Abstract
“De Winter” electrocardiogram pattern is considered an equivalent risk to ST‐elevation myocardial infarction and usually indicates occlusion of the left anterior descending artery, which needs emergent revascularization treatment. However, some conditions can mimic “de Winter” electrocardiogram pattern and may cause misdiagnosis. Here, we reported a case of hyperkalemia presented with “de Winter‐like” electrocardiogram pattern. This study aimed to increase physicians' awareness about the impact of electrolyte disorder on electrocardiographic changes.
Keywords: chronic kidney disease, De Winter, hyperkalemia, pseudo‐infarction, ST‐elevation myocardial infarction
Short abstract
“De Winter” electrocardiogram pattern usually indicates acute coronary syndrome; however, hyperkalemia can also cause “de Winter‐like” electrocardiogram pattern, especially in the setting of chronic kidney disease with elevated cardiac troponin. Therefore, an emergent biochemical test should be performed on those presented with “de Winter‐like” electrocardiogram pattern.
1. INTRODUCTION
The electrocardiographic “de Winter” pattern was firstly described in 2008 and was characterized by the absence of ST‐elevation with upsloping ST‐segment depression followed by tall symmetrical T waves in the precordial leads. 1 Although this electrocardiographic pattern was not classic ST‐elevation myocardial infarction (STEMI), it usually indicates the left anterior descending artery (LAD) occlusion, and now it is recognized as a special equivalent of STEMI needing urgent reperfusion therapy. 2 However, “de Winter‐like ECG” pattern is not specific for STEMI, and hyperkalemia‐caused electrocardiographic change is one of the most important differential diagnoses. 3 Here, we reported a case with chronic kidney disease (CKD) complicating hyperkalemia presented with “de Winter” pattern on electrocardiogram (ECG).
2. CASE PRESENTATION
An 86‐year‐old man was admitted to the emergency department after an episode of chest pain and weakness for 7 h. The patient had a history of hypertension for more than 10 years and took amlodipine and candesartan to control blood pressure; however, he did not have regular physical checkups and was nonadherent to antihypertensive medications. Two years before, he had oliguria and went to the hospital. The blood pressure was 160/75 mmHg, and a biochemical test indicated the serum creatinine level was 215 μmol/L with proteinuria. He was advised to monitor the renal function regularly and take candesartan 8 mg daily to control blood pressure and alleviate proteinuria. However, he still did not take antihypertensive agents and monitor his renal function regularly. During the past 2 years, he sometimes felt exertional dyspnea, especially when oliguria presents, and the symptoms improved after taking furosemide. Three days prior to admission, he caught a cold, and the symptoms worsened, but he did not seek medical attention. Seven hours before admission, when he was at rest, he felt extreme chest pain and shortness of breath with nausea and vomiting, then got admitted. On physical examination, the heart rate was 105 beats per minute (bpm), blood pressure was 165/100 mmHg, respirations were 24 per minute, and oxygen saturation was 94% on room air. Lung auscultation revealed moist rales bilaterally, and other physical examination findings were unremarkable. An ECG was obtained immediately (Figure 1). The cardiac troponin I (cTnI) with rapid bedside assay exceeded three times the upper limit of normal.
FIGURE 1.
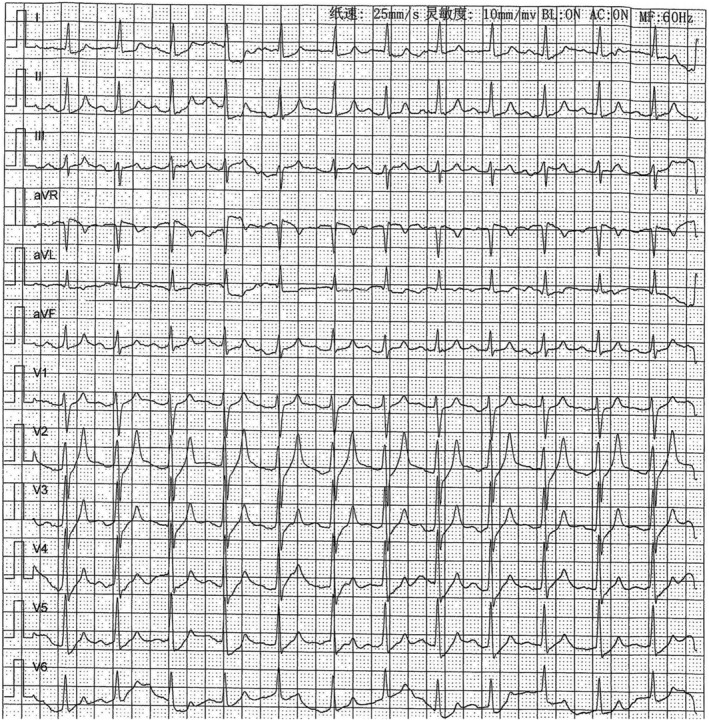
ECG on admission
3. INTERPRETATION
The ECG showed a sinus rhythm with a heart rate of 105 bpm, P‐R interval of 200 ms. The most important feature is the upsloping ST‐segment depression >1 mm with peaked T wave in leads V2–V5, which was consistent with “de Winter” pattern. 1 Moreover, this patient had chest pain and elevated cTnI, which indicated that a coronary intervention was urgently needed.
3.1. Clinical course
An emergency coronary angiography was planned; however, admission biochemical test results indicated plasma potassium 8.7 mmol/L, bicarbonate 6.4 mmol/L, and creatinine 754 μmol/L. Therefore, the patient firstly received urgent hemodialysis. After hemodialysis for 3 h, the symptom was alleviated, the plasma potassium decreased to 5.6 mmol/L, cTnI was maintained at the same level as on admission, and an ECG was obtained (Figure 2). The P‐R interval was shortened to 130 ms, and the P wave was more obvious than in Figure 1. The most significant change was the improvement of the upsloping ST‐segment depression and peaked T wave in leads V2–V5. During hospitalization, the patient received coronary angiography with mild stenosis of the left anterior descending artery. The creatinine was around 500 μmol/L still with oliguria, and therefore, regular hemodialysis therapy was advised.
FIGURE 2.

ECG after resolution of hyperkalemia. The peaked T wave and upsloping ST‐segment depression in leads V2 and V3 are markedly improved
4. DISCUSSION
As is known, the most important strategy for STEMI is to give reperfusion therapy as soon as possible. Although “de Winter” ECG pattern does not present with classic ST‐elevation on ECG, the culprit vessel is usually the occlusion of LAD, 1 and therefore, it is now regarded as an equivalent risk as STEMI, needing urgent reperfusion therapy. 4 Here, we presented a case of hyperkalemia mimicking “de Winter‐like” ECG pattern. Indeed, severely elevated potassium can produce an infarction‐like ECG pattern. 5 Although the exact mechanism of how acute hyperkalemia resembles STEMI is not well understood, it is possibly related to myocardial conduction and repolarization. The potassium channel located on myocyte cell membranes is crucial for controlling transportations of potassium ions efflux from and influx into cells, therefore, when extracellular potassium is elevated, it will increase myocyte excitability, shorten myocyte action potential, and increase the slope of phase 2 and phase 3 of the action potential, thus results in “infarction‐like” ECG pattern. 5 However, this ECG manifestation is changed once hyperkalemia is resolved; therefore, it is also called the “pseudo‐infarction” ECG pattern.
The patient we described had an initial ECG suggestive of “de Winter” pattern. Moreover, our patient presented with chest pain and elevated cTnI; thus, acute coronary syndrome was highly suspected. However, the subsequent biochemical test revealed severe hyperkalemia. Therefore, we must differentiate “de Winter” ECG pattern from hyperkalemia. Although some ECG clues may aid in differentiating this “pseudo‐infarction” pattern, such as long QT interval with broad‐based T waves more suggestive of myocardial injury, however, these characteristics are not specific in some cases. Indeed, high‐pitched T wave in hyperkalemia usually resembles the hyperacute phase of STEMI; however, the ST‐segment in hyperkalemia is usually not depressed, and “de Winter‐like” pattern was scarce. In fact, hyperkalemia‐induced pseudo‐myocardial infarction has been widely reported 3 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ; however, most cases presented with typical ST‐elevation on ECG as STEMI, with only Walker et al. 3 recently reported a similar case with hyperkalemia presented with “de Winter‐like” ECG. However, in Walker et al.'s 3 report, this case mainly complained of lethargy rather than chest pain symptoms. Moreover, this case had other characteristics of severe hyperkalemia, such as bradycardia, widened QRS duration, and sinoventricular conduction. In contrast, our case presented with chest pain and elevated cTnI, which suggest an acute coronary syndrome. In addition, although the P‐R interval and P wave had dynamic change after emergent hemodialysis, they were within the normal range and lacked remarkable electrocardiographic changes of hyperkalemia as in Walker et al.'s 3 report.
The clinical presentation in our case can be interpreted as follow. The patient had chronic kidney disease (CKD), possibly due to poorly controlled hypertension; however, he did not take antihypertensive agents regularly, as the CKD progressed, he developed heart failure eventually. This time the patient underwent a respiratory tract infection, which aggravated heart failure and renal dysfunction (acute kidney injury). Moreover, the antihypertensive agent candesartan could also precipitate hyperkalemia in the setting of CKD. It is worth noting that coronary and noncoronary diseases can cause the elevation of cTnI, especially in patients with CKD. 16 However, in the setting of CKD, the cTnI level is usually not as high as that of STEMI. 16 Moreover, the “de Winter‐like” ECG changed after hyperkalemia was improved in this case, indicating the presence of ECG was nonischemic. Subsequent coronary angiography confirmed a nonobstructive lesion because it usually presented with severe or obstructive left anterior descending artery lesion in patients with “de Winter” pattern.
Take home message from this ECG challenge was that “de Winter‐like” ECG pattern is not specific for diagnosing acute coronary syndrome, and hyperkalemia can produce “de Winter‐like” ECG pattern, especially in the setting of CKD that causes elevation of cTnI. Therefore, a rapid biochemical test to exclude hyperkalemia is warranted to avoid misdiagnosis and unnecessary coronary interventions.
AUTHOR CONTRIBUTIONS
B.H and B.R.S contributed to the conception, design, and analysis of the data. S.X.L contributed to the supervision and interpretation of data. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
None.
ETHICAL APPROVAL
Informed consent was received from the patient. This study was performed in accordance with the principle of the Declaration of Helsinki and the research protocol was approved by the institutional ethical review board of the first affiliated hospital of Chongqing medical university (April 29, 2020, No.2020–233).
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
All the authors thank the patient for allowing publication of this case study. The authors also thank the anonymous reviewers and editors for their helpful comments on the manuscript.
Sasmita BR, Luo S, Huang B. Hyperkalemia mimicking de Winter T waves: A case report. Clin Case Rep. 2022;10:e06783. doi: 10.1002/ccr3.6783
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. de Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359(19):2071‐2073. [DOI] [PubMed] [Google Scholar]
- 2. Mahajan K, Batra A, Gupta A. de Winter sign‐A STEMI Equivalent. Indian Heart J. 2018;70(5):761‐764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walker M, Vivekanantham H, Graf D. ECG of the month: a "de Winter"‐like ECG pattern in a patient presenting with progressive lethargy. Ann Emerg Med. 2021;77(4):445‐448. [DOI] [PubMed] [Google Scholar]
- 4. de Winter RW, Adams R, Verouden NJ, et al. Precordial junctional ST‐segment depression with tall symmetric T‐waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016;49(1):76‐80. [DOI] [PubMed] [Google Scholar]
- 5. Dittrich KL, Walls RM. Hyperkalemia: ECG manifestations and clinical considerations. J Emerg Med. 1986;4(6):449‐455. [DOI] [PubMed] [Google Scholar]
- 6. Bhagwat N, Sahasrabuddhe S. Two cases of pseudo inferior myocardial infarction. J Assoc Physicians India. 2016;64(6):94‐95. [PubMed] [Google Scholar]
- 7. Pothiawala SE. Hyperkalemia induced pseudo‐myocardial infarction in septic shock. J Postgrad Med. 2014;60(3):338‐340. [DOI] [PubMed] [Google Scholar]
- 8. Wang K. Images in clinical medicine. "Pseudoinfarction" pattern due to hyperkalemia. N Engl J Med. 2004;351(6):593. [DOI] [PubMed] [Google Scholar]
- 9. Dendramis G, Petrina SM, Baranchuk A. Not all ST‐segment elevations are myocardial infarction: hyperkalemia and Brugada phenocopy. Am J Emerg Med. 2017;35(4):661‐662. [DOI] [PubMed] [Google Scholar]
- 10. Peerbhai S, Masha L, Dasilva‐Deabreu A, et al. Hyperkalemia masked by pseudo‐stemi infarct pattern and cardiac arrest. Int J Emerg Med. 2017;10(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heckle M, Agarwal M, Alsafwah S. ST elevations in the setting of hyperkalemia. JAMA Intern Med. 2018;178(1):133‐134. [DOI] [PubMed] [Google Scholar]
- 12. Carrizales‐Sepulveda EF, Del CA, Jimenez‐Castillo RA, et al. Pseudomyocardial infarction in a patient with severe diabetic ketoacidosis and mild hyperkalemia. Case Rep Cardiol. 2019;2019:4063670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gonzales VM, Arizon‐Munoz JM, Villa‐Gil‐Ortega M. Pseudo inferior myocardial infarction pattern caused by hyperkalemia. Rev Esp Cardiol. 2011;64(5):416. [DOI] [PubMed] [Google Scholar]
- 14. Ziakas A, Basagiannis C, Stiliadis I. Pseudoinfarction pattern in a patient with hyperkalemia, diabetic ketoacidosis and normal coronary vessels: a case report. J Med Case Reports. 2010;4:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Idilbi N, Zbidat M. Hyperkalaemia mimics pseudostemi infarct pattern. BMJ Case Rep. 2022;15(2):e247444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Agewall S, Giannitsis E, Jernberg T, Katus H. Troponin elevation in coronary vs. non‐coronary disease. Eur Heart J. 2011;32(4):404‐411. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


