Abstract
Recent efforts to develop a vaccine against the diarrheal disease cholera have focused on the use of live attenuated strains of the causative organism, Vibrio cholerae. The Ogawa lipopolysaccharide phenotype is expressed by many epidemic strains, and motility defects reduce the risk of reactive diarrhea in vaccine recipients. We therefore converted a motile Inaba+ vaccine candidate, Peru-2, to a nonmotile Ogawa+ phenotype using a mariner-based transposon carrying rfbT, the gene required for expression of the Ogawa phenotype. Analysis of 22 nonmotile Peru-2 mutants showed that two were Ogawa+, and both of these strains had insertions in the flgE gene. It was possible to convert these strains to antibiotic sensitivity by introducing a recombinase that acts on sites flanking the antibiotic marker on the transposon. The resulting strains are competent for colonization in infant mice and may therefore be suitable as vaccine candidates for use either independently or in a combination with strains of different biotypes and serotypes.
The gram-negative bacterium Vibrio cholerae is the causative agent of the diarrheal disease cholera. Infection typically begins with ingestion of V. cholerae in contaminated food or water. Upon colonization of the host, V. cholerae produces an A-B exotoxin (cholera toxin) that acts on the cells of the intestinal epithelium to induce a secretory diarrhea so severe that death can result within a few days (7, 20, 29). The disease is endemic in the Indian subcontinent and is estimated to affect millions of persons worldwide each year (19).
Efforts to combat cholera depend primarily on oral rehydration therapy, which is both simple and relatively inexpensive (5, 40). The importance of safe water supplies and adequate sanitation has also long been recognized (43, 51, 57). Nevertheless, as evidenced by the large number of cholera-related deaths reported annually, there are practical obstacles to applying any of these strategies consistently and effectively, particularly in underdeveloped areas of the world. This has made the need for a cholera vaccine increasingly urgent.
Killed whole-cell formulations, purified cholera toxin B subunit, and purified lipopolysaccharide (LPS) have been tested as vaccines, but none has demonstrated both efficacious and long-term protection against the disease (35). Based on evidence that development of long-lived protection against V. cholerae infection is strongly favored by clinical infection and presentation of vibrio immunogens to the mucosal immune system (24, 47), recent attempts to develop cholera vaccines have focused on the use of live, attenuated strains. Many of these strains are indeed immunogenic but also cause mild diarrhea in human volunteers (30, 34, 58). There were indications that colonization of the gut was required for immunogenicity but necessarily resulted in reactogenicity (60), and it seemed that this might constitute a considerable obstacle to the construction of acceptable vaccine strains. Fortunately, nonmotile vaccine candidates demonstrate both good immunogenicity and low reactogenicity (13, 33, 60), although the exact contribution of motility to V. cholerae infection is unknown.
Of the at least 151 recognized V. cholerae serogroups, only O1 and O139 serovars are thus far known to cause epidemic cholera. Strains of the O1 serogroups are divided into two biotypes, classical and El Tor (32, 53). Two of the six cholera pandemics since 1817 are known to have been caused by classical biotype strains, but the El Tor biotype is responsible for the current pandemic (4). The O139 serovar emerged in the Indian subcontinent in 1992 and was the first non-O1 serovar known to cause epidemic cholera (2, 49). O139 strains closely resemble O1 El Tor strains but possess a unique O antigen and are encapsulated (27, 64).
The vast majority of strains within the O1 serogroup display one of two serotypes that correspond to the expression patterns of certain LPS antigens. Inaba strains express the A and C antigens, while Ogawa strains express the A and B antigens and a small amount of the C antigen (41). The precise nature of the A, B, and C antigens is unknown. However, it has been shown that the rfbT gene determines the difference between the Ogawa and Inaba serotypes, in that the presence of rfbT is sufficient for Inaba-to-Ogawa serotype conversion (55).
The first V. cholerae isolates from the Latin American epidemic were identified as O1 Inaba strains, but Ogawa strains appeared within 8 months (59, 63) and 90% of Peruvian V. cholerae isolates were of the Ogawa serotype by 1995 (17, 62). Ogawa strains are prevalent in cholera-affected areas around the world (1, 10, 16, 22, 26, 31, 45, 48, 65), and since protective immunity against V. cholerae infection is provided in large part by anti-LPS antibodies (44, 56), the development of Ogawa vaccine strains may be highly advantageous. It has already been suggested that the most effective cholera vaccine might consist of a combination of strains of different biotypes and serotypes and that development of an El Tor Ogawa vaccine strain would be critical in such an approach (33, 61).
The vaccine candidate Peru-15 is a stably nonmotile, nontoxinogenic derivative of the Peruvian isolate C6709 (33). The genetic lesion resulting in nonmotility in Peru-15 has not been characterized at the molecular level. We therefore decided to construct a new Peru derivative by inserting rfbT into a motility gene, thereby simultaneously producing an Ogawa+ phenotype and a defined motility defect. Since it was unknown what level of rfbT expression would be necessary to convert a C6709 derivative to Ogawa+, transposon delivery was selected as the method for introducing rfbT into the target strain. It was reasoned that because some bacterial motility genes are quite highly expressed, transposon delivery into a motility gene could place rfbT under the control of a sufficiently active promoter to result in an Ogawa phenotype. mariner transposons were particularly suited to this approach, since they have relatively low site specificity, increasing the chances of obtaining an insertion into a site favorable for expression of rfbT.
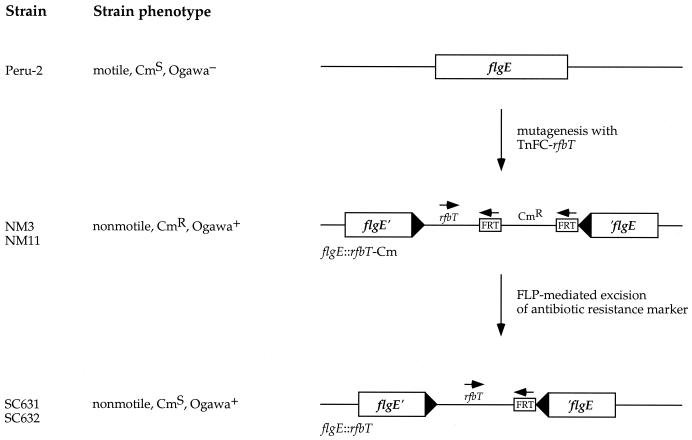
Since the presence of antibiotic markers is undesirable in vaccine candidates, the delivery transposon was engineered such that its chloramphenicol resistance (Cmr) allele is flanked by directly repeated FRT sites. The yeast FLP recombinase catalyzes excision of sequences flanked by directly repeated FRT sites (14, 15), and the FRT-Cmr cassette therefore permits the use of chloramphenicol selection to isolate transposon mutants and subsequent FLP-mediated excision to remove the Cmr marker from the chromosome. The rfbT delivery transposon was used to obtain nonmotile mutants of Peru-2, a motile precursor of Peru-15 (A. Roberts, G. D. N. Pearson, and J. J. Mekalanos, Proc. 28th Joint Conf. U.S.-Japan Coop. Med. Sci. Program Cholera Relat. Diarrheal Dis., abstr., 1992). The nonmotile mutants were then screened for expression of Ogawa antigen. Two nonmotile, Ogawa+ strains were isolated, and these were found to harbor independent insertions in the flgE gene. Expression of FLP recombinase in these strains resulted in loss of Cmr without affecting the motility and Ogawa phenotypes. The Cms derivatives were aflagellar and competent for colonization of infant mice.
Although the mariner-FRT transposon delivery system was developed to create a nonmotile, Ogawa+ C6709 derivative, this method should prove broadly useful. A similar system employing Tn5 has been used to target DNA to the Escherichia coli chromosome (25), but use of a mariner transposon offers the advantages of extremely low site specificity and an exceptionally broad host range that includes both gram-positive and gram-negative bacteria (52). The mariner-FRT system should therefore facilitate the construction of vaccine strains for a variety of pathogenic bacteria, including those for which it has been difficult to implement allelic replacement or conventional transposon delivery strategies.
MATERIALS AND METHODS
Bacterial strains and plasmids.
The strains and plasmids used in this study are listed in Table 1. All strains were stored at −75°C after addition of 80% (vol/vol) glycerol to cultures to a final concentration of 20% glycerol. All plasmids were purified using the QIAprep Spin Miniprep Kit (Qiagen Inc., Valencia, Calif.).
TABLE 1.
Strains and plasmids used in this study
| Strain or plasmid | Description | Reference or source |
|---|---|---|
| E. coli strains | ||
| SM10 λ pir | thi thr leu tonA lacY supE recA::RP-4-Tc::Mu (λ pir) | 42 |
| SC625 | TOP10 TnFC-rfbT mutant; Cmr | This study |
| V. cholerae strains | ||
| E7946 | El Tor; Ogawa | |
| Peru-2 | C6709 ΔattRS1; Inaba | 60 |
| Peru-15 | C6709 ΔattRS1 recA::htpG-ctxB; spontaneously nonmotile; Inaba | 33 |
| NM3 | Peru-2 flgE::TnFC-rfbT Fla−; Ogawa | This study |
| NM11 | Peru-2 flgE::TnFC-rfbT Fla−; Ogawa | This study |
| SC631 | NM3 ΔCmr; Ogawa | This study |
| SC632 | NM11 ΔCmr; Ogawa | This study |
| Plasmids | ||
| pBR322 | Standard cloning vector; Apr | New England Biolabs |
| pCP20 | FLP recombinase expression plasmid; pSC101 origin of replication; Apr | 8 |
| pCR2.1 | Cloning vector; Apr | Invitrogen |
| pNEB193 | Standard cloning vector; Apr | New England Biolabs |
| pSC121.1 | rfbT gene from E7946 cloned into pCR2.1; Apr | This study |
| pSC138 | TnFC-rfbT; Cmr | This study |
| pSC141 | Replicon fusion of pCP20 and pBR322; Apr Tcr | This study |
Media and buffers.
All of the buffers and media employed have been described previously. Antibiotics were used at the following concentrations: ampicillin, 100 μg/ml; chloramphenicol, 20 μg/ml for E. coli and 1 μg/ml for V. cholerae; kanamycin, 30 μg/ml; streptomycin, 100 μg/ml; tetracycline, 12.5 μg/ml for E. coli and 1.25 μg/ml for V. cholerae.
Nucleic acid manipulations.
All nucleic acid manipulations were accomplished in accordance with standard molecular biology techniques (3). Cloning of the rfbT PCR product was accomplished using the TOPO TA Cloning kit (Invitrogen, Carlsbad, Calif.) in accordance with the manufacturer's directions. Preliminary sequence data were obtained from The Institute of Genomic Research website at http://www.tigr.org.
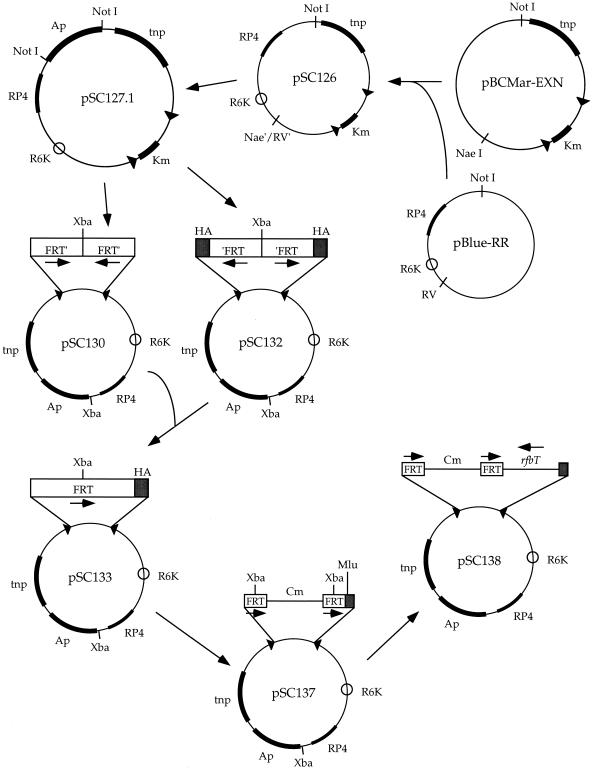
Construction of pSC138.
The 3.1-kb NaeI/NotI fragment of pBCMar-EnterpriseXN was ligated to the 2.2-kb EcoRV/NotI fragment of pBlue-R6K RP4 (28) to create pSC126. The β-lactamase gene from pBluescript KS(+) was then amplified by PCR and cloned into the NotI site of pSC126, producing pSC127.1. Next, oligonucleotide oSC53 (5′ TCTAGAGAATAGGAACTTCGGAATAGGAACTTCAGACCGGGGACTTATCAGCCAACCTGTTAG 3′) was used to amplify a 5.2-kb product from pSC127.1 and this product was treated with T4 polynucleotide kinase and self-ligated to create pSC130. A 5.2-kb fragment was similarly amplified from pSC127.1 using oligonucleotide oSC54 (5′ TCTAGAAAGTATAGGAACTTCAACGCGTAGTCTGGGACGTCGTATGGGTAAGACCGGGGACTTATCAGCCAACCTGTTA 3′), kinased, and self-ligated to produce pSC132. The 2.7-kb XbaI fragment of pSC130 and the 2.5-kb XbaI fragment of pSC132 were then ligated together to produce pSC133. This plasmid carries a single FRT site flanked by mariner arms, with a hemagglutinin epitope at the 3′ end of the FRT site.
PCR amplification of pBCMar-conditional using oligonucleotides oSC55 (5′ CGGGATCCGAAGTTCCTATTCCGAAGTTCCTATTCTCTAGAAAGTATAGGAACTTCGGCGCGCCTACCTGTGACGGAAGATCACT 3′) and oSC56 (5′ CGGGATCCGAAGTTCCTATACTTTCTAGAGAATAGGAACTTCGGAATAGGAACTTCATTTAAATGGCGCGCCTTACGCCCCGCCCTGCCACTC 3′) produced a chloramphenicol resistance allele flanked by directly repeated FRT sites, and this product was cloned into the SmaI site of pUC19 to create pSC136. Digestion of pSC136 with XbaI released a 932-bp fragment that was then cloned into pSC133 linearized by partial digestion with XbaI. The resulting plasmid (pSC137) carries a mariner transposon containing a chloramphenicol resistance allele flanked by directly repeated FRT sites. The 2.1-kb PstI/SacII fragment from pSC121.1 was subsequently cloned into the MluI site of pSC137 to create pSC138. The sequences of the FRT sites in pSC138 were verified.
Bacterial matings.
E. coli strain SM10 λ pir (42) was used as the donor strain for all matings. Fresh cultures of donor and recipient strains were washed once in Luria broth (LB), mixed together on L agar, and incubated at 37°C for 4 to 6 h.
Slide agglutination assay.
Bacterial cultures grown overnight at 37°C were mixed with an equal volume of V. cholerae anti-Ogawa or anti-Inaba typing serum (Difco, Inc., Detroit, Mich.) and scored visually for agglutination.
Electron microscopy.
Each sample was prepared by floating a carbon type A grid (300-mesh copper; Ted Pella, Inc., Redding, Calif.) on a 50-μl drop of an overnight bacterial culture for 5 min with the Formvar surface facing the drop. The grid was then transferred to a 50-μl drop of 0.5% (wt/vol) phosphotungstic acid (pH 6.5) for 30 s. Samples were viewed with a JEOL JEM-1200EX electron microscope at 60 kV.
Induction of FLP-mediated recombination.
Plasmids carrying the FLP recombinase gene (pCP20 and pSC141) were introduced into E. coli and V. cholerae strains by electroporation. E. coli was cultured overnight in LB containing chloramphenicol (20 μg/ml) and streptomycin (100 μg/ml). Cells from 0.5 ml of the culture were washed three times in 0.5 ml of sterile water and resuspended in 40 μl of sterile water prior to electroporation. For V. cholerae strains, overnight cultures were subcultured 1:1,000 in LB containing chloramphenicol (1 μg/ml) and streptomycin (100 μg/ml) and grown to mid-log phase at 37°C on a roller shaker. Cells from 1.5 ml of a mid-log-phase culture were washed three times in 1 ml of ice-cold 2 mM CaCl2 and then resuspended in 40 μl of ice-cold 2 mM CaCl2. Electroporation was carried out with a Bio-Rad Gene Pulser and Pulse Controller using cuvettes with a 0.1-cm (for E. coli) or a 0.2-cm (for V. cholerae) gap distance and the following settings: 1.8 kV, 25 mF, and 200 Ω (Bio-Rad Laboratories, Inc., Hercules, Calif.). Cells were allowed to recover at 30°C (for 1 h with agitation for E. coli and for 2 h without agitation for V. cholerae), plated on L agar containing ampicillin (100 μg/ml), and grown overnight at 30°C. A single isolate from each electroporation was then streaked on L agar containing streptomycin (100 μg/ml) and grown overnight at 37°C. Colonies from these restreaks were screened for chloramphenicol and ampicillin sensitivity by patching.
Infant mouse colonization assay.
Colonization assays were done as described previously (9), with minor modifications. Strains SC631 and SC632 were grown overnight at 37°C in LB containing streptomycin (100 μg/ml). Bacteria were pelleted in a microcentrifuge, washed once in 1 volume of LB, resuspended in 1 volume of LB, and mixed with 10 μl of blue food dye per ml of bacterial suspension. For the Peru-15 colonization assay, lyophilized vaccine obtained from D. N. Taylor (U.S. Army Medical Research Institute for Infectious Diseases) was reconstituted with sterile water and 1 ml of this reconstituted vaccine was mixed with 10 μl of blue food dye. Each inoculum was administered perorally to 6-day-old CD1 mice (Charles River, Inc., Wilmington, Mass.) at a dose of 50 μl per mouse and plated at various dilutions on L agar containing streptomycin (100 μg/ml) to determine the number of CFU present in the inoculum. The small bowel of each mouse was recovered 20 to 24 h later, homogenized in 5 ml of LB, and plated at various dilutions on L agar containing streptomycin (100 μg/ml) to determine the number of CFU present.
RESULTS
Complementation of Peru-15 to Ogawa+ by the rfbT allele of E7946.
Earlier work demonstrated that the rfbT gene alone is sufficient to convert V. cholerae Inaba strains to Ogawa, and the transcriptional start site of rfbT has been mapped by primer extension (55). PCR primers were designed to include this start site and an additional 100 bp of the 5′ flanking sequence. After amplification of the rfbT gene from V. cholerae strain E7946 (El Tor, Ogawa), the product was cloned into pCR2.1 and the resulting plasmid, pSC121.1, was introduced into V. cholerae strain Peru-15 (33) by electroporation. The presence of pSC121.1 rendered Peru-15 agglutinable by anti-Ogawa typing serum but did not abolish the ability of the strain to be agglutinated by anti-Inaba typing serum.
Construction of a mariner transposon vector for delivery of rfbT.
The construction of pSC138 is described in Fig. 1 and Materials and Methods. The mariner transposon on this plasmid (TnFC-rfbT) consists of a chloramphenicol resistance allele flanked by directly repeated FRT sites and the rfbT gene from pSC121.1. Although the rfbT gene is presumed to possess its own promoter, the gene is oriented such that its expression can be driven by a promoter adjacent to a transposon insertion. pSC138 also carries the gene encoding the Himar1 transposase, an oriR6K origin of replication, and the RP4 origin of transfer.
FIG. 1.
Construction of pSC138. Abbreviations: Ap, ampicillin resistance; Cm, chloramphenicol resistance; Km, kanamycin resistance; R6K, oriR6K conditional origin of replication; RP4, origin of transfer; tnp, transposase; HA, influenza virus hemagglutinin epitope.
Isolation and characterization of nonmotile Ogawa+ Peru-2 transposon mutants.
The motile V. cholerae strain Peru-2 (Roberts et al., Proc. 28th Joint Conf. U.S.-Japan Coop. Med. Sci. Program Cholera Relat. Diarrheal Dis.) was mutagenized with TnFC-rfbT by introducing pSC138 into Peru-2 by plate mating. The mating was then scraped into 50 ml of LB containing chloramphenicol (1 μg/ml) and streptomycin (150 μg/ml) and grown overnight at 37°C on a platform shaker. A 1-ml sample of a 1:1,000 dilution of this culture was added to 500 ml of 0.4% motility agar containing chloramphenicol (1 μg/ml) and streptomycin (100 μg/ml) and poured into petri dishes. After overnight growth at 37°C, putative nonmotile bacteria were picked and restabbed into motility agar for verification of their phenotype.
Two of 22 nonmotile isolates tested by slide agglutination were positive for expression of Ogawa antigen. Both isolates were ampicillin sensitive, indicating that the donor plasmid had not been retained. Electron microscopy (data not shown) demonstrated that NM3 and NM11 were aflagellar, and both were nonagglutinable by anti-Inaba typing serum. To determine the locations of the transposons in NM3 and NM11, the insertion junctions were cloned into pNEB193 and sequenced. The insertions were independent, but both occurred in a gene that is predicted to encode the flagellar hook protein FlgE. rfbT and flgE are oriented in the same direction in both strains.
FLP-mediated loss of chloramphenicol resistance.
The temperature-sensitive plasmid pCP20 expresses the FLP recombinase under the control of the λ pR promoter and the λ cI857 repressor (8), and the ability of pCP20 to mediate excision of the FRT-Cmr-FRT cassette was confirmed as described in Materials and Methods using SC625, an E. coli strain harboring a TnFC-rfbT insertion. However, pSC101 derivatives replicate poorly, if at all, in V. cholerae (J.J.M., unpublished data) and all attempts to introduce pCP20 into NM3 and NM11 by electroporation were unsuccessful. Therefore, pCP20 and pBR322 were linearized with PstI and ligated together to create a replicon fusion (pSC141) that could be maintained in NM3 and NM11 in the presence of ampicillin. Induction of FLP expression from pSC141 was successful and resulted in the isolation of chloramphenicol-sensitive derivatives of NM3 and NM11. Analysis of these strains (SC631 and SC632) demonstrated that they were Ogawa+, nonmotile, aflagellar, and Inaba−. Both were also ampicillin sensitive, indicating that pSC141 can be cured easily in the absence of ampicillin selection.
Colonization ability of SC631 and SC632.
Since colonization may be critical for development of a protective immune response, SC631 and SC632 were examined for colonization ability using the suckling mouse model. The results (Table 2) demonstrate that both strains are competent for colonization of infant mice, although at slightly reduced levels compared to Peru-2 (6) and Peru-15.
TABLE 2.
Colonization data for SC631, SC632, and Peru-15
| Straina and mouse no. | Total no. of CFU in intestine |
|---|---|
| SC631 | |
| 1 | 5.0 × 104 |
| 2 | 8.0 × 103 |
| 3 | 3.6 × 105 |
| 4 | 6.0 × 104 |
| 5 | 8.7 × 104 |
| 6 | 3.0 × 105 |
| 7 | 6.4 × 104 |
| SC632 | |
| 1 | 9.1 × 104 |
| 2 | 1.5 × 105 |
| 3 | 0 |
| 4 | 2.0 × 103 |
| 5 | 4.0 × 103 |
| 6 | 2.0 × 104 |
| 7 | 1.3 × 105 |
| Peru-15 | |
| 1 | 2.0 × 105 |
| 2 | 6.3 × 104 |
| 3 | 0 |
| 4 | 4.3 × 107 |
| 5 | 0 |
| 6 | 4.4 × 104 |
| 7 | 2.4 × 107 |
| 8 | 2.4 × 108 |
| 9 | 0 |
Input numbers of bacteria per mouse: SC631, 8.0 × 107 CFU; SC632, 3.8 × 106 CFU; Peru-15, 5.0 × 106 CFU.
To determine the stability of the Ogawa+ LPS phenotype during infection, four postinfection isolates were chosen for each strain, with each isolate obtained from a different mouse. All eight isolates were agglutinable by anti-Ogawa typing serum but not by anti-Inaba typing serum. In addition, the motility phenotypes of 16 postinfection isolates of each strain were assessed by stabbing into motility agar and all postinfection isolates were found to be nonmotile. These data provide evidence that the rfbT insertions in SC631 and SC632 are stable during infection.
DISCUSSION
This report describes the use of transposon delivery of the rfbT gene to obtain nonmotile, Ogawa+ derivatives of V. cholerae strain Peru-2 (Fig. 2). The two strains thus isolated carried independent insertions in flgE, which is predicted to encode the flagellar hook protein. FLP-mediated recombination was subsequently used to remove the chloramphenicol resistance marker from the chromosomal insertions. These nonmotile, Ogawa+, chloramphenicol-sensitive strains are competent for colonization as assessed in the suckling mouse model, and they may therefore be suitable as vaccine candidates either independently or in combination with other vaccine strains.
FIG. 2.
Diagram of construction of nonmotile, Ogawa+ strains using TnFC-rfbT.
The rfbT allele complements Peru-15 to Ogawa when present on the multicopy plasmid pSC121.1, but it generally does not create the Ogawa phenotype in Peru-2 when inserted into the chromosome in single copy. This indicates that single-copy expression of rfbT from its own promoter is insufficient to convert a strain to Ogawa and that it was necessary to place rfbT under the control of a chromosomal promoter in order to achieve serotype conversion. Evidence supporting this hypothesis is provided by the fact that the two insertions leading to an Ogawa phenotype occurred such that the rfbT gene was oriented in the same direction as the gene into which it was inserted.
There are approximately 50 motility genes in E. coli (39) and a comparable number of proteins in the V. cholerae genome that are predicted to be involved in flagellar function (The Institute for Genomic Research, http://www.tigr.org). Although only 22 nonmotile mutants were screened for the Ogawa phenotype, the low site specificity of mariner transposons makes it somewhat surprising that the two Ogawa+ isolates had independent insertions in flgE. The expression level of flgE relative to those of other V. cholerae motility genes is not known, but these data suggest that flgE-rfbT fusions result in appropriate levels of rfbT expression for conversion to Ogawa while fusions to other motility genes do not. This illustrates one advantage of using such a promoter trap strategy for heterologous gene expression. So long as there is a relatively simple assay for expression of the introduced gene, the empirical approach of generating a bank of transposon insertions and subsequently screening for strains displaying the desired traits may, in fact, be more effective than attempting to decide a priori which promoters or insertion sites might result in optimal levels of gene expression. It should, in certain instances, be possible to enrich or even select for strains that demonstrate the phenotype of interest.
The mariner-FRT system should be particularly useful for the construction of vaccine strains expressing specific antigens. FLP-mediated removal of antibiotic markers is simple and effective, and mariner-derived delivery vectors are especially attractive because of their low site specificity and broad host range. They are active not only in gram-positive and gram-negative bacteria but also in several eukaryotic organisms (18, 21, 36–38, 50, 52, 54, 66). This promiscuity could provide huge advantages in bacteria where there are no existing transposition systems (e.g., Borrelia spp.) or where current transposition systems demonstrate high site specificity (e.g., mycobacteria and gram-positive organisms).
The vaccine potential of the aflagellar, Ogawa+ strains SC631 and SC632 remains to be determined. Peru-2 itself has not been tested for efficacy as a cholera vaccine, but several of its derivatives (Peru-3, -14, and -15) have been shown to elicit strong and, in some cases, protective immune responses against V. cholerae in human subjects (33, 60). Since Peru-14 and Peru-15 are motility deficient and exhibit lower reactogenicity than motile strains, it seems not unreasonable to expect that nonmotile strains SC631 and SC632 will also demonstrate low reactogenicity. One important advantage of pursuing vaccine development with SC631 and SC632 is that Peru-14 and Peru-15 were isolated as spontaneous nonmotile mutants, and the molecular basis of their nonmotility is unknown. The fact that Peru-14 shows reversion to motility upon passaging (33) emphasizes the need for vaccine strains with defined motility defects.
Antibacterial immunity is thought to play the dominant role in protection against cholera, but the importance of antitoxic immunity was clearly demonstrated in a field trial in Bangladesh involving 89,000 persons. Vaccination with an oral B-subunit whole-cell vaccine provided better protection against cholera than oral whole-cell vaccine alone, although the increased efficacy of the B-subunit whole-cell preparation was evident only in the first 8 to 12 months after immunization (11, 12, 23). In order to promote a good immune response against cholera toxin, most of the Peru vaccine strains contain the ctxB gene under the control of the in vivo-inducible htpG promoter inserted into the recA locus (46, 52). It should be relatively simple to introduce the recA::htpG-ctxB mutation into SC631 and SC632, and this work is already under way. Once this is accomplished, it will be of great interest to determine the ability of those strains to stimulate long-lived immunity to cholera in human volunteers.
ACKNOWLEDGMENTS
We thank B. Akerley and E. Rubin for many helpful suggestions and M. Ericsson for assistance with the electron microscopy.
Sequencing of the V. cholerae genome was accomplished with support from the National Institute of Allergy and Infectious Diseases. This work was supported by National Institutes of Health grant AI26289 (to J.J.M.).
REFERENCES
- 1.Aidara A, Koblavi S, Boye C S, Raphenon G, Gassama A, Grimont F, Grimon P A. Phenotypic and genotypic characterization of Vibrio cholerae isolates from a recent cholera outbreak in Senegal: comparison with isolates from Guinea-Bissau. Am J Trop Med Hyg. 1998;58:163–167. doi: 10.4269/ajtmh.1998.58.163. [DOI] [PubMed] [Google Scholar]
- 2.Albert M J, Siddique A K, Islam M S, Faruque A S G, Ansaruzzaman M, Faruque S M, Sack R B. Large outbreak of clinical cholera due to Vibrio cholerae non-O1 in Bangladesh. Lancet. 1993;341:704. doi: 10.1016/0140-6736(93)90481-u. [DOI] [PubMed] [Google Scholar]
- 3.Ausubel F M, Brent R, Kingston R E, Moore D E, Seidman J G, Smith J A, Struhl K, editors. Current protocols in molecular biology. New York, N.Y: John Wiley & Sons, Inc.; 1995. [Google Scholar]
- 4.Barua D. History of cholera. In: Barua D, Greenough III W B, editors. Cholera. New York, N.Y: Plenum Publishing Corporation; 1992. pp. 1–36. [Google Scholar]
- 5.Bennish M L. Cholera: pathophysiology, clinical features, and treatment. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 229–255. [Google Scholar]
- 6.Butterton J R, Beattie D T, Gardel C L, Carroll P A, Hyman T, Killeen K P, Mekalanos J J, Calderwood S B. Heterologous antigen expression in Vibrio cholerae vector strains. Infect Immun. 1995;63:2689–2696. doi: 10.1128/iai.63.7.2689-2696.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cash R A, Music S I, Libonati J P, Snyder M J, Wenzel R P, Hornick R B. Response of man to infection with Vibrio cholerae. I. Clinical, serologic, and bacteriologic responses to a known inoculum. J Infect Dis. 1974;129:45–52. doi: 10.1093/infdis/129.1.45. [DOI] [PubMed] [Google Scholar]
- 8.Cherepanov P P, Wackernagel W. Gene disruption in Escherichia coli: TcR and KmR cassettes with the option of Flp-catalyzed excision of the antibiotic-resistance determinant. Gene. 1995;158:9–14. doi: 10.1016/0378-1119(95)00193-a. [DOI] [PubMed] [Google Scholar]
- 9.Chiang S L, Taylor R K, Koomey M, Mekalanos J J. Single amino acid substitutions in the N-terminus of Vibrio cholerae TcpA affect colonization, autoagglutination, and serum resistance. Mol Microbiol. 1995;17:1133–1142. doi: 10.1111/j.1365-2958.1995.mmi_17061133.x. [DOI] [PubMed] [Google Scholar]
- 10.Clark C G, Kravetz A N, Alekseenko V V, Krendelev Y D, Johnson W M. Microbiological and epidemiological investigation of cholera epidemic in Ukraine during 1994 and 1995. Epidemiol Infect. 1998;121:1–13. doi: 10.1017/s0950268898008711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clemens J, Sack D, Harris J R, Chakraborty J, Khan M R, Stanton B F, Kay B, Khan M U, Yunus M, Svennerholm A-M, Holmgren J. Field trial of oral cholera vaccines in Bangladesh. Lancet. 1986;i:124–127. doi: 10.1016/s0140-6736(86)91944-6. [DOI] [PubMed] [Google Scholar]
- 12.Clemens J D, Sack D A, Harris J R, Van Loon F, Chakraborty J, Ahmed F, Rao M R, Khan M R, Yunus M, Huda N. Field trial of oral cholera vaccines in Bangladesh: results from three-year follow-up. Lancet. 1990;335:270–273. doi: 10.1016/0140-6736(90)90080-o. [DOI] [PubMed] [Google Scholar]
- 13.Coster T S, Killeen K P, Waldor M K, Beattie D, Spriggs D, Kenner J R, Trofa A, Sadoff J, Mekalanos J J, Taylor D N. Safety, immunogenicity and efficacy of a live attenuated Vibrio cholerae O139 vaccine protype, Bengal-15. Lancet. 1995;345:949–952. doi: 10.1016/s0140-6736(95)90698-3. [DOI] [PubMed] [Google Scholar]
- 14.Cox M M. The FLP protein of the yeast 2mm plasmid: expression of a eukaryotic genetic recombination system in Escherichia coli. Proc Natl Acad Sci USA. 1983;80:4223–4227. doi: 10.1073/pnas.80.14.4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cox M M. FLP site-specific recombination system of Saccharomyces cerevisiae. In: Kucherlapati R, Smith G R, editors. Genetic recombination. Washington, D.C.: American Society for Microbiology; 1988. pp. 429–443. [Google Scholar]
- 16.Dalsgaard A, Forslund A, Bodhidatta L, Serichantalergs O, Pitarangsi C, Pang L, Shimada T, Echeverria P. A high proportion of Vibrio cholerae strains isolated from children with diarrhoea in Bangkok, Thailand, are multiple antibiotic resistant and belong to heterogenous non-O1, non-O139 O-serotypes. Epidemiol Infect. 1999;122:217–226. doi: 10.1017/s0950268899002137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalsgaard A, Skov M N, Serichantalergs O, Echeverria P, Meza R, Taylor D N. Molecular evolution of Vibrio cholerae O1 strains isolated in Lima, Peru, from 1991 to 1995. J Clin Microbiol. 1997;35:1151–1156. doi: 10.1128/jcm.35.5.1151-1156.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fadool J M, Hartl D L, Dowling J E. Transposition of the mariner element from Drosophila mauritiana in zebrafish. Proc Natl Acad Sci USA. 1998;95:5182–5186. doi: 10.1073/pnas.95.9.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glass R I, Black R E. The epidemiology of cholera. In: Barua D, Greenough W B D, editors. Cholera. New York, N.Y: Plenum Publishing Corporation; 1992. pp. 129–154. [Google Scholar]
- 20.Greenough W B D. Vibrio cholerae and cholera. In: Mandell G L, Bennett J E, Dolin R, editors. Principles and practice of infectious diseases. 4th ed. Vol. 2. New York, N.Y: Churchill Livingstone; 1995. pp. 1934–1945. [Google Scholar]
- 21.Gueiros-Filho F J, Beverley S M. Trans-kingdom transposition of the Drosophila element mariner within the protozoan Leishmania. Science. 1997;276:1716–1719. doi: 10.1126/science.276.5319.1716. [DOI] [PubMed] [Google Scholar]
- 22.Hoge C W, Bodhidatta L, Echeverria P, Deesuwan M, Kitporka P. Epidemiological study of Vibrio cholerae O1 and O139 in Thailand: at the advancing edge of the eighth pandemic. Am J Epidemiol. 1996;143:263–268. doi: 10.1093/oxfordjournals.aje.a008737. [DOI] [PubMed] [Google Scholar]
- 23.Holmgren J, Osek J, Svennerholm A-M. Protective oral cholera vaccine based on a combination of cholera toxin B subunit and inactivated cholera vibrios. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 415–424. [Google Scholar]
- 24.Holmgren J, Svennerholm A-M. Cholera and the immune response. Prog Allergy. 1983;33:106–119. [PubMed] [Google Scholar]
- 25.Huang L C, Wood E A, Cox M M. Convenient and reversible site-specific targeting of exogenous DNA into a bacterial chromosome by use of the FLP recombinase: the FLIRT system. J Bacteriol. 1997;179:6076–6083. doi: 10.1128/jb.179.19.6076-6083.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Israil A, Nacescu N, Cedru C L, Ciufecu C, Damian M. Changes in Vibrio cholerae O1 strains isolated in Romania during 1977–95. Epidemiol Infect. 1998;121:253–258. doi: 10.1017/s0950268896001100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson J A, Salles C A, Panigrahi P, Albert M J, Wright A C, Johnson R J, Morris J G., Jr Vibrio cholerae O139 synonym Bengal is closely related to Vibrio cholerae El Tor but has important differences. Infect Immun. 1994;62:2108–2110. doi: 10.1128/iai.62.5.2108-2110.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Judson N, Mekalanos J J. TnAraOut, a transposon-based approach to identify and characterize essential bacterial genes. Nat Biotechnol. 2000;18:740–745. doi: 10.1038/77305. [DOI] [PubMed] [Google Scholar]
- 29.Kaper J B, Fasano A, Trucksis M. Toxins of Vibrio cholerae. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 145–176. [Google Scholar]
- 30.Kaper J B, Morris J G, Levine M M. Cholera. Clin Microbiol Rev. 1995;8:48–86. doi: 10.1128/cmr.8.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaur H, Lal M. Typing and antibiotic susceptibility patterns of Vibrio cholerae during six consecutive cholera seasons in north India. Trop Gastroenterol. 1998;19:59–61. [PubMed] [Google Scholar]
- 32.Kay B A, Bopp C A, Wells J G. Isolation and identification of Vibrio cholerae O1 from fecal specimens. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 3–25. [Google Scholar]
- 33.Kenner J, Coster T, Trofa A, Taylor D, Barrera-Oro M, Hyman T, Adams J, Beattie D, Killeen K, Mekalanos J J, Sadoff J C. Peru-15, an improved live, attenuated oral vaccine candidate for Vibrio cholerae O1. J Infect Dis. 1995;172:1126–1129. doi: 10.1093/infdis/172.4.1126. [DOI] [PubMed] [Google Scholar]
- 34.Levine M M, Kaper J B, Herrington D, Losonsky G, Morris J G, Clements M, Black R E, Tall B, Hall R. Volunteer studies of deletion mutants of Vibrio cholerae O1 prepared by recombinant techniques. Infect Immun. 1988;56:161–167. doi: 10.1128/iai.56.1.161-167.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levine M M, Pierce N F. Immunity and vaccine development. In: Barua D, Greenough III W B, editors. Cholera. New York, N.Y: Plenum; 1992. pp. 285–328. [Google Scholar]
- 36.Lidholm D A, Lohe A R, Hartl D L. The transposable element mariner mediates germline transformation in Drosophila melanogaster. Genetics. 1993;134:859–868. doi: 10.1093/genetics/134.3.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Loukeris T G, Livadaras I, Arca B, Zabalou S, Savakis C. Gene transfer into the medfly, Ceratitis capitata, with a Drosophila hydei transposable element. Science. 1995;270:2002–2005. doi: 10.1126/science.270.5244.2002. [DOI] [PubMed] [Google Scholar]
- 38.Lozovskaya E R, Nurminsky D I, Hartl D L, Sullivan D T. Germline transformation of Drosophila virilis mediated by the transposable element hobo. Genetics. 1996;142:173–177. doi: 10.1093/genetics/142.1.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macnab R M. Flagella and motility. In: Neidhardt F C, Curtiss R, Ingraham J L, Lin E C C, Low K B, Magasanik B, Reznikoff W S, Riley M, Schaechter M, Umbarger H E, editors. Escherichia coli and Salmonella: cellular and molecular biology. 2nd ed. Vol. 1. Washington, D.C.: ASM Press; 1996. pp. 123–145. [Google Scholar]
- 40.Mahalanabis D, Molla A M, Sack D A. Clinical management of cholera. In: Barua D, Greenough III W B, editors. Cholera. New York, N.Y: Plenum Publishing Corporation; 1992. pp. 253–283. [Google Scholar]
- 41.Manning P A, Stroeher U H, Morona R. Molecular basis for O-antigen biosynthesis in Vibrio cholerae O1: Ogawa-Inaba switching. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 77–94. [Google Scholar]
- 42.Miller V L, Mekalanos J J. A novel suicide vector and its use in construction of insertion mutations: osmoregulation of outer membrane proteins and virulence determinants in Vibrio cholerae requires toxR. J Bacteriol. 1988;170:2575–2583. doi: 10.1128/jb.170.6.2575-2583.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mintz E D, Popovic T, Blake P A. Transmission of Vibrio cholerae O1. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 345–356. [Google Scholar]
- 44.Mosley W H, Woodward W E, Aziz K M A, Rhaman M A S M, Chowdhury A K M A, Ahmed A, Feeley J C. The 1968–1969 cholera vaccine field trial in rural East Pakistan. Effectiveness of monovalent Ogawa and Inaba vaccines and a purified Inaba antigen, with comparative results of serological and animal protection tests. J Infect Dis. 1970;121:471–479. doi: 10.1093/infdis/121.supplement.s1. [DOI] [PubMed] [Google Scholar]
- 45.Nizami S Q, Farooqui B J. Cholera in children in Karachi from 1990 through 1995: a study of cases admitted to a tertiary care hospital. J Pak Med Assoc. 1998;48:171–173. [PubMed] [Google Scholar]
- 46.Parsot C, Mekalanos J J. Expression of ToxR, the transcriptional activator of the virulence factors in Vibrio cholerae, is modulated by the heat shock response. Proc Natl Acad Sci USA. 1990;87:9898–9902. doi: 10.1073/pnas.87.24.9898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quiding M, Nordstrom I, Kilander A, Andersson G, Hanson L A, Holmgren J, Czerkinsky C. Intestinal immune responses in humans. Oral cholera vaccination induces strong intestinal antibody responses and interferon-gamma production and evokes local immunological memory. J Clin Investig. 1991;88:143–148. doi: 10.1172/JCI115270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Radhakutty G, Sircar B K, Mondal S K, Mukhopadhyay A K, Mitra R K, Basu A, Ichhpujani R L, Nair G B, Bhattacharya S K. Investigation of the outbreak of cholera in Alleppey & Palghat districts, south India. Indian J Med Res. 1997;106:455–457. [PubMed] [Google Scholar]
- 49.Ramamurthy T, Garg S, Sharma R, Bhattacharya S K, Nair G B, Shimada T, Takeda T, Karasawa T, Kurazano H, Pal A, Takeda Y. Emergence of novel strain of Vibrio cholerae with epidemic potential in southern and eastern India. Lancet. 1993;341:703–704. doi: 10.1016/0140-6736(93)90480-5. [DOI] [PubMed] [Google Scholar]
- 50.Raz E, van Luenen H G, Schaerringer B, Plasterk R H A, Driever W. Transposition of the nematode Caenorhabditis elegans Tc3 element in the zebrafish Danio rerio. Curr Biol. 1998;8:82–88. doi: 10.1016/s0960-9822(98)70038-7. [DOI] [PubMed] [Google Scholar]
- 51.Ries A A, Vugia D J, Beingolea L, Palacios A M, Vasquez E, Wells J G, Garcia Baca N, Swerdlow D L, Pollack M, Bean N H, et al. Cholera in Piura, Peru: a modern urban epidemic. J Infect Dis. 1992;166:1429–1433. doi: 10.1093/infdis/166.6.1429. [DOI] [PubMed] [Google Scholar]
- 52.Rubin R J, Akerley B J, Novik V N, Lampe D J, Husson R N, Mekalanos J J. In vivo transposition of mariner-based elements in enteric bacteria and mycobacteria. Proc Natl Acad Sci USA. 1999;96:1645–1650. doi: 10.1073/pnas.96.4.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sakazaki R. Bacteriology of Vibrio and related organisms. In: Barua D, Greenough III W B, editors. Cholera. New York, N.Y: Plenum Publishing Corporation; 1992. pp. 37–55. [Google Scholar]
- 54.Scott J R, Churchward G G. Conjugative transposition. Annu Rev Microbiol. 1995;49:367–397. doi: 10.1146/annurev.mi.49.100195.002055. [DOI] [PubMed] [Google Scholar]
- 55.Stroeher U H, Karageorgos L E, Morona R, Manning P A. Serotype conversion in Vibrio cholerae O1. Proc Natl Acad Sci USA. 1992;89:2566–2570. doi: 10.1073/pnas.89.7.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Svennerholm A-M, Jonson G, Holmgren J. Immunity to Vibrio cholerae infection. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 257–272. [Google Scholar]
- 57.Swerdlow D L, Mintz E D, Rodriguez M, Tejada E, Ocampo C, Espejo L, Greene K D, Saldana W, Seminario L, Tauxe R V, et al. Waterborne transmission of epidemic cholera in Trujillo, Peru: lessons for a continent at risk. Lancet. 1992;340:28–33. doi: 10.1016/0140-6736(92)92432-f. [DOI] [PubMed] [Google Scholar]
- 58.Tacket C O, Losonsky G, Nataro J P, Cryz S J, Edelman R, Fasano A, Michalski J, Kaper J B, Levine M M. Safety, immunogenicity, and transmissibility of live oral cholera vaccine candidate CVD112, a DctxA Dzot Dace derivative of El Tor Ogawa Vibrio cholerae. J Infect Dis. 1993;168:1536–1540. doi: 10.1093/infdis/168.6.1536. [DOI] [PubMed] [Google Scholar]
- 59.Tauxe R, Seminario L, Tapia R, Libel M. The Latin American epidemic. In: Wachsmuth I K, Blake P A, Olsvik Ø, editors. Vibrio cholerae and cholera: molecular to global perspectives. Washington, D.C.: ASM Press; 1994. pp. 321–344. [Google Scholar]
- 60.Taylor D N, Killeen K P, Hack D C, Kenner J R, Coster T S, Beattie D T, Ezzell J, Hyman T, Trofa A, Sjogren M H, Friedlander A, Mekalanos J J, Sadoff J C. Development of a live, oral, attenuated vaccine against El Tor cholera. J Infect Dis. 1994;170:1518–1523. doi: 10.1093/infdis/170.6.1518. [DOI] [PubMed] [Google Scholar]
- 61.Taylor D N, Sanchez J L, Castro J M, Lebron C, Parrado C M, Johnson D E, Tacket C O, Losonsky G A, Wasserman S S, Levine M M, Cryz S J. Expanded safety and immunogenicity of a bivalent, oral, attenuated cholera vaccine, CVD 103-HgR plus CVD 111, in United States military personnel stationed in Panama. Infect Immun. 1999;67:2030–2034. doi: 10.1128/iai.67.4.2030-2034.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vugia D J, Rodriguez M, Vargas R, Ricse C, Ocampo C, Llaque R, Seminario J L, Greene K D, Tauxe R V, Blake P A. Epidemic cholera in Trujillo, Peru, 1992: utility of a clinical case definition and shift in Vibrio cholerae O1 serotype. Am J Trop Med Hyg. 1994;50:566–569. doi: 10.4269/ajtmh.1994.50.566. [DOI] [PubMed] [Google Scholar]
- 63.Wachsmuth I K, Evins G M, Fields P I, Olsvik Ø, Popovic T, Bopp C A, Wells J G, Carrillo C, Blake P A. The molecular epidemiology of cholera in Latin America. J Infect Dis. 1993;167:621–626. doi: 10.1093/infdis/167.3.621. [DOI] [PubMed] [Google Scholar]
- 64.Waldor M K, Colwell R, Mekalanos J J. The Vibrio cholerae O139 serogroup antigen includes O-antigen capsule and lipopolysaccharide virulence determinants. Proc Natl Acad Sci USA. 1994;91:11388–11392. doi: 10.1073/pnas.91.24.11388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.World Health Organization. Cholera in 1997. Weekly Epidemiol Rep. 1998;73:201–208. [Google Scholar]
- 66.Zhang L, Sankar U, Lampe D J, Robertson H M, Graham F L. The Himar1 mariner transposase cloned in a recombinant adenovirus vector is functional in mammalian cells. Nucleic Acids Res. 1998;26:3687–3693. doi: 10.1093/nar/26.16.3687. [DOI] [PMC free article] [PubMed] [Google Scholar]