Abstract
Objectives
The aim of this mixed-method study was to explore maintenance of physical activity and health effects one year after completion of exercise interventions in transport and leisure-time domains of everyday life. We hypothesised that routinisation of active commuting would lead to better maintenance of physical activity and health effects compared with leisure-time exercise.
Study design
Mixed-methods follow-up study.
Methods
Individuals with overweight/obesity, who completed a 6-month exercise intervention (active commuting by bike (BIKE), moderate (MOD) or vigorous intensity leisure-time exercise (VIG)), were after one year invited to participate in a follow-up visit which included measurements of cardiorespiratory fitness during an incremental bicycle test and body composition using dual-energy X-ray absorptiometry. Variability in maintenance practices was assessed in a sub-sample of participants who experienced the greatest improvements (‘VO2peak improvers’) and reductions (‘VO2peak reducers’), respectively, in cardiorespiratory fitness. Semi-structured interviews were conducted (15–30 min) and analysed using systematic text condensation to identify barriers and facilitators associated with maintenance of physical activity.
Results
Out of the 74 participants completing an exercise intervention, 46 (62%) completed follow-up (BIKE: n = 14; MOD: n = 14; VIG: n = 18). Improvements in VO2peak and reductions in fat mass were maintained in BIKE and VIG. Body weight decreased in BIKE and fat free mass increased in VIG. Changes in VO2peak and anthropometry at follow-up did not differ between BIKE and MOD + VIG. Fat mass decreased and recreational physical activity increased in ‘VO2peak improvers’. Findings from the interviews suggested that self-monitoring, collective exercising, and new personal exercise challenges facilitate maintenance of a physically active lifestyle.
Conclusion
Completion of a structured exercise intervention consisting of 6 months of active commuting or vigorous intensity leisure-time exercise was associated with long-term maintenance of improvements in VO2peak and body composition, whereas moderate intensity leisure-time exercise was not. In contrast to our hypothesis, active commuting was not associated with better maintenance of physical activity and health effects after the intervention compared with leisure-time exercise.
Keywords: Exercise, Exercise maintenance, Physical activity, Follow-up, Overweight, Obesity
1. Introduction
Physical inactivity and overweight are among the most significant public health challenges today, inarguably associated with mortality and increased risk of non-communicable diseases such as cardiovascular disease and type 2 diabetes [1,2]. Hence, effective strategies for encouraging people to initiate and maintain a physically active lifestyle are much needed. Physical activity takes place in different domains of everyday life e.g., during commuting and leisure-time activities. It may be challenging to obtain sufficient physical activity during leisure-time [3] and it has been suggested that active commuting represents a promising alternative to leisure-time exercise to increase physical activity in physically inactive individuals [4]. Large observational studies have reported associations between active commuting and lower mortality [5] and degree of adiposity [[6], [7], [8]], higher fitness [8], and better cardiovascular profile [8,9] even when controlling for leisure-time physical activity. If time spent physically inactive during commuting e.g., by car is replaced by active commuting it may be a time-efficient way to increase physical activity in everyday life where time constraints likely are barriers to meet physical activity guidelines in leisure-time only.
Structured exercise interventions can improve important health outcomes, including cardiorespiratory fitness and body composition, and encourage and help people to adopt regular exercise during the intervention [[10], [11], [12], [13], [14], [15]]. However, few structured exercise intervention studies include long-term follow-up and little is known about how behavioural changes and health improvements are maintained [16]. This follow-up study aimed to investigate exercise practices and health outcomes after different exercise interventions in previously physically inactive individuals with overweight and obesity. Specifically, we aimed to 1) assess maintenance of cardiorespiratory fitness and body composition one year after a 6-month exercise trial, 2) assess participants' recent physical activity at follow-up, and 3) explore what facilitated and hindered participants’ engagements in physical activity post-intervention. We hypothesised that routinisation of active commuting during and after the intervention would lead to maintenance of physical activity and health effects at follow-up to a greater degree than leisure-time exercise.
2. Methods
This article reports results from a follow-up study completed after the GO-ACTIWE randomised controlled trial [17]. The study was conducted in accordance with the Declaration of Helsinki, approved by the Ethical Committee of The Capital Region of Denmark (H-4-2013-108) and registered at the Danish Data Protection and clinicaltrials.gov (NCT01962259 and NCT01973686). Participants received written and oral information about the trial and follow-up study and signed informed consent before a screening visit which included assessment of medical history and inclusion and exclusion criteria as described previously [15,17]. The informed consent covered both the trial and the follow-up study.
2.1. Randomised controlled trial
Briefly, 130 physically inactive women and men (20–45 years) with overweight/obesity (BMI: 25–35 kg/m2) were randomised to 6 months of habitual lifestyle (CON, n = 18), or one of three exercise groups: 1) active commuting by bike to and from work/school at a self-chosen intensity (BIKE, n = 35), 2) leisure-time exercise of moderate (MOD, 50% peak oxygen uptake (VO2peak)-reserve, n = 39) or 3) vigorous intensity (VIG, 70% VO2peak-reserve, n = 38). Exercise was prescribed 5 days/week with exercise energy expenditure at 320 kcal/day for women and 420 kcal/day for men. Participants in BIKE were offered bikes, and participants in MOD and VIG received a fitness centre membership and aerobic exercise instructions (e.g., cycling, running, or rowing). After the trial, participants had the opportunity to keep the bikes and heart rate monitors in exchange for a reduction in the honorarium. Participants in MOD and VIG had free access to the fitness centre for 6 months post-intervention. Results from the trial are published elsewhere [14,15,[18], [19], [20], [21], [22]].
2.2. Follow-up study
One year after completing the trial, participants from the three intervention groups were invited to a follow-up visit. Participants and staff were not in contact in between post-intervention testing and follow-up. No honorarium was given for the follow-up visit. 112 participants were randomised to an exercise intervention group and 74 participants completed the intervention and testing out of which 46 participants (62%) completed follow-up (BIKE: n = 14; MOD: n = 14; VIG: n = 18).
2.2.1. Analytical rationale
Our starting point in designing the follow-up study was that participants would not necessarily follow the prescribed exercise after the intervention because of the controlled nature of the primary intervention (e.g. randomisation, personalised monitoring and support), and because maintenance of physical activity is a complex behavioural process, characterised by cycles of lapse, relapse, and recovery [23]. We used VO2peak as an indicator of physical activity participation [24]. and assessed within-group changes in VO2peak from baseline to follow-up and between-group differences in VO2peak at follow-up to obtain a general indication of the participants’ maintenance of physical activity. However, because assessment of group means provides little insight into the exercise practices of individual participants, inter-individual variability, or the volatility of physical activity maintenance [23], we generated a purposive sample for mixed-method analysis to better understand differences between participants with the greatest improvements and reductions in VO2peak, respectively.
2.2.2. Biomedical testing at follow-up
Follow-up tests were performed in the morning after an overnight fast (≥10 h). Participants were instructed to refrain from exercise the day before testing.
2.2.2.1. Cardiorespiratory fitness
VO2peak was assessed by indirect respiratory calorimetry (Oxycon Pro, Jaeger, Würzburg, Germany) during an incremental test on an electronically braked bicycle ergometer (Lode Excalibur, Groeningen, Netherlands) [15].
2.2.2.2. Anthropometry
Body weight and height were measured and body composition was determined using dual-energy X-ray absorptiometry (DPX-IQ X-ray bone densitometer 4.7e, Lunar Corporation, Madison, WI, USA). Waist circumference was measured at the narrowest part between the lowest rib and the iliac crest.
2.2.3. Recent physical activity
The Recent Physical Activity Questionnaire (RPAQ) was used to assess physical activity behaviour the last four weeks [25]. Questionnaire data were coded and analysed according to the guidelines provided by the Medical Research Council, Epidemiology Unit, University of Cambridge (http://www.mrc-epid.cam.ac.uk/physical-activity-downloads/).
2.2.4. Follow-up interviews
To explore participants' experiences with exercising after the intervention we conducted an interview study to identify what had facilitated or hindered participants’ maintenance of a physically active lifestyle post-intervention. Researchers, who received guidance in interview techniques, conducted semi-structured interviews (15–30 min) with all participants after the biomedical testing.
2.2.5. A purposive sample for mixed-method analysis of exercise maintenance
To gain insight into individual participants' exercise practices after the intervention, we generated a purposive sub-sample for detailed qualitative analysis. We aimed to identify whether significant barriers, facilitators, and practice patterns were apparent between the participants who improved or maintained/reduced their fitness level from baseline to follow-up. To do this, we dissolved the group structure and ranked all participants based on relative changes in VO2peak, before selecting 12 participants from each end of the range, i.e., the 12 participants with the greatest improvements in VO2peak (‘VO2peak improvers’) and the 12 participants who experienced the greatest reduction (‘VO2peak reducers’) from baseline to follow-up.
2.2.6. Statistical analysis
Descriptive data are presented as mean (SD) for parametric data and median (Q1; Q3) for non-parametric data. We evaluated changes over time within groups and differences between changes in BIKE compared with MOD and VIG combined using a linear mixed model (unstructured covariance, repeated effect for time on participant level) with mean value as a function of time and group × time interaction adjusted for sex. For RPAQ data, time spent at different intensities of physical activity, within-group changes were analysed using Wilcoxon Signed Rank test and differences between BIKE vs. MOD + VIG and between ‘VO2peak improvers’ and ‘VO2peak reducers’ were analysed using Wilcoxon-Kruskal-Wallis test. Exercise compliance during the intervention was compared between groups using 1-way ANOVA and between ‘VO2peak improvers’ and ‘VO2peak reducers’ using t-tests. Differences and changes are presented as mean (95% CI). Changes in cardiorespiratory fitness, anthropometry, and physical activity from baseline to follow-up were compared between BIKE and MOD + VIG to explore maintenance of physical activity and health effects and is thus the primary outcomes. Other changes were considered descriptive. No statistical analyses were performed on RPAQ data on the different types of transportation owing to a small number of users/participants in each group. Statistical significance was defined as p < 0.05 (two-tailed). Statistical analyses were performed in SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA).
2.2.7. Qualitative analysis
All interviews from the purposive subsample were transcribed verbatim. Interview transcripts were then analysed using Nvivo 11 (QSR International Pty Ltd.) following the methodological principles of ‘systematic text condensation’ [26], a methodological strategy suited for thematic analysis of qualitative data such as interview transcripts. ‘Systematic text condensation’ entails a four-step procedure: 1. Establishing an overview of the qualitative data to identify preliminary themes; 2. Identifying and organising data elements to form code groups; 3. Constructing meaning units within each code group; and 4. Synthesising all analytical units to construct thematic descriptions that elucidate the study question. We interpreted the findings from the thematic text condensation procedure through a social practice-theory framework [26,27] to explore differences between the two groups that were selected based on changes in VO2peak. A social practice-theory framework is well-suited for understanding how people initiate and maintain their engagement in particular practices, such as physical exercise, over time.
3. Results
3.1. Participants
Baseline characteristics and exercise compliance are presented in Table 1.
Table 1.
Baseline characteristics and exercise compliance of all exercise group completers and participants included in the follow-up study (shown by group allocation and subgroups).
| Completers |
BIKE |
MOD |
VIG |
VO2peak Improvers |
VO2peak Reducers |
|
|---|---|---|---|---|---|---|
| (n=74) | (n=14) | (n=14) | (n=18) | (n=12) | (n=12) | |
| Characteristics | ||||||
| Age, years | 35 (7) | 34 (8) | 32 (7) | 36 (8) | 32 (9) | 38 (7) |
| Sex, women/men | 37/37 | 8/6 | 6/8 | 9/9 | 9/3 | 7/5 |
| Educational level | ||||||
| Less than college, number (%) | 40 (54%) | 11 (79%) | 6 (43%) | 9 (50%) | 7 (58%) | 10 (84%) |
| College, number (%) | 25 (34%) | 3 (11%) | 4 (29%) | 6 (33%) | 5 (42%) | 1 (8%) |
| Graduate school, number (%) | 9 (12%) | 0 (0%) | 4 (29%) | 3 (17%) | 0 (0%) | 1 (8%) |
| Job status | ||||||
| Employed, number (%) | 58 (79%) | 11 (79%) | 6 (43%) | 16 (89%) | 9 (75%) | 10 (83%) |
| Unemployed, number (%) | 7 (9%) | 1 (7%) | 4 (29%) | 1 (6%) | 0 (0%) | 2 (17%) |
| Student, number (%) | 9 (12%) | 2 (14%) | 4 (29%) | 1 (6%) | 3 (25%) | 0 (0%) |
| Civil status and children | ||||||
| Single, number (%) | 17 (23%) | 5 (36%) | 4 (29%) | 2 (11%) | 5 (42%) | 0 (0%) |
| Cohabiting, number (%) | 57 (77%) | 9 (64%) | 10 (71%) | 16 (89%) | 7 (58%) | 12 (100%) |
| Children, (yes) number (%) | 40 (54%) | 8 (57%) | 6 (42%) | 11 (61%) | 6 (50%) | 7 (58%) |
| Anthropometric variables | ||||||
| Body weight, kg | 91 (12) | 88.0 (10.0) | 90.9 (11.6) | 92.0 (12.7) | 88.0 (10.7) | 87.7 (13.3) |
| Body mass index, kg/m2 | 29.8 (2.4) | 29.9 (2.7) | 29.6 (2.0) | 29.7 (2.3) | 29.6 (3.0) | 29.5 (2.2) |
| Fat mass, kg | 34.8 (7.2) | 34.0 (7.7) | 34.5 (7.9) | 34.8 (5.6) | 35.9 (7.3) | 33.8 (7.7) |
| Fat percentage, %a | 39.0 (32.3; 44.5) | 42.3 (29.1; 45.9) | 38.1 (32.6; 43.2) | 37.7 (30.8; 44.5) | 40.9 (6.6) | 38.9 (8.3) |
| Fat free mass, kga | 54.5 (45.0; 65.2) | 53.6 (45.0; 59.7) | 54.7 (49.1; 62.8) | 54.6 (44.4; 69.3) | 52.1 (9.3) | 53.8 (12.5) |
| Waist circumference, cmab | 93.1 (87.8; 100.3) | 96.3 (88.6; 98.2) | 90.3 (88.2; 100.0) | 99.2 (87.2; 102.4) | 90.7 (7.9) | 93.5 (9.3) |
| Android fat, % | 48.8 (6.0) | 48.9 (6.7) | 47.8 (6.9) | 48.7 (5.5) | 50.3 (5.5) | 49.2 (7.0) |
| Exercise test variables | ||||||
| VO2peak, ml O2/min | 2689 (552) | 2653 (473) | 2851 (539) | 2752 (622) | 2594 (468) | 2645 (476) |
| Maximal heart rate, bpm | 183 (10) | 187 (11) | 184 (6) | 182 (11) | 185 (11) | 185 (8) |
| Peak power output, W | 194 (43) | 191 (41) | 207 (44) | 195 (44) | 186 (40) | 191 (45) |
| Exercise compliance | ||||||
| Compliance, % prescribed kcala | 90 (81; 102) | 90.0 (85.8; 100.8) | 85.0 (81; 120) | 85.0 (81.0; 99) | 96 (94; 109)* | 87 (77; 98) |
| Exercise intensity, %VO2peak-reserve | 55.9 (9.6) | 53.2 (7.8) | 48.7 (4.6) | 64.8 (6.9) | 57.7 (9.4) | 58.8 (9.8) |
| Exercise sessions per week | 3.9 (0.5) | 3.9 (0.3) | 3.8 (0.5) | 4.0 (0.6) | 4.0 (3.8; 4.2) | 3.9 (3.6; 4.2) |
| Exercise duration, min per session | 46 (12) | 46 (10) | 54 (10) | 37 (8) | 45 (11) | 42 (9) |
| Daily bike distance, km | n.a. | 14.0 (3.1) | n.a. | n.a. | n.a. | n.a. |
| Intervention duration, days | 192 (13) | 189 (10) | 192 (12) | 195 (12) | 188 (15) | 197 (10) |
| Intervention group | ||||||
| BIKE, number (%) | 6 (50%) | 2 (17%) | ||||
| MOD, number (%) | 2 (17%) | 3 (25%) | ||||
| VIG, number (%) | 4 (33%) | 7 (58%) | ||||
Data are shown as mean (SD) or number (%) except (a) which are shown as median (Q1; Q3). ‘Exercise groups’ include BIKE, MOD, and VIG. BIKE, active commuting group; MOD, moderate intensity exercise group; VIG, vigorous intensity exercise group; VO2, oxygen uptake; VO2peak improvers, participants who experienced the greatest improvements in VO2peak from baseline to follow-up; VO2peak reducers, participants who experienced the greatest reductions in VO2peak from baseline to follow-up. Exercise compliance during the intervention was compared between groups using 1-way ANOVA and between ‘VO2peak improvers’ and ‘VO2peak reducers’ using t-tests. *significantly different from ‘VO2peak reducers’. b: BIKE: n = 13.
3.2. Timing of follow-up testing
Follow-up tests took place 15 (13; 20) months (median (Q1; Q3)) after completion of the trial (BIKE: 14 (12; 20) months; MOD: 14 (13; 18) months; VIG: 15 (13; 20) months).
3.3. Changes in cardiorespiratory fitness and body composition from baseline to follow-up
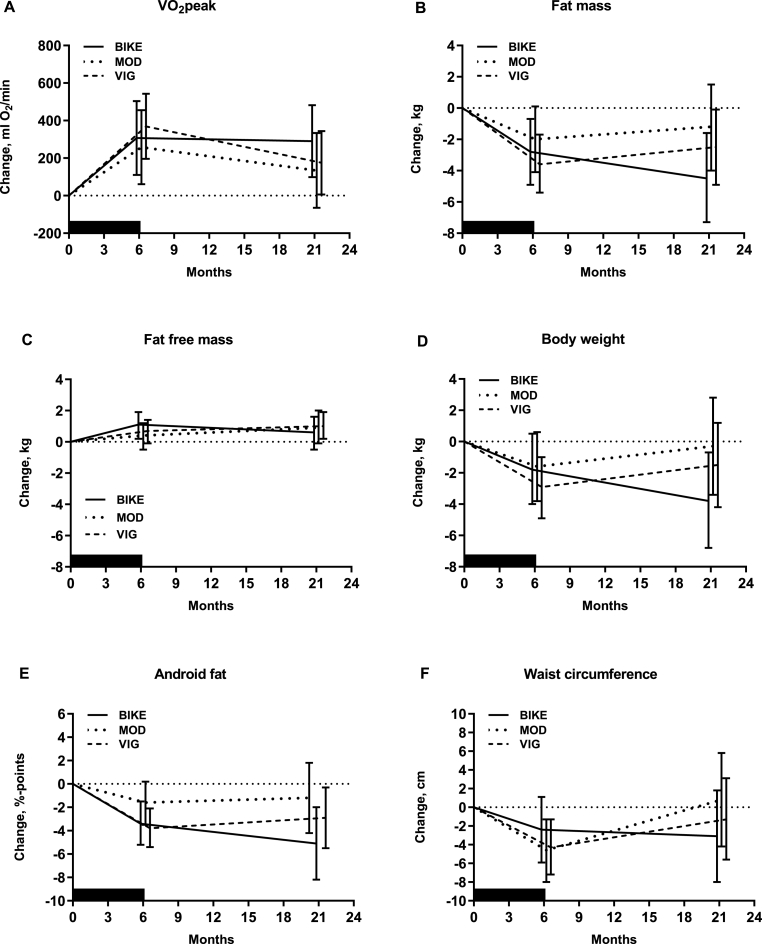
VO2peak increased and fat mass decreased in BIKE and VIG, and fat free mass increased slightly in VIG (Fig. 1A–C, Table 2). A large weight loss was observed in BIKE, and android fat decreased in BIKE and VIG (Fig. 1D–E, Table 2). Waist circumference was not lower at follow-up in any of the groups (Fig. 1F, Table 2). Changes did not differ between BIKE and MOD + VIG for any of the outcomes (Table 2).
Fig. 1.
Changes in cardiorespiratory fitness (VO2peak) (A), fat mass (B), fat free mass (C), body weight (D), android fat percentage (E), and waist circumference (F) during the 6-months intervention (black box) and follow-up period (after 6 months) in BIKE, MOD and VIG. Data are presented as estimated mean change (95% confidence interval) analysed by a mixed model adjusted for sex. Estimates and p-values are presented in Table 2. BIKE: active commuting group; MOD: moderate intensity exercise group; VIG: vigorous intensity exercise group; VO2peak, peak oxygen uptake.
Table 2.
Changes in cardiorespiratory fitness and anthropometry from baseline to post-intervention and follow-up testing among participants in the follow-up study (shown by group allocation).
| BIKE |
MOD |
VIG |
BIKE vs. MOD + VIG |
|||||
|---|---|---|---|---|---|---|---|---|
| Within-group change | P | Within-group change | p | Within-group change | p | Difference | p | |
| VO2peak, ml O2/min | ||||||||
| Baseline to post-intervention | 307 (110; 504) | 0.003 | 258 (61; 455) | 0.012 | 369 (196; 543) | <0.001 | −6 (−243; 230) | 0.957 |
| Baseline to follow-up | 290 (99; 482) | 0.004 | 135 (−65; 334) | 0.180 | 175 (6; 344) | 0.043 | 136 (−97; 368) | 0.245 |
| Fat mass, kg | ||||||||
| Baseline to post-intervention | −2.8 (−4.9; −0.7) | 0.009 | −2.0 (−4.1; 0.1) | 0.064 | −3.6 (−5.4; −1.7) | <0.001 | 0.0 (−2.6; 2.5) | 0.971 |
| Baseline to follow-up | −4.5 (−7.3; −1.6) | 0.003 | −1.2 (−4.0; 1.5) | 0.365 | −2.5 (−4.9; −0.1) | 0.041 | −2.6 (−6.0; 0.8) | 0.132 |
| Fat free mass, kg | ||||||||
| Baseline to post-intervention | 1.1 (0.2; 1.9) | 0.017 | 0.4 (−0.5; 1.2) | 0.386 | 0.7 (−0.1; 1.4) | 0.091 | 0.5 (−0.5; 1.6) | 0.293 |
| Baseline to follow-up | 0.6 (−0.5; 1.6) | 0.262 | 0.9 (−0.1; 2.0) | 0.071 | 1.0 (0.2; 1.9) | 0.023 | −3.4 (−1.7; 0.9) | 0.524 |
| Body weight, kg | ||||||||
| Baseline to post-intervention | −1.8 (−4.0; 0.5) | 0.120 | −1.6 (−3.8; 0.6) | 0.158 | −2.9 (−4.9; −1.0) | 0.004 | 0.5 (−2.1; 3.2) | 0.707 |
| Baseline to follow-up | −3.8 (−6.8; −0.7) | 0.017 | −0.3 (−3.4; 2.8) | 0.841 | −1.5 (−4.2; 1.2) | 0.278 | −2.9 (−6.6; 0.8) | 0.123 |
| Android fat, %-points | ||||||||
| Baseline to post-intervention | −3.4 (−5.2; −1.5) | <0.001 | −1.6 (−3.5; 0.2) | 0.084 | −3.8 (−5.4; −2.1) | <0.001 | −0.6 (−2.9; 1.6) | 0.567 |
| Baseline to follow-up | −5.1 (−8.2; −2,0) | 0.002 | −1.2 (−4.2; 1.8) | 0.413 | −2.9 (−5.5; −2.3) | 0.033 | −3.0 (−6.7; 0.7) | 0.104 |
| Waist circumference, cm | ||||||||
| Baseline to post-intervention | −2.4 (−5.9; 1.1) | 0.169 | −4.6 (−8.0; −1,3) | 0.008 | −4.3 (−7.2; −1,3) | 0.005 | 2.1 (−2.1; 6.2) | 0.318 |
| Baseline to follow-up | −3.1 (−8.0; 1.8) | 0.213 | 0.8 (−4.2; 5.8) | 0.749 | −1.3 (−5.6; 3.1) | 0.563 | −2.9 (−8.8; 3.1) | 0.338 |
Data are estimated mean changes (95% CI). Changes post-intervention and at follow-up were assessed using a mixed model adjusted for sex. BIKE, active commuting group; MOD, moderate intensity exercise group; VIG, vigorous intensity exercise group; VO2peak; peak oxygen uptake.
3.4. Recent physical activity
Use of car/motorized vehicles was less prevalent in BIKE than in MOD and VIG at follow-up (Table 3). Approximately half of the participants in BIKE and VIG and one third in MOD were bike users at follow-up. Although no clear pattern was observed, use of public transportation was lower at follow-up in all groups compared with baseline. Walking was rare in all three groups. Time spent on recreational physical activity increased in BIKE and a minor increase in vigorous intensity physical activity was observed in VIG from baseline to follow-up. However, there were no differences in changes in physical activity between BIKE and MOD + VIG.
Table 3.
Transportation and physical activity assessed by the Recent Physical Activity Questionnaire among participants in the follow-up study (shown by group allocation and subgroups).
| BIKE |
MOD |
VIG |
VO2peak improvers |
VO2peak reducers |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n=14) | (n=14) | (n=18) | (n=12) | (n=12) | ||||||||
| Transport domain | ||||||||||||
| Car or other motorized vehicles | ||||||||||||
| Duration, min/day (all) | ||||||||||||
| Baseline | 0 (0; 1) | 1 (0; 9) | 0 (0; 15) | 0 (0; 5) | 0 (0; 20) | |||||||
| Post-intervention | 0 (0; 3) | 0 (0; 9) | 3 (0; 18) | 0 (0; 2) | 9 (0; 35) | |||||||
| Follow-up | 0 (0; 0) | 1 (0; 34) | 1 (0; 10) | 0 (0; 0) | 4 (0; 52) | |||||||
| Users, n (%) | ||||||||||||
| Baseline | 5 (36%) | 8 (57%) | 10 (56%) | 6 (50%) | 6 (50%) | |||||||
| Post-intervention | 5 (36%) | 5 (36%) | 13 (72%) | 5 (42%) | 7 (58%) | |||||||
| Follow-up | 3 (21%) | 8 (57%) | 10 (56%) | 3 (25%) | 8 (67%) | |||||||
| Duration among users, min/day | ||||||||||||
| Baseline | 6 (1; 30) | 7 (3; 24) | 13 (1; 18) | 5 (1; 9) | 17 (15; 43) | |||||||
| Post-intervention | 35 (3; 39) | 14 (10; 42) | 7 (3; 21) | 3 (1; 3) | 33 (12; 42) | |||||||
| Follow-up | 10 (3; 106) | 21 (2; 83) | 8 (3; 30) | 2 (0; 3) | 31 (4; 89) | |||||||
| Public transport | ||||||||||||
| Duration, min/day (all) | ||||||||||||
| Baseline | 0 (0; 8) | 1 (0; 4) | 0 (0; 15) | 0 (0; 9) | 4 (0; 17) | |||||||
| Post-intervention | 0 (0; 3) | 0 (0; 3) | 0 (0; 8) | 0 (0; 2) | 0 (0; 19) | |||||||
| Follow-up | 0 (0; 3) | 0 (0; 0) | 0 (0; 0) | 0 (0; 5) | 0 (0; 16) | |||||||
| Users, n (%) | ||||||||||||
| Baseline | 7 (50%) | 7 (50%) | 8 (44%) | 6 (50%) | 6 (50%) | |||||||
| Post-intervention | 6 (43%) | 5 (36%) | 6 (33%) | 5 (42%) | 5 (42%) | |||||||
| Follow-up | 6 (43%) | 4 (29%) | 4 (22%) | 5 (42%) | 5 (42%) | |||||||
| Duration among users, min/day | ||||||||||||
| Baseline | 8 (4; 39) | 4 (2; 9) | 15 (6; 27) | 9 (4; 10) | 17 (15; 39) | |||||||
| Post-intervention | 8 (2; 26) | 3 (3; 8) | 17 (8; 21) | 2 (1; 3) | 21 (18; 35) | |||||||
| Follow-up | 5 (2; 10) | 7 (3; 10) | 18 (16; 31) | 6 (3; 8) | 16 (16; 39) | |||||||
| Bike | ||||||||||||
| Duration, min/day (all) | ||||||||||||
| Baseline | 0 (0; 5) | 0 (0; 3) | 1 (0; 7) | 4 (0; 7) | 0 (0; 0) | |||||||
| Post-intervention | 8 (0; 30) | 0 (0; 3) | 5 (0; 12) | 5 (0; 19) | 1 (0; 11) | |||||||
| Follow-up | 5 (0; 20; | 0 (0; 2) | 2 (0; 11) | 8 (2; 27) | 0 (0; 1) | |||||||
| Users, n (%) | ||||||||||||
| Baseline | 6 (43%) | 6 (43%) | 9 (50%) | 7 (58%) | 2 (17%) | |||||||
| Post-intervention | 10 (71%) | 6 (43%) | 12 (67%) | 8 (67%) | 6 (50%) | |||||||
| Follow-up | 8 (57%) | 5 (36%) | 10 (56%) | 9 (75%) | 4 (33%) | |||||||
| Duration among users, min/day | ||||||||||||
| Baseline | 5 (4; 37) | 4 (3; 16) | 7 (5; 16) | 5 (5; 37) | 4 (1; 7) | |||||||
| Post-intervention | 18 (4; 35) | 8 (2; 17) | 11 (5; 13) | 13 (5; 27) | 11 (2; 13) | |||||||
| Follow-up | 16 (6; 34) | 12 (2; 29) | 11 (4; 19) | 19 (4; 29) | 2 (1; 7) | |||||||
| Walking | ||||||||||||
| Duration, min/day (all) | ||||||||||||
| Baseline | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 12) | |||||||
| Post-intervention | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | |||||||
| Follow-up | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | 0 (0; 0) | |||||||
| Users, n (%) | ||||||||||||
| Baseline | 3 (21%) | 3 (21%) | 4 (22%) | 2 (17%) | 5 (42%) | |||||||
| Post-intervention | 2 (14%) | 3 (21%) | 2 (11%) | 2 (17%) | 2 (17%) | |||||||
| Follow-up | 2 (14%) | 2 (14%) | 1 (6%) | 1 (8%) | 2 (17%) | |||||||
| Duration among users, min/day | ||||||||||||
| Baseline | 6 (4; 12) | 16 (1; 21) | 19 (12; 32) | 11 (6; 16) | 14 (10; 24) | |||||||
| Post-intervention | 9 (4; 14) | 4 (2; 16) | 42 (31; 53) | 29 (5; 53) | 17 (2; 32) | |||||||
| Follow-up | 48 (11; 85) | 16 (3; 29) | 32* | 11* | 17 (3; 32) | |||||||
| Physical activity | ||||||||||||
| Intensity of physical activity across all activities, min/daya | P | P | P | Pa | P | P | Pb | |||||
| Sedentary | ||||||||||||
| Baseline | 1,353 (1,194; 1,391) | 1,341 (1,214; 1,409) | 1,338 (1,197; 1,409) | 1,208 (1,188; 1,389) | 1,341 (1,207; 1,394) | |||||||
| Post-intervention | 1,330 (1,186; 1,387) | 0.497 | 1,355 (1,170; 1,391) | 0.268 | 1,272 (1,163; 1,382) | 0.142 | 0.822 | 1,194 (1,140; 1,379) | 0.365 | 1,275 (1,171; 1,385) | 0.301 | 0.622 |
| Follow-up | 1,326 (1,103; 1,379) | 0.129 | 1,211 (1,188; 1,383) | 0.191 | 1,257 (1,165; 1,385) | 0.353 | 0.373 | 1,211 (1,100; 1,350) | 0.770 | 1,205 (1,176; 1,354) | 0.129 | 0.692 |
| Light | ||||||||||||
| Baseline | 0 (0; 36) | 0 (0; 9) | 0 (0; 44) | 11 (0; 40) | 0 (0; 13) | |||||||
| Post-intervention | 3 (0; 206) | 0.297 | 0 (0; 0) | 0.906 | 0 (0; 43) | 0.852 | 0.395 | 11 (0; 205) | 0.469 | 0 (0; 0) | 0.313 | 0.436 |
| Follow-up | 5 (0; 206) | 0.473 | 0 (0; 206) | 0.672 | 4 (0; 206) | 0.820 | 0.862 | 23 (0; 207) | 0.313 | 1 (0; 206) | 1.00 | 0.573 |
| Moderate | ||||||||||||
| Baseline | 47 (19; 78) | 59 (9; 115) | 44 (21; 89) | 56 (20; 150) | 60 (27; 156) | |||||||
| Post-intervention | 50 (35; 60) | 0.463 | 57 (31; 101) | 0.217 | 61 (48; 216) | 0.284 | 0.905 | 57 (46; 76) | 0.910 | 97 (47; 223) | 0.151 | 0.387 |
| Follow-up | 70 (40; 113) | 0.194 | 42 (38; 179) | 0.502 | 56 (22; 92) | 0.890 | 0.364 | 54 (31; 95) | 0.898 | 67 (31; 204) | 0.850 | 0.686 |
| Vigorous | ||||||||||||
| Baseline | 1 (1; 3) | 4 (1; 9) | 1 (0; 1) | 1 (1; 3) | 1 (0; 6) | |||||||
| Post-intervention | 1 (0; 1) | 0.547 | 2 (1; 5) | 0.380 | 2 (1; 19) | <0.001 | 0.056 | 10 (1; 27) | 0.250 | 1 (0; 3) | 0.844 | 0.172 |
| Follow-up | 15 (2; 21) | 0.106 | 9 (2; 16) | 0.052 | 4 (1; 11) | 0.023 | 0.717 | 16 (4; 22) | 0.160 | 6 (1; 17) | 0.014 | 0.792 |
| Recreational physical activity, min/dayb | ||||||||||||
| Baseline | 31 (23; 59) | 29 (14; 57) | 32 (14; 48) | 30 (5; 55) | 28 (12; 52) | |||||||
| Post-intervention | 38 (20; 74) | 0.397 | 54 (31; 68) | 0.256 | 51 (41; 76) | 0.036 | 0.563 | 58 (35; 98) | 0.019 | 50 (15; 59) | 0.736 | 0.144 |
| Follow-up | 59 (43; 108) | 0.006 | 41 (24; 55) | 0.341 | 46 (19; 70) | 0.177 | 0.146 | 71 (41; 94) | 0.001 | 39 (19; 69) | 0.410 | 0.069 |
Data are shown as median (Q1; Q3) or number (%). BIKE, active commuting group; CON, control group; MOD, moderate intensity exercise group; VIG, vigorous intensity exercise group; VO2peak, peak oxygen uptake. Time spend was calculated from frequency and usual time spend on a given activity. The section on transportation, includes four possible answers regarding the frequency: ‘never/rarely’, ‘occasionally’, ‘usually’, always'. Users were defined as participants reporting ‘occasionally’, ‘usually’, ‘always’. Owing to the small number of users/participants in each category from each group, no statistical analyses were performed on data on the different types of transportation.
Within-group changes from baseline to post-intervention and follow-up were analysed using Wilcoxon Signed Rank test, and differences between changes in BIKE vs. MOD + VIG were analysed using Wilcoxon-Kruskal-Wallis test. P-values are results from the analyses from baseline to post-intervention and baseline to follow-up and (a) comparisons between changes in BIKE vs. MOD + VIG and (b) comparisons between changes in ‘VO2peak improvers’ and ‘VO2peak reducers’.
Sum of all types of recreational exercise and physical activities. One participant in VIG and ‘VO2peak reducers’ performed 493 min/day of recreational physical activity at baseline and was omitted from analyses on recreational physical activity owing to assumptions of the statistical analysis. Changes from baseline to post-intervention and follow-up and differences between changes in BIKE vs. MOD + VIG were analysed using a mixed model adjusted for sex. *n = 1.
3.5. ‘VO2peak improvers’ and ‘VO2peak reducers’
Individual and mean changes in VO2peak are presented in Fig. 2A–B. ‘VO2peak improvers’ were slightly younger than ‘VO2peak reducers’ (Table 1). During the intervention, compliance to the prescribed exercise energy expenditure was 16% higher among ‘VO2peak improvers’ compared with ‘VO2peak reducers’, but there were no differences in exercise intensity, exercise frequency, or intervention duration between the two groups. Half of the ‘VO2peak improvers’ originated from BIKE whereas participants from VIG constituted the greatest part of ‘VO2peak reducers’ (58%). The median duration from completion of the trial to follow-up was 18.5 (14.0; 20.0) months in ‘VO2peak improvers’ and 16.5 (14.5; 20.0) months in ‘VO2peak reducers’. At follow-up, fat mass was decreased in ‘VO2peak improvers’ but not in ‘VO2peak reducers’ compared with baseline; however, changes did not differ between the two groups (Fig. 2C). In ‘VO2peak improvers’, recreational physical activity increased from baseline to follow-up but did not change in ‘VO2peak reducers’ or differ between groups at follow-up (Table 3). From baseline to follow-up, a minor increase in time spent at vigorous intensity was observed in ‘VO2peak reducers’. At follow-up, more ‘VO2peak reducers’ than ‘VO2peak improvers’ were car users and time spent car driving was greater among car users in ‘VO2peak reducers’, whereas biking was more prevalent in ‘VO2peak improvers’, which was, however, also the case at baseline.
Fig. 2.
A. Individual changes in cardiorespiratory fitness (VO2peak) from baseline to follow-up. Data are presented as percentage change from baseline. Interviews were missing from 4 out of 46 participants (VIG: n = 1; BIKE: n = 3) and data from these participants are not shown. The boxes include the 12 participants who experienced the greatest reductions (‘VO2peak reducers’) and improvements (‘VO2peak improvers’) in VO2peak, respectively. These participants were included in the mixed-methods analysis. Change in VO2peak from baseline to follow-up: ‘VO2peak improvers’: 19.4 (16.1; 29.2)% (range: 13.7–33.8%); ‘VO2peak reducers’: −3.6 (−8.7; −1.4)% (range: −34.0; −1.0%). B-D. Changes in VO2peak (B), fat mass (C), and body weight (D) during the intervention (black box) and follow-up period in ‘VO2peak improvers’ and ‘VO2peak reducers’. Data are presented as estimated mean change (95% confidence interval) analysed by a mixed model adjusted for sex. Changes from baseline to post-intervention in ‘VO2peak improvers’ vs. ‘VO2peak reducers’: VO2peak: 94 (−153; 342) ml O2/min, p = 0.438; Fat mass: 1.9 (−1.2; 5.0) kg, p = 0.217; Body weight: 2.0 (−1.3; 5.2) kg, p = 0.224. Changes from baseline to follow-up in ‘VO2peak improvers’ vs. ‘VO2peak reducers’: VO2peak: 751 (551; 950) ml O2/min, p˂0.001; Fat mass: −2.6 (−7.7; 2.4) kg, p = 0.287; Body weight: −2.2 (−6.9; 2.5) kg, p = 0.337. VO2peak: peak oxygen uptake.
3.6. Interview study
Analysis of the interviews transcripts using systematic text condensation showed that none of the participants continued the exercise practice (in terms of exercise modality, frequency, and intensity) from the intervention, even if they had found the prescribed exercise regimen engaging and easy to implement in their everyday lives. However, the analysis of interview transcripts showed that ‘VO2peak improvers’ exercised more regularly and more varied after the intervention than ‘VO2peak reducers’. The ‘VO2peak improvers’ were divided into two categories based on their descriptions of their post-intervention exercise practices: 1) Engagement in a new form of regular and structured exercise (n = 7) and 2) Engagement in unstructured but frequent exercising using different forms of exercise (n = 5). ‘VO2peak reducers’ were also divided into two general categories: 1) Occasional exercise (n = 9); 2) No exercise (n = 3).
Analysis of the interview transcripts showed that the ‘VO2peak reducers’ met more barriers and experienced more challenges with exercising after the intervention compared with the ‘VO2peak improvers’. The analysis of the accounts of the ‘VO2peak reducers’ showed that their maintenance of exercise post-intervention was complicated by challenges, such as: 1) lack of exercise motivation; 2) absence of exercise partners or a supporting social structure; 3) challenges with finding time to exercise and coordinating exercise, work, and family life; and 4) significant life events complicating maintaining a steady practice of exercising, e.g., injuries, illness, family conditions, and occupational changes. Analysis of the ‘VO2peak improvers’ showed that they were faced with similar barriers, but that they had success in developing a robust and flexible exercise practice that could be adapted to the shifting circumstance of their everyday lives after the intervention. The exercise maintenance of the ‘VO2peak improvers’ was also supported by their active use of various exercise facilitators. In particular, the analysis showed that self-monitoring, collective exercising, and engagement in new exercise projects constituted key elements in the exercise practices of the ‘VO2peak improvers’ post-intervention. Unlike the ‘VO2peak reducers’, the ‘VO2peak improvers’ used self-monitoring technologies (e.g., mobile apps, pedometers, exercise diary) as central and integrated motivational elements of their post-intervention exercise practice. Compared to the ‘VO2peak reducers’, the ‘VO2peak improvers’ also had greater success in replacing the trial's support system with other committed exercise partners, e.g., colleagues, partners, friends, fitness teams, or online exercise communities. Furthermore, several of the participants in the ‘VO2peak improvers’ had embarked on new personal “exercise challenges”, e.g., marathons, bike races, fitness events, or weight loss projects.
4. Discussion
Completion of a structured exercise intervention consisting of 6 months of active commuting (BIKE) or vigorous intensity leisure-time exercise (VIG) was associated with long-term maintenance of improvements in VO2peak and body composition, whereas moderate intensity leisure-time exercise (MOD) was not. Contrary to our hypothesis, routinisation of active commuting during the intervention did not lead to a greater degree of maintenance of cardiorespiratory fitness and anthropometry at follow-up than leisure-time exercise.
We observed that improvements in VO2peak and reductions in fat mass were maintained approximately 15 months after completion of the interventions in BIKE and VIG, suggesting maintenance of a physically active lifestyle after these interventions. Furthermore, body weight was decreased in BIKE and fat free mass was increased in VIG compared with baseline levels. In the GO-ACTIWE trial, changes in cardiorespiratory fitness (VO2peak) and fat mass were primary outcomes and we defined a 10% increase in cardiorespiratory fitness and a 5% reduction in fat mass as clinically relevant changes [17]. During the trial, we observed clinically relevant improvements in VO2peak and reductions in fat mass in all three exercise groups with greater effects in response to vigorous compared to moderate intensity leisure-time exercise [15,27]. At follow-up, VO2peak was increased by 11% in BIKE and 6% in VIG compared with baseline, respectively, meaning that only the change in BIKE is considered clinically relevant. The fat loss observed in BIKE and VIG corresponded to a clinically relevant reduction of 13% and 7%, respectively. Hence, clinically relevant effects of active commuting and vigorous intensity leisure-time exercise can be maintained for more than one year after completion of an intervention. Our findings on maintenance of improved VO2peak and reductions in fat mass in VIG are in line with our previous follow-up study among men with overweight who maintained higher VO2peak and reduced fat mass one year after completion of a 3-month exercise-induced weight loss intervention [28]. In previous exercise intervention studies, physical activity behaviour could be maintained for 6–15 months after start of the intervention [16], and in the present study this period is extended to 21 months.
In contrast to our hypothesis, we did not observe that 6 months of active commuting led to long-term maintenance of physical activity and health effects to a greater degree than leisure-time exercise. It has been suggested that active commuting represents a promising alternative to leisure-time exercise to increase physical activity in physically inactive individuals [4]. Since physical activity is limited in work and transport domains for many people in modern society and since it may be challenging to obtain sufficient physical activity during leisure-time [3], we expected that implementation and routinisation of active commuting during the trial would lead to longer-term maintenance of physical activity compared to leisure-time exercise. Furthermore, our hypothesis was based on large observational studies showing associations between active commuting and lower mortality [5] and degree of adiposity [[6], [7], [8]], higher fitness [8], and better cardiovascular profile [8,9] even when controlling for leisure-time physical activity. However, this study was the first randomised controlled trial to investigate health effects of active commuting and leisure-time exercise during and after a structured intervention. There may be several explanations for the lack of difference between the active commuting group (BIKE) and the leisure-time exercise groups (MOD and VIG) at follow-up. At the time of completion of the trial, research staff had no longer contact to participants before participants were invited to participate in the follow-up visit 12 months post-intervention. During the intervention, participants' compliance was monitored by the research staff and they were contacted in case of low compliance. This led to excellent compliance to the prescribed exercise and clinically relevant changes in cardiorespiratory fitness and fat mass in all three exercise groups during the intervention [15,27]. After the intervention, maintenance of exercise was completely dependent on the individuals’ motivation etc., and great variability would be expected within each group. A great variability in physical activity and thus health outcomes combined with the small sample size leads to low statistical power which may partly explain the lack of difference between groups.
The qualitative data show that the participants generally did not follow the originally prescribed exercise after the intervention. The nature of the main trial might be part of the explanation. During the main trial, participants were followed closely by trial staff, who would continually motivate participants to adhere to the prescribed regimen and help them overcome barriers and difficulties. This supportive social structure was abruptly discontinued upon completion of the intervention. Although some measures were put in place to support maintenance post-intervention, i.e., free gym membership and an opportunity to keep the bike and the heart rate monitor, data from the interview study suggest that dedicated social and supportive arrangements are crucial for maintaining a physically active lifestyle. Compared to the ‘VO2peak reducers’, the ‘VO2peak improvers’ had greater success in replacing the trial's support system with other committed exercise partners. The qualitative analysis also showed that the ‘VO2peak improvers’, unlike the ‘VO2peak reducers’, were actively using exercise technologies, new exercise challenges, as well as other people as motivating components of their exercise practices. This suggests that helping participants establish new supportive social arrangements after a structured exercise intervention could be an effective way of supporting maintenance of exercise post-intervention. The interview study also suggests that maintaining exercise after a structured intervention may involve some adaptation and development of the exercise practice itself, and that it is unlikely that people will stick to and comply with the specific exercise regimen prescribed during a health intervention for a more extended period. Continuous adaptation of health practices and the changing circumstances of everyday life should be considered an essential part of what it means and entails to maintain an active and healthy way of life, as suggested by a recent qualitative study [29].
Based on the interview study, we found that the ‘VO2peak reducers’ experienced greater difficulties establishing and maintaining a steady exercise practice in their everyday lives than the ‘VO2peak improvers’. Our analysis highlights how participants' ability to exercise regularly was structured by and dependent on social and contextual conditions, specific to the individual participant's everyday life, e.g., family life and constellation, work life structure, as well as significant life events. As suggested by recent social practice theory-based work, active living is about more than individual choices and motivation, but dependent on pragmatic negotiations about the distribution of roles and tasks within the household, as well as continuous management and alignment of different and sometimes conflicting practices and agendas in everyday life [[30], [31], [32], [33], [34]].
There are several limitations associated with the present study. First, the findings may be associated with selection bias. Out of 112 randomised to the exercise groups, 74 participants (66%) completed the interventions and 46 (41%) participated in the follow-up testing. Hence, results are based on individuals who were likely motivated for lifestyle changes, which limits generalisability of the findings. Furthermore, the low follow-up rate and thus small sample size may have led to low statistical power and thus ability to detect potential differences between groups. Moreover, we did not control for potential confounders in the analyses. Also, there was some variability in timing of follow-up tests that may have contributed to variability of outcomes. In the sub study of ‘VO2peak improvers’ and ‘VO2peak reducers’, participants were categorized based on individual changes in VO2peak, which may have resulted in misclassification of some participants due to measurement error and day-to-day variability [35]. Finally, we did not include objective measures of physical activity. It has been shown that RPAQ is a valid instrument for ranking people according to total and physical activity energy expenditure as well as time spent sedentary and at vigorous intensity physical activity [25,36]. However, RPAQ seems to be less valid for assessment of time spent at light and moderate intensities [36]. The questionnaire has shown high repeatability across domains of physical activity and home and work-related activities and recreational activities [36]. However, it performs less well in estimating time spent in the transport domain and the reliability increases with shorter duration between assessments [36], which may be a concern in relation to the long duration between post-intervention and follow-up visits in the present study. Although it has been suggested that the questionnaire is appropriate for assessment of physical activity in large observational studies [25], it is uncertain whether the questionnaire is sufficiently sensitive and valid for assessment of changes in physical activity in intervention studies which may have affected the results in the present study. Strengths of the study include gold standard assessment of VO2peak and measurement of body composition as well as the interdisciplinary approach, which combined quantitative and qualitative methods to understand long-term maintenance of physical activity.
In conclusion, this follow-up study suggests that 6 months of active commuting or vigorous intensity leisure-time exercise is associated with long-term maintenance of improvements in VO2peak and body composition, whereas moderate intensity leisure-time exercise is not. However, routinisation of physical activity was not more pronounced in transport than in leisure-time domains of everyday life. Qualitative data showed that self-monitoring, exercising with others, and initiation of new exercise challenges can facilitate maintenance of a physically active lifestyle. The study suggests that whether and how individuals maintain a physically active lifestyle after a structured exercise intervention largely depends on their life situation and everyday life. Therefore, public health policy should aim to provide people with various opportunities to maintain a physically active lifestyle in everyday life. Future studies should include systematic guidance upon completion of exercise interventions to support long-term maintenance of healthy lifestyle changes. Also, future follow-up studies should explore different ways of supporting meaningful transitions from the structured set-up of a trial to the inherently more complex nature of everyday life.
Ethical approval
The study was approved by the Ethical Committee of The Capital Region of Denmark (H-4-2013-108).
Funding
The study was funded by the University of Copenhagen Excellence Programme for Interdisciplinary Research (www.go.ku.dk), TrygFonden, and Gerda and Aage Haensch's Fund. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Jonas Salling Quist was supported by a PhD scholarship from the Faculty of Health and Medical Sciences, University of Copenhagen, Denmark.
Author contributions
JSQ, JW, ASG, MBB, MR, APJ, BS designed the study; BS was principal investigator; JSQ, JW, ALF, ASG, MBB, MR collected data; JSQ and JW analysed data; JSQ, JW, APJ and BS interpreted the results; JSQ and JW drafted the manuscript; all authors read and critically reviewed the manuscript and approved the final version.
Availability of data and materials
Request for data should be addressed to the corresponding author and specify how data will be used.
Declaration of competing interest
The authors report no competing interests.
Acknowledgements
We would like to thank all participants as well as biomedical laboratory assistant Desirée Hornbæk Milling and student assistants. Furthermore, we thank Isabella Sparre, Anne-Louise Bjerregaard and Stine Byberg for assistance regarding data management and analysis of RPAQ data.
References
- 1.World Health Organization Physical acitvity. Fact Sheet. 2020 https://www.who.int/news-room/fact-sheets/detail/physical-activity [Internet] Available from: [Google Scholar]
- 2.World Health Organization Obesity and overweight. Fact sheet. 2020 https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Internet] Available from: [Google Scholar]
- 3.Kraus W.E., Bittner V., Appel L., Blair S.N., Church T., Després J.P., et al. The national physical activity plan: a call to action from the American heart association A science advisory from the American heart association. Circulation. 2015;131:1932–1940. doi: 10.1161/CIR.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 4.Andersen L.B. Active commuting: an easy and effective way to improve health. Lancet Diabetes Endocrinol. 2016;4(5):381–382. doi: 10.1016/S2213-8587(16)00077-2. [DOI] [PubMed] [Google Scholar]
- 5.Andersen L.B., Schnohr P., Schroll M., Hein H.O. All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch. Intern. Med. 2000;160(11):1621. doi: 10.1001/archinte.160.11.1621. [DOI] [PubMed] [Google Scholar]
- 6.Flint E., Cummins S., Sacker A. Associations between active commuting, body fat, and body mass index: population based, cross sectional study in the United Kingdom. BMJ. 2014;349:g4887. doi: 10.1136/bmj.g4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flint E., Cummins S. Active commuting and obesity in mid-life: cross-sectional, observational evidence from UK Biobank. Lancet Diabetes Endocrinol. 2016;4(5):420–435. doi: 10.1016/S2213-8587(16)00053-X. [DOI] [PubMed] [Google Scholar]
- 8.Gordon-larsen P., Boone-heinonen J., Sidney S., Sternfeld B., Jacobs D., Lewis C.E. Active Commuting and Cardiovascular Disease Risk. Arch. Intern. Med. 2013;169(13):1216–1223. doi: 10.1001/archinternmed.2009.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayashi T., Tsumura K., Suematsu C., Okada K., Fujii S., Endo G. Walking to work and the risk for hypertension in men: the Osaka health survey. Ann. Intern. Med. 1999;130:21–26. doi: 10.7326/0003-4819-131-1-199907060-00005. [DOI] [PubMed] [Google Scholar]
- 10.Nordby P., Auerbach P.L., Rosenkilde M., Kristiansen L., Thomasen J.R., Rygaard L., et al. Endurance training per Se increases metabolic health in young, moderately overweight men. Obesity. 2012;20(11):2202–2212. doi: 10.1038/oby.2012.70. [DOI] [PubMed] [Google Scholar]
- 11.Ross R., Hudson R., Stotz P.J., Lam M. Effects of exercise amount and intensity on abdominal obesity and glucose tolerance in obese adults: a randomized trial. Ann. Intern. Med. 2015;162(5):325–334. doi: 10.7326/M14-1189. [DOI] [PubMed] [Google Scholar]
- 12.Reichkendler M.H., Rosenkilde M., Auerbach P.L., Agerschou J., Nielsen M.B., Kjaer A., et al. Only minor additional metabolic health benefits of high as opposed to moderate dose physical exercise in young, moderately overweight men. Obesity. 2014;22(5):1220–1232. doi: 10.1002/oby.20226. [DOI] [PubMed] [Google Scholar]
- 13.Shaw K., Gennat H., O'Rourke P., Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst. Rev. 2006 doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quist J.S., Rosenkilde M., Petersen M.B., Gram A.S., Sjödin A., Stallknecht B. Effects of active commuting and leisure-time exercise on fat loss in women and men with overweight and obesity: a randomized controlled trial. Int. J. Obes. 2018;42(3):469–478. doi: 10.1038/ijo.2017.253. [DOI] [PubMed] [Google Scholar]
- 15.Blond M.B., Rosenkilde M., Gram A.S., Tindborg M., Christensen A.N., Quist J.S., et al. How does 6 months of active bike commuting or leisure-time exercise affect insulin sensitivity, cardiorespiratory fitness and intra-abdominal fat? A randomised controlled trial in individuals with overweight and obesity. Br. J. Sports Med. 2019;53(18):1183–1192. doi: 10.1136/bjsports-2018-100036. [DOI] [PubMed] [Google Scholar]
- 16.Murray J.M., Brennan S.F., French D.P., Patterson C.C., Kee F., Hunter R.F. Effectiveness of physical activity interventions in achieving behaviour change maintenance in young and middle aged adults: a systematic review and meta-analysis. Soc. Sci. Med. 2017;192:125–133. doi: 10.1016/j.socscimed.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 17.Rosenkilde M., Petersen M.B., Gram A.S., Quist J.S., Winther J., Kamronn S.D., et al. The GO-ACTIWE randomized controlled trial - an interdisciplinary study designed to investigate the health effects of active commuting and leisure time physical activity. Contemp. Clin. Trials. 2017;53:122–129. doi: 10.1016/j.cct.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 18.Kern T., Blond M.B., Hansen T.H., Rosenkilde M., Quist J.S., Gram A.S., et al. Structured exercise alters the gut microbiota in humans with overweight and obesity—a randomized controlled trial. Int. J. Obes. 2019;44(1):125–135. doi: 10.1038/s41366-019-0440-y. [DOI] [PubMed] [Google Scholar]
- 19.Gram A.S., Petersen M.B., Quist J.S., Rosenkilde M., Stallknecht B., Bladbjerg E.M. Effects of 6 Months of active commuting and leisure-time exercise on fibrin turnover in sedentary individuals with overweight and obesity: a randomised controlled trial. J. Obes. 2018 doi: 10.1155/2018/7140754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gram A.S., Bladbjerg E.M., Quist J.S., Petersen M.B., Rosenkilde M., Stallknecht B. Anti-inflammatory effects of active commuting and leisure time exercise in overweight and obese women and men: a randomized controlled trial. Atherosclerosis. 2017;265(Oct):318–324. doi: 10.1016/j.atherosclerosis.2017.06.923. [DOI] [PubMed] [Google Scholar]
- 21.Quist J.S., Rosenkilde M., Gram A.S., Blond M.B., Holm-Petersen D., Hjorth M.F., et al. Effects of exercise domain and intensity on sleep in women and men with overweight and obesity. J. Obes. 2019:1–12. doi: 10.1155/2019/2189034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quist J.S., Blond M.B., Gram A.S., Steenholt C.B., Janus C., Holst J.J., et al. Effects of active commuting and leisure-time exercise on appetite in individuals with overweight and obesity. J. Appl. Physiol. 2019;126(4):941–951. doi: 10.1152/japplphysiol.00239.2018. [DOI] [PubMed] [Google Scholar]
- 23.Kahlert D. Maintenance of physical activity: do we know what we are talking about? Prev Med Reports. 2015;2:178–180. doi: 10.1016/j.pmedr.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross R., Blair S.N., Arena R., Church T.S., Després J.P., Franklin B.A., et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American heart association. Circulation. 2016;134:e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 25.Golubic R., May A.M., Benjaminsen Borch K., Overvad K., Charles M.A., Diaz M.J.T., et al. Validity of electronically administered recent physical activity questionnaire (RPAQ) in ten European countries. PLoS One. 2014;Mar 25;9(3) doi: 10.1371/journal.pone.0092829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand. J. Publ. Health. 2012;40(8):795–805. doi: 10.1177/1403494812465030. [DOI] [PubMed] [Google Scholar]
- 27.Quist J.S., Rosenkilde M., Petersen M.B., Gram A.S., Sjödin A., Stallknecht B. Effects of active commuting and leisure-time exercise on fat loss in women and men with overweight and obesity: a randomized controlled trial. Int. J. Obes. 2018;42:469–478. doi: 10.1038/ijo.2017.253. [DOI] [PubMed] [Google Scholar]
- 28.Rosenkilde M., Nordby P., Stallknecht B. Maintenance of improvements in fitness and fatness 1 year after a 3-month lifestyle intervention in overweight men. Eur. J. Clin. Nutr. 2016;70(10):1212–1214. doi: 10.1038/ejcn.2016.64. [DOI] [PubMed] [Google Scholar]
- 29.Cohn S., Lynch R. Falling into a routine: from habits to situated practices. Sociol. Health Illness. 2017;39(8):1398–1411. doi: 10.1111/1467-9566.12597. [DOI] [PubMed] [Google Scholar]
- 30.Cohn S. From health behaviours to health practices: an introduction. Sociol. Health Illness. 2014;36(2):157–162. doi: 10.1111/1467-9566.12140. [DOI] [PubMed] [Google Scholar]
- 31.Blue S., Shove E., Carmona C., Kelly M.P. Theories of practice and public health: understanding (un)healthy practices. Crit. Publ. Health. 2016;26(1):36–50. [Google Scholar]
- 32.Bønnelycke J., Sandholdt C.T., Jespersen A.P. Household collectives: resituating health promotion and physical activity. Sociol. Health Illness. 2019;41(3):533–548. doi: 10.1111/1467-9566.12832. [DOI] [PubMed] [Google Scholar]
- 33.Winther J. Routines on trial the roadwork of expanding the lab into everyday life in an exercise trial in Denmark. Ethnol. Scand. 2018;48:98–122. [Google Scholar]
- 34.Winther J., Hillersdal L. Balancing methodological purity and social relevance: monitoring participant compliance in a behavioural RCT. BioSocieties. 2020:1–25. [Google Scholar]
- 35.Ross R., Goodpaster B.H., Koch L.G., Sarzynski M.A., Kohrt W.M., Johannsen N.M., et al. Precision exercise medicine: understanding exercise response variability. Br. J. Sports Med. 2019;53:1141–1153. doi: 10.1136/bjsports-2018-100328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Besson H., Brage S., Jakes R.W., Ekelund U., Wareham N.J. Estimating physical activity energy expenditure, sedentary time, and physical activity intensity by self-report in adults. Am. J. Clin. Nutr. 2010 doi: 10.3945/ajcn.2009.28432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Request for data should be addressed to the corresponding author and specify how data will be used.