Abstract
Purpose
Informal caregivers play an important supportive care role for patients with cancer. This may be especially true for pancreatic cancer which is often diagnosed late, has a poor prognosis and is associated with a significant symptom burden. We systematically reviewed the evidence on caregiver burden, unmet needs and quality-of-life of informal caregivers to patients with pancreatic cancer.
Method
PubMed, Medline, CINAHL and Embase databases were systematically searched on 31 August 2021. Qualitative and quantitative data on informal caregivers’ experiences were extracted and coded into themes of burden, unmet needs or quality-of-life with narrative synthesis of the data undertaken.
Results
Nine studies (five qualitative, four quantitative), including 6023 informal caregivers, were included in the review. We categorised data into three key themes: caregiver burden, unmet needs and quality-of-life. Data on caregiver burden was organised into a single subtheme relating to symptom management as a source of burden. Data on unmet needs was organised into three subthemes need for: better clinical communication; support and briefings for caregivers; and help with navigating the health care system. Data on quality-of-life indicate large proportions of informal caregivers experience clinical levels of anxiety (33%) or depression (12%-32%). All five qualitative studies were graded as good quality; three quantitative studies were poor quality, and one was fair quality.
Conclusion
High-quality pancreatic cancer care should consider the impacts of informal caregiving. Prospective longitudinal studies examining multiple dimensions of caregiver burden, needs, and quality-of-life would be valuable at informing supportive care cancer delivery to pancreatic cancer informal caregivers.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00520-022-07468-7.
Keywords: Supportive care, Caregiver burden, Unmet needs, Quality-of-life, Pancreatic cancer
Introduction
Pancreatic cancer is a disease with high morbidity and a high mortality rate. The overall survival at 5-years is 6–10%, due in large part to late diagnosis which precludes curative resections [1, 2]. At diagnosis, only 10–15% of patients have localised disease and are potential candidates for curative resection [2, 3]. Even for patients who received resection, the overall 5-year survival rate is less than 25% because of early recurrence [1, 2]. Hence, the focus of treatment in the majority of the patients has been about achieving a balance between palliative chemotherapy and maintaining quality-of-life [4].
Informal caregivers — spouses/partners, other family member and/or close friends — serve an increasingly important role in the modern health system by supporting patients’ needs inside and outside the healthcare setting. In the context of cancer, informal caregivers may provide support during treatment, manage the patient’s medications, coordinate healthcare visits, and update friends and family, in addition to supporting patients with activities of daily living (e.g. feeding, bathing, and dressing patients) and instrumental activities of daily living (e.g. managing finance, cooking, and cleaning) [5, 6]. With a trend towards shorter hospital stays, the role of informal caregivers’ has expanded to include the monitoring and management of patients’ medication and symptoms [7]. Cancer caregivers are estimated to spend an average of 32.9 h a week providing care and with 72% of that duration spent on performing complex medical or nursing tasks [8].
The adverse effects of informal caregiving are increasingly appreciated in various diseases including cancer [9, 10]. In cancer, family members and friends are seldom prepared to be caregivers [11] and are thrust into the role at the time when they are coming to terms with the diagnosis. Disruptions to caregivers’ lives can be significant, and many suffer from a wide range of problems [12–14]. These effects can impact caregiver quality-of-life [15].
High-quality cancer care is now recognised as not limited to the delivery of appropriate treatment but also includes ensuring patients’ supportive care needs are met [16]. The scope of supportive care encompasses helping the patient and their family cope with cancer and its treatment across the illness trajectory and with death and bereavement [16]. The nature of the caregiver burden imposed by diseases varies according to the disease and its physical manifestations. The survival rate in pancreatic cancer is markedly lower than for other common cancers [17], and there has been little improvement over the past 30 years [18]. Most patients are diagnosed at an advanced stage, when curative treatment is impossible [19]. Patients tend to deteriorate rapidly and up to 90% have died within a year of diagnosis, demonstrating the aggressiveness of the condition [17]. All treatments and are associated with a significant side-effect burden, and patients’ quality-of-life and psychological wellbeing are notably worse compared to people without cancer and those with other forms of cancer [17]. It is therefore plausible that the impact of pancreatic cancer on informal caregivers is potentially distinct [18].
To inform the need for services and supports for informal caregivers of pancreatic cancer patients, it would be valuable to review the literature on the experiences of caregiving. This review aims to systematically identify and assess burden, unmet needs, and quality-of-life of informal caregivers of patients diagnosed with pancreatic cancer.
Materials and methods
Study selection
A systematic search was conducted using four databases: PubMed, Medline, Embase and CINAHL. The search syntax is presented in the Supplementary Table 1 (Appendix). In brief, this included terms for the disease, caregiving and burden, needs and quality-of-life. Databases were searched from inception to 31 August 2021. Both qualitative and quantitative studies were eligible, so no study design filters were applied in the searches. Reference lists of the included studies were screened to search for any additional studies not identified on the initial search and screening process.
Duplicate citations were removed. The remaining citations were screened by title and abstract by the first author (EC). Full texts of citations considered potentially eligible were obtained. Assessment of the full-text papers for eligibility was performed independently by two authors (EC and LC).
Terminology and definitions
For the purposes of this review, caregiver burden included objective and subjective burden. Objective burden referred to tangible demands due to provision of care to the patient. Subjective burden referred to subjective experience of distress in the domains of health, psychological well-being, finances and social life, or due to the relationship between the caregiver and patient [20, 21]. Unmet needs were defined as needs which could be met with help from health care professionals, including allied health workers [22]. Quality-of-life was defined as the individual’s subjective perception of their physical, emotional, social and/or role wellbeing [21].
Eligibility criteria
Inclusion criteria included studies that contained qualitative or quantitative data on the experiences of informal caregivers to patients with pancreatic cancer. Studies were included if they reported data on caregiver burden, needs of caregivers and/or caregiver quality-of-life, as defined above. To be eligible, studies had to report data collected from informal caregivers themselves. Exclusion criteria included: studies discussing caregiver experience indirectly (for example, data collected from patients or health professionals); studies not specific to pancreatic cancer; and studies that did not report separate caregiver experience for pancreatic cancer or that contained only data from a second-order analysis. Studies reporting interventions in caregivers were not eligible, as experiences and outcomes may be impacted by the intervention. Articles that were in a language other than English, case reports, editorials, opinion articles and review articles were also excluded. Conference abstracts were excluded as these generally lack sufficient detail for data extraction and synthesis and quality appraisal.
Quality appraisal
Quality appraisal was undertaken independently by two authors (EC and LC). Any disagreements were reviewed with input from third author (LS). Qualitative studies were appraised using the Critical Appraisal Skill Programme (CASP) Qualitative Checklist [23]. The CASP Qualitative Checklist contains 11 questions based on three broader questions: ‘are the results of the study valid?’, ‘what are the results?’ and ‘will the results help locally?’ Points were assigned to responses to each question: ‘Yes’ = 2 points, ‘Somewhat’ = 1, ‘No’ = 0 and ‘Can’t tell’ = 0. The maximum total points for any study were 22. A priori, it was decided that study quality was considered good if the total score was 17–22 points, fair if 11–16 points and poor if 0–10 points.
Quantitative studies were assessed using the Methodological Index of Non-randomised Studies (MINORS) [24]. MINORS includes eight items for assessment of non-comparative studies (i.e. studies which do not include a control or comparator population) and twelve items for comparative studies. Points were assigned to possible responses to each question: ‘Adequately reported = 2’, ‘Reported but inadequate = 1’ and ‘Not reported = 0’. The maximum total points for comparative and non-comparative studies were 24 and 16 respectively. Quality of a study was considered good if the total points was 16–24, fair if 8–16 and poor if 0–8, irrespective of whether the study was comparative or not.
Data extraction and synthesis
Data were extracted by two authors (EC and LC). Any disagreement in data extraction was resolved with input from a third author (LS). The extracted data included study aim, study design, country, duration, data collection method(s), number of informal caregivers included, caregiver age and gender, disease characteristics and data on caregiver experience associated with caregiver burden, unmet needs or quality-of-life.
EC (a medical practitioner) and LC (a qualitative researcher) conducted the data synthesis. Narrative synthesis of data was undertaken [25]; the limited number of eligible papers and heterogeneity in methods and outcomes precluded meta-synthesis. The aim of this study is to assess caregiver burden, unmet needs and quality-of-life. As such, these key areas formed our themes, using the definitions above, and data was coded using deductive thematic analysis [26]. In the event of any disagreement in definition due to overlap, a third reviewer (LS) was sought for categorisation.
From the papers, we took all reported quotes from caregivers and any caregiver-related statistics. Any similar quotes and statistics were coded into the themes. Quantitative data was restricted to quality-of-life only. When all data was grouped into the themes, two authors (EC and LC) went through the data to create the narrative synthesis of the current evidence on caregivers’ experience in the field of pancreatic cancer [25]. This analysis has enabled us to provide a summary of the current research available on caregiver burden in pancreatic cancer.
Results
Search results
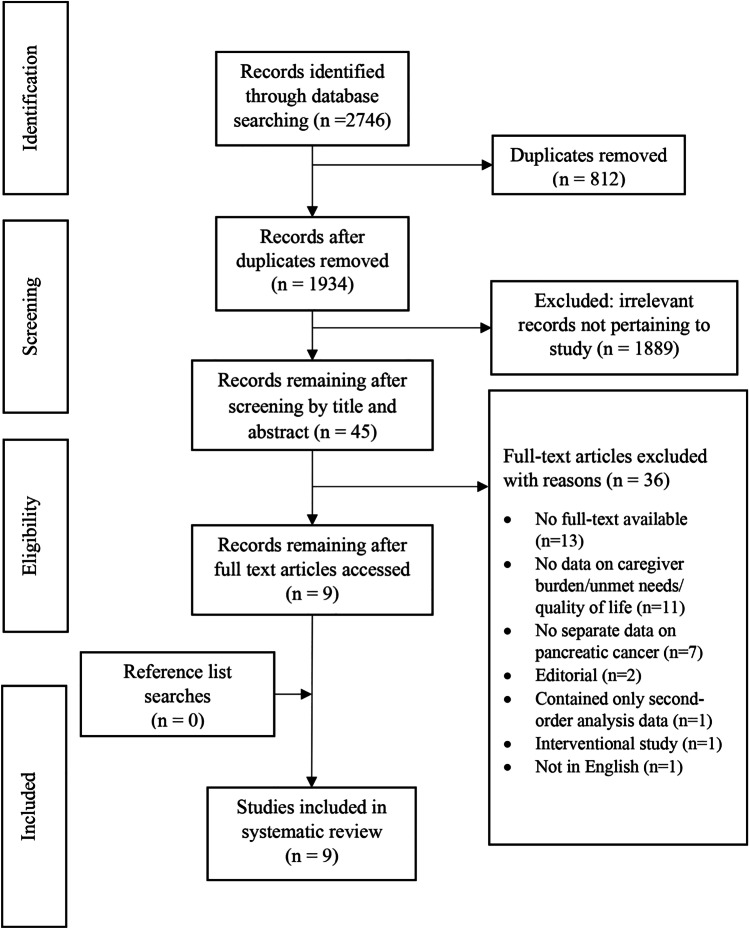
A PRISMA flowchart detailing the screening process is shown in Fig. 1. Briefly, the systematic search of databases returned 2746 citations. After removing duplicates and screening the remainder of articles by title and abstract, full texts of 45 citations were reviewed. Of these, 36 full texts were excluded. Manual searches of reference list of included studies did not return any further articles that met the inclusion criteria. Thus, nine studies were included in this review of which five were qualitative studies [27–31], and four were quantitative studies [5, 6, 32, 33].
Fig. 1.
PRISMA flowchart of literature search
Descriptions of the studies
The nine studies were published between 2008 and 2021 (Table 1). A total of 6023 informal caregivers (inclusive of family members and first-degree relatives) were included. Excluding a large study which included 5574 informal caregivers [6], a total of 77 and 363 informal caregivers were included in the qualitative and quantitative studies respectively. Five studies (three qualitative, two quantitative) were conducted in the USA [5, 28, 29, 31, 33], three (two qualitative, one quantitative) in Australia [27, 30, 32] and one quantitative study in Denmark [6]. Data was collected through questionnaires alone in four studies [5, 32, 33], semi-structured interviews with individual participants in three studies [29–31], focus groups in two studies [27, 28] and questionnaire and semi-structured interview together in one study [29]. The Danish study conducted data linkage between the national cancer registry, civil registration system and the national prescription registry database [6]. Eight studies were cross-sectional studies [5, 27–33]. One study was a prospective cohort design [6].
Table 1.
Study characteristics of eligible studies
| Study (author and year), location | Study design | Study population | Data collection | Outcomes | Relevant findings/themes |
|---|---|---|---|---|---|
| Wong et al. (2019) [28], USA |
Qualitative/cross -sectional study |
25 informal caregivers | Semi-structured interview in focus group (photovoice method was used) | Psychological distress and coping with PC |
Diagnosis of an unexpected, advanced cancer Changes in roles and identity Management of weight loss and GI symptoms Fear of the future |
| Sherman et al. (2014) [29], USA | Qualitative/cross-sectional study | 7 informal caregivers | Semi-structured interview | Caregiver experience during diagnostic/treatment phase of illness |
The caregiving context • History of illness: the sentinel event of significant symptoms • The crisis of diagnosis • The violation of assumptions about life and health • The circle of association • Contextual factors of family caregiving Primary stressors associated with family caregiving Secondary stressors association with family caregiving • Conduit of medical information |
| Gooden et al. (2013) [30], Australia |
Qualitative/cross -sectional study |
23 informal caregivers/family (including 14 bereaved caregivers) | Semi-structured interview (telephone or face-to-face) | PEI as an area of supportive care that requires an increased focus |
Impact of symptoms on quality-of-life. Lack of information and dietary assessment Access to information about pancreatic EST Carer distress |
| Petrin et al. (2009) [31], USA |
Qualitative/cross -sectional study |
22 first-degree relatives (to 9 deceased and 11 alive patients with PC) | Semi-structured interview (telephone) | Experience of family members communicating and adjusting to first-degree relative’s diagnosis of PC, treatment, and subsequent death or survival |
Reactions to initial diagnosis Coping with aftermaths of diagnosis Creating/maintaining support Family dynamics Considerations of future |
| Saunders et al. (2009) [27] Australia |
Qualitative/cross -sectional study |
11 participants (6 current and bereaved informal caregivers and 5 patients) | Semi-structured interview (telephone or face-to-face in group setting) | Consumer (i.e. patient or caregiver) thoughts and priorities in PC research |
Early detection Clinical communication Public awareness Treatment options |
| Dengsø et al. (2021) [6], Denmark | Quantitative/retrospective prospective study | 64,873 participants (5574 partners of PC patients, 59,099 partners of noncancer patients) | Data collected from DCR and CRS between 2000 and 2016 | First incidence of depression, anxiety or insomnia |
Higher first incidence of depression in partner of PC patients especially in first 2 years Risk factors for depression were female gender, older age, lower education levels and higher comorbidity Higher incidence of anxiety and insomnia in first year Higher incidence long-term insomnia |
| Janda et al. (2017) [32], Australia | Quantitative/cross-sectional study | 84 informal caregivers | Questionnaires | Association between patient and carer wellbeing | Carer and patient level of distress and QoL were correlated |
| Sherman et al. (2015) [33], USA | Quantitative/cross-sectional study | 64 informal caregivers | Questionnaires | Perceived social support, perceived health and depressive symptoms of informal caregivers of hospice patients with advanced pancreatic cancer | Family informal caregivers reported strong perceived social support, very good self-perceived health and low levels of depressive symptoms |
| Engebreston et al. (2015) [5], USA | Quantitative/cross-sectional study | 213 informal caregivers (112 current informal caregivers, 102 bereaved informal caregivers) | Questionnaires | Perceptions about diagnosis and daily life with PC from patients and informal caregivers |
Greater extent of negative emotional impact experienced by informal caregivers when compared with patients Significant differences in perception between informal caregivers and patients on the roles/tasks of informal caregivers |
CRS Civil Registration System, DCR Danish cancer registry, EST endoscopic pancreatic sphincterotomy, GI gastrointestinal, PC pancreatic cancer, PEI pancreatic exocrine insufficiency, QoL quality-of-life, USA United States of America
Informal caregivers were predominantly spouses to patients with pancreatic cancer (98.6%, 6058/6142) [5, 6, 28, 33, 34]. The majority of caregivers were female (60.6%, 3748/6178). Most patients (74.7%, 4314/5772) cared for by the informal caregivers had advanced or metastatic pancreatic cancer.
Quality appraisal
The five qualitative studies were critically appraised using the CASP qualitative study checklist (Table 2) [27–31]. All studies were considered good quality (17 to 22 points). From a maximum of 22 points, three studies scored 17 points [27–30] and two studies scored 18 points [31]. The lack of consideration for the relationship between researcher and participants [30, 31] and unsatisfactory data analysis [27–30] were the two most frequent reasons points were deducted during quality assessments.
Table 2.
CASP Checklist for qualitative studies
| Authors | CASP Checklist | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1a | Q2b | Q3c | Q4d | Q5e | Q6f | Q7g | Q8h | Q9i | Q10j | Q11k | Total | |
| Wong et al. (2019) [28] | SW | Y | SW | Y | Y | Y | N | Y | SW | Y | Y | 17 |
| Sherman et al. (2014) [29] | Y | Y | Y | Y | SW | Y | N | SW | SW | Y | Y | 17 |
| Gooden et al. (2013) [30] | Y | Y | Y | Y | Y | Y | N | Y | SW | Y | SW | 18 |
| Petrin et al. (2009) [31] | Y | Y | Y | Y | SW | Y | N | Y | SW | Y | Y | 18 |
| Saunder et al. (2009) [27] | Y | Y | Y | SW | SW | Y | N | Y | SW | Y | Y | 17 |
CASP Critical Appraisal Skills Programme, CT cannot tell, N no, SW somewhat, Y yes
aWas there a clear statement of the aims of the research?
bIs qualitative methodology appropriate?
cWas the research design appropriate to address the aims of the research?
dAre the theoretical underpinnings, clear, consistent, and conceptually coherent?
eWas the recruitment strategy appropriate to the aims of the research issue?
fWas the data collected in a way that addressed the research issue?
gHas the relationship between researcher and participants been adequately considered?
hHave ethical issues been taken into consideration?
iWas the data analysis sufficiently rigorous?
jIs there a clear statement of findings?
kHow valuable is the research?
The four quantitative studies were critically appraised using the MINORS tool (Table 3) [5, 6, 32, 33]. Three studies scored between 4 and 7 points and were graded as poor quality [5, 32, 33]. The cross-sectional design of the three studies meant they scored 0 points on items assessing duration of follow-up and loss of participants [5, 32, 33]. The one prospective study scored 14 points and was graded as fair quality [6]. All four studies scored 0 points for the item assessing prospective calculation of study size [5, 6, 32, 33].
Table 3.
Methodological Index of Non-randomized Studies checklist for quantitative studies
| Authors | MINORS questions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1a | Q2b | Q3c | Q4d | Q5e | Q6f | Q7g | Q8h | Q9i | Q10j | Q11k | Q12l | Total | |
| Dengsø et al. (2021) [6] | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 1 | 2 | 0 | 1 | 14 |
| Janda et al. (2017) [32] | 2 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 |
|
Sherman et al (2015) [33] |
2 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 |
| Engebreston et al. (2015) [5] | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
MINORS Methodological index of nonrandomized studies, NA not applicable
aA clearly stated aim
bInclusion of consecutive patients
cData was collected according to established protocol
dEndpoint appropriate to the aim of the study
eUnbiased assessment of the study endpoint
fFollow-up period appropriate of the study
gLoss to follow-up less than 5%
hProspective calculation of the study size
iAn adequate control group was used?
jStudied and control groups were managed at the same time
kBaseline equivalence of studied and control groups
lAdequate statistical analyses were used
Impact of informal caregiving in pancreatic cancer
Qualitative data of caregiver experiences were limited to describing caregiver burden and unmet needs. Supporting quotes illustrating caregiver experience are presented in Supplementary Table 2. Quantitative data on caregiver experience was limited to quality-of-life and is presented in Table 4.
Table 4.
Quantitative evidence of caregiver’s quality-of-life
| Mood symptoms | Quantitative evidence |
|---|---|
| Anxiety symptoms | HADS scores indicating clinical levels of anxiety were present in 39% of carers [30]. Feeling scared/anxious was reported by 12.2% of informal caregivers [5]. Significant association between patient and carer anxiety levels (p 0.027) [30] |
| There was a significantly higher first acute use (1 prescription only) of anxiolytics in partners of PC patients than in comparators [6] | |
| Among patients and carers, accessing professional psychological help was significantly associated with subclinical or clinical HADS anxiety, and it was additionally associated with poorer QoL among patients [30] | |
| Depression symptoms | Feeling sad or depressed was reported by 17.4% of informal caregivers [5], 15% of carers reported depression scores indicating clinical levels [30] |
| The highest adjusted HR of first depression was seen the first year after diagnosis [6] | |
| Educational level, chronic morbidity and bereavement status were associated with an increased risk of first depression [6] | |
| Informal caregivers’ mean score on depressive symptoms, as measured by the CES-D, was low (2.8) but 32% of informal caregivers scored 4 or higher [31] | |
| The correlation between patients and carers levels of depression was high (correlation 0.53; p < 0.001) [30] |
CES-D Centre for Epidemiological Studies Depression, HADS Hospital Anxiety and Depression Scale, HR hazard ratio, QoL quality-of-life
Caregiver Burden
Three studies contained qualitative data illustrating caregiver burden [28–30]. No quantitative data has been reported on caregiver burden.
Qualitative data were organised into a single subtheme: managing patients’ symptoms as a source of burden. Informal caregivers were distressed by the management of patients’ symptoms which represented a subjective burden. Digestive symptoms (for example, loss of appetite [28, 30], weight loss [30], nausea [28], and constipation [28]) and side effects of treatment [28] were the sources of informal caregivers’ distress. Informal caregivers felt sad and ‘helpless’ when patients’ symptoms persisted despite the caregivers’ efforts to control them [30]. Some informal caregivers reacted with anger and frustration towards the situation which later led to guilt [30]. Guilt was also experienced by bereaved informal caregivers when symptoms were not adequately managed when patients were alive [30]. Apart from inability to control symptoms, informal caregivers also experienced guilt for pressuring patients to adhere to a dietary regimen or treatment plan [29, 30]. Guilt also arose when patients developed treatment side effects as caregivers viewed themselves as responsible in causing the side effects due to their role in supporting patients to receive treatment [29, 30]. Informal caregivers were also distressed by tension in the patient-caregiver relationship which arose when patients were unwilling/unable to continue a treatment plan [28].
Unmet needs
Four studies reported qualitative data on unmet needs of informal caregivers [27–29, 31]. No quantitative data was available on unmet needs. The qualitative data were organised into three subthemes: need for better clinical communication, need for support and briefings for informal caregivers and need for help with navigating the health care system.
Two studies raised the need for better clinical communication [27, 29]. Informal caregivers described clinical communication at the time of diagnosis as insensitive [27]. They described the delivery of diagnosis as lacking empathy, as exemplified by phrases such as ‘brutal’ or ‘not warm’, and failing to treat the patient as a whole person [27]. Timing of delivery of diagnosis was also problematic with the possibility of cancer not mentioned ‘until after the surgery’ [29]. Unsatisfactory communication of medical decisions and rationales was reported by some informal caregivers [29]. Informal caregivers reported ineffective patient-clinician communication by mentioning, ‘inconsistent advice’ and ‘information overload [or] underload’ [29]. Informal caregivers suggested the development of ‘guidelines’ or ‘protocols’ to improve clinical communication in one study [27].
Three studies raised the need for support and briefings from health care professionals [28, 31] or a support system for informal caregivers [27, 31]. Informal caregivers felt there was a lack of interaction with medical providers or questions from medical professionals about their wellbeing despite their involvement in cancer care delivery [28]. They also reported feeling alone during the process of caregiving [31]. They reported they needed to ask clear questions to a provider [31] or have someone explain things to them [27], both of which represent unmet information needs.
Two studies raised the need for help with navigating health systems [28, 29]. Informal caregivers felt ‘lost in the health care system’ [28]. They suggested there was a need for ‘a point person to serve as coordinator’ [29].
Quality-of-life
Four studies provided quantitative data on quality-of-life of informal caregivers [5, 6, 32, 33]. No studies provided qualitative data on quality-of-life of informal caregivers.
A study which surveyed 213 informal caregivers found that upon diagnosis of pancreatic cancer, 12.2% and 17.4% of informal caregivers reported feeling scared/anxious and sad/depressed [5]. In another study, including 64 informal caregivers to pancreatic cancer patients admitted to hospice care, depressive symptoms assessed using the short form of Centre for Epidemiological Studies Depression (CES-D) showed a low mean score of 2.8 (max score of 10) among informal caregivers [29]. However, 32% of the study population reported a score of 4 and above which is indicative of clinical depression [33]. A separate study including 84 informal caregivers who were recruited soon after the diagnosis of pancreatic cancer found that 14% and 17% of the informal caregivers had subclinical levels of anxiety and depression respectively, while 33% and 12% had clinical levels of anxiety and depression, based on the Hospital Anxiety and Depression Scale (HADS) [32].
Dengso et al. (2021) [6] used data-linkage methods and demonstrated a threefold higher adjusted hazard ratio for depression (HR 3.2 (95% CI: 2.9; 3.7)) in partners of pancreatic cancer patients in the first year after diagnosis when compared to partners of non-cancer patients, based on the proxy of first prescription for antidepressants or hospital admission for clinical depression. The same study showed that partners of pancreatic cancer patients had a higher chance of first acute use of anxiolytics when compared to partners of non-cancer patients [6].
Predictors of increased risk of first depression among pancreatic cancer caregivers were low education level, chronic morbidity, and bereavement [6]. Predictors of subclinical or clinical anxiety were a history of access to professional psychological help [32]. There was a correlation between anxiety or depression levels between patients and their informal caregivers [32].
Discussion
The present systematic review, the first on caregivers of pancreatic cancer, has identified only nine studies, which reported qualitative or quantitative data on burden, unmet needs or quality-of-life, among informal caregivers to patients with pancreatic cancer. It identified the management of symptoms as a significant subjective burden among informal caregivers. It further identified three key unmet needs: the need for better clinical communication, the need of support and briefings for informal caregivers and the need for help with navigating health systems. It also found a high prevalence of depression and anxiety among informal caregivers.
Cancer patients tend to experience severe symptoms more frequently and to have a sharper decline in quality-of-life when compared to other chronic diseases [29]; this is particularly true in pancreatic cancer [2]. Healthcare policies and reforms in many countries now prioritize patients taking a more active role in (self-)managing their illness [29]; to effectively self-manage, patients need support, and that support often comes from a family member or friends [29]. Furthermore, health institutes’ policies also increasingly push for shorter length of hospital stay and more outpatient care thus placing greater responsibility on partners and families to supplement care received from professionals [29]. This evolution in the delivery of health care has led to the unintended sequelae of distress amongst caregiver when required to perform these caregiving tasks. It has been estimated that informal caregivers of cancer patients spend an estimated of 32.9 h a week on caregiving tasks, of which 72% involves performing complex medical or nursing tasks [35]. In the context of pancreatic cancer, the transition into caregiver role occurs very suddenly, and informal caregivers find themselves required to learn new medical information, coordinate appointment, manage medications, diet and nutrition, search for clinical trials and alternative treatments and prepare for medical emergencies within a short time span [28]. Given these trends and the aggressiveness of the disease course in pancreatic cancer in particular, modern health systems must allocate adequate resources to intervene and equip caregivers with basic medical or nursing competencies to cope with their caregiving task [36].
In our review, data on quality-of-life of informal caregivers was limited to their psychological wellbeing. The review showed large proportion of informal caregivers with clinical levels of anxiety (33%) and depression (12–32%). This level of psychological distress was similar to other studies on cancer caregivers [37]. Due to the lack of longitudinal studies, this review is not able to answer how pancreatic cancer caregivers’ quality-of-life changes across the trajectory of the illness; future studies on this would be of value. Predictors of psychological morbidity among informal caregivers were limited to sociodemographic and clinical characteristics including caregivers’ chronic morbidity, education status, bereavement, and history of access to professional psychological help [6, 32]. One study of patient-caregiver dyads showed correlations between anxiety and depression levels between patient and caregivers [32]. This suggests the possibility that interventions which support caregiver quality-of-life or psychological wellbeing may also yield benefits for patients (or vice versa).
Studies on cancer and non-cancer caregivers showed perceived burden as an important predictor of psychological morbidity [37, 38]. Different caregiving tasks, which constitute caregiver burden, impact caregiver distress to different extents. In one study on head and neck cancer, informal caregivers felt greater distress when assisting with caregiving tasks related to cancer-specific care (e.g. helping with medications) than those related to general supportive care (e.g. coordinating appointments) [39]. Feeling uncomfortable with cancer-specific care was predictive of informal caregivers’ anxiety and depression [39]. In this review, distress caused by managing pancreatic cancer symptoms featured prominently in the informal caregivers’ experiences. Future studies are needed to confirm the link between subjective burden of performing cancer-specific care and overall caregiver burden and their psychological quality-of-life in pancreatic cancer. Evidence that substantiates the proposed link would further justify the need to equip informal caregivers with necessary competencies to assist with cancer-specific care, in addition to providing psychological support to informal caregivers in need of such support.
Informal caregivers’ unmet needs identified in this review were the need for better clinical communication, need of support and briefings for caregivers and need for help with navigating the health system. Informal caregivers’ discontentment with clinical communication was largely directed at the delivery of diagnosis which they felt lacked empathy. In parallel with this, a survey of pancreatic cancer patients’ experience with delivery of news found two-third of patients felt their diagnosis was not given sensitively [40]. Ineffective patient-clinician communication, exemplified by contradictory, excess or inadequate information, was raised by a smaller subset of informal caregivers. This finding again echoes findings from the same patient survey wherein one-third of patients felt staff did not talk to them about their care and treatment in a way that they could understand [40]. Deficiencies in patient-clinician communication around cancer is an area that needs improvement; this is arguably especially important in a disease with such a poor prognosis, where the patient may decline very rapidly. Though tools such as guidelines and protocols have limitations, they can be useful adjuncts in supporting clinicians in navigating complexities of patient-clinical interactions when discussing cancer-related issues [41].
The second unmet need was the need for support and briefings from health care professionals. This again is related to communication with health professionals. As the focus of the health care system is to treat and care for the patient, informal caregivers felt neglected by the process of care delivery. This neglect has been studied by many researchers [42–44]. Despite the importance of informal caregiver to the modern health system, they report being seldom acknowledged, that health professional rarely show interest in them (and their health and ability to cope) and that health professionals spend insufficient time informing them about specific aspects of a disease such as symptoms and side effects [45]. Suboptimal interaction with informal caregivers may lead to caregiver distress and less competency in dealing with uncertainty and problem solving [42], thus potentially adversely impacting on the patient. This provides a rationale for seeking to find ways to better meet caregivers’ needs in this regard.
The final unmet need among pancreatic cancer informal caregivers is related to the need for help in navigating the health system. Cancer care delivery is complex, and patients may encounter multiple specialties including surgery, oncology, palliative, and occasionally emergency services across his/her disease course. Patient navigation programs could be one route to better meet caregiver (and patient) needs and improve access to the services [46].
Comparing our findings with those from past reviews suggests that there are some broad similarities between caregiving in pancreatic cancer and other cancers [14, 47]. For example, in a systematic review focused on caregiving in solid tumour patients, the management of symptoms also emerged as the foremost reported factor affecting burden [47]. In the review of Wang et al., on unmet needs in advanced cancer, the authors noted that several studies reported that caregivers had unmet needs in relation to illness and treatment information, which has some parallels with our findings, although ours are more specific [14]. Beyond this, direct comparisons between pancreatic cancer and other malignancies are difficult owing to the limited evidence base on caregiving in pancreatic cancer and differences in study methodologies.
Limitations of the review relate both to the review process and the nature of available evidence. We did not register the review protocol a priori with PROSPERO or another external database. A single author undertook the initial screening process of title and abstract. A ‘single screening’ approach is cost-effective and reduces workload [48], but risks missing studies which can impact the findings of the review [49]. Restricting inclusion to English-language studies also risked missing important evidence. Considering limitations in the evidence-base itself, quantitative data on caregiver burden and unmet needs is lacking and that on quality-of-life only covers a single dimension: psychological wellbeing. It is likely that caregivers’ role(s) across different phases of the illness trajectory evolve(s) with the changing tangible and intangible demands imposed on them. Prospective studies that track changes to caregivers’ experience (burden, needs and quality-of-life) across the trajectory of illness of pancreatic cancer are currently lacking. In addition, most data pertain to caregivers supporting patients with advanced or metastatic disease. Lastly, patient or caregiver characteristics, or other factors, that might be associated with greater burden, more needs and worse quality-of-life, and the interrelationships between different aspects of caregivers’ experience (burden, needs and quality-of-life) have largely not been examined. These limitations argue for studies with longitudinal design which use multi-method (i.e., qualitative and quantitative) approaches to characterise and understand multidimensional aspects (burden, needs and quality-of-life) of informal caregivers’ experience in pancreatic cancer across the illness trajectory. Such studies could also shed light on which caregivers are at greatest risk of poor experiences and the interrelationships between different aspects of caregiver experience.
Conclusion
Informal caregivers of pancreatic cancer patients were burdened by management of patients’ symptoms. The unmet needs encountered were for better clinical communication, support and briefings for informal caregivers and help with navigating health systems. A large proportion of the informal caregivers experience anxiety and depression. Future longitudinal studies employing multi-method approaches are needed to better characterise and understand informal caregivers’ experiences.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- CASP
Critical Appraisal Skill Programme
- CES-D
Centre for Epidemiological Studies Depression
- MINORS
Methodological Index of Non-randomised Studies
Author contribution
Sanjay Pandanaboyana, Linda Sharp, Keno Mentor, Lisa Crowe and Eric Chong contributed to the study conception and design. Material preparation, data collection and analysis were performed by Eric Chong, Lisa Crowe and Linda Sharp. Original draft was prepared by Eric Chong, Lisa Crowe and Linda Sharp, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
This work was conducted under the auspices of Research and Innovation Grant from Pancreatic Cancer UK (no grant number).
LC is funded by a grant from Macmillan Cancer Support (MRGS-705).
Data Availability
All of the relevant data is contained within the article and supplementary material.
Declarations
Ethics approval
N/A
Consent to participate
N/A
Consent for publication
N/A
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kamisawa T, Wood LD, Itoi T, Takaori K (2016) Pancreatic cancer. The Lancet 388(10039):73–85 [DOI] [PubMed] [Google Scholar]
- 2.Mizrahi JD, Surana R, Valle JW, Shroff RT (2020) Pancreatic cancer. Lancet 395(10242):2008–2020 [DOI] [PubMed] [Google Scholar]
- 3.Khalaf N, El-Serag HB, Abrams HR, Thrift AP (2021) Burden of pancreatic cancer: from epidemiology to practice. Clin Gastroenterol Hepatol 19(5):876–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kleeff J, Korc M, Apte M, La Vecchia C, Johnson CD, Biankin AV et al (2016) Pancreatic cancer. Nat Rev Dis Primers 2(1):1–22 [DOI] [PubMed] [Google Scholar]
- 5.Engebretson A, Matrisian L, Thompson C (2015) Pancreatic cancer: patient and caregiver perceptions on diagnosis, psychological impact, and importance of support. Pancreatology 15(6):701–707 [DOI] [PubMed] [Google Scholar]
- 6.Dengso KE, Thomsen T, Andersen EW, Hansen CP, Christensen BM, Hillingso J et al (2021) The psychological symptom burden in partners of pancreatic cancer patients: a population-based cohort study. Supp Care Canc 29(11):6689–6699 [DOI] [PubMed]
- 7.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS (2014) Caregiver burden: a clinical review. JAMA 311(10):1052–1060 [DOI] [PubMed] [Google Scholar]
- 8.Kent EE, Mollica MA, Buckenmaier S, Smith AW (eds) (2019) The characteristics of informal cancer caregivers in the United States. Elsevier [DOI] [PubMed] [Google Scholar]
- 9.Gerhardt S, Dengso KE, Herling S, Thomsen T (2020) From bystander to enlisted carer - a qualitative study of the experiences of caregivers of patients attending follow-up after curative treatment for cancers in the pancreas, duodenum and bile duct. Eur J Oncol Nurs : Official J Eur Oncol Nurs Soc 44:101717 [DOI] [PubMed] [Google Scholar]
- 10.Schulz R, O’Brien AT, Bookwala J, Fleissner K (1995) Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist 35(6):771–791 [DOI] [PubMed] [Google Scholar]
- 11.Applebaum AJ, Breitbart W (2013) Care for the cancer caregiver: a systematic review. Palliat Support Care 11(3):231–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Girgis A, Lambert S, Johnson C, Waller A, Currow D (2013) Physical, psychosocial, relationship, and economic burden of caring for people with cancer: a review. J Oncol Pract 9(4):197–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balfe M, Maguire R, Hanly P, Butow P, O’Sullivan E, Timmons A et al (2016) Distress in long-term head and neck cancer carers: a qualitative study of carers’ perspectives. J Clin Nurs 25(15–16):2317–2327 [DOI] [PubMed] [Google Scholar]
- 14.Wang T, Molassiotis A, Chung BPM, Tan J-Y (2018) Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care 17(1):1–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanly P, Maguire R, Hyland P, Sharp L (2015) Examining the role of subjective and objective burden in carer health-related quality of life: the case of colorectal cancer. Support Care Cancer 23(7):1941–1949 [DOI] [PubMed] [Google Scholar]
- 16.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ (2009) What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer 17(8):1117–1128 [DOI] [PubMed] [Google Scholar]
- 17.Bauer MR, Bright EE, MacDonald JJ, Cleary EH, Hines OJ, Stanton AL (2018) Quality of life in patients with pancreatic cancer and their caregivers: a systematic review. Pancreas 47(4):368–375 [DOI] [PubMed] [Google Scholar]
- 18.Harding R, Gao W, Jackson D, Pearson C, Murray J, Higginson IJ (2015) Comparative analysis of informal caregiver burden in advanced cancer, dementia, and acquired brain injury. J Pain Symptom Manage 50(4):445–452 [DOI] [PubMed] [Google Scholar]
- 19.Cancer Research UK. Pancreatic cancer incidence statistics. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/pancreatic-cancer/incidence#ref-3. Accessed 01/06/2022
- 20.Hoenig J, Hamilton MW (1966) The schizophrenic patient in the community and his effect on the household. Int J Soc Psychiatry 12(3):165–176 [DOI] [PubMed] [Google Scholar]
- 21.Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM (2003) Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage 26(4):922–953 [DOI] [PubMed] [Google Scholar]
- 22.Osse BHP, Vernooij-Dassen MJFJ, de Vree BPW, Schadé E, Grol RPTM (2000) Assessment of the need for palliative care as perceived by individual cancer patients and their families: a review of instruments for improving patient participation in palliative care. Cancer 88(4):900–911 [DOI] [PubMed] [Google Scholar]
- 23.Long HA, French DP, Brooks JM (2020) Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci 1(1):31–42 [Google Scholar]
- 24.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716 [DOI] [PubMed] [Google Scholar]
- 25.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M et al (2006) Guidance on the conduct of narrative synthesis in systematic reviews. A Prod ESRC Methods Program Version 1(1):b92 [Google Scholar]
- 26.Braun V, Clarke V (2021) Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Couns Psychother Res 21(1):37–47 [Google Scholar]
- 27.Saunders C, Gooden H, Robotin M, Mumford J (2009) As the bell tolls: a foundation study on pancreatic cancer consumer’s research priorities. BMC Res Notes 2:179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong SS, George TJ Jr, Godfrey M, Le J, Pereira DB (2019) Using photography to explore psychological distress in patients with pancreatic cancer and their caregivers: a qualitative study. Support Care Cancer 27(1):321–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sherman DW, McGuire DB, Cheon JY, Free D (2014) A pilot study of the experience of family caregivers of patients with advanced pancreatic cancer using a mixed methods approach. J Pain Symptom Manage 48(3):385 [DOI] [PubMed] [Google Scholar]
- 30.Gooden HM, White KJ (2013) Pancreatic cancer and supportive care - pancreatic exocrine insufficiency negatively impacts on quality of life. Support Care Cancer 21(7):1835–1841 [DOI] [PubMed] [Google Scholar]
- 31.Petrin K, Bowen DJ, Alfano CM, Bennett R (2009) Adjusting to pancreatic cancer: perspectives from first-degree relatives. Palliat Support Care 7(3):281–288 [DOI] [PubMed] [Google Scholar]
- 32.Janda M, Neale RE, Klein K, Beesley VL, O’Connell DL, Gooden H et al (2017) Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology 17(2):321–327 [DOI] [PubMed] [Google Scholar]
- 33.Witt Sherman D, McMillan SC (2015) The physical health of patients with advanced pancreatic cancer and the psychological health of their family caregivers when newly enrolled in hospice. J Hosp Palliat Nurs 17(3):235–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Janda M, Neale RE, Klein K, O’Connell DL, Gooden H, Goldstein D et al (2017) Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology 17(2):321–327 [DOI] [PubMed] [Google Scholar]
- 35.Trevino KM, Prigerson HG, Maciejewski PK (2018) Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psychooncology 27(1):243–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beesley VL, Turner J, Chan RJ, Yates P, Gordon LG, Burge M et al (2020) Supporting patients and carers affected by pancreatic cancer: a feasibility study of a counselling intervention. Eur J Oncol Nurs 46:101729 [DOI] [PubMed] [Google Scholar]
- 37.Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC et al (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170(12):1795–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chappell NL, Penning M (1996) Behavioural problems and distress among caregivers of people with dementia. Ageing Soc 16(1):57–73 [Google Scholar]
- 39.Balfe M, O’Brien KM, Timmons A, Butow P, O’Sullivan E, Gooberman-Hill R et al (2018) Informal caregiving in head and neck cancer: caregiving activities and psychological well-being. Eur J Cancer Care 27(2):e12520 [DOI] [PubMed] [Google Scholar]
- 40.Watson EK, Brett J, Hay H, Witwicki C, Perris A, Poots AJ et al (2019) Experiences and supportive care needs of UK patients with pancreatic cancer: a cross-sectional questionnaire survey. BMJ Open 9(11):e032681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eggly S, Penner L, Albrecht TL, Cline RJW, Foster T, Naughton M et al (2006) Discussing bad news in the outpatient oncology clinic: rethinking current communication guidelines. J Clin Oncol 24(4):716–719 [DOI] [PubMed] [Google Scholar]
- 42.Brown M-A, Stetz K (1999) The labor of caregiving: a theoretical model of caregiving during potentially fatal illness. Qual Health Res 9(2):182–197 [DOI] [PubMed] [Google Scholar]
- 43.Waldrop DP, Meeker MA, Kerr C, Skretny J, Tangeman J, Milch R (2012) The nature and timing of family-provider communication in late-stage cancer: a qualitative study of caregivers’ experiences. J Pain Symptom Manage 43(2):182–194 [DOI] [PubMed] [Google Scholar]
- 44.Gilbert E, Ussher JM, Perz J, Hobbs K, Kirsten L (2010) Positive and negative interactions with health professionals: a qualitative investigation of the experiences of informal cancer carers. Cancer Nurs 33(6):E1–E9 [DOI] [PubMed] [Google Scholar]
- 45.Lund L, Ross L, Petersen MA, Groenvold M (2015) The interaction between informal cancer caregivers and health care professionals: a survey of caregivers’ experiences of problems and unmet needs. Support Care Cancer 23(6):1719–1733 [DOI] [PubMed] [Google Scholar]
- 46.Robinson-White S, Conroy B, Slavish KH, Rosenzweig M (2010) Patient navigation in breast cancer: a systematic review. Cancer Nurs 33(2):127–140 [DOI] [PubMed] [Google Scholar]
- 47.Thana K, Lehto R, Sikorskii A, Wyatt G (2021) Informal caregiver burden for solid tumour cancer patients: a review and future directions. Psychol Health 36(12):1514–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doust JA, Pietrzak E, Sanders S, Glasziou PP (2005) Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. J Clin Epidemiol 58(5):444–9 [DOI] [PubMed] [Google Scholar]
- 49.Waffenschmidt S, Knelangen M, Sieben W, Bühn S, Pieper D (2019) Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol 19(1):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All of the relevant data is contained within the article and supplementary material.