Abstract
The need for novel biological drugs against respiratory diseases has been highlighted during the Coronavirus (COVID-19) pandemic. The use of inhalation presents challenges to drug product stability, which is especially true for delivery using nebulizers (jet versus mesh technologies). The late-stage process of drug development in the pharmaceutical industry requires the investigation of in-use stability. In-use studies generate data that are guided by the requirements of regulatory authorities for inclusion in the clinical trial application dossier. In this review, I introduce the initial aspects of in-use stability studies during the development of an aerosol formulation to deliver biologics with a nebulizer. Lessons learned from this experience can guide future development and planning for formulation, analytics, material compatibility, nebulization process, and clinical trial preparations.
Keywords: biologics, in-use stability, lung delivery, material compatibility, pharmaceutical quality
Introduction
Pharmaceutical quality gathers evidence on the consistent efficiency and safety of medicines. Every preparation, administration, and dosing regimen should be of high quality without risk to patients. Only then, a safe medicine-taking is assured.
Most stability studies focus on the drug product’s vial, as unopened, fresh from the manufacturing or filling site, with specific shelf-life instructions, including time and temperature of storage. In pharmaceutics, ready-to-use and ready-to-administer products go beyond the use of the unopened vial. Hospital pharmacists and delegates from clinical trial sites must then proceed with the compounding and/or reconstitution of the drug, whereas physicians and nurses will handle the ready-to-administer product. Regardless on whether these are biologics, its handling (compounding, storage, transport, connection to medical devices, and administration processes) should be investigated to structure the writing of a feasible instruction [1].
Using inhalation as a delivery method can be traced back to the inhalation of epinephrine against asthma in 1929 in the UK. The development of inhalable drugs has since become more widespread [2]. In combination with local pulmonary drug delivery, the targets are changing to support the development of new biological entities (NBEs). With the advent of novel respiratory diseases, such as COVID-19, the use of biologics, including monoclonal antibodies (mAbs), is considered a state-of-the-art therapeutical approach [3].
The cover model for approved inhalable biologics is Pulmozyme® as a dornase alpha replacement in the treatment of cystic fibrosis, which was approved on 1993 by the US Food and Drug Administration (FDA). Interestingly, this approval contains label information that the administration could include a vibrating mesh or a jet nebulizer; however, the specific eRapid Nebulizer System (vibrating mesh) is the one recommended, including the description of administration instructions. Matthews et al. [4] generated a table with 15 inhaled protein drugs that are in development, so according to the Purple Book [5] database from the FDA, only the inhaled Leukine® against autoimmune pulmonary alveolar proteinosis, the DAS181 sialidase against parainfluenza and COVID-19, and the Kamada-AAT against alpha-1 antitrypsin deficiency (all using mesh nebulizers) are in Phase III clinical trials.
Lung delivery allows for both local and systemic drug administration, involving non-invasive versus parenteral delivery [i.e., intravenous (i.v.) bolus/infusion]. Biological barriers to pulmonary delivery include cells with inherent matrices, and efflux and clearance mechanisms that necessitate a step-wise approach when producing and characterizing an aerosol [6]. Bronchial morphology, respiratory capacity, associated pathologies, and aerosol characteristics should also be considered as main factors that influence aerosol deposition [7].
Treatments for respiratory diseases focus on the lung itself for drug delivery instead of relying on drug transport via the bloodstream. The inhalation drug delivery route has a compatible tolerance profile with conventional chemical entities, and has been widely used against diseases, such as chronic obstructive pulmonary disease (COPD) and asthma. Depending on the required therapeutic dose, delivering antibiotics via the lung can achieve higher concentrations as aerosols compared with the i.v. route, as in the case of tobramycin and ventilator-acquired pneumonia [8]. Similarly, pulmonary delivery affords an increase in the therapeutic index when used with anticancer agents, such as doxorubicin and liposome-encapsulated paclitaxel. Additionally, complex macromolecules, such as interleukin-2, have been delivered via the respiratory tract to treat pulmonary metastases, a delivery strategy that might avoid the high doses required via the i.v. route, which can induce vascular leakage [9].
The potential of NBEs to be delivered via the lung has increased with the development of new antibody strategies, the rise of nucleic acid drugs, and cell therapy innovations. This is also related to the development of biocompatible drugs and the push for new carriers that target the nose, brain, and specific areas or cells of the lung where immunization is required [10]. An overview of NBEs delivered to the lung is given in Figure 1 and this pipeline will only grow with the current respiratory pandemic followed by a worldwide mRNA vaccination.
Figure 1.
Potential for nasal and pulmonary delivery of biologics. Adapted from [10].
mAbs are macromolecules usually comprising immunoglobulin (Ig)-G1 glycoproteins measuring ∼150 kDa. Foreign molecules (or particles) are not necessarily welcome in the respiratory environment. In fact, compared with small drug molecules, mAbs are more readily hydrolyzed when engulfed by bronchial macrophages, the first line of innate immunity in the lung. Strategies to overcome this include: rational design of Ig delivery, and conformational analysis and use of excipients, such as mannitol, sorbitol or trehalose, which prevent macrophage engulfment. Nonetheless, the methods to acquire a powder formulation, for example spray-drying, can lead to aggregation and loss of potency [11].
Another possible strategy to optimize mAb therapy is the manipulation of the mAbs via the Fc-region. Here, the neonatal constant region fragment receptor (FcRn) is known to mediate transport of maternal IgG from milk to the fetal bloodstream and it is expressed not only in the placenta, but also in the gut, kidney, and, importantly, lungs [11], [12]. Using this formulation and modified human erythropoietin, nebulized with an Aeroneb nebulizer, resulted in improved aerosol characteristics compared with unmodified IgG1 [13].
In terms of smaller medicine size, this creates advantages for local lung delivery, including increased safety and limited off-target systemic side effects, increased efficacy with higher and faster lung delivery, and the possibility of reduced costs with smaller doses being administered. Nonetheless, specific areas of the lung can allow systemic circulation via receptor-mediated drug transport into the blood, while overcoming the lung biological barriers can also benefit localized targeting toward lung cancer tissue [14], [15]. However, because of the large NBE size, there is a need to create protection against the nebulization processes and aerosol formation in a reproducible way that does not alter the drug product stability [16].
When the intended final formulation of an NBE is ready, the different phases of clinical trials demand the support of study simulations indicating product stability, and the effect of drug administration parameters, including handling, preparation, transport, temperature, humidity, and other key pharmaceutical factors. Here, the development of the analytical scope will address the possibilities of instability, when, for example, the use of a solvent/diluent could produce particulates or when the combined exposure to material and long-term storage might impact drug concentration, oxidation, potency, and consequent issues of misdosing [1].
In this review, I discuss the in-use stability study of biological drugs to be delivered via nebulization and provide insights into this specific scenario of the late-stage drug development that many pharmaceutical companies will face.
Shelf-life, in-use, beyond-use date, and expiration date
Since 1979, the FDA and European Medicine Agency (EMA) have required a shelf-life date to be placed on the label of a drug product vial. According to the International Council on Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) Q1A (R2) [17], shelf-life is the ‘period safeguarding the storage length and conditions recommended to maintain safe use of the drug’ [18]. Other regulatory authority guidelines that benefit drug development of aerosolized drugs are detailed in Table 1 .
Table 1.
Key guidelines and regulations for the pharmaceutical industry from the main regulatory authorities for drug product development using inhalation or nebulization as the route of administration
| Regulator | Guideline | Publication year | Possible parameters in nebulization studies | Refs |
|---|---|---|---|---|
| EMA | EMEA/CHMP/QWP/49313/2005 Corr: Guideline on the Pharmaceutical Quality of Inhalation and Nasal Products | 2006 | Content uniformity; protein/vehicle/viral content or concentration; biological potency; mean delivery dose; uniformity of dose; impurities and degradation products; preservatives and stabilizing excipient assays; sterility; particulate matter (<10, ≥10 and ≥25 mm); pH; weight loss (during compounding for syringes or CSTDs or during administration for nebulizer chambers/devices); leachables; particle size distribution; pump delivery for inhalation sprays; SCU for inhalation sprays; plume geometry for inhalation sprays; particle/droplet size distribution (cascade impactor; MMAD, GSD); sterility and antimicrobial preservative effectiveness; microscopic evaluation; appearance; color; clarity; functionality of pump/nebulizer components; number of actuations per container; container storage orientations (upright and inverted or upright and horizontal) |
[54] |
| EMA CHMP/SWP/28367/07: Guideline on Strategies to Identify and Mitigate Risks for First-in-Human and Early Clinical Trials with Investigational Medicinal Products (Section 5.3) | 2017 | [55] | ||
| CPMP/QWP/2934/99: Note for Guidance on In‐use Stability Testing of Human Medicinal Products | 2001 | [56] | ||
| FDA Guidance for Industry | Nasal Spray and Inhalation Solution, Suspension, and Spray Drug Products Chemistry, Manufacturing, and Controls Documentation | 2002 | [57] | |
| FDA | Reviewer Guidance for Nebulizers, Metered Dose Inhalers, Spacers and Actuators | 1993 | [58] | |
| Japanese Pharmacopeia | G-08: Preparations for Inhalation (General Chapter) and 2.9.18 Preparations for Inhalation: Aerodynamic Assessment of Fine Particles | 2005 | [59] | |
| USP | 601: Aerosols, Nasal Sprays, Metered Dose Inhalers, and Dry Powder Inhalers | 2012 | [60] | |
| 797: Pharmaceutical Compounding Sterile Preparations | 2008 | [19] | ||
| 795: Pharmaceutical Compounding Nonsterile Preparations | 2014 | [22] | ||
| 800: Hazardous Drugs Handling in Healthcare Settings | 2019 | [51] | ||
| 1049: Quality of Biotechnological Products: Stability after Reconstitution of Freeze‐Dried Product (6.6) | 2012 | [61] | ||
| 71: Sterility Tests | 2013 | [62] | ||
| 85: Bacterial Endotoxins Test | 2012 | [63] | ||
| ICH | ICH Q1A R2 Stability Testing of New Drug Substances and Drug Products: Section 2.2.7 | 2003 | [17] | |
| ICH Q8 R2: Pharmaceutical Development: Section II. F Compatibility | 2014 | [64] |
Abbreviations: CSTD, closed system drug-transfer device; CHMP, Committee for Medicinal Products for Human Use; CPMP, Committee for Proprietary Medicinal Products; GSD, geometric standard deviation; QWP, Quality Working Party; SWP, Safety Working Party; SCU, spray content uniformity.
Furthermore, quality attributes are key requirements for all commercial medicinal products and must be clarified and communicated in a transparent manner to all stakeholders, including intermediate users during clinical trial development, and end users. These attributes can be compiled in a quality in-use statement derived from tested and reproducible studies, guaranteeing that the process is practical, feasible, and produces high-quality drugs. In addition, the in-use statement contains analytical documents on the batch release of drug product and on the stability at shorter timepoints compared with shelf-life studies. A harmonized quality statement of shelf-life and in-use results includes consideration of what the stability-limiting points are, a bracketing approach of the possible dose range, and the observation of worst-case scenarios with the changes over time/process [18].
The United States Pharmacopeia (USP) 797 [19] defines expiration date is ‘the time during which a product can be expected to meet the requirements of the compendial monograph, if one exists, or maintain expected quality provided it is kept under the specified storage conditions’. One of the main issues with expiration dates is the questioning of biological activity and potency of medicinal products. In fact, not all conditions can be tested during the in-use studies, hence the bracketing and matrixing approaches. Nonetheless, the exact expiration date that relates to loss of potency and/or drug function is not necessarily described on the vial. Recently, drug development of biologics, such as mAbs, has become increasingly expensive, reflected by the cost of treatment. Hernandez et al. [20] identified that, between 1997 and 2016 in the USA, the average price of mAb treatment for 1 year was ∼US$100 000 (particularly for mAbs in the fields of oncology and hematology). In reality, this treatment is not affordable.
FDA studies with small molecules have surged with the Shelf Life Extension Program (SLEP), showing that expiration dates of some drug products could be extend for more than 1 year. Importantly, biologics with slight differences in biological activity can be highly toxic and the extrapolation of expiration dates is not recommended. This extrapolation for mAbs is a topic that will eventually emerge from the need to reduce the price of biologics and that, as leaders in the pharmaceutical industry, quality and late-stage drug development teams should be in charge of this discussion [21].
Alternatively, the beyond-use date (BUD) is based on the determinations of USP 797 [19] and 795 [22]. BUD is ‘either the date, or hour and date, after which a compounded sterile preparation (CSP) must not be used. The BUD is determined from the date/time that preparation of the CSP is initiated’. For compounded nonsterile preparations (CNSP) [22], the establishment of BUDs considers the following parameters: (i) chemical and physical stability; (ii) compatibility of the container-closure system; (iii) degradation of the container-closure system; and (iv) potential for microbial proliferation.
For CSP, the establishment of BUDs considers the risk of microbial contamination and the BUD predicted times define two CSP categories. A summary from the USP 797 [19] is provided in Table 2 . The BUD is derived from in-use data related to stability, sterility, and risk level, from which the shortest time is adopted as the BUD [23].
Table 2.
Characteristics of CSP and planning for CSP in-use studies based on USP 797
| Factors to include during BUD establishment | Detailed parameters | Personnel training (competency every 12 months) | CSP compounding methods during manufacturing | CSP category | Site of preparation per category |
|---|---|---|---|---|---|
USP 797
|
Stability factors
|
|
|
Category 1 CSP
|
Category 1 CSP
|
Sterility factors
|
|
Category 2 CSP
|
Category 2 CSP
|
With respect to CSP, the USP 797 [19] considers injections and infusions, along with ‘preparations for pulmonary inhalation’. However, nasal preparations for local application are not required to be sterile, indicating that pulmonary preparations with CSPs for nebulization for delivery to the upper (bronchial regions) and lower respiratory tract could follow this guideline. This requires support from the local and global departments of regulatory affairs to define the extent of following the USP or other guidelines.
The potential for instability during nebulization
Interfacial stress on therapeutic proteins can include vapor–liquid, solid–liquid, liquid–liquid, and air–liquid/solid contact. Prolonged exposure to interfacial stress can alter protein stability. To avoid this stress, protein modification can be carried out to facilitate conformational changes in the folded monomer that would allow interprotein bonds as strong as the previous conformation. However, the addition of monomers will increase this change and possibly form soluble high-molecular-weight (HMW) aggregates. This is the basis of protein aggregation [24].
The transport of masses during the interaction of protein and material surfaces involves interfacial stress allowing protein adsorption and possible aggregation. Convective transfer refers to migration of large masses within the surface, whereas smaller (even single) particles can be transferred via diffusive mass transfer. Depending on the interfacial stress type, the equilibrium of this mass transport might be influenced, even by short processes, such as sample agitation, mixing, transport, and pumping [23]. However, these processes can combine with shear stress to induce aggregation [25], such as removing air from infusion bags during preparation of i.v. Lumizyme®, a replacement therapy for α-glucosidase. In this case, removing the air from the i.v. bag reduced particle number [26]. Similarly, agitated protein drugs in siliconized or silicon-oil free syringes increased the layers in silicon oil, facilitating protein adsorption and consequent aggregation [27].
In terms of the quality characteristics of a protein drug, a product can exhibit alterations in increased visible and subvisible particles, decrease of protein concentration because of adsorption, and change parameters, such as charge, purity, hydrophobicity, pH, osmolality, potency, color, or clarity. Therefore, a risk analysis of preformulations should include expectations of the compounding and administration processes that will be tested during the in-use stability study [24], [28].
After manufacturing and filling of the drug product, the intended final formulation (as an aqueous solution, powder for reconstitution, or lyophilized product) will experience interfacial stress against the primary packaging, the headspace in the final container, and subsequent agitation during transportation. However the drug product in a glass vial is only the beginning of the compounding process in the hospital pharmacy or compounding centers. Here, to generate different concentrations from a stock solution, pharmacists use a diluent that can be formulated from the drug product buffer or specific admixtures of isotonic saline and polysorbates (e.g., PS 20, PS 80, or Poloxamer 188) [29]. These pharmacists will handle syringes (siliconized or not, or closed system transfer devices), needles, in-line filters, infusion bags, autoinjectors, or prefilled syringes, which will be set to interact with administration devices, most importantly with the nebulizer [30].
The success of nebulization includes reliable product and particle aerodynamics in the area of the lung for delivery. To achieve this, the development of the aerosol together with the right drug product formulation and the reliable performance of a nebulizer will define the drug delivery efficiency [31].
Types of nebulizer and nebulizer technology
For mAb development, aerosolization and the formulation itself will influence effective therapy and mAbs could be changed. Protein aggregates could decrease mAb biological potency or activity, or induce immunogenicity when nebulized. Aerosol formation depends on the dispersion of a solid phase or of liquid droplets in a medium (gas or air). These steps contribute to physical stress in biological drug production [31].
For formulation departments, this is a challenge that cannot be easily solved when changing the administration route from i.v. to inhalation. Mayor et al. [32] tested i.v. antibody formulations through 2-mesh nebulizers and compared them with formulations that were vigorously shaken. Nebulization induced increased subvisible particles at <10 mm and formation of HMW compared with shaking, which showed that repurposing formulation is complex.
The characterization of the aerosol should be designed taking into account changes in lung anatomy because of age, pathological state, and hospital versus home settings. In fact, breathing patterns and tidal volume both change aerosol delivery, especially compared across neonates, children, and adults [33]. In neonates, low lung volumes, low compliance, and irregular respiratory rates are barriers to successful aerosol lung deposition [34].
Nonetheless, for clinical settings, the choice of nebulizer within the ventilation circuit poses the question of what the alternative is to connect the nebulizer directly to the Y-piece of a ventilator [34]. With different types of ventilation, using mechanical, non-invasive, and high-flow nasal cannula could alter aerosol dynamics. To avoid this, nebulizers are adapted based on the administration route, with the option of using masks, mouthpieces, or a nebulizer attached to a ventilation device. Comparing masks wit mouthpieces has been questioned in terms of the efficiency of their drug delivery and their influence on pharmacodynamic parameters related to biological activities, such as improved forced expiratory volume in 1 second (FEV1) [35].
For inhalable protein formulations, nebulizers are the preferred device versus metered-dose or powder inhalers due to reproducible product stability. There are four types of nebulization technology, all of which have their own advantages and disadvantages (H. Padmanabhan, PhD thesis, University of Adelaide, 2019) [31], [36], [37].
In vibrating mesh nebulizers, ultrasonic vibration is used to drive a mesh plate with many tiny orifices in direct contact with a liquid reservoir, forcing out a mist of fine droplets. Disadvantages include large aggregates in the formulation, which can hinder liquid transfer through the micron-sized gaps of vibrating-mesh nebulizers. They might also not be powerful enough to aerosolize formulations of plasmid DNA (pDNA) polyplexes even at a moderate concentration of 0.2 mg/ml, because of high liquid viscosity. Their advantages include the fact that they preserve protein integrity more effectively compared with other nebulizers because they do not usually generate large changes in temperature and recycling processes. In addition, they provide improved protein stability with a cooled device to reduce reservoir heating. The addition of surfactants and increasing protein concentration can also be used to stabilize antibody formulations.
In ultrasonic nebulizers, piezoelectric crystals underneath a liquid reservoir vibrate at ultrasonic frequencies, propagating mechanical energy through the liquid to generate aerosols. However, they can generate heat, which can increase the temperature of the liquid significantly to cause thermal denaturation of biomolecules. Surface acoustic wave (SAW) nebulizers use nanometer amplitude through a piezoelectric lithium niobate (LiNbO3) substrate where the waves adjoin the liquid medium, thereby generating aerosols. Such nebulizers can effectively aerosolize pDNA and stem cells.
In jet nebulizers, compressed air is used to blast the liquid into droplets with sizes controlled by the air flow rate and the presence of baffles to avoid the escape of large droplets. Given the collection of large droplets by the baffles, jet nebulizers often result in drug recirculation, in which prolonged nebulization can impair the structural integrity of biopharmaceuticals. However, their use increases the drug concentration in the reservoir and they have a large residual volume (1–1.5 ml). They can also be operated continuously and result in substantial loss of drug formulation during exhalation, which can be resolved with breath-actuated jet nebulizers. Modifications are possible, such as adaptive aerosol delivery, which changes based on the breathing pattern of individuals and delivers the drug in pulses during the first half of the patient’s inspiratory phase.
In intratracheal sprayers, nebulization catheters are used to deliver fluid formulations as a spray to the airways of patients and animal models with the help of a bronchoscope. Placement of this device into the airway is invasive and requires sedation and endotracheal intubation of patients. However, they enable targeted delivery of the formulation to a particular region of the lung with a high degree of efficiency and control, and can deliver aerosols of a large size (25–30 μm) to the airways. In addition, they allow for the effective delivery of shear sensitive formulation, such as fibroblast cells and liposomes.
Main analytical skills required by in-use studies
After considering the regulatory guidance, a global strategy is required to perform an in-use study for all routes of administration. The in-use study should be performed at least twice during drug development.
The first instance is during preparation of a clinical trial application toward Phase I and a trial in healthy individuals. In Phase I, there is already enough information available to design a study and one can already define the type of material to be tested. The second instance is dependent on possible changes in the clinical trial design or drug product formulation. Given these changes, a new or supplemental study could confirm that the drug product compounding and administration with new conditions continues to maintain drug product stability.
When planning an in-use study, information should be gathered on which conditions to be tested. Options include: (i) study the drug product at higher temperature and humidity for Zone III/IV; (ii) use more than one batch; (iii) use end of shelf-life material; (iv) take consideration of the container system, its filling/extraction volume, and need for dilution/reconstitution; (v) possible holding time of storage based on clinical trial site experience; and (vi) specific compatibility with the different material of construction from medical devices of compounding and administration [38].
As the drug product passes through different medical devices (syringes, needles, filters, and nebulizers), it will interact with polymers, such as polypropylene, polyethylene, polyvinylchloride, polyethersulfone, polystyrene, silicone, and other materials, such as stainless steel. For example, the nebulizer chamber of the vibrating mesh Aerogen Solo (Aerogen [39]) comprises Lustran® and polycarbonate, and the jet nebulizer AeroEclipse II (Trudell [40]) contains polypropylene and silicone rubber. The choice of materials will depend on the alignment with the trial site and availability for that route of administration.
Nonetheless, the duration of interfacial contact of the drug product with materials depends on the low doses planned for Phase I/II trials. With that, the challenges to detect drug instability include using qualified methods that have adequate sensitivity and accuracy to detect low drug concentrations.
It is vital to consider the potential material surfaces, test the stability of the drug product with the proposed diluent, use conditions to mimic the most extreme conditions, use a range of concentrations, and take samples from the preparations that will be delivered to the patient (i.e., before compounding, after storage, and following simulation of administration conditions) [41], Particularly for nebulization studies, the sample volumes must be carefully considered because the nebulizer input is ∼2–6 ml and the output depends on the specific formulation. The produced aerosols are not 100% recovered and analytical methods might require higher volumes, which will demand sample pooling [31].
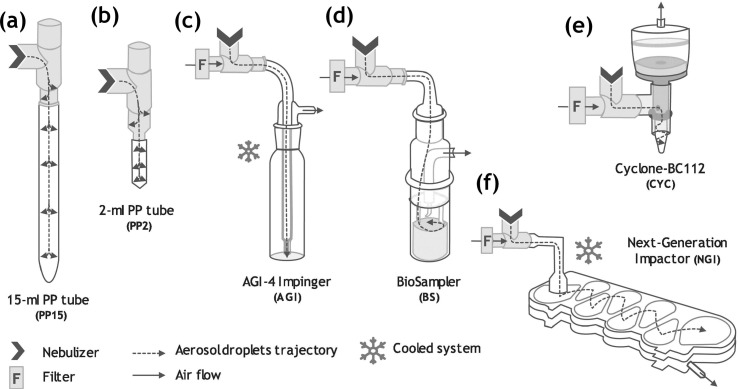
Figure 2 provides examples of devices for aerosol collection using filtration, impaction, condensation, or precipitation. This step should be carefully considered during feasibility planning of nebulization in-use studies [42].
Figure 2.
Possibilities for aerosol collection devices. (a) 15-ml conical polypropylene (PP) tubes, (b) 2-ml PP tubes, (c) AGI-4 Impinger (Ace Glass Inc.), (d) BioSampler (SKC Inc.), (e) Cyclone-BC112 (NIOSH), and (f) Next-Generation Impactor (Copley Scientific Limited). Reproduced, with permission, from [42].
For nebulization-specific parameters, the nebulizer output can be assessed using a next-generation impactor (or laser diffractometry) for definition of aerodynamic size distribution, such as mass median aerodynamic diameters (MMAD) and fine particle fraction (FPF < 5 mm); and with gravimetric methods for active substance delivery rate, total active substance delivered before and after the nebulization cycles, nebulization times, and aerosol recovery [43].
In terms of the characterization of biological activity, antibody, gene, and cell therapy products benefit from advanced technologies. For macromolecules, such as proteins, their inherent complex structure, order, glycosylation, variants and modification because of the manufacturing bioprocess present challenges. Therefore, in terms of molecule characterization, the use of mass spectrometry and infrared spectroscopy is possible, although cation-exchange or capillary electrophoresis high-performance liquid chromatography are used more routinely [44].
For functional assessment, the use of immunoassays, such as ELISAs or surface plasmonic resonance (SPR; e.g., Biacore™) is common for ligand binding and dissociation constants, although cell-based assays are a new option [44]. Similar trends are also associated with the characterization of mRNA vaccines (using virus-like particles in ELISAs) [45]. However, new products take a closer look at selectivity and function, as in the case of immunotherapy platforms, such as oncolytic virus [46] or chimeric antigen receptor T cells (CART-T) [47]. In these, the techniques used include immunoassays for tumour selectivity, donor variability, and T cell recognition using flow cytometry versus specific tumour cell cytotoxicity and cytokine-specific release [48].
In-use extra topics
If in-use stability studies are considerations toward drug product preparation and administration, then upcoming topics on nebulizer administration are important. The ancillary materials that comprise the nebulizer sets might include more strategies to protect the health professional and patient during nebulization, especially in clinical trials of infectious diseases. As for compliance and bias removal during clinical trials, the use of blinding strategies are key, although these might influence the practical activities of drug product preparation and administration; therefore, attention is required to include such strategies during in-use studies, as discussed below. Two last derived topics are then related here to clinical trial development and in-use studies.
In terms of risk management, consideration of fugitive emissions during nebulization is necessary. After aerosol characterization, the drug can be efficiently delivered to, and act in, the target region of the lung. Nebulization generates aerosols and, despite the use of a mask or mouthpiece, nebulization rooms do have increased aerosol particles in the room air for long periods of time. This is not the case for rooms in which bronchoscopies or ventilation are performed [49]. Fugitive emissions are aerosols, derived from either the patient’s exhalation (bioaerosol) or the nebulization system (medical aerosol). For in-use handling of drug products, the excess of aerosol escaping from the system can be translated as drug waste, because it is not being delivered to the lung. This means that a correct dose to be delivered should account for these emissions [50].
According to the USP 800 [51], NBEs can be considered hazardous drugs. If a medical aerosol escapes into room air, it means that all the health professional staff in the room are being exposed to microdoses of the drug product. Therefore, mechanisms to avoid nontargeted administration should be developed.
With the COVID-19 pandemic, the development of aerosolized drugs is one of the aims for new therapeutical products. After drug delivery via inhalation, the patient exhales bioaerosols, which, in the occasion of COVID-19, means numerous infectious aerosol particles [52]. To avoid this, an exhalation filter could be inserted on nebulizers, and the use of mouthpieces instead of masks might provide solutions. Furthermore, new devices or modifications are being developed, including mask open ports, valved masks, aerosol scavengers, and face tents for mask use [50]. The use of this extra filtration step or other ancillary material will influence drug product delivery and its impact should be evaluated, either with a risk assessment or included as variant during the in-use study.
The second topic is about blinding strategies for single or double-blinded clinical trials. During randomized clinical trials, treatment groups cannot be acknowledged by the trial staff, pharmacist, and/or trial participants. Placebo formulations are an essential component of blinding strategies for oral pharmaceutical forms, and are easily manufactured because appearance can be masked with the primary packaging. This is not the case for liquid formulations, where the physical properties are more difficult to disguise. For nebulizer solutions, this difficulty might also occur when nonaqueous or colored formulations disrupt the blinding procedure. The in-use group can also assess the blinding strategies, including efficacy of blinding and the handling procedures that could influence blinding. This includes the use of colored labels for syringes, the use of a blinded staff versus unblinded pharmacists, and the use of labels to cover the nebulizer chamber [53]. This might influence the design of the in-use study because an unblinded pharmacist, the study nurse or the principal investigator requires a clear view of the drug product during preparation to check for foreign/visible particles, volumes during compounding, or unusual change of color.
Concluding remarks
In-use stability studies require networking within drug development teams in the pharmaceutical companies. They also require alignment with the predicted clinical trial design in regards to dose, target population, conditions of administration, and nebulizer preferences. These factors guide production of pharmaceutical formulations that match the individual characteristics of target populations, without altering the aerosol production, delivery, and stability status of the drug product.
The use of compendial guidelines prioritizes the development of sterile drug components for lung delivery, and share parameters of interest with regulatory authorities. Therefore, appraising the compounding steps, materials, and devices during in-use allows the understanding of the need for an alignment with analytical development on methods that incorporate characteristics of NBEs (from particulate matter to product concentration), along with the right sample collection device.
The future of nebulization includes the evaluation of the in-use stability of biological products. Currently, the pharmaceutical industry is going even beyond the use of protein therapeutics and incorporating complex delivery systems and delicate biological cargoes, such as nucleic acids or even cell therapy exclusively for nebulization. It is essential to be up-to-date with the in-use literature as part of the quality management system to understand the potential risks and prepare astute in-use study designs.
Acknowledgments
This review reflects the views of the author and should not be construed to represent any company’s views or policies. I would like to thank the In-Use laboratory at the Pharmaceutical Development of Biologicals, Formulation, Primary Packaging, Device Development, Inhalation Sciences, Analytical Development of Biologicals, R&D Project Management, Clinical Trial Supply, CMC Regulatory Affairs of Boehringer Ingelheim for the experience; and Alysia Cox for scientific review and English language proofreading.
Data availability
No data was used for the research described in the article.
References
- 1.Ricci M.S., et al. In-use physicochemical and microbiological stability of biological parenteral products. Am. J. Heal. Pharm. 2015;72:396–407. doi: 10.2146/ajhp140098. [DOI] [PubMed] [Google Scholar]
- 2.Rau J.L. The inhalation of drugs: advantages and problems. Respir. Care. 2005;50:367–382. [PubMed] [Google Scholar]
- 3.Parray H.A., et al. Inhalation monoclonal antibody therapy: a new way to treat and manage respiratory infections. Appl Microbiol Biotechnol. 2021;105:6315–6332. doi: 10.1007/s00253-021-11488-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthews A.A., et al. Developing inhaled protein therapeutics for lung diseases. Mol Biomed. 2020;1:1–14. doi: 10.1186/s43556-020-00014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.FDA . FDA; Silver Spring: 2021. FDA Purple Book. [Google Scholar]
- 6.Shao J., et al. A cell-based drug delivery system for lung targeting: I. Preparation and pharmacokinetics. Drug Deliv. J. Deliv. Target Ther. Agents. 2001;8:61–69. doi: 10.1080/107175401750176981. [DOI] [PubMed] [Google Scholar]
- 7.Shen H., et al. The interaction between pulmonary fibrosis and COVID-19 and the application of related anti-fibrotic drugs. Front. Pharmacol. 2022;12:1–15. doi: 10.3389/fphar.2021.805535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guilleminault L., et al. Fate of inhaled monoclonal antibodies after the deposition of aerosolized particles in the respiratory system. J. Control. Release. 2014;196:344–354. doi: 10.1016/j.jconrel.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Maillet A., et al. The airways, a novel route for delivering monoclonal antibodies to treat lung tumors. Pharm. Res. 2011;28:2147–2156. doi: 10.1007/s11095-011-0442-5. [DOI] [PubMed] [Google Scholar]
- 10.Gonda I. Is there a future for the respiratory delivery of biologics? OnDrugDelivery. 2019;96:6–10. [Google Scholar]
- 11.Maillet A., et al. Aerodynamical, immunological and pharmacological properties of the anticancer antibody cetuximab following nebulization. Pharm. Res. 2008;25:1318–1326. doi: 10.1007/s11095-007-9481-3. [DOI] [PubMed] [Google Scholar]
- 12.Low S.C., et al. Oral and pulmonary delivery of FSH-Fc fusion proteins via neonatal Fc receptor-mediated transcytosis. Hum. Reprod. 2005;20:1805–1813. doi: 10.1093/humrep/deh896. [DOI] [PubMed] [Google Scholar]
- 13.Bitonti A.J., et al. Pulmonary delivery of an erythropoietin Fc fusion protein in non-human primates through an immunoglobulin transport pathway. Proc. Natl. Acad. Sci. U. S. A. 2004;101:9763–9768. doi: 10.1073/pnas.0403235101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mangal S., et al. Pulmonary delivery of nanoparticle chemotherapy for the treatment of lung cancers: challenges and opportunities. Acta Pharmacol. Sin. 2017;38:782–797. doi: 10.1038/aps.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mishra B., Singh J. In: Targeting Chronic Inflammatory Lung Diseases Using Advanced Drug Delivery Systems. Dua K., Hansbro P.M., Wadhwa R., Haghi M., Pont L.G., Williams K.A., editors. Elsevier; Amsterdam: 2020. Novel drug delivery systems and significance in respiratory diseases; pp. 57–95. [Google Scholar]
- 16.LoBue P.A. Inhaled tobramycin. Chest. 2005;127:1098–1101. doi: 10.1378/chest.127.4.1098. [DOI] [PubMed] [Google Scholar]
- 17.EMA . EMA; Amsterdam: 2003. ICH Harmonised Tripartite Guideline. Q1A(R2): Stability Testing of New Drug Substances and Products. [PubMed] [Google Scholar]
- 18.Capen R., et al. On the shelf life of pharmaceutical products. AAPS PharmSciTech. 2012;13:911–918. doi: 10.1208/s12249-012-9815-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.USP . USP; Rockville: 2016. USP General Chapter 797. Pharmaceutical Compounding—Sterile Preparations. [PubMed] [Google Scholar]
- 20.Hernandez I., et al. Pricing of monoclonal antibody therapies: higher if used for cancer? Am. J. Manag. Care. 2016;24:109–112. [PubMed] [Google Scholar]
- 21.Cantrell L., et al. Stability of active ingredients in long-expired prescription medications. Arch. Intern. Med. 2012;172:1685–1687. doi: 10.1001/archinternmed.2012.4501. [DOI] [PubMed] [Google Scholar]
- 22.UPS . USP; Rockville: 2014. USP General Chapter 795. Pharmaceutical Compounding Nonsterile Preparations. [Google Scholar]
- 23.Sreedhara A., et al. Stability of IgG1 monoclonal antibodies in intravenous infusion bags under clinical in-use conditions. J. Pharm. Sci. 2012;101:21–30. doi: 10.1002/jps.22739. [DOI] [PubMed] [Google Scholar]
- 24.Li J., et al. Interfacial stress in the development of biologics: fundamental understanding, current practice, and future perspective. AAPS J. 2019;21:44. doi: 10.1208/s12248-019-0312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koepf E., et al. Notorious but not understood: how liquid-air interfacial stress triggers protein aggregation. Int. J. Pharm. 2018;537:202–212. doi: 10.1016/j.ijpharm.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 26.Galush W.J., Horst T.A. Vented spikes improve delivery from intravenous bags with no air headspace. J. Pharm. Sci. 2015;104:2397–2400. doi: 10.1002/jps.24466. [DOI] [PubMed] [Google Scholar]
- 27.Krayukhina E., et al. Effects of syringe material and silicone oil lubrication on the stability of pharmaceutical proteins. J. Pharm. Sci. 2015;104:527–535. doi: 10.1002/jps.24184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghazvini S., et al. Evaluating the role of the air-solution interface on the mechanism of subvisible particle formation caused by mechanical agitation for an IgG1 mAb. J. Pharm. Sci. 2016;105:1643–1656. doi: 10.1016/j.xphs.2016.02.027. [DOI] [PubMed] [Google Scholar]
- 29.Khan T.A., et al. Key interactions of surfactants in therapeutic protein formulations: a review. Eur. J. Pharm. Biopharm. 2015;97:60–67. doi: 10.1016/j.ejpb.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Kannan A., et al. In-use interfacial stability of monoclonal antibody formulations diluted in saline i.v. bags. J. Pharm. Sci. 2021;110:1687–1692. doi: 10.1016/j.xphs.2020.10.036. [DOI] [PubMed] [Google Scholar]
- 31.Respaud R., et al. Effect of formulation on the stability and aerosol performance of a nebulized antibody. MAbs. 2014;6:1347–1355. doi: 10.4161/mabs.29938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mayor A., et al. Inhaled antibodies: formulations require specific development to overcome instability due to nebulization. Drug Deliv. Transl. Res. 2021;11:1625–1633. doi: 10.1007/s13346-021-00967-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ehrmann S. Vibrating mesh nebulisers can greater drug delivery to the airways and lungs improve respiratory outcomes? Eur. Respir. Pulm. Dis. 2018;4:33. [Google Scholar]
- 34.Bianco F., et al. Aerosol drug delivery to spontaneously-breathing preterm neonates: lessons learned. Respir. Res. 2021;22:1–31. doi: 10.1186/s12931-020-01585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kishida M., et al. Mouthpiece versus facemask for delivery of nebulized salbutamol in exacerbated childhood asthma. J. Asthma. 2002;39:337–339. doi: 10.1081/jas-120002291. [DOI] [PubMed] [Google Scholar]
- 36.Sécher T., et al. Aggregates associated with instability of antibodies during aerosolization induce adverse immunological effects. Pharmaceutics. 2022;14:671. doi: 10.3390/pharmaceutics14030671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chow M.Y.T., et al. Inhalation delivery technology for genome-editing of respiratory diseases. Adv. Drug Deliv. Rev. 2021;168:217–228. doi: 10.1016/j.addr.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.ICH . ICH; London: 2018. ICH Harmonised Tripartite Guideline. Q1F Stability Data Package for Registration Applications in Climatic Zones III and IV. [Google Scholar]
- 39.Aerogen . Aerogen; Galway: 2016. Aerogen Solo: System Instruction Manual. [Google Scholar]
- 40.Trudell . Trudell; London, ONT: 2020. AeroEclipse II. Product Sheet. [Google Scholar]
- 41.de Jong, I. and Liu, L. (2022) Physicochemical in‐use studies: industry experts insights. www.casss.org/docs/default-source/cmc-strategy-forum-north-america/2022-cmc-na-speaker-presentations/de-jong-genentech-liu-seagen-2022.pdf?sfvrsn54e09af80_5 [Accessed November 23, 2022].
- 42.Bodier-Montagutelli E., et al. Protein stability during nebulization: mind the collection step! Eur. J. Pharm. Biopharm. 2020;152:23–34. doi: 10.1016/j.ejpb.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 43.Abdelrahim M.E., Chrystyn H. Aerodynamic characteristics of nebulized terbutaline sulphate using the next generation impactor (NGI) and CEN method. J. Aerosol. Med. Pulm. Drug Deliv. 2009;22:19–28. doi: 10.1089/jamp.2008.0650. [DOI] [PubMed] [Google Scholar]
- 44.Wang X., et al. Molecular and functional analysis of monoclonal antibodies in support of biologics development. Protein Cell. 2018;9:74–85. doi: 10.1007/s13238-017-0447-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sanyal G. Development of functionally relevant potency assays for monovalent and multivalent vaccines delivered by evolving technologies. npj Vaccines. 2022;7:50. doi: 10.1038/s41541-022-00470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.EMA . EMA; Amsterdam: 2009. ICH Considerations: Oncolytic Viruses. [Google Scholar]
- 47.FDA . FDA; Silver Spring: 2011. Potency Tests for Cellular and Gene Therapy Products. [Google Scholar]
- 48.Kiesgen S., et al. Comparative analysis of assays to measure CAR T-cell-mediated cytotoxicity. Nat. Protoc. 2021;16:1331–1342. doi: 10.1038/s41596-020-00467-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.O'Neil C.A., et al. Characterization of aerosols generated during patient care activities. Clin. Infect. Dis. 2017;65:1342–1348. doi: 10.1093/cid/cix535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harnois L.J., et al. Efficacy of various mitigation devices in reducing fugitive emissions from nebulizers. Respir. Care. 2022;67:394–403. doi: 10.4187/respcare.09546. [DOI] [PubMed] [Google Scholar]
- 51.USP . USP; Rockville: 2018. USP General Chapter 800. Hazardous Drugs: Handling in Health Care Settings. [Google Scholar]
- 52.Hui D.S., et al. Exhaled air and aerosolized droplet dispersion during application of a jet nebulizer. Chest. 2009;135:648–654. doi: 10.1378/chest.08-1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schulz K.F. Assessing allocation concealment and blinding in randomised controlled trials: why bother? Evid. Based Nurs. 2001;4:4–6. doi: 10.1136/ebn.4.1.4. [DOI] [PubMed] [Google Scholar]
- 54.EMA . EMA; Amsterdam: 2012. Guideline on the Pharmaceutical Quality of Inhalation and Nasal Products Draft. [Google Scholar]
- 55.EMA . EMA; Amsterdam: 2018. EMEA/CHMP/SWP/28367/07 Rev. 1 Guideline on Strategies to Identify and Mitigate Risks for First-in-Human and Early Clinical Trials with Investigational Medicinal Products. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.EMA . EMA; Amsterdam: 2001. CPMP/QWP/2934/99 Note for Guidance on In-Use Stability Testing of Human Medicinal Products. [Google Scholar]
- 57.FDA . FDA; Silver Spring: 2002. Guidance for Industry Nasal Spray and Inhalation Solution, Suspension, and Spray Drug Products – Chemistry, Manufacturing, and Controls Documentation. [Google Scholar]
- 58.FDA . FDA; Silver Spring: 1993. Reviewer Guidance for Nebulizers, Metered Dose Inhalers, Spacers and Actuators. [Google Scholar]
- 59.Japanese Pharmacopeia . Pharmaceuticals and Medical Devices Agency; Tokyo: 2005. G-08 Preparations for Inhalation: Aerodynamic Assessment of Fine Particles. [Google Scholar]
- 60.UPS . USP; Rockville: 2012. USP General Chapter 601. Physical Tests and Determinations: Aerosols. Nasal Sprays, Metered-Dose Inhalers, and Dry Powder Inhalers. [Google Scholar]
- 61.UPS . USP; Rockville: 2012. USP General Chapter 1049. Quality of Biotechnological Products: Stability Testing of Biotechnological. [Google Scholar]
- 62.UPS . USP; Rockville: 2013. USP General Chapter 71. Sterility Tests. [Google Scholar]
- 63.UPS . USP; Rockville: 2012. USP General Chapter 85. Bacterial Endotoxins Test. [Google Scholar]
- 64.ICH . ICH; London: 2009. ICH Harmonised Tripartite Guideline. Q8 (R2) Pharmaceutical Development, Step 5: Note for Guidance on Pharmaceutical Development. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.