0.57 |
Bold*: significant finding (P<0.05); ‘-’: not calculable
Figure 2.

Risk Factors for 30-Day Complications After Revision Total Knee Arthroplasty.
Operative Time and LOS
Resident participation in rTKA cases significantly prolonged operative times (146 vs 125 minutes, p<0.001) and increased LOS duration (resident involved vs nonresident: 4.6 vs 3.9 days, p<0.001). (Table 4)
Table 4.
Comparison of Operative Time and Length of Hospital Stay
| Variable | Attending Only | Resident Involved | P-Value |
|---|---|---|---|
| n=1,424 | n= 972 | ||
| Operative time, min (SD) | 125.0 (60.1) | 145.8 (67.1) | <0.001* |
| Length of hospital stay, days (SD) | 3.9 (3.2) | 4.6 (5.3) | <0.001* |
Bold*: significant finding (P<0.05); ‘-’: not calculable
Discussion
Resident training, inside and outside of the operating room, is a fundamental pillar of academic orthopedic institutions. While maturation of the next generation of orthopedic surgeons is critical, there is concern regarding patient safety with resident participation during operative cases.2 The findings of this study are valuable in informing orthopedic residents as well as resident educators. This study determined that resident participation during rTKA was not associated with increased risk of 30-day postoperative complications. However, resident participation during rTKA was associated with significantly longer operative time as well as increased length of hospital stay.
Prior studies have assessed the impact of resident participation on postoperative complications after various orthopedic,8,10-12,15,18-21 and non-orthopedic procedures22-25 with conflicting findings. Haughom et al. assessed the impact of resident participation during primary TKA and concluded that resident participation in primary TKA does not increase risk for short-term morbidity or mortality.15 Similarly, resident participation was not associated with increased risk of short-term morbidity or mortality after primary total hip arthroplasty (THA).8 These findings have also been demonstrated for patients undergoing total shoulder arthroplasty,10,11 knee arthroscopy,18 anterior cruciate ligament reconstruction,19 and other orthopedic procedures. The findings of the present study are consistent with prior studies and demonstrates that resident participation during rTKA was not significantly associated with 30-day medical, surgical or overall complications. However, unlike prior studies, this is the first study to assess the impact of resident participation on revision cases, which involves additional skill and challenging factors.
In the current climate of cost-effective, value-based outcomes, length of procedure and postoperative hospital stay have become important parameters that have been assessed.26 This has been emphasized to the degree that there is now a growing trend to perform common inpatient procedures on an outpatient or short-stay basis. In fact, in January 2018, the Center for Medicare and Medicaid Services (CMS) removed primary TKA as an inpatient only procedure in order to facilitate cost-effective care for Medicare and Medicaid patients.27,28
The present study determined that resident participation was associated with longer operative time for rTKA when compared to non-resident cases. The fact that resident involvement in surgical procedures increases operative time is known. In 2016, Allen and colleagues evaluated 29,134 cases covering 246 procedures (including various surgical specialties) and found that overall involving, cases involving a resident consisted of significantly longer operative times.29 Orthopedic specific studies agree with these findings.8,15,20,30 Beletsky et al. retrospectively assessed the impact of resident participation during common sports medicine procedures. This study reported that resident participation was on average 15 minutes longer compared to the attending only cases (p<0.01).13 Haughom et al. determined that in primary THA, resident involvement significantly increased operative time.15 Similarly, resident participation was associated with increased operative time during primary TKA.15 However, even after multivariate regression analysis, these studies reported no difference in risk of complications associated with resident involvement.
Multiple studies have demonstrated the impact of operative length and postoperative complications. Duchman et al. recently investigated how the length operative time impacts postoperative complications. By utilizing the NSQIP database, they reported that an operative time consisting more than 120 minutes was an independent predictor of any complication, including wound complications. Additionally, multi-variate analysis showed that a subsequent increase of operative time by 30-minutes, beyond 120 minutes, significantly added additional risk of complications.4 The previously mentioned studies investigating resident involvement in primary TKA and THA procedures demonstrated with sub-analysis, that increased operative time increased the risk for postoperative complications.
Prior studies have conflicting information regarding the impact of resident participation in LOS. Recently, Perfetti et al. determined that academic teaching departments had 10% shorter LOS (p<0.001) compared to non-academy centers for elective lumbar laminectomy and discectomy for degenerative lumbar conditions.31 However, Nandyala et al. noted a significantly longer LOS for elective lumbar spine surgery at academic teaching institutions.32 However, the previously mentioned studies have established that resident participation during primary THA or TKA do not have a significant impact on LOS.8,15 Contrary to these previous studies findings, the current study demonstrated that rTKA cases involving a resident consisted of longer LOS. However, this was by only ~17 hours, limiting the significance of these findings. Additionally, our increased LOS might be due to additional factors, including increased operative time, which has been previously correlated with increased LOS.33
There are limitations that must be considered when interpreting the findings of the study. First, the retrospective nature of the study limits causal conclusions and only associations can be ascertained. Second, the NSQIP database is limited to 30-day postoperative complications; therefore, we were unable to assess complications that occur past this time point. Third, NSQIP does not collect relevant orthopedic information such as radiographic findings, type of implants used in primary TKA, type of implants used for rTKA, chronicity of symptoms, or patient reported outcome measures that may play an important role for postoperative complications. Fourth, NSQIP does not detail the extent of resident participation during the surgery and only reports whether a resident was listed during the case. Additionally, stratification of resident by year in residency was not available for all years. Therefore, associations between year of residency and 30-day complications was not studied. Lastly, NSQIP is the largest available database with information regarding resident participation during operative procedures. Therefore, the lack of short-term complications for the resident involved cohort may be secondary to a type II error.
Conclusion
Resident involvement in rTKA cases is not associated with an increased risk of 30-day postoperative complications. However, resident operative involvement was associated with longer operative time and length of hospital stay.
References
- 1.Kurtz SM, Ong KL, Schmier J, et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;3(89 Suppl):144–151. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 2.Nahhas CR, Yi PH, Culvern C, et al. Patient Attitudes Toward Resident and Fellow Participation in Orthopedic Surgery. J Arthroplasty. 2019;34(9):1884–1888. doi: 10.1016/j.arth.2019.04.035. e1885. [DOI] [PubMed] [Google Scholar]
- 3.Wascher DC. Editorial Commentary: Resident Education: At What Cost? Arthroscopy. 2020;36(3):844. doi: 10.1016/j.arthro.2019.11.102. [DOI] [PubMed] [Google Scholar]
- 4.Duchman KR, Pugely AJ, Martin CT, Gao Y, Bedard NA, Callaghan JJ. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J Arthroplasty. 2017;32(4):1285–1291. doi: 10.1016/j.arth.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Belmont PJ, Jr., Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20–26. doi: 10.2106/JBJS.M.00018. [DOI] [PubMed] [Google Scholar]
- 6.Bohl DD, Ondeck NT, Darrith B, Hannon CP, Fillingham YA, Della Valle CJ. Impact of Operative Time on Adverse Events Following Primary Total Joint Arthroplasty. J Arthroplasty. 2018;33(7):2256–2262. doi: 10.1016/j.arth.2018.02.037. e2254. [DOI] [PubMed] [Google Scholar]
- 7.Owens J, Otero JE, Noiseux NO, Springer BD, Martin JR. Risk Factors for Post-Operative Blood Transfusion Following Total Knee Arthroplasty. Iowa Orthop J. 2020;40(1):69–73. [PMC free article] [PubMed] [Google Scholar]
- 8.Haughom BD, Schairer WW, Hellman MD, Yi PH, Levine BR. Resident involvement does not influence complication after total hip arthroplasty: an analysis of 13,109 cases. J Arthroplasty. 2014;29(10):1919–1924. doi: 10.1016/j.arth.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Khazi ZM, Gulbrandsen TR, Shamrock AG, et al. Resident Involvement Is Not Associated With Increased Risk of Postoperative Complications After Arthroscopic Knee Surgery: A Propensity-Matched Study. Arthroscopy. 2020;36(10):2689–2695. doi: 10.1016/j.arthro.2020.04.040. [DOI] [PubMed] [Google Scholar]
- 10.Gulbrandsen TR, Khazi ZM, Shamrock AG, et al. The Impact of Resident Involvement on Postoperative Complications After Shoulder Arthroscopy: A Propensity-Matched Analysis. J Am Acad Orthop Surg Glob Res Rev. 2020;4(9):e2000138. doi: 10.5435/JAAOSGlobal-D-20-00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cvetanovich GL, Schairer WW, Haughom BD, Nicholson GP, Romeo AA. Does resident involvement have an impact on postoperative complications after total shoulder arthroplasty? An analysis of 1382 cases. J Shoulder Elbow Surg. 2015;24(10):1567–1573. doi: 10.1016/j.jse.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 12.Basques BA, Saltzman BM, Mayer EN, et al. Resident Involvement in Shoulder Arthroscopy Is Not Associated With Short-term Risk to Patients. Orthop J Sports Med. 2018;6(12):2325967118816293. doi: 10.1177/2325967118816293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beletsky A, Lu Y, Manderle BJ, et al. Quantifying the Opportunity Cost of Resident Involvement in Academic Orthopaedic Sports Medicine: A Matched-Pair Analysis. Arthroscopy. 2020;36(3):834–841. doi: 10.1016/j.arthro.2019.09.032. [DOI] [PubMed] [Google Scholar]
- 14.Edelstein AI, Lovecchio FC, Saha S, Hsu WK, Kim JY. Impact of Resident Involvement on Orthopaedic Surgery Outcomes: An Analysis of 30,628 Patients from the American College of Surgeons National Surgical Quality Improvement Program Database. J Bone Joint Surg Am. 2014;96(15):e131. doi: 10.2106/JBJS.M.00660. [DOI] [PubMed] [Google Scholar]
- 15.Haughom BD, Schairer WW, Hellman MD, Yi PH, Levine BR. Does resident involvement impact post-operative complications following primary total knee arthroplasty? An analysis of 24,529 cases. J Arthroplasty. 2014;29(7):1468–1472. doi: 10.1016/j.arth.2014.02.036. e1462. [DOI] [PubMed] [Google Scholar]
- 16.Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database, Registry Research. in Orthopaedic Surgery: Part 2: Clinical Registry Data. J Bone Joint Surg Am. 2015;97(21):1799–1808. doi: 10.2106/JBJS.O.00134. [DOI] [PubMed] [Google Scholar]
- 17.Karhade AV, Larsen AMG, Cote DJ, Dubois HM, Smith TR. National Databases for Neurosurgical Outcomes Research: Options, Strengths, and Limitations. Neurosurgery. 2018;83(3):333–344. doi: 10.1093/neuros/nyx408. [DOI] [PubMed] [Google Scholar]
- 18.Khazi ZM, Gulbrandsen TR, Shamrock AG, et al. Resident Involvement Is Not Associated With Increased Risk of Postoperative Complications After Arthroscopic Knee Surgery: A Propensity-Matched Study. Arthroscopy. 2020. [DOI] [PubMed]
- 19.Lebedeva K, Bryant D, Docter S, Litchfield RB, Getgood A, Degen RM. The Impact of Resident Involvement on Surgical Outcomes following Anterior Cruciate Ligament Reconstruction. J Knee Surg. 2019. [DOI] [PubMed]
- 20.Phan K, Phan P, Stratton A, Kingwell S, Hoda M, Wai E. Impact of resident involvement on cervical and lumbar spine surgery outcomes. Spine J. 2019;19(12):1905–1910. doi: 10.1016/j.spinee.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Zhu WY, Beletsky A, Kordahi A, et al. The Cost to Attending Surgeons of Resident Involvement in Academic Hand Surgery. Ann Plast Surg. 2019;82(5S Suppl 4):S285–S288. doi: 10.1097/SAP.0000000000001873. [DOI] [PubMed] [Google Scholar]
- 22.Acheampong DO, Paul P, Guerrier S, Boateng P, Leitman IM. Effect of Resident Involvement on Morbidity and Mortality Following Thoracic Endovascular Aortic Repair. J Surg Educ. 2018;75(6):1575–1582. doi: 10.1016/j.jsurg.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 23.Nocera NF, Pyfer BJ, De La Cruz LM, Chatterjee A, Thiruchelvam PT, Fisher CS. NSQIP Analysis of Axillary Lymph Node Dissection Rates for Breast Cancer: Implications for Resident and Fellow Participation. J Surg Educ. 2018;75(5):1281–1286. doi: 10.1016/j.jsurg.2018.02.020. [DOI] [PubMed] [Google Scholar]
- 24.Haskins IN, Kudsi J, Hayes K, Amdur RL, Lin PP, Vaziri K. The effect of resident involvement on bariatric surgical outcomes: an ACS-NSQIP analysis. J Surg Res. 2018;223:224–229. doi: 10.1016/j.jss.2017.11.038. [DOI] [PubMed] [Google Scholar]
- 25.Massenburg BB, Sanati-Mehrizy P, Jablonka EM, Taub PJ. The Impact of Resident Participation in Outpatient Plastic Surgical Procedures. Aesthetic Plast Surg. 2016;40(4):584–591. doi: 10.1007/s00266-016-0651-8. [DOI] [PubMed] [Google Scholar]
- 26.Bozic KJ, Kamath AF, Ong K, et al. Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin Orthop Relat Res. 2015;473(6):2131–2138. doi: 10.1007/s11999-014-4078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for M, Medicaid Services HHS. Medicare Program: Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs. Final rule with comment period. Fed Regist. 2017;82(239):59216–59494. [PubMed] [Google Scholar]
- 28.Hall MJ, Ostergaard PJ, Dowlatshahi AS, Harper CM, Earp BE, Rozental TD. The Impact of Obesity and Smoking on Outcomes After Volar Plate Fixation of Distal Radius Fractures. J Hand Surg Am. 2019;44(12):1037–1049. doi: 10.1016/j.jhsa.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 29.Allen RW, Pruitt M, Taaffe KM. Effect of Resident Involvement on Operative Time and Operating Room Staffing Costs. J Surg Educ. 2016;73(6):979–985. doi: 10.1016/j.jsurg.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 30.Prat D, Maoz O, Myerson CL, Zabtani A, Afek A, Tenenbaum S. Orthopaedic residents’ autonomy in hip fracture surgery: what is the effect on patient outcomes? Arch Orthop Trauma Surg. 2021. [DOI] [PubMed]
- 31.Perfetti DC, Job AV, Satin AM, Katz AD, Silber JS, Essig DA. Is academic department teaching status associated with adverse outcomes after lumbar laminectomy and discectomy for degenerative spine diseases? Spine J. 2020. [DOI] [PubMed]
- 32.Nandyala SV, Marquez-Lara A, Fineberg SJ, Hassanzadeh H, Singh K. Complications after lumbar spine surgery between teaching and nonteaching hospitals. Spine (Phila Pa 1976) 2014;39(5):417–423. doi: 10.1097/BRS.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 33.Garbarino LJ, Gold PA, Sodhi N, et al. The effect of operative time on in-hospital length of stay in revision total knee arthroplasty. Ann Transl Med. 2019;7(4):66. doi: 10.21037/atm.2019.01.54. [DOI] [PMC free article] [PubMed] [Google Scholar]


