Abstract
Herbal cigarettes, known as tobacco-free or nicotine-free cigarettes, are those recognized as being-tobacco free, being composed of a mixture of various herbs claimed to lessen the smoking habit hazards. However, controversial data regarding its properties occur in the literature with no comprehensive overview or analysis of its effects. Like herbal smokeless tobacco, they are often used to substitute for tobacco products (primarily cigarettes) regarded as a “nonsmoking” aid. This review capitalizes on herbal cigarettes with regard to their quality characteristics, sensory attributes, chemical composition, and health properties to rationalize their choice as a nonsmoking aid. Furthermore, the impacts of heat and/or pyrolysis that occur during smoking on its chemical composition are presented for the first time. Some herbal smokes may produce notable metabolic problems that increase the risk of several chronic metabolic diseases. In general, burning substances from plants can have a variety of negative effects on the body attributed to toxic chemicals such as carbon monoxide, polyaromatics, nicotine, and N-nitrosamines. This review compiles and discusses the phytochemical compositions detected in various herbal cigarettes alongside sensory and quality attributes and health effects.
Introduction
Smoking, which refers to inhaling and exhaling the vapors produced by the combustion of plant material, is most commonly linked with the use of tobacco products such as cigarettes, cigars, and pipes.1 Smoking became a public health threat with a prevalence of 1.1 billion smokers worldwide, causing more than 8 million deaths yearly.2 Furthermore, 7 million of those deaths are due to the direct effect of tobacco, whereas the rest are due to secondhand smoke exposure. In addition, tobacco use is linked to an elevated risk of a variety of unfavorable health outcomes, including cardiovascular disease, numerous forms of cancer, diabetes, and stroke.3−5 The value of the global tobacco market in 2021 was US $849.9 billion due in significant part to the rising number of smokers in developing nations.6 Such a smoking habit is also difficult to control due to the serious addictive consequence of tobacco associated with nicotine’s pharmacological actions. Cigarette smoke encompasses ca. 5000 different chemical compounds,7 with 44 of them confirmed to be genotoxic and cytotoxic, according to the Hoffmann list, including inorganic compounds, ethers, hydrocarbons, amines, phenols, alcohols, ketones, aldehydes, carboxylic acids, and amides. Examples of the most hazardous chemicals in tobacco smoke include nicotine, tobacco-specific nitrosamine, carbon monoxide, formaldehyde, and benzene.8 The number of smokers attempting to quit smoking has increased during the past few years. Smoking-cessation education has been implemented in a number of nations worldwide; however, few smokers have succeeded, representing ca. 4% in 1 year, attributed mostly to the strong addictive power of nicotine alkaloid in tobacco.9 With an increasing awareness of tobacco smoking hazards, several pharmacological interventions have been introduced in the smoking-cessation program such as nicotine-replacement therapies, e.g., gum, patch, lozenge, and inhaler, and non-nicotine based, such as varenicline, sustained-release bupropion, and nortriptyline.10 Other alternative practices, which are mistakenly perceived by smokers as being less harmful than cigarette smoking, are electronic cigarettes, waterpipe cigarettes, and herbal cigarettes.11,12 Addicted smokers that are unable or unwilling to quit smoking are likely to have the perception that they are benefiting from administering these products with less toxins to smokers upon inhalation.
In Western countries, herbal cigarettes employ materials, such as hazel and rose petals, that are neither considered therapeutic nor combined with tobacco. However, an herbal cigarette in an Asian region is a cigarette that contains a combination of tobacco and Asian herbs that are historically used for therapeutic purposes.13 Herbal plants were used traditionally to treat various diseases due to the presence of bioactive metabolites that exhibited numerous pharmacological effects.14−25 For example, it was believed that a cannabis cigarette is useful for neuropathic pain.26 Various studies showed the pharmacological effect of this herbal plant.27,28 Herbal cigarettes are believed generally to be healthier or safer than tobacco ones; however, there is a lack of strong proof regarding their effects, with several doubts raised for the likely miscomprehension of these herbs as being safe. This is more complicated by the fact that, although their chemical composition is well-known, little knowledge is provided regarding the post-burning action upon inhalation. Several companies advertise herbal cigarettes as a safe alternative from the perspective of being composed of safe herbal drugs.29 China was the first country to create herbal-tobacco cigarettes between 1959 and the early 1970s, originally for the treatment of asthma and bronchitis patients.13 Other Asian manufacturers of herbal cigarettes are found in South Korea, Thailand, and Taiwan.30 Changle (Long Happiness) was the first herbal cigarette brand marketed by the Beijing Cigarette Factory in 1982. Many other brands were further manufactured in China; however, Jinsheng and Wuyeshen brands achieved the highest sales during the year 2008.31 Between 1959 and 2004, 23 Asian brands of herbal cigarettes were marketed, among which 11 brands were reported to contain primarily herbal ingredients, 8 brands were reported to contain a blend of herbs, whereas only 4 brands contained one herb. The actual composition of herbal ingredients found in these herbal cigarettes and the method of preparation are not explicitly revealed, although it is stated in most of the cases.13 Asian tobacco companies claim that herbal cigarettes aid in reducing smoking-withdrawal symptoms and lessen health hazards to aid in quitting smoking.32 For example, 12 brands were claimed to treat upper respiratory tract diseases, 10 brands were declared to contain lower tar levels and carcinogens compared to tobacco cigarettes, and 3 brands asserted that they enhanced body immunity.13,30 However, no sufficient studies were conducted to prove such a hypothesis nor to evaluate its exact chemical compositions of different herbal cigarettes and/or safety.33 The production of novel chemicals from the interaction of such a complex blend comprising different herbs is also likely to occur, especially at such a high burning temperature.
With regard to the most common herbal component found in these different brands, ginseng was found to constitute a major ingredient in 4 marketed brands, such as Hsiang Yang Ginseng, YiXing, and Sante Luxury.13Panax ginseng has long been used in many Asian countries as an herbal remedy (China, Korea, and Japan) (Table 1). Apocynum venetum represents another major constituent in two herbal cigarettes products, i.e., Changle and JinJian,13 that has been used traditionally in traditional Chinese medicine (TCM) and as a tea.34 In Western countries, menthol cigarettes were endorsed in the United States in 192535 by manufacturer’s brands, such as Spud, Penguin, and Kool, as being healthier owing to their menthol content, because menthol is commonly used in throat lozenges.36,37 Print and broadcast commercials promoted menthol cigarettes to relieve throat irritation accompanying allergies and/or a common cold.29 The approach of tobacco control has been programmed by several public health groups and researchers to convince smokers to refrain from smoking and to rely more on herbal cigarettes. Studies have attempted to determine the health benefits of smoking herbal cigarettes by determining the yields of tobacco-specific nitrosamines in mainstream smoke or by evaluating cellular reactivity to mainstream smoke.33 Yet, there is not enough solid evidence of a public health benefit of herbal cigarette consumption, and this approach may dispirit smokers from quitting. A more complicated problem is that smokers might even smoke these tobacco-free herbal cigarettes more frequently than regular ones, which might pose more health hazards.31 The chronic consumption effect of these different herbal cigarettes in human studies have been evaluated in only a few reports, insufficient enough to be conclusive. The main goal of this review is to critically analyze all reports on herbal cigarettes, regarding their quality characteristics as well as sensory characters, phytochemicals, health benefits, and/or safety. Moreover, extrapolation from research on the thermal impact on these herbal drugs is made herein to fulfill the gap in the literature regarding how these herbal cigarette chemicals change upon burning. Figure 1 displays the theme of the review and different parts to be covered. By critically reviewing the advantages and disadvantages of each herbal cigarette, the perspective of the best formulation that is likely to be safer for consumption is highlighted, along with needed additional research to be conducted for proof of safety of other less-explored cigarettes. The most common herbal drugs present in herbal cigarettes are discussed in the next section.
Table 1. Herbal Cigarette Brands in the Market, Their Origins, and Their Ingredients.
| brands | origin | ingredients | references |
|---|---|---|---|
| Herbal Gold cigarettes (100% nicotine free) | U.S.A. | menthol, Prunus cerasus (cherry), Vanilla planifolia (vanilla), Althaea officinalis (marshmallow), Eriodictyon californicum (yerba santa), damiana, Passiflora incarnata (passion flower), Jasminum officinale (jasmine), and Panax ginseng (ginseng) | (64) |
| Blue | Korea | Artemisia absinthium (wormwood) | (13) |
| KangXi | China | Tropaeolum peregrinum (canary-creeper) | (13) |
| JiangShan (River & Mountain) | China | Paeoniae Radix (herbaceous peony), Bupleurum chinense (thorowax), Curculigo orchioides (curculigo) rhizome, Epimedium grandiflorum (longspur epimedium) | (13) |
| Zhongnanhai | China | Apocynum venetum (spreading dogbane) | (13) |
| Guocao | China | Artemisia vulgans (mugwort) and other herbs | (13) |
| JiangShan (River & Mountain) | China | Paeoniae Radix (herbaceous peony) | (13) |
| Herbal Krongthip | Thailand | Andrographis paniculata (Green chireta) | (13) |
| Hsiang Yang Ginseng/YiXing (Changing stars) | China | Panax ginseng (ginseng) | (13) |
| Honeyrose | England | Panax ginseng (ginseng) and Syzygium aromaticum (clove) | (13) |
| Jinjian | China | Panax ginseng (ginseng) | (13) |
| Billy | U.S.A. | Camellia sinensis (green tea) | (13) |
| Nosmo Q “Kumyeoncho” | Korea | Eucommia ulmoides (Tu-chung) | (32) |
| Herbal bidis (Darshan, Ecstacy, Azad (meaning “free”), and Sadhu (meaning “a sage”) | India | not specified | (65) |
| Yogi Mint Bidis | India | blend of cured Indian herbs wrapped in mint leaves | (65) |
| Potter’s asthma cigarettes | India and U.K. | shredded Datura stramonium (Devil’s Trumpet) leaves | (66, 67) |
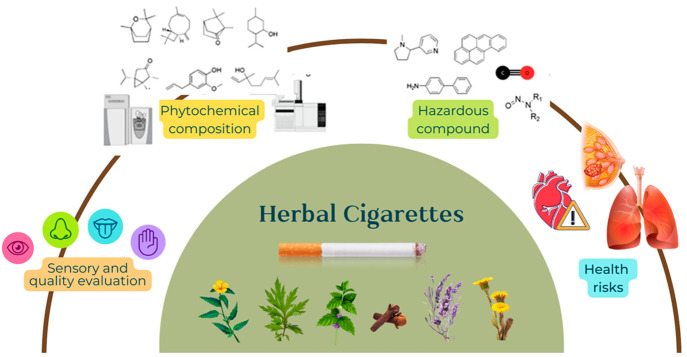
Figure 1.
Theme of the review and different parts covered about herbal cigarettes. This figure shows the main topics covered including phytochemical composition detected in various herbal cigarettes and sensory and quality evaluations from previous studies on herbal cigarettes. We also include the findings on hazardous compounds related to the health risks reported in previous studies.
Rationale for the Current Review
Smoking has become a public health threat worldwide, leading to several diseases. With an increasing awareness of tobacco smoking hazards, several pharmacological interventions are introduced in the smoking-cessation program, such as nicotine-replacement therapies. Likewise, herbal cigarettes, often known as tobacco-free cigarettes, are cigarettes that do not contain any tobacco and are instead made up of a mixture of various herbs and/or other plant materials, whereas other herbal cigarettes encompass tobacco with other herbs added to improve flavor or quality. Herbal cigarettes are categorized as a nonsmoking aid. Herbal cigarettes are also used in acting situations by nonsmokers and are becoming more prevalent in areas where antismoking legislation restricts the use of tobacco in public places. Herbal cigarettes are gaining popularity throughout the world as a substitute for tobacco products, particularly cigarettes, and are generally believed to be healthier or safer than tobacco cigarettes. Moreover, numerous companies promote herbal cigarettes as a safe alternative due to their composition of safe herbal drugs. However, there is insufficient convincing evidence that herbal cigarettes have a positive effect on public health. We summarize the current evidence on quality characteristics, sensory characteristics, phytochemicals, and health properties of herbal cigarettes. In addition, we discuss the scientific findings on how these herbal cigarette chemicals change when they are burned. This review is intended for cigarette researchers, food chemists, cigarette manufacturers, and the public worldwide.
Survey Methodology
Literature was reviewed using electronic databases, including Web of Science, Science Direct, PubMed, Google Scholar, Wiley, and SciELO. This review included English-language publications published in peer-reviewed journals between the earliest record date and February 28, 2022. The search results were obtained by utilizing phrases such as “herbal cigarettes”, “plant used for smoking”, “smokable plants”, or “danger of herbal cigarettes”. Duplicate publications were eliminated manually, yielding a total of 103 peer-reviewed papers. This review includes three main sections that include the current level of knowledge on reported plants used as herbal cigarette alternatives in terms of chemical composition, health advantages, and rationale for their inclusion in herbal cigarettes. Furthermore, for the first time, the health risks associated with such chemical changes in these substitutes are discussed. The changes incurred by burning to affect chemical composition and health hazards of the herbal cigarettes are summarized in this review. This review capitalizes on herbal cigarettes regarding both chemical composition and health properties. Because there has not been such a comprehensive compilation of studies on this topic, we investigated pertinent related literature dating back as far as the late 1980s; however, we primarily concentrated on publications from the last 10 years.
Herbal Plants Used in Herbal Cigarettes
Herbal cigarettes use herbs as the raw material instead of tobacco leaf alone. According to studies, many smokers use herbal cigarettes as a nonsmoking aid even though the safety issues are not well-documented.38 In this section, we discuss the traditional uses and physicochemical and chemical compounds of several herbs that were used as ingredients in the cigarettes.
Damiana
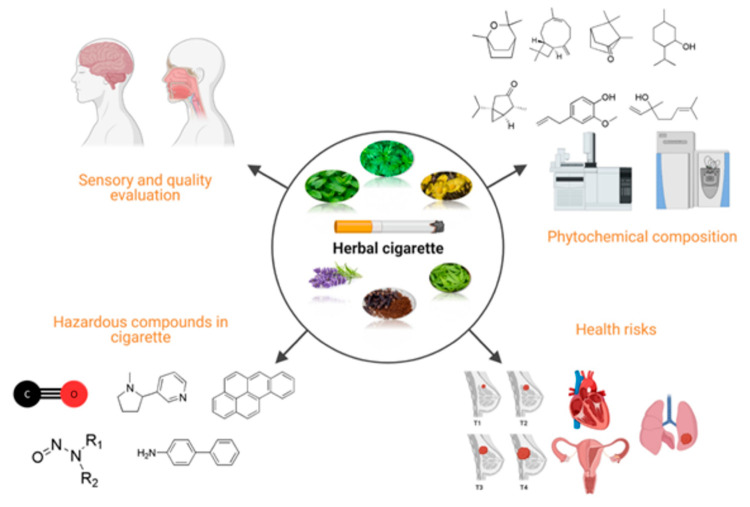
The main chemicals in herbs included in herbal cigarettes are depicted in Figure 2. Turnera diffusa (Passifloraceae) is one of the most highly valued plants used as aphrodisiacs.39 Damiana has a pleasant appearance, smell, and taste. It is a tasty herb with a hickory-like flavor that is best described as minty and peppery, and overall it produces a pleasant smoke. It has a moderately spicy smell with undertones of anise and citrus that fits this profile. Damiana tea is caffeine-free; however, it is relaxing to the digestive system and may alleviate tension and anxiety. It was banned for reportedly being incorporated in synthetic cannabis concoctions, often known as spice. Damiana can cause hallucinations in high dosages, and it is not advisible to smoke damiana or inhale it. Damiana has a long history of usage as a central nervous system (CNS) psychoactive herb, which could be the reason for its use as a substitute for tobacco40 along with its traditional uses. With regard to the aroma chemicals likely inhaled if present in herbal cigarettes, sesquiterpenes amounted to major components, viz., copaene, γ-muurolene, cubebol, δ-cadinene, nerolidol, germacrene d-4-ol, caryophyllene oxide, ledol, β-eudesmol, and juniper camphor.41
Figure 2.
Main chemicals and their sensory and health attributes in herbs included in herbal cigarettes. Six herbal plants are presented including damiana, clove, peppermint, coltsfoot, lavender, and mugwort, which are among the main ingredients in herbal cigarette alongside their main chemicals.
Mullein
Mullein (Verbascum thapsus L.) (Scrophulariaceae) is originated from North America, Europe, and temperate Asia. This medicinal herb has numerous chemical constituents, such as flavonoids, saponins, phenylethanoid glycosides, iridoids, and vitamin C, to contribute to its anti-inflammatory, antihyperlipidemic, antioxidant, antimicrobial, anticancer, antiviral, and antihepatotoxic activities.42 The mullein demulcent action is used to relieve irritation mostly attributed to the expectorant action of its saponins along with the soothing effect of its mucilage.43 The dried leaves are sometimes smoked in an ordinary tobacco pipe to relieve irritation of the respiratory mucus membrane. Nevertheless, it should be noted that both are high molecular weight polar compounds and are unlikely to be volatilized upon smoking, and it is suggestive that other chemicals are released in its smoke.
Coltsfoot
Coltsfoot (Tussilago farfara) (Asteraceae) is native to Europe and parts of Western and Central Asia.44 Its flowers and leaves have long been used to treat respiratory disorders, i.e., coughs and sore throat,45 in addition to its inclusion in beverages and foods. Although none of coltsfoot’s constituents used for its demulcent action are volatile and likely to be inhaled in smoke, herbal tobaccos with blends of coltsfoot are popular to be smoked for treating asthma, especially in United Kingdom. Mucilage has been recognized as the major ingredient accounting for coltsfoot’s pharmacological action as a demulcent. A volatile component in coltsfoot likely inhaled in herbal cigarettes is tussilagone, a sesquiterpene reported as a potent respiratory and cardiac stimulant.44 Another herb used in herbal cigarettes with a similar action, and also to exert a respiratory stimulant effect due to its alkaloid lobeline, is lobelia, which is no longer used.45 It should be noted that coltsfoot is classified as a dietary supplement and as an “herb of undefined safety” by the FDA.
Ginseng
Ginseng (Panax ginseng) (Araliaceae) is known to possess many useful pharmacological activities, which is attributed to its high content of active ingredients. Ginseng flavor is very strong, and it is usually enhanced by the inclusion of honey and fruit juices. It has been used in many Asian countries, such as China, Korea, and Japan, in folk medicine and as a flavoring herb.13 Chinese people used ginseng as an additive in herbal cigarettes,30,46 and it was found to be a major ingredient in four herbal cigarette brands.13 Ginseng is known to be used as an aphrodisiac and to improve psychologic function. However, a report stated that ginseng induced overactivity with sleep disturbances when smoked as an herbal cigarette.47
Mugwort
Mugwort (Artemisia vulgaris) has many traditional uses around the world, which is attributed to its richness of many chemicals, including essential oils.48 The plant is rich in sesquiterpenes responsible for the serotonergic mechanism, and this could be the reason for its traditional application to treat imbalances that women may suffer due to menopausal symptoms.49 According to the European Commission in 2020, this drug has historically been used as a substitute for cannabis when smoked; it possesses mild intoxicating and strong relaxing properties. The species A. vulgaris is highly prized as a spice due to the herb’s aroma and bitter taste, as well as the root’s sweet and spicy flavor. Traditional Chinese medicine also recommends inhaling the smoke that results from burning the dried and powdered leaves of A. vulgaris.48
Peppermint
Peppermint (Mentha piperita) (Lamiaceae) has a long history of safe use in mint-flavored foods and has been utilized in folk medicine for its thermoregulating “cooling” effect.50 Peppermint is commonly included in cigarettes owing to its strong menthol flavoring action together with its cooling sensation and has been postulated to mask nicotine’s irritation and harshness, soothe the taste, and add a pleasant flavor to the smoke.51,52 Menthol and nicotine have also been shown to stimulate sensory nerve endings in the nasal, oral, and pulmonary mucosae when inhaled simultaneously.53
Lavender
The effects of lavender essential oil Lavandula angustifolia (Lamiaceae) in patients with cigarette cravings54 were assessed, revealing reductions in anxiety, cravings for tobacco, blood pressure, and heart rate upon inhalation. Such an effect helped to reduce tobacco-withdrawal syndrome in adult smokers as compared to placebo and nicotine-administered groups, posing it as a potential treatment for cigarette cessation. Another study assessed the effects of lavender oil on CNS, autonomic nervous system, and mood responses in humans post-inhalation. Results revealed that lavender oil showed a reduction in heart rate, blood pressure, and skin temperature. In terms of mood responses, those inhaling lavender oil were described as being more lively, fresher, and more relaxed than those inhaling sweet almond oil alone.55 Whether such effects are ascribed to lavender oil main active C10 monoterpene linalool or a synergism of the many other volatile constituents in its oil has yet to be clarified using detailed analyses by testing single individual compounds. Linalool, on the other hand, has been shown to have anxiolytic characteristics in a light/dark test, as well as producing improved social interaction and reduced aggressive behavior in mice when inhaled.56
Thyme
Thyme (Thymus vulgaris F.) (Lamiaceae), native to Mediterranean regions and commonly used as a culinary herb, was reported to be used as an herbal cigarette,57 and this could be due to the presence of thymol, one of the major constituents of thyme essential oil (representing 10–64%).58 Thymol has a distinctive aromatic odor and is thought to have potential therapeutic uses in the treatment of respiratory, neurological, and cardiovascular diseases,59 and this can rationalize its use in herbal cigarette blends.
Clove
Clove (Eugenia caryophyllata F.) (Myrtaceae) is known to encompass the major volatile eugenol (up to 95%) in addition to acetyl eugenol, β-caryophyllene, methyl salicylate, pinene, and vanillin. Kretek cigarette manufacturers in Indonesia used cloves, and clove cigarettes are known to be imported from Southeast Asia.60 The Indonesian clove cigarettes had significantly higher levels of anethole, eugenol, and coumarin than commercial cigarette brands that existed in the United States.61 Jakarta, Gudang Garam, Djarum, Sampoerna “A”, Krakatoa, and many other Indonesian-named brands are popular clove cigarettes. Because clove cigarette smoke is thought to have a mild psychotropic and euphoric effect, the neurotoxic effects of eugenol are particularly intriguing. The exposure to high nicotine content may also contribute to the euphoric effect.62
Health Claims of Herbal Cigarettes
Starting from the year 1959, 23 Asian brands of herbal cigarettes were produced and marketed.63 Among these brands, 11 brands were reported to contain primary herbal ingredients, 8 brands were reported to contain a blend of herbs, and only 4 brands contain only herbs. The actual composition of herbal ingredients found in these herbal cigarettes and the method of preparation are not explicitly stated in most of the cases.13Table 1 lists herbal cigarette brands in the market, their origins, and their ingredients. Most of the producing companies claimed that these cigarettes have many health benefits to smokers. Twelve brands were claimed to treat upper respiratory tract diseases, 10 brands were claimed to contain much lower levels of tars and carcinogens compared to tobacco cigarettes, and 3 brands were claimed to enhance body immunity. In addition, claims have been extended to the ability of these herbal cigarettes to replace tobacco cigarettes during the period of smoking cessation.13,30
Berberine was selected as an additive in a cigarette filter to reduce the adverse effects of cigarette smoke on human health. A study was carried out to evaluate the effect of cigarette smoke on the activity of oral peroxidases after berberine was added to the cigarette filter.68 The study was performed on saliva obtained from a consenting smoker revealing that there was loss of activity of oral peroxidases by 20% and 25%, concurrent with a reduction in the hydrogen cyanide level in the mainstream cigarette smoke; hydrogen cyanide presence in cigarette smoke is likely to account for the loss of activity of salivary oral peroxidase,69 which might be related to the berberine inclusion in the cigarette filter.68 No toxicity, mutagenicity, or immunotoxicity were documented for mice inhaling a tobacco substitute primarily composed of Eucommia ulmoides leaf at levels of up to 20 cigarettes per day over 4 weeks.70Figure 2 summarizes the health attributes of herbs included in herbal cigarettes.
Herbal Cigarette Pharmacological Activities
Treatment of Chronic Bronchitis and Influence on Pulmonary Functions
Smoking an herbal cigarette containing atropine alkaloid causes a significant decrease in heart rate, which is consistent with the systemic response to atropine-like alkaloids, and a significant increase in peak expiratory flow rate, which is consistent with the bronchodilator effect of reduced cholinergic activity. Figure 3 and Table 2 reveal the main chemicals and health attributes in herbs included in herbal cigarettes. Smoking herbal cigarettes seems analogous to the inhalation of ipratropium by aerosol for a local bronchodilator effect.67
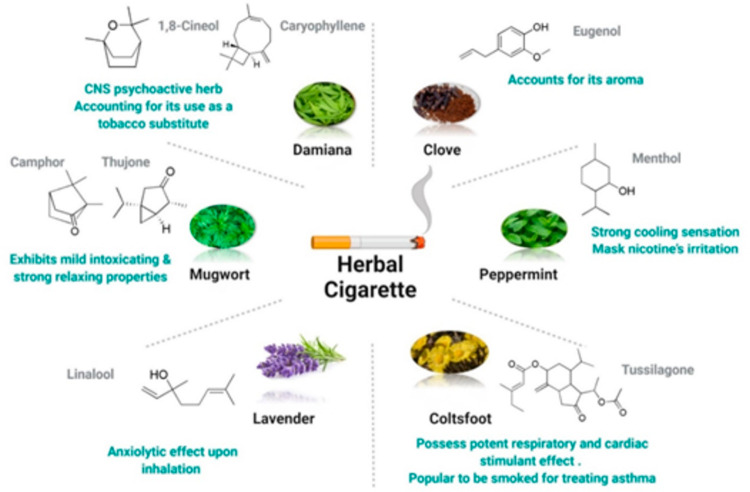
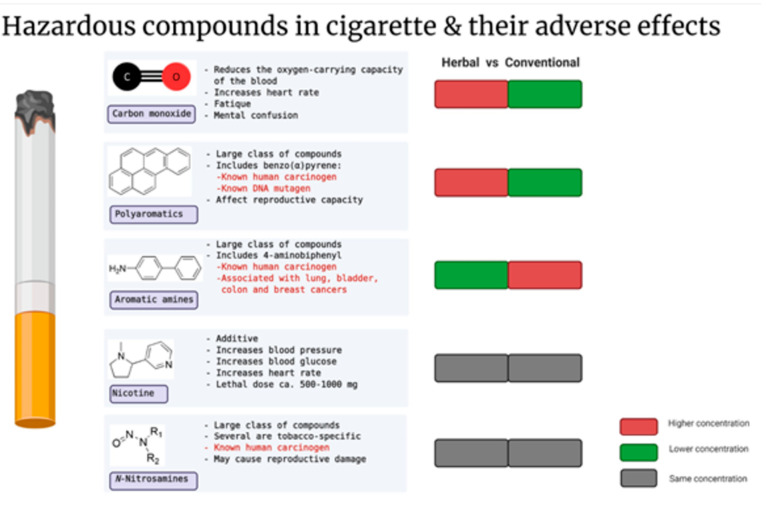
Figure 3.
Hazardous classes of compounds detected in herbal cigarettes and their adverse effects on humans. Most of the hazardous compounds such as carbon monoxide, polyaromatics, aromatic amines, nicotine, and N-nitrosamines are also found in tobacco cigarettes, which are reported for various adverse health effects, including carcinogenic effect, reproductive capacity effect and damage, and mental health issues.
Table 2. Plants Used in Herbal Cigarettes, Major Active Constituents, and Health Benefits and Hazards.
| herb | major active constituent | health benefits upon inhalation | health hazards | reference |
|---|---|---|---|---|
| spreading dogbane (Apocynum venetum) | volatile oils (fatty acids, aldehydes, ketones, esters, alkanes, and phenols) | detoxifying nicotine when used with tobacco | no severe side effects | (13, 34) |
| sedative effect | ||||
| mugwort (Artemisia vulgaris) | mono/sesquiterpenes (eucalyptol, camphor, linalool, thujone, 4-terpineol, borneol, α-cadinol, spathulenol) | smoke reduces heart rate and stress and improves the autonomic nervous system | allergic for the respiratory system and skin, causing dermatitis | (13, 48, 49, 71−74) |
| decreases pain and depression and improves ego integrity | ||||
| Tu-chung (Eucommia ulmoides) | volatile oils (aldehydes, furans, alkenes, alkanes, ketones, aromatic compounds, ethers, and esters) | aroma induces hypnotic effect; leaf extract inhalation improves sleeping and prevents insomnia progression | no signs of toxicity, mutagenicity, or immunotoxicity | (75, 76) |
| clove (Syzygium aromaticum) | eugenol | reduces noxious elements of smoking; smoking cloves relieves asthmatic symptoms | hemoptysis, bronchospasm, hemorrhagic and nonhemorrhagic pulmonary edema, pleural effusion, respiratory insufficiency, respiratory infection, and aspiration | (61, 62, 77−79) |
| Devil’s Trumpet (Datura stramonium) | alkaloids (hyoscyamine and atropine) | calming effect in schizoid patients | anticholinergic syndrome including dry skin, flushing, blurred vision, altered mental status, tachycardia, urinary retention, seizures, coma, and respiratory failure | (67, 80, 81) |
| powerful mind-altering drug | ||||
| lavender (Lavandula angustifolia) | volatile oils (linalyl acetate, β-linalool, and β-caryophyllene) | antianxiety, relaxing, and mood-control effects | some adverse effects occurred with patients receiving lavender aromatherapy | (55, 82, 83) |
| decreases blood pressure, heart rate, and skin temperature | ||||
| aromatherapy using lavender oil proved successfulness and safety in many cases, especially in reducing pain | ||||
| samiana (Turnera diffusa) | sesquiterpenes, copaene, 1,8-cineol, γ-muurolene, oplopenone, cubebol, cubenol, δ-cadinene, nerolidol, thymol, germacrene d-4-ol, caryophyllene oxide, ledol, anethole, β-eudesmol, and juniper camphor | CNS psychoactive and aphrodisiac | long-term use can lead to inflammations of the liver and tetaniform convulsions | (39−41) |
| mullein (Verbascum thapsus L.) | volatile oils obtained from the dried flowering aerial parts (6,10,14-trimethyl-2-pentadecanone and (E)-phytol) | assists in asthma, coughs, bronchitis, and whooping cough | studies proved that phytol is not considered a significant contributor to the PAHs formation in cigarette smoke | (43, 84, 85) |
| burning its dried leaves and inhaling its smoke can help with asthma attacks | ||||
| coltsfoot (Tussilago farfara) | sesquiterpene (tussilagone) | potent respiratory and cardiac stimulant, inhaling the steam from the leaves and flowers soothes bronchitis and helps in shortness of breath | deep vein thrombosis is possibly associated with the use of coltsfoot together with symptomatic pulmonary embolism | (45, 86, 87) |
Antiasthma Herbal Cigarettes
Although smoking is known to cause respiratory distress on occasion, breathing smoke from herbal combinations was recommended for the treatment of asthma and coughing as well as a range of other respiratory disorders (Table 2). Even though inhaling fumes, smoke, and some medical vapors has long been a known remedy for asthma and other respiratory problems, the smoking cure became progressively prevalent among asthmatics and their doctors. The smoking of stramonium leaf and other herbal substances has become increasingly popular to release respiratory distress, and this is due in large part to modern definitions of asthma as a condition characterized by spasmodic bronchoconstriction.88 In addition, the lack of viable alternatives and a growing cultural reliance on cannabis and opium contributed to asthmatics’ increased belief. Greek and Roman physicians such as Hippocrates, Dioscorides, and Galen suggested inhalation for asthma, which they defined as a discrete and moderately severe form of breathing or dyspnoea difficulties, associated with a wheeze and cough.89 Herbal preparations and resinous gums were also delivered in the form of a linctus or syrup, or by an inhalational apparatus. In most Western and Eastern medical traditions, inhaling vapors and smoke played a variable role in the treatment of asthma. The belief that asthma was caused by cold, moist phlegm accumulating in the lungs led to its use in many ancient medical systems, including Yurvedic, Egyptian, and Greek medicine. Despite occasional efforts to promote inhalation, most notably by inhaler inventors and manufacturers, concerns about the efficacy and safety of inhaling medicated vapors or smoke from tobacco and other herbs have pushed inhalation therapies to the periphery of clinical practice.67
Concerns regarding the harmful consequences of smoking herbal cigarettes on asthma patients have not dampened clinical or pharmacological interest in inhalational therapy in general. Major pharmaceutical corporations, on the other hand, put effort into creating inhaled adrenergic drugs and corticosteroids.67 The vaporized version of adrenaline was inhaled as an alternative to subcutaneous and intravenous delivery. Although antiasthma herbal cigarettes have nearly vanished because of such anxieties, the therapeutic values of the smoking cessation have not been completely forgotten. Inhaled treatments continue to dominate asthma management in the current time; herbalists still sell stramonium leaf concoctions for the relief of respiratory disorders, and a large range of herbal smokes are available both online and over the counter from newsagents and tobacconists.67 The Mohegans smoked mullein to relieve asthma and sore throat, whereas the Penobscots and the Forest Potawatomis, two Native American tribes, smoked its dried and powdered leaves to cure asthma.43
Sensory Characteristics of Herbal Cigarettes
To examine characterizing tastes in tobacco products, a variety of methodologies are used, including sensory analysis conducted by experts or consumers, as well as a combination of sensory and chemical analyses.90 Sensory evaluation of herbal cigarettes is necessary to meet consumer acceptability, which involves safety, organoleptic attributes, cultural uncertainty, and marketing based on the use of products. The flavor of herbal cigarettes is a significant monitoring conception in quality control involving mimicking the smoking habit as best as possible.91Figure 2 displays the sensory and health attributes in herbs involved in herbal cigarettes. For characterizing the flavor, usually a qualified expert analyzes the products to identify distinguishing flavors by smelling; such an assessment made by these sensory experts usually aids the tobacco industry to evaluate the sensory characteristics of cigarettes.91,92 In the case of herbal cigarette testing, sensory measures employed include comparing the smells of nonburned cigarettes using a trained sensory expert. The Quantitative Descriptive Analysis (QDA) 21 is commonly used in the food industry to decide upon sensory characteristics of the tested products compared to reference products.91 These sensory analyses are usually confirmed using chemical analytical tools, such as gas chromatography–mass spectrometry (GC-MS).92 A more representative sample of volatile compounds can be obtained using headspace analysis such as static solid phase microextraction and dynamic headspace techniques.93 Headspace GC-MS is one of the most suited methods for the purpose of analyzing herbal cigarette aroma in order to provide extensive coverage of active flavor compounds.94 Headspace GC-MS has been reported for analyzing hookah flavor of different brands and to reveal the burning effect on its aroma composition collected using SPME95 and has yet to be applied for herbal cigarettes. To aid in resolving the complex volatilome as typically encountered in herbal drugs and in the more complicated case of herbal cigarettes, which are composed of a mixture of several agents aside from the heat factor, multivariate data analysis ought to be applied to determine variations among tobacco products in terms of odor attributes.91,96−98 For information regarding the different methods to evaluate the flavor characteristics of tobacco products, please refer to the review in ref (90). With regard to potential problems with the sensory analysis of herbal cigarettes, the loss of cigarette refreshing smell and odor over time is often experienced. For example, these cigarettes yield a strong flavor directly after being introduced to the smokers and then fade before the end of smoking. Another problem that smokers are likely to face with the addition of herbs to tobacco products is the delayed release of flavor, and they may not realize the flavor until a portion of the cigarette is saturated with saliva in the mouth of the smoker.94 There is a strategy applied by tobacco companies for manipulating sensory attributes of cigarettes to assist the initiation of smoking by attracting youth and young adult smokers because of the added flavor and the beliefs about health benefits. This can stimulate a smoking addiction among young smokers and hence contribute to a rise of consumption of cigarette products.90
Herbal Cigarette Risks
Probability of Addiction
Addiction is defined as the loss of control over substance use. According to the evidence, the majority of smokers of herbal cigarettes in the general community are heavily reliant on it. Despite being very motivated to quit smoking and being aware of the dangers on their health, many habitual smokers who want to quit smoking are trying to replace it with herbal cigarettes (Table 2 and Figure 3). Increased addiction has been linked to a lower prospect of quitting smoking. It is possible that it is a better predictor of quitting than motivation. In the case of a man with conditions of being overly active, extremely anxious, disoriented regarding time and place, and frightened and having hallucinations, fixed widely dilated pupils, a pulse rate of 110/min, and a blood pressure of 100/70 mmHg, he had unrolled 18 Potter’s Asthma Remedy cigarettes and put them into an infusion that was likely to contain stramonium leaf, among others.99
Toxicity
In 2015 Bak et al. determined that the mainstream smoke of an herbal cigarette made of Artemesia contains toxic components (Figure 3). They analyzed some of these toxic components, ran a mutagenicity test on smoke condensates, and compared the results to the corresponding values of a standard cigarette with the same tar content, which when measured was higher than that stated on the package. The mainstream smoke of the herbal cigarette contained no detectable levels of tobacco-specific nitrosamines or nicotine, while carbon monoxide and benzo(α)pyrene contents were higher in the herbal cigarette than in the general cigarette, as were phenolic contents such as hydroquinone, resorcinol, and catechol, albeit with a lower cresol level. Aromatic amines, such as 4-aminobiphenyl, were also detected. The smoke condensates of the herbal cigarette exhibited a higher mutagenic potential than the condensates from the general cigarette at the same concentration owing to the combustion products.33
A study performed on commercial menthol cigarettes comparing their aroma profile to regular cigarette smoke concluded that menthol cigarette smoke showed cytotoxicity leading to cell death in plant and human model cells,100 resulting in larger puffs, deeper inhalation, or longer retention time in the lungs; the flavor may play an important role in initiation and sensory stimulation.51,52 Determining menthol impact on smoking behavior can give clues to the mainstream smoke yields of multiple smoke components (e.g., tar and nicotine) and smokers’ exposure to harmful compounds.52 Reports stated that smoking moxa might be considered a health risk because smoke formed during the combustion of mugwort101 revealed the presence of compounds commonly found in cigarettes, such as tar, nicotine, carbon monoxide, polycyclic aromatic hydrocarbons, ammonia, hydrogen cyanide, and polyaromatic amines, which are considered to have a high risk of causing cancer.
Tobacco toxins were measured in the bodies of Chinese herbal cigarette smokers. The principal nicotine metabolites as well as two classes of tobacco carcinogens were investigated in herbal cigarette smokers.31 Between herbal cigarette smokers and regular cigarette smokers, there was no discernible difference in nicotine level, total nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)butanol (NNAL). The metabolite of the main tobacco-specific carcinogen, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, or 1-hydroxypyrene, naphthols, hydroxyfluorene, and 3′-hydroxycotinine levels in urine were lower in herbal cigarette smokers, but not after correcting for creatinine. This finding suggests that herbal cigarette users consume somewhat less nicotine compared to regular cigarette users. The measurement of nicotine level in the various types of cigarettes was not possible; thus, an explanation for the decrease in nicotine level cannot be concluded. The fundamental toxicity of nicotine lies in its ability to sustain addiction, and it is unlikely that extremely modest changes in nicotine exposure, such as those observed in this study, would have any significant impact on the cigarettes’ addiction potential. Among reported cases, no indication of lower exposure to tobacco smoke carcinogen biomarkers has been found in herbal cigarette smokers, implying no lower cancer risk. Although their findings reveal that herbal cigarette smokers have similar levels of carcinogens in their systems as compared to normal cigarette users, they were unable to evaluate the industry’s claim that herbal ingredients reduce carcinogen toxicity. There are not many studies that investigated or supported such claims. Total NNAL or PAHs were found to have substantial relationships with nicotine metabolites (cotinine and trans-3′-hydroxycotinine). The findings are in accordance with previous studies revealing that a link between NNAL and cotinine levels exists among smokers102,103 and suggest that cotinine and trans-3′-hydroxycotinine levels in smokers’ urine reflect total NNAL and total PAH levels in Chinese herbal and regular smokers. After switching from regular cigarettes to herbal cigarettes, herbal users reported higher cigarette consumption. The current study, however, was unable to review the effect of increased consumption on nicotine and carcinogen intake from tobacco smoke due to the cross-sectional methodology among different reports. Future research, particularly with short-term or long-term switching experimental designs, would be of significance in adjusting scenarios for the protection of health and the environment.
Consequences
The health effects of herbal cigarettes are not fully recognized, and our review shows that high-quality longitudinal studies are required to effectively identify and quantify the risks associated with their usage. Despite the limitations of our evaluation methodology and the research included in the study, our findings indicate that herbal cigarettes are at least as dangerous as normal cigarettes. The lack of proof does not negate the necessity to limit the use of herbal cigarettes.
According to our findings, herbal cigarettes show a different shift in quality and safety attributes when compared to tobacco cigarettes. Given the various purported health benefits of herbal cigarettes, the chemical content may influence human health in a way that differs from tobacco cigarettes. This assumption is especially troubling in terms of the long-term health effects of herbal cigarettes. Certain herbal cigarettes, including mugwort, coltsfoot, and damiana, may produce notable metabolic problems, increasing the risk of a variety of chronic metabolic diseases, such as heart disease, stroke, and diabetes.
As a result, it is important to underline that herbal cigarettes should be carefully examined to ensure the highest level of safety. The current study gave comparative insights into the various quality and development characteristics, as well as sensory aspects, phytochemical contents, health advantages, and safety of herbal cigarettes. The risk assessment should go beyond the initial level in order to be considered safe and to deliver the promised health benefits, particularly when big pilot studies on humans of varied ages, genders, lifestyles, and/or races are used. Legislation should be enacted to check and restrict the components of freely accessible herbal cigarettes.
Conclusions and Future Recommendations
Herbal cigarettes known as tobacco-free or nicotine-free cigarettes are those recognized as being tobacco-free and composed of a mixture of various herbs claimed to lessen the smoking habit side effects. However, controversial data regarding their safety and health effects exist in the literature, warranting a detailed analysis of reports on its consumption. Our review suggests that herbal cigarettes have different shifts of quality and safety characteristics compared with tobacco. In view of the previously compiled claimed health benefits of herbal cigarettes, the compounds in herbal cigarettes possibly influence human health in a way that varies from tobacco cigarettes. This assumption is of particular concern concerning the long-term health impacts of herbal cigarettes. Certain herbal cigarettes such as mugwort, coltsfoot, and damiana may cause remarkable metabolic disorders, resulting in the increased risk of numerous chronic metabolic diseases, including heart disease, stroke, and type 2 diabetes. Hence, the suggestion ought to be emphasized that herbal blends need to be looked at carefully to ensure the best safety level. The current review provides comparative insights about the distinctive quality and development features as well as sensory attributes, phytochemical contents, health benefits, and safety of herbal cigarettes. Generally, the burning of herb-derived constituents may affect the human body in many ways and cause serious diseases. The reported alterations of phytochemicals found in herbal cigarettes can ultimately influence the human body; based on that information, a precise mechanism of diseases possibly caused by chronic exposure to herbal cigarettes is still not clear. However, the current review initiates intellectual thinking and insights about the harmful effect of herbal cigarettes. The hazardous compounds found in herbal cigarettes include carbon monoxide, polyaromatics, nicotine, and N-nitrosamines. Besides, cotinine and trans-3′-hydroxycotinine contents were assessed in smokers’ urine, reflecting total NNAL and total PAH levels in Chinese herbal smokers as compared to regular smokers. To improve the understanding of quality, sensory, and safety characteristics based on chemical composition and the health benefits of used herbs, accurate testing involving advanced technology needs to be performed frequently over an extended time. The risk assessment ought to go farther than the initial level to be deliberately safe and to fulfill the claimed health benefits, especially using large pilot studies on humans from different ages, genders, lifestyles, and/or races. Legislation should be imposed to inspect the easily accessible herbal cigarettes and control their constituents.
Glossary
Abbreviations
- NNAL
4-(Methylnitrosamino)-1-(3-pyridyl)-1-butanol
- PAHs
Polycyclic aromatic hydrocarbons
- QDA
Quantitative descriptive analysis
- GC-MS
Gas chromatography–mass spectrometry
- SPME
Solid-phase microextraction
The authors declare no competing financial interest.
References
- Ren M.; Tang Z.; Wu X.; Spengler R.; Jiang H.; Yang Y.; Boivin N. The Origins of Cannabis Smoking: Chemical Residue Evidence from the First Millennium BCE in the Pamirs. Sci. Adv. 2019, 5 (6), eaaw1391. 10.1126/sciadv.aaw1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Global Report on Trends in Prevalence of Tobacco Smoking 2000–2025; World Health Organization: Geneva, 2018.
- Śliwińska-Mossoń M.; Milnerowicz H. The Impact of Smoking on the Development of Diabetes and Its Complications. Diabetes Vasc. Dis. Res. 2017, 14 (4), 265–276. 10.1177/1479164117701876. [DOI] [PubMed] [Google Scholar]
- Kondo T.; Nakano Y.; Adachi S.; Murohara T. Effects of Tobacco Smoking on Cardiovascular Disease. Circ. J. 2019, 83 (10), 1980–1985. 10.1253/circj.CJ-19-0323. [DOI] [PubMed] [Google Scholar]
- Zhang Y.; He J.; He B.; Huang R.; Li M. Effect of Tobacco on Periodontal Disease and Oral Cancer. Tob. Induced Dis. 2019, 17, 40. 10.18332/tid/106187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobacco Market Size, Share & Trends Analysis Report By Product (Smokeless, Cigarettes, Cigars & Cigarillos, Next-Generation Products, Waterpipes), By Distribution Channel (Online, Offline), By Region, And Segment Forecasts, 2022–2030. https://www.grandviewresearch.com/industry-analysis/tobacco-market (accessed Oct 7, 2022).
- Perfetti T. A.; Rodgman A. The Complexity of Tobacco and Tobacco Smoke.. Beitrage zur Tab. Int. Contrib. to Tob. Res. 2011, 24 (5), 215–232. 10.2478/cttr-2013-0902. [DOI] [Google Scholar]
- Talhout R.; Schulz T.; Florek E.; Van Benthem J.; Wester P.; Opperhuizen A. Hazardous Compounds in Tobacco Smoke. Int. J. Environ. Res. Public Health. 2011, 8 (2), 613–628. 10.3390/ijerph8020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R.; Keely J.; Naud S. Shape of the Relapse Curve and Long-Term Abstinence among Untreated Smokers. Addiction 2004, 99 (1), 29–38. 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Cahill K.; Stevens S.; Perera R.; Lancaster T.. Pharmacological Interventions for Smoking Cessation: An Overview and Network Meta-Analysis. Cochrane Database Syst. Rev. 2015, 2015; 10.1002/14651858.CD009329.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E. S.; Seo H. G. The Factors Associated with Successful Smoking Cessation in Korea. J. Korean Acad. Fam. Med. 2007, 28 (1), 39–44. [Google Scholar]
- Fromme H.; Schober W. Waterpipes and E-Cigarettes: Impact of Alternative Smoking Techniques on Indoor Air Quality and Health. Atmos. Environ. 2015, 106, 429–441. 10.1016/j.atmosenv.2014.08.030. [DOI] [Google Scholar]
- Chen A.; Glantz S.; Tong E. Asian Herbal-Tobacco Cigarettes: “Not Medicine but Less Harmful”?. Tob. Control 2007, 16 (2), 113. 10.1136/tc.2006.016568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahan I.; Khan M. F.; Sayeed M. A.; Arshad L.; Hossen M. A.; Jakaria M.; Ağagündüz D.; Haque M. A.; Capasso R. Neuropharmacological and Antidiarrheal Potentials of Duabanga Grandiflora (DC.) Walp. Stem Bark and Prospective Ligand–Receptor Interactions of Its Bioactive Lead Molecules. Current Issues in Molecular Biology. 2022, 44, 2335–2349. 10.3390/cimb44050159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arman M.; Chowdhury K. A. A.; Bari M. S.; Khan M. F.; Huq M. M. A.; Haque M. A.; Capasso R. Hepatoprotective Potential of Selected Medicinally Important Herbs: Evidence from Ethnomedicinal, Toxicological and Pharmacological Evaluations. Phytochem. Rev. 2022, 21, 1863–1886. 10.1007/s11101-022-09812-5. [DOI] [Google Scholar]
- Fahad F. I.; Barua N.; Islam M. S.; Sayem S. A.; Barua K.; Uddin M. J.; Chy M. N.; Adnan M.; Islam M. N.; Sayeed M. A.; Emran T. B.; Simal-Gandara J.; Pagano E.; Capasso R. Investigation of the Pharmacological Properties of Lepidagathis hyalina Nees through Experimental Approaches. Life 2021, 11, 180. 10.3390/life11030180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin Chy M. N.; Adnan M.; Chowdhury M. R.; Pagano E.; Kamal A. T. M. M.; Oh K. K.; Cho D. H.; Capasso R. Central and Peripheral Pain Intervention by Ophiorrhiza rugosa Leaves: Potential Underlying Mechanisms and Insight into the Role of Pain Modulators. J. Ethnopharmacol. 2021, 276, 114182. 10.1016/j.jep.2021.114182. [DOI] [PubMed] [Google Scholar]
- Hossain S.; Urbi Z.; Karuniawati H.; Mohiuddin R. B.; Moh Qrimida A.; Allzrag A. M.; Ming L. C.; Pagano E.; Capasso R. Andrographis paniculata (Burm. f.) Wall. Ex Nees: An Updated Review of Phytochemistry, Antimicrobial Pharmacology, and Clinical Safety and Efficacy. Life 2021, 11, 348. 10.3390/life11040348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M. F.; Kader F. B.; Arman M.; Ahmed S.; Lyzu C.; Sakib S. A.; Tanzil S. M.; Zim A. F. M. I. U.; Imran M. A. S.; Venneri T.; Romano B.; Haque M. A.; Capasso R. Pharmacological Insights and Prediction of Lead Bioactive Isolates of Dita Bark through Experimental and Computer-Aided Mechanism. Biomed. Pharmacother. 2020, 131, 110774. 10.1016/j.biopha.2020.110774. [DOI] [PubMed] [Google Scholar]
- Freitas M. A.; Vasconcelos A.; Gonçalves E. C. D.; Ferrarini E. G.; Vieira G. B.; Cicia D.; Cola M.; Capasso R.; Dutra R. C. Involvement of Opioid System and TRPM8/TRPA1 Channels in the Antinociceptive Effect of Spirulina platensis. Biomolecules 2021, 11, 592. 10.3390/biom11040592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ağagündüz D.; Şahin T. Ö.; Yılmaz B.; Ekenci K. D.; Duyar Özer Ş.; Capasso R. Cruciferous Vegetables and Their Bioactive Metabolites: From Prevention to Novel Therapies of Colorectal Cancer. Evidence-Based Complementary and Alternative Medicine 2022, 2022, 1534083. 10.1155/2022/1534083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández J.; Silván B.; Entrialgo-Cadierno R.; Villar C. J.; Capasso R.; Uranga J. A.; Lombó F.; Abalo R. Antiproliferative and Palliative Activity of Flavonoids in Colorectal Cancer. Biomed. Pharmacother. 2021, 143, 112241. 10.1016/j.biopha.2021.112241. [DOI] [PubMed] [Google Scholar]
- Chakraborty A. J.; Mitra S.; Tallei T. E.; Tareq A. M.; Nainu F.; Cicia D.; Dhama K.; Emran T. B.; Simal-Gandara J.; Capasso R. Bromelain a Potential Bioactive Compound: A Comprehensive Overview from a Pharmacological Perspective. Life 2021, 11, 317. 10.3390/life11040317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq U.; Khan T.; Shah S. A.; Hossain M. S.; Ali Y.; Ullah R.; Raziq N.; Shahid M.; Capasso R. Isolation, Characterization and Neuroprotective Activity of Folecitin: An In Vivo Study. Life 2021, 11, 825. 10.3390/life11080825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goni O.; Khan M. F.; Rahman M. M.; Hasan M. Z.; Kader F. B.; Sazzad N.; Sakib M. A.; Romano B.; Haque M. A.; Capasso R. Pharmacological Insights on the Antidepressant, Anxiolytic and Aphrodisiac Potentials of Aglaonema hookerianum Schott. J. Ethnopharmacol. 2021, 268, 113664. 10.1016/j.jep.2020.113664. [DOI] [PubMed] [Google Scholar]
- Wilsey B.; Marcotte T.; Tsodikov A.; Millman J.; Bentley H.; Gouaux B.; Fishman S. A Randomized, Placebo-Controlled, Crossover Trial of Cannabis Cigarettes in Neuropathic Pain. J. Pain 2008, 9 (6), 506–521. 10.1016/j.jpain.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrarini E. G.; Paes R. S.; Baldasso G. M.; de Assis P. M.; Gouvêa M. C.; Cicco P. De; Raposo N. R. B.; Capasso R.; Moreira E. L. G.; Dutra R. C. Broad-Spectrum Cannabis Oil Ameliorates Reserpine-Induced Fibromyalgia Model in Mice. Biomed. Pharmacother. 2022, 154, 113552. 10.1016/j.biopha.2022.113552. [DOI] [PubMed] [Google Scholar]
- Vieira G.; Cavalli J.; Gonçalves E. C. D.; Braga S. F. P.; Ferreira R. S.; Santos A. R. S.; Cola M.; Raposo N. R. B.; Capasso R.; Dutra R. C. Antidepressant-Like Effect of Terpineol in an Inflammatory Model of Depression: Involvement of the Cannabinoid System and D2 Dopamine Receptor. Biomolecules 2020, 10, 792. 10.3390/biom10050792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton C. D.; Robinson R. G. The Marketing of Menthol Cigarettes in the United States: Population, Messages, and Channels. Nicotine Tob. Res. 2004, 6, S83–S91. 10.1080/14622203310001649504. [DOI] [PubMed] [Google Scholar]
- Xisoming L.Herbal Cigarettes in China: Not Quite Healthy, But...; Bates: 1988; No. 325304611–325304612.
- Gan Q.; Yang J.; Yang G.; Goniewicz M.; Benowitz N. L.; Glantz S. A. Chinese “Herbal” Cigarettes Are as Carcinogenic and Addictive as Regular Cigarettes. Cancer Epidemiol. Biomarkers Prev. 2009, 18 (12), 3497–3501. 10.1158/1055-9965.EPI-09-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheong Y. S. The Efficacy of Herbal Cigarettes (Kumyeoncho) and Nicotine Patches in Smoking Cessation. J. Korean Acad. Fam. Med. 2003, 24 (11), 1003–1009. [Google Scholar]
- Bak J. H.; Lee S. M.; Lim H. B. Safety Assessment of Mainstream Smoke of Herbal Cigarette. Toxicol. Res. 2015, 31 (1), 41–48. 10.5487/TR.2015.31.1.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie W.; Zhang X.; Wang T.; Hu J. Botany, Traditional Uses, Phytochemistry and Pharmacology of Apocynum venetum L. (Luobuma): A Review. J. Ethnopharmacol 2012, 141 (1), 1–8. 10.1016/j.jep.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Borio G.The Tobacco Timeline. Tobacco BBS; https://academic.udayton.edu/health/syllabi/tobacco/history2.htm (accessed May 30, 2021).
- Ling P. M.; Glantz S. A. Why and How the Tobacco Industry Sells Cigarettes to Young Adults: Evidence From Industry Documents. Am. J. Public Health 2002, 92 (6), 908–916. 10.2105/AJPH.92.6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson S. J. Marketing of Menthol Cigarettes and Consumer Perceptions: A Review of Tobacco Industry Documents. Tob. Control 2011, 20, ii20–ii28. 10.1136/tc.2010.041939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A.; Sharda S.; Yogitha P.; Goel S.; Goyal A.; Gauba K. Systematic Content Analysis of Online Information on Herbal Smoking Products. Indian J. Tuberc. 2021, 68, S71–S79. 10.1016/j.ijtb.2021.08.021. [DOI] [PubMed] [Google Scholar]
- Szewczyk K.; Zidorn C. Ethnobotany, Phytochemistry, and Bioactivity of the Genus Turnera (Passifloraceae) with a Focus on Damiana - Turnera Diffusa. J. Ethnopharmacol. 2014, 152 (3), 424–443. 10.1016/j.jep.2014.01.019. [DOI] [PubMed] [Google Scholar]
- Rätsch C.The Encyclopedia of Psychoactive Plants: Ethnopharmacology and Its Applications; Park Street Press: South Paris, ME, U.S.A., 2005. [Google Scholar]
- Schäffer M.; Gröger T.; Pütz M.; Zimmermann R. Assessment of the Presence of Damiana in Herbal Blends of Forensic Interest Based on Comprehensive Two-Dimensional Gas Chromatography. Forensic Toxicol. 2013, 31 (2), 251–262. 10.1007/s11419-013-0186-5. [DOI] [Google Scholar]
- Riaz M.; Zia-Ul-Haq M.; Jaafar H. Z. E. Common Mullein, Pharmacological and Chemical Aspects. Rev. Bras. Farmacogn. 2013, 23 (6), 948–959. 10.1590/S0102-695X2013000600012. [DOI] [Google Scholar]
- Turker A. U.; Gurel E. Common Mullein (Verbascum thapsus L.): Recent Advances in Pesearch. Phyther. Res. 2005, 19 (9), 733–739. 10.1002/ptr.1653. [DOI] [PubMed] [Google Scholar]
- Toxicology and Clinical Pharmacology of Herbal Products; Cupp M. J., Ed.; Springer/Humana Press: 2000. [Google Scholar]
- Dailey A.; Cupp M. J.. Coltsfoot. In Toxicology and Clinical Pharmacology of Herbal Products; Humana Press: Totowa, NJ, 2000; pp 191–202. [Google Scholar]
- Guo H.Tobacco product regulation and tobacco industry interference. In Tobacco control in China. Springer: Singapore, 2018; pp. 201−219. [Google Scholar]
- Elvin-Lewis M. Should We Be Concerned about Herbal Remedies. J. Ethnopharmacol. 2001, 75 (2), 141–164. 10.1016/S0378-8741(00)00394-9. [DOI] [PubMed] [Google Scholar]
- Ekiert H.; Pajor J.; Klin P.; Rzepiela A.; Ślesak H.; Szopa A. Significance of Artemisia Vulgaris L. (Common mugwort) in the History of Medicine and Its Possible Contemporary Applications Substantiated by Phytochemical and Pharmacological Studies. Molecules 2020, 25 (19), 4415. 10.3390/molecules25194415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams J. D.; Garcia C.; Garg G. Mugwort (Artemisia vulgaris, Artemisia douglasiana, Artemisia argyi) in the Treatment of Menopause, Premenstrual Syndrome, Dysmenorrhea and Attention Deficit Hyperactivity Disorder. Chin. Med. 2012, 3 (3), 116–123. 10.4236/cm.2012.33019. [DOI] [Google Scholar]
- Harris B. Menthol: A Review of Its Thermoreceptor Interactions and Their Therapeutic Applications. Int. J. Aromather. 2006, 16 (3–4), 117–131. 10.1016/j.ijat.2006.09.010. [DOI] [Google Scholar]
- Ahijevych K.; Garrett B. E. Menthol Pharmacology and Its Potential Impact on Cigarette Smoking Behavior. Nicotine Tob. Res. 2004, 6, S17–S28. 10.1080/14622200310001649469. [DOI] [PubMed] [Google Scholar]
- Lawrence D.; Cadman B.; Hoffman A. C.. Sensory Properties of Menthol and Smoking Topography. Tob. Induced Dis. 2011, 9, S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessirier J. M.; O'Mahony M.; Carstens E. Oral Irritant Properties of Menthol: Sensitizing and Desensitizing Effects of Repeated Application and Cross-Desensitization to Nicotine. Physiol. Behav. 2001, 73 (1–2), 25–36. 10.1016/S0031-9384(01)00431-0. [DOI] [PubMed] [Google Scholar]
- de Almeida Cunha N. B.; Orozco C. M.; de Morais Pordeus L. C.; Fernandes Braga J. E. Effects of Essential Oil of Lavandula angustifolia in Patients with Cigarette Craving. J. Med. Ther. 2018, 2 (3), 4. 10.15761/JMT.1000133. [DOI] [Google Scholar]
- Sayorwan W.; Siripornpanich V.; Piriyapunyaporn T.; Hongratanaworakit T.; Kotchabhakdi N.; Ruangrungsi N. The Effects of Lavender Oil Inhalation on Emotional States, Autonomic Nervous System, and Brain Electrical Activity. J. Med. Assoc. Thai. 2012, 95 (4), 598–606. [PubMed] [Google Scholar]
- Linck V. M.; da Silva A. L.; Figueiró M.; Caramão E. B.; Moreno P. R. H.; Elisabetsky E. Effects of Inhaled Linalool in Anxiety, Social Interaction and Aggressive Behavior in Mice. Phytomedicine 2010, 17 (8–9), 679–683. 10.1016/j.phymed.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Carpar E.; Cicikci E.; Ozer U.; Ozen S. in Psychiatry, R. Smoking of Thyme Herb in a Psychotic Patient: A Case Report. Düşünen Adam J. Psychiatry Neurol. Sci. 2014, 27 (3), 272–274. 10.5350/DAJPN2014270314. [DOI] [Google Scholar]
- Salehi B.; Mishra A. P.; Shukla I.; Sharifi-Rad M.; Contreras M. d. M.; Segura-Carretero A.; Fathi H.; Nasrabadi N. N.; Kobarfard F.; Sharifi-Rad J. Thymol, Thyme, and Other Plant Sources: Health and Potential Uses. Phyther. Res. 2018, 32 (9), 1688–1706. 10.1002/ptr.6109. [DOI] [PubMed] [Google Scholar]
- Al-Bayati F. A. Synergistic Antibacterial Activity between Thymus vulgaris and Pimpinella anisum Essential Oils and Methanol Extracts. J. Ethnopharmacol. 2008, 116 (3), 403–406. 10.1016/j.jep.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Nurdjannah N.; Bermawie N.. Cloves. In Handbook of Herbs and Spices, second ed.; Woodhead Publishing: 2012; Vol. 1, pp 197–215. [Google Scholar]
- Polzin G. M.; Stanfill S. B.; Brown C. R.; Ashley D. L.; Watson C. H. Determination of Eugenol, Anethole, and Coumarin in the Mainstream Cigarette Smoke of Indonesian Clove Cigarettes. Food Chem. Toxicol. 2007, 45 (10), 1948–1953. 10.1016/j.fct.2007.04.012. [DOI] [PubMed] [Google Scholar]
- Singh D.; Gupta R.; Saraf S. A. Herbs–Are They Safe Enough?. An Overview. Crit. Rev. Food Sci. Nutr. 2012, 52 (10), 876–898. 10.1080/10408398.2010.512426. [DOI] [PubMed] [Google Scholar]
- Gupta A.; Sharda S.; Yogitha P.; Goel S.; Goyal A.; Gauba K. Herbal Smoking Products: A Systematic Content Analysis and Mapping of the e-Retail Market. Tob. Control 2021, 31 (4), 572–575. 10.1136/tobaccocontrol-2020-056340. [DOI] [PubMed] [Google Scholar]
- Woolston C.; Calhoun N.. The Hazards of Herbal Cigarettes. Health Day; https://consumer.healthday.com/encyclopedia/smoking-and-tobacco-cessation-36/smoking-cessation-news-628/the-hazards-of-herbal-cigarettes-645340.html (accessed Aug 4, 2021).
- Gupta P. C.; Asma S.. Bidi Smoking and Public Health; Ministry of Health and Family Welfare India: New Delhi, 2008. [Google Scholar]
- Stein S. W.; Thiel C. G. The History of Therapeutic Aerosols: A Chronological Review. J. Aerosol Med. Pulm. Drug Delivery 2017, 30 (1), 20–41. 10.1089/jamp.2016.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson M. Divine Stramonium”: The Rise and Fall of Smoking for Asthma. Med. Hist. 2010, 54 (2), 171–194. 10.1017/S0025727300000235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.; Ye X.; Cui X.; Li X.; Zheng L.; Chen Z. Reducing the Inhibitory Effect of Cigarette Smoke on the Activity of Oral Peroxidase by the Addition of Berberine in Cigarette Filter. Toxicol. Ind. Health 2013, 29 (4), 317–324. 10.1177/0748233711433933. [DOI] [PubMed] [Google Scholar]
- Klein I.; Nagler R. M.; Toffler R.; Van Der Vliet A.; Reznick A. Z. Effect of Cigarette Smoke on Oral Peroxidase Activity in Human Saliva: Role of Hydrogen Cyanide. Free Radic. Biol. Med. 2003, 35 (11), 1448–1452. 10.1016/j.freeradbiomed.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Kim M. Y.; Yoo G. Y.; Yoo W. H.; Choi J. H.; Bae M. O.; Kim J. S.; Kim H. W.; Moon S. H.; Kim J. H.; Han K. T.; Chae C. H.; Kim M. S.; Cho M. H. Four-Week Inhalation Toxicity, Mutagenicity and Immunotoxicity Studies of Keum-Yeon-Cho (NosmoQ), Tobacco Substitute Composition, in Mice. Environ. Toxicol. Pharmacol. 2003, 13 (1), 37–46. 10.1016/S1382-6689(02)00128-X. [DOI] [PubMed] [Google Scholar]
- Abiri R.; Silva A. L. M.; de Mesquita L. S. S.; de Mesquita J. W. C.; Atabaki N.; de Almeida E. B.; Shaharuddin N. A.; Malik S. Towards a Better Understanding of Artemisia vulgaris: Botany, Phytochemistry, Pharmacological and Biotechnological Potential. Food Res. Int. 2018, 109, 403–415. 10.1016/j.foodres.2018.03.072. [DOI] [PubMed] [Google Scholar]
- Barney J. N.; DiTommaso A. The Biology of Canadian Weeds. 118. Artemisia Vulgaris L. Can. J. Plant Sci. 2003, 83, 205–215. 10.4141/P01-098. [DOI] [Google Scholar]
- Zhao B.; Litscher G.; Li J.; Wang L.; Cui Y.; Huang C.; Liu P. Effects of Moxa (Artemisia vulgaris) Smoke Inhalation on Heart Rate and Its Variability. Chin. Med. 2011, 2 (2), 53–57. 10.4236/cm.2011.22010. [DOI] [Google Scholar]
- Malik S.; de Mesquita L. S. S.; Silva C. R.; de Mesquita J. W. C.; de Sá Rocha E.; Bose J.; Abiri R.; de Maria Silva Figueiredo P.; Costa-Júnior L. M. Chemical Profile and Biological Activities of Essential Oil from Artemisia vulgaris L. Cultivated in Brazil. Pharmaceuticals 2019, 12 (2), 49. 10.3390/ph12020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki S.; Oikawa H.; Nakamichi S.; Hirata T.; Yamasaki H.; Yamaguchi Y.; Zhang W.; Nishibe S.; Ogata M.; Fujikawa T. Aroma of Eucommia Leaf Extract (ELE) Causes Reduced Locomotor Activity and Increased NREM Sleep, Acting like the Partially Related Factors of Oral ELE’s Effects with Locomotor-Activity-Dependent-Increase in NREM- and REM-Sleep. Global Drugs Ther. 2017, 3 (2), 5–7. 10.15761/GDT.1000S2001. [DOI] [Google Scholar]
- Chai X.; Wang Y.; Su Y. F.; Bah A. J.; Hu L.; Gao Y.; Gao X. M. A Rapid Ultra Performance Liquid Chromatography–Tandem Mass Spectrometric Method for the Qualitative and Quantitative Analysis of Ten Compounds in Eucommia ulmodies Oliv. J. Pharm. Biomed. Anal. 2012, 57 (1), 52–61. 10.1016/j.jpba.2011.08.023. [DOI] [PubMed] [Google Scholar]
- Malson J. L.; Lee E. M.; Murty R.; Moolchan E. T.; Pickworth W. B. Clove Cigarette Smoking: Biochemical, Physiological, and Subjective Effects. Pharmacol., Biochem. Behav. 2003, 74 (3), 739–745. 10.1016/S0091-3057(02)01076-6. [DOI] [PubMed] [Google Scholar]
- Roemer E.; Dempsey R.; Schorp M. K. Toxicological Assessment of Kretek Cigarettes: Part 1: Background, Assessment Approach, and Summary of Findings. Regul. Toxicol. Pharmacol. 2014, 70 (S1), S2–S14. 10.1016/j.yrtph.2014.11.015. [DOI] [PubMed] [Google Scholar]
- Soldz S.; Huyser D. J.; Dorsey E. Characteristics of Users of Cigars, Bidis, and Kreteks and the Relationship to Cigarette Use. Prev. Med. 2003, 37 (3), 250–258. 10.1016/S0091-7435(03)00121-X. [DOI] [PubMed] [Google Scholar]
- Charpin D.; Orehek J.; Velardocchio J. M. Bronchodilator Effects of Antiasthmatic Cigarette Smoke (Datura stramonium). Thorax 1979, 34 (2), 259–261. 10.1136/thx.34.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaire B. P.; Subedi L. A Review on the Pharmacological and Toxicological Aspects of Datura stramonium L. J. Integr. Med. 2013, 11 (2), 73–79. 10.3736/jintegrmed2013016. [DOI] [PubMed] [Google Scholar]
- Cavanagh H. M. A.; Wilkinson J. M. Lavender Essential Oil: A Review. Aust. Infect. Control 2005, 10 (1), 35–37. 10.1071/HI05035. [DOI] [Google Scholar]
- Salamati A.; Mashouf S.; Mojab F. Effect of Inhalation of Lavender Essential Oil on Vital Signs in Open Heart Surgery ICU. Iran. J. Pharm. Res. 2017, 16 (1), 404–409. [PMC free article] [PubMed] [Google Scholar]
- Morteza-Semnani K.; Saeedi M.; Akbarzadeh M. Chemical Composition and Antimicrobial Activity of the Essential Oil of Verbascum thapsus L. J. Essent. Oil Bear. Plants 2012, 15 (3), 373–379. 10.1080/0972060X.2012.10644063. [DOI] [Google Scholar]
- Moldoveanu S. C.; Coleman W. M.; Kulshreshtha N. P. Evaluation of the Effect of Phytol on the Formation of PAHs in Cigarette Smoke. Beitrage zur Tab. Int. 2010, 24 (1), 10–23. 10.2478/cttr-2013-0876. [DOI] [Google Scholar]
- Chen S.; Dong L.; Quan H.; Zhou X.; Ma J.; Xia W.; Zhou H.; Fu X. A Review of the Ethnobotanical Value, Phytochemistry, Pharmacology, Toxicity and Quality Control of Tussilago farfara L. (Coltsfoot). J. Ethnopharmacol. 2021, 267, 113478. 10.1016/j.jep.2020.113478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freshour J. E.; Odle B.; Rikhye S.; Stewart D. W. Coltsfoot as a Potential Cause of Deep Vein Thrombosis and Pulmonary Embolism in a Patient Also Consuming Kava and Blue Vervain. J. Diet. Suppl. 2012, 9 (3), 149–154. 10.3109/19390211.2012.708391. [DOI] [PubMed] [Google Scholar]
- Sanders M. Inhalation Therapy: An Historical Review. Prim. Care Respir. J. 2007, 16 (2), 71–81. 10.3132/pcrj.2007.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessanges J.-F. A History of Nebulization. J. Aerosol Med. 2004, 14 (1), 65–71. 10.1089/08942680152007918. [DOI] [PubMed] [Google Scholar]
- Talhout R.; van de Nobelen S.; Kienhuis A. S. An Inventory of Methods Suitable to Assess Additive-Induced Characterising Flavours of Tobacco Products. Drug Alcohol Depend. 2016, 161, 9–14. 10.1016/j.drugalcdep.2015.12.019. [DOI] [PubMed] [Google Scholar]
- Krüsemann E. J. Z.; Lasschuijt M. P.; De Graaf C.; De Wijk R. A.; Punter P. H.; Van Tiel L.; Cremers J. W. J. M.; Van De Nobelen S.; Boesveldt S.; Talhout R. Sensory Analysis of Characterising Flavours: Evaluating Tobacco Product Odours Using an Expert Panel. Tob. Control 2019, 28 (2), 152–160. 10.1136/tobaccocontrol-2017-054152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cigarette Product Development: Blending and Processing Know-How; Tobacco Reporter: Raleigh, NC, U.S.A., 2004. [Google Scholar]
- Farag M. A.; Song G. C.; Park Y.-S.; Audrain B.; Lee S.; Ghigo J.-M.; Kloepper J. W.; Ryu C.-M. Biological and Chemical Strategies for Exploring Inter- and Intra-Kingdom Communication Mediated via Bacterial Volatile Signals. Nat. Protoc. 2017, 12 (7), 1359–1377. 10.1038/nprot.2017.023. [DOI] [PubMed] [Google Scholar]
- Krüsemann E. J. Z.; Visser W. F.; Cremers J. W. J. M.; Pennings J. L. A.; Talhout R. Identification of Flavour Additives in Tobacco Products to Develop a Flavour Library. Tob. Control 2018, 27 (1), 105–111. 10.1136/tobaccocontrol-2016-052961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farag M. A.; Elmassry M. M.; El-Ahmady S. H. The Characterization of Flavored Hookahs Aroma Profile and in Response to Heating as Analyzed via Headspace Solid-Phase Microextraction (SPME) and Chemometrics. Sci. Rep. 2018, 8 (1), 17028. 10.1038/s41598-018-35368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issa M. Y.; Mohsen E.; Younis I. Y.; Nofal E. S.; Farag M. A. Volatiles Distribution in Jasmine Flowers Taxa Grown in Egypt and Its Commercial Products as Analyzed via Solid-Phase Microextraction (SPME) Coupled to Chemometrics. Ind. Crops Prod. 2020, 144, 112002. 10.1016/j.indcrop.2019.112002. [DOI] [Google Scholar]
- Farag M. A.; Otify A. M.; El-Sayed A. M.; Michel C. G.; ElShebiney S. A.; Ehrlich A.; Wessjohann L. A. Sensory Metabolite Profiling in a Date Pit Based Coffee Substitute and in Response to Roasting as Analyzed via Mass Spectrometry Based Metabolomics. Molecules 2019, 24 (18), 3377. 10.3390/molecules24183377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalil M. N. A.; Fekry M. I.; Farag M. A. Metabolome Based Volatiles Profiling in 13 Date Palm Fruit Varieties from Egypt via SPME GC–MS and Chemometrics. Food Chem. 2017, 217, 171–181. 10.1016/j.foodchem.2016.08.089. [DOI] [PubMed] [Google Scholar]
- Ram A.; Balachandar S.; Vijayananth P.; Singh V. P. Medicinal Plants Useful for Treating Chronic Obstructive Pulmonary Disease (COPD): Current Status and Future Perspectives. Fitoterapia 2011, 82 (2), 141–151. 10.1016/j.fitote.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Noriyasu A.; Konishi T.; Mochizuki S.; Sakurai K.; Tanaike Y.; Matsuyama K.; Uezu K.; Kawano T. Menthol-Enhanced Cytotoxicity of Cigarette Smoke Demonstrated in Two Bioassay Models. Tob. Induced Dis. 2013, 11 (1), 18. 10.1186/1617-9625-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler M. J.; Coppock B.; Chen C. Does the Burning of Moxa (Artemisia vulgaris) in Traditional Chinese Medicine Constitute a Health Hazard?. Acupunct. Med. 2009, 27 (1), 16–20. 10.1136/aim.2009.000422. [DOI] [PubMed] [Google Scholar]
- Stepanov I.; Feuer R.; Jensen J.; Hatsukami D.; Hecht S. S. Mass Spectrometric Quantitation of Nicotine, Cotinine, and 4-(Methylnitrosamino)-1-(3-Pyridyl)-1-Butanol in Human Toenails. Cancer Epidemiol. Biomarkers Prev. 2006, 15 (12), 2378–2383. 10.1158/1055-9965.EPI-06-0265. [DOI] [PubMed] [Google Scholar]
- Stepanov I.; Hecht S. S.; Lindgren B.; Jacob P.; Wilson M.; Benowitz N. L. Relationship of Human Toenail Nicotine, Cotinine, and 4-(Methylnitrosamino) −1-(3-Pyridyl)-1-Butanol to Levels of These Biomarkers in Plasma and Urine. Cancer Epidemiol. Biomarkers Prev. 2007, 16 (7), 1382–1386. 10.1158/1055-9965.EPI-07-0145. [DOI] [PubMed] [Google Scholar]