ABSTRACT
The prevalence of lung disease caused by Mycobacterium abscessus is increasing among patients with cystic fibrosis. M. abscessus is a multidrug resistant opportunistic pathogen that is notoriously difficult to treat due to a lack of efficacious therapeutic regimens. Currently, there are no standard regimens, and treatment guidelines are based empirically on drug susceptibility testing. Thus, novel antibiotics are required. Natural products represent a vast pool of biologically active compounds that have a history of being a good source of antibiotics. Here, we screened a library of 517 natural products purified from fermentations of various bacteria, fungi, and plants against M. abscessus ATCC 19977. Lysobactin and sorangicin A were active against the M. abscessus complex and drug resistant clinical isolates. These natural products merit further consideration to be included in the M. abscessus drug pipeline.
IMPORTANCE The many thousands of people living with cystic fibrosis are at a greater risk of developing a chronic lung infection caused by Mycobacterium abscessus. Since M. abscessus is clinically resistant to most anti-TB drugs available, treatment options are limited to macrolides. Despite macrolide-based therapies, cure rates for M. abscessus lung infections are 50%. Using an in-house library of curated natural products, we identified lysobactin and sorangicin A as novel scaffolds for the future development of antimicrobials for patients with M. abscessus infections.
KEYWORDS: Mycobacterium abscessus, natural products, lysobactin, sorangicin A
INTRODUCTION
Mycobacterium abscessus (M. abscessus) complex consists of three subspecies (M. abscessus subsp. abscessus, M. abscessus subsp. massiliense, M. abscessus subsp. bolletii) that cause disease in immunocompromised and immunocompetent hosts (1–5). Although M. abscessus was first isolated from a knee abscess in 1953, the most common clinical presentation is pulmonary disease in patients with cystic fibrosis (CF), chronic lung disease, or undergoing lung transplantation and is becoming more frequent (6–8). In some instances, extrapulmonary disease can result from dissemination or surgical site infections that lead to skin and soft tissue infections (6, 9).
Clinical management of M. abscessus pulmonary disease is challenged by notoriously drug resistant phenotypes and a lack of effective antimicrobials. M. abscessus is intrinsically resistant to most antitubercular agents used to treat tuberculosis despite having a homolog of the target (10). The treatment for M. abscessus pulmonary disease in a patient with CF includes an intensive phase of an oral macrolide like clarithromycin or azithromycin, intravenous amikacin, and an additional intravenous agent like cefoxitin or imipenem (11). The intensive phase of treatment lasts for up to 3 months depending on the severity of the infection and the tolerability of the regimen. Subsequently, patients continue with the oral macrolide and substitute the injectable agents with oral clofazimine, minocycline, moxifloxacin, and nebulized amikacin for 14 months (11).
Treatment regimens can be further complicated by various susceptibilities among the subspecies where M. abscessus subsp. abscessus and bolletii display inducible resistance to macrolides conferred by the ribosomal methyltransferase encoded by erm(41), resulting in worse treatment outcomes. Comparatively, M. abscessus subsp. massiliense has a truncated erm(41) and higher treatment success rates (12–14). Consequently, the intrinsic resistance mechanisms of the bacteria and the lack of effective antimicrobials against M. abscessus necessitate additional drug discovery efforts to identify novel antimicrobials.
Natural products are a reservoir of genetically encoded microbial metabolites with vast chemical diversity (15, 16). These metabolites have been crafted by evolution to mediate chemical signaling roles and thus, possess the required properties for microbial penetration and an affinity for biological targets (17, 18). Considering that two-thirds of antibiotics used in the clinic are natural products or derived from a natural product scaffold, they are a proven source for antimicrobial discovery (16, 19). Here, we screened an in-house HZI/HIPS library of 517 natural products purified from fermentations of various bacteria (mostly myxobacteria) and fungi against M. abscessus ATCC 19977. We discovered that the cyclic depsipeptide lysobactin (LYB) and the macrolide sorangicin A (SOR) have activity against the reference strain and against a panel of drug resistant clinical isolates from CF patients.
RESULTS
Validation of M. abscessus lux for phenotypic screening.
To identify new antimicrobial agents against the difficult-to-treat pulmonary pathogen M. abscessus, we investigated the feasibility of M. abscessus constitutively expressing luciferase from the luxCDABE operon as a primary screening strain (M. abscessus lux). We showed that expression of luxCDABE did not interfere with the growth kinetics of M. abscessus lux compared to M. abscessus ATCC 19977 by CFU/mL over 72 h, and that luxCDABE provided 1,000-fold more luminescence than background (Fig. 1a). More importantly, luminescence production had a positive correlation (Pearson r2 = 0.9887) with growth kinetics (Fig. 1b). Therefore, we substituted the luminescence readout as a proxy for bacterial growth.
FIG 1.
Validation of luminescence from M. abscessus constitutively expressing lux. (a) M. abscessus 19977 ATCC 19977 was made to constitutively express the luxCDABE operon (M. abscessus lux). Reference strain ATCC 19977 (circles) and M. abscessus lux (squares) were grown in 7H9 complete with CFU/mL (black symbols) and luminescence (purple symbols) measured at 12-h intervals. Data shown is n = 3 with mean ± SD. P-values from 2-way ANOVA with Sidak’s multiple-comparison test. (b) Correlation between luminescence output and bacterial growth measured with Pearson’s correlation coefficient. (c) Z’ Factor measured using OD600nm, resazurin microtiter assay (REMA), and Bactiter Glo readouts on M. abscessus ATCC 19977, and luminescence readout on M. abscessus lux. Data shown is median with 95% CI of n = 3.
Primary screens of chemical libraries often include false positives that later prove to be inactive against the microorganism of interest and thus, incur additional time and resources on screening campaigns. Conversely, compounds with bona fide activity may be missed as false negatives. To limit both scenarios, screening conditions are subjected to a Z’ factor measurement to determine the robustness of a particular readout. We compared the Z’ factor of our M. abscessus lux to three other readouts of bacterial growth, namely: optical density at 600 nm (OD600nm) (20, 21), resazurin microtiter assay (REMA) (22–24), and Bactiter Glo (25, 26). M. abscessus ATCC 19977 and M. abscessus lux were grown until mid-log phase, diluted to OD600nm of 0.005 (5x106 CFU/mL), and incubated with 1% DMSO or 100 μM amikacin in a 96-well plate format for 48 h. We measured the highest Z’ factor of 0.70 (95% CI,0.65 to 0.82) using luminescence from M. abscessus lux while luminescence from the commercial Bactiter Glo kit generated the lowest Z’ factor of 0.51 (95% CI,0.13 to 0.50) (Fig. 1b). Importantly, the reproducibility between Z’ factors was highest with M. abscessus lux as measured by the 95% CI range (M. abscessus lux = 0.17, REMA = 0.23, Bactiter Glo = 0.38, OD = 0.39). The high Z’ factor and its reproducibility for the M. abscessus lux readout gave us confidence to use it in our primary screening assays (Fig. 1c).
Lysobactin and sorangicin A are identified as inhibitors of M. abscessus ATCC 19977 from a natural product library.
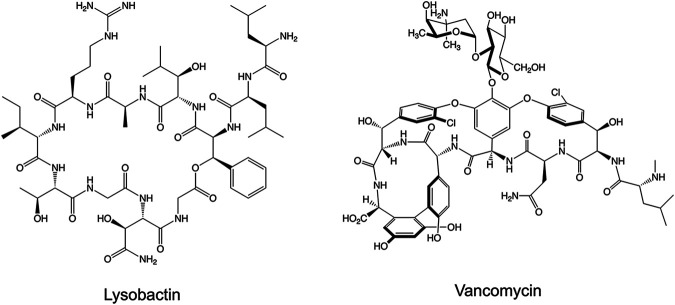
To identify novel antimicrobials against M. abscessus, we carried out a phenotypic screen with an in-house HZI/HIPS library of 517 natural products against M. abscessus lux. The natural products originated from the fermentation of various biological sources, fungi, and myxobacteria. Fermentations were fractionated into single compounds at 1 mM in DMSO. We screened the natural products at 10 μM (1% DMSO) and applied a threshold of 90% and 50% reduction in luminescence compared to drug free controls (1% DMSO). These criteria provided us with compounds with MIC90 and MIC50 ≤10 μM, respectively. The last column of each plate contained drug free wells and 100 μM AMK wells as negative and positive controls, respectively. After screening in duplicate, we identified 12 compounds that met our threshold of 90% loss of viability and 20 compounds at 50% loss of viability at 10 μM (Fig. 2, Table S1). Many of the compounds identified are known DNA intercalators and were flagged as potentially cytotoxic. Telithromycin was omitted through de-replication as it shares a similar mechanism of action to CLR. Two compounds identified with specific targets were LYB (Fig. 3) and SOR (Fig. 4). LYB was a compound of interest since there are currently no lead compounds that target lipid II in the cell wall in the M. abscessus drug pipeline (27). Although traditional cyclic peptides like vancomycin (VAN) do exhibit in vitro activity against M. abscessus (28), VAN is associated with an increased risk ratio for total adverse events, nephrotoxicity, and vancomycin flushing reaction (29). SOR, a known RNA polymerase (RNAP) inhibitor, was a compound of interest since RNAP is a validated drug target in Mycobacterium tuberculosis targeted by the front-line drug rifampicin (RIF) (30). Relatedly, rifabutin (RFB) has been shown to be active against M. abscessus (31, 32), and so SOR could be added to the group of repurposed RNAP inhibitors for M. abscessus.
FIG 2.
Natural product primary screen. A library of 517 natural products was screened against M. abscessus lux at a concentration of 10 μM. Dashed red line indicates 90% luminescence reduction cut off. Natural product library includes 176 compounds fractionated from diverse sources (blue, cyan), 88 compounds fractionated from fungi (green), 253 compounds fractionated from myxobacteria (red, orange, yellow), 1% DMSO as vehicle control (purple), and 100 μM amikacin as positive control (white). Data shown is mean of duplicate screening.
FIG 3.
Structures of nonribosomal peptide synthetase-derived cyclic peptides targeting peptidoglycan biosynthesis.
FIG 4.
Structures of polyketide synthase-derived sorangicin A and semisynthetic rifamycins targeting RNA polymerase.
Lysobactin and sorangicin A maintain activity in different media compositions.
To confirm the activity of LYB and SOR and determine the minimum concentration of each drug that inhibits 90% of bacterial growth (MIC90), fresh LYB and SOR powder was obtained and tested against the M. abscessus ATCC 19977 reference strain. We observed low micromolar dose-response activity for both LYB and SOR as illustrated in Table 1. It was previously shown that some antimycobacterial agents have carbon dependent activities (33). Therefore, we measured the pMIC90 of LYB and SOR for M. abscessus ATCC 19977 grown in traditional Middlebrook 7H9 with glycerol, Middlebrook 7H9 with acetate, and Sauton’s minimal mycobacteria medium with glycerol. Alternatively, from a clinical perspective, the Clinical and Laboratory Standards Institute guidelines recommend M. abscessus drug susceptibility testing in cation-adjusted Mueller-Hinton (CaMH) broth (34). LYB and SOR retained activity across glycerol and acetate as carbon sources, in a minimal media, and in media adjusted for Mg2+ and Ca2+ (Table 1, Table S2).
TABLE 1.
Effect of carbon source and minimal media on potencies of natural product hits against M. abscessus ATCC 19977 smooth reference strain
| Compound | pMIC90 (M) |
|||
|---|---|---|---|---|
| 7H9a glycerol | 7H9a acetate | CaMHb glycerol | Sautonc glycerol | |
| Lysobactin | 5.5 | 5.5 | 5.4 | 5.3 |
| Sorangicin A | 4.9 | 4.8 | 4.8 | 4.4 |
Middlebrook 7H9 media.
Cation-adjusted Mueller Hinton media.
Sauton mycobacteria minimal media.
Lysobactin and sorangicin A are active against the M. abscessus complex and drug resistant clinical isolates.
To compare the activity of LYB and SOR against other drugs with a similar target, we measured the pMIC90 of M. abscessus ATCC 19977 S and R reference strains against VAN as a representative cyclic peptide cell wall antimicrobial, and RIF and RFB as representative RNAP inhibitors. LYB and VAN demonstrated similar potencies against both M. abscessus S and M. abscessus R reference strains while SOR and RIF exhibited lower potencies than RFB (Table 2 and 3, Table S3). To determine if LYB and SOR are active against the M. abscessus complex, we measured the pMIC90 of the natural products against drug resistant clinical isolates that include M. abscessus subsp. abscessus (n = 5), M. abscessus subsp. massiliense (n = 5), and M. abscessus subsp. bolletii (n = 1). These clinical isolates are resistant to a variety of antibiotics used to treat M. abscessus pulmonary disease (Table S4). Whole-genome sequencing of the clinical isolates identified SNPs in erm(41), rrl, and rpoB that were confirmed with Sanger sequencing (Table 2). Clinical isolates represented T28 sequevars with a functional erm(41) for inducible CLR resistance and C28 sequevars with a nonfunctional erm(41). Two strains possessed the A2058G (A2270G in M. abscessus) or A2059C (A2271C in M. abscessus) SNP in the rrl gene that conferred constitutive CLR resistance (Table 2). Most isolates harbored a D523E substitution in RpoB. LYB and VAN demonstrated nearly equipotent activities against the clinical isolates (Median LYB pMIC90 = 5.3 [95% CI,4.9 to 5.4], VAN pMIC90 = 5.3 [95% CI,5.1 to 5.6], P = 0.46) (Fig. 5a). SOR and RIF were less potent compared to best-in-class RFB (Median SOR pMIC90 = 4.9 [95% CI,4.7 to 5.1], RIF pMIC90 = 4.9 [95% CI,4.4 to 5.2], RFB pMIC90 = 5.8 [95% CI,5.5 to 5.9]) (Fig. 5b). However, to measure preexisting resistance to the new compounds, pMIC90 values were standardized to the ATCC 19977 S reference strain. We measured up to a 10-fold change in pMIC90 of the clinical isolates relative to the ATCC 19977 reference strain for LYB with median LYB ΔpMIC90 = 0.4 [95% CI,0.3 to 0.9] and VAN ΔpMIC90 = −0.1 [95% CI, −0.4 to 0.1] (Fig. 5a). Although the RpoBD523E variant was commonly identified in these M. abscessus clinical isolates, M. tuberculosis naturally encodes E523 in the rifampicin resistance determining region. Fig. 5b illustrates a similar activity spectrum to SOR, RIF, and RFB. Taken together, these data suggest a lack of acquired resistance in the clinic to LYB and SOR.
TABLE 2.
Characterization of M. abscessus clinical isolates
| Isolate | Subspecies | Morphotype | rpoB AA | rrl SNP |
erm(41) sequevar |
Clarithromycin susceptibility |
|---|---|---|---|---|---|---|
| ATCC19977 | abscessus | Smooth | None | None | T28 | Sensitive |
| ATCC19977 | abscessus | Rough | None | None | T28 | Sensitive |
| MB084806 | abscessus | Smooth | D523E | None | T28 | Sensitive |
| MB092927 | abscessus | Smooth | D523E | None | C28 | Sensitive |
| MB093261 | abscessus | Smooth | None | None | T28 | Sensitive |
| L0007906 | abscessus | Rough | D523E | A2270G | T28 | Resistant |
| MB086151 | abscessus | Rough | D523E | None | C28 | Sensitive |
| MB088425 | massiliense | Smooth | D523E | None | Deletion | Sensitive |
| MB088215 | massiliense | Smooth | D523E | None | Deletion | Sensitive |
| MB092961 | massiliense | Rough | D523E | None | Deletion | Sensitive |
| L00042522 | massiliense | Rough | D523E | A2271C | Deletion | Resistant |
| AV | massiliense | Smooth | D523E | None | Deletion | Sensitive |
| 167P | bolletii | Rough | D523E | None | T28 | Resistant |
TABLE 3.
Potencies of natural product hits against M. abscessus reference strain and clinical isolates
| Isolate | Subspecies | Morphotype | pMIC90 (M)a |
||||
|---|---|---|---|---|---|---|---|
| Cell wall |
RNA polymerase |
||||||
| LYB | VAN | SOR | RIF | RFB | |||
| ATCC19977 | abscessus | Smooth | 5.7 | 5.2 | 5.0 | 4.9 | 5.7 |
| ATCC19977 | abscessus | Rough | 5.7 | 5.0 | 4.7 | 4.6 | 5.7 |
| MB084806 | abscessus | Smooth | 5.4 | 5.6 | 5.1 | 5.2 | 6.1 |
| MB092927 | abscessus | Smooth | 5.1 | 5.5 | 4.7 | 4.8 | 5.8 |
| MB093261 | abscessus | Smooth | 5.1 | 5.1 | 4.8 | 5.0 | 5.8 |
| L0007906 | abscessus | Rough | 4.9 | 5.3 | 4.7 | 4.2 | 5.3 |
| MB086151 | abscessus | Rough | 5.3 | 5.6 | 4.9 | 4.9 | 5.8 |
| MB088425 | massiliense | Smooth | 5.4 | 5.3 | 5.1 | 5.2 | 5.8 |
| MB088215 | massiliense | Smooth | 5.4 | 5.3 | 5.1 | 5.1 | 5.8 |
| MB092961 | massiliense | Rough | 5.4 | 5.3 | 5.1 | 5.2 | 5.9 |
| L00042522 | massiliense | Rough | 4.7 | 5.1 | 4.3 | 4.3 | 5.2 |
| AV | massiliense | Smooth | 4.8 | 5.1 | 4.5 | 4.4 | 5.5 |
| 167P | bolletii | Rough | 5.3 | 5.7 | 5.5 | 5.4 | 6.1 |
LYB, lysobactin; VAN, vancomycin; SOR, sorangicin A; RIF, rifampicin; RFB, rifabutin.
FIG 5.
Potencies of natural product hits against M. abscessus ATCC 19977 S and R reference strains and clinical isolates. Clinical isolates comprise M. abscessus complex (M. abscessus n = 5, M. massiliense n = 5, M. bolletii n = 1). (a) MIC90 (μM) of LYB and VAN converted to pMIC90 (M) (left). Change in pMIC90 relative to M. abscessus ATCC 19977 (pMIC90 ATCC − pMIC90 clin iso). Values greater than 0 indicate lower potency against the clinical isolate. Dashed lines represent 10-fold change in potency. Data shown is median with P-values from Wilcoxon matched-pairs rank test. (b) MIC90 (μM) of SOR, RIF, and RFB converted to pMIC90 (M) (left). Change in pMIC90 relative to M. abscessus ATCC 19977 (pMIC90 ATCC − pMIC90 clin iso). Values greater than 0 indicate lower potency against the clinical isolate. Dashed lines represent 10-fold change in potency. Data shown is median with P-values from Friedman test with Dunn’s multiple-comparison test.
DISCUSSION
Ten hits were identified from a library of 517 natural products from fermented microorganisms. Two compounds of interest are LYB and SOR. LYB, also known as katanosin B, is a cyclic depsipeptide secondary metabolite produced by Lysobacter ezymogenes (35, 36). First identified in 1988, LYB was found to inhibit peptidoglycan synthesis in Gram-positive bacteria, but its molecular mechanism remained undefined (35, 36). Later, it was shown that while VAN binds to the terminal d-Ala-d-Ala residue of the pentapeptide stem on N-acetylmuramic acid/N-acetylglucosamine units, LYB binds to the reducing end of the lipid-anchored peptidoglycan precursor, lipid II (27). Cyclic peptides have recently been investigated for activity against M. abscessus. Teicoplanin showed synergy in combination with the glycylcycline, tigecycline, and VAN synergized with the macrolide, clarithromycin (37, 38). Due to previous work showing that LYB causes moderate toxicity in mice when administered intravenously (36) but the absence of clinical resistance shown here, LYB could benefit from novel formulations to increase the oral bioavailability and limit side effects.
SOR is produced by the gliding myxobacterium Sorangium cellulosum and targets eubacterial but not eukaryotic RNAPs (39, 40). Like RIF and RFB, SOR inhibits bacterial transcription via binding to the RpoB subunit of wild-type RNAP but in M. tuberculosis, SOR was shown to prevent promoter DNA unwinding specifically in RIFR mutants (30, 41). Importantly, SOR maintained activity against E. coli and M. tuberculosis rpoB mutants despite being resistant to RIF. This has important implications for the treatment of M. tuberculosis as RIF is a front-line agent and for the treatment of M. abscessus since the activity of RFB has recently been explored (31, 32, 42). SOR could be a promising candidate for the M. abscessus drug pipeline as it not only retains activity against M. tuberculosis RIFR mutants but induces cytochrome P450 3A4 to a lesser degree than the classic RNAP inhibitors RIF and RFB (30). Cytochrome P450 3A4 induction from rifampicin has been shown to reduce the efficacy of the cftR corrector, ivacaftor, for patients with CF through drug-drug interactions (43).
M. abscessus drug discovery could benefit from additional library screening to identify novel scaffold/drug target pairs like the oxaboroles and tRNA synthetases, but attrition rates are high (44–46). Alternatively, focusing on pharmacologically and clinically validated drug targets like peptidoglycan and RNAP might accelerate the drug discovery process (47). Although inhibitors for these targets do not exert the most potent in vitro activity, they provide novel scaffolds with subtly different mechanism of action, whose potency and drug disposition properties can be improved through careful medicinal chemistry optimization or alternative biotechnological approaches for compound improvement (16). Future studies should include structure activity relationship analysis and novel formulations to improve the activity and bioavailability while minimizing toxicity of the natural products LYB and SOR for the development of M. abscessus antibiotics.
MATERIALS AND METHODS
Compounds.
Myxobacteria and fungi are prolific sources of structurally diverse metabolites displaying innovative modes-of-action (48, 49). The labs at HZI/HIPS focus on exploring understudied sources and expanding the natural product space in biodiversity-driven approaches (15). Production and isolation procedures are being developed and adapted to match compound properties, and we typically aim at isolating compounds at > 90% purity. The library plates and master stocks are stored at −80°C and undergo routine quality control via HPLC-MS/UV. For hit confirmation and dose response, independent powder stocks are provided which are typically at 95% purity. An in-house collection of 517 natural products were included in the screen. The library includes 176 compounds isolated from diverse sources, 88 compounds isolated from fungi, and 253 compounds isolated from myxobacterial fermentation. The natural products were prepared at 1 mM in 100% dimethyl sulfoxide (DMSO). Amikacin (AMK) was resuspended in distilled H2O (dH2O). Vancomycin (VAN) was resuspended in dH2O while lysobactin (LYB), rifampicin (RIF), and rifabutin (RFB) were resuspended in 100% DMSO. Sorangicin A (SOR) was prepared in-house and resuspended in 100% DMSO. For Sorangicin A, fermentation and downstream processing is described elsewhere and the provided sample was > 95% purity. All drugs were purchased from Sigma-Aldrich unless otherwise stated.
Bacterial strains.
Mycobacterium abscessus ATCC 19977 reference strain was used to create a constitutively luminescent strain by integration of the luxCDABE operon (M. abscessus lux) for screening assays. The integration was accomplished by electroporating the plasmid plux that targets the attP site of the mycobacterial genome and selecting on 7H10 plates containing 250 μg/mL of kanamycin. M. abscessus lux cultures were grown in 100 μg/mL kanamycin for plasmid maintenance. Cultures were passaged in antibiotic-free media one night prior to the primary screen assay. Clinical isolates of M. abscessus subsp. abscessus and subsp. massiliense from patients with cystic fibrosis were obtained from an epidemiologic study of M. abscessus transmission on the island of Montreal. Isolates were characterized by Illumina Mi-Seq whole-genome sequencing. M. abscessus subsp. bolletii clinical isolate was obtained from France. Single nucleotide polymorphisms (SNPs) in erm(41), rpoB, and rrl were detected using Galaxy. Briefly, whole-genome sequence qualities were checked with FASTQC, and adapter sequences were trimmed with Trimmomatic. Snippy was used to map whole-genome sequences to erm(41), rpoB, and rrl from ATCC 19977 reference (GenBank accession: CU458896.1) with a minimum mapping quality of 60 and minimum coverage of 40. SNPs in erm(41), rpoB, and rrl were confirmed with Sanger sequencing. erm(41) primers: PF GTGTCCGGCCAACGGTCGCGA; PR TCAGCGCCGCCTGATCACCAGC; rpoB primers: PF TGTCGCAGTTCATGGACCAGAA; PR GTCGTGCTCGAGGAACGGGAT; rrl primers: PF GACGATGTATACGGACTGACGC; PR CGTCCAGGTTGAGGGAACCTT. Phenotypic clarithromycin resistance was confirmed genotypically by erm(41) sequevar (T28 for active erm[41] or C28 for inactive erm[41]) or A2058/2059 polymorphisms in rrl.
Culture conditions.
M. abscessus strains were grown in rolling liquid culture at 37°C in Middlebrook 7H9 broth (BD Difco) supplemented with 10% (vol/vol) albumin dextrose catalase enrichment (ADC), 0.2% (vol/vol) glycerol, and 0.05% (vol/vol) Tween 80 (7H9 complete) or on 7H10 agar plates supplemented with 10% (vol/vol) oleic acid ADC enrichment and 0.5% (vol/vol) glycerol at 37°C unless otherwise stated; 7H9 broth supplemented with 10% (vol/vol) ADC enrichment, 0.2% (vol/vol) sodium acetate, and 0.05% (vol/vol) Tween 80 was used as an alternative carbon source. Cation-adjusted Mueller-Hinton broth (BD Difco) with 10% (vol/vol) ADC enrichment, 0.2% (vol/vol) glycerol, and 0.05% (vol/vol) Tween 80 was used as an alternative media and bacteria were grown at 30°C. Sauton’s minimal medium was used as a defined minimal media (0.5 g/L monobasic potassium phosphate, 4.0 g/L l-asparagine monohydrate, 2.0 g/L citric acid monohydrate, 0.05 g/L ferric ammonium citrate, 0.1 mL of 1% zinc sulfate, 0.5 g/L magnesium sulfate heptahydrate, 60 mL of 100% glycerol, 2.5 mL of 20% Tween 80, pH 7).
Screening assay.
The natural product library was screened against M. abscessus lux at a single-point concentration of 10 μM in duplicate in 96-well flat-bottom white plates in 7H9 complete media. The culture was grown to log phase (OD600 0.4–0.8) and diluted to an OD600 of 0.005 (5×106 CFU/mL). 90 μL of culture was mixed with 10 μL of 100 μM compound diluted in a mixture of 10% DMSO/90% 7H9. The final concentration of DMSO in each well was 1%. Plates were sealed with parafilm and incubated at 37°C for 48 h. The last column of each plate had 1% DMSO as negative control in quadruplicate (drug-free conditions) and 110 μM AMK as positive control in quadruplicate. Luminescence was measured with an Infinite F200 Tecan plate reader. Percentage of luminescence relative to DMSO control was plotted using GraphPad Prism version 9. Compounds that decreased the luminescence to ≤ 10% or ≤ 50% of the drug-free conditions were classified as strong or moderate hits, respectively.
Determination of MICs.
MIC values were determined using the resazurin microtiter assay (REMA). Cultures were grown to log phase (OD600 of 0.4–0.8) and diluted to OD600 of 0.005 (5×106 CFU/mL). Drugs were prepared in 2-fold serial dilutions in 96-well plates with 90 μL of bacteria per well to a final volume of 100 μL. 96-well clear, flat-bottom plates were incubated at 37°C until drug-free wells were turbid (48 h for M. abscessus). 10 μL of resazurin (0.025% wt/vol) was added to each well. Once the drug-free wells turned pink (3 to 4 h), the fluorescence (ex/em 560 nm/590 nm) was measured using an Infinite F200 Tecan plate reader. Fluorescence intensities were converted to % viable cells relative to drug-free conditions and fit to the modified Gompertz equation using GraphPad Prism version 9. MIC values at 90% growth inhibition were determined from the nonlinear regression Gompertz equation (50). To compare MICs across media or clinical isolates, MIC values were log transformed (pMIC = –log[MIC]).
Supplementary Material
ACKNOWLEDGMENT
The luxCDABE plasmid was kindly gifted by Jeffery S. Cox.
Footnotes
Supplemental material is available online only.
Contributor Information
Marcel A. Behr, Email: marcel.behr@mcgill.ca.
Amit Singh, Indian Institute of Science Bangalore.
Gerard Wright, McMaster University.
REFERENCES
- 1.Johansen MD, Herrmann J-L, Kremer L. 2020. Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat Rev Microbiol 18:392–407. doi: 10.1038/s41579-020-0331-1. [DOI] [PubMed] [Google Scholar]
- 2.Bronson RA, et al. 2021. Global phylogenomic analyses of Mycobacterium abscessus provide context for non cystic fibrosis infections and the evolution of antibiotic resistance. Nat Commun 12. doi: 10.1038/s41467-021-25484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tortoli E, Fedrizzi T, Meehan CJ, Trovato A, Grottola A, Giacobazzi E, Serpini GF, Tagliazucchi S, Fabio A, Bettua C, Bertorelli R, Frascaro F, De Sanctis V, Pecorari M, Jousson O, Segata N, Cirillo DM. 2017. The new phylogeny of the genus Mycobacterium: the old and the news. Infect Genet Evol 56:19–25. doi: 10.1016/j.meegid.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Moreno-Izquierdo C, Zurita J, Contreras-Yametti FI, Jara-Palacios MA. 2020. Mycobacterium abscessus subspecies abscessus infection associated with cosmetic surgical procedures: cases series. IDCases 22:e00992. doi: 10.1016/j.idcr.2020.e00992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hui SH, Noonan L, Chavada R. 2015. Post liposuction Mycobacterium abscessus surgical site infection in a returned medical tourist complicated by a paradoxical reaction during treatment. Infect Dis Rep 7:87–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrd TF, Ryan K. 2018. Mycobacterium abscessus: shapeshifter of the Mycobacterial World. Front Microbiol 9:2642. doi: 10.3389/fmicb.2018.02642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore M, Frerichs JB. 1953. An unusual acid-fast infection of the knee with subcutaneous, abscess-like lesions of the gluteal region; report of a case with a study of the organism, Mycobacterium abscessus, n. sp. J Invest Dermatol 20:133–169. doi: 10.1038/jid.1953.18. [DOI] [PubMed] [Google Scholar]
- 8.Cassidy PM, Hedberg K, Saulson A, McNelly E, Winthrop KL. 2009. Nontuberculous mycobacterial disease prevalence and risk factors: a changing epidemiology. Clin Infect Dis 49:e124–e129. doi: 10.1086/648443. [DOI] [PubMed] [Google Scholar]
- 9.Lee M-R, Sheng W-H, Hung C-C, Yu C-J, Lee L-N, Hsueh P-R. 2015. Mycobacterium abscessus complex infections in humans. Emerg Infect Dis 21:1638–1646. doi: 10.3201/2109.141634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu ML, Aziz DB, Dartois V, Dick T. 2018. NTM drug discovery: status, gaps and the way forward. Drug Discov Today 23:1502–1519. doi: 10.1016/j.drudis.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Floto RA, Olivier KN, Saiman L, Daley CL, Herrmann J-L, Nick JA, Noone PG, Bilton D, Corris P, Gibson RL, Hempstead SE, Koetz K, Sabadosa KA, Sermet-Gaudelus I, Smyth AR, van Ingen J, Wallace RJ, Winthrop KL, Marshall BC, Haworth CS. 2016. US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis. Thorax 71:i1–i22. doi: 10.1136/thoraxjnl-2015-207360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richard M, Gutiérrez AV, Kremer L. 2020. Dissecting erm(41)-mediated macrolide-inducible resistance in mycobacterium abscessus. Antimicrob Agents Chemother 64:e01879-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nash KA, Brown-Elliott AB, Wallace RJ. 2009. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of mycobacterium abscessus but is absent from mycobacterium chelonae. Antimicrob Agents Chemother 53:1367–1376. doi: 10.1128/AAC.01275-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Svetlov MS, Syroegin EA, Aleksandrova EV, Atkinson GC, Gregory ST, Mankin AS, Polikanov YS. 2021. Structure of Erm-modified 70S ribosome reveals the mechanism of macrolide resistance. Nat Chem Biol 17:412–420. doi: 10.1038/s41589-020-00715-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann T, et al. 2018. Correlating chemical diversity with taxonomic distance for discovery of natural products in myxobacteria. Nat Commun 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hug JJ, Krug D, Müller R. 2020. Bacteria as genetically programmable producers of bioactive natural products. Nat Rev Chem 4:172–193. doi: 10.1038/s41570-020-0176-1. [DOI] [PubMed] [Google Scholar]
- 17.Wright GD. 2014. Something old, something new: revisiting natural products in Antibiotic drug discovery. Can J Microbiol 60:147–154. doi: 10.1139/cjm-2014-0063. [DOI] [PubMed] [Google Scholar]
- 18.Crawford JM, Tang G-L, Herzon SB. 2021. Natural products: an era of discovery in organic chemistry. J Org Chem 86:10943–10945. doi: 10.1021/acs.joc.1c01753. [DOI] [PubMed] [Google Scholar]
- 19.Fischbach MA, Walsh CT. 2009. Antibiotics for emerging pathogens. Science 325:1089–1093. doi: 10.1126/science.1176667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarathy JP, et al. 2020. TBAJ-876, a 3,5-dialkoxypyridine analogue of Bedaquiline, is active against Mycobacterium abscessus. Antimicrob Agents Chemother 64:e02404-19. doi: 10.1128/aac.02404-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warrier T, Martinez-Hoyos M, Marin-Amieva M, Colmenarejo G, Porras-De Francisco E, Alvarez-Pedraglio AI, Fraile-Gabaldon MT, Torres-Gomez PA, Lopez-Quezada L, Gold B, Roberts J, Ling Y, Somersan-Karakaya S, Little D, Cammack N, Nathan C, Mendoza-Losana A. 2015. Identification of novel anti-mycobacterial compounds by screening a pharmaceutical small-molecule library against nonreplicating Mycobacterium tuberculosis. ACS Infect Dis 1:580–585. doi: 10.1021/acsinfecdis.5b00025. [DOI] [PubMed] [Google Scholar]
- 22.Niles AL, Moravec RA, Riss TL. 2008. Update on in vitro cytotoxicity assays for drug development. Expert Opin Drug Discov 3:655–669. doi: 10.1517/17460441.3.6.655. [DOI] [PubMed] [Google Scholar]
- 23.Lupien A, et al. 2018. Optimized background regimen for treatment of active tuberculosis with the next-generation benzothiazinone macozinone (PBTZ169). Antimicrob Agents Chemother 62:e00840-18. doi: 10.1128/AAC.00840-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malin JJ, Winter S, van Edeltraud G, Plum G, Rybniker J. 2019. Extremely low hit rate in a diverse chemical drug screen targeting Mycobacterium abscessus. Antimicrob Agents Chemother 63:e01008-19. doi: 10.1128/AAC.01008-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ballell L, Bates RH, Young RJ, Alvarez-Gomez D, Alvarez-Ruiz E, Barroso V, Blanco D, Crespo B, Escribano J, González R, Lozano S, Huss S, Santos-Villarejo A, Martín-Plaza JJ, Mendoza A, Rebollo-Lopez MJ, Remuiñan-Blanco M, Lavandera JL, Pérez-Herran E, Gamo-Benito FJ, García-Bustos JF, Barros D, Castro JP, Cammack N. 2013. Fueling open-source drug discovery: 177 small-molecule leads against tuberculosis. ChemMedChem 8:313–321. doi: 10.1002/cmdc.201200428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szekely R, et al. 2020. 11-Dioxobenzo[f]pyrido[1,2-a]indoles kill Mycobacterium tuberculosis by targeting iron-sulfur protein Rv0338c (IspQ) a putative redox sensor. ACS Infect Dis 6:3015–3025. doi: 10.1021/acsinfecdis.0c00531. [DOI] [PubMed] [Google Scholar]
- 27.Lee W, Schaefer K, Qiao Y, Srisuknimit V, Steinmetz H, Müller R, Kahne D, Walker S. 2016. The mechanism of action of Lysobactin. J Am Chem Soc 138:100–103. doi: 10.1021/jacs.5b11807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chew KL, Octavia S, Go J, Ng S, Tang YE, Soh P, Yong J, Jureen R, Lin RTP, Yeoh SF, Teo J. 2021. In vitro susceptibility of Mycobacterium abscessus complex and feasibility of standardizing treatment regimens. J Antimicrob Chemother 76:973–978. doi: 10.1093/jac/dkaa520. [DOI] [PubMed] [Google Scholar]
- 29.Svetitsky S, Leibovici L, Paul M. 2009. Comparative efficacy and safety of vancomycin versus teicoplanin: systematic review and meta-analysis. Antimicrob Agents Chemother 53:4069–4079. doi: 10.1128/AAC.00341-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lilic M, Chen J, Boyaci H, Braffman N, Hubin EA, Herrmann J, Müller R, Mooney R, Landick R, Darst SA, Campbell EA. 2020. The antibiotic sorangicin A inhibits promoter DNA unwinding in a Mycobacterium tuberculosis rifampicin-resistant RNA polymerase. Proc Natl Acad Sci USA 117:30423–30432. doi: 10.1073/pnas.2013706117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aziz DB, et al. 2017. Rifabutin Is active against mycobacterium abscessus complex. Antimicrob Agents Chemother 61:e00155-17. doi: 10.1128/AAC.00155-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dick T, Shin SJ, Koh WJ, Dartois V, Gengenbacher M. 2020. Rifabutin is active against mycobacterium abscessus in mice. Antimicrob Agents Chemother 64:01943-19. doi: 10.1128/AAC.01943-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pethe K, Sequeira PC, Agarwalla S, Rhee K, Kuhen K, Phong WY, Patel V, Beer D, Walker JR, Duraiswamy J, Jiricek J, Keller TH, Chatterjee A, Tan MP, Ujjini M, Rao SPS, Camacho L, Bifani P, Mak PA, Ma I, Barnes SW, Chen Z, Plouffe D, Thayalan P, Ng SH, Au M, Lee BH, Tan BH, Ravindran S, Nanjundappa M, Lin X, Goh A, Lakshminarayana SB, Shoen C, Cynamon M, Kreiswirth B, Dartois V, Peters EC, Glynne R, Brenner S, Dick T. 2010. A chemical genetic screen in Mycobacterium tuberculosis identifies carbon-source-dependent growth inhibitors devoid of in vivo efficacy. Nat Commun 1:57. doi: 10.1038/ncomms1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hatakeyama S, Ohama Y, Okazaki M, Nukui Y, Moriya K. 2017. Antimicrobial susceptibility testing of rapidly growing mycobacteria isolated in Japan. BMC Infect Dis 17. doi: 10.1186/s12879-017-2298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Sullivan J, et al. 1988. Lysobactin, a novel antibacterial agent produced by lysobacter sp. I. Taxonomy, isolation and partial characterization. J Antibiot (Tokyo) 41:1740–1744. doi: 10.7164/antibiotics.41.1740. [DOI] [PubMed] [Google Scholar]
- 36.Bonner DP, O'Sullivan J, Tanaka SK, Clark JM, Whitney RR. 1988. Lysobactin, a novel antibacterial agent produced by lysobacter sp. II. biological properties. J Antibiot (Tokyo) 41:1745–1751. doi: 10.7164/antibiotics.41.1745. [DOI] [PubMed] [Google Scholar]
- 37.Mukherjee D, Wu ML, Teo JWP, Dick T. 2017. Vancomycin and clarithromycin show synergy against Mycobacterium abscessus in vitro. Antimicrob Agents Chemother 61:e01298-17. doi: 10.1128/AAC.01298-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aziz DB, Teo JWP, Dartois V, Dick T. 2018. Teicoplanin - Tigecycline combination shows synergy against Mycobacterium abscessus. Front Microbiol 9:932. doi: 10.3389/fmicb.2018.00932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jansen R, Wray V, Irschik H, Reichenbach H, Höfle G. 1985. Isolation and spectroscopic structure elucidation of sorangicin a, a new type of macrolide-polyether antibiotic from gliding bacteria - XXX. Tetrahedron Lett 26:6031–6034. doi: 10.1016/S0040-4039(00)95117-7. [DOI] [Google Scholar]
- 40.Irschik H, Gerth K, Reichenbach H, Jansen R, Hofle G. 1987. The sorangicins, novel and powerful inhibitors of eubacterial rna polymerase isolated from myxobacteria. J Antibiot (Tokyo) 40:7–13. doi: 10.7164/antibiotics.40.7. [DOI] [PubMed] [Google Scholar]
- 41.Campbell EA, Pavlova O, Zenkin N, Leon F, Irschik H, Jansen R, Severinov K, Darst SA. 2005. Structural, functional, and genetic analysis of sorangicin inhibition of bacterial RNA polymerase. EMBO J 24:674–682. doi: 10.1038/sj.emboj.7600499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ganapathy US, Dartois V, Dick T. 2019. Repositioning rifamycins for Mycobacterium abscessus lung disease. Expert Opin Drug Discov 14:867–878. doi: 10.1080/17460441.2019.1629414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guimbellot JS, Acosta EP, Rowe SM. 2018. Sensitivity of ivacaftor to drug-drug interactions with rifampin, a cytochrome P450 3A4 inducer. Pediatr Pulmonol 53:E6–E8. doi: 10.1002/ppul.23971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim T. 2021. A screening of the mmv pandemic response box reveals epetraborole as a new potent inhibitor against mycobacterium abscessus. Int J Mol Sci 22:5936. doi: 10.3390/ijms22115936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ganapathy US, Gengenbacher M, Dick T. 2021. Epetraborole is active against mycobacterium abscessus. Antimicrob Agents Chemother 65:e01156-21. doi: 10.1128/AAC.01156-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sullivan JR, Lupien A, Kalthoff E, Hamela C, Taylor L, Munro KA, Schmeing TM, Kremer L, Behr MA. 2021. Efficacy of epetraborole against Mycobacterium abscessus is increased with norvaline. PLoS Pathog 17:e1009965-28. doi: 10.1371/journal.ppat.1009965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dartois V, Dick T. 2022. Drug development challenges in nontuberculous mycobacterial lung disease: TB to the rescue. J Exp Med 219:e20220445. doi: 10.1084/jem.20220445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Herrmann J, Fayad AA, Müller R. 2017. Natural products from myxobacteria: novel metabolites and bioactivities. Nat Prod Rep 34:135–160. doi: 10.1039/c6np00106h. [DOI] [PubMed] [Google Scholar]
- 49.Becker K, Stadler M. 2021. Recent progress in biodiversity research on the Xylariales and their secondary metabolism. J Antibiot (Tokyo) 74:1–23. doi: 10.1038/s41429-020-00376-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lambert RJW, Pearson J. 2000. Susceptibility testing: accurate and reproducible minimum inhibitory concentration (MIC) and non-inhibitory concentration (NIC) values. J Appl Microbiol 88:784–790. doi: 10.1046/j.1365-2672.2000.01017.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1 to S4. Download spectrum.02672-22-s0001.pdf, PDF file, 0.3 MB (268.5KB, pdf)