Abstract
Introduction:
The purpose of this study was to examine geographic variation in the availability of and barriers to school-based mental health services.
Methods:
A weighted, nationally representative sample of U.S. public schools from the 2017–2018 School Survey on Crime and Safety was used. Schools reported the provision of diagnostic mental health assessments and/or treatment as well as factors that limited the provision of mental health services. Availability of mental health services and factors limiting service provision were examined across rurality, adjusting for school enrollment and grade level. The analysis was conducted in December 2021.
Results:
Half (51.2%) of schools reported providing mental health assessments, and 38.3% reported providing treatment. After adjusting for enrollment and grade level, rural schools were 19% less likely, town schools were 21% less likely, and suburban schools were 11% less likely to report providing mental health assessments than city schools. Only suburban schools were less likely than city schools to provide mental health treatment (incidence rate ratio=0.85; 95% CI=0.72, 1.00). Factors limiting the provision of services included inadequate access to professionals (70.9%) and inadequate funding (77.0%), which were most common among rural schools.
Conclusions:
Significant inequities in school-based mental health services exist outside of urban areas.
INTRODUCTION
Millions of children and adolescents in the U.S.experience mental health conditions, such as anxiety and depression.1 Some studies have identified geographic variation in the prevalence of mental health conditions, with higher rates observed among children in rural areas than in urban areas.2 Suicide rates among rural children are higher than that among their urban peers, a disparity that has widened over time.3,4 Rural–urban disparities in youth suicide are especially alarming because rural youth have lower access to mental health services than their urban counterparts.5,6 Lack of providers and geographic isolation are 2 major contributors to reduced access to youth mental health services in rural areas.7
Public schools are integral to providing youth with mental health services such as counseling, diagnosis, and treatment.8-10 School social workers, mental health therapists, and psychologists provide varying levels of counseling and psychotherapy within the school setting, either individually or in a group milieu.11 School-based mental health professionals assist in developing and executing individualized education programs through diagnostic assessments, advocacy, support, and participation.10 They also develop and implement programs for behavior management, crisis intervention, violence prevention, and substance abuse counseling.12 School counselors deliver programming aimed at facilitating student success, including strategies to reinforce students’ academic, interpersonal, or emotional skills.13 Although school counselors may provide short-term counseling within their scope of practice,13 diagnostic and long-term mental health support services, including assessment and treatment for mental health disorders, are typically managed by school psychologists and, in some instances, clinical social workers.
Common models of mental health service delivery in schools include school-employed or contracted mental health professionals providing assessment and treatment at or outside school.14 In smaller schools, mental health professionals may be contracted part-time.15 However, rural schools face a scarcity of mental health professionals.16 This shortfall may be attributable to budget constraints, small student populations, or scarcity of providers.14,17 Workforce shortages and inadequate funding limit the ability of rural schools to recruit and retain mental health professionals.18
Using data from the 2015–2016 School Survey on Crime and Safety (SSOCS), Shelton and Owens reported that access to mental health services was lower in rural high schools than in high schools in city/urban and suburban areas.14 Although their study provided important insight into rural–urban inequities in the availability of high school-based mental health services, their exclusion of schools that serve lower grade levels and schools located within urban clusters but outside urbanized areas (i.e., schools in towns) precluded generalizability across grades and along more granular rural–urban gradients that often include towns.19 Examining the availability of school-based mental health services among all grade levels and across the full rural–urban gradient is warranted to generate more nuanced insights on geographic inequities in access to youth mental health services. Moreover, more recent SSOCS data are available (collected in 2017–2018), enabling an updated exploration of rural–urban variation in the provision of school-based mental health services in the U.S. This study aimed to examine the geographic variation in the availability of school-based mental health services across grade levels using the most recent nationally representative data available.
METHODS
Study Sample
Publicly available data from the National Center for Education Statistics (NCES) 2017–2018 SSOCS were used for this study.20 This nationally representative, cross-sectional survey includes school-level information about school violence prevention efforts, policies, and infrastructure. The survey was administered by mail, e-mail, and telephone from February 2018 to July 2018 to a stratified, random sample of public-school principals. The SSOCS sample is sufficiently large to allow for the generation of national estimates and stratification across select school characteristics.21
Measures
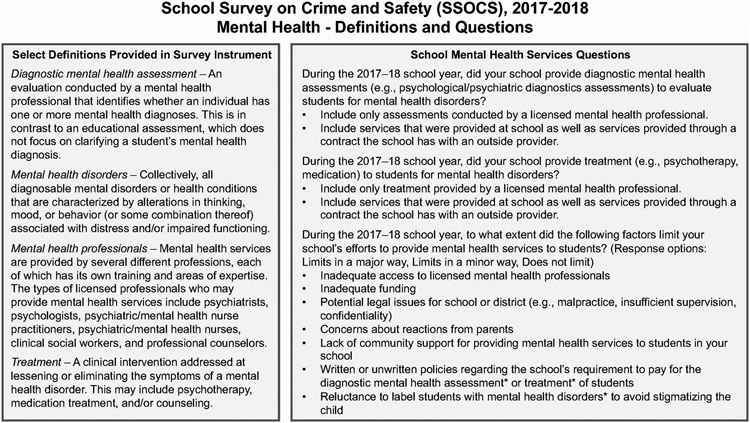
The SSOCS survey section about school mental health services included 2 questions regarding whether schools provided diagnostic mental health assessments and/or mental health treatment in the 2017–2018 school year (Figure 1). Data were also collected on whether mental health service provision was limited by access to providers, funding, legal issues, parental concerns, community support, payment policies, or stigma. The survey instrument provided definitions for technical terms used in the survey, including definitions for diagnostic mental health assessment, mental health disorders, mental health professionals, and treatment (Figure 1).21
Figure 1. Terminology definitions and questions related to mental health included in the 2017–2018 SSOCS.
Note: Available from https://nces.ed.gov/pubs2020/2020054.pdf.
SSOCS, School Survey on Crime and Safety.
School rurality was based on the NCES locale framework, which is composed of 4 types: city, suburban, town, and rural location. These definitions were developed with U.S. Census Bureau data and are based on proximity to urban areas and immediate area population size.22 City locations, which the populace may consider urban, are classified as areas within principal cities within urbanized areas (urban areas containing 50,000 or more people) and include densely populated, small, medium, and large metropolitan areas. The NCES suburban locale designation refers to areas inside an urbanized area but outside the boundaries of a principal city; suburban locales can be contained within metropolitan and micropolitan areas. Towns are urbanized clusters (urban areas containing 2,500–49,999 people), often located near urbanized areas. The NCES rural locale designation consists of census-defined rural territories and captures all areas outside of urbanized areas and urbanized clusters.22 Other school characteristics provided in the survey data included grade level (primary, middle, high school, or combined across all grades) and school enrollment (<300, 300–499, 500–999, or ≥1,000 students).
Statistical Analysis
Using Stata/MP, Version 15.1, the proportion of schools providing mental health services and the factors reported limiting service provision were calculated across degrees of rurality. Cochran-Armitage tests were used to examine trends in these outcomes across levels of rurality.23 Modified Poisson regression models24,25 (Poisson regression models with robust standard errors) were used to estimate the likelihood of providing mental health services (assessment or treatment) across rurality, adjusting for school enrollment and grade level (included as categorical covariates). These models produce incidence rate ratios (IRRs), which are similar to and can be interpreted as risk ratios. Adjusted modified Poisson models were also used to describe the association between factors limiting mental health services and rurality (adjusting for the covariates mentioned earlier). All analyses accounted for survey weighting. This study was not considered human subjects research because it involved analysis of publicly available data. The analysis took place in December 2021.
RESULTS
Of 4,803 schools included in the SSOCS probability sample, 2,762 completed the survey (weighted response rate: 61.7%), representing a weighted total of 82,300 public schools.21 City, suburban, town, and rural schools represented 27.3%, 33.2%, 12.8%, and 26.7% of the sample, respectively. School enrollment was negatively associated with rurality; 43.9% of rural schools had fewer than 300 students compared with 13.0% of city schools, 8.5% of suburban schools, and 18.2% of town schools (test for trend, p<0.001). Proportionally more rural schools were combined across all grade levels (19.2%) than city (4.6%), suburban (2.1%), and town (4.6%, p<0.001) schools.
Overall, 51.2% of schools reported providing diagnostic mental health assessments, and 38.3% reported providing mental health treatment (Table 1). The proportion of schools that provided diagnostic mental health assessments decreased significantly as rurality increased, from 58.4% of schools in city locales to 44.3% of rural schools (p<0.001). There was not a significant trend in the provision of mental health treatment by rurality (p=0.399).
Table 1.
Mental Health Services Provided and Factors Limiting Mental Health Service Provision in US Public Schools, by Urbanicity, School Survey on Crime and Safety, 2017-2018.
| Category | City/Urban (N=22,489) % |
Suburban (N=27,311) % |
Town (N=10,508) % |
Rural (N=21,979) % |
Total (N=82,288) % |
p-value* |
|---|---|---|---|---|---|---|
| Mental health services provided | ||||||
| Diagnostic mental health assessments | <0.001 | |||||
| Services not provided | 41.6 | 47.1 | 53.7 | 55.7 | 48.8 | |
| Services provided | 58.4 | 52.9 | 46.3 | 44.3 | 51.2 | |
| Mental health treatment | 0.399 | |||||
| Services not provided | 58.3 | 64.3 | 59.5 | 62.9 | 61.7 | |
| Services provided | 41.7 | 35.7 | 40.5 | 37.1 | 38.3 | |
| Factors limiting efforts to provide school-based mental health services | ||||||
| Inadequate access to professionals | 0.003 | |||||
| Limits in a major way | 40.9 | 35.7 | 41.1 | 46.0 | 40.5 | |
| Limits in a minor way | 27.6 | 30.5 | 32.0 | 32.3 | 30.4 | |
| Does not limit | 31.5 | 33.8 | 27.0 | 21.7 | 29.1 | |
| Inadequate funding | 0.025 | |||||
| Limits in a major way | 53.3 | 47.4 | 51.5 | 57.0 | 52.1 | |
| Limits in a minor way | 21.3 | 26.4 | 29.9 | 24.4 | 24.9 | |
| Does not limit | 25.4 | 26.3 | 18.6 | 18.6 | 23.0 | |
| Potential legal issues | 0.218 | |||||
| Limits in a major way | 22.5 | 18.8 | 14.4 | 15.4 | 18.3 | |
| Limits in a minor way | 23.5 | 27.4 | 36.4 | 30.4 | 28.3 | |
| Does not limit | 54.0 | 53.8 | 49.2 | 54.2 | 53.4 | |
| Concerns about reactions from parents | 0.002 | |||||
| Limits in a major way | 15.0 | 7.6 | 10.1 | 5.9 | 9.5 | |
| Limits in a minor way | 30.1 | 29.5 | 31.1 | 30.9 | 30.2 | |
| Does not limit | 54.9 | 63.0 | 58.9 | 63.2 | 60.3 | |
| Lack of community support | <0.001 | |||||
| Limits in a major way | 16.7 | 11.2 | 7.5 | 6.5 | 11.0 | |
| Limits in a minor way | 28.9 | 25.1 | 33.0 | 25.8 | 27.3 | |
| Does not limit | 54.5 | 63.7 | 59.5 | 67.7 | 61.7 | |
| Payment policies | 0.854 | |||||
| Limits in a major way | 23.1 | 18.7 | 18.8 | 21.3 | 20.6 | |
| Limits in a minor way | 24.0 | 24.2 | 32.8 | 23.9 | 25.1 | |
| Does not limit | 52.9 | 57.1 | 48.4 | 54.9 | 54.3 | |
| Reluctance to label students | 0.339 | |||||
| Limits in a major way | 12.7 | 8.8 | 10.2 | 10.6 | 10.5 | |
| Limits in a minor way | 28.3 | 29.1 | 35.1 | 25.0 | 28.6 | |
| Does not limit | 59.1 | 62.1 | 54.7 | 64.4 | 60.9 |
Diagnostic mental health assessments include psychological/psychiatric diagnostic assessments to evaluate students for mental health disorders. Mental health treatment includes psychotherapy or medication for students with mental health disorders.
Significance based on Cochran-Armitage test for rural trend. Post-estimation survey weights applied to account for survey sampling design.
Note: Boldface indicates statistical significance (p<0.05).
After adjusting for school enrollment and grade level, schools in rural, town, and suburban locales were significantly less likely to report providing diagnostic mental health assessments for mental health disorders than city schools (Table 2). No significant association was identified between the provision of treatment for students with mental health disorders and school rurality in multivariable models except for suburban schools, which were 15% less likely to offer mental health treatment than city schools (IRR=0.85; 95% CI=0.72, 1.00).
Table 2.
Provision of Mental Health Services and Barriers Faced by US Public Schools by Rurality, 2017-2018, School Survey on Crime and Safety, 2017-2018.
| Category | City/ Urban |
Suburban IRR (95% CI) |
Town IRR (95% CI) |
Rural IRR (95% CI) |
|---|---|---|---|---|
| Mental health services provided a | ||||
| Diagnostic mental health assessments | Ref | 0.89 (0.79-1.00) * | 0.79 (0.67-0.94) ** | 0.81 (0.69-0.95) ** |
| Mental health treatment | Ref | 0.85 (0.72-1.00) * | 0.96 (0.79-1.18) | 0.93 (0.76-1.13) |
| Factors limiting efforts to providing school-based mental health services b | ||||
| Inadequate access to professionals | Ref | 0.97 (0.88-1.06) | 1.07 (0.96-1.19) | 1.15 (1.04-1.27) ** |
| Inadequate funding | Ref | 0.99 (0.91-1.07) | 1.09 (1.00-1.19) | 1.10 (1.01-1.20) * |
| Potential legal issues | Ref | 1.00 (0.87-1.15) | 1.10 (0.93-1.31) | 1.00 (0.84-1.19) |
| Concerns about reactions from parents | Ref | 0.81 (0.66-0.95) ** | 0.92 (0.75-1.12) | 0.85 (0.71-1.03) |
| Lack of community support | Ref | 0.81 (0.69-0.94) ** | 0.87 (0.71-1.06) | 0.70 (0.57-0.85) ** |
| Payment policies | Ref | 0.91 (0.79-1.05) | 1.10 (0.93-1.31) | 0.96 (0.81-1.14) |
| Reluctance to label students | Ref | 0.93 (0.79-1.09) | 1.11 (0.92-1.35) | 0.89 (0.73-1.09) |
Diagnostic mental health assessments include psychological/psychiatric diagnostic assessments to evaluate students for mental health disorders. Mental health treatment includes psychotherapy or medication for students with mental health disorders. Values indicate adjusted relative risk estimated and 95% confidence intervals for services or factors listed, adjusted for school enrollment and grade level. Post-estimation survey weights applied to account for survey sampling. Model includes primary schools, middle schools, high schools, and schools with combined grade levels.
Abbreviations: IRR, incidence rate ratio; CI, confidence interval
Refers to services provided by a school-employed or contracted mental health professional.
Factors limiting in a major or minor way vs. not limiting at all.
p<0.05
p<0.01
Note: Boldface indicates statistical significance (p<0.05).
Common factors reported to limit the provision of school-based mental health services included inadequate access to professionals (70.9%) and inadequate funding (77.0%). These barriers were most common among schools in rural locales; as rurality increased, tests for trend indicated significantly higher proportions of schools reporting these limitations to implementing mental health efforts (Table 1). In contrast, a higher proportion of city schools reported concerns about reactions from parents and lack of community support limiting school-based mental health services than that of rural schools (Table 1).
Regression models indicated that after accounting for school size and grade level, rural schools were more likely to cite inadequate access to professionals (IRR=1.15; 95% CI=1.04, 1.27) and inadequate funding (IRR=1.10; 95% CI=1.01, 1.20) than schools in city locales (Table 2). However, rural and suburban schools were 30% and 19% less likely to report a lack of community support as a limitation to mental health efforts, respectively, than city schools (rural IRR=0.70; 95% CI=0.57, 0.85; suburban IRR: 0.81; 95% CI=0.69, 0.94). Suburban schools were also less likely to report that parental concerns limited mental health efforts than city schools (IRR=0.81; 95% CI=0.66, 0.95).
DISCUSSION
The primary findings of this study were that schools located outside of cities were less likely to provide diagnostic mental health assessments. There were no differences across rurality for the provision of mental health treatment, except for suburban schools being less likely to provide treatment than city schools. Results from this study extend the work of Shelton and Owens who examined the provision of mental health services in U.S. high schools using 2015–2016 SSOCS data.14 In their analysis, the authors conducted bivariate comparisons across 3 levels of rurality (city/urban, suburban, and rural) and found that proportionately fewer students in rural schools had access to diagnostic assessments at school by school-employed mental health professionals. In addition, they found that proportionately fewer students in rural schools had access to treatment at school by school-employed or school-funded mental health professionals.
Consistent with Shelton and Owens, we found that inadequate access to professionals and inadequate funding were reported as factors that limit schools’ efforts to provide mental health services, particularly for rural schools. Interestingly, this study identified schools in rural locales as having a lower likelihood of reporting a lack of community support as a limitation to providing mental health services, whereas Shelton and Owens found no variation across school locations.
Limited access to qualified providers was a common barrier for all schools, particularly for rural schools. In the long term, provider shortages may be addressed through targeted financial incentives (e.g., loan repayment, scholarships) and pipeline recruitment and education efforts to cultivate a sustainable workforce of qualified mental health professionals to support students in rural schools.18,26 Strategies such as the National Health Service Corps Loan Repayment Program have been credited with disproportionately increasing visits for depression and anxiety in rural relative to those in urban settings.27,28 Other approaches for recruiting and retaining providers in rural areas include increasing exposure through rural-focused curricula or rotations29 and supporting the needs of rural providers (e.g., addressing professional isolation and barriers to continuing education).30 More immediately, however, remote technology solutions, including synchronous video-based or text-oriented approaches to telemental health, could be considered.31
Inadequate funding for providing school-based mental health services was a common barrier facing schools but was most prevalent for schools in rural areas. Financial hurdles can be overcome by alternative models of care, including expanding experiences for student trainees in rural communities,29,32 task sharing and expanding practice among healthcare professionals and paraprofessionals,26,33 integration of mental health into primary care,27,33 and school-based mental health centers (i.e., supported by state funding).34 School budget models that fund support services, such as those that proportionally distribute funding for staffing ratios on the basis of student enrollment, are challenging for small, rural school districts.35 This aligns with arguments that market-based approaches to healthcare and public health financing are structural barriers to optimizing health in rural areas.36 More creative approaches to providing mental healthcare services may need to be adopted by rural school districts, such as models that share staff across districts or crisis protocols to address after hours or urgent mental health concerns. Remote, synchronous mental health services can also be provided to students through telehealth based at schools,37,38 which can increase access to care among those with broadband and technology barriers at home.39 It is likely that some rural schools have already been adopting creative approaches to increasing mental healthcare access, which could explain why schools in rural areas were as likely as schools in cities to provide mental health treatment services.
Although rural schools were less likely than those in city locales to offer diagnostic mental health assessments and were more likely to report financial-related barriers to providing school-based mental health services, community support was less likely to be a limitation in providing school-based mental health services in rural schools. This finding may reflect broad recognition within rural communities that access to health care and mental health are leading rural health priorities40 and that access to school-based mental health services would help address critical needs in the community. Suburban schools were significantly less likely to report a lack of community support or concerns about parental reactions as barriers to providing school-based mental health services than city schools. This finding may reflect suburban–city differences in unmeasured sociocultural factors such as greater racial and ethnic diversity in urban areas41 in which principals may perceive greater diversity in parental perspectives regarding school-based treatment for mental health.
Despite evidence that increasing access to school-based mental health services has been associated with reduced suicidal ideation and attempts,34 opposition to increasing access to school-based mental health services has been reported in the media.42 Efforts to expand access to school-based mental health services should consider the diverse sociopolitical contexts that exist across geographic settings in the U.S. Future research to identify the most substantial barriers across the rural–urban continuum may inform more targeted efforts aimed at increasing access to school-based mental health services.
Compared with city schools, suburban schools were less likely to offer mental health treatment. This finding aligns with previous research, which has reported healthcare access barriers in suburban communities, particularly for uninsured or low-income residents.43 The increase in suburban poverty and changes in the demographic composition of suburban communities has generated concern about healthcare access in these communities.44 With population growth in suburban areas of the U.S. outpacing that in urban areas,41 additional research is needed to examine whether suburban areas are experiencing growing healthcare access inequities in light of population and sociodemographic changes. The lack of variation between city and town or rural schools also beckons further examination. Given the challenges in staffing school-based mental health professionals,16 few schools may offer mental health treatment to students with diagnosed mental health disorders. Instead, students may be referred to community-based mental health professionals for treatment. Future research into these relationships and solutions is needed to ensure equitable access to services; some solutions, such as relying on community-based providers, may be a concern for those in rural areas where mental health professionals remain scarce.
Limitations
Findings from this study should be interpreted within the context of its limitations. First, the SSOCS only provides information about the availability of services, and the accessibility and acceptability of school-based mental health services were not examined. In addition, the survey does not provide information about schools’ integration of mental health assessment and treatment in the context of safety, including violence prevention. Second, the SSOCS data are based on a probability sample of U. S. schools, and although survey weighting accounts for possible selection bias by school locale, the possibility that respondent schools differed significantly from non-respondent schools across unmeasured characteristics remains.21 Third, the SSOCS data provide limited information on school or community characteristics, which hinders the ability to examine the relationships between these characteristics and the availability of mental health services. Although previous research was able to delineate whether school-based services were offered at school or outside of school,14 small numbers of observations across these subcategories, together with multiple levels of rurality and covariates did not allow analysis in this study. Fourth, in the 2017–2018 SSOCS, the complex definition of mental health disorders (Figure 1) may have been interpreted by respondents as serious mental illnesses, which could lead to underreporting of services for other diagnosable mental health conditions, such as depression. However, no evidence of such misinterpretation was noted, and the definitions provided are a strength of the SSOCS and likely led to more consistent findings. Finally, the definition of a mental health provider in the SSOCS includes a wide range of licensed health professionals (Figure 1), and schools did not specify the type of licensed professional who provided services in their schools. Thus, it is not possible to determine rural–urban differences in access to mental health providers with prescriptive authority or those with advanced training to address complex child and adolescent mental health needs. Nonetheless, previous evidence confirms that inequities remain in rural youths’ access to mental health services by rurality.5,6
CONCLUSIONS
This study found that the provision of some school-based mental health services varies across rurality, as do factors limiting the implementation of these services. In this study, suburban schools were less likely to provide mental health treatment than city schools, and schools’ provision of mental health assessments decreased with increasing rurality. The lack of diagnostic mental health assessments outside of cities generates concern that students in need of mental health and related services may not be readily identified. Timely diagnostic assessments help ensure that evidence-based interventions are provided early, including services beyond psychotherapy and medications, such as accommodations for intellectual or other developmental disabilities. Such services also include violence prevention efforts, which are critically interconnected with school-based mental health services.45,46
Inequitable access to school-based mental health services is particularly important in rural areas, where students more frequently report signs of depression and anxiety than urban youth2 and have higher suicide rates.3,4 Strategies to improve rural mental health services through innovative treatment models, policies, financing, and provider recruitment and retention are critical to addressing mental health disparities among rural children and adolescents.
ACKNOWLEDGMENTS
The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Institute for Research and Education to Advance Community Health.
Research reported in this publication was supported by the Faculty Pilot Grant Program from the Institute for Research and Education to Advance Community Health at Washington State University. DAA was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number K23MD013899.
No financial disclosures were reported by the authors of this paper.
Footnotes
CREDIT AUTHOR STATEMENT
Janessa M. Graves: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing–original draft. Demetrius A. Abshire: Formal analysis, Funding acquisition, Writing–original draft. Jessica L. Mackelprang: Formal analysis, Writing–review and editing. Julia A. Dilley: Writing–review and editing. Solmaz Amiri: Writing–review and editing. Christina M. Chacon: Writing–review and editing. Anne Mason: Writing–review and editing.
REFERENCES
- 1.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and treatment of depression, anxiety, and conduct problems in U.S. children. J Pediatr. 2019;206:256–267.e3. 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health Resources and Services Administration (HRSA), Maternal Child Health Bureau, Data Brief NSCH. Rural/urban differences in children’s health. https://mchb.hrsa.gov/sites/default/files/mchb/data-research/rural-urban-differences.pdf. Published 2020. Accessed February 24, 2021. [Google Scholar]
- 3.Fontanella CA, Hiance-Steelesmith DL, Phillips GS, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatr. 2015;169(5):466–473. 10.1001/jama-pediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ivey-Stephenson AZ, Crosby AE, Jack SPD, Haileyesus T, Kresnow-Sedacca MJ. Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death - United States, 2001-2015. MMWR Surveill Summ. 2017;66(18):1–16. 10.15585/mmwr.ss6618a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cummings JR, Case BG, Ji X, Marcus SC. Availability of youth services in U.S. mental health treatment facilities. Adm Policy Ment Health. 2016;43(5):717–727. 10.1007/s10488-015-0685-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graves JM, Abshire DA, Mackelprang JL, Amiri S, Beck A. Association of rurality with availability of youth mental health facilities with suicide prevention services in the U.S. JAMA Netw Open. 2020;3(10):e2021471. 10.1001/jamanetworkopen.2020.21471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H. Growth and distribution of child psychiatrists in the United States: 2007-2016. Pediatrics. 2019;144(6):e20191576. 10.1542/peds.2019-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taras HL. American Academy of Pediatrics Committee on School Health. School-based mental health services. Pediatrics. 2004;113(6):1839–1845. 10.1542/peds.113.6.1839. [DOI] [PubMed] [Google Scholar]
- 9.Duong MT, Bruns EJ, Lee K, et al. Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm Policy Ment Health. 2021;48(3):420–439. 10.1007/s10488-020-01080-9. [DOI] [PubMed] [Google Scholar]
- 10.Marsh RJ, Mathur SR. Mental Health in Schools: an overview of multitiered systems of support. Interv Sch Clin. 2020;56(2):67–73. 10.1177/1053451220914896. [DOI] [Google Scholar]
- 11.School based mental health. Youth.gov. https://youth.gov/youth-topics/youth-mental-health/school-based. Accessed May 16, 2022.
- 12.Teich JL, Robinson G, Weist MD. What kinds of mental health services do public schools in the united states provide? Adv Sch Ment Health Promot. 2008;1(suppl 1):13–22. 10.1080/1754730X.2008.9715741. [DOI] [Google Scholar]
- 13.American School Counselor Association. The role of the school counselor. Alexandria, VA: American School Counselor Association; 2022. https://www.schoolcounselor.org/getmedia/ee8b2e1b-d021-4575-982c-c84402cb2cd2/Role-Statement.pdf. [Google Scholar]
- 14.Shelton AJ, Owens EW. Mental health services in the United States public high schools. J Sch Health. 2021;91(1):70–76. 10.1111/josh.12976. [DOI] [PubMed] [Google Scholar]
- 15.Edwards LM, Sullivan AL. School psychology in rural contexts: ethical, professional, and legal issues. J Appl Sch Psychol. 2014;30(3):254–277/07/03. 10.1080/15377903.2014.924455. [DOI] [Google Scholar]
- 16.National Association of School Psychologists. Shortages in school psychology: challenges to meeting the growing needs of U.S. students and schools [research summary]. Bethesda, MD: National Association of School Psychologists; 2021. https://www.nasponline.org/Documents/Research%20and%20Policy/Research%20Center/School_Psychology_Shortage.pdf. [Google Scholar]
- 17.O’Malley M, Wendt SJ, Pate C. A view from the top: superintendents’ perceptions of mental health supports in rural school districts. Educ Admin Q. 2018;54(5):781–821. 10.1177/0013161X18785871. [DOI] [Google Scholar]
- 18.Baum N, King J. The behavioral health workforce in rural America: developing a national recruitment strategy. Ann Arbor, MI: Center for Health Research Transformation, University of Michigan; 2020. https://www.behavioralhealthworkforce.org/wp-content/uploads/2020/02/Recruitment-and-Retention-of-BH-Providers-Full-Report-2.2020.pdf. [Google Scholar]
- 19.2010 Rural-urban commuting area (RUCA) codes. United States Department of Agriculture, Economic Research Service; 2020. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/. [Google Scholar]
- 20.School survey on crime and safety 2017–18. National Center for Educational Statistics. https://nces.ed.gov/surveys/ssocs/data_products.asp#2018. Accessed January 24, 2022. [Google Scholar]
- 21.Padgett Z, Jackson M, Correa S, et al. School survey on crime and safety 2017–18: public-use data file user’s manual (NCES 2020–054). Washington, DC: National Center for Educational Statistics; 2020. https://nces.ed.gov/pubs2020/2020054.pdf. [Google Scholar]
- 22.Geverdt DE. Education demographic and geographic estimates (EDGE) program: locale boundaries, 2015. NCES 2016-032. Washington, DC: U.S. Department of Education, National Center for Education Statistics; 2017. https://nces.ed.gov/programs/edge/docs/edge_nces_locale_2015.pdf. [Google Scholar]
- 23.Armitage P Tests for linear trends in proportions and frequencies. Biometrics. 1955;11(3):375–386. 10.2307/3001775. [DOI] [Google Scholar]
- 24.Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003;3(1):21. 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zou G A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 26.Kepley HO, Streeter RA. Closing behavioral health workforce gaps: a HRSA program Expanding direct mental health service access in underserved areas. Am J Prev Med. 2018;54(6):S190–S191 (suppl 3). 10.1016/j.amepre.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Han X, Ku L. Enhancing staffing in rural community health centers can help improve behavioral health care. Health Aff (Millwood). 2019;38(12):2061–2068. 10.1377/hlthaff.2019.00823. [DOI] [PubMed] [Google Scholar]
- 28.Han X, Pittman P, Erikson C, Mullan F, Ku L. The role of the National Health Service Corps clinicians in enhancing staffing and patient care capacity in community health centers. Med Care. 2019;57(12):1002–1007. 10.1097/MLR.0000000000001209. [DOI] [PubMed] [Google Scholar]
- 29.Guerrero APS, Balon R, Beresin EV, et al. Rural mental health training: an emerging imperative to address health disparities. Acad Psychiatry. 2019;43(1):1–5. 10.1007/s40596-018-1012-5. [DOI] [PubMed] [Google Scholar]
- 30.Brooks RG, Walsh M, Mardon RE, Lewis M, Clawson A. The roles of nature and nurture in the recruitment and retention of primary care physicians in rural areas: a review of the literature. Acad Med. 2002;77 (8):790–798. 10.1097/00001888-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Patel SY, Huskamp HA, Busch AB, Mehrotra A. Telemental health and U.S. Rural-urban differences in specialty mental health use, 2010–2017. Am J Public Health. 2020;110(9):1308–1314. 10.2105/AJPH.2020.305657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huber BJ, Austen JM, Tobin RM, Meyers AB, Shelvin KH, Wells M. Overcoming barriers to rural children’s mental health: an interconnected systems public health model. Adv Sch Ment Health Promot. 2016;9(3–4):219–241. 10.1080/1754730X.2016.1224121. [DOI] [Google Scholar]
- 33.Hoeft TJ, Fortney JC, Patel V, Unützer J. Task-sharing approaches to improve mental health care in rural and other low-resource settings: a systematic review. J Rural Health. 2018;34(1):48–62. 10.1111/jrh.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paschall MJ, Bersamin M. School-based mental health services, suicide risk and substance use among at-risk adolescents in Oregon. Prev Med. 2018;106:209–215. 10.1016/j.ypmed.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kolbe T, Baker BD, Atchison D, Levin J, Harris P. The additional cost of operating rural schools: evidence from Vermont. AERA Open. 2021;7 2332858420988868. 10.1177/2332858420988868. [DOI] [Google Scholar]
- 36.Probst J, Eberth JM, Crouch E. Structural urbanism contributes to poorer health outcomes for rural America. Health Aff (Millwood). 2019;38(12):1976–1984. 10.1377/hlthaff.2019.00914. [DOI] [PubMed] [Google Scholar]
- 37.Abdul-Raheem JN, Liu AJ, Collins ME. Reimagining the role of school-based health centers during the COVID-19 pandemic. J Sch Health. 2021;91(4):271–273. 10.1111/josh.13000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fox K, Burgess A, Williamson ME, et al. Implementation of telehealth services in rural schools: a qualitative assessment. J Sch Health. 2022;92(1):71–78. 10.1111/josh.13104. [DOI] [PubMed] [Google Scholar]
- 39.Graves JM, Abshire DA, Amiri S, Mackelprang JL. Disparities in technology and broadband internet access across rurality: implications for health and education. Fam Community Health. 2021;44(4):257–265. 10.1097/FCH.0000000000000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural Healthy People 2020: new decade, Same challenges. J Rural Health. 2015;31(3):326–333. 10.1111/jrh.12116. [DOI] [PubMed] [Google Scholar]
- 41.Parker K, Horowitz J, Brown A, Fry R, Cohn DV, Igielnik R. What unites and divides urban, suburban and rural communities: demographic and economic trends in urban, suburban and rural communities. Washington, DC: Pew Research Center; 2018. https://www.pewresearch.org/social-trends/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/. [Google Scholar]
- 42.Barry E A mental health clinic in school? No, thanks, says the school board. The New York Times; 2022. June 5 https://www.nytimes.com/2022/06/05/health/killingly-ct-mental-health-clinic-school.html. [Google Scholar]
- 43.Schnake-Mahl AS, Sommers BD. Health care in the suburbs: an analysis of suburban poverty and health care access. Health Aff (Millwood). 2017;36(10):1777–1785. 10.1377/hlthaff.2017.0545. [DOI] [PubMed] [Google Scholar]
- 44.Felland LE, Lauer JR, Cunningham PJ. Suburban poverty and the health care safety net. Res Brief. 2009(13):1–12. http://www.hschange.org/CONTENT/1074/. [PubMed] [Google Scholar]
- 45.Briesch A, Chafouleas SM. School mental health resources critical to ensuring safe school environments. The Conversation. June 7, 2022. https://theconversation.com/school-mental-health-resources-critical-to-ensuring-safe-school-environments-183967. [Google Scholar]
- 46.Leaf PJ, Keys SG. Collaborating for violence prevention: training health professionals to work with schools. Am J Prev Med. 2005;29(5):279–287 (suppl 2). 10.1016/j.amepre.2005.08.032. [DOI] [PubMed] [Google Scholar]