Abstract
Background
Intravenous calcium channel blockers or beta-blockers are the preferred rate control medications for hemodynamically stable patients with atrial fibrillation with rapid ventricular rate (AF-RVR) in the emergency department.
Objectives
To compare the efficacy of intravenous diltiazem and metoprolol for rate control and safety with respect to development of hypotension and bradycardia in patients with AF-RVR.
Methods
For this systematic review and meta-analysis, we searched PubMed, Embase, Cochrane databases, and the clinicaltrials.gov registry between database inception and 30th May 2021. Articles were included if they compared efficacy and safety of diltiazem versus metoprolol in critically ill adult patients hospitalized with AF-RVR. Outcome measures were achievement of rate control, development of new hypotension, and bradycardia after drug administration.
Results
Of 86 records identified, 14 were eligible, all of which had a low to moderate risk of overall bias. The meta-analysis (Mantel-Haenszel, random-effects model) showed that diltiazem use was associated with increased achievement of rate control target compared to metoprolol [14 studies, n = 1732, Odds Ratio (OR): 1.92; 95% Confidence Intervals (CI):1.26 to 2.90; I2 = 61%]. In the pooled analysis, no differences were seen in hypotension using diltiazem vs metoprolol [12 studies, n = 1477, OR: 0.96; 95% CI:0.61 to 1.52; I2 = 35%] or bradycardia [9 studies, n = 1203, OR: 2.44; 95% CI: 0.82 to 7.31; I2 = 48%].
Conclusions
Intravenous diltiazem is associated with increased achievement of rate control target in patients with AF-RVR compared to metoprolol, while both medications are associated with similar incidence of hypotension and bradycardia.
Keywords: Atrial fibrillation, Rapid ventricular rate, Diltiazem, Metoprolol, Rate control
1. Introduction
Atrial fibrillation (AF) is the most common arrhythmia leading to emergency department (ED) visits. Consensus guidelines suggest that most patients with AF can be safely managed in the emergency department without the need for hospital admission.1 For emergency patients with Atrial Fibrillation (AF) with Rapid Ventricular Rate (RVR), a strategy of either rate control or rhythm control could be selected based on multiple factors including the duration of AF and hemodynamic stability. When the duration of AF is > 48 h or uncertain, ventricular rate control with non-dihydropyridine calcium channel blockers or beta-blockers is the preferred initial strategy for hemodynamically stable patients. Intravenous diltiazem and metoprolol are commonly used to achieve rate control in patients with atrial fibrillation with rapid ventricular rate. No comprehensive review is available of the evidence regarding the impact of the choice of diltiazem compared to metoprolol on the achievement of desired rate control target and hemodynamic adverse events with the use of these medications in the emergency department. The current review was undertaken to inform emergency physicians on the choice of medication for rate control in patients with atrial fibrillation with rapid ventricular rate presenting to the emergency department based on the available evidence. The purpose of this review was to assess whether there was an association between the use of intravenous diltiazem versus metoprolol for rate control in AF with RVR patients, with successful rate control and hemodynamic adverse events, in particular, hypotension and bradycardia.
2. Objectives
The primary objective of this systematic review and meta-analysis was to compare the efficacy of intravenous diltiazem and metoprolol for rate control in patients with atrial fibrillation with rapid ventricular rate. The secondary objective was to evaluate the safety of intravenous diltiazem and metoprolol in patients with atrial fibrillation with rapid ventricular rate, with respect to the development of new hypotension and bradycardia after administration of these medications.
3. Methods
ELIGIBILITY CRITERIA- Articles were included if they compared efficacy and safety of intravenous diltiazem versus metoprolol in adult (age ≥18 years) patients with atrial fibrillation with rapid ventricular rate in the emergency department or intensive care unit. To be included, the study had to use a defined clinical outcome relating to efficacy (achievement of rate control target) and safety (hypotension or bradycardia occurring as an adverse event) of the two medications. Our primary outcome measure was the achievement of ventricular rate control <110/min in patients hospitalized with atrial fibrillation with rapid ventricular rate, and secondary outcomes were development of new hypotension (systolic blood pressure <90 mm Hg) and bradycardia (heart rate <60/min) after administration of intravenous diltiazem or metoprolol. There were no restrictions on study design. Articles were excluded if they studied oral medications for chronic rate control in outpatients with atrial fibrillation. We also excluded articles, if they studied management of atrial fibrillation in patients with pre-excitation syndromes.
4. Information sources
One investigator (SCS) designed and conducted a comprehensive search of the following electronic databases and trial registers- PubMed, Embase, Cochrane, and clincaltrials.gov up to and including 30th May 2021. The strategies used a combination of controlled vocabulary as follows: (a) Medical Subject Headings in PubMed-((atrial fibrillation[MeSH Terms]) AND (diltiazem[MeSH Terms])) AND (metoprolol[MeSH Terms]); (b) Embase- 'atrial fibrillation'/exp/mj AND 'diltiazem'/exp/mj AND 'metoprolol'/exp/mj; (c) Cochrane-atrial fibrillation in Title Abstract Keyword AND diltiazem in Title Abstract Keyword AND metoprolol in Title Abstract Keyword; (d) clinicaltrials.gov-diltiazem metoprolol | Completed Studies | Atrial Fibrillation. No language restrictions were applied and all studies indexed in the databases since their inception were included. We also identified additional studies by searching the reference lists of publications eligible for full-text review. In phase 1, the investigators (SCS and MSB), screened all titles and abstracts for eligibility. Records considered potentially relevant were assessed in full text for eligibility in phase 2 (SCS and MSB).
5. Data analysis
Pertinent data were extracted-citation details; the study site (Emergency Department or Intensive Care Unit); retrospective or prospective study; observational or interventional study; treatment assignment mechanism; details of the intervention; and outcomes of interest. One investigator (SCS) entered the data into Review Manager program. Another investigator (MSB) checked this for accuracy. We assessed the risk of bias in the following specific domains: (a) bias arising from the randomization process; (b) bias due to blinding of participants and personnel; (c) bias due to blinding of outcome assessment; (d) bias due to missing outcome data; and (e) bias due to selective reporting of the results.2 The quality of evidence was evaluated with the Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence document and graded from Level 1 (High Quality) to Level 5 (Low Quality).3
Eligible outcomes were achievement of rate control target and development of new hypotension and bradycardia after administration of intravenous diltiazem or metoprolol. The primary efficacy endpoint of achievement of rate control target was defined as ventricular rate <110/min within 6 h of intravenous administration of diltiazem or metoprolol. Where multiple outcomes were reported, we selected one outcome for inclusion in the analysis, choosing the result that provided the most relevant information (e.g., sustained rate control at 2 h was prioritized over rate control at 5min). With respect to safety endpoints, hypotension was defined as SBP <90 mm Hg, and bradycardia as heart rate <60/min within 6 h after the administration of rate control drugs.
We considered it reasonable to pool the data from Emergency Department and Intensive Care Unit studies to have a better understanding of the comparative outcomes with the use of diltiazem and metoprolol in patients with atrial fibrillation with rapid ventricular rate in emergency settings. We used Review Manager (RevMan- Computer program, Version 5.4, The Cochrane Collaboration, 2020) for meta-analyses. Dichotomous outcomes were assessed for odds ratio (OR) with 95% confidence intervals (CI) using Mantel-Haenszel (M−H) random-effects model to account for the clinical and statistical heterogeneity between studies. P-value < 0.05 indicated statistical significance. The heterogeneity was assessed by visual inspection of Forest Plots, and statistical tests for heterogeneity variance (τ2) and inconsistency (I2). Heterogeneity was deemed significant if I2 > 50%.
6. Results
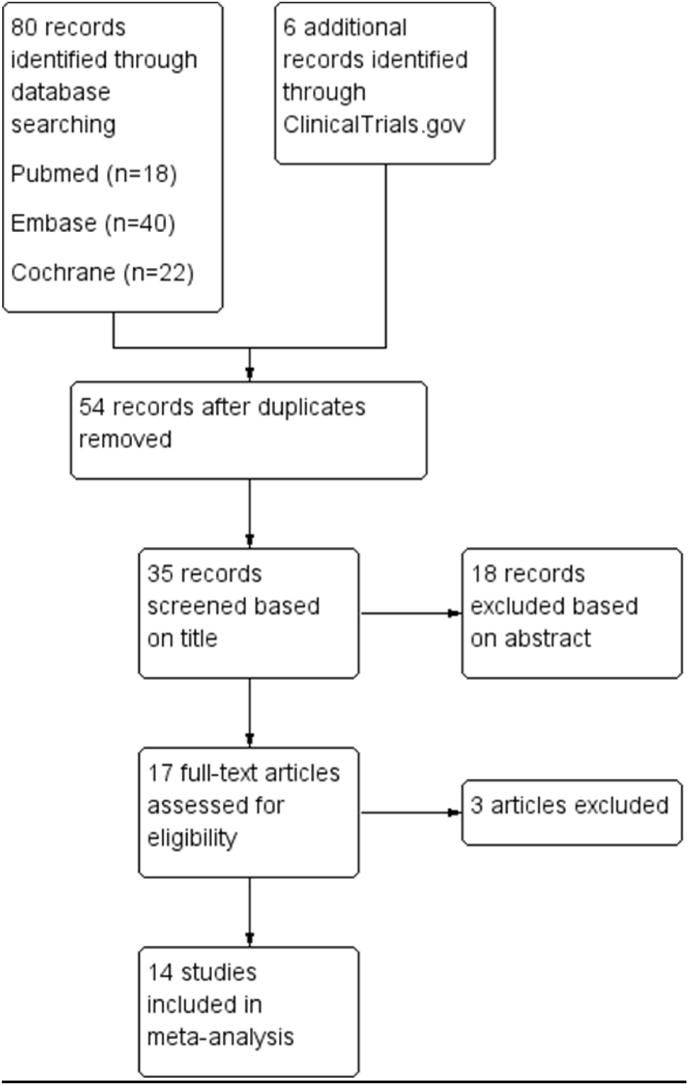
We found 86 records in database and trial registry search (Fig. 1). After duplicate removal and screening titles, we screened abstracts of 35 records, from which we selected 17 studies for full-text review, and finally included 14 studies (Table 1). Details of inclusion criteria, exclusion criteria, doses of diltiazem and metoprolol, and outcome definitions for rate control, hypotension and bradycardia in the included studies are provided in Supplement 1 (Table 2). We collected the outcome data from eleven retrospective studies and three randomized controlled trials. All fourteen studies contained outcome data for achievement of rate control target with diltiazem compared to metoprolol in patients with atrial fibrillation with rapid ventricular rate, twelve studies contained data for the development of new hypotension as an adverse event with diltiazem versus metoprolol, and nine studies contained data for bradycardia as an adverse event. With respect to our primary efficacy endpoint of achievement of rate control target, three of the fourteen included studies- Demircan 2005, Katchi 2014, and Nicholson 2020 defined the efficacy outcome as either ventricular rate control or conversion to sinus rhythm after administration of intravenous diltiazem or metoprolol. We excluded three studies from our review- Lopez 20204, Chen 20165, and Moskowitz 2017.6 For Lopez 2020, only the research abstract could be accessed, and complete outcome data were unavailable. We excluded Chen 2016 (Conference Poster Contribution) and Moskowitz 2017, because, in these studies, outcome measures of rate control, hypotension and bradycardia were not assessed and reported.
Fig. 1.
Systematic database search flow diagram.
Table 1.
Characteristics of included studies.
| Interventions | Outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author (year) | Study design | Country | Sample size | Source of participants | Diltiazem | Metoprolol | Rate Control | Hypotension | Bradycardia | Level of Evidencea |
| Demir 2021(7) | Retrospective Comparative | Turkey | 50 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Demircan 2005(8) | Randomized Controlled Trial | Turkey | 40 | Emergency Department | ✓ | ✓ | ✓ | ✓ | X | 2 |
| Feeney 2018(9) | Retrospective Comparative | USA | 332 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Fromm 2015(10) | Randomized Controlled Trial | USA | 54 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 2 |
| Hargrove 2021(11) | Retrospective Comparative | USA | 51 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Hines 2016(12) | Retrospective Comparative | USA | 100 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Hirschy 2019(13) | Retrospective Comparative | USA | 48 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Katchi 2014(14) | Retrospective Comparative | USA | 173 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| McGrath 2020(15) | Retrospective Comparative | USA | 349 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Medeiros 2021(16) | Retrospective Comparative | USA | 78 | Emergency Department | ✓ | ✓ | ✓ | ✓ | ✓ | 3 |
| Memis 2018(17) | Randomized Controlled Trial | Turkey | 100 | Emergency Department | ✓ | ✓ | ✓ | X | X | 2 |
| Nicholson 2020(18) | Retrospective Comparative | USA | 108 | Emergency Department | ✓ | ✓ | ✓ | ✓ | X | 3 |
| Nunez Cruz 2020(19) | Retrospective Comparative | USA | 160 | Emergency Department | ✓ | ✓ | ✓ | X | X | 3 |
| Personett 2014(20) | Retrospective Comparative | USA | 121 | Postoperative patients (Intensive Care Unit) | ✓ | ✓ | ✓ | ✓ | X | 3 |
Evaluated according to Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence Document with levels from 1 (High) to 5(Low).3
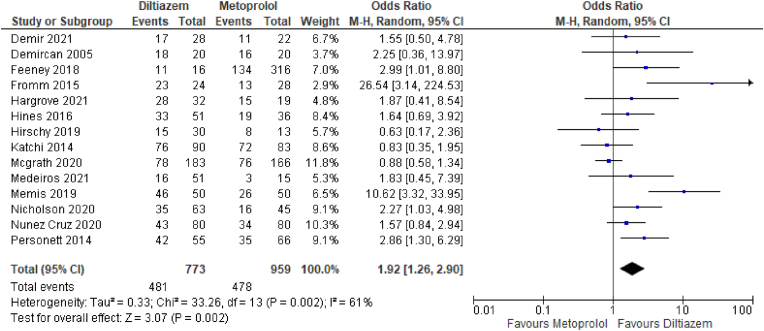
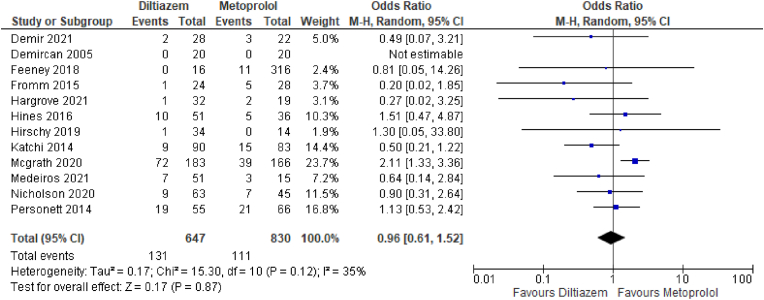
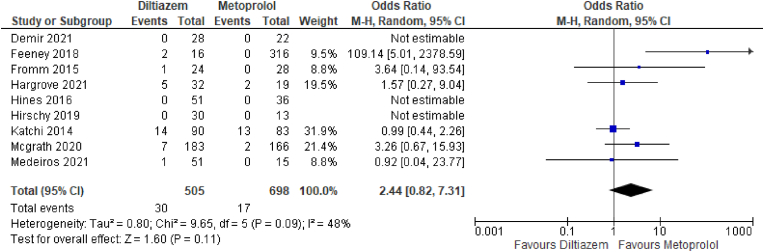
Fourteen studies, including eleven retrospective studies and three randomized controlled trials (RCTs), directly compared the achievement of rate control target between diltiazem and metoprolol groups (Fig. 2).7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 These studies enrolled 1732 patients in emergency departments (thirteen studies) and intensive care unit settings (one study). These fourteen studies were pooled, as they each reported achievement of rate control target with diltiazem (n = 773) compared to metoprolol (n = 959) in patients with atrial fibrillation with rapid ventricular rate. Patients treated with intravenous diltiazem had significantly greater achievement of rate control target compared to patients treated with intravenous metoprolol (odds ratio: 1.92; 95% CI: 1.26 to 2.90; p = 0.002); with significant heterogeneity (I2 = 61%). Twelve studies, including 1477 patients, reported the rate of hypotension as an adverse event with diltiazem versus metoprolol (Fig. 3).7, 8, 9, 10, 11, 12, 13, 14, 15, 16,18,20 Meta-analysis of outcomes of these twelve studies showed no significant difference in the occurrence of hypotension as an adverse event with diltiazem (n = 647) vs. metoprolol (n = 830) in patients with atrial fibrillation with rapid ventricular rate (odds ratio: 0.96; 95% CI: 0.61 to 1.52; p = 0.87); without significant heterogeneity (I2 = 35%). Nine studies, including 1203 patients, reported the rate of bradycardia as an adverse event with diltiazem versus metoprolol (Fig. 4).7,9, 10, 11, 12, 13, 14, 15, 16 Meta-analysis of outcomes of these nine studies did not show a significant difference in the occurrence of bradycardia as an adverse event with intravenous diltiazem (n = 505) vs. metoprolol (n = 698) in patients with atrial fibrillation with rapid ventricular rate (odds ratio: 2.44; 95% CI: 0.82 to 7.31; p = 0.11); without significant heterogeneity (I2 = 48%). A summary of the risk of bias assessments is provided in Fig. 5. Regarding the overall risk of bias, there were concerns about a low to moderate risk of bias for all the included studies, but none of these were assessed as having a high risk of bias.
Fig. 2.
Forest plot of Rate Control Success with Diltiazem (n = 773) vs. Metoprolol (n = 959) in patients with Atrial Fibrillation with Rapid Ventricular Rate.
Fig. 3.
Forest plot of Hypotension as an adverse event with Diltiazem (n = 647) vs. Metoprolol (n = 830) in patients with Atrial Fibrillation with Rapid Ventricular Rate.
Fig. 4.
Forest plot of Bradycardia as an adverse event with the use of Diltiazem (n = 505) vs. Metoprolol (n = 698) in patients with Atrial Fibrillation with Rapid Ventricular Rate.
Fig. 5.
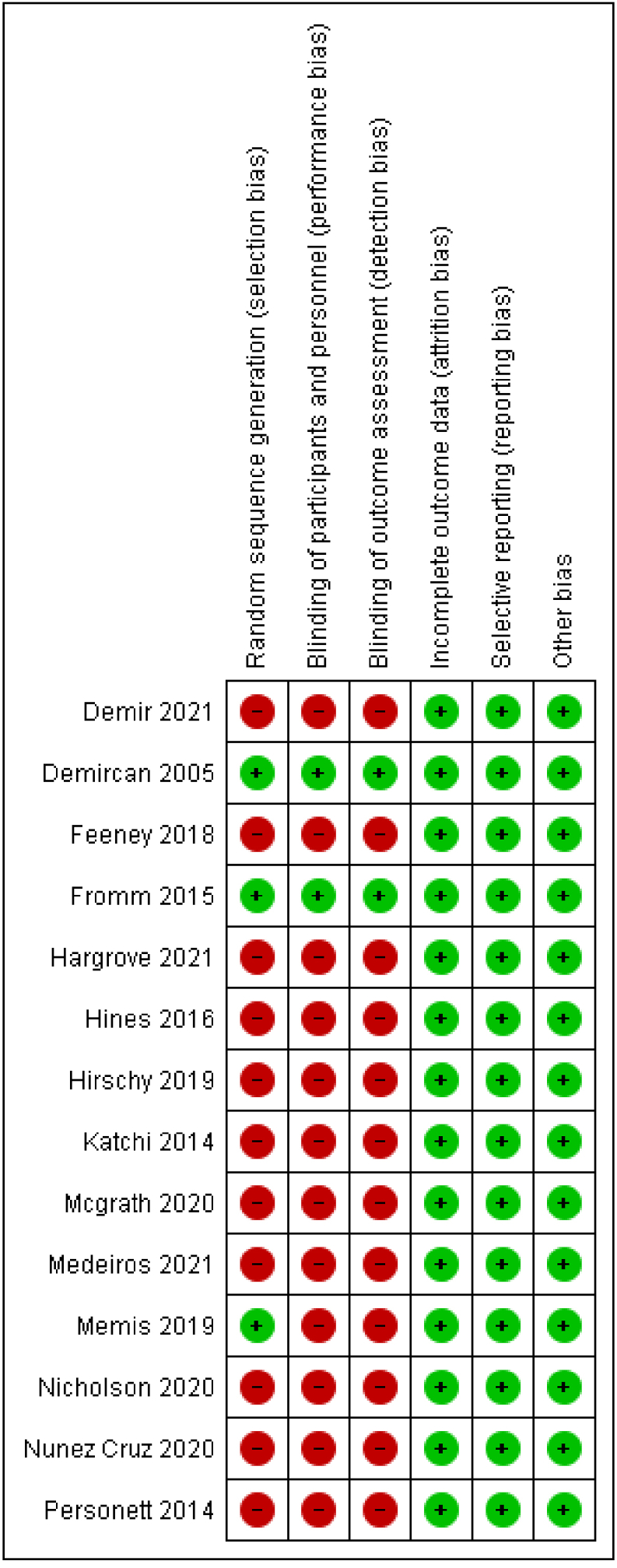
Risk of bias summary for included studies.
Subgroup analysis of studies from emergency departments (excluding studies from intensive care unit) included thirteen studies (n = 1611) for the primary outcome of achievement of rate control target with diltiazem compared to metoprolol (Supplement 2). In the subgroup of emergency department patients, diltiazem use was associated with increased achievement of rate control compared to metoprolol (odds ratio: 1.85; 95% CI: 1.19 to 2.87; p = 0.006). Similarly, the single study focused on intensive care unit (ICU) patients showed increased rate control with diltiazem (n = 55) compared to metoprolol (n = 66) (odds ratio: 2.86; 95% CI: 1.30 to 6.29; p = 0.009).
Sensitivity analysis was undertaken for the primary outcome of successful rate control, by including only the three randomized controlled trials comparing diltiazem and metoprolol for atrial fibrillation with rapid ventricular rate (Supplement 3). The results were consistent with the primary meta-analysis, with intravenous diltiazem being associated with increased achievement of rate control target compared to metoprolol (odds ratio: 8.38; 95% CI: 2.46 to 28.52; p = 0.0007).
7. Discussion
The aim of rate control in atrial fibrillation with rapid ventricular response is to reduce symptoms, improve hemodynamics, prevent heart failure and reduce the risk of adverse cardiovascular outcomes.21 In patients presenting to the emergency department with atrial fibrillation with rapid ventricular response, who are symptomatic but not unstable, initial therapy usually involves rate control with intravenous calcium-channel blockers or beta-blockers. Beta-blockers act by blocking sympathetic activity in the atrioventricular node to slow ventricular rate. Non-dihydropyridine calcium-channel antagonists, such as verapamil and diltiazem, slow atrioventricular node conduction by blocking calcium channels, thereby increasing the refractory period of the atrioventricular node. They are often used as the first-line rate-controlling agents. Intravenous metoprolol is administered as a bolus of 2.5–5.0 mg over 2 min; and may be repeated up to 3 doses.22 Intravenous diltiazem is given at a dose of 0.25 mg/kg over 2 min. A second bolus may be given after 15 min if the heart rate continues to be more than 100 beats per minute, followed by an infusion at the rate of 5–15 mg/h. This systematic review and meta-analysis compared the safety and efficacy of the first-line intravenous rate control medications diltiazem and metoprolol with respect to the achievement of rate control target and adverse events, i.e., hypotension and bradycardia. The certainty of evidence from this meta-analysis is considered moderate, because of concerns for bias due to the largely observational nature of included studies.23 The results of this meta-analysis favor intravenous diltiazem for significantly better achievement of rate control target compared to intravenous metoprolol in patients with atrial fibrillation with rapid ventricular rate in emergency settings. This is especially important because suboptimal rate control is associated with increased cardiovascular adverse events.24 However, the result came with significant heterogeneity between the studies. This was primarily due to the results of Hirschy 2019 and Katchi 2014, which showed no significant difference in the achievement of the rate control target between the two groups. Hirschy 2019 studied the effects of diltiazem versus metoprolol in atrial fibrillation with rapid ventricular response in patients with heart failure with reduced ejection fraction (HFrEF), and Katchi 2014 focused on patients with acute decompensated heart failure (ADHF), conditions where the use of non-dihydropyridine calcium channel blockers is not recommended by American College of Cardiology/American Heart Association/Heart Rhythm Society practice guidelines.22 In patients with a previous history of atrial fibrillation who present to the emergency department with AF-RVR, physicians often favour the intravenous formulation of the patient's oral home rate control medication, which may not be ideal for ventricular rate control in emergency settings.9,11 Another important consideration is the development of new hypotension and bradycardia after administration of intravenous rate control medications. This meta-analysis showed no significant difference in the incidence of adverse events (hypotension and bradycardia) with the use of intravenous diltiazem and metoprolol for rate control. This result suggests a similar safety profile for both medications for use in patients with atrial fibrillation with rapid ventricular rate. Jafri et al conducted a systematic review and meta-analysis of three studies on paroxysmal atrial fibrillation and found that the mean reduction in heart rate was greater at 5, 10, and 15 min in the group of patients treated with intravenous diltiazem compared to metoprolol, with no significant differences in systolic blood pressures between the two groups.25 A recent systematic review and meta-analysis by Lan et al also found greater efficacy of intravenous diltiazem compared to metoprolol for rate control at 30 min in atrial fibrillation with rapid ventricular rate, and no significant difference in adverse events.26 These findings are consistent with the results of the present meta-analysis, and provide important evidence for selecting intravenous diltiazem as the preferred medication for rate control in atrial fibrillation with rapid ventricular rate in the emergency department.
8. Limitations
The studies included predominantly retrospective studies and only three randomized controlled trials. The included studies were often limited by selection bias, small sample sizes, and lack of blinding of personnel and outcome assessment. Functional outcomes, such as 30-day mortality, readmission rates, and worsening heart failure, were not assessed in the present meta-analysis. We did not evaluate the association of comorbidities, such as coronary artery disease, hypertension, diabetes mellitus, obesity, prior stroke or transient ischemic attack, asthma or chronic obstructive pulmonary disease, infections, kidney disease and peripheral vascular disease, with achievement of rate control target and adverse effects with diltiazem and metoprolol use. In addition, the results are not applicable to patients with pre-excitation syndromes as they were excluded from the meta-analysis.
9. Conclusions
Findings from the meta-analysis suggest that the use of intravenous diltiazem is associated with increased achievement of rate control target in patients with atrial fibrillation with rapid ventricular response compared with metoprolol, while both medications are associated with similar incidence of hypotension and bradycardia. These results favour the selection of diltiazem as the preferred agent over metoprolol for rate control in emergency settings. However, our understanding of the impact of choice of rate control medication for atrial fibrillation with rapid ventricular response in the emergency department would further benefit from future high-quality blinded randomized controlled trials that make direct comparisons within subgroups with heart failure with preserved ejection fraction and heart failure with reduced ejection fraction.
Funding
None.
Author contribution
SCS conceived and designed the study. SCS and MSB searched and reviewed the articles for eligibility and extracted the data. SCS performed the statistical analysis and drafted the manuscript, and MSB contributed significantly to its revision. All authors agree to take responsibility for the paper as a whole.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2022.10.195.
Contributor Information
Saurabh C. Sharda, Email: saurabhcsharda@gmail.com.
Mandip S. Bhatia, Email: drmandip@yahoo.co.in.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Stiell I.G., Macle L., CCS Atrial Fibrillation Guidelines Committee Canadian Cardiovascular Society atrial fibrillation guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011 Feb;27(1):38–46. doi: 10.1016/j.cjca.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 2.Higgins J.P., Savovic J., Page M.J., Sterne J.A. 2019 Aug 22. Revised Cochrane Risk-Of-Bias Tool for Randomized Trials (RoB 2)https://www.riskofbias.info/welcome/rob-2-0-tool/current-version-of-rob-2 [cited 2021 Jun 1]; Available from: [Google Scholar]
- 3.OCEBM Levels of Evidence Working Group The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine [Internet] https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence [cited 2021 Jun 1]; Available from:
- 4.Lopez B., Maloney R. Evaluation of metoprolol versus diltiazem for treatment of atrial fibrillation in critical care unit. Crit Care Med. 2020 Jan;48(1):121. [Google Scholar]
- 5.Wei Chen Ching, Daniele Massera, Chino Aneke, Pina Ileana. Intravenous diltiazem, as compared to intravenous metoprolol, for atrial fibrillation/flutter is associated with increased admission from the emergency department. J Am Coll Cardiol. 2016 Apr 5;67(13_suppl ment) 786–786. [Google Scholar]
- 6.Moskowitz A., Chen K.P., Cooper A.Z., Chahin A., Ghassemi M.M., Celi L.A. Management of atrial fibrillation with rapid ventricular response in the intensive care unit: a secondary analysis of electronic health record data. Shock. 2017 Oct;48(4):436–440. doi: 10.1097/SHK.0000000000000869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DemiR M.C., Doğan M., Polat E., AkpiNar G. 2021 Feb 16. Intravenous Diltiazem or Metoprolol Administration in the Emergency Department for Acute Rate Control of Atrial Fibrillation Patients with Rapid Ventricular Response with Unknown Ejection Fraction. Düzce Tıp Fakültesi Derg [Internet]https://dergipark.org.tr/en/doi/10.18678/dtfd.839698 [cited 2021 Jul 6]; Available from: [Google Scholar]
- 8.Demircan C. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005 Jun 1;22(6):411–414. doi: 10.1136/emj.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feeney M.E., Rowe S.L.B., Mah N.D., Barton C.A., Ran R. Achieving ventricular rate control in patients taking chronic beta-blocker therapy. Am J Emerg Med. 2018 Jan;36(1):110–113. doi: 10.1016/j.ajem.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Fromm C., Suau S.J., Cohen V., et al. Diltiazem vs. Metoprolol in the management of atrial fibrillation or flutter with rapid ventricular rate in the emergency department. J Emerg Med. 2015 Aug;49(2):175–182. doi: 10.1016/j.jemermed.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Hargrove K.L., Robinson E.E., Lusk K.A., Hughes D.W., Neff L.A., Fowler A.L. Comparison of sustained rate control in atrial fibrillation with rapid ventricular rate: metoprolol vs. Diltiazem. Am J Emerg Med. 2021 Feb;40:15–19. doi: 10.1016/j.ajem.2020.11.073. [DOI] [PubMed] [Google Scholar]
- 12.Hines M.C., Reed B.N., Ivaturi V., Bontempo L.J., Bond M.C., Hayes B.D. Diltiazem versus metoprolol for rate control in atrial fibrillation with rapid ventricular response in the emergency department. Am J Health Syst Pharm. 2016 Dec 15;73(24):2068–2076. doi: 10.2146/ajhp160126. [DOI] [PubMed] [Google Scholar]
- 13.Hirschy R., Ackerbauer K.A., Peksa G.D., O'Donnell E.P., DeMott J.M. Metoprolol vs. diltiazem in the acute management of atrial fibrillation in patients with heart failure with reduced ejection fraction. Am J Emerg Med. 2019 Jan;37(1):80–84. doi: 10.1016/j.ajem.2018.04.062. [DOI] [PubMed] [Google Scholar]
- 14.Katchi F., Nagabandi S., Shuster J., Novak E., Joseph S. Treating rapid atrial fibrillation in acute decompensated heart failure: metoprolol and diltiazem are equally safe, yet metoprolol increases conversion to sinus rhythm. J Card Fail. 2014 Aug;20(8):S41. [Google Scholar]
- 15.McGrath P., Kersten B., Chilbert M.R., Rusch C., Nadler M. Evaluation of metoprolol versus diltiazem for rate control of atrial fibrillation in the emergency department. Am J Emerg Med. 2020 Nov doi: 10.1016/j.ajem.2020.11.039. [DOI] [PubMed] [Google Scholar]
- 16.Medeiros T., Bui V., Almekdash M.H., Keesari R., Lee Y.R. Rate control with intravenous diltiazem, verapamil, and metoprolol in acute atrial fibrillation with rapid ventricular rate. SAGE Open Med. 2021 Jan;vol. 9 doi: 10.1177/20503121211017756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Memiş M.B., Ak R., Cimilli Öztürk T., Onur Ö., Ordu Ö. Which one is the first choice for rapid ventricular rate atrial fibrillation in emergency department: metoprolol or Diltiazem? A randomized clinical trial. J Surg Med. 2018 Aug 11 https://dergipark.org.tr/en/doi/10.28982/josam.443209 Available from: [Google Scholar]
- 18.Nicholson J., Czosnowski Q., Flack T., Pang P.S., Billups K. Hemodynamic comparison of intravenous push diltiazem versus metoprolol for atrial fibrillation rate control. Am J Emerg Med. 2020 Sep;38(9):1879–1883. doi: 10.1016/j.ajem.2020.06.034. [DOI] [PubMed] [Google Scholar]
- 19.Nuñez Cruz S., DeMott J.M., Peksa G.D., Slocum G.W. Evaluation of the blood pressure effects of diltiazem versus metoprolol in the acute treatment of atrial fibrillation with rapid ventricular rate. Am J Emerg Med. 2020 Oct doi: 10.1016/j.ajem.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Personett H.A., Smoot D.L., Stollings J.L., Sawyer M., Oyen L.J. Intravenous metoprolol versus diltiazem for rate control in noncardiac, nonthoracic postoperative atrial fibrillation. Ann Pharmacother. 2014 Mar;48(3):314–319. doi: 10.1177/1060028013512473. [DOI] [PubMed] [Google Scholar]
- 21.Low B., Shah M., Nassour V., Fox K. Acute management of atrial fibrillation with rapid ventricular response. Br J Hosp Med Lond Engl. 2019 Jun 2;80(6):C82–C85. doi: 10.12968/hmed.2019.80.6.C82. 2005. [DOI] [PubMed] [Google Scholar]
- 22.January C.T., Wann L.S., Alpert J.S., et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 2;130(23):2071–2104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 23.Granholm A., Alhazzani W., Møller M.H. Use of the GRADE approach in systematic reviews and guidelines. Br J Anaesth. 2019 Nov 1;123(5):554–559. doi: 10.1016/j.bja.2019.08.015. [DOI] [PubMed] [Google Scholar]
- 24.Wong B.M., Green M.S., Stiell I.G. Rate control management of atrial fibrillation with rapid ventricular response in the emergency department. Can J Cardiol. 2020 Apr;36(4):509–517. doi: 10.1016/j.cjca.2019.08.040. [DOI] [PubMed] [Google Scholar]
- 25.Jafri S.H., Xu J., Warsi I., Cerecedo-Lopez C.D. Diltiazem versus metoprolol for the management of atrial fibrillation: a systematic review and meta-analysis. Am J Emerg Med. 2021 Oct;48:323–327. doi: 10.1016/j.ajem.2021.06.053. [DOI] [PubMed] [Google Scholar]
- 26.Lan Q., Wu F., Han B., Ma L., Han J., Yao Y. Intravenous diltiazem versus metoprolol for atrial fibrillation with rapid ventricular rate: a meta-analysis. Am J Emerg Med. 2022 Jan;51:248–256. doi: 10.1016/j.ajem.2021.08.082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.