Abstract
The public health crisis of chronic pain has only increased in recognition since the Institute of Medicine’s (IOM) Relieving Pain in America (2011) called for a cultural transformation in the way pain is viewed and treated and put forward specific recommendations for action. The National Pain Strategy (NPS) provides a roadmap for putting these recommendations into practice. We implemented a program that placed nurses and behavioral specialists at the head of an interdisciplinary team utilizing best practices. In this program, nurses enacted the NPS recommendations to advance care for patients with persistent pain on long-term opioid treatment. This program promoted professional growth in nurses along with fostering success for patients. Compared to patients receiving usual care, patients in the program achieved greater reductions in pain severity, pain-related disability, and pain-related functional interference and reported greater satisfaction with pain-related care and primary care services. This article will detail the NPS-aligned practice approaches these nurses and their teams used, describe the training for the nurses, and speak to opportunities to enhance the nurse’s capacity for this role in hopes of providing a model for the future implementation of an NPS-based approach by nurses.
Keywords: chronic pain, nursing, interdisciplinary health team, primary healthcare
Introduction
In 2011, the Institute of Medicine (IOM) published Relieving Pain in America, a call to action specifying the need for a cultural transformation in the way pain is viewed and treated (IOM, 2011, p. 44). This report outlined our moral imperative to view persistent pain as a disease in and of itself, to utilize known best practices such as comprehensive, interdisciplinary approaches, and for clinicians to expand their familiarity with and use of existing knowledge. In 2016, the Interagency Pain Research Coordinating Committee (IPRCC), established under the US Department of Health and Human Services, published the National Pain Strategy (NPS) (IPRCC, 2016). The NPS set forth a vision to advance all recommendations made by the IOM report, outlining a roadmap for achieving pain care that is biopsychosocial, grounded in scientific evidence, integrated into the healthcare system, and interdisciplinary, while personalized to each individual patient’s needs (IPRCC, 2016, p.5). The NPS sets forth specific goals, providing clear steps for improved pain care. These recommendations include administering a comprehensive, interdisciplinary assessment leading to a patient-centered plan of care, training clinicians on biopsychosocial contributors to and management of pain, implementing team-based selfmanagement programs for patients, and integrating interdisciplinary, evidence-based care into the health care system.
In recognizing that shifting the paradigm of pain care relies on research to identify care innovations, the IPRCC put forward the Federal Pain Research Strategy (FPRS). Among the FPRS’ top priorities was developing, evaluating, and improving models of pain care (Gatchel et al., 2018). Specifically highlighted in this research priority was establishing models of integrated care with team-based delivery.
The Pain Program for Active Coping and Training (PPACT), an interdisciplinary biopsychosocial program implemented in three regions of Kaiser Permanente —Northwest, Hawaii, and Georgia as part of a pragmatic clinical trial (DeBar et al., 2018)—provides an exemplar for operationalizing the recommendations set forth by the NPS and a key research priority of the FPRS. The program, targeting individuals with persistent pain on long-term opioid therapy and embedded in the primary care environment, brought together a team of nurses, behavioral specialists, physical therapists, pharmacists, and primary care providers (PCPs) to help patients actively integrate pain self-management skills into their daily lives. The program used a comprehensive assessment to inform a patient-centered plan of coordinated care. An interdisciplinary team worked with the patient and his/her PCP over a course of four months to enact the plan of care through partnership with the patient. As leads of the interdisciplinary team, nurses and behavioral specialists underwent a multi-faceted training to ensure proficiency in the practices and skills taught in the program.
Investigations regarding interdisciplinary care for persistent pain management recognize the importance of the nurse’s role on the team (Broderick et al., 2014). Williams (2017) outlined the importance of the nurse in actualizing the NPS, exploring the nurse’s potential role in identifying and implementing its recommendations and goals. PPACT demonstrated how nurses, serving on an interdisciplinary team, provided care in line with the NPS recommendations to enhance care for patients with persistent pain. This article will detail the practice approaches the nurses and interdisciplinary teams used, describe the training for the nurses, and speak to opportunities to enhance the nurse’s capacity for this role. We hope to provide a model for future implementation of an NPS-based approach by nurses.
Methods
PPACT combined evidence-based approaches from the Chronic Care Model (Wagner et al., 2001), collaborative care approach (Dobscha et al., 2009), multidisciplinary approach to pain care (Loeser, 2005), coping skills training for pain (Keefe & Somers, 2010 and Keefe et al., 2004), and chronic pain treatment guidelines (American Society of Anesthesiologists & American Society of Regional Anesthesia and Pain Medicine, 2010 and Chou et al., 2009). Recognizing that care of individuals with persistent pain is frequently fragmented, leading to poor outcomes (Roth et al., 2012), PPACT sought to use an interdisciplinary, collaborative approach to holistically address the needs of patients. PPACT chose to embed this interdisciplinary team within the primary care environment, given that more than half of all patients with persistent pain rely on PCPs for their pain care (Breuer et al., 2010). The interdisciplinary teams, led by nurses and/or behavioral specialists, and including physical therapists and pharmacists, worked closely with patients’ PCPs to help patients integrate pain coping skills into their daily lives and decrease reliance on opioid medication. Please see Table 1 for an outline of each interdisciplinary team member’s role and responsibility in PPACT.
Table 1.
Interdisciplinary team roles
| Interdisciplinary Team Member | Role within PPACT |
|---|---|
| Nurse |
|
| Behavioral Specialist |
|
| Physical Therapist |
|
| Pharmacist |
|
A total of 851 patients participated in the PPACT program for 16-18 weeks (DeBar et al., 2022). Eligibility criteria included 1) age ≥18 years, 2) current Kaiser Permanente (KP) health plan member with ≥180 days of membership, 3) ≥ two dispensing’s of long-acting opioids in the prior 6 months or a cumulative 90-day (or greater) supply of short-acting opioids during any 4-month period within the prior 6 months, and 4) any type of pain diagnosis within the previous year. Exclusion criteria included 1) two or more cancer diagnoses associated with an oncology-related encounter in the prior 60 days, 2) hospice or other end-of-life palliative care within the past year, 3) current enrollment in addiction medicine services or active substance dependence diagnosis, and 4) cognitive impairment severe enough to preclude participation in a behavioral/lifestyle change program. The 851 participating patients had an average age of 60.3 (standard deviation 12.2).
Female participants made up 67.4% of the sample with a racial distribution of 76.6% white participants, 13% black or African American participants, 3% Asian participants, 2.7% identifying as Hawaiian or Pacific Islander, 2% identifying as American Indian or Alaskan Native, 2.7% identifying as mixed race, other race, or unknown and 3.3% participants of Hispanic ethnicity. During the first month of the program, the PPACT interdisciplinary team conducted a biopsychosocial assessment of each patient’s situation. The nurse or behavioral specialist conducted a semi-structured interview, patients completed a series of questionnaires, and the pharmacist conducted a chart-based medication review. The physical therapist conducted a functional assessment and devised a plan focused on physical function. The nurse or behavioral specialist then compiled all interdisciplinary assessments and worked with patients to devise an overarching, evidence-based plan of care in line with the patient’s unique needs. The nurse and behavioral specialists discussed this plan with each patient’s PCP to promote collaboration in putting the plan into action and helping the patient achieve their goals.
For the next twelve weeks of the program, patients engaged in weekly supported self-care management group sessions where nurses and/or behavioral specialists led patients in practicing evidence-based pain coping skills and adapted movement practice. During those twelve weeks, patients had the opportunity to work with the PPACT nurses and/or behavioral specialists during weekly coaching calls to discuss progress, home-practice activities, and to problem-solve barriers to practicing skills and adapted movement. At the program’s midpoint, patients met again with a PPACT physical therapist to receive reinforcement for progress and additional recommendations on progressing towards their physical function goals. Following the coping skill training (individual and group work), the nurse or behavioral specialist met individually with patients who completed the program to discuss successes achieved and areas of continual work, and to devise a plan for the patient’s continued progress in using pain coping skills during their daily lives. When possible, the nurse and/or behavioral specialist met with the patient’s PCP to ensure a patient-centered plan for continued success following the PPACT program. A face to face meeting was not always possible; at minimum, the PPACT team communicated the plan electronically, offering to discuss it at the PCP’s convenience. See Figure 1 for a visual overview of the PPACT program. Patients provided consent for overall participation in the program, as part of the pragmatic clinical trial, along with consent to be audio recorded during the group sessions. The Institutional Review Boards (IRBs) at all three Kaiser Permanente sites—KP-Northwest, KP-Hawaii, and KP-Georgia—retained oversight and approved the trial procedures. Throughout the program, the nurses and behavioral specialists, as leads of the interdisciplinary team, utilized practices in line with NPS recommendations for evidence-based pain management approaches. Following, we specify the details of those approaches.
Figure 1.
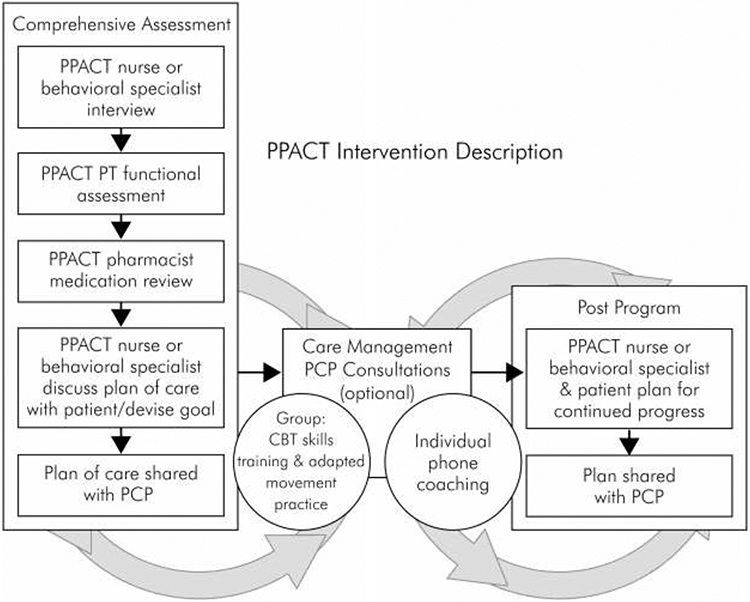
PPACT: Pain Program for Active Coping and Training, PT: Physical Therapy, PCP: Primary Care Provider, CBT: Cognitive Behavioral Therapy.
NPS-aligned Approaches Used in PPACT: Comprehensive Assessment with Biopsychosocial Care Plan
The NPS states, “treatment should begin with a comprehensive assessment, followed by creation of a care plan that can evolve over time to address the full range of biological, psychological, and social effects of pain on the individual” (IPRCC, 2016, p.4). In line with this approach, the PPACT program began with a comprehensive, interdisciplinary assessment of the patient’s biopsychosocial adjustment to pain. The nurse or behavioral specialist conducted thorough biopsychosocial assessments upon each patient’s entry into the program. The assessment began with a semi-structured interview to understand, from the patient’s perspective, the cause of their pain, the impact pain had on multiple facets of their life, and treatment strategies used, both successfully and unsuccessfully. The interview also elicited information on patient-recognized strengths, which provided a foundation for the nurse and behavioral specialist to draw upon throughout the program. Information from the interview was combined with data collected from validated questionnaires that assessed patients’ pain-related function (Brief Pain Inventory {Cleeland & Ryan, 1994}, Roland Morris Disability Questionnaire {Roland & Fairbank, 2000}, Modified Oswestry Low Back Pain Disability Questionnaire {Roland & Fairbank, 2000}), depression (Patient Health Questionnaire {PHQ}−8 {Kroenke et al., 2008}), anxiety (Generalized Anxiety Disorder {GAD}−7 {Spitzer et al., 2006}), alcohol use (alcohol use disorders identification {AUDIT-C} {Bush et al., 1998}), daytime sleepiness (Epworth Sleepiness Scale {Johns, 1991}), adverse childhood events (Adverse Childhood Experiences {ACE} Questionnaire {Felitti et al., 1998}), kinesiophobia (fear of movement, Tampa Scale for Kinesiophobia {Shelby et al., 2012}), use of pain coping strategies (Coping Strategies Questionnaire {Rosenstiel & Keefe, 1983}), and the patient’s self-efficacy in pain control (Chronic Pain Self-Efficacy Scale {Anderson et al., 1995}). We used this data to inform the patient-specific plan of care devised for each patient. For example, if a patient demonstrated use of active and productive coping strategies on the Coping Strategies Questionnaire or demonstrated strong self-efficacy on the Chronic Pain Self Efficacy Scale, this would be noted as areas of strength on the plan of care, encouraging patients to draw upon these assets during their work in PPACT. Alternatively, if a patient demonstrated significant pain-related interference with functioning as measured by the Roland Morris Disability Questionnaire or fear of movement interfering with moderate physical activity as assessed by the Tampa Scale for Kinesiophobia, these were documented as targets for improving function on the plan of care and, accordingly, a focus of the work between the patient and interdisciplinary team. Scores and interpretations where applicable (according to each tool’s author’s specification) were documented on the pre and post program plan of care, with the purpose of allowing patients and their providers to see changes over time. Any pre or post program scores indicating moderate or severe depression, anxiety, sleepiness, or alcohol use were reported to the patient’s PCP for further action or referral. As a whole, we used data from the interview and questionnaires to understand each patient’s situation, and to help align each patient’s plan with their current ability.
Building on this knowledge, a PPACT physical therapist met with each patient to assess factors affecting their physical function. The physical therapist worked with the patient to devise an individualized plan for graded physical activity, recommend movement adaptations, and suggest ways to increase the patient’s engagement in daily activities. In addition, a PPACT pharmacist completed an in-depth medication review with the goal of recommending options for maximizing non-opioid medications to the PCP (e.g. gabapentinoids, tricyclic antidepressants, serotonin and norepinephrine reuptake inhibitors, non-steroidal anti-inflammatories, topical agents).
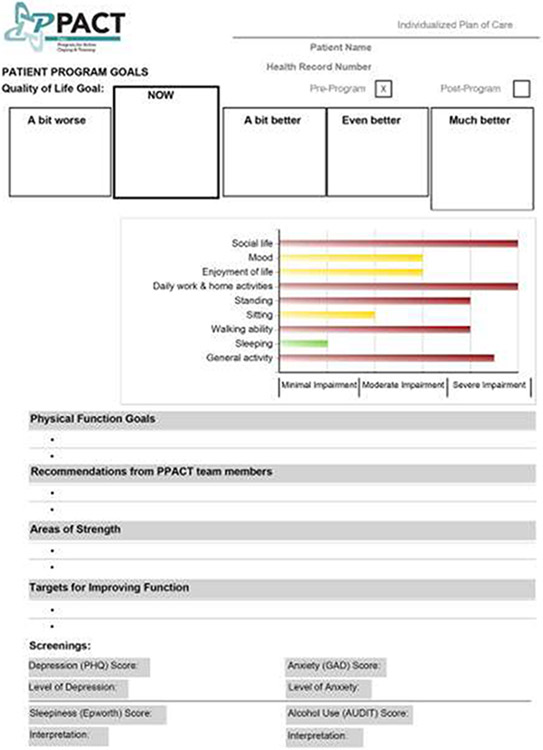
Following this interdisciplinary, multifaceted biopsychosocial assessment, the nurse compiled the data collected to formulate an individualized, patient-centered plan to guide the work of the nurse, behavioral specialist, physical therapist, and patient throughout the program. Please see Figure 2 for a template of the PPACT plan of care. Nurses met with the patients to ensure that this plan of care accurately reflected their situation and worked with the patient to devise a goal by which to monitor progress. While nurses are well trained and experienced in patient assessment, this structured, multifaceted approach provided a more standardized, thorough, and comprehensive understanding of the patient’s biopsychosocial situation as compared to a standard nursing assessment. The team recognized the necessity of standardizing this comprehensive assessment to adequately address the complex needs of these patients.
Figure 2.
PPACT: Pain Program for Active Coping and Training, PHQ: Patient Health Questionnaire, GAD: Generalized Anxiety Disorder, AUDIT: Alcohol Use Disorders Identification Test.
Goal Setting
The NPS identifies goal setting as an important component of pain self-management programs. The PPACT program used Goal Attainment Scaling (GAS) to guide patients in the development of personally valued goals that can be used to assess clinically meaningful improvements during the program. GAS is a validated approach to elicit goals that are most important to patients, assess improvement on domains most relevant to patients during multidisciplinary pain programs, and demonstrate clinically meaningful change (Fischer, 2008; Mullis & Hay, 2010). While meeting with patients to discuss the patient’s plan of care moving forward in the program, nurses utilized a semi-structured interview (Mullis & Hay, 2010) to guide the patient through GAS. See Figure 2 for a visual representation of the PPACT GAS, embedded in the PPACT Plan of Care. The nurse began by working with the patient to identify a pain-related problem of importance: one that limited day-to-day life, interfered with valued activities, or prevented the patient from engaging with family or friends. Next the nurse worked with the patient to formulate a goal related to an activity impaired by the specified pain-related problem. Through a series of questions and guided discussion, the nurse helped the patient to scale progress on achieving his/her goal by identifying states of goal achievement if the patient was a bit better, even better, much better, or a bit worse. This denotes an important aspect of GAS, as it lays out a framework for stepwise progress, allows patients to start where they are, and encourages patients to strive for realistic goals, within their reach, while moving towards a larger goal for success.
Throughout the program, the nurse and behavioral specialist worked with the patient to assess their progress on their goal. The stepwise scaling of the patient’s goal allowed the patient to recognize small markers of success, while allowing the nurse to objectively evaluate patients’ functional progress on activities of value to the patient. This goal also provided both context and motivation for the patient’s work on coping skill development. Patients sometimes used a particular coping skill to advance progress on achieving the next step of their goal or looked towards goal achievement as motivation for continuing coping skill engagement. For instance, a patient with an end goal of dancing at their daughter’s wedding might use activity-rest cycling to build endurance on their feet, one sequential step of their GAS. In addition, that same patient might look to the final, end goal as motivation to remain engaged in daily practice of coping skills, recognizing the necessity of these skills in fulfilling their future vision. GAS, through its overarching goal and stepwise sequence of progress toward that goal, gave patients the incentive to remain committed to their practice.
Developing Coping Skills
The NPS advocates for self-management programs that foster skill development and provide patients with the practice and confidence to manage their own pain (IPRCC, 2016, p.25). After their series of interdisciplinary assessments and after formulating their patient-centered plan of care, patients began participating in weekly group sessions and were offered regular, individual coaching calls, although not all patients made use of the calls. During these sessions and calls, nurses and behavioral specialists worked with patients to practice evidence-based pain-coping skills such as: progressive muscle relaxation and mini-practices (applied relaxation), activity-rest cycling, pleasant activity scheduling, pleasant imagery, emotional regulation skills, cognitive restructuring, challenging negative thoughts with use of calming self-statements, problem-solving, and relapse prevention and maintenance. Please see Table 2 for a brief description of these pain coping skills.
Table 2.
Pain-coping skills
| Coping Skill | Description of Coping Skill |
|---|---|
| Activity-rest cycling | Identification of activities that predispose a patient to overactivity, development of a plan to break that activity into periods of rest and activity, with a targeted plan for increasing activity and decreasing rest over time. |
| Progressive muscle relaxation | Tensing and relaxing muscle groups from head to toe with the purpose of enhancing patients’ ability to identify and release tension. |
| Mini-practice (applied relaxation) | 30-second brief relaxation where patients focus on sensations of relaxation throughout the body with the purpose of applying this practice throughout the day. |
| Pleasant activity scheduling | Group-brainstorm of pleasant activities, individual identification of activities that enhance engagement with valued activities, with creation of weekly activity goals. |
| Pleasant imagery | Visualization of a pleasant image/experience where patients use their five senses to immerse themselves in imagining the pleasant scene. |
| Emotional regulation | Exploration of patients’ experience of resistance (to their situation) and willingness (to stay present with their experience) with guidance for distress tolerance. |
| Cognitive restructuring | Guided example of cognitive restructuring to help patients recognize connections between their behaviors, thoughts, and feelings. |
| Challenging negative thoughts with use of calming selfstatements | Identification of maladaptive thoughts, formulation of more productive coping thoughts, and planned practice for using calming self-statements. |
| Problem solving | Stepwise problem-solving plan to break down a problem and understand its impact, brainstorm solutions, and implement solutions while using skills taught in program. |
| Relapse prevention | Identification of signs indicating a setback in skill use, planned strategy for using coping skills in midst of setback, and plan for continued use of coping skills. |
The PPACT program used an experiential approach to skill development to enhance patients’ self-efficacy. To ensure maximal opportunity for the patient to experience and practice the coping skill, the nurse or behavioral specialist provided a brief rationale for use of the skill, then worked to immediately engage the patient in skills practice. For example, the nurse began training in the group setting by grounding the rationale for the coping skill in the mechanisms by which a patient’s cognition impacts pain signals. The nurse used patient-friendly language to help patients understand how cognitive-behavioral coping skills could influence a biopsychosocial phenomenon such as persistent pain. Laying this foundation enhanced patients’ recognition of the skill as an effective and legitimate strategy. The nurse then led patients in an experience of pleasant imagery using a script that engaged the patients’ five senses. Immediately following that, the nurse guided patients in a reflection on their experience. During this discussion, the nurse guided patients to recognize how their own experience and cognitions aligned with the biopsychosocial mechanisms discussed during the opening rationale. Through this practice, patients were able to reflect on the ways in which this coping skill impacted their experience of pain. The experience and space for reflection allowed patients to gain confidence in the efficacy of using this coping skill in their daily lives.
To further ensure patients’ success in embedding coping skills into their daily lives, the nurse and/or behavioral specialist worked with each patient to devise weekly home practice goals. These goals specified intentions for frequency of coping skill use, targeted times when use of coping skills would be most beneficial for the patient, and, when needed, details of practice to increase the likelihood of patient success. Each week, between group sessions, the nurse or behavioral specialist would attempt to contact patients by phone to discuss progress on coping skill goals and provide guidance when barriers to practice arose. The nurse or behavioral specialist’s engagement with the patient during the group session practice and goal planning frequently alerted them to potential challenges that might arise for the patient. This experience, along with the team member’s thorough knowledge of each patients’ situation, gained through the comprehensive biopsychosocial assessment, allowed them to motivate patients and help them navigate specific barriers. This background of work with the patient gave the nurse and behavioral specialist a strong foundation from which to guide the patient during the weekly coaching calls.
Training Nurses in Cognitive Behavioral Work with Patients
Both the IOM report (IOM, 2011) and the NPS (IPRCC, 2016) highlight clinician education as a central component of the cultural transformation of pain treatment. The authors of the NPS caution that, without adequate education, practitioners often rely too heavily on procedural or pharmacological approaches, which alone are ineffective (IPRCC, 2016). While nurses are typically well versed in procedural, pharmacological, and non-pharmacological approaches, their training and proficiency in cognitive behavioral therapy (CBT) for pain is often limited. A recent symposium of national experts, held at an American Pain Society (APS) scientific meeting, confirmed psychotherapies for pain management (cognitive behavioral therapy, pain coping skills training, and relaxation training) as one of the most evidence-supported and effective therapies for reducing pain intensity and improving psychological and physical functioning (American Pain Society, 2016). The incoming president of APS reiterated the use of psychotherapies as an NPS recommendation.
The nurses’ and behavioral specialists’ group and individual work with patients in PPACT used a cognitive behavioral therapy (CBT) approach, with a focus on helping patients develop pain coping skills. To ensure adherence to evidence-based approaches, the nurses and behavioral specialists underwent comprehensive training from experts in CBT for pain and pain coping skills training (CST) (FJK, LLD) (Schrubbe et al., 2016). At the launch of the training, an expert in persistent pain management (FJK) discussed the state of the science for persistent pain management, providing evidence and a rationale for CBT and CST. Training included a 3-day in-person working session with instruction, role plays, and feedback; audio-recorded small group role plays with feedback; and consultation calls to strengthen nurse and behavioral specialists’ work with patients and bring a team approach to solving patient problems and achieving best care.
For each coping skill, nurses and behavioral specialists received instruction in how to engage patients in practice of the coping skill, then moved right into a role-play of engaging patients in practice with that skill. Each aspect of the training relied heavily on the nurses’ and behavioral specialists’ engagement in behavioral rehearsal to enhance their self-efficacy and proficiency in CBT and CST. While not regularly used to train nurses, behavioral rehearsal as a training tool has been shown to be an effective method for clinical skill development, allowing clinicians to experience and reflect through practice (Beidas et al., 2014). During the role-play, one nurse or behavioral specialist served as the clinician, guiding patients through the coping skill practice, while the other nurses and behavioral specialists served as the patients. The nurses and behavioral specialists then received feedback from colleagues and PPACT program supervisors regarding areas of successful patient engagement and opportunities to enhance the patients’ coping skill practice. The in-person training gave nurses and behavioral specialists experience and practice with each coping skill.
In the following weeks, nurses and behavioral specialists audio recorded role-plays of each of the 12 group sessions within the program. Program supervisors reviewed each of the role-plays, providing written feedback to assist the nurses and behavioral specialists in becoming fully proficient to deliver the program. The study team held consultation calls to discuss this feedback. Feedback can be an effective method for enhancing professional practice and improving patient outcomes, although studies show that effectiveness depends on how feedback is provided (Ivers et al., 2012). Feedback has been shown to be most effective when given both verbally and in writing, when it provides a clear target and action plan, and when it is provided more than once. Audiotapes of nurse and behavioral specialist-patient role plays were reviewed and rated by supervisors; once the nurses and behavioral specialists achieved proficiency, they were certified to begin working with patients. Ongoing recording of group sessions (with patient consent) allowed program supervisors to continue clinical supervision and assist the nurses and behavioral specialists in delivering care in a way that was faithful to the intervention protocol and in accordance with unique patient needs.
While nurses generally receive training in the management of acute pain and motivational interviewing for chronic conditions, and are familiar with CBT approaches, they receive less training in the therapeutic use of CBT for pain, particularly for patients with complex biopsychosocial disorders. The NPS and other nationally recognized reports clearly denote CBT as a critical best-practice for managing patients with persistent pain. Nurses have the physiologic and psychosocial foundation to co-lead this best practice movement with behavioral health specialists. To serve in this much needed role, nurses need enhanced training and experience with these approaches. We propose our training approach as one method to best prepare nurses for this role.
How Nurses Regarded the Training
As part of the qualitative evaluation of this trial, a subset of nurses was interviewed to gain their perception of the training received and work conducted during the PPACT program. In speaking to nurses about how this training helped them in their work with patients with persistent pain on long term opioids, one nurse compared the standard nursing approach to the training and experience she gained while working in PPACT:
Nurses are really taught to provide recommendations and to kind of be there to support patients, find out what they need, and then either kind of outsource them to other disciplines that they need, or then kind of tell them what it is they need to do.
In describing the PPACT approach, she noted:
Versus this model is more about self-activation of patients. And that’s the key component that I think nurses would benefit from training on, is understanding that difference and that this isn’t about you just sending [them] out with a really nice stack of paperwork telling people what to do. But making sure they can practice it, they can do it with you. That it’s something that comes from them.
Another nurse noted:
I am looking for small successes and focusing more attention on these areas and then exploring barriers with patients. I see changes in my questions that invite the patient to participate and take responsibility for their own care in ways that I wasn’t inviting prior to the PPACT training. This has resulted in creating more curiosity for both myself and my patients.
Discussion
PPACT utilized an approach in line with the NPS, drawing upon many strategies and practices inherent in nursing practice (biopsychosocial assessment, goal setting, focus on selfmanagement), while utilizing other practices that pushed the traditional style of nursing practice (work grounded in CBT, consistent use of experiential engagement, and training via behavioral rehearsal to fully support this shift in practice). As denoted in the nurses’ reflections, this shift in practice came with great reward and growth, but was not without challenges and lessons learned. Patient education in self-management lies at the heart of nursing, although many nurses were trained in a model that relies on information-giving, instruction-based handouts, or simply telling patients the necessary next steps. Working alongside patients to achieve the cognitive and behavioral changes necessary for optimal persistent pain management requires a more active and engaged approach with patients. The PPACT training focused on assisting nurses to utilize an interactive and experiential approach with patients, which necessitates responding and flexing based on patients’ experiences as they occur, as opposed to providing a pre-defined list of patient information and instructions. This approach of guided discovery and experiential engagement was often less familiar to nurses and necessitated consistent and supportive guidance to maintain this approach, particularly in instances of increased stress (such as when faced with a challenging patient or when running short on time), when nurses often reverted to the more comfortable and familiar approach of information-giving.
Through the training, consultation calls, and review of group sessions, we worked to embed new principles of practice into the nurses’ work with patients. We worked with nurses to cultivate a practice of curiosity when working with patients. Approaching patients’ successes and challenges with a sense of curiosity allows the patient to explore, for themselves, the underlying barriers and facilitators to their achievements. Embedding this curiosity in the patient helps them cultivate a practice of reflection and discovery that places them at the center of change and shifts the nurse from the problem solver to the coach. To facilitate this cultivated reflection and shift from the nurses doing the work to supporting the patients doing the work, we maintained a practice of drilling deep, not wide. As opposed to reviewing a long list of pain management strategies, we mindfully focused on a handful of key patient practices with evidence to support promoting patient-centered cognitive and behavioral change. This targeted focus allowed nurses to fully engage in experiential practice with the patient, explore patient-identified barriers and facilitators to practice, guide the patient to discover solutions for practice, and facilitate success experiences in the moment that enhance patient self-efficacy for practice at home. To further enable nurses to shift from problem solver or information giver to coach, nurses engaged patients in thought experiments that allowed them to imagine new patterns of behavior. In these experiments, nurses guided patients through an alternate reality where they had mastered a given coping skill. The nurse encouraged the patient to consider how their life might be different in this imagined future state. Drawing upon curiosity and experiential engagement once again, nurses stood alongside the patient as they explored tangible motivations for changing behavior. Throughout the training and implementation, we worked to provide nurses with an abundance of these CBT-based strategies and skills to assist in this shift towards a more experiential approach with patients.
Given this goal of encouraging a slight shift in the nurses’ approach, we recognized the need to monitor and address drift in utilizing the practices specified for PPACT. As a foundation to ensure consistent practice, we utilized an intervention manual that specified content, activities, tips for patient engagement, tips for handling potential challenges, exemplar scripting, and patient materials. In our review of nurses’ audio-recorded group sessions, we monitored specifically for alignment with the practice principles denoted previously and use of experiential patient engagement. At points were nurses drifted from utilizing these approaches, specific strategies for re-alignment with the principles were offered. Nurses were provided written documentation for strategies to use in similar, future situations and these points were discussed either individually with the nurse or as part of group consultation calls. Knowing that components of this style of practice were areas of learning for nurses, we recognized the importance of guided and supported coaching to facilitate growth in the nurses’ utilization of this approach.
This program not only promoted achievement in the nurses’ professional growth, but also success for patients. Patients engaged with PPACT, as compared to patients receiving usual care, achieved greater reductions in pain severity, pain-related disability, and pain-related interference with enjoyment of life, general activity, and sleep over one full year of follow up from baseline (DeBar et al., 2022). PPACT participants also reported greater satisfaction with their pain-related care and primary care services as compared to those receiving usual care (DeBar et al., 2022). There was no significant differences between groups in regard to opioid use (DeBar et al., 2022). Complete outcomes are reported elsewhere (DeBar et al., 2022).
Conclusion
The NPS offers clear guidance for achieving pain care based on strong scientific evidence, utilizes an interdisciplinary approach, and provides patients with the skills necessary for optimal self-management. We put forward a program, PPACT, that placed nurses and behavioral specialists at the head of an interdisciplinary team utilizing these evidence-based, best practice approaches for patients with complex persistent pain. Nurses received training to enhance their proficiency in implementing CBT and NPS-aligned approaches. This training and ongoing feedback helped nurses to utilize interactive and experiential engagement, drew upon a foundation of guided discovery, and trained the nurses utilizing the same principles used to train the patients, thereby actualizing the experiential approach for behavior change in the nurses. We hope the PPACT program and training approach might serve as a model, illustrating how nurses can advance the NPS’ vision of care for patients with persistent pain.
Funding:
The PPACT study was supported the National Institutes of Health (NIH) Common Fund, through a cooperative agreement (UH2AT007788, UH3NS088731) from the Office of Strategic Coordination within the Office of the NIH Director.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of conflict of interest: none
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Clinical Trials Registration Number: NCT02113592
References
- American Pain Society (2016). Evidence shows benefit of psychological care in pain management. Retrieved from: http://americanpainsociety.org/about-us/press-room/evidence-shows-benefits-of-psychological-care-in-pain-management. [Google Scholar]
- American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine (2010). Practice guidelines for chronic pain management: an updated report. Anesthesiology, 112(4), 810–833. [DOI] [PubMed] [Google Scholar]
- Anderson KO, Dowds BN, Pelletz RE, Edwards WT, & Peeters-Asdourian C (1995). Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain, 63(1):77–84 [DOI] [PubMed] [Google Scholar]
- Beidas RS, Cross W, & Dorsey S (2014). Show me, don’t tell me: Behavioral rehearsal as a training and analogue fidelity tool. Cognitive and Behavioral Practice, 21, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breuer B, Cruciani R, & Portenoy RK. (2010). Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: A national survey. South Med J, 103 (8), 738–747. [DOI] [PubMed] [Google Scholar]
- Broderick JE, Keefe FJ, Bruckenthal P, Junghaenel DU, Schneider S, Schwartz JE, Kaell AT, Caldwell DS, McKee D, Reed S, & Gould E (2014). Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: A randomized, controlled trial. Pain, 155 (9), 1743–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan D, McDonell M, Fihn S, & Bradley K (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Archives of Internal Medicine, 158(16), 1789–1795. [DOI] [PubMed] [Google Scholar]
- Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, & Mist SD (2010). A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain, 151 (2), 530–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson JW, Carson KM, Keefe FJ, & Seewaldt VL (2009). Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer, 17(10), 1301–1309. [DOI] [PubMed] [Google Scholar]
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM, & American Pain Society Low Back Pain Guideline Panel, (2009). Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976), 34(10), 1066–1077. [DOI] [PubMed] [Google Scholar]
- Chouinard M, Hudon C, Dubois M, Roberge P, Loignon C, Tchouaket E, Fortin M, Couture E-M, Sasseville M (2013). Case management and self-management support for frequent users with chronic disease in primary care: a pragmatic randomized controlled trial. BMC Health Serv Res, 13, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleeland CS and Ryan KM (1994). Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med, 23(2), 129–138. [PubMed] [Google Scholar]
- DeBar L, Benes L, Bonifay A, Deyo RA, Elder CR, Keefe FJ, McMullen C, Mayhew M, Owen-Smith A, Smith DH Trinacty CM, & Vollmer WM (2018). Interdisciplinary team-based care for patients with chronic pain on long-term opioid treatment in primary care (PPACT) – protocol for a pragmatic cluster randomized trial. Contemporary Clinical Trials, 67, 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBar L, Mayhew M, Benes L, Bonifay A, Deyo RA, Duffy S, Elder CR, Keefe FJ, Leo MC, McMullen C, Owen-Smith A, Porter L, Smith DH Trinacty CM, & Vollmer WM (2022). A primary care-based cognitive behavioral therapy intervention for long-term opioid users with chronic pain: A randomized pragmatic clinical trial. Annals of Internal Medicine, 175(1), 46–55. doi: 10.7326/M21-1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobscha SK, Corson K, Perrin NA, Hanson GC, Leibowitz RQ, Doak MN, Dickinson KC, Sullivan MD, & Gerrity MS (2009). Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA, 301(12), 1242–1252. [DOI] [PubMed] [Google Scholar]
- Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V, Koss MP, & Marks J (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Fischer K (2008). Assessing clinically meaningful change following a programme for managing chronic pain. Clinical Rehabilitation, 22, 252–259. [DOI] [PubMed] [Google Scholar]
- Gatchel R, Reuben D, Dagenais S, Turk D, Chou R, Hershey A, Hicks GE, Licciardone JC, & Horn S (2018). Research agenda for the prevention of pain and its impact: Report of the work group on the prevention of acute and chronic pain of the federal pain research strategy. The Journal of Pain, 19(8), 837–851. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM). (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, D.C: National Academies Press. [PubMed] [Google Scholar]
- Interagency Pain Research Coordinating Committee (IPRCC) (2016). National Pain Strategy: A comprehensive population health-level strategy for pain. Washington, D.C: National Academies Press. [Google Scholar]
- Ivers N, Jamtvedt G, Flottorp S, Young J, Odgaard-Jensen J, French S, O’Brien MA, Johansen M, Grimshaw J, & Oxman A (2012). Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MW (1991). A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep, 14(6), 540–545. [DOI] [PubMed] [Google Scholar]
- Keefe FJ and Somers TJ, Psychological approaches to understanding and treating arthritis pain. Nat Rev Rheumatol, 2010. 6(4): p. 210–216. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Blumenthal J, Baucom D, Affleck G, Waugh R, Caldwell DS, Beaupre P, Kashikar-Zuck S, Wright K, Egert J, & Lefebvre J (2004). Effects of spouse-assisted coping skills training and exercise training in patients with osteoarthritic knee pain: a randomized controlled study. Pain, 110(3), 539–549. [DOI] [PubMed] [Google Scholar]
- Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM, Asch SM, & Kroenke K (2009). Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med, 24 (6), 733–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine T, Spitzer R, Williams J, Berry J, & Mokdad A (2008). The PHQ-8 as a measure of current depression in the general population. J Affect Disord, 114, 163–174. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Krebs EE, Wu J, Yu Z, Chumbler NR, & Bair MJ (2014). Telecare collaborative management of chronic pain in primary care: a randomized clinical trial. JAMA, 312 (3), 240–8. [DOI] [PubMed] [Google Scholar]
- Loeser J (2005). Multidisciplinary pain management, in The paths of pain, Merskey H, Loeser J, and Dubner R, Editors. IASP: Seattle. p. 503–511. [Google Scholar]
- Mullis R & Hay EM (2010). Goal scaling for low back pain in primary care: development of a semi-structured interview incorporating minimal important change. Journal of Evaluation in Clinical Practice, 16, 1209–1214. [DOI] [PubMed] [Google Scholar]
- Pain Action Alliance to Implement a National Strategy (PAINS) (2017). Lost in chaos: The state of chronic pain in 2016. Downloaded from: http://painsproject.org/wp/wp-content/uploads/2017/02/STATEOFPAIN_web.pdf
- Roland M and Fairbank J (2000). The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine, 25(24), 3115–3124. [DOI] [PubMed] [Google Scholar]
- Rosenstiel AK and Keefe FJ (1983). The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain, 17(1), 33–44. [DOI] [PubMed] [Google Scholar]
- Roth RS, Geisser ME, & Williams DA (2012). Interventional pain medicine: retreat from the biopsychosocial model of pain. Transl Behav Med. 2 (1), 106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrubbe L, Ravyts S, Benas B, Campbell L, Cenn C, Coffman C, … Allen K (2016). Pain coping skills training for African Americans with osteoarthritis (STAART): Study protocol of a randomized controlled trial. BMC Musculoskeletal Disorders, 17(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelby R, Somers T, Keefe F, DeVellis B, Patterson C, Renner J, & Jordan J (2010) Brief fear of movement scale for osteoarthritis. Arthritis Care Res, 64(6), 862–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R, Kroenke K, Williams J, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, & Bonomi A (2001). Improving chronic illness care: translating evidence into action. Health Aff (Millwood), 20(6), 64–78. [DOI] [PubMed] [Google Scholar]
- Williams H (2017). The unspoken importance of the nurse in the 2016 National Pain Strategy. Pain Management Nursing, 18(3), 123–128. [DOI] [PubMed] [Google Scholar]