Abstract
Background
Expressive writing about a traumatic event is promising in treating posttraumatic stress disorder (PTSD) symptoms in adult trauma survivors. To date, the comparative efficacy and acceptability of this approach is uncertain. Therefore, we aimed to examine the comparative efficacy and acceptability of expressive writing treatments.
Methods
We included 44 RCTs with 7724 participants contributing 54 direct comparisons between expressive writing (EW), enhanced writing (i.e. including additional therapist contact or individualized writing assignments; EW+), PTSD psychotherapies (PT), neutral writing (NW), and waiting-list control (WL).
Results
EW, EW+, PT, and NW were statistically significantly more efficacious than WL at the longest available follow-up, with SMDs (95% CI) of −0.78 (−1.10 to −0.46) for PT, −0.81 (−1.02 to −0.61) for EW+ , −0.43 (−0.65 to −0.21) for EW, and −0.37 (−0.61 to −0.14) for NW. We found small to moderate differences between the active treatments. At baseline mean PTSD severity was significantly lower in EW+ compared with WL. We found considerable heterogeneity and inconsistency and we found elevated risk of bias in at least one of the bias dimensions in all studies. When EW+-WL comparisons were excluded from the analyses EW+ was no longer superior compared with EW.
Conclusions
The summarized evidence confirms that writing treatments may contribute to improving PTSD symptoms in medium to long-term. Methodological issues in the available evidence hamper definite conclusions regarding the comparative efficacy and acceptability of writing treatments. Adequately sized comparative randomized controlled trials preferably including all four active treatment approaches, reporting long-term data, and including researchers with balanced preferences are needed.
Key words: comparative efficacy, expressive writing, network meta-analysis, (partial) PTSD, PTSD symptoms
Introduction
After the experience of a traumatic event negative health-related symptoms can be observed in many adult trauma survivors. The range of negative symptoms typically includes re-experiencing the trauma, hyperarousal and avoidance of trauma-associated stimuli – the three core symptom clusters of the posttraumatic stress disorder diagnosis – however, alterations in mood and cognition occur as well (American Psychiatric Association, 2013). About 10% to 20% of trauma survivors show all symptoms of a full-blown posttraumatic stress disorder (PTSD; Norris & Slone, 2007), and around 8% of adults meet PTSD criteria at least once in their life (de Vries & Olff, 2009; Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). However, the diagnosis of PTSD is not very distinct, with many possible manifestations and combinations of symptoms (Galatzer-Levy & Bryant, 2013). In addition, partial PTSD is also associated with considerable impairments (Marshall et al., 2001), and with similar health-seeking behaviour as observed among individuals who fulfil diagnostic criteria for PTSD (Stein, Walker, Hazen, & Forde, 1997). PTSD symptoms have a high risk for chronicity, comorbid medical and psychiatric symptoms, and suicide (Frayne et al., 2004; Kessler et al., 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Krysinska & Lester, 2010; Pietrzak, Goldstein, Southwick, & Grant, 2011, 2012; Wittchen et al., 2011). Further, PTSD symptoms often lead to social and occupational impairment, and are associated with substantial economic and societal costs (Kessler, 2000). National treatment guidelines suggest several efficacious treatments for PTSD (Forbes et al., 2010), including a variety of trauma-focused psychotherapeutic treatment approaches (American Psychological Association, 2017; Foa, Keane, Friedman, & Cohen, 2009; Forbes et al., 2007; Institute of Medicine, 2008; National Institute for Health and Care Excellence, 2005; World Health Organization, 2013), but also pharmacological treatments (American Psychological Association, 2017; Foa et al., 2009). However, many patients with PTSD do not receive adequate treatment for their symptoms (Lewis et al., 2019; Liebschutz et al., 2007; Rodriguez et al., 2003).
In 1986, writing about one's own trauma experience was proposed as potentially beneficial treatment for trauma survivors by Pennebaker and Beall (1986). Expressive writing originally consisted of four writing sessions of 15 minutes duration and did not involve additional contact with a mental health professional. Initially, promising results have been demonstrated for expressive writing treatment in reducing symptom severity and increasing well-being (Smyth, 1998). However, benefits in subsequent meta-analyses were mostly small to moderate reflecting considerable variations of treatment effects across meta-analyses (Frattaroli, 2006; Frisina, Borod, & Lepore, 2004; Mogk, Otte, Reinhold-Hurley, & Kröner-Herwig, 2006; Smyth & Pennebaker, 2008). These findings motivated adaptions of the original paradigm in order to increase the initially observed beneficial treatment effects of writing treatments (Smyth & Pennebaker, 2008). Such adaptions, for instance, included the addition of interactions with a therapist or the provision of more detailed and guided writing instructions. Importantly, the main component of the treatment remained the writing itself and a number of mechanisms have been described to explain the observed treatment benefits (including improved self-regulation, cognitive processing of the trauma memory, and restoring perceptions of control; Andersson & Conley, 2008; Frattaroli, 2006; Smyth & Pennebaker, 2008). Besides the assumed beneficial health effects, the parsimony of writing treatments, as well as the huge potential to close gaps in the provision of PTSD treatment through remote (e.g. online) delivery may have contributed to the treatment's continuing popularity over the last three decades. Several meta-analyses have been conducted over the last 20 years that showed small to moderately sized beneficial effects of the original expressive writing assignments in improving PTSD symptoms (Frattaroli, 2006; Frisina et al., 2004; Mogk et al., 2006; Smyth, 1998; Smyth & Pennebaker, 2008). More recent meta-analyses focused on novel developments in writing treatments and did not include studies using the original writing paradigm (Kuester, Niemeyer, & Knaevelsrud, 2016; van Emmerik, Reijntjes, & Kamphuis, 2013).
While early randomized clinical trials (RCTs) evaluating the effects of writing treatments primarily used neutral writing assignments as control groups (e.g. writing about daily activities), more recent RCTs also incorporated passive comparators (i.e. waiting list control), and psychotherapeutic PTSD treatments. Today's plethora of available RCTs creates the opportunity to make multiple comparisons between the original and adapted writing treatments, psychotherapeutic PTSD treatments, as well as active and passive control groups in RCTs of writing treatments. The complex pattern of evidence from these differently controlled RCTs complicates the integration of available research findings using conventional pairwise meta-analytic approaches and calls for a network meta-analytic summary of available RCTs.
We conducted a systematic review and network meta-analysis including studies with full and partial PTSD as well as studies which included participants who had been exposed to trauma and suffered from PTSD symptoms. We included all available direct comparisons between an expressive writing treatment as stand-alone treatment (i.e. not as part of a complex treatment package) that was compared with a psychotherapeutic PTSD treatment, with an active writing control, or with a passive waiting-list control. We distinguished between original and enhanced writing treatments and summarized the available evidence in the short- and long-term.
Methods
This study was conducted in accordance with the PRISMA-NMA statement (Hutton et al., 2015; Moher, Liberati, Tetzlaff, Altmann, & Group, 2009), and was registered on PROSPERO (number: CRD 42018094075; Gerger, Gaab, & Werner, 2018).
Identification of studies
We searched EMBASE, Medline, PsycINFO, and Cochrane Controlled Trials Register using key words and text words related to writing treatments, trauma experience and RCTs (see eAppendix 1). In addition, one researcher (CW) searched through the reference lists of relevant systematic reviews, and meta-analyses (Frattaroli, 2006; Frisina et al., 2004; Kuester et al., 2016; Mogk et al., 2006; Smyth, 1998; van Emmerik et al., 2013) for potentially relevant trials. The initial literature search was conducted between 8 June 2016 and 15 November 2016. The last update of the database search was conducted on 6 September 2020. Study inclusion was finished on 5 October 2020. Two reviewers (CW and HG) independently screened the full texts of potentially relevant publications using a structured manual. Disagreements were resolved by consensus.
Selection criteria
We included RCTs that applied at least one trauma-focused writing treatment, which aimed at reducing PTSD symptoms, and which was not part of a complex treatment package. We allowed any delivery method (e.g. paper and pencil or electronic or internet-based ), as long as it was a purely written intervention and not mixed with any other intervention like verbal cognitive behavioural therapy. RCTs were included even when the trauma-focused writing treatment was not the main focus of the experimental investigation but served as a control condition for psychotherapy. We included comparisons between trauma-focused expressive writing treatments with PTSD psychotherapies, neutral writing and waiting-list control groups.
We defined trauma-focused writing as a writing treatment that targeted the traumatic event the participant had experienced. We classified expressive writing treatments as 1st those that referred to the original paradigm by Pennebaker and Beall (1986), and 2nd as enhanced writing interventions those that included additional elements assumed to increase their efficacy (i.e. therapist contact exceeding the initial writing instruction, or more elaborated and directive instructions for each individual writing session). Writing treatments were classified as expressive writing (EW) if authors either explicitly referred to the original paradigm by Pennebaker and Beall (1986), or writing treatments were similarly structured as the original writing paradigm (e.g. three3–four sessions of 15–30 min duration). Importantly, to be considered EW no therapist involvement was allowed. Also, no individualized instructions for each writing session were allowed. Writing treatments were classified as enhanced writing (EW+) if the treatment description 1st did not explicitly refer to the original Pennebaker writing paradigm and if 2nd writing treatments included additional elements assumed to increase their efficacy: the treatments included either the presence of a therapist during writing sessions, or any therapist feedback. In many cases experimental manipulation of the writing content was used (e.g. more directive writing instructions which changed for each writing session). Enhanced writing treatments typically also used more or longer writing sessions compared with the original paradigm. However, the use of longer sessions alone was not sufficient for a writing treatment to classify as enhanced writing. Studies that used only experimental manipulations of formal aspects of the writing task (e.g. writing in the first-person v. writing in the third-person; Andersson & Conley, 2013; Kenardy & Tan, 2006) but which had no additional comparator were not included in the analyses. Neutral control writing was defined as a writing task that did not focus on a traumatic event (e.g. writing about daily tasks). We included RCTs with adults (i.e. mean age of the study sample was 18 or above). Participants needed to have experienced at least one traumatic event according to the Diagnostic and Statistical Manual of Mental Disorders fifth edition PTSD criterion A (DSM-5; American Psychiatric Association, 2013), and they needed to report the occurrence of either full or partial PTSD, or the presence of PTSD symptoms in the aftermath of trauma experience (see eAppendix 2 for a more detailed description). We excluded studies on expressive writing with samples that did not report the presence of PTSD symptoms (e.g. Burton & King, 2004; Pennebaker & Beall, 1986; Ramirez & Beilock, 2011; Tondorf et al., 2017). We had no language restrictions and we did not require studies to be double-blind for inclusion, as a blinding of therapists and participants is not possible in psychotherapy research.
Outcomes
Our primary outcome was the longest available follow-up assessment of PTSD symptom severity measured on a continuous validated scale, or using structured interviews assessing PTSD symptoms according to diagnostic criteria. In addition to the longest available follow-up, we assessed treatment effects immediately after treatment termination (⩽1 month after treatment termination) and long-term effects (>1 month after termination). If more than one PTSD scale was used in the trial, we used a predefined hierarchy, which gave most frequently used scales precedence (see eAppendix 2 for the pre-defined hierarchy). Results from intention-to-treat (ITT) analyses were preferred over results from per-protocol or completer analyses, and observer-rated outcomes were used in our analyses only if self-rated outcomes were not reported. As secondary outcome we included the acceptability of PTSD treatments as indicated by patients dropping out of treatment before treatment termination. If no reasons for early termination were provided, we used the total drop-out rates per group.
Data collection
For the effect size calculation, we extracted sample sizes (N), means (M) and standard deviations (s.d.) for each treatment group. In case these values were missing, other statistical data that can be converted into means and standard deviations were extracted. Conversions were calculated according to formulas previously suggested (Cohen, 1988; Higgins & Green, updated March 2011; Lakens, 2013; Lipsey & Wilson, 2001). If the N was missing in the table of analysis, we used the N of the descriptive statistics, and if group Ns were missing, we assumed same sample size per group. We contacted one study author, because insufficient information was available, but the author did not reply. Studies were excluded, if the outcome data could not be calculated, imputed, or obtained from the authors. For the calculation of risk ratios (RRs) as indicators of treatment acceptability we extracted the number of drop-outs between beginning and end of treatment.
In addition to the data for effect size calculation characteristics of the included population (e.g. type of trauma, age of the study sample, PTSD diagnosis), the intervention (e.g. number of treatment sessions, reference to the original Pennebaker writing paradigm, presence of a therapist during writing sessions, location of writing), and the study (e.g. year of publication) were coded. We rated risk of bias for the results presented in each individual included study using the dimensions defined in the Cochrane Risk of Bias (RoB) Assessment Tool (Higgins & Green, updated March 2011). Across studies we rated the indirectness of the available evidence (i.e. whether a single study differed from the target studies we were interested in with respect to population, intervention, outcome assessment, or the type of comparison; Guyatt et al., 2011). In order to rate the confidence in the entire network meta-analytic results on a meta-level across all included studies we used the CINeMA framework (Salanti, Del Giovane, Chaimani, Caldwell, & Higgins, 2014) (see eAppendix 2 for a detailed description of ratings for RoB, indirectness, and network confidence). Two independent raters (HG and CW) extracted all data from all included studies on a standardized form (Microsoft Office Excel 2011 and 2018) after intensive training in using the manual with operational descriptions of each item. Disagreements were solved by consensus between these two raters.
Data analysis
Standardized mean differences (SMDs) were calculated first with the data collected at the end of treatment (34 studies), and second with the data from long-term follow-up (26 studies). In our analyses using the longest available follow-up data we included all 44 identified studies with a preference for long-term data if both, end of treatment and long-term data, were available. In our protocol, we defined the analyses using short-term data as primary outcomes. This choice was made because we expected that all studies would report results at the end of treatment and we wanted the main analyses to include all available studies. Contrary to our expectations, several studies reported long-term follow-up data only. Therefore, we decided to use the most complete results using the longest available follow-up data as primary outcome (i.e. we used these data for subsequent explorations of heterogeneity and robustness of findings in our sensitivity analyses). However, in accordance with the protocol, we report all results, using short-term data only (34 studies), long-term data only (26 studies), and using all available data (i.e. the longest available follow-up from 44 studies). The magnitude of SMD was interpreted as small (0.20 s.d. units), moderate (0.50 s.d. units), or large (0.80 s.d. units; Cohen, 1988). RRs were calculated for the drop-out rates between start and end of treatment: losses to follow-up were not considered. We used a 2-sided p < 0.05 to indicate statistical significance.
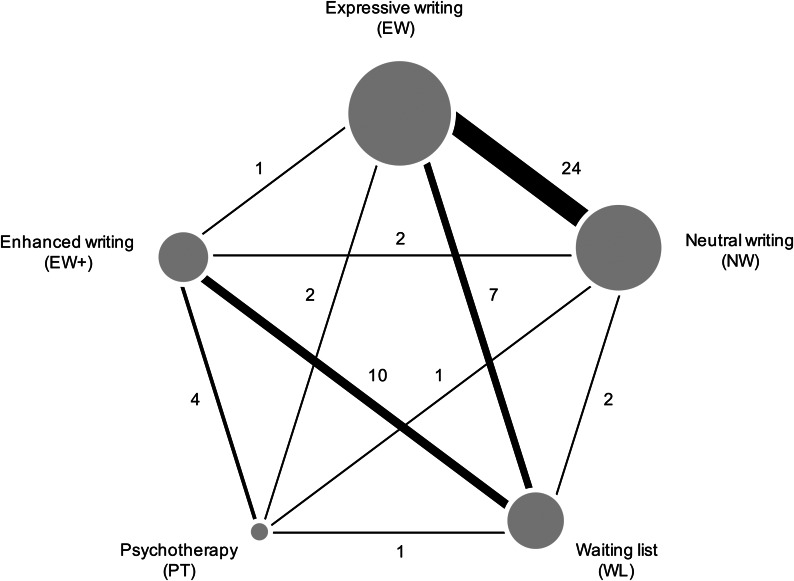
A network was created including five jointly randomizable treatments: 1st expressive writing (original; EW), 2nd enhanced expressive writing (EW+), 3rd PTSD psychotherapies (PT), and we included 4th neutral writing controls (NW), and 5th waiting list controls (WL). Network geometry was summarized in a graph which presents the five treatments as nodes (larger nodes indicate a larger number of studies per treatment), and the available comparisons between treatments as edges between the nodes (the thickness of the edges represents the number of available comparisons). We assumed that any patient that meets all inclusion criteria is likely, in principle, to be randomized to any of the interventions in the synthesis comparator set. We addressed the assumption of transitivity in the network meta-analysis (Salanti, 2012), by 1st assessing whether the included interventions are similar across studies using a different design, and 2nd checking whether the distribution of potential moderators is balanced across comparisons (Jansen & Naci, 2013).
We considered random-effects models rather than a fixed-effect model because the included studies were different with respect to clinical and other factors (see eTable 1). SMDs were calculated for all relevant comparisons within each study. In addition, indirect evidence was estimated using the entire network of evidence. To conduct network meta-analyses within a frequentist framework we used the package netmeta version 0.9–7 (Rücker, Schwarzer, Krahn, & König, 2018) for the open-source software environment R (version 3.5.1; R Core Team, 2018). The R function pairwise transformed the dataset to the contrast-based format, which is needed for conducting the network meta-analysis.
To express heterogeneity between studies the Q statistic was used (Cochran, 1950). Further τ2 was calculated to get an estimate of the variance between studies (Higgins, 2008). For the primary outcome a value of τ2 = 0.04 was considered as low heterogeneity, 0.09 as moderate and 0.16 as high heterogeneity (Borenstein, Hedges, Higgins, & Rothstein, 2011). In addition we used I2 as an indicator of the amount of observed variance that can be attributed to between-study heterogeneity (Higgins, Thompson, Deeks, & Altman, 2003) which can roughly be interpreted as follows: 0%–40%: might not be important; 30%–60%: may represent moderate heterogeneity; 50%–90%: may represent substantial heterogeneity; 75%–100%: considerable heterogeneity (Borenstein et al., 2011). In the network meta-analyses, we assumed a common estimate for the between-study heterogeneity variance across all included comparisons.
We used local, as well as global methods to detect inconsistency in the network (Efthimiou et al., 2016): 1st locally using the netsplit command (i.e. splitting direct and indirect evidence), and 2nd globally using the decomp.design command (i.e. using the design-by-treatment interaction model). We compared the magnitude of heterogeneity between consistency and inconsistency models to determine how much of the total heterogeneity was explained by inconsistency.
We conducted sensitivity analyses excluding studies with imputed standard deviations, studies with high indirectness ratings, studies that reported only observer-rated outcomes, studies that did not use established but rather experimental PTSD psychotherapies, and studies that included only patients who reported PTSD symptoms but not full or partial PTSD, in order to test the robustness of results.
Results
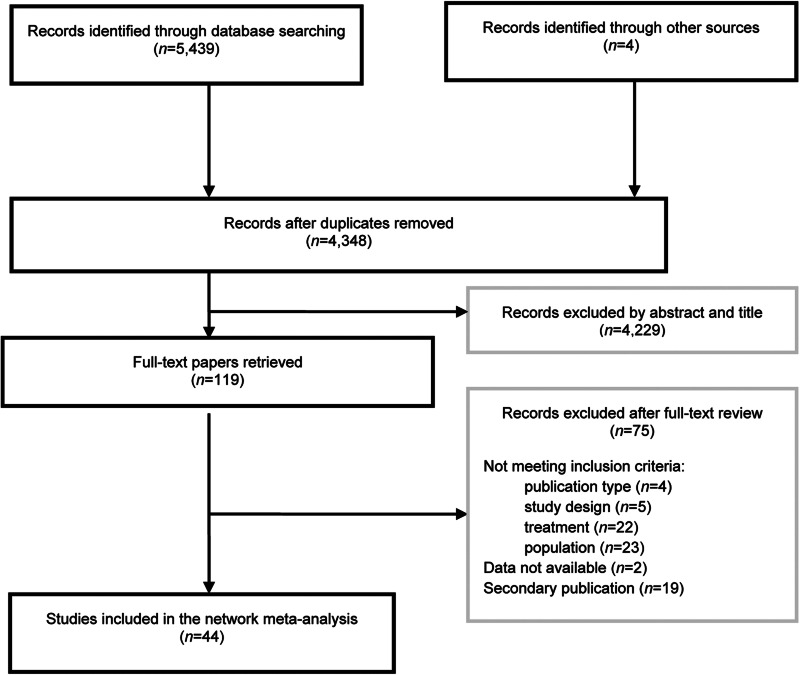
The systematic database search identified 5439 records. Following the title and abstract screening 119 full-text articles were considered potentially relevant. However, 44 RCTs* with a total of 7724 participants were included in our analyses (see Fig. 1). Nine included studies were publicly available dissertation theses. All included studies were published between 1996 and 2018, and were available in English. The time to last available follow-up ranged between 7 and 420 days with a median of 42 days (see eTable 1), and longer intervals for the last follow-up assessment were observed in studies with enhanced writing and psychotherapy (see eTable 2). Forty-one studies reported self-rated outcomes and three studies reported only observer-rated outcomes, two of which reported adequate blinding of outcome assessors, in one study with observer-rated outcomes we found no information regarding blinding of outcome assessors. Six studies used psychotherapeutic PTSD treatments as comparator including cognitive behavioural treatment (CBT) in one study, cognitive processing therapy (CPT) in two studies (Resick et al., 2008; Sloan, Marx, Lee, & Resick, 2018; van Emmerik, Kamphuis, & Emmelkamp, 2008), eye movement desensitization and reprocessing (EMDR) in one study (Largo-Marsh, 1996; Largo-Marsh & Spates, 2002), one study applied a psychotherapeutic approach described as active facilitator disclosure (Slavin-Spenny, Cohen, Oberleitner, & Lumley, 2011), which includes talking about the trauma experience and the emotions relating to that experience, as well as the identification of missing content in the participant's story, and one study applied a highly directive protocol aimed at promoting evidence-based processes to improve PTSD symptoms (Alessandri, 2017). In four studies experimental manipulations of the writing paradigm (e.g. instruction to focus on emotion v. on insights) were applied in addition to NW as control. In these cases, we combined the groups that used experimental manipulations (see eTable 1). In studies with psychotherapeutic PTSD treatments or waiting list control as comparator the proportion of participants with full or partial PTSD was larger (83.3% and 66.7%, respectively) than in the studies that used writing assignments as treatment (33.3% for EW and 32% for EW+) and neutral writing as comparator (30.4%; see eTable 2).
Fig. 1.
Flow chart of study inclusion.
We identified a network of treatments in which comparisons were available for all possible treatment combinations. This allowed for estimating inconsistency between direct and indirect evidence for each comparison. See Fig. 2 for the identified network of comparisons and eTable 1 for additional characteristics of the included studies.
Fig. 2.
Network of included comparisons. The size of the nodes indicates the number of studies per treatment. The thickness of the edges represents the number of comparisons between two treatment approaches.
RoB was considered moderate in 14 studies and high in 30 studies (eTable 3). Indirectness was considered low in eight studies, moderate in 27 studies and high in nine studies (eTable 4). The network meta-analyses relied mostly on evidence with moderate to high RoB and with moderate indirectness (see eFigs 1 and 2). Confidence in the network meta-analyses was considered moderate for one comparison and low for three comparisons (i.e. EW v. NW, EW+ v. WL, and EW+ v. PT; eTable 5).
We checked for baseline differences between PTSD scores and found PTSD scores to be significantly smaller in the EW+ groups compared with the WL groups with an SMD of −0.12 (95% CI −0.23 to −0.02; see Table 1 and eAppendix 3).
Table 1.
Comparative efficacy between active treatments and waiting list across different (sensitivity) analyses from network meta-analyses (SMD and 95% CI)
| Model | No. of studies (pairwise comparisons) | PT | EW+ | EW | NW | τ2 | I2 (%) | Inconsistency (p value) |
|---|---|---|---|---|---|---|---|---|
| Baseline (all studies in) | 44 (54) | −0.09 (−0.27 to 0.10) | −0.12 (−0.23 to −0.02) | −0.06 (−0.14 to 0.02) | −0.05 (−0.13 to 0.02) | 0 | 0 | 0.46 |
| Only end-of-treatment | 34 (36) | −1.03 (−1.49 to −0.56) | −0.90 (−1.19 to −0.62) | −0.40 (−0.81 to 0.01) | −0.36 (−0.81 to 0.09) | 0.17 | 73.8 | 0.005 |
| Only long-term | 26 (36) | −0.73 (−1.11 to −0.35) | −0.74 (−1.09 to −0.38) | −0.42 (−0.69 to −0.16) | −0.37 (−0.65 to −0.09) | 0.08 | 71.3 | <0.001 |
| Longest available FU (all studies in) | 44 (54) | −0.78 (−1.10 to −0.46) | −0.81 (−1.02 to −0.61) | −0.43 (−0.65 to −0.21) | −0.37 (−0.61 to −0.14) | 0.08 | 67.6 | <0.001 |
| Sensitivity analyses (longest available FU): | ||||||||
| comparisons EW+ v. WL excluded | 35 (45) | −0.52 (−0.84 to −0.19) | −0.41 (−0.72 to −0.10) | −0.29 (−0.49 to −0.09) | −0.22 (−0.43 to −0.001) | 0.05 | 55.8 | 0.03 |
| Studies with imputed data excluded | 40 (48) | −0.82 (−1.19 to −0.45) | −0.85 (−1.08 to −0.61) | −0.51 (−0.79 to −0.24) | −0.44 (−0.74 to −0.14) | 0.12 | 70.5 | <0.001 |
| Studies with high indirectness excluded | 35 (45) | −0.60 (−0.95 to −0.24) | −0.74 (−1.02 to −0.46) | −0.33 (−0.54 to −0.12) | −0.25 (−0.48 to −0.03) | 0.06 | 59.8 | 0.002 |
| Studies with observer-rated outcomes excluded | 41 (51) | −0.69 (−1.01 to −0.36) | −0.73 (−0.93 to −0.54) | −0.39 (−0.60 to −0.19) | −0.33 (−0.55 to −0.11) | 0.06 | 63.5 | <0.001 |
| Studies with experimental PTSD psychotherapies excluded | 42 (50) | −0.82 (−1.21 to −0.42) | −0.82 (−1.03 to −0.61) | −0.43 (−0.65 to −0.20) | −0.35 (−0.59 to −0.11) | 0.08 | 67.8 | <0.001 |
| Studies reporting only enhanced PTSD symptoms (no diagnosis) excluded | 19 (23) | −0.99 (−1.49 to −0.49) | −0.95 (−1.30 to −0.60) | −0.60 (−1.17 to −0.03) | −0.26 (−0.89 to 0.37) | 0.16 | 71.7 | 0.02 |
EW, expressive writing; EW+, enhanced writing; FU, follow-up; NW, neutral writing; PT, psychotherapy; WL, waiting list.
SMDs below 0 indicate superiority of a comparator over WL. SMDs above 0 indicate superiority of WL over a comparator. Statistically significant results are printed bold.
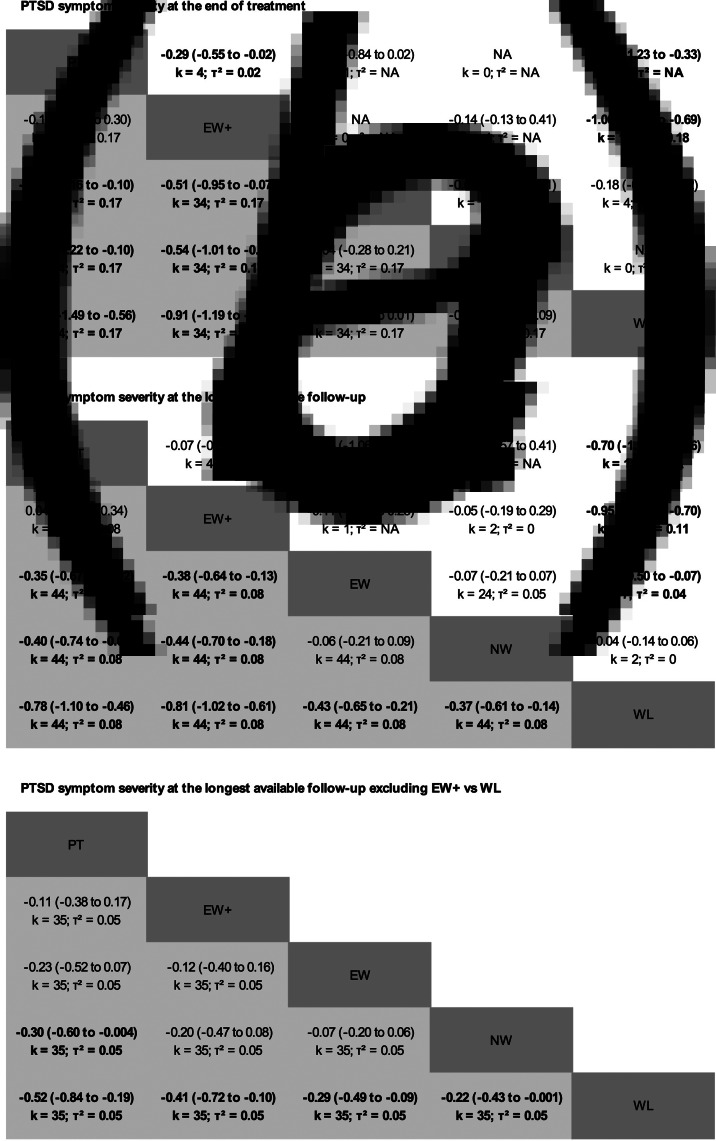
Comparative efficacy
At the end of treatment EW+ and PT were significantly more efficacious than EW, NW, and WL in reducing PTSD symptoms (Fig. 3a), and there were no significant differences between EW, NW, and WL observed (Fig. 3a and Table 1). We found evidence for very large between study heterogeneity (τ2 = 0.17) and significant inconsistency (Q = 14.78; df = 4; p = 0.005).
Fig. 3.
Comparative efficacy of expressive writing as compared with active and passive comparators. Results (SMD and 95% CI) on the comparative efficacy from network meta-analyses (grey) and from standard pairwise meta-analyses (white) at the end of treatment (a), at longest available follow-up including all 44 RCTs (b), and from the exploratory analyses excluding two-arm studies which directly compared EW+ with WL (c). To make network and pairwise meta-analysis results directly comparable, estimates are presented as column v. row for the network meta-analyses, and row v. column for the pairwise meta-analyses. Statistically significant results are printed in bold. EW, expressive writing; EW+, enhanced writing; CI, confidence interval; NW, neutral writing; PT, psychotherapy; SMD, standardised mean difference; WL, waiting list.
At the longest available follow-up superiority of EW+ and PT over EW, NW, and WL decreased slightly but was still statistically significant (Fig. 3b; Table 1). Also, EW and NW showed moderately sized significant superiority over WL in the long-term. We found moderate heterogeneity (τ2 = 0.08) and significant inconsistency (Q = 49.23; df = 10; p < 0.0001; eAppendix 4) in this analysis. Sensitivity analyses indicated some variation in the observed SMDs (Table 1). The general pattern of results, however, shows significant superiority of all active treatment groups over WL, and small to moderate differences between the active treatment groups (eAppendix 5). Pairwise meta-analyses confirmed this overall pattern (Figs 3a and b; eAppendix 6).
Exploratory findings excluding two-arm comparisons between EW+ and WL
In a post-hoc analysis we excluded two-arm studies that compared EW+ with WL because of the finding of significant baseline differences in this comparison (Table 1) and the observation that this comparison contributed considerably to the inconsistency observed in the network meta-analysis (see eAppendix 4). This analysis showed small to moderate significant superiority of all active treatments over WL (Fig. 3c; Table 1). PT was significantly superior over NW, and no significant differences were found between EW+, EW, and NW using longest available follow-up data (Fig. 3c). Heterogeneity was low to moderate in this analysis (τ2 = 0.05) and inconsistency was reduced but still significant (Q = 18.28; df = 9; p = 0.03).
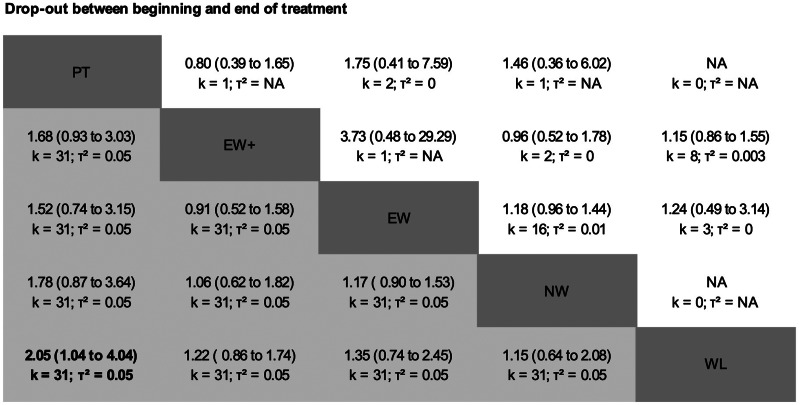
Comparative acceptability
With respect to the acceptability of treatments we observed significantly more drop-outs in PT as compared with WL (RR = 2.05, 1.04 to 4.04; Fig. 4). Between EW+, EW, NW, and WL no significant differences were observed (Fig. 4; eAppendix 7). We found low to moderate heterogeneity (τ2 = 0.05) and statistically non-significant inconsistency (Q = 3.28; df = 6; p = 0.77). Pairwise meta-analyses confirmed the statistically non-significant differences in drop-outs between the different treatment approaches (Fig. 4; eAppendix 8).
Fig. 4.
Comparative acceptability of expressive writing as compared with active and passive comparators. Results (RR and 95% CI) based on drop-out rates between beginning and end of treatment from network meta-analyses (grey) and standard pairwise meta-analyses (white). To make network and pairwise meta-analysis results directly comparable, estimates are presented as column v. row for the network meta-analyses, and row v. column for the pairwise meta-analyses. Statistically significant results are printed in bold. EW, expressive writing; EW+, enhanced writing; CI, confidence interval; NW, neutral writing; PT, psychotherapy; RR, relative risk; WL, waiting list.
Discussion
Our network meta-analysis addresses the comparative efficacy between expressive writing treatments as compared with psychotherapeutic PTSD treatments, neutral writing treatment and waiting list controls. In order to consider recent developments in writing treatments we classified them into those that referred to the original paradigm developed by Pennebaker & Beall (EW) and those that included additional elements assumed to increase their efficacy (i.e. therapist contact and more elaborated and structured instructions for the individual writing sessions; EW+). To the best of our knowledge this is the most comprehensive summary of RCTs on the efficacy of writing treatments on PTSD symptoms so-far. Using network-meta-analysis we were able to include all available comparisons between writing treatments and active as well as passive comparators in one statistical model. From a clinical perspective it is important to consider that most of the studies which used EW and EW+ as treatment included trauma survivors who reported some PTSD symptoms, but who would not qualify for a partial or full PTSD diagnosis.
Our results show that in the short-term EW+ and PT significantly outperformed EW, NW and WL, with EW and NW showing only small and non-significant superiority over WL. In the long-term, however, all active treatments outperformed WL significantly, with EW+ and PT again significantly outperforming EW and NW. It is important to note that the average duration of treatment and the number of treatment sessions were considerably higher in EW+ and PT as compared with EW and NW (see eTable 2). Thus, the amount of time spent in treatment is confounded with the type of treatment. Our analyses do not allow for conclusions whether the actual content of EW+ and PT or the time spent in treatment contributed most to the treatments' effects. The observed superiority of EW+ and PT was small to moderate and probably not of clinical significance (Stefanovics, Rosenheck, Jones, Huang, & Krystal, 2018). We found evidence for significantly more drop-out in PT as compared with WL. Although we aimed to extract data on treatment drop-outs only (as opposed to more general losses to follow-up), a huge variability in definitions and the reporting of drop-outs, but also different reasons for dropping out (e.g. occurrence of adverse effects v. symptom improvement) complicate data extraction, and in turn interpretations of these data with respect to treatment acceptability. Our analyses, including several sensitivity analyses, showed considerable variability between results from individual studies, as indicated by between study heterogeneity, but there were also differences between direct and indirect estimates of comparative efficacy, as indicated by significant inconsistency.
Based on previous reports (Mylle & Maes, 2004; Pavlacic, Buchanan, Maxwell, Hopke, & Schulenberg, 2019; Pietrzak et al., 2011, 2012) we conducted a sensitivity analysis in which we excluded studies which had reported only increased levels of PTSD symptoms (as opposed to full or partial PTSD diagnoses). We found somewhat larger effect sizes of PT, EW+ and EW in this analysis as compared to the main analysis, but also a considerable increase in heterogeneity, which hampers clear conclusions based on this analysis. Due to the observation that the studies comparing EW+ with WL showed significant differences at baseline already, and the observation that this particular comparison contributed considerably to network inconsistency, we conducted an exploratory analysis in which we excluded this respective comparison from the network. In this analysis, the superiority of EW+ and PT compared to EW, NW and WL was considerably reduced and superiority of EW+ and PT over EW and NW were no longer statistically significant. In this analysis heterogeneity was reduced to a small to moderate level.
Thus, when discussing our study findings, the studies comparing EW+ with WL need some additional attention. In general, the problems associated with the use of WL as control in psychotherapy RCTs has been described previously (Cuijpers & Cristea, 2016; Eysenck, 1993; Furukawa et al., 2014; Staines & Cleland, 2007). Unfortunately, despite the availability of a credible active control treatment in RCTs on writing treatments (i.e. the neutral writing control), which has typically been used in the earlier trials, more recent RCTs increasingly implemented WL as comparator. Accordingly, after excluding comparisons between EW+ and WL nine out of 15 RCTs using EW+ had to be excluded from the analyses. In addition to the problems associated with the use of WL controls, the nine two-arm RCTs using EW+ as treatment and WL as control are also prone to the so-called investigator or researcher allegiance bias. In all nine studies the authors were involved in the development of the EW+ treatment protocol, one of the strongest indicators of researcher allegiance (Munder, Gerger, Trelle, & Barth, 2011). The presence of strong researcher preferences in favour of the investigated treatment have been shown to be associated with larger benefits of the preferred treatment in psychotherapy RCTs (Gerger & Gaab, 2016; Munder, Brütsch, Leonhart, Gerger, & Barth, 2013), and this association has been shown to be mediated by low methodological quality of the RCTs (Munder et al., 2011). The choice of WL as comparator, instead of using a more credible active comparator may contribute to such bias.
Strengths and limitations
In network meta-analyses multiple comparisons between more than two treatment approaches are integrated in one analysis. This provides a more comprehensive overview regarding the comparative efficacy and acceptability of writing treatments in comparison to other treatment options, but also compared to passive and active comparators. This analytic approach allowed us to detect potential differences in the efficacy of the original and adapted writing treatments, and to check whether results are consistent across different research designs. We reduced the risk for the occurrence of publication bias by including published research articles but also publicly available dissertation theses. In order to warrant transitivity in the network we included only studies in which participants were randomly assigned to a writing intervention in at least one treatment group and to an additional comparator. We did however not include studies which directly compared only a psychotherapeutic PTSD treatment with a control treatment (e.g. waiting list) as these studies might differ from the writing intervention studies regarding clinical or methodological characteristics. Regarding the combination of different psychotherapeutic PTSD treatments in one node of the network, one could question whether the PTSD psychotherapies were similar enough with respect to their effects in order to be combined. A previous network meta-analysis demonstrated that there were no significant differences between treatment effects of EMDR, CBT, and CPT (Gerger et al., 2014). A sensitivity analysis in which we excluded two studies which used newly developed psychotherapeutic treatments (i.e. directive protocol and active facilitator writing) replicated the findings using all five studies which used psychotherapeutic PTSD treatments as comparators.
The most relevant limitation of our study is the observed heterogeneity and inconsistency. However, this observation reflects the diversity of findings reported in previous meta-analyses (Frattaroli, 2006; Frisina et al., 2004; Mogk et al., 2006; Smyth, 1998; Smyth & Pennebaker, 2008; van Emmerik et al., 2013). Unfortunately, even using the currently most elaborate statistical approach to summarize available research evidence (i.e. network meta-analysis) did not provide results that allow definite conclusions. However, using network meta-analysis we were able to show, that the superiority of PT and EW+ might be overestimated when 1st focusing on short-term results only, and 2nd when including mainly comparisons between EW+ and WL. A further limitation of our study is that we focused only on PTSD symptoms and treatment acceptance as outcomes, but ignored additional potentially relevant outcomes, for instance well-being, as well as additional indicators of potential harm, for instance adverse events.
It is important to note, that many of the included studies have to be considered underpowered, as a minimum of 64 participants per group would be needed in an RCT comparing a treatment with an active comparator and expecting a medium SMD of 0.50 with a desired power of 0.80 and a two-tailed p of 0.05 (Schnurr, 2007). The inclusion of underpowered trials in a meta-analysis increases the risk of biased results, partly due to the fact that underpowered studies with negative or non-significant findings have a smaller chance of being published (contributing to the so-called publication bias). We tried to minimize the impact of publication bias by including unpublished studies in addition to studies which were published in scientific journals.
Conclusions
In our network meta-analysis using data from the longest available follow-up assessments all active treatments (including NW) outperformed WL with small to moderate superiority of trauma-focused treatments (i.e. PT, EW+, EW) over NW. We found only small to moderate superiority of PT and EW+ over EW, which was statistically significant in some analyses, but probably not of clinical significance. We conclude that as it stands methodological issues to a considerable extent might explain the observed superiority of EW+ over EW. Definite conclusions are hampered to-date because of the predominant use of WL controls in EW+ RCTs, the lack of direct comparisons between the original EW and recently developed EW+, as well as a lack of RCTs investigating EW+ efficacy, which are conducted by independent researchers. Thus, particularly the superiority of EW+ over the original EW paradigm but also over NW controls await confirmation from adequately sized comparative RCTs preferably including all four active treatment approaches (i.e. EW, EW+, PT, and NW), reporting long-term data and including researchers with balanced preferences.
From a clinical perspective the potential of writing interventions to fill treatment gaps in mental health care by offering the possibility to treat patients with only minimal therapist contact is highly relevant and our analyses confirm significant benefits of writing treatments in improving PTSD symptoms. However, to date no definite conclusions are possible regarding the exact magnitude of these benefits, the increase in benefits by enhancing expressive writing with additional treatment components, and the effectiveness of writing treatments in comparison with PTSD psychotherapies.
Acknowledgements
We would like to thank Franziska Z'graggen who conducted a pilot study for this network meta-analysis.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291721000143.
click here to view supplementary material
Author contributions
Dr Gerger had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Gerger and Werner conceptualized and designed the study. Cuijpers, Gaab, Gerger, and Werner acquired, analysed or interpreted data. Gerger and Werner drafted the manuscript. Cuijpers, Gaab, Gerger, and Werner critically revised the manuscript for important intellectual content. Gerger performed statistical analyses. Gerger supervised the study.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
As the study did not involve human subjects no ethical approval was necessary.
References
*An asterisk indicates studies which were included in the meta-analyses.
- *Alessandri, F. T. (2017). Testing a brief directive intervention to reduce symptoms associated with trauma. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: : American Psychiatric Pub. [Google Scholar]
- American Psychological Association. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Retrieved from https://www.apa.org/about/offices/directorates/guidelines/ptsd.pdf.
- Andersson, M. A., & Conley, C. S. (2008). Expecting to heal through self-expression: A perceived control theory of writing and health. Health Psychology Review, 2, 138–162. doi: 10.1080/17437190802660890. [DOI] [Google Scholar]
- Andersson, M. A., & Conley, C. S. (2013). Optimizing the perceived benefits and health outcomes of writing about traumatic life events. Stress and Health: Journal of the International Society for the Investigation of Stress, 29, 40–49. doi: 10.1002/smi.2423. [DOI] [PubMed] [Google Scholar]
- *Barry, L. M. (2001). The benefits of journal writing: reducing maternal psychological distress levels after the Neonatal Intensive Care Unit. Dissertation Abstracts International Section A: Humanities and Social Sciences. [Google Scholar]
- *Batten, S. V. (2001). Testing the effects of a written disclosure task with sexual abuse survivors. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- *Beyer, J. A. (2011). The effects of web-based interactive emotional disclosure on stress and health: A randomized, controlled study. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2011). Introduction to meta-analysis. Chichester, UK: John Wiley & Sons. [Google Scholar]
- *Bugg, A., Turpin, G., Mason, S., & Scholes, C. (2009). A randomised controlled trial of the effectiveness of writing as a self-help intervention for traumatic injury patients at risk of developing post-traumatic stress disorder. Behaviour Research and Therapy, 47, 6–12. doi: 10.1016/j.brat.2008.10.006. [DOI] [PubMed] [Google Scholar]
- Burton, C. M., & King, L. A. (2004). The health benefits of writing about intensely positive experiences. Journal of Research in Personality, 38, 150–163. doi: 10.1016/S0092-6566(03)00058-8. [DOI] [Google Scholar]
- Cochran, W. G. (1950). The comparison of percentages in matched samples. Biometrika, 37, 256–266. doi: 10.1093/biomet/37.3-4.256 14801052. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the social sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cuijpers, P., & Cristea, I. (2016). How to prove that your therapy is effective, even when it is not: A guideline. Epidemiology and Psychiatric Sciences, 25, 428–435. doi: 10.1017/S2045796015000864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Deters, P. B., & Range, L. M. (2003). Does writing reduce posttraumatic stress disorder symptoms? Violence and Victims, 18, 569. doi: 10.1891/vivi.2003.18.5.569. [DOI] [PubMed] [Google Scholar]
- de Vries, G.-J., & Olff, M. (2009). The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. Journal of Traumatic Stress, 22, 259–267. doi: 10.1002/jts.20429. [DOI] [PubMed] [Google Scholar]
- Efthimiou, O., Debray, T. P., van Valkenhoef, G., Trelle, S., Panayidou, K., & Moons, K. G., … Get Real Methods Research Group (2016). Getreal in network meta-analysis: A review of the methodology. Research Synthesis Methods, 7, 236–263. doi: 10.1002/jrsm.1195. [DOI] [PubMed] [Google Scholar]
- Eysenck, H. (1993). Forty years on: The outcome problem in psychotherapy revised. In Giles T. R. (Ed.), Handbook of effective psychotherapy (pp. 3–20). New York: Plenum Press. [Google Scholar]
- Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (2009). Effective treatments for PTSD: Practice guidelines from the international society for traumatic stress studies (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Forbes, D., Creamer, M., Bisson, J. I., Cohen, J. A., Crow, B. E., Foa, E. B., … Ursano, R. J. (2010). A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress, 23, 537–552. doi: 10.1002/jts.20565. [DOI] [PubMed] [Google Scholar]
- Forbes, D., Creamer, M., Phelps, A., Bryant, R., McFarlane, A. C., Devilly, G. J., … Newton, S. (2007). Australian guidelines for the treatment of adults with acute stress disorder and post-traumatic stress disorder. Australian and New Zealand Journal of Psychiatry, 41, 637–648. doi: 10.1080/00048670701449161. [DOI] [PubMed] [Google Scholar]
- Frattaroli, J. (2006). Experimental disclosure and its moderators: A meta-analysis. Psychological Bulletin, 132, 823. doi: 10.1037/0033-2909.132.6.823. [DOI] [PubMed] [Google Scholar]
- Frayne, S. M., Seaver, M. R., Loveland, S., Christiansen, C. L., Spiro III, A., Parker, V. A., & Skinner, K. M. (2004). Burden of medical illness in women with depression and posttraumatic stress disorder. Archives of Internal Medicine, 164, 1306–1312. doi: 10.1001/archinte.164.12.1306. [DOI] [PubMed] [Google Scholar]
- *Freyd, J. J., Klest, B., & Allard, C. B. (2005). Betrayal trauma: Relationship to physical health, psychological distress, and a written disclosure intervention. Journal of Trauma & Dissociation, 6, 83–104. doi: 10.1300/J229v06n03_04. [DOI] [PubMed] [Google Scholar]
- Frisina, P. G., Borod, J. C., & Lepore, S. J. (2004). A meta-analysis of the effects of written emotional disclosure on the health outcomes of clinical populations. Journal of Nervous and Mental Disease, 192, 629–634. doi: 10.1097/01.nmd.0000138317.30764.63. [DOI] [PubMed] [Google Scholar]
- Furukawa, T., Noma, H., Caldwell, D., Honyashiki, M., Shinohara, K., Imai, H., … Churchill, R. (2014). Waiting list may be a nocebo condition in psychotherapy trials: A contribution from network meta-analysis. Acta Psychiatrica Scandinavica, 130, 181–192. doi: 10.1111/acps.12275. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy, I. R., & Bryant, R. A. (2013). 636120 Ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8, 651–662. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- Gerger, H., & Gaab, J. (2016). Researcher allegiance as hidden moderator in psychohterapy outcome research. Verhaltenstherapie, 26, 41–45. doi: 10.1159/000443543. [DOI] [Google Scholar]
- Gerger, H., Gaab, J., & Werner, C. (2018). A network meta-analysis on the efficacy and acceptability of writing interventions for traumatised adults. PROSPERO International Prospective Register of Systematic Reviews. Retrieved from https://www.crd.york.ac.uk/prospero/.
- Gerger, H., Munder, T., Gemperli, A., Nüesch, E., Trelle, S., Jüni, P., & Barth, J. (2014). Integrating fragmented evidence by network meta-analysis: Relative effectiveness of psychological interventions for adults with post-traumatic stress disorder. Psychological Medicine, 44, 3151–3164. doi: 10.1017/S0033291714000853. [DOI] [PubMed] [Google Scholar]
- *Gidron, Y., Peri, T., Connolly, J. F., & Shalev, A. Y. (1996). Written disclosure in posttraumatic stress disorder: Is it beneficial for the patient? Journal of Nervous and Mental Disease, 184, 505–507. doi: 10.1097/00005053-199608000-00009. [DOI] [PubMed] [Google Scholar]
- *Greenberg, M. A., Wortman, C. B., & Stone, A. A. (1996). Emotional expression and physical health: Revising traumatic memories or fostering self-regulation? Journal of Personality and Social Psychology, 71, 588–602. doi: 10.1037//0022-3514.71.3.588. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H., Oxman, A. D., Kunz, R., Woodcock, J., Brozek, J., Helfand, M., … Vist, G. (2011). GRADE Guidelines: 8. Rating the quality of evidence – indirectness. Journal of Clinical Epidemiology, 64, 1303–1310. doi: 10.1016/j.jclinepi.2011.04.014. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T. (2008). Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. International Journal of Epidemiology, 37, 1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Green, S. (updated March 2011). Cochrane handbook for systematic reviews of interventions. Retrieved from www.cochrane-handbook.org.
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327, 557–560. doi: 10.1136/bmj.327.7414.55712958120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Horsch, A., Tolsa, J.-F., Gilbert, L., Du Chêne, L. J., Müller-Nix, C., & Graz, M. B. (2016). Improving maternal mental health following preterm birth using an expressive writing intervention: A randomized controlled trial. Child Psychiatry and Human Development, 47, 780–791. doi: 10.1007/s10578-015-0611-6. [DOI] [PubMed] [Google Scholar]
- Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., … Jansen, J. P. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Annals of Internal Medicine, 162, 777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2008). Treatment of posttraumatic stress disorder: An assessment of the evidence. Washington, DC: National Academies Press. [Google Scholar]
- *Ironson, G., O'Cleirigh, C., Leserman, J., Stuetzle, R., Fordiani, J., Fletcher, M., & Schneiderman, N. (2013). Gender-specific effects of an augmented written emotional disclosure intervention on posttraumatic, depressive, and HIV-disease-related outcomes: A randomized, controlled trial. Journal of Consulting and Clinical Psychology, 81, 284–298. doi: 10.1037/a0030814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen, J. P., & Naci, H. (2013). Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Medicine, 11, 159. doi: 10.1186/1741-7015-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jensen-Johansen, M. B., Christensen, S., Valdimarsdottir, H., Zakowski, S., Jensen, A. B., Bovbjerg, D. H., & Zachariae, R. (2013). Effects of an expressive writing intervention on cancer-related distress in Danish breast cancer survivors – results from a nationwide randomized clinical trial. Psycho-Oncology, 22, 1492–1500. doi: 10.1002/pon.3193. [DOI] [PubMed] [Google Scholar]
- *Kearns, M. C., Edwards, K. M., Calhoun, K. S., & Gidycz, C. A. (2010). Disclosure of sexual victimization: The effects of Pennebaker's emotional disclosure paradigm on physical and psychological distress. Journal of Trauma & Dissociation, 11, 193–209. doi: 10.1080/15299730903502979. [DOI] [PubMed] [Google Scholar]
- Kenardy, J., & Tan, L.-J. (2006). The role of avoidance coping in the disclosure of trauma. Behaviour Change, 23, 42–54. doi: 10.1375/bech.23.1.42. [DOI] [Google Scholar]
- *Kersting, A., Dolemeyer, R., Steinig, J., Walter, F., Kroker, K., Baust, K., & Wagner, B. (2013). Brief internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: A randomized controlled trial. Psychotherapy and Psychosomatics, 82, 372–381. doi: 10.1159/000348713. [DOI] [PubMed] [Google Scholar]
- *Kersting, A., Kroker, K., Schlicht, S., Baust, K., & Wagner, B. (2011). Efficacy of cognitive behavioral internet-based therapy in parents after the loss of a child during pregnancy: Pilot data from a randomized controlled trial. Archives of Women's Mental Health, 14, 465–477. doi: 10.1007/s00737-011-0240-4. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry, 61, 4–14. [PubMed] [Google Scholar]
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H.-U. (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- *Knaevelsrud, C., Böttche, M., Pietrzak, R. H., Freyberger, H. J., & Kuwert, P. (2017). Efficacy and feasibility of a therapist-guided internet-based intervention for older persons with childhood traumatization: A randomized controlled trial. American Journal of Geriatric Psychiatry, 25, 878–888. doi: 10.1016/j.jagp.2017.02.024. [DOI] [PubMed] [Google Scholar]
- *Knaevelsrud, C., Brand, J., Lange, A., Ruwaard, J., & Wagner, B. (2015). Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: Randomized controlled trial. Journal of Medical Internet Research, 17, e71. doi: 10.2196/jmir.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Knaevelsrud, C., & Maercker, A. (2007). Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: A randomized controlled clinical trial. BMC Psychiatry, 7, 13. doi: 10.1186/1471-244X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Koopman, C., Ismailji, T., Holmes, D., Classen, C. C., Palesh, O., & Wales, T. (2005). The effects of expressive writing on pain, depression and posttraumatic stress disorder symptoms in survivors of intimate partner violence. Journal of Health Psychology, 10, 211–221. doi: 10.1177/1359105305049769. [DOI] [PubMed] [Google Scholar]
- Krysinska, K., & Lester, D. (2010). Post-traumatic stress disorder and suicide risk: A systematic review. Archives of Suicide Research, 14, 1–23. doi: 10.1080/13811110903478997. [DOI] [PubMed] [Google Scholar]
- Kuester, A., Niemeyer, H., & Knaevelsrud, C. (2016). Internet-based interventions for posttraumatic stress: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 43, 1–16. doi: 10.1016/j.cpr.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t tests and ANOVAs. Frontiers in Psychology, 4, 863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lange, A., Rietdijk, D., Hudcovicova, M., van de Ven, J.-P., Schrieken, B., & Emmelkamp, P. M. (2003). Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. Journal of Consulting and Clinical Psychology, 71, 901–909. doi: 10.1037/0022-006X.71.5.901. [DOI] [PubMed] [Google Scholar]
- *Lange, A., van de Ven, J.-P., Schrieken, B., & Emmelkamp, P. M. (2001). Interapy. Treatment of posttraumatic stress through the Internet: A controlled trial. Journal of Behavior Therapy and Experimental Psychiatry, 32, 73–90. doi: 10.1016/S0005-7916(01)00023-4. [DOI] [PubMed] [Google Scholar]
- *Largo-Marsh, L. K. (1996). The relationships among expectancy, hypnotizability, and treatment outcome associated with eye movement desensitization in the treatment of post-traumatic stress disorder. Dissertaton. [Google Scholar]
- *Largo-Marsh, L. K., & Spates, C. (2002). The effects of writing therapy in comparison to EMD/R on traumatic stress: The relationship between hypnotizability and client expectancy to outcome. Professional Psychology, Research and Practice, 33, 581–586. doi: 10.1037/0735-7028.33.6.581. [DOI] [Google Scholar]
- Lewis, S. J., Arseneault, L., Caspi, A., Fisher, H. L., Matthews, T., Moffitt, T. E., … Danese, A. (2019). The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. The Lancet Psychiatry, 6, 247–256. doi.org/10.1016/S2215-0366(19)30031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lichtenthal, W. G., & Cruess, D. G. (2010). Effects of directed written disclosure on grief and distress symptoms among bereaved individuals. Death Studies, 34, 475–499. doi: 10.1080/07481187.2010.483332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebschutz, J., Saitz, R., Brower, V., Keane, T. M., Lloyd-Travaglini, C., Averbuch, T., & Samet, J. H. (2007). PTSD In urban primary care: High prevalence and low physician recognition. Journal of General Internal Medicine, 22, 719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Thousand Oaks, CA: Sage. [Google Scholar]
- Marshall, R. D., Olfson, M., Hellman, F., Blanco, C., Guardino, M., & Struening, E. L. (2001). Comorbidity, impairment, and suicidality in subthreshold PTSD. American Journal of Psychiatry, 158, 1467–1473. doi: 10.1176/appi.ajp.158.9.1467. [DOI] [PubMed] [Google Scholar]
- *Milbury, K., Spelman, A., Wood, C., Matin, S. F., Tannir, N., Jonasch, E., … Cohen, L. (2014). Randomized controlled trial of expressive writing for patients with renal cell carcinoma. Journal of Clinical Oncology, 32, 663. doi: 10.1200/JCO.2013.50.3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogk, C., Otte, S., Reinhold-Hurley, B., & Kröner-Herwig, B. (2006). Health effects of expressive writing on stressful or traumatic experiences-a meta-analysis. GMS Psycho-Social-Medicine, 3, 1–9. [PMC free article] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., Altmann, D. G., & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munder, T., Brütsch, O., Leonhart, R., Gerger, H., & Barth, J. (2013). Researcher allegiance in psychotherapy outcome research: An overview of reviews. Clinical Psychology Review, 33, 501–511. doi: 10.1016/j.cpr.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Munder, T., Gerger, H., Trelle, S., & Barth, J. (2011). Testing the allegiance bias hypothesis: A meta-analysis. Psychotherapy Research, 21, 670–684. doi: 10.1080/10503307.2011.602752. [DOI] [PubMed] [Google Scholar]
- Mylle, J., & Maes, M. (2004). Partial posttraumatic stress disorder revisited. Journal of Affective Disorders, 78, 37–48. doi: 10.1016/s0165-0327(02)00218-5. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. (2005). Post-traumatic stress disorder: management. Retrieved from https://www.nice.org.uk/guidance/cg26. [PubMed]
- *Nguyen, D. D. (2005). The effects of expressive writing on the psychological and physical well-being of Vietnamese ex-political detainees. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- Norris, F. H., & Slone, L. B. (2007). The epidemiology of trauma and PTSD. In Friedman M. J., Keane T. M. & Resick P. A. (Eds.), Handbook of PTSD: Science and practice (pp. 78–98). New York: Guilford Press. [Google Scholar]
- Pavlacic, J. M., Buchanan, E. M., Maxwell, N. P., Hopke, T. G., & Schulenberg, S. E. (2019). A meta-analysis of expressive writing on posttraumatic stress, posttraumatic growth, and quality of life. Review of General Psychology, 23, 230–250. doi: 10.1177/1089268019831645. [DOI] [Google Scholar]
- Pennebaker, J. W., & Beall, S. K. (1986). Confronting a traumatic event: Toward an understanding of inhibition and disease. Journal of Abnormal Psychology, 95, 274. doi: 10.1037//0021-843x.95.3.274. [DOI] [PubMed] [Google Scholar]
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Medical comorbidity of full and partial posttraumatic stress disorder in United States adults: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Psychosomatic Medicine, 73, 697. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2012). Psychiatric comorbidity of full and partial posttraumatic stress disorder among older adults in the United States: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. The American Journal of Geriatric Psychiatry, 20, 380–390. doi: 10.1097/JGP.0b013e31820d92e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Possemato, K. A. (2008). An internet-based expressive writing intervention for kidney transplant recipients. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- *Possemato, K., Ouimette, P., & Geller, P. A. (2010). Internet-based expressive writing for kidney transplant recipients: Effects on posttraumatic stress and quality of life. Traumatology, 16, 49–54. doi: 10.1177/1534765609347545. [DOI] [Google Scholar]
- Ramirez, G., & Beilock, S. L. (2011). Writing about testing worries boosts exam performance in the classroom. Science (New York, N.Y.), 331, 211–213. doi: 10.1126/science.1199427. [DOI] [PubMed] [Google Scholar]
- *Resick, P. A., Galovski, T. E., Uhlmansiek, M. O. B., Scher, C. D., Clum, G. A., & Young-Xu, Y. (2008). A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76, 243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, B. F., Weisberg, R. B., Pagano, M. E., Machan, J. T., Culpepper, L., & Keller, M. B. (2003). Mental health treatment received by primary care patients with posttraumatic stress disorder. The Journal of Clinical Psychiatry, 64, 1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rücker, G., Schwarzer, G., Krahn, U., & König, J. (2018). netmeta: network meta-analysis using requentist methods. R package version 0.9-8. Retrieved from https://CRAN.R-project.org/package=netmeta.
- Salanti, G. (2012). Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: Many names, many benefits, many concerns for the next generation evidence synthesis tool. Research Synthesis Methods, 3, 80–97. doi: 10.1002/jrsm.1037. [DOI] [PubMed] [Google Scholar]
- Salanti, G., Del Giovane, C., Chaimani, A., Caldwell, D. M., & Higgins, J. P. T. (2014). Evaluating the quality of evidence from a network meta-analysis. PLoS ONE, 9, e99682. doi: 10.1371/journal.pone.0099682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sayer, N. A., Noorbaloochi, S., Frazier, P. A., Pennebaker, J. W., Orazem, R. J., Schnurr, P. P., … Litz, B. T. (2015). Randomized controlled trial of online expressive writing to address readjustment difficulties among U.S Afghanistan and Iraq war veterans. Journal of Traumatic Stress, 28, 381–390. doi: 10.1002/jts.22047. [DOI] [PubMed] [Google Scholar]
- Schnurr, P. P. (2007). The rocks and hard places in psychotherapy outcome research. Journal of Traumatic Stress, 20, 779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- *Schoutrop, M. J., Lange, A., Hanewald, G., Davidovich, U., & Salomon, H. (2002). Structured writing and processing major stressful events: A controlled trial. Psychotherapy and Psychosomatics, 71, 151–157. doi: 10.1159/000056282. [DOI] [PubMed] [Google Scholar]
- *Slavin-Spenny, O. M., Cohen, J. L., Oberleitner, L. M., & Lumley, M. A. (2011). The effects of different methods of emotional disclosure: Differentiating post-traumatic growth from stress symptoms. Journal of Clinical Psychology, 67, 993–1007. doi: 10.1002/jclp.20750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sloan, D. M., & Marx, B. P. (2004). A closer examination of the structured written disclosure procedure. Journal of Consulting and Clinical Psychology, 72, 165–175. doi: 10.1037/0022-006X.72.2.165. [DOI] [PubMed] [Google Scholar]
- *Sloan, D. M., Marx, B. P., Bovin, M. J., Feinstein, B. A., & Gallagher, M. W. (2012). Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy, 50, 627–635. doi: 10.1016/j.brat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sloan, D. M., Marx, B. P., & Epstein, E. M. (2005). Further examination of the exposure model underlying the efficacy of written emotional disclosure. Journal of Consulting and Clinical Psychology, 73, 549–554. doi: 10.1037/0022-006X.73.3.549. [DOI] [PubMed] [Google Scholar]
- *Sloan, D. M., Marx, B. P., Epstein, E. M., & Lexington, J. M. (2007). Does altering the writing instructions influence outcome associated with written disclosure? Behavior Therapy, 38, 155–168. doi: 10.1016/j.beth.2006.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sloan, D. M., Marx, B. P., & Greenberg, E. M. (2011). A test of written emotional disclosure as an intervention for posttraumatic stress disorder. Behaviour Research and Therapy, 49, 299–304. doi: 10.1016/j.brat.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sloan, D. M., Marx, B. P., Lee, D. J., & Resick, P. A. (2018). A brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry, 75, 233–239. doi: 10.1001/jamapsychiatry.2017.4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth, J. M. (1998). Written emotional expression: Effect sizes, outcome types, and moderating variables. Journal of Consulting and Clinical Psychology, 66, 174. doi: 10.1037//0022-006x.66.1.174. [DOI] [PubMed] [Google Scholar]
- *Smyth, J. M., Hockemeyer, J. R., & Tulloch, H. (2008). Expressive writing and post-traumatic stress disorder: Effects on trauma symptoms, mood states, and cortisol reactivity. British Journal of Health Psychology, 13, 85–93. doi: 10.1348/135910707X250866. [DOI] [PubMed] [Google Scholar]
- Smyth, J. M., & Pennebaker, J. W. (2008). Exploring the boundary conditions of expressive writing: In search of the right recipe. British Journal of Health Psychology, 13, 1–7. doi: 10.1348/135910707X260117. [DOI] [PubMed] [Google Scholar]
- *Southern, D. S. (2014). Use of expressive writing to mediate the effects of PTSD symptomology on female domestic violence victims. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- Staines, G. L., & Cleland, C. M. (2007). Bias in meta-analytic estimates of the absolute efficacy of psychotherapy. Review of General Psychology, 11, 329–347. doi: 10.1037/1089-2680.11.4.329. [DOI] [Google Scholar]
- Stefanovics, E. A., Rosenheck, R. A., Jones, K. M., Huang, G., & Krystal, J. H. (2018). Minimal clinically important differences (MCID) in assessing outcomes of post-traumatic stress disorder. Psychiatric Quarterly, 89, 141–155. doi: 10.1007/s11126-017-9522-y. [DOI] [PubMed] [Google Scholar]
- Stein, M. B., Walker, J. R., Hazen, A. L., & Forde, D. R. (1997). Full and partial posttraumatic stress disorder: Findings from a community survey. The American Journal of Psychiatry, 154, 1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- *Stockton, H., Joseph, S., & Hunt, N. (2014). Expressive writing and posttraumatic growth: An internet-based study. Traumatology: An International Journal, 20, 75. [Google Scholar]
- *Thompson-Hollands, J., Marx, B. P., Lee, D. J., Resick, P. A., & Sloan, D. M. (2018). Long-term treatment gains of a brief exposure-based treatment for PTSD. Depression and Anxiety, 35, 985–991. doi: 10.1002/da.22825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tondorf, T., Kaufmann, L.-K., Degel, A., Locher, C., Birkhäuer, J., Gerger, H., … Gaab, J. (2017). Employing open/hidden administration in psychotherapy research: A randomized-controlled trial of expressive writing. PLoS ONE, 12, e0187400. doi: 10.1371/journal.pone.0187400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Truijens, F. L., & van Emmerik, A. A. (2014). Visual feedback in written imaginal exposure for posttraumatic stress: A preliminary study. Journal of Loss and Trauma, 19, 403–415. doi: 10.1080/15325024.2013.794664. [DOI] [Google Scholar]
- *van Emmerik, A. A., Kamphuis, J. H., & Emmelkamp, P. M. (2008). Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: A randomized controlled trial. Psychotherapy and Psychosomatics, 77, 93–100. doi: 10.1159/000112886. [DOI] [PubMed] [Google Scholar]
- van Emmerik, A. A., Reijntjes, A., & Kamphuis, J. H. (2013). Writing therapy for posttraumatic stress: A meta-analysis. Psychotherapy and Psychosomatics, 82, 82–88. doi: 10.1159/000343131. [DOI] [PubMed] [Google Scholar]
- *Wagner, B., Knaevelsrud, C., & Maercker, A. (2006). Internet-based cognitive-behavioral therapy for complicated grief: A randomized controlled trial. Death Studies, 30, 429–453. doi: 10.1080/07481180600614385. [DOI] [PubMed] [Google Scholar]
- Wittchen, H. U., Jacobi, F., Rehm, J., Gustavsson, A., Svensson, M., Jonsson, B., … Steinhausen, H. C. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21, 655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013). Guidelines for the management of conditions specifically related to stress. Retrieved from http://www.who.int/mental_health/emergencies/stress_guidelines/en/. [PubMed]
- *Yanko, J. I. (2001). The effects of indirect versus direct disclosure of traumatic experience on psychological and physical well-being. Dissertation Abstracts International: Section B: The Sciences and Engineering. [Google Scholar]
- *Zakowski, S. G., Herzer, M., Barrett, S. D., Milligan, J. G., & Beckman, N. (2011). Who benefits from emotional expression? An examination of personality differences among gynaecological cancer patients participating in a randomized controlled emotional disclosure intervention trial. British Journal of Psychology, 102, 355–372. doi: 10.1348/000712610X524949. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291721000143.
click here to view supplementary material