Abstract
Background
Ankle osteoarthritis (AO) is often secondary to prior trauma and frequently presents with joint deformity. Total ankle replacement (TAR) has been shown as a viable surgical option to reduce pain, improve function, and preserve ankle joint range of motion. The standard TAR uses an anterior approach, but recently a lateral trans-fibular approach has been developed. Our aim was to determine if the lateral TAR was able to correct alignment and improve patient reported outcomes (PROs) in patients with end-stage AO.
Methods
This IRB-approved, retrospective comparative study included 14 consecutive patients that underwent lateral trans-fibular approach TAR for end-stage AO. All patients had received pre-and post-operative WBCT imaging on the affected foot and ankle. Using multiplanar reconstruction of WBCT images, measures of coronal and sagittal plane ankle alignment: Foot and Ankle Offset (FAO), Talar Tilt Angle (TTA), Hindfoot Moment Arm (HMA), and Lateral Talar Station (LTS) were performed. PROs were collected pre- and postoperatively at the latest clinical follow-up.
Results
All patients demonstrated a significant deformity correction in all measurements performed: FAO (7.73%-3.63%, p=0.031), HMA (10.93mm – 5.10mm, p=0.037), TTA (7.9o-1.5o, p=0.003), and LTS (5.25mm-2.83mm, p=0.018). Four of the PROs measured exhibited significant improvement postoperatively, the Tampa Scale for Kinesiophobia (TSK) (42.7-34.5, p=0.012), PRO-MIS Global Physical Health (46.1-54.5, p=0.011), EFAS (5-10.3, p=0.004), and FAAM Daily Living (60.5-79.7, p=0.04). Multivariate analysis assessing the influence of deformity correction in the improvements of PROs found that PROMIS Global Physical Health was significantly associated with improvements in FAO and LTS, TSK associated with HMA, and FAAM Daily Living with FAO and TTA (p<0.05).
Conclusion
The results of this retrospective comparative cohort study suggest that the lateral trans-fibular TAR can correct different aspects of AO deformity. The method also impacted PROs, particularly TSK, PROMIS Global Physical Health, EFAS, and FAAM Daily Living. Direct correlation between some of the deformity correction measurements and the significantly improved PROs was found. The obtained data could help surgeons when making treatment decisions and be the base for comparative prospective studies.
Level of Evidence: III
Keywords: ankle osteoarthritis, arthritis, deformity, total ankle replacement, weigh-bearing computed tomography, foot and ankle offset, talar station
Introduction
Ankle osteoarthritis (OA) is a frequent, debilitating condition that can dramatically reduce patient’s function and quality of life.1 Different from other joints, ankle arthritis is usually posttraumatic, which often adds a deformity component to the condition. Rotational ankle fractures or sprains are known to cause secondary osteoarthritis in patients of all ages.2 Surgical intervention is often required for moderate to severe cases in attempt to reduce pain and improve mobility when non-operative treatment fails.3
Total ankle replacement (TAR) has been advocated with the idea of reducing pain and maintaining motion in patients with end-stage AO. Surgical techniques and implant evolutions during the last decades have significantly improved TAR short and long-term results.4,5 Several authors have also described the capacity of TAR in correcting malalignment, a characteristic previously only associated with ankle arthrodesis.6,7
Standard TAR technique uses an anterior approach to access and prepare the joint, correct deformities, and insert the prosthesis. The anterior approach allows for adequate rebalancing of soft-tissue structures in the medial and lateral aspects of the ankle; however, correction of major coronal plane and sagittal plane deformities in particular can be challenging.8,9 The alternative lateral trans-fibular approach TAR has the theorical advantages of allowing better correction of major coronal plane and sagittal plane deformities.10 This is done by providing direct visualization of the center of rotation of the ankle joint, access to the frequently contracted posterior joint capsule, and most importantly by removing the rigid lateral strut by means of the needed fibular osteotomy.11 This technique also has the added benefit of being able to lengthen and shorten the fibula to further correct the overall ankle deformity.10 Still, this relatively new technique has not been fully tested in its ability to correct overall alignment and deformity aspects.9
Weight bearing computed tomography (WBCT), an imaging method that properly evaluates foot and ankle anatomical disposition under physiological standing load,12-14 has been utilized previously to portray deformity correction and complications of residual deformity following TAR.8,15 The foot and ankle offset (FAO) is an established WBCT three-dimensional, biometric measurement that gauges the overall balance and alignment between the ankle joint and the foot tripod.16,17 FAO has been used in several previous studies to assess a multitude of different, complex foot and ankle deformities, demonstrating extremely high reliability when characterizing 3D alignment.18-22
The primary objective of this study was to use WBCT measurements to assess the lateral trans-fibular approach TAR’s ability to correct coronal and sagittal plane ankle deformity. Secondly, our aim was to report the technique’s ability to improve patient reported outcomes (PROs). Our main hypothesis was that lateral trans-fibular TAR would allow for significant correction of sagittal and coronal plane deformities, and that the corrections would be associated with improvement of PROs.
Methods
Study Design and Subjects
This retrospective comparative study received institutional review board approval (IRB# 201912144) and complied with the Health Insurance Portability Accountability Act (HIPAA) and the Declaration of Helsinki. Inclusion criteria consisted of adult patients (more than 18 years of age) that underwent lateral trans-fibular approach TAR for end-stage ankle OA, with at least 5° of coronal and/or sagittal plane deformity, and that underwent preoperative and postoperative WBCT. Exclusion criteria included patients that underwent anterior ankle approach TAR, patients without ankle deformity in the coronal or sagittal planes, and patients with less than 9 months of clinical follow-up. PROs data was collected preoperatively and on the last post-operative visit. This study included a total of 14 ankles (5 right, 9 left) in 14 patients (7 male, 7 female). The average age and BMI were 63.9 years (range 43-83) and 32.7 kg/m2 (standard deviation, 7.5), respectively. All included patients signed a written informed consent.
Conventional Surgical Procedure
All surgical procedures were performed by a single fellowship-trained foot and ankle orthopedic surgeon with more than 10 years of experience. All patients received the Zimmer-Biomet® (Warsaw, Indiana, US) Trabecular Metal™ TAR (Figure 1).
Figure 1.
Summarized lateral trans-fibular Total Ankle Replacement technical sequence. After anesthesia, the patient is positioned supine with an ipsilateral bump to place the ankle in neutral rotation (A). The incision is marked at the fibular posterior edge aiming distally to the fourth ray (B). Fibular osteotomy is carried 1.5cm proximally to the ankle joint and its distal fragment rotated inferiorly and provisionally fixated to the calcaneus with a Kirschner wire (C). Posterior and anterior capsules are released. The frame is positioned in relation to the limb, placing the foot in 15 degrees of internal rotation (D). A Schanz pin is introduced on the calcaneal tuberosity and, by placing medial or lateral forces, the coronal position of the talus to the tibia is corrected (E). Talar rotation is adjusted using the same calcaneal pin, and another Schanz pin is placed on the talar body (F) from medial to lateral (G). Proximal alignment is secured by placing the outer stem centered on the lateral tibial spine (H). The hole alignment is again checked, and the tibia is fixed to the frame with two Schanz pins (I). Sizing is determined (J) and confirmed after first drilling the talus (K). Coupled arch drilling of the tibia and talus is performed (L), and the rails trials are positioned (M). After establishing proper rail and implant positioning on the anteroposterior (N) and lateral (O) views, rails are drilled. Final trials are placed, sagittal and coronal stability are checked clinically and radiographically, and the proper polyethylene size is determined. The final implant is introduced (P), and the final positioning is checked on the anteroposterior (Q) and lateral (R) views. The fibula is reduced, necessary lengthening or shortening is performed (when applied), and plate osteosynthesis is executed (S).
Patients were positioned supine on the operating table with a tourniquet on the ipsilateral upper thigh. A long approach was performed longitudinally in the lateral aspect of the ankle joint, immediately posterior to the distal fibula. The incision was curved and extended distally towards the sinus tarsi. A long oblique fibular osteotomy was then performed using an oscillating saw and constant saline irrigation, with the osteotomy line ending 1.5-2cm proximal to the ankle joint level. The fibular fragment was then provisionally fixed into the lateral aspect of the heel and into the calcaneal tuberosity with a 0.062 K-wire.
The pre-assembled correcting frame was brought into the field. A calcaneus pin was then inserted, transfixing the calcaneal tuberosity from medial to lateral. Once inserted, the calcaneal pin was grabbed by two pin hooks that were used to provide asymmetric traction, medially to correct varus deformity and laterally to correct valgus deformity. This was done until the talar dome was found to be parallel to the transverse horizontal bar/probe under fluoroscopic evaluation. With the coronal plane articular deformity corrected, a second pin was then inserted into the medial aspect of the talar neck under fluoroscopic guidance.
Anterior or posterior displacements of the tibia were corrected by applying manual or pin traction to the distal tibia. Once adequate correction was achieved, the tibia was fixed into the frame by two additional pins. The probe was then utilized to check the position and curvature needed for an adequate cut. Once positioned, burring of the arthritic surfaces of the talus and the distal tibia was performed. Rail hole drill guides were then inserted and the position was checked under fluoroscopy to ensure appropriate alignment of the implants and adequate contact with the bone surfaces. Implant trials were inserted in the joint to assess for soft tissue tensioning, particularly deltoid ligament stability. Based on that, the thickness of the polyethylene was chosen. The definitive implants were then inserted, first the talar component followed by the tibial component, laterally to medially into the rail holes under press-fit. Range of motion was assessed again. Achilles’ tendon lengthening was considered when less than 10 degrees of dorsiflexion was achieved with the knee in full extension. Lengthening or shortening of the fibula was performed based on fluoroscopic guidance and the amount of coronal plane deformity corrected. A lateral ligament reconstruction was performed with a soft-tissue anchor, reattaching the anterior talofibular ligament. Syndesmotic stability was checked and trans-syndesmotic fixation with suture buttons were performed when necessary. Postoperatively, patients were non-weightbearing in the splint for two weeks. Range of motion exercises and aggressive protocol of standing, deep knee bends were started at two weeks. Progressive weightbearing was initiated in a walking boot at 6-weeks. At 3-months, patients were transitioned out of the boot into protective sneakers and a hinged ankle brace. After 4-5 months, patients were weaned off the brace.
WBCT Measurements
WBCT scans were performed with a cone-beam CT low-extremity scanner (HiRise; CurveBeam, LLC, Warrington, PA, USA). Participants were instructed to bear weight normally and equally between the lower limbs, with feet shoulder width apart.23 Raw, multiplanar, de-identified data was converted into sagittal, coronal, and axial plane images and evaluated using dedicated software (CubeVue™, CurveBeam®, LLC, Warrington, PA, USA). Measurements were performed by a single fellowship-trained foot and ankle orthopedic surgeon.
FAO was used to represent a measurement of three-dimensional deformity and was calculated using dedicated software (TALAS™, CubeVue™). Four points were manually marked, three on the weight bearing tripod of the foot and ankle (the first metatarsal head most plantar voxel, the fifth metatarsal head most plantar voxel, the calcaneal tuberosity most plantar voxel) and one at the center of the ankle joint (most proximal and central point of the talar dome).18,23,24 FAO was then automatically calculated as a percentage by computing the amount of deviation from the center of the ankle joint to the bisecting line of the foot tripod. Physiological alignment (2 standard deviations) was determined to be from - 0.6% to 5.2%.17,23
For assessment of sagittal plane deformity, lateral talar station (LTS) was obtained using sagittal plane WBCT views. LTS was performed by drawing three circles, one on the tibia 10cm above the plafond, one on the tibia 5cm above the plafond, and the final circle fitting over talar dome configuration. A line connecting the center of the circles in the tibia is drawn and the distance from this sagittal line to the center of the talus circle is measured, portraying the LTS. The determined normal established range (2 standard deviations) was from −0.8076 mm to 3.1496 mm.25
To measure deformity in the coronal plane, Hindfoot Moment Arm (HMA) and Talar Tilt Angle (TTA) were calculated. HMA was calculated by first marking the axis of the distal tibia, which is found by measuring the midpoints of the tibial shaft at 5cm and 10cm proximal to the ankle joint line. The weight bearing point of the calcaneal tuberosity was then found and the distance between that point and the axis line of the distal tibia was measured in millimeters. Normal mean values were described as 6.1mm ± 13.6.26,27 TTA was measured by tracing two lines, one tangent to the distal tibia articular surface and one tangent to the articular line of the talar dome. Normality was set as 0.0 ± 0.0.28 Examples of the measurements performed are presented in Figure 2.
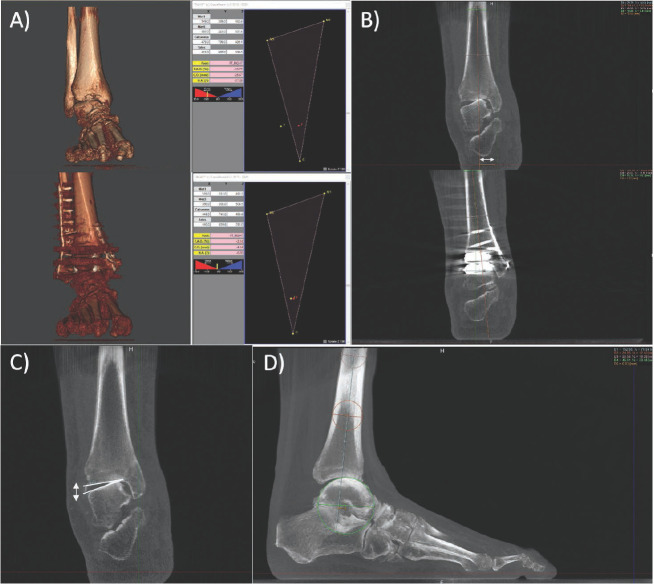
Figure 2.
Section A shows an example of a FAO measurement pre/post-surgery. Section B shows an example of a HMA measurement pre/post-surgery. Sections C and D shows an example of a pre surgery measurement for TTA and LTS, respectively.
Patient Reported Outcomes (PROs)
Functional outcomes were prospectively gathered for patients preoperatively and at their latest follow-up. We assessed the PROMIS Global Physical Health score, the Tampa Scale of Kinesiophobia (TSK), the European Foot and Ankle Society (EFAS) score, the Pain Catastrophizing Scale (PCS), the Foot and Ankle Ability Measure (FAAM) Daily Living Score, and the FAAM Sports Score.29-33
Statistical Analysis
Measurements were assessed for normality by the Shapiro-Wilk test. One-way ANOVA and Wilcoxon tests were used for comparison among timeframes. A multivariate regression analysis was then performed to evaluate the influence of the improvements in deformity correction with the improvements of PROs. R2 values were utilized as measures of association/correlation. Statistical significance was established for p values under 0.05. The JMP Pro 15 Software was used for statistical analysis.
Results
The average follow-up time was 16.1 months (range, 11 to 24 months). A significant amount of deformity correction was observed in the coronal and sagittal planes, and three-dimensionally as well. Regarding 3D measurements, the mean FAO improved from 7.73% to 3.63%, with a mean improvement of 4.1% (95% CI, 0.41 to 7.8; p=0.031). In the coronal plane, the mean HMA decreased from 10.93mm to 5.10mm, with a mean difference of 5.8mm (95% CI, 0.4 to 11.3mm; p=0.037). The mean TTA decreased from 7.9 degrees to 1.5 degrees, with a mean difference of 6.5 degrees (95% CI, 2.4 to 10.6 degrees; p=0.003). Finally, in the sagittal plane the average LTS improved from 5.25mm to 2.83mm with a mean difference of 2.42mm (95% CI, 0.45 to 4.4mm; p=0.018). Graphical plots of the comparison between preoperative and postoperative alignment measurements are presented in Figure 3.
Figure 3.
Average pre-operative vs. post-operative measurements with 95% confidence interval outlines and p-values for FAO (A), HMA (B), TTA (C), and LTS (D).
When considering improvement in PROs following surgery, at the latest follow-up, significant changes were seen on the following scores: PROMIS Global Physical Health improved from 46.1 to 54.5, with a mean improvement of 8.46 (95% CI, 2.2 to 14.7; p=0.011); TSK improved from 42.7 to 34.5, with a mean improvement of 8.2 (95% CI, 2.1 to 14.4; p=0.012); the mean EFAS score improved from 5 to 10.3, with a mean difference of 5.3 (95% CI, 1.9 to 8.6; p=0.004); lastly, the FAAM Daily Living Score improved from 60.5 to 79.7, with a mean difference of 19.2 (95% CI, 0.2 to 38.2; p=0.048). No significant changes were observed for the PCS (11.4 to 3.9, p=0.09) or FAAM Sports (36.15 to 52.9, p=0.23). Graphical plots of the comparison between preoperative and postoperative PROs are presented in Figure 4, along with 95% confidence intervals in Table 1.
Figure 4.
Graphical Plots of Patient Reported outcomes with 95% CI outlines. The averages of the specific measurements are included along with p-values.
Table 1.
Patient Reported Outcome Measures Pre/post Operation
| PRO Survey | PGPH | TSK | PCS | EFAS | FAAM Daily Living | FAAM Sports |
|---|---|---|---|---|---|---|
| Pre-Op Mean | 46.1 | 42.7 | 11.4 | 5 | 60.5 | 36.1 |
| Pre-Op 95% CI | 41-51 | 37.72- 47.61 | 4.58- 18.31 | 2.35- 7.65 | 45.43- 75.65 | 13.9158.41 |
| Post-Op Mean | 54.5 | 34.5 | 3.9 | 10.3 | 79.7 | 52.9 |
| Post-Op 95% CI | 50.65- 58.46 | 30.80- 38.105 | (-)2.031- 9.86 | 8.22- 12.28 | 68.2- 91.28 | 35.1470.64 |
Mean Values and 95% CI are Included. PGPH: PROMIS Global Physical Health.
In the multivariate analysis assessing the influence of deformity correction on the improvement of PROs, the PROMIS Global Physical Health was found to be significantly associated (p=0.0015) with improvements in FAO (p=0.00065) and LTS (p=0.00436), with a R2 of 0.98. Improvements in TSK were significantly associated with changes exclusively in the HMA (p=0.0074), with a R2 of 0.66. The improvements on FAAM Daily Living Score were significantly correlated (p=0.048) with improvements in the FAO (p=0.023) and TTA (p=0.029), with a R2 of 0.78.
Eight out of the 14 patients received a concurrent associated bone alignment surgical procedure on their foot and ankle. The procedures performed with the TAR included first tarsometatarsal joint fusion, cotton osteotomy, medial malleolus prophylactic fixation, peroneal tendon synovectomy, and Achilles’ tendon lengthening. A summary of all associated procedures performed is presented in Table 2.
Table 2.
Associated Procedures to Total Ankle Replacements (TAR)
| Patient | Associated Procedures to TAR | Implant Size | Polyethilene Size |
|---|---|---|---|
| 1 | Bröstrom | 3 | 0 |
| 2 | Bröstrom. Syndesmosis Fixation. LapiCotton. MDCO. | 4 | 0 |
| 3 | Bröstrom | 2 | 2 |
| 4 | Bröstrom. Syndesmosis Fixation. | 6 | 2 |
| 5 | Bröstrom. Syndesmosis Fixation. PB lenghtening. Cotton. MDCO. LCL. | 4 | 4 |
| 6 | Bröstrom | 3 | 0 |
| 7 | Bröstrom | 4 | 2 |
| 8 | Bröstrom. Syndesmosis Fixation. | 4 | 2 |
| 9 | Bröstrom. Protective medial malleolus screw | 4 | 2 |
| 10 | Bröstrom. Medial malleolar fixation with anti-gliding plate | 2 | 0 |
| 11 | Bröstrom. Protective medial malleolus screw. | 5 | 2 |
| 12 | Bröstrom. LapiCotton. | 4 | 2 |
| 13 | Bröstrom. Achilles lengthening. | 3 | 2 |
| 14 | Bröstrom. Achilles lengthening. Fibular lenghtening. | 4 | 2 |
MDCO: medial displacement.
Discussion
In this retrospective comparative study, we evaluated deformity in pre- and post- operative WBCT imaging of patients who underwent lateral approach trans-fibular TAR for end stage OA. Patient reported outcomes were assessed and correlated with the deformity correction. All measurements of deformity were found to be significantly improved and some of the PROs were significantly improved. An association was found between these improved PROs and our deformity correction measurements. These findings confirm our hypothesis.
Early studies of the lateral approach TAR have reported safe and effective surgical technique, reliable implant, and positive initial outcomes.10,11,34-36 Usuelli et al. investigated alignment of the lateral approach TAR by measuring the tibial slope (beta angle) on weight bearing radiographs. They compared the slope of anterior approach and lateral approach TARs to a control group. They found that the tibial slopes of the lateral approach TAR, on average, were more similar to the anatomic tibial slope measured in normal ankles.37 The authors also found a mean alpha angle (medial distal tibial angle) of 89.3 degrees. Usuelli et al., in a large series, reported a sagittal alignment on the lateral group of 35.1%, an alpha angle of 2.7 degrees, and a HMA of 4.8mm on the 24th week follow-up.38 They also noticed an increase in valgus position of the hindfoot over the temporal course.38 DeVries et al. used the lateral distal tibial angle (LDTA) and anterior distal tibial angle (ADTA) to measure changes in deformity and alignment when using the lateral approach. They had 11 patients for a 12 month follow up with weight bearing radiograph imaging, and found significant improvement in both LDTA (91.8 to 90.5) and ADTA (84.6 to 85.7) measures. Using Magnetic Resonance Imaging (MRI) with a metal artifact reduction software, de Cesar Netto et al. showed a mean TLS of 0.22mm in lateral approached TAR.39 We did not measure the lateral slope (beta angle) or the MDTA/ADTA in our study, but our mean TTA, a coronal plane alignment representation, was 1.5 degrees (complementary: 88.5), our mean HMA was 5.10mm, and mean TTS was 2.83mm. These results were consistent with the balance the other authors exhibited. These findings may support evidence that the lateral approach trans-fibular TAR can significantly correct coronal and sagittal alignment.40
Mosca et al. compared PROs from patients undergoing lateral total ankle replacement and found significant improvement in American Orthopaedic Foot and Ankle Society score (AOFAS) (45 to 91.8), the 36-Item Short-Form survey (SF36) (62.5 to 88.9), and the Visual Analogue Scale (VAS) (8.2 to 1.2).41 Usuelli et al., in a minimal 2 years follow-up, demonstrated a mean VAS of 1.43, a mean 86.82 for the AOFAS, a 12-Item Short-Form survey (SF12) with a mean Physical Component Summary (PCS) of 46.25, and a mean Mental Component Summary (MCS) of 53.12.42 In a 12-month period, Bianchi et al. showed improvement in the FFI-pain (53.67 to 16.95), in the FFI-disability (64.19 to 20.76), in the VAS (7.81 to 2.29), and in the AOFAS (40.95 to 86.38).43 Barg et al., in a series of 55 patients undergoing lateral TAR with a high number of concomitant procedures and a 24-month minimal clinical follow-up, also demonstrated good functional results.44 Improvement on VAS (7.9 to 0.8), PROMIS physical (37.0 to 48.1), and PROMIS pain (65.4 to 54.9) were reported.44 Our functional results were in line with what was previously published, although it is difficult to compare different outcome measures. We were able to show significant (ps<0.048) changes in PROMIS Global Physical Health (46.1 to 54.5), TSK (42.7 to 34.5), EFAS (5 to 10.3), and FAAM Daily Living (60.5 to 79.7), but not for the PCS (11.4 to 3.9, p=0.09) or FAAM Sports (36.15 to 52.9, p=0.23).
Our study adds to this body of evidence by providing measures of FAO improvement, a three-dimensional assessment of foot and ankle alignment. The only study that made this assessment was performed by Lintz et al., who performed a comparison between this three-dimensional tool and cystic formation after anterior TAR.8 Values in FAO below -2.75% and above 4.5% were associated with a higher cyst volume. The mean FAO presented by our study, 3.63%, remained on the safe range proposed by Lintz et al., which could explain the improvement and correlation of this measurement with the PROs we demonstrated. Many studies found relations between preoperative malignment and postsurgical results, but few made associations among postoperative alignment and postoperative outcomes.45,46 When analyzing anterior TARs, Nielson et al. did not find associations between postoperative sagittal balance and short-term functional outcomes.47 Johnson-Lynn et al. were able to find association among a coronal plane alignment value, the MDTA, Foot and Ankle Outcome Score, and AOFAS scale.48 Our study was the first to describe positive relations between improvement in three-dimensional measurements and PROs, supporting the idea that these two entities are related. We could also demonstrate that 98% of changes in PROMIS Global Physical Health were explained by improvements in FAO and LTS. TSK rises were 66% explained by HMA. 78% of the enhancements in FAAM Daily Living Score were attributed to FAO and TTA improving. This could be a brief representation of the lateral total ankle replacement’s capacity in correcting deformities that might be translated into clinical results.
It is important to recognize the weaknesses of this study. First, it was a retrospective study that used clinical and radiographical collected data. The lateral approach TAR was also not compared to other treatments or techniques. We only included certain PROs, which in total could not represent the multitude of patients’ idiosyncrasies. This study did not access complications or the need for follow up surgeries in the long term. Only one reader and one surgeon were responsible for the observations and interventions. We did not present a large sample, which could have contributed to the absence of some correlations between alignment and reported outcomes. Finally, a significant percentage of patients in the study received concurring associated procedures that can confound the correction assessment. On the other hand, adjuvant procedures are performed on most of the performed TAR worldwide and we found statically significant differences in our small sample.
Conclusion
In conclusion, this study showed that the lateral approach trans-fibular TAR can significantly correct ankle deformity in the coronal and sagittal planes in patients presenting with end-stage AO. Clinical benefit was also demonstrated with improvement in multiple PROs during follow up. Additionally, association was found between alignment improvement and functional results. Further prospective and comparative studies are needed to support these results.
References
- 1.Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–6. Epub 2005/08/11. PubMed PMID: 16089071; PubMed Central PMCID: PM-CPMC1888779. [PMC free article] [PubMed] [Google Scholar]
- 2.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–44. doi: 10.1097/01.bot.0000246468.80635.. Epub 2006/11/16. doi: ef. PubMed PMID: 17106388. [DOI] [PubMed] [Google Scholar]
- 3.Nwankwo EC, Jr., Labaran LA, Athas V, Olson S, Adams SB. Pathogenesis of Posttraumatic Osteoarthritis of the Ankle. Orthop Clin North Am. 2019;50(4):529–37. doi: 10.1016/j.ocl.2019.05.008.. Epub 2019/08/31. doi: PubMed PMID: 31466668. [DOI] [PubMed] [Google Scholar]
- 4.Veljkovic AN, Daniels TR, Glazebrook MA, Dryden PJ, Penner MJ, Wing KJ, et al. Outcomes of Total Ankle Replacement, Arthroscopic Ankle Arthrodesis, and Open Ankle Arthrodesis for Isolated Non-Deformed End-Stage Ankle Arthritis. J Bone Joint Surg Am. 2019;101(17):1523–9. doi: 10.2106/JBJS.18.01012.. Epub 2019/09/05. doi: PubMed PMID: 31483394. [DOI] [PubMed] [Google Scholar]
- 5.Norvell DC, Ledoux WR, Shofer JB, Hansen ST, Davitt J, Anderson JG, et al. Effectiveness and Safety of Ankle Arthrodesis Versus Arthroplasty: A Prospective Multicenter Study. J Bone Joint Surg Am. 2019;101(16):1485–94. doi: 10.2106/jbjs.18.01257.. Epub 2019/08/23. doi: PubMed PMID: 31436657; PubMed Central PMCID: PMCPMC7001770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piga C, Maccario C, D’Ambrosi R, Romano F, Usuelli FG. Total Ankle Arthroplasty With Valgus Deformity. Foot Ankle Int. 2021;42(7):867–76. doi: 10.1177/1071100720985281.. Epub 2021/02/02. doi: PubMed PMID: 33517787. [DOI] [PubMed] [Google Scholar]
- 7.Saito GH, Sanders AE, de Cesar Netto C, O’Malley MJ, Ellis SJ, Demetracopoulos CA. Short-Term Complications, Reoperations, and Radiographic Outcomes of a New Fixed-Bearing Total Ankle Arthroplasty. Foot Ankle Int. 2018;39(7):787–94. doi: 10.1177/1071100718764107.. Epub 2018/03/29. doi: PubMed PMID: 29589784. [DOI] [PubMed] [Google Scholar]
- 8.Lintz F, Mast J, Bernasconi A, Mehdi N, de Cesar Netto C, Fernando C, et al. 3D, Weight-bearing Topographical Study of Periprosthetic Cysts and Alignment in Total Ankle Replacement. Foot Ankle Int. 2020;41(1):1–9. doi: 10.1177/1071100719891411.. Epub 2019/11/30. doi: PubMed PMID: 31779466. [DOI] [PubMed] [Google Scholar]
- 9.Halai MM, Pinsker E, Mann MA, Daniels TR. Should 15 degrees of valgus coronal-plane deformity be the upper limit for a total ankle arthroplasty? Bone Joint J. 2020;102-B(12):1689–96. doi: 10.1302/0301-620X.102B12.BJJ-2020-0140.R1.. Epub 2020/12/01. doi: PubMed PMID: 33249899. [DOI] [PubMed] [Google Scholar]
- 10.Tan EW, Maccario C, Talusan PG, Schon LC. Early Complications and Secondary Procedures in Transfibular Total Ankle Replacement. Foot Ankle Int. 2016;37(8):835–41. doi: 10.1177/1071100716644817.. Epub 2016/04/22. doi: PubMed PMID: 27098127. [DOI] [PubMed] [Google Scholar]
- 11.Barg A, Bettin CC, Burstein AH, Saltzman CL, Gililland J. Early Clinical and Radiographic Outcomes of Trabecular Metal Total Ankle Replacement Using a Transfibular Approach. J Bone Joint Surg Am. 2018;100(6):505–15. doi: 10.2106/JBJS.17.00018.. Epub 2018/03/21. doi: PubMed PMID: 29557867. [DOI] [PubMed] [Google Scholar]
- 12.Barg A, Bailey T, Richter M, de Cesar Netto C, Lintz F, Burssens A, et al. Weightbearing Computed Tomography of the Foot and Ankle: Emerging Technology Topical Review. Foot Ankle Int. 2018;39(3):376–86. doi: 10.1177/1071100717740330.. Epub 2017/11/25. doi: PubMed PMID: 29171283. [DOI] [PubMed] [Google Scholar]
- 13.Godoy-Santos AL, Cesar CN. Weight-Bearing Ct International Study G. Weight-Bearing Computed Tomography of the Foot and Ankle: An Update and Future Directions. Acta Or-top Bras. 2018;26(2):135–9. doi: 10.1590/1413-785220182602188482.. Epub 2018/07/10. doi: PubMed PMID: 29983632; PubMed Central PMCID: PM-CPMC6032618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lintz F, de Cesar Netto C, Barg A, Burssens A, Richter M. Weight Bearing CTISG. Weight-bearing cone beam CT scans in the foot and ankle. EFORT Open Rev. 2018;3(5):278–86. doi: 10.1302/2058-5241.3.170066.. Epub 2018/06/29. doi: PubMed PMID: 29951267; PubMed Central PMCID: PMCPMC5994636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hintermann B, Susdorf R, Krahenbuhl N, Ruiz R. Axial Rotational Alignment in Mobile-Bearing Total Ankle Arthroplasty. Foot Ankle Int. 2020;41(5):5218. doi: 10.1177/1071100720902838.. Epub 2020/01/31. doi: PubMed PMID: 31996033. [DOI] [PubMed] [Google Scholar]
- 16.Lintz F, Barton T, Millet M, Harries WJ, Hepple S, Winson IG. Ground Reaction Force Calcaneal Offset: A new measurement of hindfoot alignment. Foot Ankle Surg. 2012;18(1):9–14. doi: 10.1016/j.fas.2011.01.003.. Epub 2012/02/14. doi: PubMed PMID: 22325996. [DOI] [PubMed] [Google Scholar]
- 17.Rojas EO, Barbachan Mansur NS, Dibbern K, Lalevee M, Auch E, Schmidt E, et al. Weight-bearing Computed Tomography for Assessment of Foot and Ankle Deformities: The Iowa Experience. Iowa Orthop J. 2021;41(1):111–9. Epub 2021/09/24. PubMed PMID: 34552412; PubMed Central PMCID: PMCPMC8259196. [PMC free article] [PubMed] [Google Scholar]
- 18.de Cesar Netto C, Bernasconi A, Roberts L, Pontin PA, Lintz F, Saito GH, et al. Foot Alignment in Symptomatic National Basketball Association Players Using Weightbearing Cone Beam Computed Tomography. Orthop J Sports Med. 2019;7(2):2325967119826081. doi: 10.1177/2325967119826081.. Epub 2019/03/01. doi: PubMed PMID: 30815498; PubMed Central PMCID: PMCPMC6385333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Cesar Netto C, Shakoor D, Dein EJ, Zhang H, Thawait GK, Richter M, et al. Influence of investigator experience on reliability of adult acquired flatfoot deformity measurements using weight-bearing computed tomography. Foot Ankle Surg. 2019;25(4):495–502. doi: 10.1016/j.fas.2018.03.001.. Epub 2018/10/17. doi: PubMed PMID: 30321961. [DOI] [PubMed] [Google Scholar]
- 20.Bernasconi A, Cooper L, Lyle S, Patel S, Cullen N, Singh D, et al. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg. 2020;26(5):564–72. doi: 10.1016/j.fas.2019.07.005.. Epub 2019/08/06. doi: PubMed PMID: 31378592. [DOI] [PubMed] [Google Scholar]
- 21.Dagneaux L, Dufrenot M, Bernasconi A, Bedard NA, de Cesar Netto C, Lintz F. Three-Dimensional Biometrics to Correlate Hindfoot and Knee Coronal Alignments Using Modern Weightbearing Imaging. Foot Ankle Int. 2020;41(11):1411–8. doi: 10.1177/1071100720938333.. Epub 2020/07/24. doi: PubMed PMID: 32698631. [DOI] [PubMed] [Google Scholar]
- 22.Day J, de Cesar Netto C, Nishikawa DRC, Garfin-kel J, Roney A, JOM M, et al. Three-Dimensional Biometric Weightbearing CT Evaluation of the Operative Treatment of Adult-Acquired Flatfoot Deformity. Foot Ankle Int. 2020;41(8):930–6. doi: 10.1177/1071100720925423.. Epub 2020/06/09. doi: PubMed PMID: 32506953. [DOI] [PubMed] [Google Scholar]
- 23.de Cesar Netto C, Bang K, Mansur NS, Garfin-kel JH, Bernasconi A, Lintz F, et al. Multiplanar Semiautomatic Assessment of Foot and Ankle Offset in Adult Acquired Flatfoot Deformity. Foot Ankle Int. 2020;41(7):839–48. doi: 10.1177/1071100720920274.. Epub 2020/05/23. doi: PubMed PMID: 32441540. [DOI] [PubMed] [Google Scholar]
- 24.Lintz F, Welck M, Bernasconi A, Thornton J, Cullen NP, Singh D, et al. 3D Biometrics for Hindfoot Alignment Using Weightbearing CT. Foot Ankle Int. 2017;38(6):684–9. doi: 10.1177/1071100717690806.. Epub 2017/02/12. doi: PubMed PMID: 28183212. [DOI] [PubMed] [Google Scholar]
- 25.Veljkovic A, Norton A, Salat P, Saltzman C, Femino J, Phisitkul P, et al. Lateral talar station: a clinically reproducible measure of sagittal talar position. Foot Ankle Int. 2013;34(12):1669–76. doi: 10.1177/1071100713500489.. Epub 2013/08/24. doi: PubMed PMID: 23966113. [DOI] [PubMed] [Google Scholar]
- 26.de Cesar Netto C, Schon LC, Thawait GK, da Fonseca LF, Chinanuvathana A, Zbijewski WB, et al. Flexible Adult Acquired Flatfoot Deformity: Comparison Between Weight-Bearing and Non-Weight-Bearing Measurements Using Cone-Beam Computed Tomography. J Bone Joint Surg Am. 2017;99(18):e98. doi: 10.2106/JBJS.16.01366.. Epub 2017/09/20. doi: PubMed PMID: 28926392. [DOI] [PubMed] [Google Scholar]
- 27.Arena CB, Sripanich Y, Leake R, Saltzman CL, Barg A. Assessment of Hindfoot Alignment Comparing Weightbearing Radiography to Weightbearing Computed Tomography. Foot Ankle Int. 2021;42(11):1482–90. doi: 10.1177/10711007211014171.. Epub 2021/06/11. doi: PubMed PMID: 34109833. [DOI] [PubMed] [Google Scholar]
- 28.Wang B, Saltzman CL, Chalayon O, Barg A. Does the subtalar joint compensate for ankle malalignment in end-stage ankle arthritis? Clin Orthop Relat Res. 2015;473(1):318–25. doi: 10.1007/s11999-014-3960-8.. Epub 2014/10/16. doi: PubMed PMID: 25315275; PubMed Central PMCID: PMCPMC4390960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richter M, Agren PH, Besse JL, Cöster M, Kofoed H, Maffulli N, et al. EFAS Score - Multilingual development and validation of a patient-reported outcome measure (PROM) by the score committee of the European Foot and Ankle Society (EFAS). Foot Ankle Surg. 2018;24(3):185–204. doi: 10.1016/j.fas.2018.05.004.. Epub 20180523. doi: PubMed PMID: 29933960. [DOI] [PubMed] [Google Scholar]
- 30.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PRO-MIS) global items. Qual Life Res. 2009;18(7):873–80. doi: 10.1007/s11136-009-9496-9.. Epub 20090619. doi: PubMed PMID: 19543809; PubMed Central PMCID: PMCPMC2724630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin RL, Irrgang JJ, Burdett RG, Con-ti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26(11):968–83. doi: 10.1177/107110070502601113.. doi: PubMed PMID: 16309613. [DOI] [PubMed] [Google Scholar]
- 32.Roelofs J, Goubert L, Peters ML, Vlaeyen JW, Crombez G. The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain. 2004;8(5):495–502. doi: 10.1016/j.ejpain.2003.11.016.. doi: PubMed PMID: 15324781. [DOI] [PubMed] [Google Scholar]
- 33.Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20(6):589–605. doi: 10.1023/a:1025570508954.. doi: PubMed PMID: 9429990. [DOI] [PubMed] [Google Scholar]
- 34.Usuelli FG, D’Ambrosi R, Manzi L, Maccario C, Indino C. Treatment of Ankle Osteoarthritis with Total Ankle Replacement Through a Lateral Transfibular Approach. J Vis Exp. 2018;(131) doi: 10.3791/56396.. Epub 2018/02/15. doi: PubMed PMID: 29443030; PubMed Central PMCID: PMCPMC5908692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Usuelli FG, Indino C, Maccario C, Manzi L, Liuni FM, Vulcano E. Infections in primary total ankle replacement: Anterior approach versus lateral transfibular approach. Foot Ankle Surg. 2019;25(1):19–23. doi: 10.1016/j.fas.2017.07.643.. Epub 2018/02/08. doi: PubMed PMID: 29409263. [DOI] [PubMed] [Google Scholar]
- 36.Bianchi A, Martinelli N, Hosseinzadeh M, Flore J, Minoli C, Malerba F, et al. Early clinical and radiological evaluation in patients with total ankle replacement performed by lateral approach and peroneal osteotomy. BMC Musculoskelet Disord. 2019;20(1):132. doi: 10.1186/s12891-019-2503-6.. Epub 2019/03/29. doi: PubMed PMID: 30917817; PubMed Central PMCID: PMCPMC6437854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Usuelli FG, Maccario C, Indino C, Manzi L, Gross CE. Tibial slope in total ankle arthroplasty: Anterior or lateral approach. Foot Ankle Surg. 2017;23(2):84–8. doi: 10.1016/j.fas.2016.10.001.. Epub 2017/06/06. doi: PubMed PMID: 28578799. [DOI] [PubMed] [Google Scholar]
- 38.Usuelli FG, Maccario C, Indino C, Manzi L, Romano F, Gross CE. Evaluation of Hindfoot Alignment After Fixed- and Mobile-Bearing Total Ankle Prostheses. Foot & Ankle International. 2020;41(3):286–93. doi: 10.1177/1071100719891160.. doi: [DOI] [PubMed] [Google Scholar]
- 39.De Cesar Netto C, Schon LC, Da Fonseca LF, Chinanuvathana A, Stern SE, Fritz J. Metal artifact reduction MRI for total ankle replacement sagittal balance evaluation. Foot and Ankle Surgery. 2019;25(6):739–47. doi: 10.1016/j.fas.2018.09.005.. doi: [DOI] [PubMed] [Google Scholar]
- 40.DeVries JG, Derksen TA, Scharer BM, Limoni R. Perioperative Complications and Initial Alignment of Lateral Approach Total Ankle Arthroplasty. J Foot Ankle Surg. 2017;56(5):996–1000. doi: 10.1053/j.jfas.2017.04.016.. Epub 2017/06/25. doi: PubMed PMID: 28645548. [DOI] [PubMed] [Google Scholar]
- 41.Mosca M, Caravelli S, Vocale E, Maitan N, Grassi A, Massimi S, et al. Clinical-radiological outcomes and complications after total ankle replacement through a lateral transfibular approach: a retrospective evaluation at a mid-term follow-up. Int Orthop. 2021;45(2):437–43. doi: 10.1007/s00264-020-04709-4.. Epub 2020/07/16. doi: PubMed PMID: 32666242. [DOI] [PubMed] [Google Scholar]
- 42.Usuelli FG, Indino C, Maccario C, Manzi L, Romano F, Aiyer A, et al. A Modification of the Fibular Osteotomy for Total Ankle Replacement Through the Lateral Transfibular Approach. J Bone Joint Surg Am. 2019;101(22):2026–35. doi: 10.2106/JBJS.19.00307.. Epub 2019/11/26. doi: PubMed PMID: 31764365. [DOI] [PubMed] [Google Scholar]
- 43.Bianchi A, Martinelli N, Hosseinzadeh M, Flore J, Minoli C, Malerba F, et al. Early clinical and radiological evaluation in patients with total ankle replacement performed by lateral approach and peroneal osteotomy. BMC Musculoskeletal Disorders. 2019;20(1) doi: 10.1186/s12891-019-2503-6.. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barg A, Bettin CC, Burstein AH, Saltzman CL, Gililland J. Early Clinical and Radiographic Outcomes of Trabecular Metal Total Ankle Replacement Using a Transfibular Approach. JBJS. 2018;100(6):505–15. doi: 10.2106/jbjs.17.00018.. doi: PubMed PMID: 00004623-201803210-00008. [DOI] [PubMed] [Google Scholar]
- 45.Le V, Escudero M, Symes M, Salat P, Wing K, Younger A, et al. Impact of Sagittal Talar Inclination on Total Ankle Replacement Failure. Foot Ankle Int. 2019;40(8):900–4. doi: 10.1177/1071100719847183.. Epub 20190426. doi: PubMed PMID: 31027427. [DOI] [PubMed] [Google Scholar]
- 46.Lee GW, Wang SH, Lee KB. Comparison of Intermediate to Long-Term Outcomes of Total Ankle Arthroplasty in Ankles with Preoperative Varus, Valgus, and Neutral Alignment. J Bone Joint Surg Am. 2018;100(10):835–42. doi: 10.2106/jbjs.17.00703.. doi: PubMed PMID: 29762278. [DOI] [PubMed] [Google Scholar]
- 47.Nielsen NM, Saito GH, Sanders AE, Ellis SJ, Sofka CM, Demetracopoulos CA. Sagittal Tibiotalar Alignment May Not Affect Functional Outcomes in Fixed-Bearing Total Ankle Replacement: A Retrospective Cohort Study. HSS Journal ®. 2020;16(S2):300–4. doi: 10.1007/s11420-019-09728-5.. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson-Lynn S, Siddique M. The Effect of Sagittal and Coronal Balance on Patient-Reported Outcomes Following Mobile-Bearing Total Ankle Replacement. J Foot Ankle Surg. 2019;58(4):663–8. doi: 10.1053/j.jfas.2018.11.007.. Epub 20190406. doi: PubMed PMID: 30962111. [DOI] [PubMed] [Google Scholar]