Abstract
Between 2010 and 2021, the annual prevalence of nontuberculous mycobacterial (NTM) diseases in South Korea increased from 11.4 to 56.7 cases per 100 000 population. Prevalence in the population aged ≥65 years quadrupled from 41.9 to 163.1 cases per 100 000 population. Accordingly, the overall cost associated with NTM diseases increased.
Keywords: epidemiology, expenditure, Mycobacterium abscessus, Mycobacterium avium, prevalence
Nontuberculous mycobacteria (NTM) are ubiquitous, opportunistic pathogens that commonly manifest as chronic pulmonary disease (PD), which accounts for 90% of all NTM-related diseases [1]. The incidence and prevalence of NTM diseases are increasing worldwide, partly due to a growing susceptible population as a result of the use of immunosuppressive agents, solid organ transplantation, aging, alterations in the environment favoring pathogen growth and increased interaction with human hosts, and diminished antimycobacterial immunity following the fall in tuberculosis (TB) cases [2–4]. The increasing number of patients and low rate of successful treatment mean that the socioeconomic burden of NTM diseases is expected to rise. Here, we examined existing national health insurance data to determine the prevalence and related costs of NTM diseases in South Korea between 2010 and 2021.
METHODS
Approximately 97.1% of the population in South Korea (51.4 million persons) is covered by the National Health Insurance Service (NHIS), a universal, government-run, single-payer health care system [5]. To be reimbursed for the medical services provided, health care providers submit claims data to the Health Insurance Review and Assessment Service (HIRA). We searched the HIRA's nationwide claims database [6] using International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10), diagnostic codes related to NTM diseases, including NTM-PD (A31) [7] and both pulmonary and extrapulmonary TB (A15, A17, A18, A19) [8], to gather information on the volume of patients, health care utilization, and associated direct medical expenditure.
We calculated the annual crude prevalence of NTM and TB diseases after obtaining data on the total population for each year from the Statistics Korea database [9]. Overall, the study period prevalence of NTM diseases by age group was estimated and presented by sex. We calculated the direct medical expenditure associated with NTM and presented it by age group after evaluating claims data for medical practices, both inpatient and outpatient, with NTM as the primary diagnostic code. We also determined the annual crude prevalence and direct medical expenditure incurred by patients aged 65 years or older.
More specifically, direct medical expenditure was defined as any cost claimed by health care providers and pharmacies that was directly related to the use of health care intervention and drugs due to illness. Direct medical expenditure is presented in Korean Republic Won (KRW) and United States dollars (USD) based on the 2021 exchange rate (1 KRW ≈ 0.00084 USD).
Patient Consent
As we used deidentified data collected from a publicly accessible database, neither patient consent nor institutional review board approval was necessary.
RESULTS
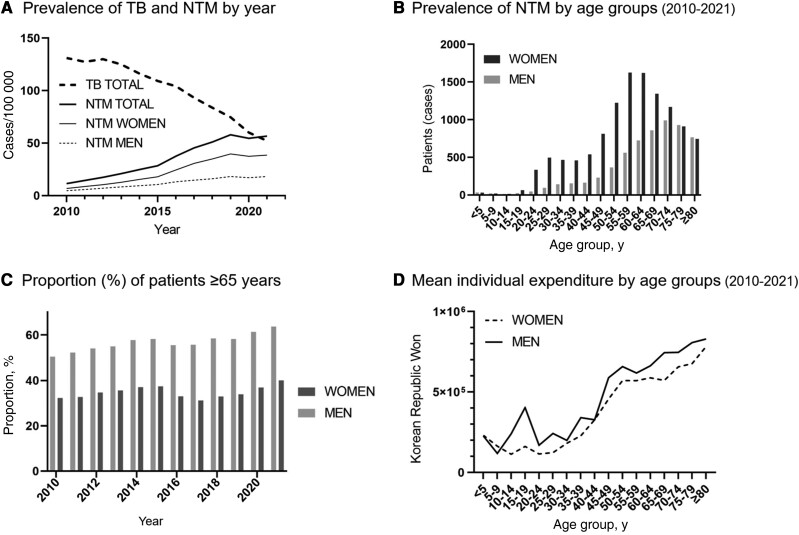
The annual crude prevalence of NTM diseases increased from 11.4 cases/100 000 population in 2010 to 56.7 cases/100 000 population in 2021. Except for 2020, the annual crude prevalence was higher than the preceding year. In fact, it surpassed the prevalence of TB in 2021, which fell from 131.1 cases/100 000 population to 52.1 cases/100 000 population within the same time period (Figure 1A). Overall between 2010 and 2021, the number of female NTM patients peaked in the age range of 55–59 years, whereas male NTM patients peaked in the age range of 70–74 years (Figure 1B). During the same period, the annual crude prevalence of NTM diseases in the population aged 65 years or older quadrupled from 41.9 cases/100 000 population to 163.1 cases/100 000 population. The proportion of patients aged 65 years or older increased from 39.6% in 2010 (men, 50.4%; women 32.7%) to 47.6% in 2021 (men, 63.7%; women, 40.0%), and this was particularly significant in the male population (Ptrend < .001) (Figure 1C).
Figure 1.
The epidemiology and direct medical expenditure associated with NTM diseases in South Korea between 2010 and 2021. (A) Prevalence of TB and NTM by year. (B) Prevalence of NTM by age groups (2010–2021). (C) Proportion (%) of patients ≥65 years. (D) Mean individual expenditure by age groups (2010–2021). Abbreviations: NTM, nontuberculous mycobacterial; TB, tuberculosis.
The annual direct expenditure related to NTM diseases expanded more than 5.8-fold, from 3.6 billion KRW (3 043 220 USD) in 2010 to 20.9 billion KRW (17 599 890 USD) in 2021, reflecting the trend in annual crude prevalence. For both men and women, mean individual direct expenditure of NTM diseases increased with age, peaking in the age range of 80 years or older (Figure 1D). Consequently, the proportion of annual direct medical expenditure incurred by patients aged 65 years or older increased from 47.1% in 2010 (men, 53.6%; women 41.5%) to 59.6% in 2021 (men, 71.6%; women 51.3%).
DISCUSSION
We investigated the annual crude prevalence and direct medical expenditure of NTM diseases in South Korea between 2010 and 2021 and compared them with those of TB. Overall, the prevalence of NTM diseases significantly increased with time, surpassing TB for the first time in 2021. The annual direct medical expenditure for NTM diseases has also risen over time, owing primarily to an increase in the proportion of older adult patients.
Unlike TB, which is required by Korean law to be reported at the time of diagnosis [10], there is no obligation to report NTM; hence its prevalence may have been underestimated. Even so, the annual prevalence of NTM diseases is consistently rising compared with a previous study conducted in South Korea with similar methodology that reported an annual prevalence of 39.6 cases/100 000 population in 2016 [2]. During the observation period, this number declined only once, in 2020, when the COVID-19 pandemic occurred. This may be a result of fewer patients seeking health care services due to the pandemic rather than a true decline in patients with NTM.
One of the most noticeable aspects of this study is a 20% increase in the proportion of patients aged 65 years or older. Because South Korea is expected to become a super-aged society by 2025, and 30% of the total population will be aged 65 years or older by 2035 [9, 11], this figure is likely to grow. More research and investment in the development of effective treatments are needed to adequately address this growing concern.
The direct medical expenditure for NTM diseases has increased 5.8 times within the past 12 years. This represents significant growth even considering the consumer price inflation rate, which was 18.7% overall during the same period [12]. Unfortunately, throughout this time period, no notable innovations or improvements in the management of NTM diseases occurred; hence, this increase can be attributed to the increase in prevalence.
Our study has several limitations. First, we were unable to distinguish NTM-PD from other forms of NTM diseases. Second, because we searched patients using diagnostic codes, the prevalence may have been overestimated. Third, we evaluated direct medical expenditures claimed by individual hospitals, clinics, and pharmacies to the HIRA and not the entire cost. Spending on unlisted drugs that are not reimbursed by the NHIS, as well as indirect costs, was outside the scope of this study.
In conclusion, between 2010 and 2021, the annual crude prevalence and direct medical expenditure of NTM diseases increased by 5 times and 5.8 times, respectively. Notably, the prevalence of NTM diseases in the older population quadrupled during this period. Therefore, national and global efforts to tackle NTM diseases, particularly among older adults, are urgently needed.
Acknowledgments
Financial support. None.
Author contributions. J.-Y.K.: conceptualization, methodology, data curation, formal analysis, writing—original draft, writing—review & editing; N.K.: methodology, writing—review & editing; J.-J.Y.: conceptualization, methodology, supervision, writing—review & editing.
Contributor Information
Joong-Yub Kim, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea.
Nakwon Kwak, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea.
Jae-Joon Yim, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea.
References
- 1. Griffith DE, Aksamit T, Brown-Elliott BA, et al. . An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 2007; 175:367–416. [DOI] [PubMed] [Google Scholar]
- 2. Lee H, Myung W, Koh WJ, Moon SM, Jhun BW. Epidemiology of nontuberculous mycobacterial infection, South Korea, 2007–2016. Emerg Infect Dis 2019; 25:569–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U. S. Medicare beneficiaries. Am J Respir Crit Care Med 2012; 185:881–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cowman S, van Ingen J, Griffith DE, Loebinger MR. Non-tuberculous mycobacterial pulmonary disease. Eur Respir J 2019; 54:1900250. [DOI] [PubMed] [Google Scholar]
- 5. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan 2009; 24:63–71. [DOI] [PubMed] [Google Scholar]
- 6. Healthcare Bigdata Hub . Health Insurance Review and Assessment Service. Available at: http://opendata.hira.or.kr/op/opc/olap3thDsInfo.do. Accessed September 1, 2022.
- 7. Winthrop KL, Marras TK, Adjemian J, Zhang H, Wang P, Zhang Q. Incidence and prevalence of nontuberculous mycobacterial lung disease in a large U.S. managed care health plan, 2008–2015. Ann Am Thorac Soc 2020; 17:178–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Tuberculosis (A15-A19) . ICD-10 Version: 2019. Available at: https://icd.who.int/browse10/2019/en#/A15-A19. Accessed September 1, 2022.
- 9.Statistics Korea. KOrean Statistical Information System (KOSIS) . Available at: https://kosis.kr/eng. Accessed September 1, 2022.
- 10. Cho KS. Tuberculosis control in the Republic of Korea. Epidemiol Health 2018; 40:e2018036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baek JY, Lee E, Jung HW, Jang IY. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res 2021; 25:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Statistics Korea. K-indicator . Available at: http://www.index.go.kr/. Accessed September 1, 2022.