Abstract
Background
The aim of the present review was to identify the effect of the post-space preparation (PSP) timing (immediate or delayed) on endodontically treated teeth.
Methods
All studies in any language that compared the effect of immediate versus delayed PSP on the outcomes of an endodontically treated tooth were searched in PubMed, Scopus, Web of Science, Cochrane, ProQuest, WorldCat, and Google Scholar databases by two independent researchers until February 12, 2022. Studies assessing merely the immediate or delayed PSP were excluded. A descriptive analysis was performed to evaluate the study design and the characteristics of the included studies.
Results
The initial search yielded 2612 records, of which 68 were included. Except for one randomized controlled trial, all were in vitro. The evaluated variables were apical/coronal microleakage (n = 48/n = 1), post-bond strength (n = 8), bacterial infiltration (n = 7), presence of voids (n = 3), apical extrusion and residual of filling material (n = 1), and post-operative pain (n = 1). The number of publications had steady growth per year and fast growth per decade. "Post-space preparation" was the most popular keywords.
Conclusions
The present review highlights the need for further investigations due to the various design of studies, controversial results, and an inadequate number of randomized controlled trials.
Trial registration
Retrospectively registered. Open Science (10.17605/OSF.IO/2YTM6).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-022-02564-w.
Keywords: Post-space preparation, Immediate, Delayed, Leakage
Introduction
Endodontically treated teeth have undergone extensive loss of coronal structure and lack an adequate support for a permanent restoration. In these cases, additional retention from the root canal may be required [1]. Thus, these teeth may need core retention through intracanal post placement [2, 3]. Despite a paradigm shift in dentistry in the last decades regarding replacing the conventional mechanically retained restorations with modern methods which depend on adhesion, these conventional methods of restoring teeth, have been supported by long-term studies as treatment options for restoring endodontically treated teeth because of their good reliability and predictability [4]. Post-space may be prepared by hot pluggers instantly after pulp space obturation or by rotary instruments after sealer setting, categorized as immediate or delayed, respectively [5–7].
During the post space preparation (PSP), the root canal filling material may be twisted, vibrated, or dislocated, consequently creating voids [8]. Several factors, including apical integrity, the remaining amount of root canal filling materials, the obturation techniques, the gutta-percha removal techniques, sealer type, and preparation time, may affect the integrity of root canal filling materials and cause microleakage and bacterial infiltration [2, 5, 6]. Thus, it is essential not to deteriorate the integrity of the residual filling material to provide an appropriate apical sealing and to avoid re-infection or re-colonization of bacteria [5, 6].
It is recommended that the same clinician who has performed the endodontic treatment perform PSP with a rubber dam to avoid contamination [9]. The immediate PSP allows the prepared root canal to receive the post in a unique session and to, assess the condensation of the remaining gutta-percha, and if necessary, some modifications can be considered. However there are disagreements regarding the time interval between the root canal filling and the PSP [7]. The time of PSP may influence some outcomes in endodontically treated teeth such as void formation [10], displacement of filling material [9], the bond strength of the post [5], and post-operative pain [11]. Nevertheless, there are no consensus on the post-operative pain induced by post-endodontic restorations after single- or two-visit root canal treatments [11].
Owing to controversial reports regarding the effect of the interval between root canal treatment and PSP on the outcome of the endodontically treated tooth, it is necessary to identify the existing reports and evaluate the quality of evidence by performing a comprehensive review. Therefore, based on the heterogeneous set of data, this scoping review was conducted to map the research done in this area and to evaluate the outcomes related to immediate or delayed PSP in endodontically treated teeth.
Materials and Methods
Protocol and scope of review
The protocol of this study was based on the framework proposed by Peters et al. [12] according to the Joana Briggs Institute. It is available at https://osf.io/yc9nb/. In addition, this scoping review was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) Checklist (Online Resource 1, Table S1). This review focused on the following evidence-based practice: What is the best time for PSP after endodontic treatment?
Eligibility criteria
Studies that considered the effect of PSP time on endodontically treated teeth were selected. This included experimental studies (in vivo or in vitro), case reports, case series, clinical studies, or systematic reviews that compared the effects of immediate and delayed PSP on endodontically treated teeth. Literature reviews, book sections, congress papers, commentaries, methodological approaches, opinion or hypothesis articles, and editorial letters were excluded.
Information source and search strategy
An electronic search without date or language restriction was conducted on Medline (PubMed), Scopus, Web of Science and Cochrane databases from their date of inception to February 12, 2022, using the keywords ((((post OR dowel OR fiber post OR intracanal post OR intraradicular post) AND (space AND prepar*)) AND (time OR timing OR immediate* OR early OR late OR delay*))), where asterisk symbol was used for truncation. Grey literature was also searched through ProQuest, WorldCat, and Google Scholar (first 100 hits). Furthermore, the reference lists of included studies, reviews, and textbooks were searched through manual search (Online Resource 1, Table S2).
Screening
After excluding the duplicated records, the titles and abstracts of the retrieved studies were independently screened by two authors (S.M and P.I). Then the full texts of studies were read and evaluated for the eligibility criteria independently. In all stages, any disagreements were resolved through discussion with the third author (M.Z.J).
Data extraction
The data of records that met the eligibility criteria were extracted by two reviewers independently(S.M and P.I). A standard form was designed using Excel software (Office, Microsoft, EUA). The studies were categorized into the experimental and randomized controlled trial (RCT) categories according to their design. The data extracted from the included studies were first authors’ last names, year of publication, sample size, time of preparation, and main outcome. Any disagreement was resolved through discussion with other reviewers(M.Z.J). If data were missing, the co-author was contacted via email.
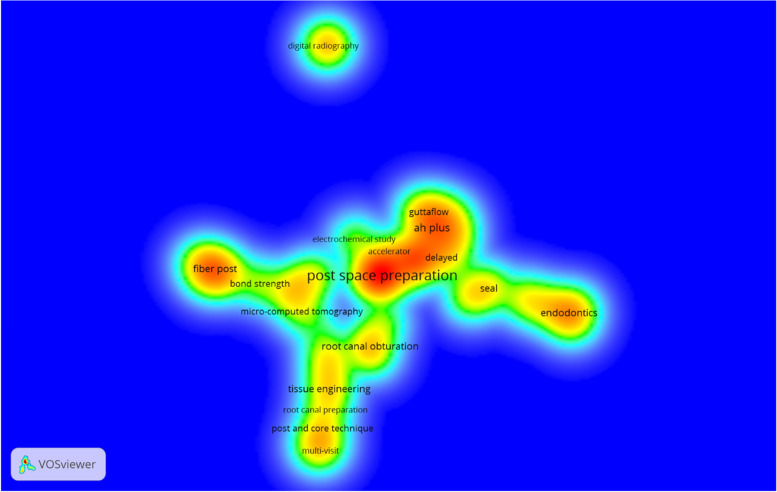
Bibliometric analyses
The trend line of published articles per year and decade was calculated. The bibliometric data of included articles were retrieved from Scopus and imported as a CSV file to VOS viewer 1.6.15 software (http://www.vosviewer.com/, Centre for Science and Technology Studies, Leiden University, Leiden, the Netherlands) to identify the frequency of journal, country of origin, organization, and authorship involved in publishing the PSP. The hot topics were illustrated using density visualization of author keywords co-occurrence.
Qualitative analysis
Data were presented on tabular and bar charts based on the number of articles accordant with immediate or delayed PSP or were unclear.
Results
Description of the included records
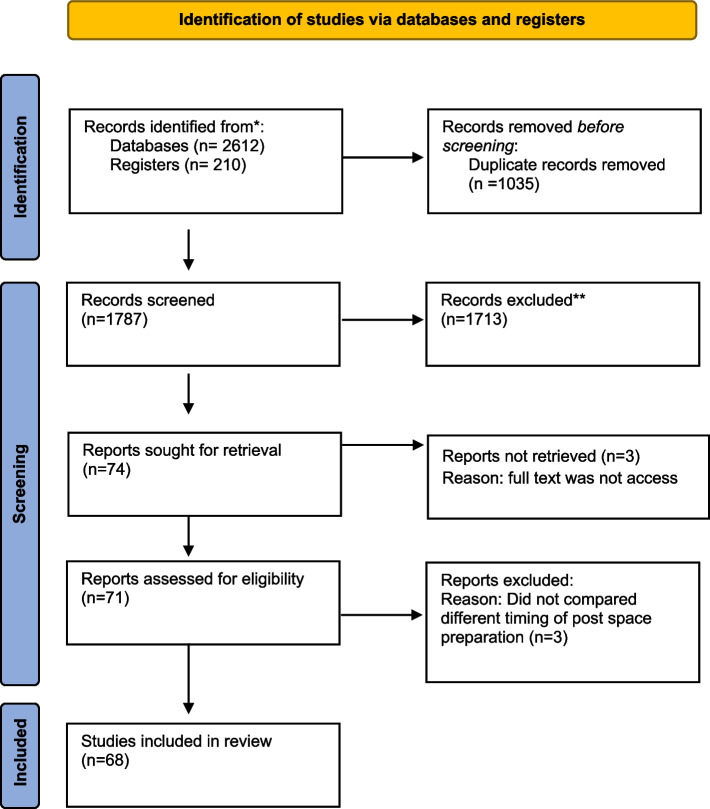
The initial search yielded 412records from PubMed,911 from Scopus, 588 from Web of Science, 210 from Cochrane library, 385 from ProQuest, 72 from WorldCat, 100 from Google Scholar and 144 from hand search. After the removal of duplicated records (1035), 1713 records were excluded in the initial screening of titles and abstracts. At full-text evaluation stage, 6 records were excluded [13–18]. The reasons for exclusion are described in the Online Resource 1, Table S3. Finally, 68 records published between 1981 and 2022 were included (Figure 1).
Fig. 1.
PRISMA flow chart
Characteristics of Records
Tables 1, 2, 3, 4, 5, 6 and 7 summarize the main data. According to the study design, one record was RCT, and the rest were experimental studies (67 records). Two studies were performed on bovine teeth, while others were conducted on human teeth.
Table 1.
Characteristics of the included studies evaluating apical leakage
| Author (Year) |
Sample size (N) |
Groups | System of preparation/Apical size preparation | Filling material / Obturation technique | PSP method | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome |
|---|---|---|---|---|---|---|---|---|---|
|
Al-Ashou et al. (2021) [22] |
102 |
G1:Seal Root / G2:AH Plus /G3:GuttaFlow2 SubGroups: I: 24 h/ II: 1W/ GA: 3mm/ GB: 4mm/ GC: 5mm remaining GP |
K3 system/ #40, 0.06 | GP/ AH Plus, sure seal root canal sealer, GuttaFlow2/ single-cone technique | Peeso reamer #1-4 | Penetration depth of MB dye | 24 h | 7 days |
Delay> immediate MIN: sure Seal root sealer 3mm>4mm>5mm |
|
Gujarathi et al. (2021) [26] |
60 | GA1: AH Plus, imm/ GA2: AH Plus, 1 W/ GB1: sure seal , imm/ GB2: sure seal, 1 W |
ProTaper system/ F2 |
GP/ AH Plus, sure seal root canal sealer / N.r. | Peeso reamer #1-4 | depth of dye penetration ,mm, Image Analysis System | Immediately | 7 days |
Immediate – delay * sure seal > AH Plus |
|
Tiwari et al. (2021) [25] |
66 |
G1:AH Plus/ G2: Apexit Plus / G3:Endosequence SubGroups: A: imm/ B: delay |
ProTaper system/ F3 |
GP/ AH Plus sealer, Apexit Plus sealer, Bioceramic sealer |
Heated plugger Peeso reamer |
Penetration depth of MB dye | Immediately | After setting time of the sealers |
Delay> immediate Apexit Plus> AH Plus> Bioceramic |
|
Raslan et al. (2020) [1] |
20 |
GA: rotary/NO solvent GB: rotary/ solvent |
Mtwo system/ #35 |
GP/ resin sealer ADSEAL/ WVC | Gates Glidden / solvent (Xylol) | Penetration depth of MB dye in apical third/ stereomicroscope | 24 h | 7 days |
Immediate – delay GA: immediate-delay GB: 24h >one week |
|
Tanompetsanga et al (2020) |
60 |
G1:imm/twisting GP cone G2:1W/hot plugger |
Mtwo system/ 50/0.04 |
GT GP impregnated + BC particles/ BC Sealer/ single-cone technique |
Peeso reamer #3 | Fluid filtration device | Immediately | 7 days | immediate-delay |
|
Jieqi1 et al. (2019) |
86 | GA1:imm,4mm/ GB1:imm,5mm/ GC1: imm,6mm/ GA2:1W,4mm/ GB2:1W,5mm/ GC2:1W,6mm |
ProTaper Universal system/ F2 |
GP/ AH Plus sealer/ LC | N.r.. | glucose microleakage model | Immediately | 7 days |
delay>immediate IMM: 4mm - 5mm - 6mm Delay: 4mm > 6mm |
|
Lan Y-y et al. (2017) [63] |
48 | GA1: imm, AH-Plus / GB1:1W, AH-Plus/ GA2:imm, MTA/ GB2: 1W, MTA | N.r./ #30 | GP/ AH Plus sealer, MTA/ LC | Peeso reamer #3 | Apical dye penetration | Immediately | 7 days |
immediate-delay AH Plus > MTA |
|
Kim et al. (2017) [23] |
50 | GI,G8H, G24H, G72H, & G1W | K3 system/40/0.06 | GP/ AH Plus sealer/ WVC | Parapost drill, size 1 | Linear penetration of the stain; mm | Immediately | 8 h, 24 h, 72h & 7days | G1W>GI,G8H, G24H, G72H |
|
Padmanabhan et al. (2017) [6] |
130 | G1:EndoflasFS,imm/ G2:EndoflasFS, 1W/G3: AH Plus, imm/ G4: AHPlus, 1W/ G5:GuttaFlow, imm/ G6:GuttaFlow, 1W/ G7:MTAFillapex, imm/ G8:MTAFillapex,1W |
HyFlex CM/ #40/ 0.04% |
GP/sealers: Endoflas FS,AH Plus, GuttaFlow ,MTA Fillapex/ single-cone technique | Gates Glidden 1-4 | Linear penetration of the stain; mm | Immediately | 7 days |
delay>immediate MAX: G2 MIN: G3 G5,G6: immediate-delay |
|
Rui⁃tian et al. (2016) |
30 | GA: imm/ GB: 2 days/ GC: 7days |
ProTaper system/ F3 |
GP/ AH Plus sealer/ WVC | Fiber post bur | Apical dye penetration | Immediately | 48 h, 7 days | Immediate - delay |
|
Nagas et al. (2016) [2] |
90 |
G1: GP+ AH Plus/G2: Resilon + Epiphany/G3: Sealite Ultra/ SubGroups: I: single cone/II: CLC/ III: system B |
ProFile system/ 30,0.06% |
GP+ AH Plus or Sealite Ultra, Resilon + Epiphany sealer /single cone; CLC, System B | Gates Glidden | Modified fluid transport test; L/min/cmh2o | Immediately |
24 h and 7 days |
immediate> delay Resilon + Epiphany > Sealite Ultra > AH Plus single cone - CLC - System B |
|
Kala et al. (2015) [30] |
70 | G1: imm, EndoREZ sealer /G2: 1W, EndoREZ sealer/ G3:imm, RoekoSeal sealer/ G4: 1W, RoekoSeal sealer/ |
K3 system/ # 30/ 0.06% |
GP/ EndoREZ sealer, RoekoSeal sealer/WVC | peeso reamers 1-4 | Linear measurement of the dye penetration / stereomicroscope | Immediately | 7 days |
Immediate - delay EndoREZ> RoekoSeal |
|
Pushpa et al. (2014) [31] |
45 | G1: imm/ G2: 7days/ G3: 15 days |
K-file/ #80 |
GP/AH Plus/ WVC | heated pluggers Gates Glidden | Apical dye penetration | Immediately | 7 days and 15 days | delay>immediate |
|
Dhaded et al. (2013) [7] |
80 | G1:AH Plus, imm/ G2:AH Plus, 1W/ G3:Resilon/Epiphany, imm/ G4:Resilon/Epiphany, 1W |
Protaper universal/ #40 |
GP/ AH Plus, Resilon + Epiphany/ CLC | peeso reamer | SEM analysis; mm/ stereomicroscope | Immediately | 7 days |
delay>immediate immediately: AH Plus-Resilon + Epiphany delayed: AH Plus >Resilon/Epiphany |
|
Cheng. Et al (2013) |
100 | G1: pulp canal sealer /G2: Tubli-Seal EWT /G3: pulp canal sealer EWT/G4: control |
K3 system/ #35 |
GP/ pulp canal sealer, Tubli-Seal EWT, pulp canal sealer EWT/WVC | heated plugger | Apical dye penetration | Immediately |
72h and 7 Days |
immediate-delay pulp canal sealer > Tubli-Seal EWT, pulp canal sealer EWT |
|
Güngör et al (2013) [34] |
44 | GA1:GP+AH-Plus imm/ GA2: GP+AH-Plus, 1W/ GE1: EndoREZ, imm/ GE2:EndoREZ, 1W |
K-file/ #40 |
GP/ AH-Plus sealer , EndoREZ /LC | heated pluggers Gates Glidden |
computerized fluid filtration device |
Immediately | 7 days |
GE2> GA1- GE1>GA2 EndoREZ > AH-Plus |
|
Pina-Vaz et al. (2013) |
40 | G1: imm, G2: delay |
K-file / N.r. |
GP/ Sealapex sealer/ LC | Protaper universal retreatment file | Apical dye penetration | Immediately | 8 days | Immediate - delay |
|
Al-Sabawi et al. (2012) [33] |
200 |
G1: CLC, imm/ G2: single-cone, imm/ G3: CLC, 1W/ G4: single-cone, 1W SubGroups: heated pluggers, Gates-Glidden, ProTaper rotary, peeso reamers |
ProTaper rotary/ F3 | GP/ Tgadseal root canal sealer/ CLC, single-cone technique |
heated pluggers/ Gates-Glidden/ ProTaper rotary/ peeso reamers |
Apical dye penetration | Immediately | 7 days |
immediate – delay CLC – single cone technique |
|
Yue et al. (2012) |
55 |
G1: imm/ G2: 2 days/ G3: 1W Sub Groups: Post and core preparation after 15, 30 and 60 minutes of cements mixing |
K-file/ #40 |
GP/ N.r. / LC | Gates Glidden/ Peeso reamer | Apical dye penetration | Immediately | 48h, 7 days |
7days > 2days> immediate 15 - 30 - 60 |
|
dezan junior et al. (2012) |
90 | Group I (Sealapex, immediately) to Group IX (Topseal, 60 days) |
Kerr file/ #60 |
GP/ Sealapex, Endométhazone, Topseal/ LC | Gates Glidden | Dye infiltration | Immediately | 30 days and 60 days |
delay>immediate Type of sealer : no statistical differences |
|
Chen & Chang (2011) [37] |
100 | G1: LC / G2: WVC / G3: injectable thermoplasticized GP / G4: control | K3 system/ 0.4 mm | GP/Sealapex / LC ,WVC , injectable thermoplasticized | heated pluggers | Linear penetration of the stain; mm | Immediately |
72h and 7 Days |
(Immediate, 3 days) > 7 days |
|
Attam & Talwar (2010) [36] |
150 | G2: imm, 5mm/ G3: 1W, 5mm/ G4: imm, 3mm/ G5: 1W, 5mm | K3 system/ 45, 0.04% |
Epiphany sealer /Resilon system/ |
Peeso reamers 2,3,4 | Fluid transport device | Immediately | 7 days |
delay>immediate 3mm > 5mm |
|
Paiva et al. (2010) [41] |
40 | G1: imm, ZOE/ G2: ZOE, delay | N.r. | GP/ ZEO sealer/ LC |
ProTaper Universal retreatment files/ H-files |
Apical dye penetration | Immediately | 8 days | delay>immediate |
|
Aydemir et al. (2009) [8] |
64 | G1: CLC, Sealapex, 30 days / G2: CLC, Sealapex, 40 min/ G3: CLC, Diaket, 30 days/ G4: CLC, Diaket,40 min/ G5: WVC, Diaket, 30 days/ G6: WVC, Sealapex, 30 days |
K-file/ #50 |
GP/ Sealapex , Diaket /CLC, WVC | Gates Glidden 1-4 | Electrical current; micro-siemens | 40 min | 30 days |
immediate-delay Sealapex- Diaket CLC > WVC |
|
Chen Mei et al. (2009) [44] |
60 | GA1:imm, temporary materials / GA2:imm,fiber post and cores / GB1: 1W,temporary materials / GB2: 1W,fiber post and cores | hand ProTaper instruments/ F3 | GP/ AH Plus/ LC | Peeso reamers #2 | Apical dye penetration | Immediately | 7 days |
delay>immediate fiber post and core - temporary materials |
|
Kalra et al (2009) [64] |
70 | G1: AH-Plus, imm /G2: AH-Plus, 1W/ G3: RC Seal, imm/ G4: RC Seal, 1W |
K-file/ #50 |
GP/ AH-Plus, RC Seal sealer/ E & Q Plus system | Peeso reamers #3 | Apical dye penetration | Immediately | 7 days |
delay>immediate RC Seal > AH-Plus |
|
Ehsani et al. (2009) [39] |
76 | G1: AH26, imm/ G2: AH26, 1W/ G3: Apatite root sealer , imm,/ G4: Apatite root sealer , 1W |
K-file/ #35 |
GP/ AH26, Apatite root sealer / LC | Peeso reamers #3 | Apical dye penetration | Immediately | 7 days |
delay>immediate AH26 - Apatite root sealer |
|
Yildirim et al. (2009) [43] |
51 | G1: GP+AH-Plus+LC , imm / G2: GP+AH-Plus+LC , 1 W/ G3: 5 mm MTA |
K-files/ #60 |
GP/ AH-Plus sealer , MTA plug /LC |
heated pluggers Gates-Glidden |
Computerized fluid filtration method | Immediately | 7 days |
immediate-delay (GP/ AH-Plus sealer) > MTA |
|
Cobankara et al. (2008) [38] |
50 | G1: CLC, EndoREZ (A_), imm / G2: CLC, EndoREZ (A+), imm / G3: CLC, EndoREZ (A_), 1 W/ G4: CLC, EndoREZ (A+),1 W |
ProFile system/ 0.465 mm |
GP/ EndoREZ sealer with or without accelerator / CLC | heated pluggers | Computerized fluid filtration method | Immediately | 7 days |
delay>immediate (A+) - (A_) |
|
Salim et al. (2008) [42] |
40 | G1a: imm, heated pluggers/ G1b: imm, peeso reamer/ G2a: 1W, heated pluggers/ G2b: 1W, peeso reamer | hand ProTaper instruments/ F1,F2,F3 | GP/ Zinc oxide eugenol sealer/ LC |
heated pluggers peeso reamer |
Apical dye penetration | Immediately | 7 days |
delay > immediate MIN: G1a MAX: G2b |
|
Corrêa Pesce et al. (2007) [20] |
60 | GA1: EndoFill , no post/ GA2: EndoFill, 24 h/ G A3: EndoFill, 72h/ G B1: AH-Plus, no post/ G B2: AH-Plus, 24 h/ G B3: AH-Plus, 72 h |
K-file/ #55 |
GP/ EndoFill or AH-Plus sealer/ CLC |
heated pluggers | Apical dye penetration | 24 h | 72 h |
Immediate - delay EndoFill > AH-Plus In all groups: 1mm > 2mm >3 mm from the apex |
|
Bodrumlu et al. (2007) [47] |
72 | G1:AH Plus, imm/ G2:AH Plus, 1W/ G3:Resilon/Epiphany, imm/ G4:Resilon/Epiphany, 1 W |
K-file/ #40 |
GP/ AH-Plus or Resilon + Epiphany /LC | Gates-Glidden 3-4 | Fluid transport device | Immediately | 7 days |
GP/AH Plus: delay > immediate Epiphany/Resilon: Immediate > delay Immediate: (AH-Plus) –(Resilon Epiphany) Delay:(AH-Plus) > (Epiphany/Resilon) |
|
Shahi et al. (2007) [51] |
96 | GA: peeso reamer, imm/ GB: peeso reamer, 1W/ GC: heated pluggers, imm/ GD: heated pluggers, 1W |
K-file/ #35 |
GP/ AH26 sealer/ LC | heated pluggers /peeso reamer | Apical dye penetration | Immediately | 7 days |
Immediate - delay MIN: GC MAX: GB heated pluggers - peeso reamer |
|
Sadeghi et al. (2007) [50] |
74 | G1: LC, imm/G2: LC, 1W/ G3: WVC, imm /G4: WVC, 1W |
K-file/ #40 |
GP/ Tubliseal sealer/ LC, WVC | heated pluggers | Apical dye penetration | Immediately | 7 days |
delay>immediate WVC > LC |
|
Javidi et al. (2007) [49] |
76 | G1:AH 26, imm/ G2:AH 26, 1W/ G3:Apexit Plus , imm/ G4:Apexit Plus , 1W |
K-file/ #45 |
GP/ AH26 sealer, Apexit Plus / LC | heated pluggers | Apical dye penetration | Immediately | 7 days |
delay>immediate G4> G1 AH26 -Apexit Plus |
|
Solano et al. (2005) [52] |
46 | G1:AH Plus, imm/ G2:AH Plus, 1W |
K3 system/ #30 .06 |
GP/ AH-Plus sealer/ WVC | heated pluggers / Gates-Glidden | Apical dye penetration | Immediately | 7 days | delay>immediate |
|
Rastegar et al. (2004) [48] |
76 | G1: AH26, imm/ G2: AH26, 7 days/ G3: Roth sealer, imm/ G4: Roth sealer, 14 days |
K-file/ #45 |
GP/ AH26, Roth sealer/ LC | peeso reamer | Apical dye penetration | Immediately | 7 days and 14 days |
delay>immediate MIN: G1 MAX:G4 AH26 - Roth sealer |
|
Ashraf et al. (2003) [46] |
96 | G1:imm, AH26/ G2: delay, AH26/ G3: imm, Apexit/ G4: delay, Apexit |
K-file/ #40 |
GP/ AH26, Apexit/ LC | peeso reamer #2,3 | Apical dye penetration | Immediately | 7 days |
Immediate - delay AH26- Apexit |
|
Abramovitz et al. (2000) [45] |
53 |
GA:imm/ heated pluggers GB: 1W/Gates-Glidden 3-4 |
K-file/ #35 |
GP/ AH-Plus sealer/ LC | heated pluggers / Gates-Glidden 3-4 | Pressure-driven system; cpm, Leakage without Pressure, and Leakage under Pressure | Immediately | 7 days |
immediate-delay heated pluggers- drills |
|
Fan et al. (1999) [55] |
90 | G1: AH26, imm / G2:AH26, 1W/ G3: Pulp Canal Sealer ,imm/ G4: Pulp Canal Sealer, 1W |
K-file/ #50 |
GP/ AH26 or Pulp Canal Sealer / LC | Gates-Glidden #90 | Fluid transport device | Immediately | 7 days | delay>immediate |
|
Karapanou et al. (1996) [56] |
80 | G1: imm, Roth 801 sealer/ G2:1W, Roth 801 sealer / G3:imm, AH26 / G4:1W, AH26 | N.r. | GP/ Roth 801 sealer, AH26/ CLC | Gates-Glidden | Linear penetration of the stain; mm | Immediately | 7 days |
Roth 801 sealer: delay>immediate AH-26 sealer: immediate-delay |
|
Rybick & Zillich (1994) [60] |
60 | G1: imm, Thermafil / G2:delay, Thermafil / G3:noPSP, Thermafil / G4: no PSP, CLC |
K-file/ #35-70 |
Thermafil, ThermaSeal epoxy resin-based sealer /CLC | Thermafil Prepi burs | Volumetric analysis; absorbance | Immediately | 72 h | Immediate - delay |
|
Saunders et al. (1993) [61] |
72 | G1: imm/ G2: 1 W |
Flex 0 Files/ #40-50 |
Thermafil/ Sealapex | Peeso reamer #110 | Apical dye penetration ; score | Immediately | 7 days | Immediate - delay |
|
Moon et al. (1988) [58] |
76 | GA1: imm, thermatic condensation/ GA2: delay, LC/ GB1: imm, thermatic condensation/ GB2: delay, LC | H-file/ #25 | GP/ AH26 sealer/ thermatic condensation, LC | heated pluggers/ Gates-Glidden/ Peeso reamers | Apical dye penetration | Immediately | 7 days |
Immediate - delay LC > Thermatic condensation |
|
Madison & Zakariasen (1984) [57] |
80 | G1: imm, solvent/ G2:imm, heat/ G3:imm, drill / G4: 48h, solvent/ G5:48h, heat /G6: 48h, drill/ |
K-file/ #40 |
GP/ Roth's root canal cement/ LC |
Peeso reamers/ heated pluggers/ chloroform & files | (Linear penetration of the stain; mm) and (*Volumetric analysis; μl) | Immediately | 48h |
immediate-delay solvent - heat – rotary instrument |
|
Portell et al. (1982) [59] |
47 | G1: imm, 3mm/ G2: imm, 7mm/ G3: 2 W, 3mm/ G4: 2 W, 7 mm |
K-file/ #50 |
GP/ non staining root canal cement/ CLC | heated pluggers | (Autoradiographic investigation; mm) (Analysis of the incidence; (number teeth with leakage) & degree of leakage: mm) | Immediately | 2 week |
delay > immediate 3mm > 7mm (At all distances from W.L) |
|
Dickey et al. (1982) [54] |
60 | GA1: Peeso reamers, 1 W/ GA2: Peeso reamers, imm/ GB1: solvent, 1 W/ GB2: solvent, imm |
K-file/ #55 |
GP/ Grossman's sealer/ LC | Peeso reamers/ chloroform & files | Autoradiographic investigation; mm | Immediately | 7 days |
Immediate > delay solvent - rotary instrument |
|
Bourgeois & Lemon (1981) [26] |
44 | GA: delay /GB: imm | N.r. |
GP/ AH26 or Grossman's sealer / LC |
heated pluggers | Autoradiographic investigation; mm | Immediately | 7 days |
Immediate –delay AH26 > Grossman |
(A+)/(A_); with or without accelerator, CLC; cold lateral compaction, G; group, GP; gutta-percha, h; hours, imm; Immediate, L; lateral condensation, MB; methylene blue, mm; millimeter, N.r.; not reported, PSP; post space preparation, W; week, WL; working length, WVC; warm vertical compaction, ZOE; zinc oxide eugenol sealer, - ; similar outcome.
Table 2.
Characteristics of the included studies evaluating coronal microleakage
| Author (year) |
Sample size (N) |
Groups | System of preparation/Apical size preparation | Obturation technique | PSP method | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Lan Y-y et al., (2016) [63] | 48 | Based on the sealer: AH-Plus, MTA | N.r./ #30 | Lateral condensation: GP/ AHPlus or MTA | Peeso reamer #3 | Dye penetration | Immediately | 7 days |
AH Plus: delay MTA: - |
PSP; post space preparation, GP: gutta-percha, N.r.; not reported, - ; similar outcome
Table 3.
Characteristics of the included studies evaluating bacterial infiltration
| Author (Year) |
Sample size (N) |
Groups | Rotary system/ Apical size |
Filling material/ Obturation technique | Bacteria type | PSP technique | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
|
Sharma et al. (2020) [68] |
32 | GA: CLC, imm/ GB:MTA plug,imm/ GC:4mm MTA plug, delay |
K-file/ #40 |
GP/ MTA plug | N.r. | N.r. | bacterial leakage test | Immediately | N.r. |
Immediate – delay GA> GB – GC GP > MTA plug |
|
Reyhani et al. (2015) [69] |
76 | G1: AH Plus, imm/ G2: AH Plus, 1W/ G3: MTA Fillapex, imm/ G4: MTA Fillapex, 1W | Race rotary files/ #25, 6% |
GP/ MTA Fillapex , AH Plus sealer/ LC |
E.F/ 90 days |
Peeso reamer #3 | bacterial microleakage system; number of samples with leakage during study | Immediately | 7 days |
Immediate - delay MTA Fillapex - AH Plus |
|
Nikhil et al. (2011) [66] |
90 | G1ax: AH 26, imm, 5mm GP/ G1ay: AH 26, imm ,4mm GP+1mm GIC/ G1bx: AH 26, 1W, 5mm GP/ G1by: AH 26, 1W, 4mm GP+1mm GIC/ G2ax: Resilon+Epiphany, imm, 5mm resilon/ G2ay: Resilon+Epiphany, imm, 1mm GIC/ G2bx: Resilon+Epiphany, 1W, 5mm resilon/ G2by: Resilon+Epiphany, 1W, 4mm GP+1mm GIC |
K-file/ #40 |
GP/AH26 , Resilon/Epiphan/ LC | Staphylococcus species/ 90 days | heated pluggers | bacterial microleakage test | Immediately | 7 days | Delay > immediate |
|
Jalalzadeh et al. (2010) [67] |
86 | GA: imm, AH26/ GB: imm, ZOE/ GC: 1W, AH26/ GD: 1W, ZOE |
K-file/ #35 |
GP/ AH26, ZOE sealer/ LC | Staphylococcus epidermidis/ 70 days | Peeso reamer #3 | bacterial microleakage test | Immediately | 7 days |
Immediate - delay ZOE: Immediate - delay AH26: Delay > immediate ZOE – AH26 |
|
Zmener et al. (2010) [19] |
48 | G1: EndoREZ (A_), 22min / G2: EndoREZ (A+), 8 min / G3: EndoREZ (A_), 1 W / G4: EndoREZ (A+),1 W |
K-file/ #40 |
GP/ EndoREZ sealer with or without accelerator / LC |
E.F/ 60 days |
Gates Glidden #2-5/ Para Post System drill #5, 5.5, 6 |
Dual-chamber microbial leakage model; % teeth without coronal bacterial leakage |
22 min, 8 min |
7 days |
Delay > immediate (A+) - (A_) |
|
Lyons et al. (2009) [71] |
80 | G1: imm/ G2: delay/ G3: imm/ G4: delay |
EndoSequence/ #50 .06 |
Resilon + Epiphany sealer / WVC-System B- Obtura II |
S.M/ 3, 7, 10, 14 up to maximum 28 days |
System B + Gates Glidden | Dual-chamber microbial leakage model; % teeth with bacterial leakage | Immediately | 5 days |
Immediate - delay all groups showed leakage after 14 days: failure of the Resilon/Epiphany to create a true ‘monoblock’ |
|
Grecca et al. (2009) [70] |
66 | G1: imm, burs/ G2: 1W, burs/ G3: imm, heated pluggers / G4: 1W, heated pluggers/ G5: imm, solvent/ G6: 1W, solvent |
K-file/ #50 |
GP/ AH Plus sealer/ Tagger’s hybrid technique |
E.F/ 90 days |
LA Axxess Bur/ heated pluggers /solvent xylol |
Dual-chamber device; number of teeth with bacterial leakage | Immediately | 7 days |
Immediate - delay Bur - heated pluggers - solvent |
(A+)/(A_); with or without accelerator, CLC cold lateral compaction, G group, GP gutta-percha, imm Immediate, L lateral condensation, mm millimeter, MTA mineral trioxide aggregate, N.r. not reported, PSP post space preparation, W week, WVC warm vertical compaction, ZOE zinc oxide eugenol sealer, - ; similar outcome.
Table 4.
Characteristics of the included studies evaluating voids
| Author (Year) |
Sample size (N) |
Groups | System of preparation/ Apical size | Filling material/ Obturation technique | PSP method | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome |
|---|---|---|---|---|---|---|---|---|---|
|
Kataia1 et al. (2020) |
56 |
GA1: penetrating drill/ GA2: heated plugger & EXACTO bur SubGroups: single cone, System-B Minor SubGroups: imm, 1W |
ProTaper Universal System/ F5 |
GP/AH Plus sealer /single cone, System-B | penetrating drill, heated plugger & EXACTO bur | By micro-CT scanner; % voids | Immediately | 7 days |
Delay > Immediate single cone > System-B penetrating drill > heated plugger & EXACTO bur |
|
Long et al (2019) [5] |
40 | GA: single cone, imm/ GB: CWC, imm/ GC: single cone , 1W/ GD: CWC, 1W |
M3 Rotary system/ 30.04 |
GP/ iRoot SP sealer/ single cone or CWC/ | heated plugger | By micro-CT imaging; % volume | Immediately | 7 days |
immediate-delay CWC - single cone |
|
Dhaded et al. (2013) [72] |
80 | G1:AH Plus, imm/ G2:AH Plus, 1W/ G3:Resilon/Epiphany, imm/ G4:Resilon/Epiphany, 1W |
Protaper universal/ #40 |
GP+ AH Plus, Resilon + Epiphany/ CLC | peeso reamer | SEM analysis; mm/ stereomicroscope | Immediately | 7 days |
Delay > immediate immediately: AH Plus-Resilon + Epiphany delayed: AH Plus >Resilon/Epiphany |
CLC cold lateral compaction, CWC continuous wave of condensation, G groups, GP gutta percha, imm Immediate, PSP post space preparation, W week, - ; similar outcome.
Table 5.
Characteristics of the included studies evaluating bond strength of the posts
| Author (Year) |
Sample size (N) |
Groups | System of preparation/ Apical size/ Irrigation Protocol | Obturation material/ Technique |
PSP method/ Dentin adhesion/ Luting agent | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome |
|---|---|---|---|---|---|---|---|---|---|
|
Long et al (2019) [5] |
40 | GA: single cone, imm/ GB: CWC, imm/ GC: single cone , 1W/ GD: CWC, 1W |
M3 Rotary system/ 30.04/ 2.5% NaOCl, 17% EDTA, 1% NaOCl |
GP/ iRoot SP sealer/ single cone or CWC | heated plugger/ ScotchbondTM Universal Adhesive/ RelyX | Push-out test in fiber post; mpa | Immediately | 7 days |
immediate-delay* CWC - single cone |
|
Vilas-Boas et al (2017) [73] |
84 | GA1: imm, Endofill/ GB1: imm, BC Sealer/ GC1: imm, AH Plus/ GA2: 1W, Endofill/ G B2: 1W, BC Sealer / GC2: 1W, AH Plus |
Reciproc/ R40/ 2.5% NaOCl, 17%EDTA |
GP/ Endofill Endosequence BC Sealer, AH Plus / thermo filling with McSpadden compactor |
Largo burs #3/ ScotchbondMulti Purpose / RelyX | Micropush-out bond strength of the fiber post; mpa | Immediately | 7 days |
Immediate > delay AH Plus sealer >Endofill, Endosequence BC |
|
Aleisa, et al (2016) [21] |
72 | G1: 24 h G2: 2 W |
Protaper system / F2/ 5.25% NaOCl |
GP/ Endofil sealer / LC | Peeso reamer #5/ ParaBond adhesive A/B/ Variolink II, RelyX, ParaCoreColtèene/ | pull-out test of fiber post (parapost) | 24 h | 14 days |
Immediate > delay 24h: RelyX>Variolink II, ParaCore 2 W: RelyX>Variolink II |
|
Machado et al. (2015) [77] |
12 | G1: imm/ G2: 21 days |
Protaper universal system/ N.r./ 2.5% NaOCl |
GP/ AH Plus / WVC | Largo drills 3-5/ self-adhesive Resin cement Rely-X |
Push-out test in cylindrical fiber post; mpa (Cervical ,medium and apical third) |
Immediately | 21 days |
Delay > Immediate Imm: Cervical - medium -apical third Delay: apical > Cervical, medium third |
|
Dias et al. (2009) [62] |
60 | GI: imm/ GII: 72 h/ GIII: 4 months |
K-file/ #45/ 1% NaOCl |
GP/ Endofill/ LC | Largo drills 1-3/ Kuraray adhesive system / zinc phosphate cement, Panavia F | Push out test in the cylindrical SS post | Immediately | 72 h and120 days |
immediate-delay zinc phosphate >Panavia F |
|
Vano et al. (2008) [74] |
68 | G1: imm/ G2: 24 h/ G3: 1 W |
K-files (#08-10-15), M-two (#10-15-20-25), Profiles .06 (#30-35-40)/ 5.25% NaOCl |
GP/ AH Plus sealer/ CWC | heated plugger / Monobond-S |
Push out test in post; mpa ( ENA post , DT Light Post and FRC Postec) |
Immediately |
24 h and 7 days |
Delay > Immediate FRC Postec, DT Light Post > ENA post |
|
Vano et al. (2006) [75] |
60 | G1: imm/ G2: 24h/ G3:1W |
K-files (#08-10-15), M-two (#10-15-20-25), Profiles .06 (#30-35-40)/ 5.25% NaOCl |
GP/ Pulp Canal sealer/ CWC | low-speed post drills | (Push out test in the post; mpa) FRC Postec , ENA Post and DT Light Post | Immediately |
24 h and 7 days |
Delay > Immediate FRC Postec, DT Light Post > ENA post |
|
Boone et al. (2001) [76] |
120 | G1: imm, Roth’s 801, O/S/ G2: imm, AH26, O/S/ G3: imm, , Roth’s 801, S/O/ G4: imm, AH26, S/O/ G5: 1W, Roth’s 801, O/S/ G6: 1W, AH26, O/S/ G7:1W, Roth’s 801, S/O/ G8: 1W, AH26, S/O |
ProFile system /50, .04/ 5.25% NaOCl, 17% EDTA |
GP/ Roth’s 801, AH26/ LC | Touch ’n Heat/ Panavia 21 | (Push out test in the #6 parallel-sided stainless-steel Parapost XP post) | Immediately | 7 days |
immediate-delay Roth’s 801 - AH26 O/S > S/O |
CWC continuous wave of condensation G; group, GP gutta-percha, h hours, imm Immediate, L lateral condensation, N.r. not reported, O/S- S/O obturated before post space prepared - post space prepared before obturation, PSP post space preparation, W week, WVC warm vertical compaction, - ; similar outcome
Table 6.
Characteristics of the included studies evaluating apical displacement and residual filling material
| Author (Year) |
Sample size (N) |
Groups | System of preparation / Apical size | Filling material/ Obturation technique | PSP method | Measurement | Time of immediate PSP | Time of delayed PSP | Outcome of residual filling | Outcome of apical displacement (extrusion) |
|---|---|---|---|---|---|---|---|---|---|---|
|
Rosatto et al (2020) [9] |
20 | G1: imm, drill/ G2: imm, thermo/ G3: 2 W, drill/ G4: 2 W, thermo |
K-file/ #30 |
GP/ AH Plus sealer /single cone | Peeso reamers 2-3 , thermo using M and FM tips – Odous Touch | Micro-CT Analysis; volume (mm3) in cervical, middle and apical thirds | 30 min | 14 days |
Both Methods: Delay > Immediate Cervical, Middle: drill - thermo Apical: thermo > drill Imm: cervical- middle -apical All Other Combinations: middle ,apical > cervical |
immediate-delay thermo: imm, delay drill: imm |
G; group, GP; gutta-percha, h; hours, imm; Immediate, PSP; post space preparation, W; week, - ; similar outcome
Table 7.
The clinical trial study evaluating post operative pain after PSP
| Author (Year) |
Sample size (N) |
Prescribed analgesics | System of preparation/ Apical size | Filling material/ Obturation technique | PSP method | Postoperative pain evaluation | Time of immediate PSP | Time of delayed PSP | utcome |
|---|---|---|---|---|---|---|---|---|---|
| Eyuboglu et al. (2020) [11] | 100 | (naproxen sodium, 550 mg) at the end of the first appointment | 2Shape rotary system/ TS2 (#25/.06) or 2Shape F35 (#35/.06) | GP /calcium silicate-based root canal sealer / Single cone | fiber post drills | An electronic pain rating scale program + (VAS) in 1, 2, 3 days and 1 week after the first visit | first-visit: immediately | second-visit :at least 1 W | 1-visit > 2-visits |
G, group, GP gutta-percha, imm Immediate, PSP post space preparation, VAS visual analogue scale, W week, - ; similar outcome
In Vitro Studies
For the in vitro category, 67 studies were included (Tables 1, 2, 3, 4, 5 and 6). Regarding the timing of PSP, the immediate preparation times were 8 min and 22 min [19], 30 min [9], 40 min [8] in one study each, and 24 hours in four studies [1, 20–22]. The exact time of immediate PSP was not reported in other included studies [2, 6, 7, 10, 23–61]. There was a great range regarding the exact time of delayed PSP. For the delayed preparation group, the included studies considered a wide range from4 months [62] to 48 h or 72 h [20, 23, 28, 29, 35, 37, 57, 60, 62]. One study evaluated the effect of four delayed preparation times, including 8 h, 24 h, 72 h, and 7 days [23].
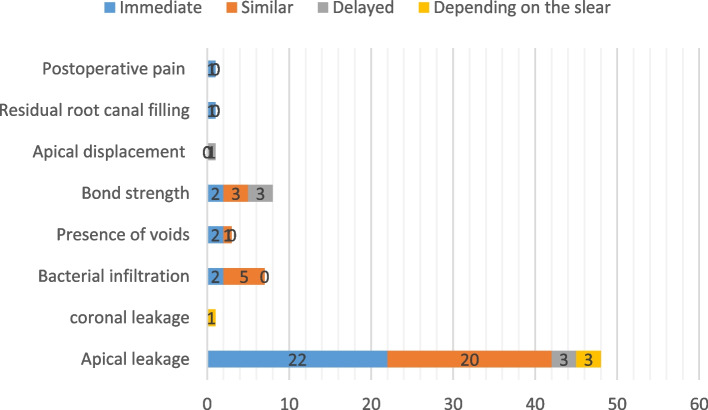
In experimental studies, the effects of timing of PSP on 6 variables, including graphical microleakage (n=48), coronal microleakage (n=1), bacterial infiltration (n=7), presence of void (n=3), bond strength (n=8), and apical displacement and residual root canal filling (n=1), were evaluated (Tables 1, 2, 3, 4, 5 and 6 and Fig. 2).
Fig. 2.
The summery of superiority of delay vs immediately post space preparation according the included studies
Apical Microleakage
Apical microleakage was assessed in 48 in vitro studies [1, 2, 6–8, 20, 22–61, 63, 64] using different methods such as autoradiographic investigation [53, 54, 59], linear dye penetration [1, 6, 20, 22, 23, 25, 26, 28–33, 35, 37, 39–42, 44, 46, 48–52, 56–58, 61, 63, 64], glucose microleakage model [27], fluid transport device [2, 24, 36, 47, 55], volumetric analysis [60], computerized fluid filtration method [34, 38, 43], electrical curren t[8], pressure-driven system [45], and scanning electron microscopy (SEM) [7]. Different outcomes were reported in this regard. While most studies showed the benefit of immediate PSP [6, 7, 22, 23, 25, 27, 31, 35, 36, 38–42, 44, 48–50, 52, 55, 59, 64], others showed no superiority of either timing [1, 8, 20, 24, 26, 28–30, 32, 33, 43, 45, 46, 51, 53, 57, 58, 60, 61, 63], and a few showed lower apical microleakage after delayed PSP [2, 37, 54]. In three studies based on the type of sealers used, different results were achieved, which will be discussed further [34, 47, 56].
Coronal Microleakage
A study examined coronal microleakage using different filling materials [65] and showed the length of coronal microleakage depended on the sealer and timing of the PSP. When mineral trioxide aggregate (MTA) paste was used as a filling material, the timing of PSP did not affect coronal microleakage. However, when AH plus paste was used, immediate PSP resulted in lower coronal microleakage (Table 2).
Bacterial Infiltration
Seven invitro studies evaluated bacterial infiltration [19, 66–71], three used Enterococcus faecalis [19, 69, 70], two used Staphylococcus species [66, 67], and one used Streptococcus mutans as the bacterial marker [71] for the preparation of the infected specimens. The microbial microleakage model in three studies consisted of the dual chamber test [70, 71] or a slight modification of it [19], and four studies used the bacterial microleakage system, which provides qualitative rather than quantitative results [66–69]. All the studies considered extracted human single-rooted teeth. Overall, they found no significant difference in the bacterial microleakage between immediate and delayed PSP groups, except two studies [19, 66], which reported lower bacterial infiltration was reported in the immediate PSP group.
Presence of Voids
Three studies evaluated the presence of voids; one with SEM [72] and the two other with micro-computed tomography (micro-CT) imaging [5, 10]. The micro-CT imaging showed no significant differences between the immediate or delayed PSP [5] based on the measurement of the volume of voids. However, another micro-CT imaging analysis reported the lowest mean value of voids in the immediate PSP group [10], the same results as those of another SEM analysis [72].
Bond Strength
Considering the bond strength, all eight studies analyzed adhesive resistance by the push-out test of the post after cementation. They sectioned the specimens perpendicularly to the long axis of the root, and a cylindrical plunger was applied in the apical-coronal direction loading until the filling material or the post was dislodged from the slice. Teeth that were used were human single-rooted teeth in 6 studies [21, 62, 73–76], human premolar teeth with double root canals in one study [5], and bovine teeth in one study [77]. Various techniques and materials were used for post cementation. Experimental procedures were done on fiber posts in all studies, whereas stainless-steel posts were used in two studies [62, 76]. Sodium hypochlorite (NaOCl) [5, 21], NaOCl and EDTA 17% [76], and distilled water [73, 78] were among the solutions used for post space irrigation. Moreover, in a study by Vano et al. [75], an additional SEM analysis was done to assess the cleanliness of the post-space qualitatively. In general, the outcomes of the studies were heterogeneous. Three studies indicated no significant differences [5, 62, 76], while three [74, 75, 77] and two studies [21, 73] reported higher bond strength in the delayed and immediate preparation groups, respectively.
Apical displacement and residual root canal filling
A study analyzed apical displacement and residual root canal filling [9]. Bovine teeth were scanned by micro-CT before and after PSP. No significant difference was reported for the displacement of the filling material in the apical direction (extrusion). However, regarding residual root filling, immediate PSP, either with thermo or drill methods, resulted in lower residues in the root canal. In general, PSP with a drill resulted in more homogeneous root canal preparation, mainly when performed immediately.
Clinical studies
An electronic pain rating scale program with a vertical visual analog scale (VAS) was used after the first visit for both groups to evaluate post-operative pain by an RCT (Table 7) [11]. Results presented no post-operative pain in patients with delayed post cementation, in contrast, there was significantly higher post-operative pain in immediate post installation on days 1, 2 and 3 and 1 week after the first visit.
Bibliometric Analysis
Linear trend line analysis showed that the number of publications on PSP in endodontology had a steady growth per year but had a fast growth per decade (Fig. 3). Totally, 44 journals contributed to publishing articles on PSP, of which “Journal of Endodontics” with 11 published articles, acquired the top rank (Online Resource 1, Figure S1). Among19 countries that contributed to the research and publications in the field of immediate and delayed PSP, India had the highest number of publications (n = 11), followed by the USA, China, and Iran (n = 8 for each) (Online Resource 1, Figure S2). Furthermore, the U.S.A. with, 5 links had the highest international collaboration (Online Resource 1, Figure S3). At the author level, 175 authors within 37 clusters from 88 organizations contributed to the publishing of articles on PSP (Online Resource 1, Figure S4). Density visualization indicated that “post-space preparation”, “fiber post", and “AH plus” were the most popular keywords used by authors (Fig. 4).
Fig. 3.
The trend of published studies regarding immediate and delayed PSP comparison over the past 40 years per year (blue line) and decade (red line)
Fig. 4.
Author hot topics among 67 included articles using density visualization. Red–yellow–green–blue color scheme was used; red corresponds to the highest and blue corresponds to the lowest density of keyword co-occurrence. The distance-based approach was used; smaller the distance between two item means the higher relatedness
Discussion
This scoping review provides information about the publishing metrics of PSP. Articles with a steady growth evaluated the influence of different time intervals of PSP on various aspects of an endodontically treated tooth over four decades. It should be noted that there was no well-designed randomized controlled trial on this subject. Furthermore, the present scoping review categorized the effect of the timing of PSP on the apical sealing of the remaining root canal filling material, bacterial infiltration, presence of voids, post-bond strength, apical extrusion, residual filling material, and post-operative pain in endodontically treated teeth. Overall immediate PSP would be the safest clinical choice regarding most of these parameters. Other than post-operative pain, there were lower apical microleakage and lower residues into the root canal after immediate PSP, and no difference was found regarding bacterial microleakage and displacement of filling materials. However, further studies are required to explore some parameters such as the presence of voids and post-bond strength.
The data regarding apical microleakage were very heterogeneous, and most of the in vitro studies indicated lower penetration of dyes or fluids into the immediate PSP some suggesting no difference in bacterial infiltration. However, a recent meta-analysis with strict eligibility criteria, which included 3 studies, reported higher apical microleakage in one week delayed PSP [79]. Moreover, a systematic review reported all techniques used for evaluating apical microleakage were helpful if the study had a large sample size and a proper control group [80]. In addition to these factors, variations in sealer type and root filling materials, PSP methods, and the amount of the remaining root filling material may be other reasons for this difference [2, 47, 79]. Regarding the different properties of the sealers, a lower apical microleakage was shown in the immediate PSP using the AH plus compared with delayed PSP and zinc oxide-eugenol-based seale r[6, 20, 48, 53, 55, 56]. For AH plus, higher adhesion to dentin and expansion capacity may significantly reduce the apical microleakage [5, 45, 55]. Different PSP methods and the amount of remaining root filling materials may affect the outcome of apical microleakage. For instance, a heated endodontic plugger for immediate PSP may remove the gutta-percha without disturbing the apical seal and eliminate the possibility of inadvertent damage to dentin [81]. In any case, PSP should allow a minimum length of 3-5 mm gutta-percha in the apical third to preserve the seal [81]. In two studies comparing the effect of the length of the remaining apical filling material on apical microleakage, the more was the remaining apical filling material, the lower was the apical microleakage [22, 27]. In conclusion, many factors may affect the outcome of apical microleakage, so more studies are required to be conducted in this regard.
Among three studies that evaluated the presence of void and adaptation of filling materials, Dhaded et al. [72] and Kataia et al. [10] reported better adaptation in the immediate PSP group. On the other hand, no difference was reported by Long et al. [5] which might be due to different obturation techniques and sealers. For instance, the single-cone technique provides void-free obturation and improves the apical sealing along with a minimal sealer thickness [2]. The delayed PSP may cause the fracture of the bonding of the sealer (AH Plus, Resilon / Epiphany) to dentin when the sealer is set [10]. Still, considering the excellent properties of calcium silicate-based sealers, the bonding integrity is maintained [4]. In general, due to limited studies, more studies are suggested to be performed in this regard.
Bond strength was evaluated by the push-out test in the included studies [5, 21, 62, 73–76, 78] with controversial results regarding the timing of PSP. The adhesive system, surface treatment, and cement curing methods that guaranteed efficient adhesion of the post to the root dentin [82] were different and might be the reason for controversy. Post-space surface treatment such as the use of ethanol or sodium hypochlorite removes the smear layer efficiently and increases the infiltration depth of the adhesive and types of cement into the dentinal tubules [83, 84]. Regarding the effect of the cement curing methods on bond strength, dual or chemically activated adhesive resin cements are the most appropriate for the cementation of fiberglass posts since, with a longer working time, they allow better control of the post adaptation [82]. The use of photoactivated cement, because of limited light transmission to the apical third, results in a low degree of conversion of resin monomers, thereby compromising the integrity of the adhesive interface [82]. Future studies are required to investigate the influence of these factors and an appropriate time of PSP that guarantee effective bond strength.
Apical displacement and residual root filling after PSP were analyzed through micro-CT analysis in one study [9]. The micro-CT provides high-resolution images and allows for quantitative analyses. While no difference was reported regarding apical displacement of the filling material, a lower percentage of residual filling material was reported for immediate PSP, which is probably related to the technical difficulty of root filling material removal over time.
A randomized controlled trial evaluated the post-operative pain of PSP and showed the vibrations generated during post-installation by a low-speed handpiece with dedicated fiber post drills from the post kit in the same visit of root canal filling might increase the post-operative pain. Therefore, the cumulative effect of root canal treatment and post installation in the first visit might increase the intensity of pain [11]. Although delayed PSP was recommended, more studies are necessary to thoroughly investigate the effects of the timing of PSP on post-operative pain.
Strength and limitation
This review was compatible with the framework of the PRISMA-ScR Checklist in identifying the research question and relevant studies, charting the data and handling, and summarizing and reporting the result s[85]. A comprehensive search with no language restrictions was conducted. The screening of records and data extraction were done by two independent reviewers. All variables regarding the impact of PSP time in endodontically treated teeth were considered, which were compatible with bibliometric analysis.
Implications for further research
Considering controversial outcomes on apical microleakage and scarcity of studies on other variables, further investigations, particularly clinical studies, are suggested. Several materials and techniques were applied, which might have affected the outcomes, indicating a lack of a standard reporting checklist and standard control group.
Conclusion
The number of studies on the comparison of immediate and delayed PSP increased over time; however, almost all studies were experimental. The studied variables included apical microleakage, coronal microleakage, bacterial infiltration, bond strength of posts, presence of voids, apical displacement of the filling material, adhesion of the remaining filling material, and post-operative pain. Most of the evidence indicated lower apical microleakage and lower residues into the root canal after immediate PSP, lower post-operative pain in delayed PSP, and no difference regarding bacterial microleakage and displacement of filling materials. Considering coronal microleakage, presence of voids, and bond strength, outcomes of the evidence were heterogeneous, indicating that future studies are needed to explore this issue. However, it remains unclear whether factors such as gutta-percha removal methods, obturation techniques, sealer properties, type of cement and adhesive, length of the remaining filling material, and irrigation protocol are effective or not, which requires further investigations.
Supplementary Information
Acknowledgments
Not applicable
Abbreviations
- PSP
post space preparation
- RCT
randomized controlled trial
- SEM
scanning electron microscopy
- MTA
mineral trioxide aggregate
- micro-CT
micro computed tomography
Authors’ contributions
M.Z.J.& S.Kh.; Study design– P.I. & S.M.; Literature search, study selection and data collection – P.I., S.M & S.Kh.; Bibliometric analyses– P.I.; Interpretation of data for the work–S.Kh & M.Z.J.; Manuscript drafting – P.I. & S.M.; Manuscript revision –M.Z.J. &S.Kh.; All authors have read and approved the manuscript.
Funding
None
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sadaf Mahmoudi, Email: mahmoudi.sadaf@yahoo.com.
Pedram Iranmanesh, Email: pedram.iranmanesh@yahoo.com.
Saber Khazaei, Email: saber.khazaei@yahoo.com.
Maryam Zare Jahromi, Email: m.zare@khuisf.ac.ir.
References
- 1.Raslan D, Almarrawi K. In vitro comparative study of the influence of post space preparation timing on apical sealing of root canal. Int J Appl Dental Sci. 2020;6(2):588–592. [Google Scholar]
- 2.Nagas E, Karaduman E, Sahin C, Uyanik O, Canay S. Effect of timing of post space preparation on the apical seal when using different sealers and obturation techniques. J Dental Sci. 2016;11(1):79–82. doi: 10.1016/j.jds.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metgud SS, Shah HH, Hiremath HT, Agarwal D, Reddy K. Effect of post space preparation on the sealing ability of mineral trioxide aggregate and Gutta-percha: A bacterial leakage study. J Conserv Dentistry. 2015;18(4):297. doi: 10.4103/0972-0707.159729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu-Awwad M. A modern guide in the management of endodontically treated posterior teeth. Eur J Gen Dentistry. 2019;8(03):63–70. doi: 10.4103/ejgd.ejgd_76_19. [DOI] [Google Scholar]
- 5.Long W, Li J, Liu Y, Jiang H. Effect of obturation technique with immediate and delayed post space preparation on apical voids and bond strength of apical gutta-percha. J Int Med Res. 2019;47(1):470–480. doi: 10.1177/0300060518814604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Padmanabhan P, Das J, Kumari RV, Pradeep P, Kumar A, Agarwal S. Comparative evaluation of apical microleakage in immediate and delayed postspace preparation using four different root canal sealers: An in vitro study. J Conserv Dentistry. 2017;20(2):86. doi: 10.4103/0972-0707.212230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhaded N, Uppin VM, Dhaded S, Patil C. Evaluation of immediate and delayed post space preparation on sealing ability of Resilon–Epiphany and Gutta percha-AH plus sealer. J Conserv Dentistry. 2013;16(6):514. doi: 10.4103/0972-0707.120962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aydemir H, Ceylan G, Tasdemir T, Kalyoncuoglu E, Isildak I. Effect of immediate and delayed post space preparation on the apical seal of root canals obturated with different sealers and techniques. J Appl Oral Sci. 2009;17(6):605–610. doi: 10.1590/S1678-77572009000600013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosatto CMP, Oliveira LV, Ferraz DC, Soares PBF, Soares CJ, Moura CCG. Apical Displacement and Residual Root Canal Filling with Single-Cone After Post Space Preparation: A Micro-CT Analysis. Braz Dent J. 2020;31:25–31. doi: 10.1590/0103-6440202002597. [DOI] [PubMed] [Google Scholar]
- 10.Kataia EM, Kataia MM. Micro-computed tomographic evaluation of the apical seal of endodontically treated teeth by two obturating techniques and two post space preparation techniques. J Int Oral Health. 2020;12(1):41. doi: 10.4103/jioh.jioh_168_19. [DOI] [Google Scholar]
- 11.Eyuboglu TF, Kim HC. When to install the endodontic post? First visit with root canal filling versus a separate second visit for post-restoration: A randomized controlled trial. J Oral Rehabil. 2020;47(10):1247–1253. doi: 10.1111/joor.13056. [DOI] [PubMed] [Google Scholar]
- 12.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implement. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 13.Sawsan TAZ, El Sayed M. The effect of immediate post-space preparation on the apical seal of endodontically treated teeth obturated with various root canal sealers. 1993. [Google Scholar]
- 14.De Nys M, Martens L, De Coster W, Thys M. Evaluation of dowel space preparation on the apical seal using an image processing system. Int Endod J. 1989;22(5):240–247. doi: 10.1111/j.1365-2591.1989.tb00517.x. [DOI] [PubMed] [Google Scholar]
- 15.Al-Shimmary AH, Al-Huwaizi HF. Comparison of apical seal of four obturation techniques after delayed post space preparation. J Baghdad Coll Dentistry. 2012;24(special issue 2):1-4.
- 16.Roitman ML, Pinasco LB, Loiacono R, Panetta VC, Anaise CA, Rodríguez PA. Efficacy of different instruments for the mechanical removal of the smear layer in immediate post preparations: a comparative study. Acta odontologica latinoamericana. 2021;34(2):166–172. doi: 10.54589/aol.34/2/166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerogianni P, Chrepa V, Haney S. Cat of the month. Critically Appraised Topics. Time of Post Space Preparation Affects the Amount of Coronal Microleakage in Endodontically Treated Teeth When a Resin Sealer Is Used (UT CAT #2773) Texas Dental J. 2015;132(5):302. [PubMed] [Google Scholar]
- 18.Ibrahim RM, Seef RE, Seniour SH. The effect of immediate and delayed post space preparation and post length on the apical seal. Egypt Dent J. 1995;41(4):1457–1462. [PubMed] [Google Scholar]
- 19.Zmener O, Pameijer CH, Alvarez SS. Effect of immediate and delayed post space preparation on coronal bacterial microleakage in teeth obturated with a methacrylate-based sealer with and without accelerator. Am J Dent. 2010;23(2):116–120. [PubMed] [Google Scholar]
- 20.Corrêa Pesce AL, González López S, González Rodríguez MP. Effect of post space preparation on apical seal: influence of time interval and sealer. Medicina Oral, Patología Oral y Cirugía Bucal (Internet) 2007;12(6):464–468. [PubMed] [Google Scholar]
- 21.Aleisa K, Al-Dwairi ZN, Alsubait SA, Morgano SM. Pull-out retentive strength of fiber posts cemented at different times in canals obturated with a eugenol-based sealer. J Prosthet Dent. 2016;116(1):85–90. doi: 10.1016/j.prosdent.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 22.Al-Ashou WMO, Al-Shamaa RM, Hassan SS. Sealing Ability of Various Types of Root Canal Sealers at Different Levels of Remaining Gutta Percha After Post Space Preparation at Two Time Intervals. J Int Soc Prev Commun Dentistry. 2021;11(6):721–728. doi: 10.4103/jispcd.JISPCD_178_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H-R, Kim YK, Kwon T-Y. Post space preparation timing of root canals sealed with AH Plus sealer. Restorative Dentistry Endodontics. 2017;42(1):27–33. doi: 10.5395/rde.2017.42.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanompetsanga P, Pakit T. Microleakage in Immediate vs Delayed Post Space Preparation in Root Canals Filled with Bioceramic-based Root Canal Sealer. World J Dent. 2020;11(3):172–178. doi: 10.5005/jp-journals-10015-1720. [DOI] [Google Scholar]
- 25.Dixit T, Vanapatla A, Tulasi Priya N, Neethu Nanda B, Sneha P, Avinash M. Comparision of apical leakage between immediate versus delayed post space preparation using various root canal sealers–an invitro study. Turkish J Physiotherap Rehab. 2021;32(3):18701–18705. [Google Scholar]
- 26.Gujarathi NN, Mandlik J, Singh S, Chaubey S. Evaluation of apical leakage after immediate and delayed postspace preparation using different root canal sealers: An in vitro study. J Conserv Dentistry. 2021;24(2):174–178. doi: 10.4103/jcd.jcd_79_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang J, Zheng M, Wu H, Li X, Xie W. Microleakage from the crown to the root canal after post space preparation with different timing and remaining length. Chin J Tissue Eng Res. 2019;23(10):1552–1557. [Google Scholar]
- 28.Chen G, Chang Y. The effect of immediate and delayed post-space preparation using extended working time root canal sealers on apical leakage. J Dental Sci. 2013;8(1):31–36. doi: 10.1016/j.jds.2012.10.001. [DOI] [Google Scholar]
- 29.RT D, SQ L, FY G, HW L, YT F, XY W. An in vitro/comparative study on the effect of different timing of post space preparation on apical microleakage of fiber posts. J PrevTreat Stomatol Dis. 2016;24(9):515–518. [Google Scholar]
- 30.Kala M, Torvi SJ. An in vitro comparision of apical leakage in immediate versus delayed post space preparation using EndoREZ and RoekoSeal root canal sealers. J Int Clin Dental Res Organ. 2015;7(1):30. doi: 10.4103/2231-0754.153492. [DOI] [Google Scholar]
- 31.Pushpa S, Geeta, Benal Vijayalaxmi D, Bharati SH, Prashanth R, Karuna An in-vitro comparison of apical leakage in immediate versus delayed post space preparation. Maharaja Krishnakumarsinhji Bhavnagar University. 2014;4(1):19–22. [Google Scholar]
- 32.Vaz I, Carvalho MJ, Barros J, Cruz J. Influence of the timing of post space preparation on apical sealing. RGO - Rev Gaúcha Odontol. 2013;61(2):199–204. [Google Scholar]
- 33.Al-Sabawi NA, Ismail SA, Al-Askary RA. Effect of different techniques of immediate and delayed post space preparation on apical seal. Al-Rafidain Dental J. 2012;12(2):249–256. doi: 10.33899/rden.2012.65073. [DOI] [Google Scholar]
- 34.Güngör G, Türkaydin D, Tarçin B, Öveçoğlu H, Günday M, Oruçoğlu H. Comparison of apical sealing of two canal sealers between immediate versus delayed post space preparation. Marmara. Dent J. 2013;1(1):20–23. [Google Scholar]
- 35.Xiao Y, Yu J, Wang JP, Guo H. Effects of post space and post core preparation at different time on apical microleakage with fiber post sealing. Chinese Journal of Tissue Engineering. Research. 2012;16(29):5366–5370. [Google Scholar]
- 36.Attam K, Talwar S. A laboratory comparison of apical leakage between immediate versus delayed post space preparation in root canals filled with Resilon. Int Endod J. 2010;43(9):775–781. doi: 10.1111/j.1365-2591.2010.01742.x. [DOI] [PubMed] [Google Scholar]
- 37.Chen G, Chang Y-C. Effect of immediate and delayed post space preparation on apical leakage using three root canal obturation techniques after rotary instrumentation. J Formos Med Assoc. 2011;110(7):454–459. doi: 10.1016/S0929-6646(11)60067-3. [DOI] [PubMed] [Google Scholar]
- 38.Cobankara FK, Orucoglu H, Ozkan HB, Yildirim C. Effect of immediate and delayed post preparation on apical microleakage by using methacrylate-based EndoREZ sealer with or without accelerator. J Endod. 2008;34(12):1504–1507. doi: 10.1016/j.joen.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 39.Ehsani M, Mesgarani A, Soltani-Garmabi M. Comparison of apical leakage using AH26 and Apatite root sealers with immediate and delayed post space preparation. J Iranian Dental Assoc. 2009;21(2):132–137. [Google Scholar]
- 40.Junior ED, Garcetti riBeiro G, de Castilho Jacinto R, Juvenal nerY M, JA OFH, JEG FH, et al. Marginal leakage evaluation of three endodontic sealers according to the moment of post preparation. Dental Press Endodontics. 2012;2(2):37–41. [Google Scholar]
- 41.Paiva J, Barros J, Noites R, Carvalho MF, Pina-Vaz I. Comparação da Infiltração Apical entre a Desobturação Imediata do Canal Radicular e a Desobturação após 8 Dias para a Preparação do Espaço para o Espigão. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial. 2010;51(4):197–205. doi: 10.1016/S1646-2890(10)70098-4. [DOI] [Google Scholar]
- 42.Salim BM. A comparison between immediate and delayed post space preparation on the apical seal prepared by hand protaper instruments. MJD. 2008;5:232–238. [Google Scholar]
- 43.Yildirim T, Taşdemir T, Orucoglu H. The evaluation of the influence of using MTA in teeth with post indication on the apical sealing ability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(3):471–474. doi: 10.1016/j.tripleo.2009.04.036. [DOI] [PubMed] [Google Scholar]
- 44.Chen M, Feng YZ. The effects of post space preparation and post restoration on apical sealing ability. Hua xi kou qiang yi xue za zhi = Huaxi kouqiang yixue zazhi = West ChinaJ Stomatol. 2009;27(5):512–515. [PubMed] [Google Scholar]
- 45.Abramovitz I, Tagger M, Tamse A, Metzger Z. The effect of immediate vs. delayed post space preparation on the apical seal of a root canal filling: a study in an increased-sensitivity pressure-driven system. J Endod. 2000;26(8):435–439. doi: 10.1097/00004770-200008000-00001. [DOI] [PubMed] [Google Scholar]
- 46.Ashraf H, Joolaey J, S. JA. Effect of immediate and delayed post space preparation on apical dye leakage using two different sealers. Journal of Dental School Shahid Beheshti University of Med Sci 2003;20(4):558-67.
- 47.Bodrumlu E, Tunga U, Alaçam T. Influence of immediate and delayed post space preparation on sealing ability of resilon. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(6):e61–ee4. doi: 10.1016/j.tripleo.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 48.Fallah Rastegar A, Ghaziani P, Zarei M. The effect of immediate and delayed preparation of post space using AH26 and Roth sealers on apical leakage. J Mashhad Dental School. 2004;28(Issue):77-82.
- 49.Javidi M, Sedigh Shams M, Mesgarani A. Apical Leakage in Obturated Canals Using two Different Sealers after Immediate and Delayed Post Space Preparation. J Dent. 2007;8(2):48–55. [Google Scholar]
- 50.Sadeghi S, Kangarlou A. Comparison of sealing ability of lateral and vertical techniques in two different post space preparations. Iranian Endodontic J (IEJ) 2007;2(2):61–64. [Google Scholar]
- 51.Shahi S, Hoseini M. An in vitro study of the effect of immediate and delayed post space preparation with two different methods on apical seal. Med J Tabriz Univ Med Sci. 2007;28(4):71–75. [Google Scholar]
- 52.Solano F, Hartwell G, Appelstein C. Comparison of apical leakage between immediate versus delayed post space preparation using AH Plus sealer. J Endod. 2005;31(10):752–754. doi: 10.1097/01.don.0000158241.96250.0e. [DOI] [PubMed] [Google Scholar]
- 53.Bourgeois RS, Lemon RR. Dowel space preparation and apical leakage. J Endod. 1981;7(2):66–69. doi: 10.1016/S0099-2399(81)80244-0. [DOI] [PubMed] [Google Scholar]
- 54.Dickey DJ, Harris GZ, Lemon RR, Luebke RG. Effect of post space preparation on apical seal using solvent techniques and Peeso reamers. J Endod. 1982;8(8):351–354. doi: 10.1016/S0099-2399(82)80192-1. [DOI] [PubMed] [Google Scholar]
- 55.Fan B, Wu MK, Wesselink P. Coronal leakage along apical root fillings after immediate and delayed post space preparation. Dent Traumatol. 1999;15(3):124–126. doi: 10.1111/j.1600-9657.1999.tb00768.x. [DOI] [PubMed] [Google Scholar]
- 56.Karapanou V, Vera J, Cabrera P, White RR, Goldman M. Effect of immediate and delayed post preparation on apical dye leakage using two different sealers. J Endod. 1996;22(11):583–585. doi: 10.1016/S0099-2399(96)80025-2. [DOI] [PubMed] [Google Scholar]
- 57.Madison S, Zakariasen KL. Linear and volumetric analysis of apical leakage in teeth prepared for posts. J Endod. 1984;10(9):422–427. doi: 10.1016/S0099-2399(84)80263-0. [DOI] [PubMed] [Google Scholar]
- 58.Moon E-W, Lee I-S, Choi G-W. The effect of post-space preparation time on the apical seal of endodontically treated teeth. Restorative Dentistry Endodontics. 1988;13(1):151–158. [Google Scholar]
- 59.Portell FR, Bernier WE, Lorton L, Peters DD. The effect of immediate versus delayed dowel space preparation on the integrity of the apical seal. J Endod. 1982;8(4):154–160. doi: 10.1016/S0099-2399(82)80211-2. [DOI] [PubMed] [Google Scholar]
- 60.Rybicki R, Zillich R. Apical sealing ability of Thermafil following immediate and delayed post space preparations. J Endod. 1994;20(2):64–66. doi: 10.1016/S0099-2399(06)81182-9. [DOI] [PubMed] [Google Scholar]
- 61.Saunders W, Saunders E, Gutmann J, Gutmann M. An assessment of the plastic Thermafil obturation technique: Part 3 The effect of post space preparation on the apical seal. Int Endod J. 1993;26(3):184–189. doi: 10.1111/j.1365-2591.1993.tb00791.x. [DOI] [PubMed] [Google Scholar]
- 62.Dias LL, Giovani AR, Silva Sousa YT, Vansan LP, Alfredo E, Sousa-Neto MD, et al. Effect of eugenol-based endodontic sealer on the adhesion of intraradicular posts cemented after different periods. J Appl Oral Sci. 2009;17(6):579–583. doi: 10.1590/S1678-77572009000600008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lan YY, Huang H-x, Fan L-y, Pu L, Liu M, Sun L-b. Influence of immediate or delayed post space preparation on the apical sealing ability of different root canal sealers. Chinese Journal of Tissue Engineering. Research. 2017;21(10):1483. [Google Scholar]
- 64.Kalra PK, Mulay S, Aggarwal S. Comparison of apical leakage between immediate versus delayed post space preparation using two resin sealers. J Int Clin Dental Res Organ. 2009;1(2):57. [Google Scholar]
- 65.Lan YY, Pu L, Huang H-x, Fan L-y, Liu M, Sun L-b. Effects of immediate versus delayed post space preparation on coronal microleakage using different filling materials. Chinese Journal of Tissue Engineering. Research. 2016;20(25):3757. [Google Scholar]
- 66.Nikhil V, Khanna P, Gupta D. Influence of timing of post space preparation and presence/absence of intracanal barrier on coronal bacterial microleakage: An ex-vivo study. Indian J Stomatol. 2011;2(2):102. [Google Scholar]
- 67.Jalalzadeh SM, Mamavi A, Abedi H, Mashouf RY, Modaresi A, Karapanou V. Bacterial microleakage and post space timing for two endodontic sealers: an in vitro study. J Mass Dent Soc. 2010;59(2):34–37. [PubMed] [Google Scholar]
- 68.Sharma AK, Sharma PP, Mandhotra P, Bhutia KS, Rathee M, Sawhney K. Assessment of effect of post space preparation on the sealing ability of mineral trioxide aggregate and gutta-percha. Group. 2020;18(11.57) 90.25-14.23.
- 69.Frough Reyhani M, Rahimi S, Fathi Z, Shakouie S, Salem Milani A, Soroush Barhaghi MH, et al. Evaluation of Antimicrobial Effects of Different Concentrations of Triple Antibiotic Paste on Mature Biofilm of Enterococcus faecalis. J Dent Res Dent Clin Dent Prospects. 2015;9(3):138–143. doi: 10.15171/joddd.2015.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grecca FS, Rosa AR, Gomes MS, Parolo CF, Bemfica JR, Frasca LC, et al. Effect of timing and method of post space preparation on sealing ability of remaining root filling material: in vitro microbiological study. J Can Dent Assoc. 2009;75(8):583. [PubMed] [Google Scholar]
- 71.Lyons W, Hartwell G, Stewart J, Reavley B, Appelstein C, Lafkowitz S. Comparison of coronal bacterial leakage between immediate versus delayed post-space preparation in root canals filled with Resilon/Epiphany. Int Endod J. 2009;42(3):203–207. doi: 10.1111/j.1365-2591.2008.01501.x. [DOI] [PubMed] [Google Scholar]
- 72.Dhaded N, Dhaded S, Patil C, Patil R, Roshan JM. The Effect of Time of Post Space Preparation on the Seal and Adaptation of Resilon-Epiphany Se & Gutta-percha-AH Plus Sealer- An Sem Study. J Clin Diagn Res. 2014;8(1):217–220. doi: 10.7860/JCDR/2014/6787.3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vilas-Boas DA, Grazziotin-Soares R, Ardenghi DM, Bauer J, de Souza PO, de Miranda Candeiro GT, et al. Effect of different endodontic sealers and time of cementation on push-out bond strength of fiber posts. Clin Oral Investig. 2018;22(3):1403–1409. doi: 10.1007/s00784-017-2230-z. [DOI] [PubMed] [Google Scholar]
- 74.Vano M, Cury AH, Goracci C, Chieffi N, Gabriele M, Tay FR, et al. The effect of immediate versus delayed cementation on the retention of different types of fiber post in canals obturated using a eugenol sealer. J Endod. 2006;32(9):882–885. doi: 10.1016/j.joen.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 75.Vano M, Cury A, Goracci C, Chieffi N, Gabriele M, Tay F, et al. Retention of fiber posts cemented at different time intervals in canals obturated using an epoxy resin sealer. J Dent. 2008;36(10):801–807. doi: 10.1016/j.jdent.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 76.Boone KJ, Murchison DF, Schindler WG, Walker WA., 3rd Post retention: the effect of sequence of post-space preparation, cementation time, and different sealers. J Endod. 2001;27(12):768–771. doi: 10.1097/00004770-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 77.Machado MBM, Morgan LFSA, Gomes GM, Vasconcellos WA, Cardoso FP, de Castro AR. Effects of immediate and delayed intraradicular preparation on bond strength of fiber posts. Indian J Dent Res. 2015;26(3):244. [DOI] [PubMed]
- 78.Machado MB, Alves Morgan LF, Gomes GM, Vasconcellos WA, Cardoso FP, Albuquerque RC. Effects of immediate and delayed intraradicular preparation on bond strength of fiber posts. Indian J Dental Res. 2015;26(3):244–247. doi: 10.4103/0970-9290.162879. [DOI] [PubMed] [Google Scholar]
- 79.dos Reis-Prado AH, Abreu LG, Tavares WLF, da Cunha Peixoto IF, Viana ACD, de Oliveira EMC, et al. Comparison between immediate and delayed post space preparations: a systematic review and meta-analysis. Clin Oral Investig. 2021;1-24. [DOI] [PubMed]
- 80.Jafari F, Jafari S. Importance and methodologies of endodontic microleakage studies: A systematic review. J Clin Experiment Dentistry. 2017;9(6):e812. doi: 10.4317/jced.53604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dangra Z, Gandhewar M. All about Dowels-A review part I. Considerations before Cementation. J Clin Diagnostic Res. 2017;11(8):ZG06. doi: 10.7860/JCDR/2017/26472.10518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Özcan M, Volpato CAM. Current Perspectives on Dental Adhesion (3): Adhesion to Intraradicular Dentin: Concepts and Applications. Jap Dental Sci Rev. 2020. [DOI] [PMC free article] [PubMed]
- 83.Bohrer T, Fontana P, Rocha R, Kaizer O. Post-Space Treatment Influences the Bond Strength In Endodontically Treated Teeth: A Systematic Review and Meta-Analysis of In Vitro Studies. Oper Dent. 2021;46(3):E132–EE57. doi: 10.2341/19-277-LIT. [DOI] [PubMed] [Google Scholar]
- 84.Kosan E, Prates-Soares A, Blunck U, Neumann K, Bitter K. Root canal pre-treatment and adhesive system affect bond strength durability of fiber posts ex vivo. Clin Oral Investig. 2021;25(11):6419–6434. doi: 10.1007/s00784-021-03945-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.