Abstract
To evaluate the clinical efficacy of 1-stage anterior focus debridement, interbody bone graft, and anterior instrumentation and fusion in the treatment of short segment thoracic tuberculosis with paraplegia or incomplete paralysis. A total of 16 adult patients with short segment thoracic spinal thoracic tuberculosis who underwent surgery were enrolled in this retrospective study. All patients received anterior focus debridement, interbody bone graft and anterior instrumentation and fusion. All patients were followed up for 24 to 48 months. Clinical manifestations, laboratory examinations, neurological symptoms, bone fusion and imaging results were analyzed. All patients successfully underwent operations. The symptoms of chest and back pain were alleviated and even disappeared during postoperative 1 to 6 months. There was no recurrence. All patients got bony spinal fusion within postoperative 4 to 8 months assessed by spinal X-ray film. The levels of erythrocyte sedimentation rate and C-reactive protein were significantly decreased from 72.6 ± 27.5 mm/h and 75.7 ± 25.9 mg/L to 15.9 ± 4.6mm/h and 4.7 ± 2.0mg/L at the final follow-up, respectively (P < .05). The thoracic kyphosis angle was also notably decreased from 15.0 ± 3.4° to 9.1 ± 1.9° after operation(P < .05). During the follow-up, the symptom of paraplegia or incomplete paralysis was significantly improved. Neurologic status in all patients was also improved to some extent. The combination of 1-stage anterior focus debridement, interbody bone graft and anterior instrumentation and fusion is an effective and feasible treatment method for short segmental thoracic tuberculosis with paraplegia or incomplete paralysis.
Keywords: anterior instrumentation and fusion, interbody bone graft, one-stage anterior focus debridement, paraplegia, short segmental thoracic tuberculosis
1. Introduction
In recent years, the incidence of spinal tuberculosis (TB) has been increasing again due to population growth, human immunodeficiency virus infection, diabetes mellitus, drug resistance, et cetera.[1] Spinal tuberculosis is 1 of the most common types of extrapulmonary tuberculosis, accounting for the first place in total bone and joint tuberculosis.[2] It is a severe spinal disease that frequently causes kyphotic deformity, neurologic deficit and even spinal cord compression. Particularly, spinal tuberculosis with paraplegia or incomplete paralysis accounts for 10% to 46% of all spinal tuberculosis cases.[3] If spinal tuberculosis is not diagnosed and treated in time, it may result in serious complications.
Spinal tuberculosis forms abscesses, sequestrum, and tuberculous granulation tissues, which enter the spinal canal to compress the spinal cord to cause nerve damage or even paraplegia. Tuberculous spondylitis (Pott’s disease), a common extrapulmonary manifestation of tuberculosis, typically presents with back pain, tenderness, paraparesis/paraplegia, and various constitutional symptoms. Although there have been great advances in anti-TB drug treatment, surgical management is still critical. Based on combination chemotherapy, active surgical treatment has been widely accepted, which can effectively shorten the treatment cycle, promote the cure, reduce the morbidity, and improve the quality of life.[4]
In most cases, TB destroys the load-bearing area of the front of the spine, also known as anterior column. Paravertebral abscess formation is often associated. Destruction of the anterior column not only alters the biomechanics and stability of the spine, but also increases the risk of progression of kyphosis and paraplegia.[5,6] It has been reported that anterior focus debridement combined with interbody bone graft is a classic surgical procedure for the treatment of spinal TB.[7] It can directly reach the lesion site with a larger operative horizon to completely remove lesions. Moreover, anterior surgery can completely expose the lesions that can be completely removed to reduce the compression of the spinal cord. Bone graft can correct kyphotic deformities and reestablish spinal stability.[8] Therefore, anterior surgery is more suitable for spinal TB with paraplegia or incomplete paralysis, especially Pott’s paralysis of short segment thoracic TB.
In this study, we investigated the clinical efficacy of 1-stage anterior focus debridement, interbody bone graft, and anterior instrumentation and fusion in the treatment of short segment thoracic TB with paraplegia or incomplete paralysis.
2. Subjects and Methods
2.1. Subjects
We confirmed that all methods were carried out in accordance with relevant guidelines and regulations. This study was approved by the Institutional Ethics Committee for Medical Scientific research of Xi’an Chest Hospital at April 7th, 2020 (Approval No.: 2020-S0022). Written informed consent were obtained from all patients. From September 2013 to March 2017, 16 patients with short segment thoracic vertebrae tuberculosis with paraplegia or incomplete paralysis who underwent surgery in our hospital were enrolled in the study. Inclusion criteria were as follows: patients with thoracic tuberculous with destruction of 1 or 2 segments of the vertebral body; patients with a mild kyphotic deformity (Cobb angle < 25º); patients with intermittent back pain caused by spinal instability; the effect of anti-tuberculosis treatment was not ideal; patients without the contraindications of anterior thoracotomy; patient who had developed paraplegia or incomplete paralysis. Exclusion criteria were as follows: patients with 3 or more thoracic vertebral lesions; patient who did not have paraplegia or incomplete paralysis; patients with severe kyphotic deformity (Cobb angle > 25º); patients with the contraindications of anterior thoracotomy; and patients who cannot tolerate 1 lung ventilation.
2.2. The diagnosis criteria
The diagnosis criteria of spinal tuberculosis was guided by the laboratory examinations (anemia, hypoproteinemia, T-spot, tuberculosis antibody, erythrocyte sedimentation rate [ESR], and C-reactive protein [CRP]), imaging (spinal X-ray films, computed tomography, and agentic resonance imaging) and patients’ symptoms (local pain and percussion pain accompanied with fever, night sweats, and neurological dysfunction). All diagnoses were confirmed by postoperative pathology examinations.
2.3. Preoperative procedure
All patients received at least 2 to 4 weeks of first-line anti-tuberculous treatment (rifampicin 0.45 g, isoniazid 0.4 g, pyrazinamide 1.5 g, and ethambutol 0.75 g) before operation. Supporting therapy and symptomatic treatment were conducted when the patients were hospitalized. The doses of anti-TB drugs were appropriately increased in patients with tuberculosis in other parts of the body, or in patients weighing more than 50 kilograms. For patients with paraplegia or incomplete paralysis, surgery should be performed as early as possible.
2.4. Operative technique
Informed consent for surgery was signed by the patients. Patients who received tracheal intubation with a double lumen tube were in the left decubitus position. The side lobe was collapsed intraoperatively. A standard right anterior posterolateral surgical incision was performed. Skin and subcutaneous tissues and the right latissimus dorsa muscle and pectoralis major muscle were dissected layer by layer. The upper rib corresponding to the diseased vertebral body on the right side was exposed, and some of the ribs were stripped, cut, and snipped as autograft. The chest was opened with a thoracotomy, the right lung was collapsed, and the right thoracic spine was exposed. The right diseased vertebral body and anterior fascia were examined with obvious swelling and abnormal color. The paravertebral abscess was aspirated with a syringe as a culture specimen. The anterior fascia of the diseased vertebral body was cut longitudinally, and segmental vessels were ligated. Cheese-like substance, necrotic granulation tissues, dead bone particles and other lesions were completely removed, while normal vertebral bone tissues were retained. The compression of the spinal cord was completely relieved. The wound was washed repeatedly with normal saline, and streptomycin (1 g) was administered. Autogenous bone and graft fusion with a titanium cage strut combined with an anterior vertebral screw-plate internal fixation system were used to recover the normal spinal curvature and reconstruct the spine stability (Figs. 1–3). The drainage tube was placed postoperatively, and culture specimens were sent for pathological examination.
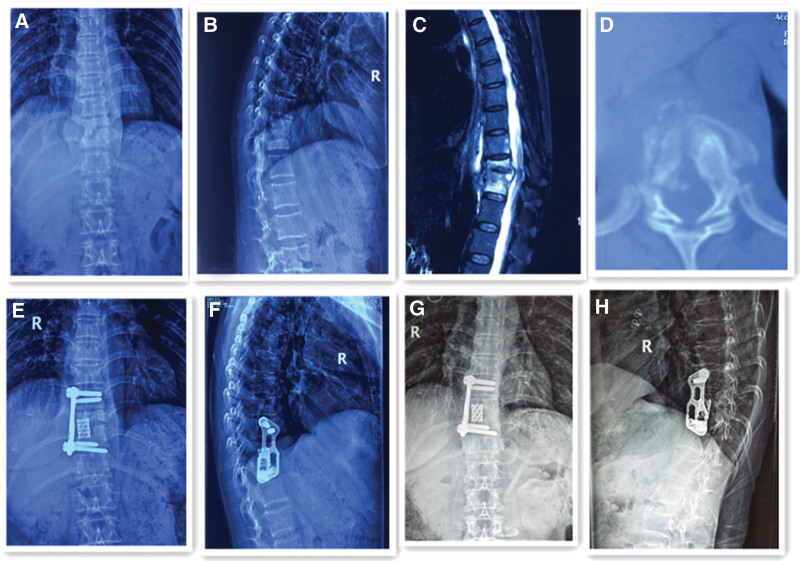
Figure 1.
Forty-eight-year-old female with short segment thoracic vertebra tuberculosis (T10-11 level). (A, B) Preoperative frontal and lateral x-rays showed bone destruction in the 10/11 vertebral body and narrowing of the vertebral space, with a kyphosis angle of 20°. (C) Preoperative magnetic resonance imaging scan. (D) Preoperative computed tomography scan demonstrate vertebral body destruction. (E, F) Radiographs postoperatively showing well-positioned internal fixation. (G, H) Radiographs showing satisfactory focal clearance and strut graft stability at the final follow-up.
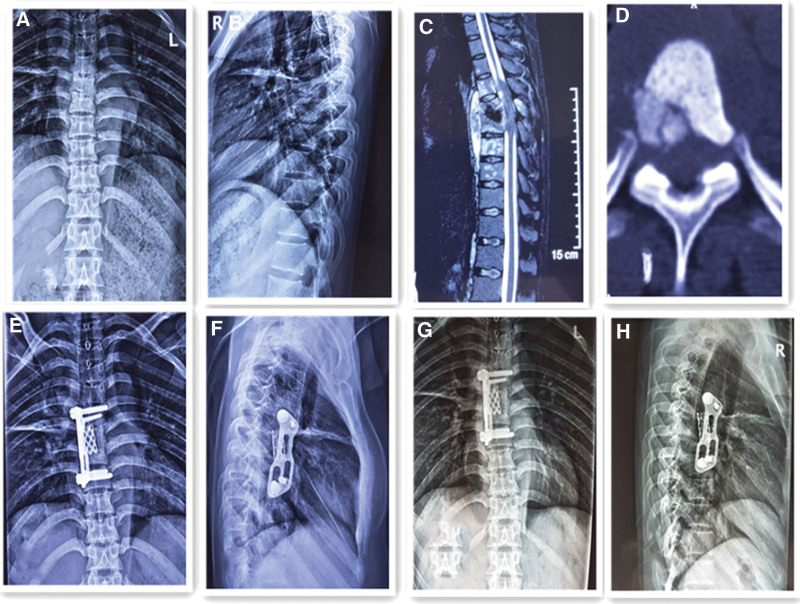
Figure 3.
Thity-two-year-old girl with short segment thoracic vertebra tuberculosis (T10-T11 level). (A, B) Preoperative frontal and lateral x-rays showed bone destruction in the 10/11 vertebral body and narrowing of the vertebral space, with a kyphosis angle of 16°. (C) Preoperative computed tomography scans demonstrate vertebral body destruction. (D) Preoperative magnetic resonance imaging scan shows vertebral body destruction and abscess. The lesion compressed the dural sac. (E, F) Radiographs postoperatively showing well-positioned internal fixation and Kyphotic deformity was corrected. (G, H) Postoperative axial CT showed satisfactory internal fixation device at the final follow-up. CT = computed tomography.
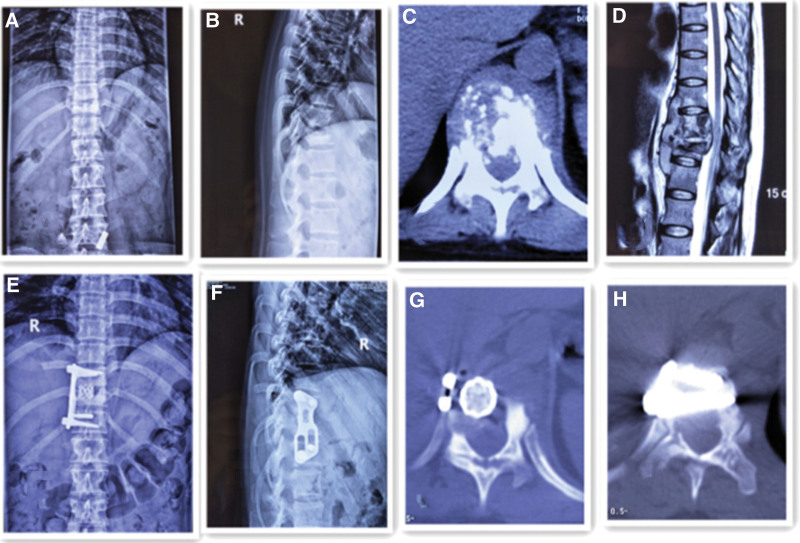
Figure 2.
Fifty-six-year-old man with short segment thoracic vertebra tuberculosis (T6-T7 level). (A, B) Preoperative frontal and lateral x-rays showed bone destruction in the 6/7 vertebral body and narrowing of the vertebral space, with a kyphosis angle of 15°. (C) Preoperative magnetic resonance imaging scan shows vertebral body destruction and abscess. (D) Preoperative computed tomography scans demonstrate vertebral body destruction. (E, F) Radiographs postoperatively showing well-positioned internal fixation. (G, H) Radiographs showing satisfactory focal clearance and strut graft stability at the final follow-up.
2.5. Postoperative care
After the operation, the postural drainage was adopted, and complete lung expansion was confirmed by radiography. The drainage tube was pulled out when the 24-hour drainage flow was < 50 mL. Postoperative anti-TB, anti-infection treatment, electrocardiogram monitoring and other comprehensive treatment were provided. Patients continued to perform HREZ chemotherapy. Nutritional support was provided in patients with postoperative anemia, low serum albumin levels, or loss of appetite. Patients were required to get out of bed for 2 weeks after the operation. After discharge, anti-TB therapy was maintained for 18 to 24 months.
2.6. Evaluation of clinical outcomes
All patients were examined clinically and radiologically at 1, 3, 6 and 12 months after the operation and at the last follow-up. The levels of ESR and CRP were the important indexes to evaluate the activity of short segment thoracic vertebrae tuberculosis with paraplegia or incomplete paralysis. Preoperative and postoperative Frankel Grade, kyphotic Cobb angle, and bony fusion were recorded to evaluate the symptom changes (Table 1). The definition of Kyphosis Angle was referred to the following literature.[9] According to the lateral X-ray, the kyphotic angel was the angle formed by 2 lines obtained by joining the antero-superior and postero-superior corners of the above lesions, and the antero-inferior and postero-inferior corners of the vertebral below lesion. Postoperative radiographs were conducted to assess the bony fusion level using the radiologic criteria of Bridwell.[10]
Table 1.
Summary of the patients’ data.
| Patients (no.) | Age (yr)/sex | Levels | Follow-up (mo) | Kyphosis angle (º) | Frankel grade | Fusion (mo) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PRE | ▲POST | ▼FFU | PRE | POST | FFU | |||||
| 1 | 23/M | T8–T9 | 24 | 19 | 11 | 11 | A | B | D | 4 |
| 2 | 47/F | T9–T10 | 36 | 12 | 8.4 | 10 | A | B | E | 5 |
| 3 | 48/F | T8–T9 | 48 | 14 | 10.6 | 11 | C | D | E | 5 |
| 4 | 56/M | T6–T7 | 48 | 15 | 10 | 10 | B | C | D | 6 |
| 5 | 57/M | T9–T10 | 42 | 17 | 9 | 9 | B | C | E | 5 |
| 6 | 37/M | T5–T6 | 24 | 18 | 10.2 | 12 | A | B | D | 4 |
| 7 | 42/F | T7–T8 | 24 | 13 | 7.2 | 8 | A | B | E | 5 |
| 8 | 29/M | T8–T9 | 30 | 12 | 7 | 6 | B | D | E | 4 |
| 9 | 32/F | T10–T11 | 36 | 16 | 8.8 | 10 | C | D | E | 4 |
| 10 | 48/F | T10–T11 | 24 | 20 | 10.3 | 12 | C | D | E | 5 |
| 11 | 45/F | T9–T10 | 36 | 18 | 9.6 | 11 | A | C | D | 6 |
| 12 | 55/M | T9–T10 | 48 | 14 | 9.8 | 11 | B | C | E | 6 |
| 13 | 24/M | T9–T10 | 24 | 11 | 5.6 | 7 | A | C | E | 5 |
| 14 | 62/M | T8–T9 | 48 | 13 | 13 | 11 | B | D | E | 6 |
| 15 | 74/F | T7–T8 | 42 | 15 | 8 | 10 | C | D | D | 8 |
| 16 | 61/F | T6–T7 | 36 | 13 | 6.4 | 6 | C | D | E | 6 |
| Mean values | 46.3 ± 14.5 | 35.6 ± 9.6 | 15.0 ± 3.4 | 9.1 ± 1.9 | 9.7 ± 1.9 | 5.3 ± 1.1 | ||||
FFU = final follow-up, P = .041, POST = 4 weeks postoperation, PRE = preoperation, t = –2.239, t = 8.969.
Analyzed by paired t-test, comparing 4 weeks postoperative with preoperative in Kyphosis angle, P = .000, ▼Analyzed by paired t-test, comparing final follow-up with 4 weeks postoperative in Kyphosis angle.
2.7. Statistical analysis
SPSS statistical software (IBM Corp.) was used to perform statistical analysis. The differences between the preoperative and postoperative indicators were analyzed using the independent sample t test. P < .05 was considered statistically significant.
3. Results
3.1. Basic clinical characteristics
There were 7 males and 9 females. They aged from 23 to 74 years, with an average age of 46.3 ± 14.5 years. Preoperative images showed that there was vertebral body destruction, intervertebral space collapse, paravertebral abscess and intraspinal invasion. There was 1 case of thoracic 5/6 vertebral destruction, 2 cases of thoracic 6/7 vertebral destruction, 2 cases of thoracic 7/8 vertebral destruction, 4 cases of thoracic 8/9 vertebral destruction, 5 cases of thoracic 9/10 vertebral destruction and 2 cases of thoracic 10/11 vertebral destruction.
All patients successfully underwent operation. During the follow-up, spinal paraplegia or incomplete paralysis was significantly improved in all patients. The symptoms of chest and back pain were alleviated or even disappeared within postoperative 1 to 6 months. Patients were followed up for 24 to 48 months, with an average time of 35.6 ± 9.6 months. There was no recurrence among the 16 patients. They all got bony spinal fusion within 4 to 8 months after surgery, which was assessed by spinal X-ray film and/or computed tomography scan.
3.2. The levels of ESR and CRP were decreased after operation
The preoperative ESR and CRP levels in the 16 patients were 72.6 ± 27.5 mm/h and 75.7 ± 25.9 mg/L, respectively. They were significantly decreased to 46.6 ± 24.1 mm/h and 41.6 ± 15.0 mg/L at 4 weeks after surgery, and even to 15.9 ± 4.6 mm/h and 4.7 ± 2.0 mg/L at the final follow-up, respectively (Table 2).
Table 2.
Laboratory data of all patients.
| n | ESR (mm/h) | CRP (mg/L) | ||||
|---|---|---|---|---|---|---|
| PRE | POST | FFU | PRE | POST | FFU | |
| 16 | 72.6 ± 27.5 | 46.6 ± 24.1● | 15.9 ± 4.6▪ | 75.7 ± 25.9 | 41.6 ± 15.0▫ | 4.7 ± 2.0◊ |
CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, FFU = final follow-up, P = .000, P = .000, POST = 4 weeks postoperation, PRE = preparation, t = 10.639, t = 5.194, t = 5.776, t = 6.654.
● Analyzed by paired t-test, comparing 4 weeks postoperative with preoperative in ESR, □ Analyzed by paired t-test, comparing 4 weeks postoperative in CRP, P = .000; Analyzed by paired t-test, comparing final follow-up with 4 weeks postoperative in ESR, P = .000; ◊ Analyzed by paired t-test, comparing final follow-up with 4 weeks postoperative in ESR.
3.3. Neurologic functions and symptoms were improved by the operation
Neurological symptoms of all patients were manifested as complete paraplegia or incomplete paralysis, lower limb weakness, chest sensation or related numbness and paresthesia. Neurological functions were evaluated by the Frankel classification. All patients had improved function status at different degrees. During the follow-up, spinal paraplegia was significantly improved in all patients. Neurologic status of 3 patients with grade A in preoperative neurologic deficits was recovered to normal, that of 4 patients with grade B was recovered to normal, that of 4 patients with grade C was recovered to normal, that of 3 patients with grade A was recovered to grade D, that of 1 patient with grade B was recovered to grade D, and that of 1 patient with grade C was recovered to grade D. Moreover, the thoracic kyphosis angle was ameliorated from preoperative 15.0 ± 3.4° to postoperative 9.1 ± 1.9°. At the final follow-up, the loss of correction was only 0.6°. It still significantly improved in comparison to the preoperative measurements (Table 1).
3.4. Complications
There were 3 cases of postoperative intercostal neuralgia, and 4 of electrolyte disturbance, 6 of anemia and hypoproteinemia. All of the complications were relieved after symptomatic treatment. There were no patients with pneumothorax or cerebrospinal fluid leak. Wounds were healed without chronic infection or sinus formation. There were no complications related to instrumentation. There was only a small amount of pleural effusion in all patients after surgery, which had been absorbed at 3 months after operation.
4. Discussion
Vertebral body lesions caused by tuberculosis always lead to the development of kyphosis, paravertebral abscesses, and even progressive neurological impairment.[11,12] Neurological impairment is more common in thoracic tuberculosis than elsewhere in spinal tuberculosis. Due to the narrower spinal canal, there are physiological kyphosis in the thoracic region, and greater biomechanical forces in the thoracolumbar region. Godlwana et al have reported that thoracic spinal tuberculosis accounts for 52% of all spinal tuberculosis cases with neurological deficits.[13] Therefore, patients who met these characteristics were enrolled in the retrospective study. Our results revealed that Pott’s disease or incomplete paralysis was primarily caused by nerve compression by epidural abscesses, tuberculous debris, necrotic intervertebral discs, and caseous and granulomatous tissue.
It has been reported that although patients with spinal tuberculosis have actively received anti-tuberculosis treatment, there are still 3% to 5% patients with severe progression followed by paraplegia or incomplete paralysis.[14] Moreover, surgical intervention is very necessary for patients with severe progression.[15] Various surgical techniques have been used to treat spinal tuberculosis, but there are few studies on short segmental thoracic tuberculosis with paraplegia or incomplete paralysis. We found that anterior approach was very suitable for patients with short segment thoracic tuberculosis accompanied by paraplegia or incomplete paralysis. Several severe complications related to anterior surgical approaches to the thoracic spine have been reported.[16,17] Anterior debridement and bone graft directly and thoroughly enable surgeons to treat thoracic spinal tuberculosis with paraplegia or incomplete paralysis, which are more favorable for biomechanical reconstruction. Anterior internal fixation can still maintain the spinal stability and correction of kyphosis when tuberculosis invades short thoracic vertebra segments. The anterior approach enables surgeons to directly reach the lesion site, and operators also have a more spacious and a direct field of vision, simplifying the operative procedures.[18]
In our study, we carried out 1-stage anterior focus debridement, interbody bone graft, and anterior instrumentation and fusion in the surgical treatment of short segment thoracic tuberculosis. The operation went smoothly, and there were no serious complications after the operation. All patients obtained satisfactory functional restoration and recovery from short segment tuberculosis through the operation within about a 48-month follow-up. We believe that 1-stage anterior surgical indications mainly are as follows: The damaged portion of the vertebra being located in the anterior and middle columns of the spine; the abscess or bone mass invades the anterior wall of the spinal canal causing compression and resulting in paraplegia or incomplete paralysis; intractable thoracic pain; laminectomy having been performed and posterior bone graft fusion being prevented; and when the number of damaged vertebrae is < 3.[19] Patients who did not meet these conditions were excluded.
It has been reported that most spinal tuberculosis operations are performed with autologous ribs, autologous ilium or allograft fusion.[20] However, due to their own characteristics, the ribs are tenuous. They do not provide adequate stability to the anterior column, because of plastic deformation and the small surface area of contact with the adjacent normal vertebral bodies.[21] Many recent studies have reported that titanium mesh cages show potential for reliable spinal reconstruction, high bone fusion, sufficient sagittal profile maintenance, and low implant-related problems.[22] Especially, Zhang et al[23] have reported that titanium mesh with autologous ribs is used for fusion with satisfactory short-term follow-up with several advantages. During the operation, we cut autogenous ribs into particles to implant into the titanium mesh, which was then implanted between the remaining thoracic vertebrae, thus maintaining immediate stability and good compression force. The larger load-bearing surface of the titanium mesh provides a stable interfacial strength. It is mechanically strong enough to prevent discrete loss of height from a fused motion segment.[24] In our study, all patients used the titanium mesh cage, and they achieved bone fusion.
Anterior spinal surgery may suffer the disadvantages of greater surgical trauma and more complications, including vascular and visceral injury, chylous leakage and others. Subsidence of titanium mesh cages is reported in anterior column reconstruction after anterior spine surgery.[25] However, these defects did not appear during surgery, and these complications also did not appear during follow-up in our study. It may be related to our years of experience in thoracic surgery and our proficiency in open-heart surgery. Moreover, it may also be related to the limited extent of damage and minor injury of short-segment vertebral tuberculosis. Our results showed that no serious complications occurred after the operation. No complications of atelectasis and aggravation of pulmonary tuberculosis were found. All patients had only a small amount of pleural effusion after surgery, which had been absorbed at the third month after the operation. There were 3 cases of postoperative intercostal neuralgia, 4 cases of electrolyte disturbance, and 6 cases of anemia and hypoproteinemia. They were all relieved after symptomatic treatment. There was no case of pneumothorax and no case of cerebrospinal fluid leak. Wounds were healed without chronic infection or sinus formation. There were no complications related to instrumentation, which may be related to our experience as a specialist tuberculosis hospital. However, tuberculosis cure still relies on formal chemotherapy.[26] Sixteen patients in our study had sturdy implant and favorable curative states. A titanium cage supplemented by autologous bone or allograft bone graft achieved satisfying outcomes in our study. At the last follow-up, all patients recovered well without breakage or transposition of the implant or kyphosis recurrence. All patients had achieved bone fusion, relief from pain, and neurological recovery or significant improvement.
There are also several limitations in this study. Firstly, this is a retrospective study with a shorter follow-up period, which may affect the reliability of the evaluation results. Secondly, a few eligible cases were included, and clinical studies with large samples were lacking, which may cause a certain degree of bias.
One-stage anterior focus debridement, interbody bone graft, and anterior instrumentation and fusion are suitable and effective surgical treatment methods for short segment thoracic tuberculosis complicated with paraplegia or incomplete paralysis. Surgery should be based on the characteristics of the patient’s thoracic vertebra lesions and specific conditions to develop a personalized program. Adequate and necessary systemic anti-tuberculosis treatment remains essential. Comprehensive measures must be taken to improve the cure rate of short segmental thoracic tuberculosis with paraplegia or incomplete paralysis. Meanwhile, further studies with a large number of cases and longer follow-up will be necessary.
Acknowledgements
We acknowledge Huijun Zhang, Zenghui Lu, Chao Ding and Lin Wei for their assistance with database collection.
Author contributions
Conceptualization: Zenghui Lu, Huijun Zhang.
Data curation: Zenghui Lu, Chao Ding, Lin Wei, Huijun Zhang.
Formal analysis: Chao Ding, Lin Wei, Huijun Zhang.
Investigation: Huijun Zhang.
Methodology: Zenghui Lu, Huijun Zhang.
Project administration: Huijun Zhang.
Resources: Huijun Zhang.
Writing – original draft: Zenghui Lu, Huijun Zhang.
Writing – review & editing: Zenghui Lu, Chao Ding, Lin Wei, Huijun Zhang.
Abbreviations:
- CRP =
- C-reactive protein
- ESR =
- erythrocyte sedimentation rate
- TB =
- thoracic tuberculosis
Written informed consent was obtained from all patients. The study protocol was approved by the Institutional Ethics Review Board of Xi’an Chest Hospital (Approval No.: 2020-S0022).
All authors agree to be submitted for publication. Written consent to publish patient identifiable information and data was obtained from the patients.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Lu Z, Ding C, Wei L, Zhang H. One-stage anterior focus debridement, interbody bone graft, and anterior instrumentation and fusion in the treatment of short segment TB. Medicine 2022;101:50(e32210).
Contributor Information
Zenghui Lu, Email: luzenghuidr@163.com.
Chao Ding, Email: captain19982003@sina.com.
Lin Wei, Email: abroad520@sina.com.
References
- [1].Wibaux C, Moafo-Tiatsop M, Andrei I, et al. Changes in the incidence and management of spinal tuberculosis in a French university hospital rheumatology department from 1966 to 2010. Joint Bone Spine. 2013;80:516–9. [DOI] [PubMed] [Google Scholar]
- [2].Wang Z, Wu Q, Geng G. Anterior debridement and bone grafting with posterior single-segment internal fixation for the treatment of mono-segmental spinal tuberculosis. Injury. 2013;44:253–7. [DOI] [PubMed] [Google Scholar]
- [3].Kumar A, Sahu BP. Ghost vertebra: do we need to reconsider treatment strategy for sub-axial cervical spine tuberculosis? J Neurosci Rural Pract. 2013;4:237–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cheng ZH, Wang J, Zheng QX, et al. Anterolateral radical debridement and interbody bone grafting combined with transpedicle fixation in the treatment of thoracolumbar spinal tuberculosis. Medicine (Baltim). 2015;94:e721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rajasekaran S. Natural history of Pott’s kyphosis. Eur Spine J. 2013;22:634–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zeng H, Shen X, Luo C, et al. Comparison of three surgical approaches for cervicothoracic spinal tuberculosis: a retrospective case-control study. J Orthop Surg Res. 2015;10:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Luk KD. Commentary: instrumentation in the treatment of spinal tuberculosis, anterior or posterior. Spine. 2011;11:734–6. [DOI] [PubMed] [Google Scholar]
- [8].Li ZW, Li ZQ, Tang BM, et al. Efficacy of one-stage posterior debridement and bone grafting with internal fixation in the treatment of monosegmental thoracolumbar tuberculosis. World Neurosurg. 2019;121:e843–51. [DOI] [PubMed] [Google Scholar]
- [9].Zhang HQ, Lin MZ, Shen KY, et al. Surgical management for multilevel noncontiguous thoracic spinal tuberculosis by single-stage posterior transforaminal thoracic debridement, limited decompression, interbody fusion, and posterior instrumentation (modified TTIF). Arch Orthop Trauma Surg. 2012;132:751–7. [DOI] [PubMed] [Google Scholar]
- [10].Bridwell KH, Lenke LG, McEnery KW, et al. Anetrior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 1995;20:1410–8. [PubMed] [Google Scholar]
- [11].Liu HP, Luo J, Wang XD, et al. Efficacy of surgery via the single anterior and single posterior approaches for treatment of thoracic spinal tuberculosis. J Int Med Res. 2020;48:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905–13. [DOI] [PubMed] [Google Scholar]
- [13].Godlwana L, Gounden P, Ngubo P, et al. Incidence and profile of spinal tuberculosis in patients at the only public hospital admitting such patients in KwaZulu-Natal. Spinal Cord. 2008;46:372–4. [DOI] [PubMed] [Google Scholar]
- [14].Rajasekaran S, Soundararajan DCR, Shetty AP, et al. Spinal tuberculosis: current concepts. Global Spine J. 2018;8:96S–108S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dunn RN, Ben Husien M. Spinal tuberculosis: review of current management. Bone Joint J. 2018;100-B:425–31. [DOI] [PubMed] [Google Scholar]
- [16].Tuli SM. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res. 2007;460:29–38. [DOI] [PubMed] [Google Scholar]
- [17].ointillart V, Aurouer N, Gangnet N, et al. Anterior approach to the cervicothoracic junction without sternotomy: a report of 37 cases. Spine (Phila Pa 1976). 2007;32:2875–9. [DOI] [PubMed] [Google Scholar]
- [18].Benli IT, Kaya A, Acaroğlu E. Anterior instrumentation in tuberculous spondylitis: is it effective and safe? Clin Orthop Relat Res. 2007;460:108–16. [DOI] [PubMed] [Google Scholar]
- [19].Zhang H, Zeng K, Yin X, et al. Debridement, internal fixation, and reconstruction using titanium mesh for the surgical treatment of thoracic and lumbar spinal tuberculosis via a posterior-only approach: a 4-year follow-up of 28 patients. J Orthop Surg Res. 2015;10:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Govender S, Kumar KP. Cortical allografts in spinal tuberculosis. Int Orthop. 2003;27:244–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Govender S, Parbhoo AH. Support of the anterior column with allografts in tuberculosis of the spine. J Bone Joint Surg Br. 1999;81:106–9. [DOI] [PubMed] [Google Scholar]
- [22].Sundararaj GD, Amritanand R, Venkatesh K, et al. The use of titanium mesh cages in the reconstruction of anterior column defects in active spinal infections: can we rest the crest? Asian Spine J. 2011;5:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zhang HQ, Li M, Wang YX, et al. Minimum 5-year follow-up outcomes for comparison between titanium mesh cage and allogeneic bone graft to reconstruct anterior column through posterior approach for the surgical treatment of thoracolumbar spinal tuberculosis with kyphosis. World Neurosurg. 2019;127:e407–15. [DOI] [PubMed] [Google Scholar]
- [24].Pee YH, Park JD, Choi YG, et al. Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine. 2008;8:405–12. [DOI] [PubMed] [Google Scholar]
- [25].Dvorak MF, Kwon BK, Fisher CG, et al. Effectiveness of titanium mesh cylindrical cages in anterior column reconstruction after thoracic and lumbar vertebral body resection. Spine (Phila Pa 1976). 2003;28:902–8. [DOI] [PubMed] [Google Scholar]
- [26].LoBue PA, Enarson DA, Thoen TC. Tuberculosis in humans and its epidemiology, diagnosis and treatment in the United States. Int J Tuberc Lung Dis. 2010;14:1226–32. [PubMed] [Google Scholar]