Abstract
Objective
The predominant mechanism driving hyperuricemia in gout is renal uric acid underexcretion; however, the standard urate‐lowering therapy (ULT) recommendation is first‐line xanthine oxidase inhibitor (XOI), irrespective of the cause of hyperuricemia. This comparative effectiveness clinical trial was undertaken to compare first‐line nontitrated low‐dose benzbromarone (LDBen) uricosuric therapy to XOI ULT with low‐dose febuxostat (LDFeb) in gout patients with renal uric acid underexcretion.
Methods
We conducted a prospective, randomized, single‐center, open‐label trial in men with gout and renal uric acid underexcretion (defined as fractional excretion of urate <5.5% and uric acid excretion ≤600 mg/day/1.73 m2). A total of 196 participants were randomly assigned to receive LDBen 25 mg daily or LDFeb 20 mg daily for 12 weeks. All participants received daily urine alkalization with oral sodium bicarbonate. The primary end point was the rate of achieving the serum urate target of <6 mg/dl.
Results
More participants in the LDBen group achieved the serum urate target than those in the LDFeb group (61% compared to 32%, P < 0.001). Rates of adverse events, including gout flares and urolithiasis, did not differ between groups, with the exception of greater transaminase elevation in the LDFeb group (4% for LDBen compared to 15% for LDFeb, P = 0.008).
Conclusion
Compared to LDFeb, LDBen has superior urate‐lowering efficacy and similar safety in treating relatively young and healthy patients with renal uric acid underexcretion–type gout.
INTRODUCTION
In gout, increased serum urate, called hyperuricemia, promotes crystal deposition of monosodium urate monohydrate crystals in articular and periarticular structures, which can trigger acute episodes of very painful inflammatory arthritis (gout flare) (1, 2). Longstanding hyperuricemia and gout can also lead to palpable tophi, joint damage, and urolithiasis (1). Urate‐lowering therapy (ULT) is the central strategy for effectively controlling hyperuricemia and gout (3, 4, 5). However, the pathophysiology of hyperuricemia is heterogeneous in gout patients (6, 7, 8, 9, 10).
Renal uric acid underexcretion is the predominant cause of hyperuricemia (~70–90% of gout patients) (7). However, uric acid overproduction and intestinal uric acid underexcretion with renal uric acid overload can also drive hyperuricemia alone or in combination with renal uric acid underexcretion in gout (6, 8, 9, 10). Ichida et al (9) developed criteria to classify hyperuricemia in gout into uric acid overproduction, renal uric acid underexcretion, extrarenal uric acid underexcretion, and combined mechanism types, via clinical and genetic test results and via fractional excretion of urate and uric acid excretion under low‐purine diet conditions. As such, fractional excretion of urate <5.5% and uric acid excretion ≤600 mg/day/1.73 m2 is used as criteria to define renal uric acid underexcretion–type gout (9).
The principal oral ULT agents are the xanthine oxidase inhibitors (XOIs) allopurinol and febuxostat, and uricosuric agents that all act as inhibitors of the renal urate transporter 1 (URAT1) (benzbromarone and probenecid) (11, 12, 13, 14). Based on available evidence to date, the 2020 American College of Rheumatology (ACR) gout management guidelines and 2016 EULAR gout management guidelines recommend XOI using allopurinol as the first‐line ULT approach (12, 13). Whereas the 2016 EULAR guidelines recommend uricosuric therapy as a second‐line ULT option in gout, the 2020 ACR guidelines only provide conditional recommendation for probenecid use as a second‐line agent after treatment failure with allopurinol, and benzbromarone is not part of this clinical guideline, since the drug is not approved for use in the US (12, 13). Allopurinol, febuxostat, and benzbromarone are all broadly used in Asia and are comparably effective in achieving serum urate target and gout flare burden reduction in ULT treat‐to‐target dose titration studies in Asian populations; however, the prevalence of HLA–B*5801 that is associated with allopurinol hypersensitivity is higher in those of Han Chinese, Korean, and Thai descent (7.4%) (11, 12, 15, 16, 17, 18). Notably, febuxostat is a recommended ULT in China, though at a dose of only 20–40 mg daily (13, 19).
Moreover, a randomized controlled trial in Chinese gout patients that did not separate patients according to pathophysiology driving hyperuricemia used a 20‐mg daily febuxostat dose, which is a quarter of the maximum approved in the US (and a sixth of the maximum dose prescribed outside the US), and used benzbromarone 25 mg daily (a quarter of the typical maximum dose used in clinical practice and an eighth of the maximum advised dose most often used in moderate‐to‐severe renal impairment); the rate of achieving the serum urate target was similar compared to these low‐dose regimens (15) (low‐dose febuxostat [LDFeb] and low‐dose benzbromarone [LDBen]).
We hypothesized that LDBen would have superior urate‐lowering ability and similar safety compared to first‐line LDFeb in patients with renal uric acid underexcretion–type gout. The aim of this randomized comparative trial was to compare efficacy and safety of LDFeb and LDBen to treat renal uric acid underexcretion–type gout.
PATIENTS AND METHODS
Study design and participants
This open‐label, prospective, randomized study was conducted at the Gout Clinic of the Affiliated Hospital of Qingdao University. We compared the efficacy and safety of LDBen and LDFeb in men with renal underexcretion–type gout who were treated with 12 weeks of ULT. Inclusion criteria included the following: gout according to the 2015 ACR/EULAR gout classification criteria (19), male sex, age ranging from 18 years to 70 years, serum urate levels between 7.0 mg/dl and 10.0 mg/dl, and renal uric acid underexcretion. Renal underexcretion–type gout is defined as fractional excretion of urate of <5.5% and uric acid excretion of ≤600 mg/day/1.73 m2 (9). Participants were excluded if 1 of the following criteria was met: fractional excretion of urate of ≥5.5% or uric acid excretion of >600 mg/day/1.73 m2, gout flare within 2 weeks before enrollment, urinary calculi, elevated transaminases (>2.0 times the upper limit of normal [ULN]), estimated glomerular filtration rate (eGFR) of <60 ml/minute/1.73 m2, or the need to take any urate‐lowering drug or other medicine affecting serum urate levels (Supplementary Table 1, available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.42266). The ethics committee at the Affiliated Hospital of Qingdao University approved the trial. It was registered in the Chinese Clinical Trial Registration Center (identifier: ChiCTR1900022981). Written informed consent was obtained from all participants.
Treatment and procedures
As described in the previous study (16), all participants enrolled in the trial underwent a 14‐day washout period, which indicated that they stopped receiving urate‐lowering drugs and adhered to a low‐purine diet. During the study, other urate‐lowering drugs or drugs that are known to affect the serum urate level were prohibited. A randomization list was created using a random number generator. Participants were assigned a random code and were randomized in a 1:1 ratio to receive either LDBen or LDFeb. Participants received oral febuxostat or benzbromarone once daily in the morning. All participants received daily urine alkalization with oral sodium bicarbonate, 1 gm/3 times daily. During treatment with the study drug, colchicine and/or nonsteroidal antiinflammatory drugs were prescribed to participants if they experienced a gout flare. In participants with serum transaminase elevation that more than doubled from baseline values, hepatoprotective treatment (diammonium glycyrrhizinate, silibinin, or polyene phosphatidylcholine) was prescribed.
The clinician did not know which treatment option a participant would receive before randomization. Both the participant and the treating clinician knew the treatment allocation after randomization. Participants were given advice on nondrug treatment approaches, including diet and exercise.
Information collected at baseline included age, age at disease onset, disease duration, lifestyle, body weight, height, body mass index (BMI) (weight [kg]/height [m2]), disease history (tophus, hypertension, fatty liver, hyperlipidemia, diabetes, cardiovascular disease [CVD]), and family history of gout. Serum biochemical data that were collected included serum urate levels, alanine aminotransferase (ALT) level, aspartate aminotransferase (AST) level, fasting glucose values, triglycerides, total cholesterol, and creatinine levels. Renal function was assessed as the eGFR, determined using Chronic Kidney Disease Epidemiology Collaboration design formulas: for creatinine ≤80 μmoles/liter (0.9 mg/dl), eGFR (in ml/minute/1.73 m2) = 141 × (creatinine [mg/dl]/0.9)−0.411 × 0.993age(years); for creatinine >80 μmoles/liter (0.9 mg/dl), eGFR (in ml/minute/1.73 m2) = 141 × (creatinine [mg/dl]/0.9)−1.209 × 0.993age(years). Clinical obesity was defined as a BMI of ≥28 kg/m2, based on criteria in Asian populations (20, 21). We measured the biochemical parameters at every visit. Participants were considered withdrawn cases after 3 consecutive days without medication.
Outcomes
The primary efficacy outcome was the rate of achieving the target serum urate level of <6.0 mg/dl at week 12 of treatment. Secondary efficacy outcomes included the rate of achieving the target serum urate level of <5.0 mg/dl, the change in serum urate (serum urate Δ% [baseline serum urate level–visit serum urate level]/baseline serum urate level), and changes in other laboratory parameters including serum urate level, fasting glucose values, total cholesterol, triglycerides, AST level, ALT level, creatinine level, and eGFR. Safety outcomes included the incidence of gout flares and the percentage of participants with treatment‐emergent adverse events (AEs). Changes in renal function, changes in liver function, and urolithiasis were AEs of particular interest in this study.
Sample size
Sample size was determined based on the primary end point (rate of achieving the target serum urate level <6.0 mg/dl at week 12 of treatment). Based on findings from the previous study and the preliminary study, we estimated that the rate of achieving the serum urate target would be 60% in the LDBen group and 38% in the LDFeb group (15, 16). We calculated that a sample size of 78 patients per group would be required according to a 5% 2‐sided significance level and 80% power to detect a difference between the LDBen group and LDFeb group (in a 1:1 allocation). A sample size of 98 was calculated for each group to account for an estimated 20% dropout rate.
Statistical analysis
Statistical analyses were performed using SPSS version 22.0 (IBM). All continuous variables are shown as the mean ± SD or the median (interquartile range) and categorical variables are shown as percentages. Continuous variables were compared using t‐test for independent samples or Mann‐Whitney U test, and categorical variables between the 2 groups were compared using chi‐square test. Within‐group variables from each visit were compared to baseline values using paired‐sample t‐test or Wilcoxon signed rank test. P values less than 0.05 were considered statistically significant.
RESULTS
Study flow and clinical characteristics
The clinical trial was initiated on May 3, 2019 and completed on January 26, 2021. In this trial, 196 participants were randomized to receive ULT with LDBen (N = 98) or LDFeb (N = 98) (Figure 1). Overall, 183 participants (93.4%) completed the trial, and 13 participants dropped out before the end of the study (6 in the LDBen group, 7 in the LDFeb group). The reasons cited for discontinuation included voluntarily withdrawal (4 in the LDBen group, 5 in the LDFeb group) and drug discontinuation (1 in the LDBen group, 2 in the LDFeb group). One participant in the LDBen group dropped out of the trial because of gout flare at week 4 (Figure 1). Patients in both groups received medication according to the regimen, as confirmed by pill counts.
Figure 1.
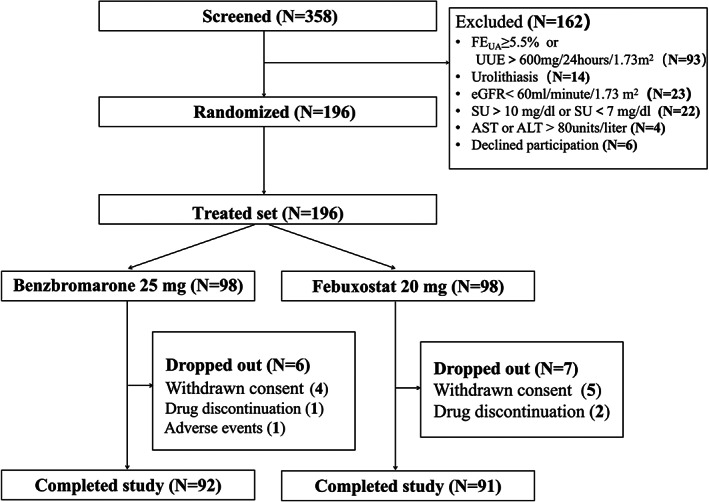
Flow chart of the study design showing how patients with renal underexcretion–type gout were organized into the benzbromarone and febuxostat treatment groups. FEUA = fractional excretion of urate; UUE = uric acid excretion; eGFR = estimated glomerular filtration rate; SU = serum urate; ALT = alanine aminotransferase; AST = aspartate aminotransferase.
Clinical characteristics at baseline were similar between the 2 groups (Table 1). Participants receiving either LDBen or LDFeb were a mean age of 43.89 years and 43.29 years, respectively. The mean ± SD duration of gout was similar in the 2 groups (LDBen 5.2 ± 4.6 years versus LDFeb 5.6 ± 4.8 years). More than 75% of study participants had not received prior ULT. Baseline serum urate levels were 8.72 ± 0.73 mg/dl in the LDBen group and 8.59 ± 0.70 mg/dl in the LDFeb group. Laboratory parameters and coexisting conditions (obesity, hypertension, fatty liver, hyperlipidemia, diabetes, and CVD) were similar at baseline between the groups (Table 1).
Table 1.
Baseline demographic and clinical characteristics of patients with renal underexcretion–type gout receiving either LDBen or LDFeb*
| LDBen (n = 98) | LDFeb (n = 98) | |
|---|---|---|
| Demographic and clinical characteristics | ||
| Age, mean ± SD years | 43.89 ± 13.10 | 43.29 ± 12.22 |
| Male, no. (%) of patients | 98 (100) | 98 (100) |
| Height, mean ± SD cm | 174.01 ± 5.84 | 175.37 ± 5.73 |
| Body weight, mean ± SD kg | 81.07 ± 9.82 | 82.98 ± 11.27 |
| Body mass index, mean ± SD kg/m2 | 26.77 ± 2.85 | 26.97 ± 3.21 |
| SBP, mean ± SD mm Hg | 133.19 ± 16.23 | 134.18 ± 15.32 |
| DBP, mean ± SD mm Hg | 84.21 ± 10.80 | 85.84 ± 12.09 |
| Gout feature | ||
| Serum urate, median (IQR) mg/dl | 8.70 (7.91–9.06) | 8.77 (8.10–9.27) |
| Age at onset, mean ± SD years | 39 ± 12 | 38 ± 10 |
| Duration of gout, mean ± SD years | 5.2 ± 4.6 | 5.6 ± 4.8 |
| Gout flare frequency, no. (%) of patients | ||
| Less than twice a year | 48 (49) | 45 (46) |
| Twice or more than twice a year | 50 (51) | 53 (54) |
| Tophus, no. (%) of patients | 18 (18) | 18 (18) |
| Family history of gout, no. (%) of patients | 16 (16) | 21 (21) |
| ULT naive, no. (%) of patients | 75 (77) | 79 (81) |
| Coexisting conditions, no. (%) of patients | ||
| Obesity | 40 (41) | 32 (33) |
| Hypertension | 16 (16) | 20 (20) |
| Cardiovascular disease | 2 (2) | 0 (0) |
| Fatty liver | 17 (17) | 24 (24) |
| Hyperlipidemia | 20 (20) | 17 (17) |
| Diabetes | 15 (15) | 14 (14) |
| Blood chemistry parameters | ||
| Serum creatinine, median (IQR) μmoles/liter | 82 (76–93) | 85 (76–95) |
| Fasting glucose, mean ± SD mmoles/liter | 5.52 ± 0.68 | 5.56 ± 0.63 |
| Cholesterol, mean ± SD mmoles/liter | 4.84 ± 0.82 | 4.76 ± 1.17 |
| Triglyceride, median (IQR) mmoles/liter | 1.69 (1.17–2.34) | 1.67 (1.25–2.53) |
| AST, median (IQR) units/liter | 21.00 (18.00–24.25) | 19 (17–24) |
| ALT, median (IQR) units/liter | 26.0 (18.0–37.5) | 23.50 (16.75, 36.00) |
| eGFR, mean ± SD ml/minute/1.73 m2 | 96.30 ± 15.51 | 94.60 ± 15.09 |
LDBen = low‐dose benzbromarone; LDFeb = low‐dose febuxostat; SBP = systolic blood pressure; DBP = diastolic blood pressure; IQR = interquartile range; ULT = urate‐lowering therapy; AST = aspartate aminotransferase; ALT = alanine aminotransferase; eGFR = estimated glomerular filtration rate.
Efficacy
The primary efficacy outcome was the proportion of participants with serum urate levels of <6 mg/dl during the treatment period. The proportion of participants who achieved the treatment urate target was significantly higher in the LDBen group than in the LDFeb group at week 4 (58% versus 42%, P = 0.03), week 8 (59% versus 33%, P < 0.001), and week 12 (61% versus 32%, P < 0.001) (Figure 2A).
Figure 2.
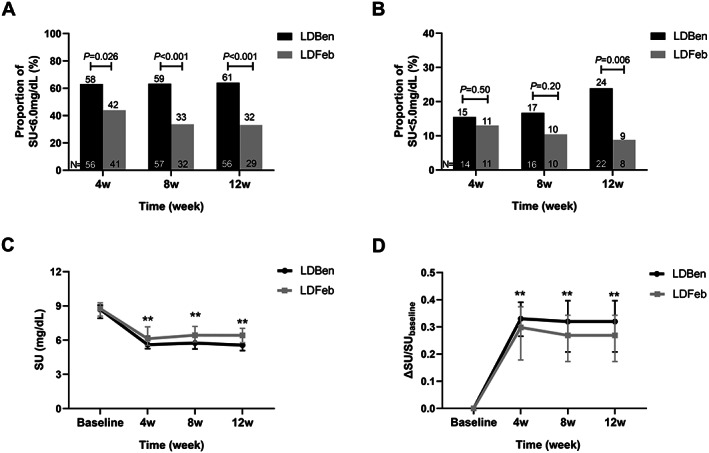
Efficacy of low‐dose benzbromarone (LDBen) and low‐dose febuxostat (LDFeb) in patients with renal underexcretion–type gout. A and B, Proportion of participants with serum urate levels of <6.0 mg/dl (A) and <5.0 mg/dl (B) at weeks 4, 8, and 12 after the initiation of treatment. Values at the bottom of the bars show the number of participants and values at the top of the bars show the percentage of participants. C, Trend of serum urate level in the 2 groups at weeks 4, 8, and 12. D, Change in serum urate levels in the 2 groups at weeks 4, 8, and 12, calculated as Δ = (baseline serum urate level — visit serum urate level)/baseline serum urate level. Results at each timepoint in C and D are the mean ± SD. ** = P < 0.01.
The proportion of participants who achieved a serum urate level of <5.0 mg/dl in the 2 groups was similar at weeks 4 and 8, but more participants in the LDBen group achieved this lower serum urate level after 12 weeks (LDBen 24% versus LDFeb 9%, P = 0.006) (Figure 2B). The mean serum urate concentration during the entire study period in the LDBen group was significantly lower than in the LDFeb group (P < 0.001). At week 12, the mean ± SD serum urate level decreased from 8.59 ± 0.70 mg/dl to 5.81 ± 1.19 mg/dl in the LDBen group and from 8.72 ± 0.73 mg/dl to 6.39 ± 0.94 mg/dl in the LDFeb group, respectively (Figure 2C). The mean ± SD percentage change in serum urate level (serum urate Δ = [baseline serum urate level – visit serum urate level]/baseline serum urate level) at week 12 was 32.0% in the LDBen group and 26.5% in the LDFeb group (P < 0.001) (Figure 2D).
No differences were detected in terms of glucose and lipid metabolic markers between the 2 groups at week 12 (Table 2). However, the mean fasting glucose concentration in the LDBen group was significantly lower than in the LDFeb group at weeks 4 and 8 (P < 0.001 at both time points) (Table 2).
Table 2.
Major clinical parameters during the trial in 98 participants receiving LDBen and 98 participants receiving LDFeb*
| Baseline | Week 4 | Week 8 | Week 12 | |
|---|---|---|---|---|
| Completed follow‐up, no. (%) of patients | ||||
| LDBen | 98 (100) | 97 (99) | 96 (98) | 92 (94) |
| LDFeb | 98 (100) | 98 (100) | 96 (98) | 91 (93) |
| Serum urate, median (IQR) mg/dl | ||||
| LDBen | 8.70 (7.91–9.06) | 5.60 (5.26–6.34)†, ‡ | 5.74 (5.22–6.60)†, ‡ | 5.57 (5.08–6.46)†, ‡ |
| LDFeb | 8.77 (8.10–9.27) | 6.12 (5.55–7.16)‡ | 6.44 (5.84–7.21)‡ | 6.42 (5.77–7.03)‡ |
| Fasting glucose, mean ± SD mmoles/liter | ||||
| LDBen | 5.52 ± 0.68 | 5.35 ± 0.54†, ‡ | 5.34 ± 0.44†, ‡ | 5.39 ± 0.51 |
| LDFeb | 5.56 ± 0.63 | 5.65 ± 0.58 | 5.69 ± 0.59§ | 5.54 ± 0.58 |
| Cholesterol, mean ± SD mmoles/liter | ||||
| LDBen | 4.84 ± 0.82 | 4.80 ± 0.84 | 4.84 ± 0.86 | 4.80 ± 0.85 |
| LDFeb | 4.76 ± 1.17 | 4.77 ± 0.99 | 4.83 ± 0.93 | 4.85 ± 1.01 |
| Triglycerides, median (IQR) mmoles/liter | ||||
| LDBen | 1.69 (1.17–2.34) | 1.57 (1.19–1.99) | 1.56 (1.14–2.00)§ | 1.50 (1.19–2.11)‡ |
| LDFeb | 1.67 (1.25–2.52) | 1.74 (1.22–2.67) | 1.65 (1.17–2.44) | 1.77 (1.17–2.50) |
| AST, median (IQR) units/liter | ||||
| LDBen | 21.00 (18.00–24.25) | 20 (17–23)†, § | 21.00 (17.25–23.75) | 20.00 (16.25–23.00)† |
| LDFeb | 19 (17–24) | 22 (18–27)‡ | 21 (18–28)‡ | 22 (18–28)‡ |
| ALT, median (IQR) units/liter | ||||
| LDBen | 26.0 (20.0–37.5) | 24 (18–33)‡ | 25.00 (19.00–33.75) | 24 (17–33)‡, ¶ |
| LDFeb | 23.50 (16.75–36.00) | 27 (18–37)§ | 27.00 (18.00–40.75)§ | 28 (19–40) |
| Creatinine, median (IQR) μmoles/liter | ||||
| LDBen | 82 (76–93) | 79.5 (72.0–88.0)‡ | 84 (76–91) | 81 (75–89) |
| LDFeb | 85.00 (76.00–95.25) | 81.0 (74.0–90.5)‡ | 82.5 (75.0–90.0)§ | 83 (74–91) |
| eGFR, mean ± SD ml/minute/1.73 m2 | ||||
| LDBen | 96.30 ± 15.51 | 100.57 ± 19.96§ | 96.86 ± 15.00 | 98.39 ± 15.42 |
| LDFeb | 94.60 ± 15.09 | 97.33 ± 16.71‡ | 97.85 ± 15.58§ | 97.40 ± 15.87 |
IQR = interquartile range; AST = aspartate aminotransferase; ALT = alanine aminotransferase; eGFR = estimated glomerular filtration rate.
P < 0.01 for low‐dose benzbromarone (LDBen) compared to low‐dose febuxostat (LDFeb).
P < 0.01 for baseline values compared to weeks 4, 8, and 12 in the LDBen group or LDFeb group.
P < 0.05 for baseline values compared to weeks 4, 8, and 12 in the LDBen group or LDFeb group.
P < 0.05 for LDBen compared to LDFeb.
Safety
Over the 12‐week study period, the incidence rates of AEs were similar between the 2 groups (60% in the LDBen group and 65% in the LDFeb group). There were no serious AEs (Table 3). There were no skin reactions, gastrointestinal AEs, fulminant hepatitis, or major adverse cardiac events in either group (data not shown). No between‐group differences were observed in terms of the proportion of participants with gout flare (LDBen 30% versus LDFeb 36%, P = 0.36) (Table 3).
Table 3.
Frequency of adverse events in patients with renal underexcretion–type gout during the trial of LDBen and LDFeb*
| LDBen (n = 98) | LDFeb (n = 98) | P | |
|---|---|---|---|
| Urolithiasis | 5 (5) | 2 (2) | 0.25 |
| Gout flare | 30 (31) | 36 (37) | 0.36 |
| Once | 18 (18) | 16 (16) | 0.71 |
| Twice | 9 (9) | 14 (14) | 0.27 |
| More than twice | 3 (3) | 6 (6) | 0.50 |
| New‐onset AST level elevation† | 1 (1) | 9 (9) | 0.009‡ |
| 1–2‐times elevation | 1 (1) | 8 (8) | 0.035‡ |
| 2–3‐times elevation | 0 (0) | 1 (1) | 1.00 |
| New‐onset ALT level elevation† | 4 (4) | 10 (10) | 0.10 |
| 1–2‐times elevation | 3 (3) | 8 (8) | 0.12 |
| 2–3‐times elevation | 1 (1) | 2 (2) | 1.00 |
| eGFR <60 ml/minute/1.73 m2 | 0 (0) | 0 (0) | 1.00 |
| Other level of eGFR | 0 (0) | 0 (0) | 1.00 |
Values are the number (%) of patients. LDBen = low‐dose benzbromarone; LDFeb = low‐dose febuxostat; AST = aspartate aminotransferase; ALT = alanine aminotransferase; eGFR = estimated glomerular filtration rate.
New‐onset elevation indicates an elevation above the upper limit of normal from baseline to week 12.
P value was statistically significant.
Liver and kidney function were monitored throughout the trial. An increase from baseline AST level was observed at each follow‐up visit in patients in the LDFeb group (P < 0.001). In contrast, AST levels in the LDBen group did not increase over time and were lower than the LDFeb group at weeks 4 and 12 (P < 0.01 at both time points). The percentage of participants with AST elevation was significantly lower in the LDBen group than in the LDFeb group (1% versus 9%, P = 0.02) (Table 3). Furthermore, fewer participants in the LDBen group had a 1–2‐times elevation from baseline in their AST level compared to participants in the LDFeb group (1% versus 8%, P = 0.03). The ALT level decreased in the LDBen group but increased in the LDFeb group at weeks 4 and 8, and at week 12, the ALT level remained lower in the LDBen group compared to the LDFeb group (P = 0.03). Overall, the percentage of participants with transaminase elevation above the ULN was lower in the LDBen group than in the LDFeb group (4% versus 15%, P = 0.008) (Table 3).
There were no significant differences between the 2 groups in terms of serum creatinine levels and eGFR during the treatment period (Table 2). No participant in either group developed an eGFR of <60 ml/minute/1.73 m2. Urolithiasis was observed in 5 participants in the LDBen group and 2 participants in the LDFeb group (5% versus 2%, P = 0.25) (Table 3).
DISCUSSION
The findings from this randomized clinical trial provide important new insights into gout management. Specifically, despite advanced understanding of the pathophysiologic basis of hyperuricemia and gout, prescribing ULT according to the hyperuricemia classification type is not generally recommended and is rarely done in Western clinical practice (12, 13, 19). Earlier findings from observational studies suggested that benzbromarone may be more effective than allopurinol in the reduction of serum urate levels in hyperuricemia caused by renal uric acid underexcretion (22). This Chinese gout study population–based trial was unique, not only by comparing the efficiency and safety of benzbromarone and febuxostat in randomized clinical trial participants with renal underexcretion–type gout, but also by comparing low‐dose regimens. LDBen (25 mg/day) had greater urate‐lowering efficacy and an excellent safety profile compared to LDFeb (20 mg/day) over 12 weeks of therapy. Low‐dose benzbromarone had significantly greater serum urate–lowering treatment success than LDFeb in patients with renal underexcretion–type gout.
Importantly, the trial was designed to test a hypothesis by comparing uricosuric ULT to XOI ULT in patients with gout with a single predominant cause of hyperuricemia. This design promoted the enrollment of a relatively healthy population of younger participants with disease onset particularly common in the 30–40‐year‐old age group. It is well recognized that the capacity to renally excrete uric acid is partly modulated by the functional capacity for glomerular filtration of urate. In this context, stage 3 chronic kidney disease, which is very prevalent in gout patients (23, 24), was an exclusion criterion in this study. In addition, this Chinese gout study population had substantially lower prevalence of hypertension, dyslipidemia, and CVD than typical Western gout clinical trial populations (25). Furthermore, all participants received 1 gm/3 times daily oral sodium bicarbonate for the purpose of alkalinizing the urine, which likely limited urolithiasis (16) and may have enhanced urate‐lowering efficacy (26).
Moreover, use of ULTs differed from that in Western clinical trials and typical Western medical practice patterns and recommendations for gout, where allopurinol is the recommended first‐line ULT (12, 13, 27). In this context, US Food and Drug Administration–approved dosing of febuxostat is 40 mg/day and 80 mg/day, and benzbromarone is not approved in the US and is only recommended as a second‐line ULT drug in Europe due to potentially lethal hepatotoxicity reactions not believed to be due to modulation of URAT1 activity (12). Furthermore, in countries where benzbromarone is approved, the starting dosages of benzbromarone range from 12.5 mg to 50 mg daily (28, 29, 30, 31). Hence, as emerging URAT1 inhibitor uricosuric therapies are developed as potential monotherapies in clinical trials among Western patient populations (27), careful consideration will likely be needed in clinical trial patient selection for the pathophysiologic type of hyperuricemia, comorbidities, and use of urine alkalization with agents such as potassium citrate (16).
The comparison of results in distinctly designed clinical trials is clearly imperfect. However, in the current low‐dose ULT trial in this selective cohort of renal uric acid underexcretion–type gout, the percentage of participants achieving the serum urate target of <6.0 mg/dl was 61% in the LDBen group, which was approximately double that observed in the LDFeb group. In contrast, Naoyuki et al (28) found that the percentage of patients who achieved the serum urate target (<6.0 mg/dl) was 45.7% in the 20 mg/day febuxostat treatment group. Liang et al (15) indicated that, similar to our results, the frequency of achieving the serum urate target was 39.5% among 105 gout patients who were not selected for primary uric acid underexcretion and who received febuxostat 20 mg/day, whereas the frequency of achieving the serum urate target was only 35.7% among 109 patients receiving benzbromarone 25 mg/day.
In this study, the urate‐lowering effect of benzbromarone appeared to be steadier than febuxostat over the trial period. Importantly, febuxostat does lead to a sustained reduction at the final time point compared to baseline values. While we did not observe differences in terms of medication adherence using pill counts between groups, it is possible that these differences might be attributed to the following: differences in adherence behavior; differences in the mechanisms of the ULT; a decline in fractional excretion of urate as serum urate levels were reduced by treatment with febuxostat (32); or differences due to chance. There were no differences in reported medication adherence between the LDBen group and LDFeb group. Some variation in urate levels over time is often observed in ULT trials (15, 33).
Not surprisingly, lack of clinical trial evidence to date has been accompanied by lack of consensus regarding use of assays for renal uric acid underexcretion in clinical practice for promoting precision in gout management. For example, the 2006 EULAR gout management guidelines recommended that renal uric acid excretion should be determined in selected gout patients, especially those with a family history of early‐onset gout, those with gout onset at age <25 years, or those with renal calculi (strength of recommendation 72 [95% confidence interval 62–81]) (18). The 2012 ACR Guidelines for the Management of Gout recommended that clinicians consider causes of hyperuricemia in gout patients (evidence grade C) (34). However, the most recent update of the ACR guidelines for management of gout conditionally recommended against using urinary uric acid levels to determine the precision of therapy choice and strategy in ULT (34, 35).
We did not observe severe hepatotoxicity associated with LDBen, but ethnic background may affect drug responses, and severe hepatotoxicity with benzbromarone has rarely been reported in Asia (11). Notably, elevated transaminases and the rare occurrence of severe liver injury have been reported in patients receiving febuxostat (14, 36). In our study, the proportion of participants with liver damage in the LDFeb group was higher than that in the LDBen group, most clearly demonstrated by the increase in AST level. No significant change in triglyceride levels was reported in this study, though a previous study suggested that febuxostat could cause elevated triglycerides (15). In this study, the incidence of urolithiasis in the LDBen group (5%) was numerically but not significantly higher than that in the LDFeb group (2%). Incidence rates of urolithiasis of ~3% have been reported with benzbromarone 75–120 mg/day (37, 38), including in a trial in China using benzbromarone 25 mg/day (16), similar to our results.
Several other study limitations should be noted, such as the single center, open‐label design and relatively short treatment period, which did not allow for the assessment of long‐term safety. We only included patients who were relatively young, had few comorbidities, and had a baseline serum urate level ranging from 8.0 mg/dl to 10 mg/dl; therefore, study results may not be generalizable to patients with higher serum urate levels or impaired kidney function, and may also not be generalizable to patients from other geographic regions, age groups, and ethnic groups. Only men were recruited in this study, and the findings may not be generalizable to women with gout. Furthermore, the scope to more widely implement this treatment strategy is currently limited because the availability of benzbromarone and other uricosurics varies across the globe and in many countries is very limited. The efficacy of benzbromarone and febuxostat in gout patients with normal renal uric acid excretion was not compared in this study. Last, the serum urate–lowering efficacy of both benzbromarone and febuxostat was not maximal at doses of the ULT used here.
In conclusion, this study demonstrates that LDBen has greater serum urate–lowering efficacy than LDFeb in relatively young and healthy patients with renal underexcretion–type gout. Further investigation is warranted to test precision in the model for use of an URAT1 inhibitor in selecting first‐line ULT according to primary renal uric acid underexcretion, as opposed to decreased renal function. However, the results suggest that LDBen may warrant stronger consideration as a safe and effective therapy to achieve serum urate target in gout patients without moderate chronic kidney disease.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Drs. C. Li and Terkeltaub had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
C. Li.
Acquisition of data
Yan, Xue, Lu, Qi, Yu, Wang, Sun, Cui, Liu, He, Yuan, Chen, Cheng, Ma, H. Li, Ji, Hu, Ran.
Analysis and interpretation of data
Yan, Xue, Lu, Dalbeth, Terkeltaub.
Supporting information
Disclosure Form
Supplementary Table1 Drugs affecting serum urate.
Supported by the National Key Research and Development Program (award 2022YFE0107600), Shandong Provincial Key Research and Development Plan Major Scientific and Technological Innovation Project (award 2021CXGC011103), the National Natural Science Foundation of China (awards 31900413, 81770869, and 81900636), and Shandong Provincial Science Foundation for Outstanding Youth Scholars (award ZR2021YQ56). Dr. Terkeltaub's work was supported by the NIH (grants AR‐060772 and AR‐075990) and the VA Research Service.
Drs. Yan, Xue, and Lu contributed equally to this work.
Author disclosures are available at https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1002%2Fart.42266&file=art42266‐sup‐0001‐Disclosureform.pdf.
Contributor Information
Robert Terkeltaub, Email: rterkeltaub@ucsd.edu.
Changgui Li, Email: lichanggui@medmail.com.cn.
REFERENCES
- 1. Dalbeth N, Gosling AL, Gaffo A, et al. Gout. Lancet 2021;397:1843–55. [DOI] [PubMed] [Google Scholar]
- 2. Dalbeth N, Merriman TR, Stamp LK. Gout. Lancet 2016;388:2039–52. [DOI] [PubMed] [Google Scholar]
- 3. Perez‐Ruiz F. Treating to target: a strategy to cure gout. Rheumatology (Oxford) 2009;48 Suppl:ii9–14. [DOI] [PubMed] [Google Scholar]
- 4. Liu X, Zhai T, Ma R, et al. Effects of uric acid‐lowering therapy on the progression of chronic kidney disease: a systematic review and meta‐analysis. Ren Fail 2018;40:289–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shoji A, Yamanaka H, Kamatani N. A retrospective study of the relationship between serum urate level and recurrent attacks of gouty arthritis: evidence for reduction of recurrent gouty arthritis with antihyperuricemic therapy. Arthritis Rheum 2004;51:321–5. [DOI] [PubMed] [Google Scholar]
- 6. Mandal AK, Mount DB. The molecular physiology of uric acid homeostasis. Annu Rev Physiol 2015;77:323–45. [DOI] [PubMed] [Google Scholar]
- 7. Vitart V, Rudan I, Hayward C, et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet 2008;40:437–42. [DOI] [PubMed] [Google Scholar]
- 8. Dalbeth N, Merriman T. Crystal ball gazing: new therapeutic targets for hyperuricaemia and gout. Rheumatology (Oxford) 2009;48:222–6. [DOI] [PubMed] [Google Scholar]
- 9. Ichida K, Matsuo H, Takada T, et al. Decreased extra‐renal urate excretion is a common cause of hyperuricemia. Nat Commun 2012;3:764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Woodward OM, Kottgen A, Coresh J, et al. Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc Natl Acad Sci U S A 2009;106:10338–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Azevedo VF, Kos IA, Vargas‐Santos AB, et al. Benzbromarone in the treatment of gout. Adv Rheumatol 2019;59:37. [DOI] [PubMed] [Google Scholar]
- 12. FitzGerald JD, Dalbeth N, Mikuls T, et al. 2020 American College of Rheumatology guideline for the management of gout. Arthritis Rheumatol 2020;72:879–95. [DOI] [PubMed] [Google Scholar]
- 13. Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence‐based recommendations for the management of gout. Ann Rheum Dis 2017;76:29–42. [DOI] [PubMed] [Google Scholar]
- 14. Frampton JE. Febuxostat: a review of its use in the treatment of hyperuricaemia in patients with gout. Drugs 2015;75:427–38. [DOI] [PubMed] [Google Scholar]
- 15. Liang N, Sun M, Sun R, et al. Baseline urate level and renal function predict outcomes of urate‐lowering therapy using low doses of febuxostat and benzbromarone: a prospective, randomized controlled study in a Chinese primary gout cohort. Arthritis Res Ther 2019;21:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xue X, Liu Z, Li X, et al. The efficacy and safety of citrate mixture vs sodium bicarbonate on urine alkalization in Chinese primary gout patients with benzbromarone: a prospective, randomized controlled study. Rheumatology (Oxford) 2021;60:2661–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yamanaka H, Tamaki S, Ide Y, et al. Stepwise dose increase of febuxostat is comparable with colchicine prophylaxis for the prevention of gout flares during the initial phase of urate‐lowering therapy: results from FORTUNE‐1, a prospective, multicentre randomised study. Ann Rheum Dis 2018;77:270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang W, Doherty M, Pascual E, et al. EULAR evidence based recommendations for gout. Part I: Diagnosis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2006;65:1301–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Neogi T, Jansen TL, Dalbeth N, et al. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheumatol 2015;67:2557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhou BF, Cooperative Meta‐Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut‐off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002;15:83–96. [PubMed] [Google Scholar]
- 21. WHO Expert Consultation . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies [review]. Lancet 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- 22. Perez‐Ruiz F, Alonso‐Ruiz A, Calabozo M, et al. Efficacy of allopurinol and benzbromarone for the control of hyperuricaemia. A pathogenic approach to the treatment of primary chronic gout. Ann Rheum Dis 1998;57:545–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roughley MJ, Belcher J, Mallen CD, et al. Gout and risk of chronic kidney disease and nephrolithiasis: meta‐analysis of observational studies. Arthritis Res Ther 2015;17:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roughley M, Sultan AA, Clarson L, et al. Risk of chronic kidney disease in patients with gout and the impact of urate lowering therapy: a population‐based cohort study. Arthritis Res Ther 2018;20:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mackenzie IS, Ford I, Nuki G, et al. Long‐term cardiovascular safety of febuxostat compared with allopurinol in patients with gout (FAST): a multicentre, prospective, randomised, open‐label, non‐inferiority trial. Lancet 2020;396:1745–57. [DOI] [PubMed] [Google Scholar]
- 26. Wiederkehr MR, Moe OW. Uric acid nephrolithiasis: a systemic metabolic disorder. Clin Rev Bone Miner Metab 2011;9:207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Benn CL, Dua P, Gurrell R, et al. Physiology of hyperuricemia and urate‐lowering treatments. Front Med (Lausanne) 2018;5:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kamatani N, Fujimori S, Hada T, et al. An allopurinol‐controlled, multicenter, randomized, open‐label, parallel between‐group, comparative study of febuxostat (TMX‐67), a non‐purine‐selective inhibitor of xanthine oxidase, in patients with hyperuricemia including those with gout in Japan: phase 2 exploratory clinical study. J Clin Rheumatol 2011;17:S44–9. [DOI] [PubMed] [Google Scholar]
- 29. Multidisciplinary Expert Task Force on Hyperuricemia and Related Diseases. Chinese multidisciplinary expert consensus on the diagnosis and treatment of hyperuricemia and related diseases. Chin Med J (Engl) 2017;130:2473–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yamanaka H, Japanese Society of Gout and Nucleic Acid Metabolism. Japanese guideline for the management of hyperuricemia and gout: second edition. Nucleosides Nucleotides Nucleic Acids 2011;30:1018–29. [DOI] [PubMed] [Google Scholar]
- 31. Yu KH, Chen DY, Chen JH, et al. Management of gout and hyperuricemia: multidisciplinary consensus in Taiwan. Int J Rheum Dis 2018;21:772–87. [DOI] [PubMed] [Google Scholar]
- 32. Liu S, Perez‐Ruiz F, Miner JN. Patients with gout differ from healthy subjects in renal response to changes in serum uric acid. Joint Bone Spine 2017;84:183–8. [DOI] [PubMed] [Google Scholar]
- 33. Lin Y, Chen X, Ding H, et al. Efficacy and safety of a selective URAT1 inhibitor SHR4640 in Chinese subjects with hyperuricaemia: a randomized controlled phase II study. Rheumatology (Oxford) 2021;60:5089–97. [DOI] [PubMed] [Google Scholar]
- 34. Khanna D, Fitzgerald JD, Khanna PP, et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 2012;64:1431–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jansen TL. Rational pharmacotherapy (RPT) in goutology: define the serum uric acid target & treat‐to‐target patient cohort and review on urate lowering therapy (ULT) applying synthetic drugs. Joint Bone Spine 2015;82:225–9. [DOI] [PubMed] [Google Scholar]
- 36. Bohm M, Vuppalanchi R, Chalasani N, et al. Febuxostat‐induced acute liver injury. Hepatology 2016;63:1047–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Masbernard A, Giudicelli CP. Ten years' experience with benzbromarone in the management of gout and hyperuricaemia. S Afr Med J 1981;59:701–6. [PubMed] [Google Scholar]
- 38. Stamp LK, Haslett J, Frampton C, et al. The safety and efficacy of benzbromarone in gout in Aotearoa New Zealand. Intern Med J 2016;46:1075–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure Form
Supplementary Table1 Drugs affecting serum urate.


