Abstract
Introduction:
Patient groups who pose behavioral challenges during dental attendance may be offered more restricted dental treatment options. Unsuccessful participation with dental visit tasks and demands has been commonly reported for autistic children.
Objectives:
This study aimed to examine parental perceptions of difficulties associated with dental attendance and oral care for autistic children and young adults, to highlight reported challenges and potential adaptations, and to identify interventions that will encourage positive experiences of dental attendance.
Methods:
Qualitative data were gathered through 2 focus groups with parents of primary school and secondary school pupils with autism, interviewed in separate groups. Questions about parents’ perceptions of dental attendance and oral care were asked. The groups were audio-recorded and transcribed verbatim. The transcripts were analyzed and initial codes generated. Development of subthemes and themes followed a process of thematic analysis.
Results:
Parental perceptions, which confirmed data from other studies, included the need for understanding and training, awareness of sensory issues, recognition of the individuality of autistic traits, time and clarity for communication, and factors affecting the confidence of parents to advocate in the clinical environment. Focus group participants identified the critical value of empathizing with an autistic perspective and highlighted the importance of positive oral health messages. They also noted the lack of understanding regarding the complexity of altering self-imposed, ritualistic dietary regimes and attempting to enact good dental preventive habits for their children.
Conclusions:
Analysis of data from parent focus groups provided a greater understanding of the needs and responsivity required for successful dental visits for autistic children and young adults. A range of potential interventions was identified and incorporated within a model of needs. Interventions based on Partnership Working, System Change, and Training of Dental Staff could be effective in reducing challenges posed by dental attendance for many children with autism.
Knowledge Transfer Statement:
Sensory sensitivities, communication difficulties, comorbid intellectual disability, and dental anxiety are barriers to successful participation during dental attendance for autistic children. This research proposes that interventions supporting Partnership Working, System Change, and Training of Dental Staff can reduce challenges posed by dental attendance. The model of interventions developed as part of this project can be used by oral care teams to help reduce barriers and improve the success of dental visits for autistic children.
Keywords: autistic spectrum disorder, oral health, young person, dentistry, qualitative research, caregivers
Introduction
Oral diseases are among the most prevalent diseases globally, often reducing the quality of life for those affected (Peres et al., 2019). Oral diseases are largely preventable, with disparities in prevalence and outcomes often related to social determinants including special health care needs (Anders and Davis 2010; Watt et al. 2018). Data describing oral health outcomes in populations with special health care needs have frequently been gathered through research involving adults with intellectual disability (ID). The results suggest that the inability to positively participate with oral health care team requests is more likely to result in tooth extractions as a treatment, at an earlier age, even when dental caries rates are similar or lower than that of the general population (Gabre et al. 2001; Anders and Davis 2010; Mac Giolla Phadraig et al. 2015; Mac Giolla Phadraig et al. 2018).
Searching for evidence of disparity in dental outcomes and experience specifically associated with a diagnosis of autistic spectrum disorder (ASD) suggests autistic patient reliance on dental general anesthesia services (Mangione et al. 2020, Parry et al. 2021) and frequent use but less satisfaction with health services. A study specifically examining the experience of dental services revealed that autistic adults without ID more often felt forced to proceed with dental treatment they were not prepared for and recalled more painful dental experiences than a neurotypical control group (Blomqvist et al. 2014). A UK online survey reported significantly more negative overall experiences and lower satisfaction scores associated with dental communication, sensory sensitivities, and knowing what was going to happen at a dental visit from autistic adults without ID (McMillion et al. 2021). Although higher dental anxiety levels were reported in both studies, neither study specifically investigated a relationship between previous child oral health experience and current reported anxiety or interaction with dental services.
In the child population, the inability to engage with oral health team expectations, including refusal to open the mouth, screaming, and hitting/lashing out, have been found to be more common in children diagnosed with ASD (Stein et al. 2011; Barry et al. 2014). Sensory sensitivities as well as communication difficulties, comorbid ID, and dental fear and anxiety have been found to predict barriers to successful participation for children diagnosed with ASD during dental visits. These factors also complicate the delivery of oral self-care (Marshall et al. 2007; Weil and Inglehart 2012; Du et al. 2019). Difficulties with task engagement and unpredictable behavior have been cited by parents as barriers, which may be associated with unmet dental treatment need, for their children diagnosed with ASD (Lai et al. 2012; Barry et al. 2014; Du et al. 2019). The anxiety of dental staff regarding the treatment of children with ASD and absorption of parents with other urgent medical concerns have also been highlighted as barriers to dental care (Du et al. 2019).
Responsible and ethical health care delivery should aim to reduce oral health inequalities including barriers to accessing care (Peres and Heilmann 2015). Tackling obstacles and disparities in oral health for children and young adults (CYA) diagnosed with ASD requires understanding of these barriers and the difficulties faced by families and the dental team. A diagnosis of ASD for a child has been described by parents as a life-changing family event accompanied by feelings of despair, sadness, denial, confusion, and anger (Altiere and von Kluge 2009). However, research also demonstrates that parents recognize and are proud of the positive personality traits, strengths, and assets of their autistic children (Cost et al. 2021). Social skills, communication skills, self-care skills, and problem behavior are important treatment priorities for parents (Spann et al. 2003; Pituch et al. 2011).
Given the increased recognition of ASD and relatively high community prevalence (Matson and Kozlowski 2011), the oral health team should be prepared to encounter patients with ASD attending for oral health guidance and dental care provision. Strategies to promote oral health communication and encourage good oral habits from an early age are likely to yield the best outcomes for the individual and reduce health disparities and economic health care burden. For example, there is evidence that dental desensitization, stimulus-fading techniques, visual pedagogies, and social stories can increase participation with toothbrushing programs for autistic children (Bishop et al. 2013; Nelson et al. 2017; Du et al. 2021). The aim of this qualitative focus group study was to gain an understanding of parental perceptions of dental access, delivery, and efforts to accommodate dental services for CYA with ASD and to identify what adaptations and interventions might be required to reduce barriers to dental attendance for CYA with ASD and their families.
Method
Recruitment
A focus group design and purposeful sampling strategy was selected. The objective was to identify a sample, within which elements of similarity and difference could be explored, as a basis to gain understanding of parental experiences regarding dental visits and oral care for their CYA diagnosed with ASD. The specific inclusion criteria were English-speaking parents or guardians of at least 1 child, aged between 5 and 16 y, with a confirmed multidisciplinary team diagnosis of ASD, with or without coexisting medical conditions, and at least 1 experience of attending the dentist. Following appropriate university research ethical approval (UCC SREC Log 2019-172), information regarding the project, including focus group invitations, were circulated to a primary and secondary school recognized as providers of education for CYA with ASD. The primary and secondary school are state-funded schools associated with action plans to maximize the chances of every child getting the best possible opportunity to fulfill her or his potential in life. Both schools are co-educational and selected with the aim of providing a wide age span of CYA, along with information-rich parent participants. The participant sample included parents with a range of educational attainment and socioeconomic backgrounds, whose CYA had a range of verbal ability/disability that allowed us to capture reflective variation within a common core of participants. Variation in parent views according to location could not be captured, as both target schools were located within urban areas. The secondary school has a student population of approximately 200, comprising 125 boys and 75 girls. The primary school had approximately 270 pupils enrolled with 5 special class teachers for pupils diagnosed with ASD. Focus groups were carried out separately at each school location.
Data Collection
A topic guide was constructed by the lead investigator that was informed by a literature review, personal clinical experience, and a previous focus study (Parry and Shepherd 2018) and that highlighted the relevance of sensory difficulties, dentist expectations, and lack of previsit preparation on successful dental attendance.
The topic guide was refined through collaboration with all members of the research team and developed to draw out information from participants regarding positive and negative aspects of dental attendance, elicit perspectives regarding challenges and solutions from lived experience, and understand differences in interest, activity, or motivation relevant to CYA with ASD. The first author moderated both focus groups, with the lead supervisor and clinical psychologist (C.R.) present at the first focus groups to confirm observations and perceptions. Neither of the researchers were known to the focus groups participants nor involved in the organization or provision of dental care for any of the CYA represented in the sessions. As a pediatric dentist with experience providing treatment to CYAs with special health care needs, the first author made a conscious effort to ensure her role was moderation without participation in discussion.
Participants
Three parents attended each focus group, representing 10 CYP diagnosed with ASD. Focus group sessions were carried out during January and February 2020. Parents attending the primary school focus group each had 1 child diagnosed with ASD. Participants attending the secondary school focus group were parents of 7 CYA diagnosed with ASD. Two participants had more than 1 child diagnosed with ASD (Table). Between the 2 focus groups, there was an even spread of children across the age range of 9 to 18 y. All focus group participants provided informed consent to participate. Most parent participants identified as female. The 1 male participant was a father of a 15-y-old boy. Participants continued to use the nomenclature from the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (American Psychiatric Association 1994) when identifying their CYA within the ASD spectrum. Four children were described by parents as having Asperger syndrome. Five children were described by participants as having an additional disability: ID (1), language impairment (2), ADHD (1), and other behavior problem (1). The regularity of dental attendance varied between families: 5 CYA were taken to a dentist every 6 months, 3 of them yearly, and 2 of them only when in pain.
Table.
Focus Group Participant Identifier and Gender with Details of Age, Number, and Gender of ASD Child/Children.
| Gender of Parent | Gender of Child | Age of Child, y | |
|---|---|---|---|
| Primary school participant code | |||
| F1 | Female | Male | 9 |
| F2 | Female | Male | 10 |
| F3 | Female | Male | 11 |
| Secondary school participant code | |||
| F4 | Female | Female | 12 |
| Female | 8 | ||
| M1 | Male | Male | 15 |
| F5 | Female | Male | 9 |
| Female | 13 | ||
| Female | 16 | ||
| Male | 18 |
ASD, autistic spectrum disorder.
Data Analysis
Demographic data to identify gender, nationality, education, and employment status were collected from each participant at the start of the focus group. Audio recordings were used to fully capture all parent data during focus group meetings. The audio recordings were transcribed verbatim. Demographic data and audio recordings were anonymized by allocation of a code to each participant. The data were analyzed using a content-based, inductive thematic analytic approach, a common qualitative method, through which researchers identify themes in the data based on the specific content, rather than on preexisting theory (Braun and Clarke, 2006; Neuendorf, 2018). Transcripts were read and re-read by researchers J.A.P. and C.R. to familiarize the researchers with the scope of the data. As the transcripts were analyzed, initial codes were generated and the process of thematic analysis advanced. The research team collaborated in an iterative process to draw out the most pertinent codes, with documentation of progress and development of codes, subthemes and themes during data analysis. Codes were linked according to frequency and prevalence of iteration to broader emerging subthemes and themes. Cross-comparison with similar qualitative studies in the dental literature from the United Kingdom (Barry et al. 2014; Thomas et al. 2018) and North America (Marshall et al. 2007; Lewis et al. 2015; Stein Duker et al. 2019) revealed a high degree of commonality of parent experience across geographically dispersed populations. Data saturation following analysis of parent perceptions representing 10 CYA diagnosed with ASD enabled identification of needs and adaptations that might be required to manage challenges toward positive outcomes. We were able to consider the needs of users and providers of dental care and consider interventions required to tackle those needs.
Results
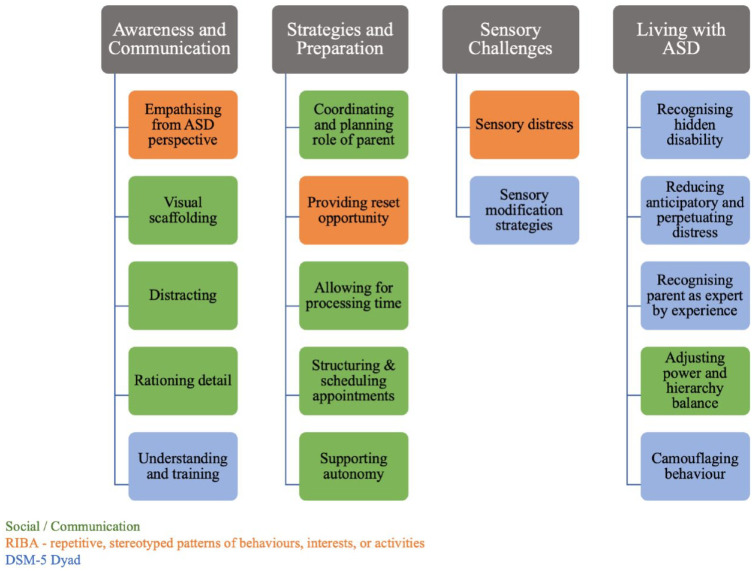
Four main themes emerged that represented parental perceptions of challenges and solutions regarding dental access, outcomes, and efforts to accommodate dental services for CYA diagnosed with ASD. These were awareness and communication, strategies and preparation, sensory challenges, and living with ASD. Each theme emerged from subthemes (Fig. 1) that were developed, ensuring they accurately represented the codes generated from the participant data.
Figure 1.
Themes and subthemes linked to individual or dyad of Diagnostic and Statistical Manual of Mental Disorders, fifth edition, autistic spectrum disorder diagnostic traits.
Awareness and Communication
Subthemes
Empathizing from ASD perspective
Parents of primary school children were particularly keen to emphasize the need for an immersive style of empathy in which oral health team members (OHTMs) reflected sameness. Understanding a CYA’s distress response following dental manipulation and treatments requires consideration of complex sensory sensitivities from an ASD perspective.
Autism now and Asperger’s and stuff like that it’s like they are drawn to each because they understand each other, it’s the other kids they don’t get—so if you relate to them like basically as if you have Asperger’s yourself then they will interact, they can understand you, but if you are trying to communicate on a different level that’s not theirs, it just doesn’t happen. (F1)
He just couldn’t understand there would be a hole [after extraction]. He kept going to the mirror saying “I think my tongue misses my tooth.” (F3)
When you think of it even to pull their lip down that’s like digging your nails into their lip you know especially when they are so sensitive. (F4)
Visual scaffolding
The importance of visual understanding for communication was agreed upon across the focus groups. Successful visual scaffolding requires time and needs to be thought about and worked on with the CYA to establish the required relational understanding. An important point made by participants was the quality of images used for oral health promotion. Participants were unanimously in favor of images reflecting the positive aspects of dentistry rather than attempts to change or encourage behavior using negative images or tactics involving guilt or fear.
We did the social story from the day we got the appointment; we went through it twice a day. (F5)
Another child would walk in and they see the chair and the dentist whereas ours go in and they see they are looking at everything in the room. (F1)
It’s all negative . . . . “Oh my god mom are my teeth going to be like that?” . . . put the big white smile face . . . this is what you get from coming here . . . you get the perfect smile. (F2)
Distracting
As a behavior-guidance technique, participants agreed that distraction and engagement of CYA in communication, where possible, was more likely to be associated with positive outcomes.
When someone is chatty, “oh you are looking great, what class [school year] are you in” talking through the whole thing . . . constantly talking my son is constantly engaging with her then and all of a sudden, it’s over. (M1)
She knows her stuff with autism and you can see it a mile away . . . the distraction is there all the time, when she is doing something, she to talking to my daughter about something else. (F5)
Rationing detail
The repercussions of mishandling information regarding complex or invasive treatment strategies was a concern highlighted by participants within the secondary school focus group. Parents want to provide input regarding anxieties and coping styles to avoid overwhelming the CYA.
Some information she doesn’t need to know, do you know what I mean, like they were talking about what the next plan was . . . I’d be “sh,sh,sh” . . . they are taking it in they are taking in every bit of it. (F5)
The positives are good . . . but if there was anything like say they spotted something wrong in the mouth . . . I would say nothing about that because that could hit the switch—cause a flare up . . . you have to know your child that way too. (M1)
Understanding and training
Parents acknowledged difficulties associated with the breadth of the ASD spectrum. However, both focus groups recounted a lack of progress among OHTMs toward recognizing and understanding the range of traits and individual needs of CYA diagnosed with ASD.
They’re not dogs and one training session will do for everyone it’s very difficult, it’s even difficult for the parents. (F2)
I don’t think they have an understanding of it to be honest with you. I think they see one child with autism . . . they think that everybody with autism is the same. (F3)
The professionals have to stop look and listen—okay what way is the child coming in, is he tense, is he stressed, is he flapping? F2
I said to him straight up—I said will you talk to my son he’s not stupid he has autism just talk to him . . . just explain it bit by bit by bit. F1
Strategies and Preparation
Subthemes
Coordinating and planning role of parent
A dental visit was described as a “military operation” requiring clear planning and no surprises. Participants were keen to advise that the attention required to manage the CYA’s attendance meant that a dental appointment was not the time to engage parents in discussion on new ideas for behavior or dietary change.
When you go to a visit with a child on the spectrum your whole focus is trying to keep them calm. (F4)
It’s a military operation. (M1)
You’re not going to able to say wait there now 2 minutes and I might just ask the dentist 10 questions . . . . (F4) [agreement F5]
Providing reset opportunity
Participants highlighted the regulatory strategies required by many CYA diagnosed with ASD and the need to plan “reset” time into the dental appointment. Parents want OHTMs to understand the importance of regulating using stimming and benefit of breaks, particularly during longer attendances.
He needs a movement break—he kind of resets, so if the leg is going, I would say “oh do you want 2 minutes and sit back down or something like that.” (M1)
He is standing up now because he needs to stim. I said he does this to regulate himself. He’s regulating, yeah. I said he is not doing this to get on anyone’s nerves. (F1)
Allowing for processing time
Patience and clarity were identified as powerful tools required by health care professionals to unlock barriers and help facilitate communication with CYA.
My child would process it a bit slower than a normal person so the dentist will think he is not going to answer my question, but he is just processing what the dentist is asking. Give a bit more time to answer questions I think yeah don’t make the questions too long, keep them short. (M1)
Repeat the same thing do not change it because then it just confuses them all again . . . simple instructions . . . one, two, three. (F1)
Structuring and scheduling appointments
Participants reflected on the inflexible and regimented nature of dental services and voiced concern regarding the lack of strategies and perceived lack of willingness to deal effectively with challenges of noncompliance.
Allow an extra 10 minutes . . . we go up there and straight away the nurse is trying to get my son to sit in the chair . . . give them the little 10 minutes to have a look at the stuff . . . it just changes things for them. (F1)
The dentist didn’t kind of have the patience for her because she wouldn’t put the glasses on, and she wouldn’t sit on his chair and she wouldn’t open her mouth wide and it all kind of escalated from there so then he was shouting at her. (F4)
They are like an assembly line (F1) . . . calling out the teeth and the child is like, “what’s happening here no one is saying anything to me.” . . . They are communicating between themselves and my child is lying in the middle of the two of them. (F2)
Supporting Autonomy
CYA engagement for decision making to provide choice and control were identified as important and effective elements to support positive behavior.
One of the tricks I use is to bring him down to the supermarket to pick out the toothpaste and he would pick out the most expensive one obviously because he thought they were the best. (M1)
I think if you give them the opportunity that it’s their decision—you are not just taking control. (F2)
We do sleeps . . . you are counting it down and then he would get up in the morning and he is ticking off . . . we live by the countdown. (F2) [agreement F1]
Sensory Challenges
Subthemes
Sensory distress
Participants described the extent of sensory sensitivities experienced by CYA in response to dental sensations and dental environment challenges. They also provided insight into the toll on parents’ emotions having to witness the intensity of these reactions.
Sensation of the stuff for the cleaning . . . gritty . . . normally he doesn’t do tantrums he’s just laid back. . . . If he knows this thing is coming, he will just cry and sweat and just panic like someone possessed. (F3)
It was a disaster for her I mean I actually had to get my husband to go with her the second time to do it because I just couldn’t do it with her . . . she was constantly gagging with it . . . she wasn’t happy, she would always try but there is only so much she can take. (F5)
Sensory modification strategies
Examples of the time, effort, and dedication required to reduce, transform, and occasionally eliminate sensory sensitivities were described by participants.
It took us about 3 months to get the electric toothbrush into his mouth, sitting on the couch with no tooth paste. (F1)
Huge sensory issues . . . you just keep going with it, he did get used to it, there is still a fight in the morning but it’s a lot better. Before he used to lock his jaw so you couldn’t even get the toothbrush in. (F5)
Living with ASD
Subthemes
Recognizing hidden disability
Participants described how the needs of CYA with ASD can be ignored or misinterpreted if their verbal or intellectual skill are similar or more advanced than peers.
It’s tough enough as it is for them, like, without making it harder—they are missed—but if you can solve their situation before it escalates, they are calm. (F2)
They told me we have treated a load of children with intellectual disabilities—my child doesn’t have ID—he has ASD. (F1)
There is not even an autism box, it’s like disability but they don’t look like they have any disability, the child is speaking and they think when an autistic child speaks they are not autistic. (F5)
Reducing anticipatory and perpetuated distress
Participants were keen for OHTMs to understand that dental attendance involves far more than just the scheduled appointment. Building up to the appointment and calming down after the appointment can involve days or even weeks of preparation, processing, and stress.
She will ask a hundred questions every day about the thing that’s happening in 2 weeks’ time (F4), and then it plays on them and then they will lack sleep, then they are anxious and the school work is falling behind probably because it is all playing in their head (F5). It’s a major thing (M1).
When the dentist is due . . . it’s like 3 days, 4 days beforehand she knows it’s coming and you will see a change in her. (F5)
They don’t realize when that child goes out the door, that our child is there at 11 o’clock that night with the same issue and the same thing going over and over and over again in their head, repeating what happened because they have not disconnected . . . it’s very hard to explain. (F1)
Recognizing parent as expert by experience
Parents were open about their ongoing learning needs and efforts to achieve the best outcomes for their CYA diagnosed with ASD. They cited patience as a “must have” quality. Parents were willing and eager to share their learning and be heard regarding the needs of their CYA. Many participants were wearied by the lack of understanding of OHTMs regarding the ASD obstacles to perceived simple oral health changes to dietary or daily routines.
Patience! (F5). Lots of patience. I keep going back to patience because I think it all boils down to patience. (F4)
It would be easier for the professionals to do their job if they understand what they are going in to. I am not telling them their job but I am just going to say—if you do it like this it’s just a way easier (F1). We are mothers and we are still learning daily (F2).
Since he is 3, he has a bread and butter sandwich, a banana, and 2 custard cream biscuits and he has that every day going to school. If he is not at school he will still say to me, “I think its lunch time now in school, I should have my sandwich and my banana and my 2 custard creams.” (F1)
My son wouldn’t drink plain water . . . . and the dentist said you can’t be drinking that it’s bad for your teeth you have to drink ordinary water—not a hope in hell. He’s still drinking flavored water. (F3)
Adjusting power and hierarchy balance
Participants provided examples of trying to share knowledge and experience to work with OHTMs. All participants had experienced rejection of offers to help guide care for their CYA.
Well I did suggest it . . . an attitude comes across like you are questioning the professional but they are a professional dentist they are not a professional specific person to deal with autism. (F2)
I wouldn’t say anything because I feel like I am back in school myself. (F3)
Camouflaging behavior
Secondary school participants noticed changes in their CYA with age, which involved self-initiated regulation and control of habits and behaviors to simulate those of their neurotypical peers.
I think he is at the age where he is trying to fit in everywhere now so if he needs to wait, he is watching everyone they are all waiting so I am waiting. (M1)
They are at that age where they want to be the same as everybody else. They know they are different, you know it boils down to everything. (F4)
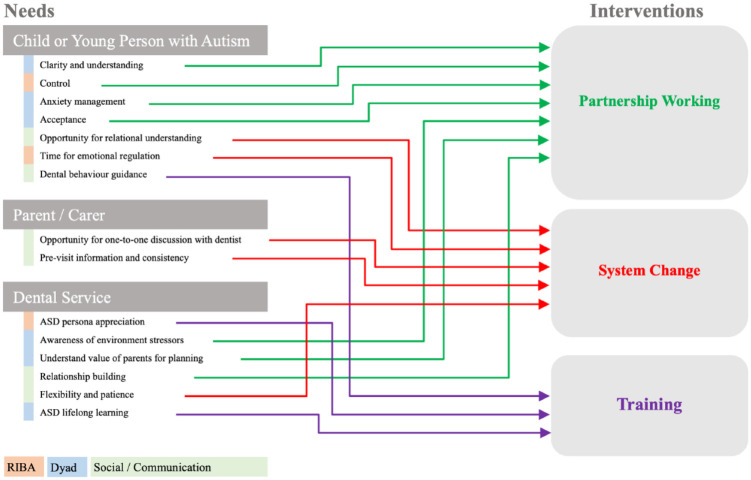
The aim of this project was not just to identify needs and challenges posed by oral health attendance for CYA but also to analyze the data to identify which actions and interventions might be required to manage challenges toward positive outcomes. Using parental perspectives from our focus groups, we constructed a model of ownership of needs linked to likely interventions required to resolve those needs (Fig. 2).
Figure 2.
Needs and interventions identified by subject and linked to Diagnostic and Statistical Manual of Mental Disorders, fifth edition, autistic spectrum disorder diagnostic traits.
Themes and subthemes informed the needs analysis regarding dental attendance, which we linked to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; American Psychiatric Association 2013) behavioral ASD domains of difficulties in social communication and social interaction and unusually restricted interests and repetitive behaviors (RIBA). Our participant data and thematic analysis identified 3 subject groups (the child or young person with autism, the parent or carer, and the dental service) with needs and interventions that should be considered to avoid barriers to dental attendance for CYA diagnosed with ASD (Fig. 2).
Within the CYA subject group, needs identified that linked to RIBA were Time for emotional regulation and Control. These needs were identified by examining the codes informing the Providing reset opportunity and Supporting autonomy subthemes. Parents highlighted the need for OHTMs to understand that engaging in stimming may be important for CYAs with ASD during a dental visit. There was unanimous agreement that observational monitoring is needed when a CYA with ASD attends the dental clinic. Parents described stimming as repetitive but soothing body movements involving a part or all of the body and that OHTMs should be aware and accommodate the need to stim, thereby allowing the CYA to self-regulate anxiety symptoms. CYA needs that linked closely to the ASD domains of difficulties in social communication and social interaction were Opportunity for Relational Understanding, which mapped to action requiring system change, and Behavior guidance, which mapped to training needs for OHTMs. The subtheme Visual scaffolding identified the need for Relational understanding through system change, to provide time and opportunity for a CYA to scan and assimilate information from the dental environment prior to proceeding with demands for participation. Parents reported examples, and stressed the importance of enhancing Control for engagement and Clarity for understanding. We believe that both can be actioned through partnership working. The need for tailored anxiety management strategies for autistic CYA was highlighted by participants, to help prevent avoidable pre- and postoperative anticipatory anxiety, replay, and catastrophizing. Parents were keen for OHTMs to understand that a dental attendance is not an isolated event but a journey for the family that requires partnership and planning for success. Experience was shared about observing a CYA’s need to fit in with peers, which might facilitate delivery of complex dental procedures in the presence of appropriate dental behavior guidance, with increasing age. Parents of secondary school children observed a trajectory of change and camouflaging behavior with age that they described as “needing to fit in” with peers. This has been identified as need for Acceptance in our model.
Parents wanted opportunities to share expertise they had developed from providing day-to-day support for their CYA and skills they had acquired from other sources, including other parents, therapists, or through accessing formal autism education and training. The parent needs identified in our model were drawn from codes associated with the Coordinating and planning role of parent and Rationing detail subthemes. Parent input in providing advice about how to present and introduce information regarding invasive or complex treatment was perceived as vitally important. They reported a need to avoid delivery of dental information that could encourage catastrophizing thought processes. Parents valued opportunities to discuss anticipated CYA challenges and anxieties with OHTMs, without their CYA present. This was seen as integral for success along with formulation of a dental visit plan which was followed, where at all possible, without deviation. These elements are identified in the model as Previsit information and consistency. Parents recommended opportunity for one-to-one discussion with the OHTM as a system change, if not already in place, and requested previsit information to help strategically prepare for tasks and clinic attendance.
The dental service needs identified to ensure removal of avoidable barriers to dental attendance were analyzed. Three dental service needs mapped to Partnership working. These were need for Awareness of environment stressors, Understanding the value of parents for planning, and Relationship building. Training needs for OHTMs emerged strongly from the participant data, which coded for the Understanding and training and Recognizing hidden disability subthemes. Parents continue to experience a disconnected understanding of ASD and dismissal of complexity and support for CYA with less prototypical presentations. Participants in our study defined a quality of empathy that requires the dental team to empathize from an autistic rather than neurotypical perspective. We described this as ASD persona appreciation in our model. The need for Relationship building addresses barriers that may result from attitudes, demonstrated or perceived, regarding medical authority and hierarchy within the parent-OHTM relationship. Parents revealed feeling that their value as an expert with lived experience was usually ignored. They perceived blame and lack of understanding that obstacles to maintaining good oral health may be different for an autistic CYA. They often felt ignored and unable to discuss barriers to implementation of oral health advice. Parents were unanimous and passionate regarding the need for system change to allow Flexibility and patience in the structure and duration of the dental appointment for CYA.
Discussion
Research results from this Irish participant group identified similarities with previous qualitative studies from the United Kingdom and North America (Barry et al. 2014; Brown et al. 2014; Lewis et al. 2015; Thomas et al. 2018; Stein Duker et al. 2019) and commonality of many key themes. The importance of considering sensory sensitivity has been highlighted by parents (Thomas et al. 2018; Stein Duker et al. 2019) as has need for awareness of the individual, time to process information, and clarity in communication (Brown et al. 2014; Thomas et al. 2018; Stein Duker et al. 2019). Our participants also confirmed perceptions of being unfairly judged, because OHTMs lack understanding of ASD and perceived a power imbalance that affected parent confidence to advocate for their CYA (Lewis et al. 2015; Thomas et al. 2018). Given the level of consensus, we believe that development of a model of ownership of needs linked to likely interventions required to resolve those needs (Fig. 2) builds on previous work and is a useful addition to the literature for future research and service development.
The approach taken in the model, to “unravel” the diagnostic criteria of ASD for understanding of oral health–related behavior has been used previously (Weil and Inglehart 2012). We acknowledge that some needs identified in our model could map to more than 1 intervention, indicating the need for further research to test the proposed model.
Clarity for understanding and time are required for processing information and a necessity for the CYA with ASD. Parents appreciated that lack of understanding of the additional time required to process information might result in clinicians changing a question or request, to try to get a quicker response. This is likely to be counterproductive. Advice to avoid simply talking for the sake of talking has been highlighted previously (Brown et al. 2014). There was agreement from our participant group that the dental behavior management and guidance techniques used by OHTMs need to be tailored for the individual CYA with ASD. This is in line with professional society guidance for use of behavior guidance for pediatric dental patients (American Academy of Pediatric Dentistry 2020). As a behavior management and guidance tool, distraction was favored to redirect attention away from dental tasks. Positive reinforcement, even when a child had been unsuccessful but tried hard, has been highlighted as a priority by parents in other studies (Thomas et al. 2018; Stein Duker et al. 2019) but did not emerge as integral to success from our participant groups. Obtaining the correct balance between being chatty to encourage relaxation, engaging for effective distraction, and supplying the right amount and level of information for anxiety management is likely to be impossible without partnership working with families. There is increasing recognition that interprofessional collaboration, with existing teams and therapists involved in the CYA’s care, is also an important element of partnership working for successful dental visit outcomes (Como et al. 2020). Good relationships and partnership working in early childhood may provide opportunity for more complex procedures with reduced barriers to care with age. Parents suggested this may be particularly relevant to orthodontics when CYAs aspire to receiving the same treatment as their peers for oral esthetics. However, they may not be ready to overcome the challenges associate with delivery of orthodontic treatment until they are older than their neurotypical peers.
The importance of relational understanding was highlighted by participants’ pleas for positive imagery in health promotion material and language. Our data support results from other researchers (Stein Duker et al. 2019; Du et al. 2021), but contrasts with the lack of importance of visual pedagogy reported by Thomas et al. (2018). System change providing time to accommodate self-regulation (“reset” time) was nonnegotiable for participants in this study. The need for system change to allow flexibility in the structure and duration of the dental appointment for CYA with ASD has been highlighted by other researchers (Thomas et al. 2018; Stein Duker et al. 2019). In many health care systems, obtaining this flexibility and opportunities for interprofessional collaborations are likely to be easier for clinicians working within services dedicated to and provided with resources for treating CYA with special health care needs.
Our findings regarding the role of parents as experts by experience were similar to those of Thomas et al. (2018). Parents were dedicated to advocating for their CYA, but advocacy was often burdensome because of the lack of public understanding of real-life challenges associated with a diagnosis of ASD. Lack of OHTM understanding regarding the complexity of altering ritualistic dietary regimes and introducing dental preventive habits were associated with perceptions of being unfairly judged by the focus group participants. The need to understand and value the role of parents in planning treatment requires a recognition of parents as experts by experience. This parental role has been identified previously (Stein Duker et al. 2019). Parental guidance and agreement with OHTMs regarding processes for dealing with noncompliance need a partnership approach. Acceptability of restraint and clinical holding needs to be considered and agreed in advance with parents, using the parents’ experience to anticipate the likelihood of sudden changes in behavior. Avoiding preconceived ideas, including a presumption of ID, has been highlighted by other researchers (Stein Duker et al. 2019). Parents want areas of strength as well as difficulties to be recognized. Our findings regarding the stipulation for no surprises represent commonality of parent views from different studies in different parts of the world (Stein Duker et al. 2019) as does parent advice that the dental appointment is not the appropriate time to engage parents in oral health education and discussion (Lewis et al. 2015). Data from our study supply more evidence to confirm the value of appropriate preoperative information gathering and delivery and the need to promote a one-to-one discussion opportunity for parents with OHTMs. Supporting positive engagement through choice and structured preparation was described as a daily norm by parents. Successful preparation by counting down days, hours, and weeks could be adapted and useful for dental attendance. Clinicians often use counting as behavior management. Information provided in this study suggests that counting down rather than counting up may be more useful for CYA who are accustomed to a countdown process of preparation.
The negative impact of lack of empathy and failure of dentists to adapt to the anxieties of CYA with ASD has been identified (Brown et al. 2014). The focus group participants in this project introduced empathizing from an autistic perspective. Recommendation for this immersive empathy, which we term ASD persona appreciation, has implications for training of dental health care staff. Persona generation is frequently used by designers to imagine the kind of users to be accommodated for product sales (Pruitt and Adlin 2010). ASD persona generation could be a relevant and useful adjunct for training at both the undergraduate and postgraduate level (Clarkson et al. 2017). Parents appreciated and recognized that designing training to capture the full “spectrum” nature of ASD and prepare dental health care professionals for all possible scenarios is not possible. However, they expected training to provide recognition of the spectrum, awareness of key components, and the need to design advice and appointment structure to provide individualized support.
The Sensory Challenges theme and need for OHTMs to be aware of potential environment stressors in the dental environment is one that has been identified from many studies (Cermak et al. 2010; Barry et al. 2014; Thomas et al. 2018; Stein Duker et al. 2019; Como et al. 2020). Recognition of sensory sensitivities has already stimulated research to develop strategies for success (Shapiro et al. 2009; Stein Duker et al. 2019). The description by participants of physiologic and behavioral transformation that sensory sensitivity can produce correlated with data from Thomas et al. (2018), linked to both DSM-5 behavioral domains in our model and identified the need for partnership working with parents to continue to develop strategies to reduce sensory sensitivities. Identification and appreciation of complex sensory sensitivities will help clinicians to anticipate intraoperative reactions in the dental surgery and the postoperative information required, for example, following multiple extractions under general anesthesia.
If the aim of this study had been to gather parent perspectives alone, a limitation would be the size of the focus groups and number of participants. However, this study aimed to consider parents’ perspectives from this study and those previously recorded in the literature, to develop a model (Fig. 2) identifying how the dental community can move forward to reduce barriers to dental attendance for CYA with autism.
A number of key service recommendations can now be made to facilitate positive participation of CYA with autism during dental visits. First, OHTMs should listen carefully to parent experiences of previous interactions with health care services and advice. This level of meaningful participation will aid understanding of sensory sensitivities and help to anticipate challenges and promote openness for discussion when proposing treatment or changes to dietary and oral hygiene habits. Second, OHTMs should engage positively in partnerships to replicate strategies that have proved successful. Strategies highlighted by parents include developing insight, with training, to enable an OHTM to empathize from an autistic perspective and to provide positive oral health messaging accompanied by positive imagery. Third, OHTMs should ensure ample time is allocated for the dental visit. Appropriate appointment structure, along with patience and careful delivery and clarity of participation requests, will help to facilitate a dental visit that encourages time for processing information and acclimatization to the clinical environment.
Further research is required to test the proposed model and to refine and enrich the model with added perspectives from child and adolescent autistic patients. Feasibility studies are also required to identify resource implications required to respond to parents’ requests for preparation and change to the structure and time allocated for dental visits for autistic patients.
Conclusion
This study considered barriers to dental attendance in relation to the diagnostic criteria of ASD and within the context of avoiding disparity to dental access for satisfactory oral health quality of life. Analysis of the focus group data supplied by participants and consensus with data from the dental literature allowed us to establish a needs analysis relating to CYA, parents, and dental health care services that was mapped to interventions to reduce avoidable dental attendance barriers. Further research to investigate the model we have developed is now required to establish if the proposed interventions involving Partnership Working, System Change, and Training can effectively reduce avoidable barriers to dental attendance and prevent possible disparities in access and uptake of dental services for CYA diagnosed with ASD.
Author Contributions
J.A. Parry, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; T. Newton, C. Linehan, contributed to design, data analysis, and interpretation, critically revised the manuscript; C. Ryan, contributed to conception, design, data analysis, and interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank the focus group participants for giving up their time to be involved in this research and Jochen and Maebh Glemser for assistance with figure graphics for this document. Governance: Research ethics and governance approval given through University College Cork social research ethics committee (UCC SREC Log 2019-172).
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: J.A. Parry  https://orcid.org/0000-0001-9789-0326
https://orcid.org/0000-0001-9789-0326
References
- Altiere MJ, von Kluge S. 2009. Searching for acceptance: challenges encountered while raising a child with autism. J Intellect Dev Disabil. 34(2):142–152. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry. 2020. Behavior guidance for the pediatric dental patient. The Reference Manual of Pediatric Dentistry. Chicago (Ill): American Academy of Pediatric Dentistry. p. 292–310 [Google Scholar]
- American Psychiatric Association 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington (DC): American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. 1994. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington (DC): American Psychiatric Association. [Google Scholar]
- Anders PL, Davis EL. 2010. Oral health of patients with intellectual disailities: a systematic review. Spec Care Dentist. 30(3):110–117. [DOI] [PubMed] [Google Scholar]
- Barry S, O’Sullivan E, Toumba K. 2014. Barriers to dental care for children with autism spectrum disorder. Eur Arch Paediatr Dent. 15(2):127–134. [DOI] [PubMed] [Google Scholar]
- Bishop MR, Kenzer AL, Coffman CM, Tarbox CM, Tarbox J, Lanagan TM. 2013. Using stimulus fading without escape extinction to increase compliance with toothbrushing in children with autism. Res Autism Spectr Disord. 7(6):680–686. [Google Scholar]
- Blomqvist M, Dahllöf G, Bejerot S. 2014. Experiences of dental care and dental anxiety in adults with autism spectrum disorder. Autism Res Treat. 2014(2014):238764-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. 2006. Using thematic analysis in psychology. Qual Res Psychol. 3(2):77–101. [Google Scholar]
- Brown J, Brown J, Woodburn J. 2014. Dental services for children with autism spectrum disorder. Learn Disabil Pract. 17(3):20–25. [Google Scholar]
- Cermak SA, Curtin C, Bandini LG. 2010. Food selectivity and sensory sensitivity in children with autism spectrum disorders. J Am Diet Assoc. 110(2):238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson PJ, Bogle D, Dean J, Tooley M, Trewby J, Vaughan L, Adams E, Dudgeon P, Platt N, Shelton P. 2017. Engineering Better Care: A Systems Approach to Health and Care Design and Continuous Improvement. London: Royal Academy of Engineering. [Google Scholar]
- Como DH, Stein Duker LI, Polido JC, Cermak SA. 2020. Oral health and autism spectrum disorders: a unique collaboration between dentistry and occupational therapy. Int J Environ Res Public Health. 18(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cost KT, Zaidman-Zait A, Mirenda P, Duku E, Zwaigenbaum L, Smith IM, Ungar WJ, Kerns C, Bennett T, Szatmari P. 2021. “Best things”: parents describe their children with autism spectrum disorder over time. J Autism Dev Disord. February 2, 2021. doi: 10.1007/s10803-021-04890-4. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Du RY, Yang W, Lam PPY, Yiu CKY, McGrath CP. 2021. Developing a toothbrushing visual pedagogy (tbvp) for preschool children with autism spectrum disorder. J Autism Dev Disord. March 10, 2021. doi: 10.1007/s10803-021-04946-5. Online ahead of print.. [DOI] [PubMed] [Google Scholar]
- Du RY, Yiu CK, King NM. 2019. Oral health behaviours of preschool children with autism spectrum disorders and their barriers to dental care. J Autism Dev Disord. 49(2):453–459. [DOI] [PubMed] [Google Scholar]
- Gabre P, Martinsson T, Gahnberg L. 2001. Longitudinal study of dental caries, tooth mortality and interproximal bone loss in adults with intellectual disability. Eur J Oral Sci. 109(1):20–26. [DOI] [PubMed] [Google Scholar]
- Lai B, Milano M, Roberts MW, Hooper SR. 2012. Unmet dental needs and barriers to dental care among children with autism spectrum disorders. J Autism Dev Disord. 42(7):1294–1303. [DOI] [PubMed] [Google Scholar]
- Lewis C, Vigo L, Novak L, Klein EJ. 2015. Listening to parents: A qualitative look at the dental and oral care experiences of children with autism spectrum disorder. Pediatr Dent. 37(7):98E–104E. [PubMed] [Google Scholar]
- Mac Giolla Phadraig C, McCallion P, Cleary E, McGlinchey E, Burke E, McCarron M, Nunn J. 2015. Total tooth loss and complete denture use in older adults with intellectual disabilities in Ireland. J Public Health Dent. 75(2):101–108. [DOI] [PubMed] [Google Scholar]
- Mac Giolla Phadraig C, Nunn J, McCallion P, McCarron M. 2018. Prevalence of edentulism among adults with intellectual disabilities: a narrative review informed by systematic review principles. Spec Care Dentist. 38(4):191–200. [DOI] [PubMed] [Google Scholar]
- McMillion A, Van Herwegen J, Johnson A, Monteiro J, Cronin AJ, Remington A. 2021. Dental experiences of a group of autistic adults based in the united kingdom. Spec Care Dentist. 41(4):474–488. [DOI] [PubMed] [Google Scholar]
- Mangione F, Bdeoui F, Monnier-Da Costa A, Dursun E. 2020. Autistic patients: a retrospective study on their dental needs and the behavioural approach. Clin Oral Investig. 24(5):1677–1685. [DOI] [PubMed] [Google Scholar]
- Marshall J, Sheller B, Williams BJ, Mancl L, Cowan C. 2007. Cooperation predictors for dental patients with autism. Pediatr Dent. 29(5):369–376. [PubMed] [Google Scholar]
- Matson JL, Kozlowski AM. 2011. The increasing prevalence of autism spectrum disorders. Res Autism Spectr Disord 5(1):418–425. [Google Scholar]
- Nelson T, Chim A, Sheller BL, McKinney CM, Scott JM. 2017. Predicting successful dental examinations for children with autism spectrum disorder in the context of a dental desensitization program. J Am Dent Assoc. 148(7):485–492. [DOI] [PubMed] [Google Scholar]
- Neuendorf KA. 2018. Content analysis and thematic analysis. In: Brough P, editor. Advanced Research Methods for Applied Psychology: Design, Analysis and Reporting. Abingdon (UK): Routledge. p. 211–223. [Google Scholar]
- Parry JA, Brosnan S, Newton JT, Linehan C, Ryan C. 2021. Brief report: analysis of dental treatment provided under general anaesthesia for children and young adults with autistic spectrum disorder and identification of challenges for dental services. J Autism Dev Disord. February 8, 2021. doi: 10.1007/s10803-021-04898-w. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Parry J, Shepherd J. 2018. Understanding oral health challenges for children and young people with autistic spectrum conditions: views of families and the dental team.J Disabil Oral Health. 19(4):170–174. [Google Scholar]
- Peres M, Heilmann A. 2015. Social Inequalities in Oral Health: From Evidence to Action. London: International Centre for Oral Health Inequalities Research & Policy. [Google Scholar]
- Peres MA, Macpherson LM, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C. 2019. Oral diseases: a global public health challenge. Lancet. 394(10194):249–260. [DOI] [PubMed] [Google Scholar]
- Pituch KA, Green VA, Didden R, Lang R, O’Reilly MF, Lancioni GE, Sigafoos J. 2011. Parent reported treatment priorities for children with autism spectrum disorders. Res Autism Spectr Disord. 5(1):135–143. [Google Scholar]
- Pruitt J, Adlin T. 2010. The Persona Lifecycle: Keeping People in Mind throughout Product Design. Amsterdam: Elsevier Science & Technology. [Google Scholar]
- Shapiro M, Sgan-Cohen HD, Parush S, Melmed RN. 2009. Influence of adapted environment on the anxiety of medically treated children with developmental disability. J Pediatr. 154(4):546–550. [DOI] [PubMed] [Google Scholar]
- Spann SJ, Kohler FW, Soenksen D. 2003. Examining parents’ involvement in and perceptions of special education services: an interview with families in a parent support group. Focus Autism Other Dev Disabl. 18(4):228–237. [Google Scholar]
- Stein Duker LI, Floríndez LI, Como DH, Tran CF, Henwood BF, Polido JC, Cermak SA. 2019. Strategies for success: a qualitative study of caregiver and dentist approaches to improving oral care for children with autism. Pediatr Dent. 41(1):4E–12E. [PMC free article] [PubMed] [Google Scholar]
- Stein LI, Polido JC, Mailloux Z, Coleman GG, Cermak SA. 2011. Oral care and sensory sensitivities in children with autism spectrum disorders. Spec Care Dentist. 31(3):102–110. [DOI] [PubMed] [Google Scholar]
- Thomas N, Blake S, Morris C, Moles DR. 2018. Autism and primary care dentistry: parents’ experiences of taking children with autism or working diagnosis of autism for dental examinations. Int J Paediatr Dent. 28(2):226–238. [DOI] [PubMed] [Google Scholar]
- Watt RG, Mathur MR, Aida J, Bönecker M, Venturelli R, Gansky SA. 2018. Oral health disparities in children: a canary in the coalmine? Pediatr Clin North Am. 65(5):965–979. [DOI] [PubMed] [Google Scholar]
- Weil TN, Inglehart MR. 2012. Three-to 21-year-old patients with autism spectrum disorders: parents’ perceptions of severity of symptoms, oral health, and oral health-related behavior. Pediatr Dent. 34(7):473–479. [PubMed] [Google Scholar]