Abstract
Diabetes seriously affects the health of middle-aged and elderly. What we can do is to suppress the progression and avoid complications of diabetes. The aim of this study was to evaluate the prevalence, management and influencing factors in middle-aged and elderly diabetics. The data used in our study came from the follow-up survey (2015) of China Health and Retirement Longitudinal Study. After all the questionnaire data of participants was acquired, the first screening step was conducted and the participants without blood glucose or glycosylated hemoglobin test results were excluded. In the second screening step, participants without self-reported diabetes, age <45 were excluded. After data screening, STATA 16.0 software (StataCorp, USA) was used to conduct statistical analysis. Multiple logistics regression was used to analyze the influencing factors of diabetes in middle-aged and elderly. After data screening, A total of 9738 participants were enrolled in the survey of the China Health and Retirement Longitudinal Study in 2015, including diabetes 1965 and control 7773. The prevalence of diabetes in age >60 (22.20%) was significantly higher than that in age 45 to 60 (16.60%). Age, residence, physical activity, drinking, smoking and body mass index were key influencing factors according to the results of logistics regression. 46.92% diabetics were diagnosed in hospital, 22.14% were diagnosed by community medical care. 1298 among 1965 diabetes patients had standardized medication to control blood glucose, the rate was only 66.01%. The awareness rate of diabetes was only 28.75%, and the monitoring, treatment and accepting medical advice rates were 68.32%, 66.01% and 56.99% separately. The follow-up rate of diabetes was only 14.16%. Diabetes is widely prevalent in the middle-aged and elderly with the prevalence of 16.60% in the participants with age 45 to 60. The rate of self-rated diabetics underestimated the true prevalence of diabetes. Age, residence, physical activity, drinking, smoking and body mass index are key influencing factors to diabetes. Although a national diabetes health management model has been established, the awareness of diabetes was only 28.75%. Standardized diabetes registration and regular follow up should also be strictly implemented.
Keywords: awareness, CHARLS, diabetes, health management
1. Introduction
Diabetes is a chronic disease that threatens the population worldwide, it seriously affects the health of middle-aged and elderly people. In 2017, the number of patients with diabetes mellitus (DM) in the world was about 425 million (20–79 years old). It was estimated that the number of DM will increase from 415 to 642 million by 2040.[1] Type 2 diabetes mellitus (T2DM) accounts for 90 to 95% of all diabetes.[2] The onset of T2DM is usually later in life cycle, and most patients with T2DM are overweight or obese, and excess weight causes insulin resistance.[3] T2DM has a prevalence of about 9% in the total population of the US, but approximately 25% in those >65 years. T2DM also imposes a significant health and economic burden on the patients and society. As diabetes is a chronic lifestyle related disease, what we can do is to suppress the progression of the disease and avoid complications. Effective health management, health screening and early intervention for DM are critical to avoid complications and improve the quality of life of DM.[4,5]
The China Health and Retirement Longitudinal Study (CHARLS) is a large-scale interdisciplinary survey project hosted by the National Development Research Institute of Peking University and jointly implemented by the Chinese Social Science Survey Center of Peking University and the Youth League Committee of Peking University. The major project was funded by the National Natural Science Foundation of China aiming to collect a set of high-quality micro-data representing the families and individuals of middle-aged and elderly people aged ≥45 years to promote an interdisciplinary research on aging problems, and improve the relevant policies to provide a more scientific basis. CHARLS conducted 4 waves of national follow-up in 2011, 2013, 2015 and 2018 respectively,[6] and the sample had covered 19,000 respondents in a total of 12,400 households. The contents of the CHARLS included questionnaire, biomedical assay, and body measurement.
In this study, all the data were acquired from CHARLS. We explored the key influencing factors of diabetes in middle-aged and elderly through multiple logistics regression. And we also analyzed the awareness and health management, such as diabetes monitoring, treatment, medical advice and the follow-up rate to assess the effectiveness of community and personal diabetes health management in diabetics. The purpose of our research is to explore the prevalance of diabetes in middle-aged and elderly and the effectiveness of health care and management.
2. Materials and Methods
2.1. Population and data
CHARLS adopted the multi-stage probability proportionate to size sampling method, sampling through the 4 stages of county (district)-village (resident)-household-individual. At the county (district) level, based on the population of each county (district), probability proportionate to size sampling sampling was used to select 150 counties (districts) from 28 provinces or municipalities across the country. At the village (resident) and household level, the sampling method was similar to county (district). At the individual level, filter questionnaires were used to confirm whether there were respondents who met the age-appropriate requirements in the households if there are multiple middle-aged and elderly people aged ≥45 in the household, one is randomly selected as the survey object. If the member of the proper participants cannot answer the question, they designated an agent respondent to help him or her answer the question.
The previous research has been published which was used to describe the questionnaire and the quality assurance measures of the survey.[6–8] The data and information used in our study can be acquired from CHARLS dataset (http://charls.pku.edu.cn). The CHARLS study has got the approval for interviewing respondents and collecting data by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and the informed consent was required to sign by the respondents.
2.2. Variables and definitions
2.2..1. Participants and demographic characteristics.
In the questionnaire, participants were asked if a doctor had ever diagnosed them that they had suffered from diabetes. Participants who answered “yes” were identified as self-reported diabetics, and the others were not self-reported diabetics.[9–11] Participants with fasting blood glucose ≥126 mg/dL (7.0 mmol/L) or glycosylated hemoglobin ≥6.5% were considered to be bio-assayed diabetics. Both self-reported and bio-assayed diabetics were considered to be diabetics. Age was divided into 45 to 60 and >60. Marital status was divided into married and never married or divorced. Education level of participants was divided into 3 groups, namely no formal education, primary education, secondary education and above.
2.2..2. Biomedical assay.
In the 2015 survey of CHARLS, blood samples were taken twice. A total of 13,388 participants participated in the biomedical assay in 2015, and 9989 participants had both serum glucose or HbA1c and self-reported diabetes results.
2.2..3. Health behaviors.
Health behaviors mainly focus on drinking, smoking and physical activity. Participants who reported they had ever smoked in the past, but have stopped smoking were defined as “ever smoker.” Participants who were still smoking were defined as “current smoker.” Participants who reported they had drunk any alcoholic beverages, such as beer, wine, or liquor in the past year were divided into less than once a month and more than once a month group. Physical activity was divided into 3 categories, <30 min/d, 30 min to 2 h/d and ≥2 h/d, and the intensity was divided into vigorous, moderate and mild activities.
2.2..4. Health management.
The diabetics who had glucose test at least once in the past 12 months were identified as standardized monitoring; the diabetics who had received current medical treatment (taking Chinese traditional medicine or Western modern medicine or taking insulin injection or other treatments) for this chronic condition were identified as standardized treatment; the diabetics who had received medical recommendations (weight control or exercise or diet control or smoking control or foot self-care) from their doctor were identified as standard health care. Diabetes follow-up rate was calculated from “The number of diabetics who often received periodic inspection from community doctors or village doctors/the number of diabetics who had known they had diabetes.” Among all diabetics, the participants who self-reported they were diabetics were considered to be aware of their diabetic condition. The participants with blood glucose ≥126 mg/dL or hemoglobin ≥6.5%, but did not self-reported they had diabetes, were considered to be not aware of their diabetic condition.
2.3. Statistical analysis
STATA 16.0 software was used to conduct statistical analysis. The mean and standard deviation were used to describe quantitative variables, and rate or composition ratio were used to describe categorical variables. t test was used to analyze the mean difference of quantitative variables and χ2 test was used to analyze rate or composition ratio difference of categorical variables. Logistic regression was used to calculate the odds ratio and 95% confidence interval, when P value was <.05 (2-sided test), the difference was considered to be statistically significant.
3. Results
3.1. Demographic characteristics
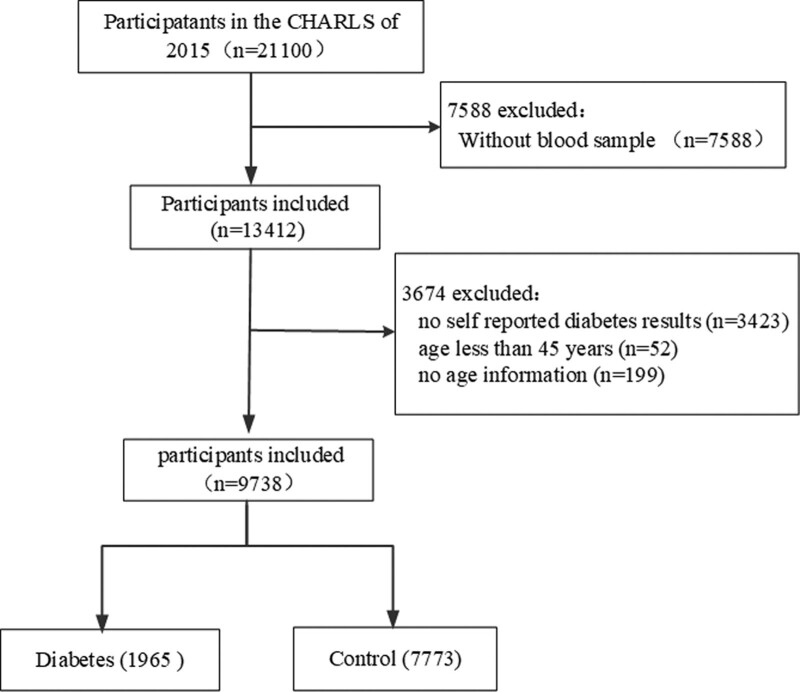
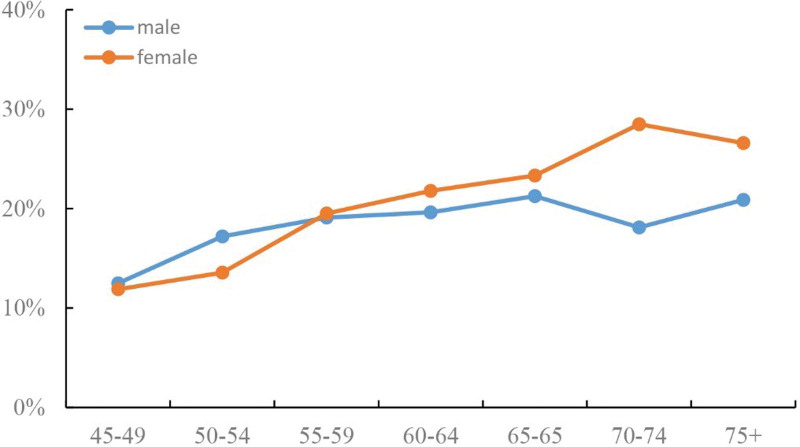
After data screening, a total of 9738 participants were enrolled, including diabetes 1965 and control 7773 (Fig. 1). The prevalence of diabetes in age >60 (22.20%) was significantly higher than that in age 45 to 60 (16.60%), which rapidly increased with age in middle-aged and elderly, especially in female (Fig. 2). The prevalence of diabetes in female (20.90%) and city participants (26.04%) was significantly higher than that of male (19.36%) and rural participants (18.89%). Residence, physical activity, smoking, drinking and body mass index (BMI) were observed to be associated with the prevalence of diabetes (Table 1).
Figure 1.
Flow chat of participants screening.
Figure 2.
Prevalence of diabetes in different gender with age.
Table 1.
Characteristics of included participants.
| Characteristics | n | Diabetes | No diabetes | χ2/t | P | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Age (yr) | |||||||
| 45–60 | 3518 | 584 | 16.60 | 2934 | 83.40 | 43.79 | <.01* |
| >60 | 6220 | 1381 | 22.20 | 4839 | 77.80 | ||
| Gender | |||||||
| Male | 4546 | 880 | 19.36 | 3666 | 80.64 | 3.57 | .06 |
| Female | 5192 | 1085 | 20.90 | 4107 | 79.10 | ||
| Residence | |||||||
| City | 1755 | 457 | 26.04 | 1298 | 73.96 | 45.66 | <.01* |
| Rural | 7983 | 1508 | 18.89 | 6475 | 81.11 | ||
| Marital status | |||||||
| Married | 8336 | 1672 | 20.06 | 6664 | 79.94 | 0.53 | .47 |
| Never married or divorced | 1402 | 293 | 20.90 | 1109 | 79.10 | ||
| Education | |||||||
| No formal education | 769 | 149 | 19.38 | 620 | 80.62 | 0.52 | .77 |
| Primary education | 1354 | 280 | 20.68 | 1074 | 79.32 | ||
| Secondary education and above | 7615 | 1536 | 20.17 | 6079 | 79.83 | ||
| Physical activity | |||||||
| <30 min | 5960 | 1251 | 20.99 | 4709 | 79.01 | ||
| 30 min–2 h | 1564 | 325 | 20.78 | 1238 | 79.16 | 12.55 | .002* |
| >2 h | 2214 | 388 | 17.52 | 1826 | 82.48 | ||
| Smoking | |||||||
| No smoking | 5725 | 1168 | 20.40 | 4557 | 79.60 | ||
| Ever smoking | 1344 | 300 | 22.32 | 1044 | 77.68 | 8.03 | .018* |
| Current smoking | 2669 | 497 | 18.62 | 2172 | 81.38 | ||
| Drinking | |||||||
| No drinking | 6408 | 1378 | 21.50 | 5030 | 78.50 | 20.45 | <.01* |
| Drinking | 3330 | 587 | 17.63 | 2743 | 82.37 | ||
| BMI (mean ± SD) | 9530 | 1901 | 24.99 ± 3.94 | 7629 | 23.53 ± 3.61 | 15.48 | <.01* |
BMI = body mass index, SD = standard deviation.
P<0.05.
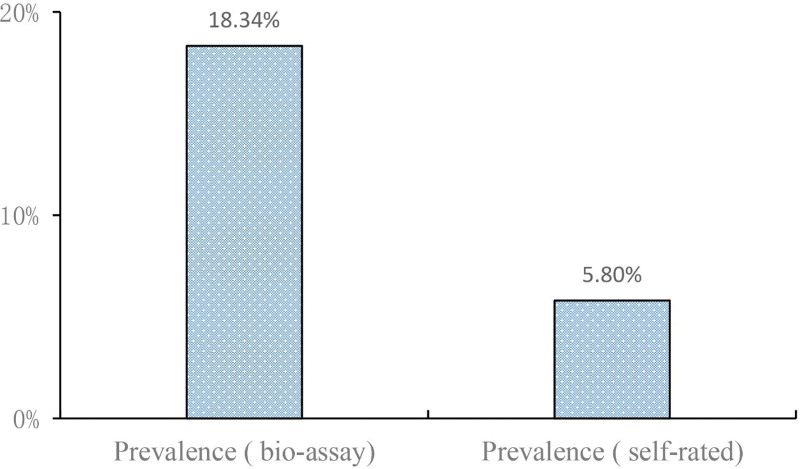
3.2. The rate of bioassay and self-reported diabetes in middle aged and elderly diabetics
Three hundred eighty-six participants had self-reported diabetes and biomedical test confirmed diabetes, 7773 participants had self-reported and biomedical test confirmed no diabetes. One hundred seventy-nine participants self-reported that they had diabetes but with normal biomedical blood glucose, and 1400 participants were confirmed to be diabetics by biomedical test but they had not self-reported. The prevalence of diabetes was 18.34% according to the results of biomedical test, and the prevalence of diabetes was only 5.80% according to the self-reported results by participants themselves, which indicated that the self-reported prevalence underestimated the true prevalence of diabetes (Table 2 and Fig. 3).
Table 2.
The difference between bioassay and self-reported diabetes.
| Group | Self-reported diabetes | Total | ||
|---|---|---|---|---|
| (+) | (−) | |||
| Bioassay diabetes | (+) | 386 | 1400 | 1786 |
| (−) | 179 | 7773 | 7952 | |
| Total | 565 | 9173 | 9738 | |
Figure 3.
Comparison of diabetes prevalence between biomedical and self-reported results.
3.3. Awareness and health management of diabetes
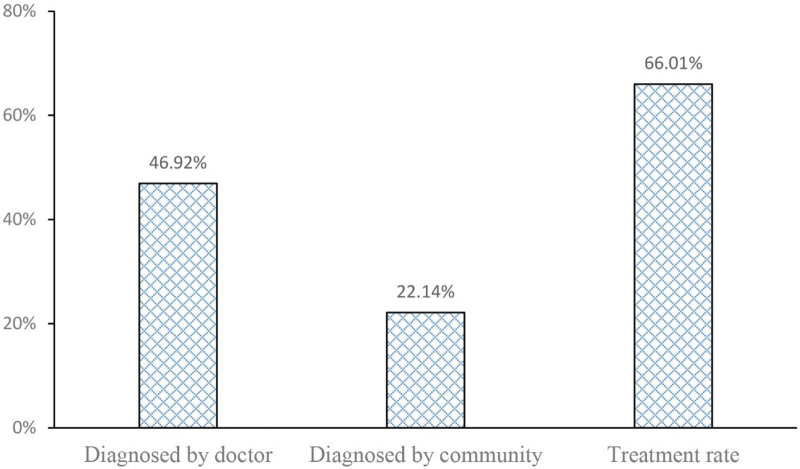
Among all the diabetics, 46.92% diabetics were diagnosed in hospital, 22.14% diabetics were diagnosed by community medical institutions, and the others were diagnosed by themselves or other ways. One thousand two hundred ninety-eight among 1965 diabetes patients had standardized medication to control blood glucose, the rate was only 66.01% (Fig. 4).
Figure 4.
Diagnosis and treatment rate of diabetes.
A total of 565 diabetics self-reported that they had diabetes, and the awareness rate was only 28.75% (565/1965), and the monitoring, treatment and accepting medical advice rates of these diabetes patients was displayed in Table 3. Self-reported diabetes patients had a diabetic monitoring rate 68.32%. Three hundred twenty-two of 565 self-reported diabetes announced they had received medical advice from doctors in hospital or community hospitals, with the rate of 56.99%. Only 80 of 565 diabetes patients reported that they were filed and registered by community or other medical and health institutions, the follow-up rate was only 14.16%.
Table 3.
Health management of self-reported diabetes.
| Variables | n | Number of positive | Rate |
|---|---|---|---|
| Awareness | 1965 | 565 | 28.75% |
| Monitoring | 565 | 386 | 68.32% |
| Treatment | 565 | 373 | 66.01% |
| Medical advice | 565 | 322 | 56.99% |
| Follow-up rate | 565 | 80 | 14.16% |
3.4. Multiple logistics regression of influencing factors of diabetes in middle-aged and elderly
The influencing factors of diabetes in middle-aged and elderly were shown in Table 4. The participants with older age, living in the rural, with less physical activity, smoking, drinking and with higher BMI were prone to diabetes comparing to the control. These results were in consistency with the multiple logistics regression results of influencing factors of diabetes in middle-aged and elderly which were shown in Table 5. Participants with older age, living in the rural, with less physical activity, drinking, smoking and with higher BMI were more likely to develop diabetes.
Table 4.
The influencing factors of diabetes in middle aged and elderly.
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Age | |||
| ≥45–<60 | 1 | <.05 | |
| ≥60 | 1.02 | 1.01–1.03 | |
| Gender | |||
| Male | 1 | .06 | |
| Female | 1.10 | 0.99–1.22 | |
| Residence | |||
| City | 1 | <.05 | |
| Rural | 0.66 | 0.59–0.75 | |
| Marital status | |||
| Married | 1 | .47 | |
| Never married or divorced | 1.05 | 0.92–1.21 | |
| Education | |||
| Primary and below | 1 | .82 | |
| Secondary and above | 1.01 | 0.93–1.10 | |
| Physical activity | |||
| <30 min/d | 1 | ||
| 30 min–2 h/d | 1.02 | 0.89–1.16 | .82 |
| ≥2 h/d | 0.89 | 0.84–0.95 | <.05 |
| Drinking | |||
| No drinking | 1 | <.05 | |
| Drinking | 0.78 | 0.70–0.87 | |
| Smoking | |||
| No smoking | 1 | ||
| Ever smoking | 1.12 | 0.97–1.29 | .12 |
| Current smoking | 0.94 | 0.89–1.00 | .06 |
| BMI | 1.11 | 1.10–1.13 | <.05 |
BMI = body mass index, CI = confidence interval, OR = odds ratio.
Table 5.
Multiple logistics regression of the influencing factors in middle aged and elderly diabetes.
| Variables | Regression coefficient β | 95% CI | P value |
|---|---|---|---|
| Age | 0.032 | <.05 | |
| Gender | 0.083 | .27 | |
| Residence | −0.301 | <.05 | |
| Marital status | −0.142 | .08 | |
| Education | 0.005 | .91 | |
| Physical activity | −0.066 | <.05 | |
| Drinking | −0.185 | <.05 | |
| Smoking | 0.097 | <.05 | |
| BMI | 0.121 | <.05 |
BMI = body mass index, CI = confidence interval.
4. Discussion
Diabetes is one of the most common chronic diseases with high mortality and disability rates worldwide.[12] Asia is the main area of DM epidemic in the world, China is one of the top 2 countries in Asia.[1] An epidemic survey indicated the prevalence of adult diabetes was 13.27% in Guangzhou province of China in 2020,[13–15] which was higher than that in Jiangsu province (11.00%), Changsha province (10.06%) and Tianjin province (12.00%) in 2012 to 2014. In recent years, although breakthroughs have been achieved in basic and clinical research on diabetes, it is still an incurable chronic disease. The pathogenesis of diabetes has not yet been fully elucidated, and the existing prevention and control methods still lack obvious effects. Behavior and lifestyle are the most important factors affecting individual health and playing an important role in the occurrence and development of DM. Studies have shown that smoking,[16,17] drinking,[18] sedentary lifestyle, lack of exercise,[19] and lack of sleep[20,21] and so on are closely related to DM. Regarding chronic disease health management, the World Health Organization states that “increasing adherence may have a greater effect on health than improvements in specific medical therapy.”[22] Therefore, early diagnosis, regular blood glucose monitoring, standardized medical treatment, appropriate exercise and other health management are effective measures to control the progress of diabetes and prevent complications.
According to the results of our survey, we found that the prevalence of diabetes was 18.34% (according to blood glucose or HbA1c) in middle-aged and elderly, which was consistent with published cross-sectional studies. Wang L et al[23] reported an estimated standardized prevalence of total diagnosed and undiagnosed diabetes was 10.9%, diagnosed diabetes, 4.0% among the Chinese adult population in 2013. Wang ZH et al[24] reported that the prevalence of diabetes in the population >60 years old in China reached 19.60%. The prevalence of diabetes significantly increased with the age, especially in female. The participants with age >60 (22.20%) was significantly higher than that with age 45 to 60 (16.60%). The prevalence of diabetes in female (20.90%) and city participants (26.04%) was also significantly higher than that of male (19.36%) and rural participants (18.89%). The early diabetic patients often did not know they had higher blood glucose, and did not take any health care measures to control blood glucose. On the one hand, they missed the opportunity to restore health, on the other hand, it promoted the progress of diabetes. Our results demonstrated that a large number of early diabetes were not diagnosed in time, the rate of self-reported diabetes underestimated the true prevalence of diabetes, which showed a lower self-reported prevalence of diabetes in middle-aged and elderly with age >45 in China.
Physical activity, drinking, smoking and BMI were also key influencing factors. Our results demonstrated it was less of physical activity (>30 min/d) in diabetics (36.30%) compared with non-diabetics (39.42%). Moderate physical activity should be adopted by diabetics. The ever-smoking rate was higher in diabetics than that in non-diabetics, although current smoking rate was lower, maybe the occurrence of diabetes prompted participants to change adverse health behavior. Studies have reported that T2DM and related complications are associated with increased BMI,[25,26] and regular physical activity can help diabetics maintain healthy blood glucose levels and prevent or delay complications.[27] The relationship between drinking and diabetes is still controversial. Some studies reported that moderate alcohol consumption was protective and decreased the risk of type 2 diabetes,[28,29] but others demonstrated that frequent drinking and some other factors have combined effect to increase the risk of T2DM.[30] The frequency of drinking in diabetics (29.87%) was lower than that in non-diabetics (35.28%) in our study. Maybe, the occurrence of diagnosed diabetes prompted participants to change their drinking habits, or the drinking rate in diabetics was indeed lower than the non-diabetic group, which needs further investigation to confirm.
We also investigated the awareness and health management of diabetes. Only 565 diabetics reported that they had known they were diabetes patients, and the awareness rate was only 28.75% (565/1965). Because they were not conscious of their abnormal blood glucose condition, and diet control, exercise and other measures were not implemented to avoid the progress of diabetes, serious consequences of high blood glucose and complication might occur to them. Among all the diabetics, 46.92% diabetics were diagnosed in hospital, 22.14% diabetics were diagnosed by community medical care, and the others were diagnosed by themselves or other ways. The awareness of community health care and self-care still need to be strengthened. 68.32% diabetics who were aware of their condition had a diabetic monitoring, 56.99% received medical advice from doctors or community hospitals, and only 14.16% of all diabetics had follow-up by community health management department for chronic disease registration. Lifestyle modifications and self-management are crucial to the management of DM, especially T2DM.[31,32] Diabetes self-management education and regular follow-up should be provided by chronic disease prevention and health care in community or hospital, including diet/nutrition education, blood glucose monitoring, medication management, and so on.[33]
Despite our best efforts, our study still has several limitations. First, diabetes diagnosis and some other health status information were reported only by the participants themselves, some recall bias was inevitable. Second, the diabetics did not provide the time for the first diagnosis of diabetes, and the health management of newly diagnosed diabetic patients was significantly different from that with long-term patients. Third, health behaviors were also self-reported, some participants might have concealed their real cigarette and alcohol consumption. Fourth, the CHARLS did not provide information on whether the diabetes was type 1 diabetes or type 2 diabetes. The change of biomedical assay and health management of patients with different types of diabetes was also different. Nonetheless, our study preliminarily provided a comprehensive and up to date assessment of health status, health management, health care and risk factors in middle-aged and elderly diabetics in China according to a large cohort study. Some adverse health behavior of diabetic patients should be given special attention. Health management such as early diagnosis, regular monitoring, standardized medication and regular follow-up should be further strengthened. Effective health management and health care measures should be used to improve the quality of life and psychological state of diabetics.
5. Conclusion
Diabetes is widely prevalent in the middle-aged and elderly with the prevalence of 16.60% in the participants with age 45 to 60, and the prevalence rapidly increased with age in middle-aged and elderly, especially in female. The prevalence of diabetes in female and city participants was significantly higher than that of male and rural participants. Residence, physical activity, smoking, drinking and BMI were observed to be associated with the prevalence of diabetes. Although a national diabetes health management model has been established, the rate of diabetes awareness, monitoring, treatment and accepting medical advice rates were only 28.75%, 68.32%, 66.01% and 56.99% separately. Glucose monitoring, health management and other medical advice should be given to improve the condition of diabetics. Standardized diabetes registration and regular follow up should also be strictly implemented by hospital or community medical care.
Acknowledgments
The authors thank all the participants in CHARLS team for their time and effort devoted to the project.
Author contributions
Bin-Jiang Wu and Yu-Ling Zhang wrote the main manuscript text. Pei Chen prepared data processing and statistical analysis. Hong-Hua Wen prepared figures and tables.
Data curation: Pei Chen.
Formal analysis: Bin-Jiang Wu.
Investigation: Hong-Hua Wen.
Methodology: Pei Chen.
Resources: Hong-Hua Wen.
Writing – original draft: Yu-Ling Zhang, Bin-Jiang Wu.
Writing – review & editing: Yu-Ling Zhang.
Abbreviations:
- BMI =
- body mass index
- CHARLS =
- China Health and Retirement Longitudinal Study
- DM =
- diabetes mellitus
- T2DM =
- type 2 diabetes mellitus
Y-LZ and B-JW contributed equally to this work.
Informed consent was obtained from all subjects involved in the study. The CHARLS was approved by the Ethical Review Committee of Peking University, and all participants signed an informed consent form before the start of the investigation. No separate ethical approval was required for our study.
The authors have no funding and conflicts of interest to disclose.
The datasets generated and/or analyzed during the current study are publicly available. The data and information used in our study was acquired from CHARLS dataset (http://charls.pku.edu.cn).
How to cite this article: Zhang Y-L, Wu B-J, Chen P, Wen H-H. The prevalence, awareness, management and influencing factors of diabetes in middle-aged and elderly in China, evidence from the CHARLS in 2015. Medicine 2022;101:50(e32348).
Contributor Information
Bin-Jiang Wu, Email: bjwu@njmu.edu.cn.
Pei Chen, Email: xiaolajiao1983@126.com.
Hong-Hua Wen, Email: 1432301360@qq.com.
References
- [1].Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88–98. [DOI] [PubMed] [Google Scholar]
- [2].2. Classification and diagnosis of diabetes: standards of medical care in diabetes – 2018. Diabetes Care. 2018;41(Suppl 1):S13–27. [DOI] [PubMed] [Google Scholar]
- [3].Boles A, Kandimalla R, Reddy PH. Dynamics of diabetes and obesity: Epidemiological perspective. Biochim Biophys Acta Mol Basis Dis. 2017;1863:1026–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Olczuk D, Priefer R. A history of continuous glucose monitors (CGMs) in self-monitoring of diabetes mellitus. Diabetes Metab Syndr. 2018;12:181–7. [DOI] [PubMed] [Google Scholar]
- [5].Radermecker RP. [Continuous glucose monitoring in the management of diabetes: state-of-the art and perspectives] [in French]. Rev Med Suisse. 2019;15: 1444–7. [PubMed] [Google Scholar]
- [6].Zhao Y, Hu Y, Smith JP, et al. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zhou L, Ma X, Wang W. Relationship between cognitive performance and depressive symptoms in Chinese older adults: the China Health and Retirement Longitudinal Study (CHARLS). J Affect Disord. 2021;281:454–8. [DOI] [PubMed] [Google Scholar]
- [8].Yao Y, Wang K, Xiang H. Association between cognitive function and ambient particulate matters in middle-aged and elderly Chinese adults: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). Sci Total Environ. 2022;828:154297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ning M, Zhang Q, Yang M. Comparison of self-reported and biomedical data on hypertension and diabetes: findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open. 2016;6:e009836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ab Majid NL, Rodzlan Hasani WS, Mat Rifin H, et al. Self-reported diabetes, hypertension and hypercholesterolemia among older persons in Malaysia. Geriatr Gerontol Int. 2020;20(Suppl 2):79–84. [DOI] [PubMed] [Google Scholar]
- [11].Suzuki S, Sugihara N, Kamijo H, et al. Self-reported diabetes mellitus and tooth extraction due to periodontal disease and dental caries in the Japanese population. Int J Environ Res Public Health. 2021;18:9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785–95. [DOI] [PubMed] [Google Scholar]
- [13].Zeng LY, Cheng ZQ, Liu DH. Epidemic status and influencing factors of diabetes in Guangzhou in 2020. Pract Prev Med. 2022;29:119–21. [Google Scholar]
- [14].Xie W, Zhang JX, Zhu QR, et al. Prevalence of diabetes among adult residents in Jiangsu Province in 2014. Jiangsu Prev Med. 2019;30:522–5. [Google Scholar]
- [15].Pan Y, Jiang GH, Chang G, et al. Analysis of diabetes prevalence and related risk factors in Tianjin. China Chronic Dis Prev Control. 2015;23:908–12. [Google Scholar]
- [16].Akter S, Goto A, Mizoue T. Smoking and the risk of type 2 diabetes in Japan: a systematic review and meta-analysis. J Epidemiol. 2017;27:553–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wu J, Pan G, Huang YT, et al. Effects of passive smoking and its duration on the prevalence of prediabetes and type 2 diabetes mellitus in Chinese women. Aging (Albany NY). 2020;12:9440–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bellou V, Belbasis L, Tzoulaki I, et al. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13:e0194127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Karstoft K, Pedersen BK. Exercise and type 2 diabetes: focus on metabolism and inflammation. Immunol Cell Biol. 2016;94:146–50. [DOI] [PubMed] [Google Scholar]
- [20].Ferrie JE, Kivimäki M, Akbaraly TN, et al. Change in sleep duration and type 2 diabetes: the Whitehall II study. Diabetes Care. 2015;38:1467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Nuyujukian DS, Beals J, Huang H, et al. Sleep duration and diabetes risk in American Indian and Alaska native participants of a lifestyle intervention project. Sleep. 2016;39:1919–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317:2515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang ZH, Wang LH, Li YC, et al. Investigation on the status of hypertension, diabetes and dyslipidemia among residents over 60 years old in China in 2010 [in Chinese]. Chin J Prev Med. 2012:922–926. [Google Scholar]
- [25].Nordstrom P, Pedersen NL, Gustafson Y, et al. Risks of myocardial infarction, death, and diabetes in identical twin pairs with different body mass indexes. JAMA Intern Med. 2016;176:1522–9. [DOI] [PubMed] [Google Scholar]
- [26].Gray N, Picone G, Sloan F, et al. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med J. 2015;108:29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Centers for Disease Control and Prevention. National diabetes statistics report, 2014. [Google Scholar]
- [28].Baliunas DO, Taylor BJ, Irving H, et al. Alcohol as a risk factor for type 2 diabetes: a systematic review and meta- analysis. Diabetes Care. 2009;32:2123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Brath H, Kaser S, Tatschl C, et al. Alkohol and diabetes mellitus (Update 2019) [Smoking, alcohol and diabetes (Update 2019)] [in German]. Wien Klin Wochenschr. 2019;131(Suppl 1):67–70. [DOI] [PubMed] [Google Scholar]
- [30].Xue S, Mu M, Li W, et al. [Interaction between alcohol-drinking and other factors of lifestyles on the risk of type 2 diabetes mellitus] [in Chinese]. Wei Sheng Yan Jiu. 2017;46:918–929. [PubMed] [Google Scholar]
- [31].Powers M, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin Diabetes. 2016;34:70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Brunisholz K, Briot P, Hamilton S, et al. Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. J Multidiscip Healthc. 2014;7:533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Chester B, Babu JR, Greene MW, et al. The effects of popular diets on type 2 diabetes management. Diabetes Metab Res Rev. 2019;35:e3188. [DOI] [PubMed] [Google Scholar]