Abstract
Background:
Few brief suicide risk screening instruments are validated for use in both adult and pediatric medical populations. Using the pediatric Ask Suicide-Screening Questions (ASQ) development study as a model, this study aimed to determine whether the ASQ is a valid suicide risk screening instrument for use among adults medical patients, as well as to evaluate a set of other potential screening questions for use in adults.
Methods:
Adult patients hospitalized on inpatient medical/surgical units from four hospitals were recruited to participate in a cross-sectional instrument validation study. The four-item ASQ and other candidate items were compared against the 25-item, previously validated Adult Suicidal Ideation Questionnaire (ASIQ), as the criterion standard.
Results:
A total of 727 adult medical inpatients completed the screening process. As compared to the ASIQ, the ASQ performed best among the full set of candidate items, demonstrating strong psychometric properties, with a sensitivity of 100% (95% CI = 90% - 100%), a specificity of 89% (95% CI = 86% - 91%), and a negative predictive value of 100% (95% CI = 99% - 100%). A total of 4.8% (35/727) of the participants screened positive for suicide risk based on the standard criterion ASIQ.
Conclusions:
The ASQ is a valid and brief suicide risk screening tool for use among adults. Screening medical/surgical inpatients for suicide risk can be done effectively for both adult and pediatric patients using this brief, primary screener.
Keywords: suicide risk screening, adult medical inpatients, instrument validation study, medical settings
Introduction
Suicide is the 10th leading cause of death in the United States, with more than 46,000 deaths by suicide among adults in 2018.1 Most who attempt and die by suicide are seen by a medical provider for non-psychiatric reasons in the months prior to their attempt,2 placing non-mental health settings in a critical position to identify individuals at risk for suicide. Nearly 95% of suicide attempters visited a medical provider within a year prior to an attempt, of which 60% of visits were within just one month of an attempt.3 Among individuals who died by suicide, 83% had a health care visit in the year prior to death.4 These patients often report somatic complaints, but unless directly asked, they typically will not disclose psychiatric symptoms.5
Individuals with medical problems are at elevated risk for suicidal thoughts and behaviors6–8 further establishing medical settings as important venues for detecting suicide risk. Hospital suicides are one of the five most common Sentinel Events reported to The Joint Commission, with 14% of these suicides occurring in non-behavioral health care units.9 In 2016, The Joint Commission issued Sentinel Event Alert 56, recommending screening all patients, including medical patients, for suicidal risk using a brief tool that is standardized and evidence-based.10 After a patient screens positive, a more in depth assessment of suicide risk is necessary. A three-tiered suicide risk screening clinical pathway developed for use among medical patients can be used to effectively and efficiently manage positive screens.11 Following these recommendations, more medical settings are beginning to implement universal suicide risk screening programs.12,13
It is important to utilize validated, population-specific and site-specific instruments when screening, however very few suicide risk screening tools have been validated on medical patients.14 In addition, not all tools created for adults are valid for use with youth, and vice versa. Many hospitals currently use separate tools to screen adult and youth medical patients which can create confusion for frontline staff hospital as well as for medical record informatics who have to juggle and track two different tools and age ranges. The four-item Ask Suicide-Screening Questions (ASQ) was one of the first suicide risk screening tools developed specifically for young medical patients in the emergency department, using a sample of 10 to 21 year olds.15 Given its brevity and ease of use, some hospitals have been using it for adults without difficulty. Using the ASQ development study15 as a model, this study aimed to determine whether the ASQ is a valid suicide risk screening instrument for use with adult medical patients, as well as to evaluate a set of other potential screening questions for use in adults.
Material and methods
Study Settings and Sample
Data collection occurred between June 2014 and October 2019. A convenience sample of adult medical/surgical inpatients was enrolled in this study. Participants were enrolled at four study sites located throughout the United States: the National Institutes of Health Clinical Center (NIHCC), Rhode Island Hospital (RIH), Walter Reed National Military Medical Center (WRNMMC), and John Peter Smith Health Network (JPS). Patients were eligible to participate if they were admitted to designated inpatient medical units, 18 years or older, capable of providing consent, English-speaking, and not previously enrolled in this study. Exclusion criteria included: severe cognitive impairment (e.g. patients with delirium), being under the age of 18, non-English speaking, previous enrollment in the study, and imminent discharge. Inpatient medical units were selected by each hospital, with the hopes of including typical medical/surgical patients, and for ease of data collection. Units with patients with psychiatric presenting chief complaints were avoided. No individuals were excluded from the study based on sex, race, or ethnicity.
Measures
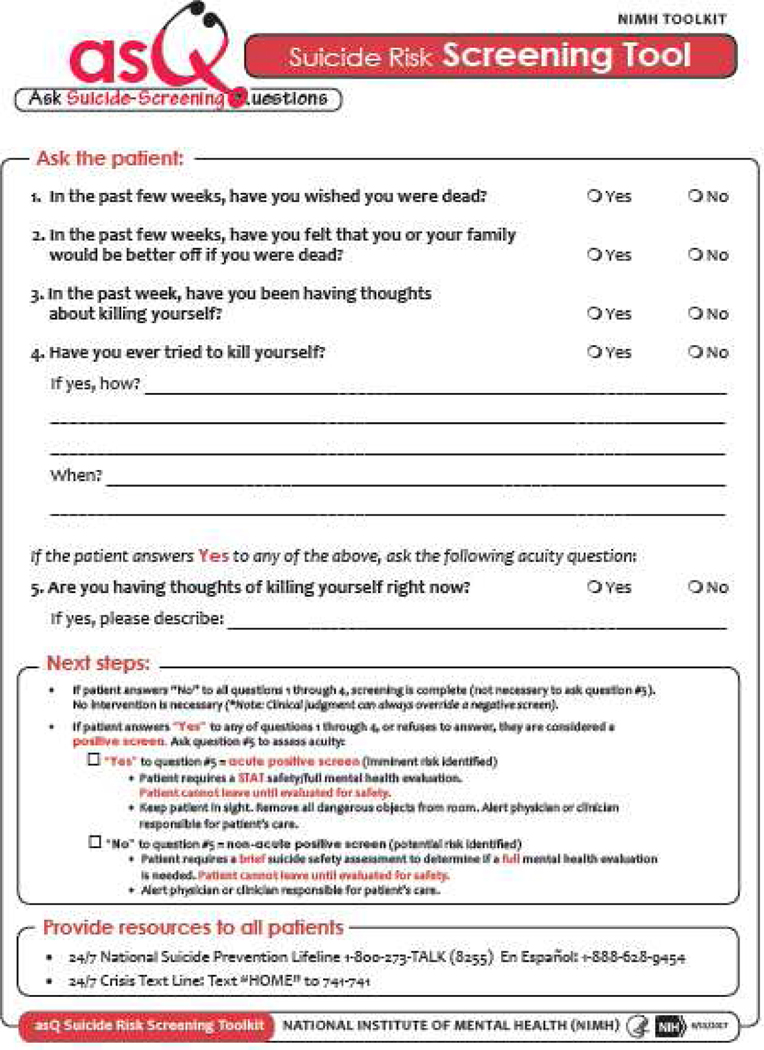
The Ask Suicide-Screening Questions (ASQ)15 is a 4-item self-report suicide risk screening measure (Figure 1) that assess recent suicidal ideation and lifetime suicidal behaviors. The ASQ has strong psychometric properties among youth presenting to the ED, with a sensitivity of 96.9%, a specificity of 87.6%, and a negative predictive value of 99.7% among pediatric patients presenting with medical chief complaints.15 The ASQ has also been found to have predictive validity for 3-month suicidal behavior post ED discharge.16 For this validation study, the ASQ was embedded into a list of 20 candidate items. Of note, the tool was not administered intact, but rather as items randomly dispersed among the candidate items.
Figure 1: Ask Suicide-Screening Questions.
https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/asq-tool/screening-tool_155867.pdf (public domain)
A list of 20 potential items thought to be appropriate for screening adult medical patients for suicide risk was generated to be candidate items for a final shorter tool, replicating the process originally used to develop the ASQ.15 These candidate questions were drawn from several sources, including published literature about adult suicide risk, interviews with senior mental health researchers, clinicians, and survey methodologists, and empirically validated risk factors and warning signs associated with adult suicide attempts. These 20 Yes/No questions included all items from the ASQ tool.15 Participants were deemed positive for suicide risk on this measure if they endorsed any critical candidate items (6, 7, 13, 15, 16, 17, 18, 19, and 20) that indicated need for further evaluation, which then triggered a brief suicide safety assessment – these are referred to as “trigger” items.
The Adult Suicide Ideation Questionnaire (ASIQ)17,18 is a 25-item measure to assess suicidal ideation among adults. Participants rate the frequency of their suicidal thoughts in the past month. Items are scored on a 7-point Likert scale, ranging from 0 (“never had this thought”) to 6 (“almost every day”). Scores range from 0 to 150. The ASIQ has been validated in several populations, with subject’s age ranging from 18 to 88 years, and has high internal consistency, with Cronbach’s alpha coefficient ranging from 0.96 to 0.98.17,18 The ASIQ has been highly correlated with clinician-evaluated suicide risk as measured by the suicide item on the Hamilton Rating Scale for Depression (r=.77) and able to discriminate between those who have and those who have not tried to kill themselves in the past.17,18 The ASIQ is included in this study as the criterion standard measure of suicide ideation. A cutoff score of 31 or above was considered “positive” for suicide risk in the present study.
Procedures
During designated data collection days, hospital unit charge nurses provided data collectors with the patient census for pre-selected medical/surgical units and all eligible participants were approached for study enrollment. Informed consent was obtained directly from all participants. After the consent process, each participant completed a battery of self-report questionnaires administered orally, including the 20 candidate items, the ASIQ, and a demographics questionnaire. The order of administering the candidate items and the ASIQ were rotated to avoid order effects. Those who screened positive on the candidate items and/or ASIQ received a brief suicide safety assessment by a trained clinician. A full psychiatric consultation was done when clinically indicated. This study was approved by the institutional review boards at the National Institute of Mental Health, RIH, WRNMMC, and JPS.
Theory/calculation
In order to measure the validity of each of the candidate items, chance-correlated Cohen’s kappa statistics, the C statistic, which represents the area under the receiver operating characteristic curve (AUC), and log likelihood ratio (LR+ and LR-) were estimated to determine the agreement and predictive ability of each candidate item and the risk for suicide as assessed by the ASIQ. The LR+ indicates how much more likely the positive test results is to occur for participants with suicide risk, compared to those without suicide risk, while the LR-signifies how much less likely the negative test result is to occur in a participant with suicide risk than in a participant without suicide risk. Logistic regression models were constructed to examine the ability of different combinations of the candidate items to predict the ASIQ-assessed suicide risk. Stepwise regression and best subsets regression were data-driven methods used to determine the best-fitting models. Only those candidate items with kappa of 0.40 or greater were considered in the models. An a priori decision was made to also evaluate the psychometric validity of a model with the four candidate items that make up the ASQ. As in the ASQ development paper,15 the item assessing past suicidal behavior was retained in all models (candidate item #7: “Have you ever tried to kill yourself?). Studies have shown that previous suicide attempts remain the most potent risk factor for future suicidal behavior.19
Standard validity statistics were calculated to assess the diagnostic accuracy of each model including sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV), likelihood ratios (LRs), AUC, and kappa statistic (using ASIQ as ‘true’ test). Ninety-five percent confidence intervals for the sensitivity, specificity, PPV, and NPV were estimated using exact binomial methods. Due to the clinical importance of limiting the number of individuals at risk for suicide being classified falsely as negatives, the number of participants at risk for suicide as assessed by the ASIQ (‘true’ test) who would have been undetected by each model was calculated.
In selecting the final model that maintained strong psychometric properties, we sought to choose a parsimonious model that maximized sensitivity, specificity and NPV, such that the minimum number of suicide positive patients would be misclassified as negatives while ensuring clinicians would not be overburdened managing false-positive patients.
The sample size calculation was based on an estimated suicide risk screen positive rate of 4%,12,20 with 97% sensitivity,15 88% specificity,15 and a two-tailed alpha of .05. A minimum of 497 participants was needed to achieve 7.5% precision (95% confidence interval) around the estimates of sensitivity and specificity. Buderer’s formula for calculating sample size was used to make these estimates.21 Data analyses were conducted using SAS software version 9.4.22
Results
Across the four study sites, 995 eligible patients were approached to participate in the study. A total of 740 patients provided consent and enrolled in the study, resulting in a 74.4% enrollment rate. Twelve participants withdrew from the study after data collection began and one was excluded based on incomplete responses, resulting in a final sample of 727 participants. The sample was 53.4% male (388/727), 61.8% White (449/727), and had a mean age of 50.2 years (SD=16.3, range 18–93). Most participants (54.9%; 399/727) were admitted to the hospital for general medical conditions (e.g. fever, stomach pain), followed by general surgery (24.2%; 176/727), injury (5.5%; 40/727), general medical conditions/psychiatric reasons (1.0%; 7/727), and psychiatric reasons (0.4%; 3/727). The reason for admittance was unknown for 14.0% (102/727) of participants. A total of 281 (38.7%; 281/727) participants reported having been diagnosed with at least one mental health issue in the past, by either a primary care provider or a mental health professional, with some participants reporting multiple mental health diagnoses. The two most common reported mental health diagnoses were depression (24.8%; 180/727) and anxiety (22.0%; 160/727). Demographic characteristics of study participants are in Table 1.
Table 1:
Participant demographics and suicide risk by study site
| Total Sample N=727 |
NIH CC N=198; 27.2% |
RIH N=178; 24.5% |
WRNMMC N=176; 24.2% |
JPS N=175; 24.1% |
|
|---|---|---|---|---|---|
| Gender | |||||
| Male | 388 (53.4%) | 88 (44.4%) | 92 (51.7%) | 113 (64.2%) | 95 (54.3%) |
| Female | 337 (46.4%) | 110 (55.6%) | 86 (48.3%) | 61 (34.7%) | 80 (45.7%) |
| Unknown | 2 (0.2%) | 0 (0.0%) | 0 (0.0%) | 2 (1.1%) | 0 (0.0%) |
| Race or ethnicity | |||||
| White | 449 (61.8%) | 143 (72.2%) | 125 (70.2%) | 100 (56.8%) | 81 (46.3%) |
| Black | 140 (19.3%) | 25 (12.6%) | 15 (8.4%) | 44 (25.0%) | 56 (32.0%) |
| Hispanic/Latino | 70 (9.6%) | 13 (6.6%) | 8 (4.5%) | 16 (9.1%) | 33 (18.9%) |
| Asian | 20 (2.8%) | 12 (6.1%) | 2 (1.1%) | 4 (2.4%) | 2 (1.1%) |
| Multiple Races | 20 (2.8%) | 4 (2.0%) | 10 (5.6%) | 5 (2.8%) | 1 (0.6%) |
| Other | 25 (3.4%) | 1 (0.5%) | 17 (9.6%) | 5 (2.8%) | 2 (1.1%) |
| Unknown | 3 (0.4%) | 0 (0.0%) | 1 (0.6%) | 2 (1.1%) | 0 (0.0%) |
| Mean Age (SD) | 50.1 (16.3) | 49.3 (13.4) | 51.8 (18.5) | 47.1 (19.3) | 53.1 (12.3) |
| Positive ASIQ screen rate | 35 (4.8%) | 6 (3.0%) | 11 (6.2%) | 4 (2.3%) | 14 (8.0%) |
| Suicide attempts | 66 (9.1%) | 11(5.6%) | 18 (10.1%) | 4 (2.3%) | 33 (18.9%) |
| Type of hospital | ----- | Research | Teaching | Military | Teaching |
| Total hospital beds | ----- | 200 | 719 | 244 | 573 |
NIH CC = National Institutes of Health Clinical Center, RIH = Rhode Island Hospital, WRNMMC = Walter Reed National Military Medical Center, JPS = John Peter Smith Health Network
The range for chance-corrected agreement between individual candidate items and ASIQ determined suicide risk was from a κ of .71 (95% CI = 0.59–0.82) to .05 (95% CI = −0.05–0.15) (See Table 2). The validity statistics of the six best-fitting combinations of candidate items, including the 4-item ASQ model, are shown in Table 3. The two models with 4-item combinations maximized sensitivity, specificity and NPV. Beyond the two best-fitting 4-item models, the subsequent 5-item best-fitting models had limited improvement in psychometric properties. When comparing the AUC for the two 4-item models, they were substantially in agreement with the ASIQ (‘true’ test) and there was no statistically significant difference between the ASQ model (AUC=0.944; 95% CI = 0.93–0.96) and the 4-item best-fitting model (AUC=0.941; 95% CI = 0.93–0.96). These two 4-item models had equivalent values in other validity statistics as well. Both models detected all positives suicide risk screens, as assessed by the ASIQ. The best-fitting models with three or fewer items had superior specificity rates to the ASQ model, but poorer sensitivity rates, each misclassifying at least one participant as negative. Given that the psychometric measures between the two 4-item models were almost identical, we selected the ASQ, a tool that many clinicians are already familiar with for youth, as the optimal model for a suicide risk screening tool for adult medical inpatients.
Table 2:
Chance-Corrected Agreement Between Candidate Screening Items and the ASIQ for the Assessment of Risk for Suicide (N=727)
| Item No. | Question | Yes, % |
LR+ | LR− | kappa | AUC | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Est | 95% CI | Est | 95% CI | Est | 95% CI | Est | 95% CI | |||
| 1 | In the past few weeks, have you felt so nervous or worried in a way that felt unbearable, like you couldn’t stand it anymore? |
22.6 | 4.47 | 3.57, 5.37 | 0.17 | 0.03, 031 | 0.25 | 0.17, 0.33 | 0.82 | 0.76, 0.89 |
| 2 | In the past few weeks, have you felt hopeless, like things would never get better? | 25.3 | 4.51 | 3.82, 5.20 | 0.04 | −0.03, 0.10 | 0.26 | 0.19, 0.33 | 0.87 | 0.84, 0.91 |
| 3 | In the past few weeks, have you felt so sad or depressed in a way that felt unbearable, like you couldn’t stand it anymore? | 17.7 | 6.07 | 4.70, 7.44 | 0.16 | 0.03, 0.29 | 0.32 | 0.23, 0.41 | 0.85 | 0.78, 0.92 |
| 4 | Do you have close friends or family members that you can go to when you have serious problem? (REVERSE CODED) | 92.7 7.3 | 4.03 | 1.48, 6.58 | 0.79 | 0.64, 0.95 | 0.16 | 0.04, 0.27 | 0.60 | 0.52, 0.68 |
| 5 | Do you feel like you might as well give up because you can’t make things better for yourself? | 5.5 | 16.63 | 7.98, 25.27 | 0.49 | 0.31, 0.66 | 0.46 | 0.31, 0.60 | 0.74 | 0.65, 0.83 |
| 6b | In the past few weeks, has your medical condition led you to seriously consider killing yourself? | 2.8 | 59.23 | 2.66, 115.79 | 0.58 | 0.41, 0.74 | 0.53 | 0.37, 0.69 | 0.71 | 0.62, 0.79 |
| 7a,b,c | Have you ever tried to kill yourself? | 9.1 | 5.17 | 2.65, 7.68 | 0.66 | 0.49, 0.83 | 0.22 | 0.11, 0.34 | 0.67 | 0.58, 0.76 |
| 8 | In the past few weeks, have you been more irritable or grouchier than usual? | 44.7 | 1.88 | 1.46, 2.16 | 0.39 | 0.15, 0.63 | 0.07 | 0.04, 0.11 | 0.67 | 0.60, 0.75 |
| 9 | In the past few weeks, have you felt like you are a failure? | 16.4 | 6.75 | 5.16, 8.34 | 0.16 | 0.03, 0.29 | 0.35 | 0.25, 0.45 | 0.87 | 0.81, 0.93 |
| 10 | Do you or anyone in your life think you have a problem with drugs or alcohol? | 10.0 | 4.55 | 2.38, 6.73 | 0.67 | 0.49, 0.84 | 0.20 | 0.09, 0.32 | 0.67 | 0.58, 0.76 |
| 11 | Do you have chronic pain that affects your daily life? | 49.9 | 1.60 | 1.30, 1.91 | 0.43 | 0.17, 0.70 | 0.06 | 0.02, 0.09 | 0.68 | 0.61, 0.75 |
| 12 | In the past few weeks, have you felt hopeless about your medical condition, like things would never get better? | 27.0 | 3.46 | 2.78, 4.15 | 0.22 | 0.06, 0.38 | 0.19 | 0.13, 0.26 | 0.78 | 0.71, 0.86 |
| 13b | In the past few weeks, have you thought that your life was so bad that you didn’t want to live anymore? | 7.3 | 27.05 | 15.35, 38.74 | 0.14 | 0.03, 0.26 | 0.68 | 0.56, 0.79 | 0.90 | 0.84, 0.97 |
| 14 | In the past few weeks, have you felt like a burden on others? | 33.1 | 2.60 | 2.08, 3.13 | 0.29 | 0.10, 0.48 | 0.13 | 0.08, 0.18 | 0.77 | 0.70, 0.83 |
| 15b,c | In the past few weeks, have you wished you were dead? | 7.2 | 22.36 | 12.72, 31.99 | 0.23 | 0.09, 0.37 | 0.61 | 0.49, 0.74 | 0.87 | 0.79, 0.94 |
| 16b,c | In the past few weeks, have you felt that you or your family would be better off if you were dead? | 6.5 | 28.29 | 14.78, 41.79 | 0.23 | 0.09, 0.37 | 0.66 | 0.53, 0.78 | 0.87 | 0.80, 0.95 |
| 17b | In the past month, have you had thoughts about suicide? | 6.1 | 37.11 | 17.57, 56.65 | 0.20 | 0.07, 0.33 | 0.71 | 0.59, 0.82 | 0.88 | 0.80, 0.95 |
| 18b,c | In the past week, have you been having thoughts about killing yourself? | 2.2 | 83.18 | − 17.62, 183.97 | 0.64 | 0.48, 0.80 | 0.48 | 0.32, 0.65 | 0.71 | 0.62, 0.80 |
| 19b | Are you having thoughts of killing yourself right now? | 0.1 | - | - | 0.97 | 0.88, 1.06 | 0.05 | −0.05, 0.15 | - | - |
| 20a,b | Have you ever made a suicide attempt? | 9.5 | 5.34 | 2.87, 7.87 | 0.63 | 0.46, 0.81 | 0.24 | 0.12, 0.36 | 0.69 | 0.60, 0.78 |
Patients who answered “yes” to items 7 and 20 were only considered positive if the attempt was in the past 10 years.
Trigger items.
ASQ items.
Table 3:
Predictive Abilities for the Best-Fitting Combinations of Screening Questions (N=727)
| Model | Screening Questions | Rate (95% CI) | Rate (95% CI) | LR (95% CI) | # of ASIQ positive cases misclassified as no risk | ||||
|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | LR+ | LR− | AUC | |||
| 5 | 7,13,15,16,17 | 1.00 (0.90 - 1.00) | 0.88 (0.85 - 0.90) | 0.30 (0.22 - 0.38) | 1.00 (0.99 - 1.00) | 7.89 (6.30, 9.48) | 0.02 (−0.03, 0.06) | 0.938 (0.93 - 0.95) | 0 |
| 4 | 7,13, 16,17 | 1.00 (0.90 - 1.00) | 0.88 (0.86 - 0.91) | 0.31 (0.23 - 0.40) | 1.00 (0.99 - 1.00) | 8.38 (6.63, 10.12) | 0.02 (−0.03, 0.06) | 0.941 (0.93 - 0.95) | 0 |
| 3 | 7,16,17 | 0.97 (0.85 - 1.00) | 0.90 (0.87 - 0.92) | 0.33 (0.24 - 0.42) | 1.00 (0.99 - 1.00) | 9.16 (7.07, 11.25) | 0.05 (−0.03, 0.12) | 0.934 (0.90 - 0.96) | 1 |
| 2 | 7,17 | 0.89 (0.74 - 0.97) | 0.91 (0.89 - 0.93) | 0.35 (0.25 - 0.45) | 0.99 (0.98 - 1.00) | 10.05 (7.33, 12.76) | 0.13 (0.02, 0.25) | 0.901 (0.85 - 0.95) | 4 |
| 1 | 7 | 0.39 (0.23 - 0.57) | 0.92 (0.90 - 0.94) | 0.21 (0.12 - 0.33) | 0.97 (0.95 - 0.98) | 5.17 (2.67, 7.66) | 0.66 (0.48, 0.83) | 0.657 (0.58 - 0.74) | 22 |
| ASQ | 7,15,16,18 | 1.00 (0.90 - 1.00) | 0.89 (0.86 - 0.91) | 0.32 (0.23 - 0.41) | 1.00 (0.99 - 1.00) | 8.81 (6.93, 10.69) | 0.02 (−0.03, 0.06) | 0.944 (0.93 - 0.96) | 0 |
In this adult sample, using the ASIQ as a gold standard, the ASQ had a sensitivity (true positive rate) of 100% (95% CI = 0.90–1.00), indicating that the ASQ identified all participants who screened positive on the ASIQ. The specificity of 89% (95% CI = 0.86–0.91) indicates the percentage of adults who were negative on the ASIQ and were correctly identified as such on the ASQ (true negatives). The NPV was 100% (95% CI = 0.99–1.00) and the PPV was 32% (95% CI = 0.23–0.41). The LR+ was 8.81 (95% CI = 6.93, 10.69) and the LR- was 0.02 (95% CI = −0.03, 0.06). Finally, the AUC was 94.4% (95% CI = 0.93–0.96), indicating substantial agreement between the ASIQ and the ASQ for detecting elevated suicide risk.
A total of 4.8% (35/727) of the participants screened positive for suicide risk based on the standard criterion ASIQ. Positive screen rates on the ASIQ varied by site, with screen positive rates of 2.3% (4/176) at WRNMMC, 3.0% (6/198) at NIH, 6.2% (11/178) at RIH, and 8.0% (14/175) at JPS. Only one participant in the full sample (0.1%; 1/727), endorsed current suicidal thoughts, indicating imminent risk for suicide. Sixty-six participants (9.1% of total sample) reported a previous suicide attempt when asked “Have you ever tried to kill yourself?”. Notably, 77.3% (51/66) of the reported most recent suicide attempts had occurred more than three years ago.
Discussion
The ASQ is a valid screening tool for detecting suicide risk among adult medical inpatients. This study aimed to determine the best possible combination of items for screening adult medical patients for suicide risk. Several different models were tested. Compared to other best-fitting models, the four-item ASQ demonstrated strong psychometric ability, with the least number of questions, to accurately detect suicide risk among adult medical patients. Though another 4-item model had similar psychometric properties to the ASQ, a central aim of this study was to not only determine the best-fitting model but also to ascertain whether the ASQ was a viable screening tool for adult medical patients. The psychometric properties of the ASQ proved to be robust for this adult sample, surpassing even the sound psychometric properties found in the sample of pediatric emergency department patients for which the ASQ was initially developed.15
The content validity of the ASQ is strong, as the four items assess the major components of suicide risk factors. Three questions focus on passive and active suicidal ideation, burdensomeness, and a final question assessing the most potent risk factor for future suicidal behavior: a history of suicide attempts. The ASQ had a sensitivity or true positive rate of 100%, showing that endorsing any of the four ASQ items identified each adult that the ASIQ deemed at clinically elevated risk. The high specificity rate of 89% helps to ensure that individuals who are not at elevated risk for suicide are correctly identified as such, minimizing the false positive rate. With this high true negative rate, screening for suicide risk with the ASQ is less likely to overburden hospital resources. The NPV rate of 100% is also essential in making sure that individuals who screen negative on the ASQ are not at elevated risk for suicide, according to their own self-report.
Positive suicide risk screens varied on the criterion standard ASIQ from 2.3% to 8.0% depending on the study site. The wide range of positive screen rates highlights that there may be additional factors that contribute to reporting of suicide risk; for example, the highest rates were from a hospital in a state and county with higher than average rates of suicide suggesting geographic and environmental contexts may play a role in detection rates (Texas/Tarrant County).1 The elevated rate at JPS demonstrates that suicide risk is prevalent and warrants universal screening.20 Conversely, the screen positive rate at WRNMMC was lower than expected. It is possible that military participants, some of whom were on active duty, were hesitant to endorse symptoms of psychiatric illness, as perceived stigma against mental health treatment is a known complexity of military healthcare.23
It is important to note the difference between screening and assessment, which are distinct. The screening tool is used to rapidly identify someone at risk, whereas the assessment confirms risk and guides next steps. Importantly, some patients who endorse a past suicide attempt on a screening tool may not be at high risk for self-harm since, notably, 77% of the reported most recent past suicide attempts had taken place more than three years beforehand. This is encouraging data for medical settings implementing screening programs, as a significant proportion of positive screens, due to reporting of distant past suicide attempts, may not require immediate action in the medical setting. In some cases, where the patient only endorses past suicidal behavior that occurred several years prior, providers may be able to focus on the primary presenting medical concern and then be sure to discharge the patient with information about local mental health resources.
Data from this study further underscores the importance of thoughtful responses to positive screens to prevent over-responding to patients who screen positive on a brief primary screener so the program does not unnecessarily overburden scarce mental health resources in the hospital. However, the data regarding a patient’s previous distress, behaviors and coping remains important clinical information about the patient. Furthermore, the majority of positive risk screens are identified as “non-acute.” Many do not require full safety precautions (1:1 sitter) and extensive psychiatric assessments. Instead, all positive screens should be followed up with a brief suicide safety assessment (BSSA) to determine the patient’s disposition and risk level, as well as the next steps that need to occur to ensure patient safety. In this sample, only one participant (0.1% of total sample) endorsed acute suicidal thoughts. This translated into only one patient of the 727 requiring immediate full safety precautions, such as 1:1 observations. These findings suggest that taking the time to not only identify adults at risk, but to invest in a brief suicide safety assessment to follow up on positive screens, will spare valuable resources on inpatient medical units. Clinicians trained to conduct the brief suicide safety assessment can also decide if the patient would benefit from a mental health referral either while in the hospital or post-discharge. Of note, if patients who screen non-acute positive choose to leave before they are assessed, this is considered in the same category as discharge “against medical advice,” as only acute positives are considered at imminent risk.
There are several limitations in this study. First, the study sites were all hospitals located in urban or suburban settings, thereby limiting generalizability to other inpatient settings in more rural areas. Second, the use of convenience sampling may have introduced a selection bias in that patients with suicidal thoughts may be more likely to agree to participate in the study, potentially inflating prevalence rates. However, the converse may also be true, as some patients with suicidal thoughts may be less likely to participate in the study due to not wanting to disclose their suicidal thoughts. Data from hospitals implementing screening on medical units, as opposed to research studies, have shown positive screen rates around 2–4%.12,13 In particular, the ASQ is used for universal screening of adult medical patients at the NIH CC with a positive screen rate less than 3%.13 Third, a fatigue effect may have been present due to repeatedly asking participants about suicidal thoughts. To limit this effect, we alternated the order in which the candidate items and ASIQ were administered. Fourth, study eligibility was limited to English-speaking patients, limiting generalizability to non-English speakers. Lastly, this study did not have longitudinal outcome data, preventing us from determining whether adults who endorsed items in the ASQ model were more likely to engage in suicidal behavior after being discharged from the hospital.
Hospital systems can employ iterative plan-do-study-act techniques24 of quality improvement projects (QIP) to adapt and implement their own versions of a three-tiered pathway.11 to help ensure feasible and effective adaptations of screening programs.13 Screening with brief interventions and care management has been shown to decrease suicide risk post discharge from ED settings.25 Future research should focus on how screening affects suicide and suicidal behavior, studying suicide risk clinical pathways adapted for adults in medical settings and developing brief interventions to attenuate suicide risk post-discharge for hospitalized adult medical patients.
Conclusion
In conclusion, the ASQ is a valid tool for use among adults. With this suicide risk screening tool, universal screening for medical patients of all ages can be effectively implemented with a single instrument across medical institutions for both youth and adult populations. Utilizing the medical setting to prevent suicide is a national goal of the Surgeon General,26 the National Action Alliance for Suicide Prevention,26 the NIMH,27 and the Joint Commission.10 In using the ASQ to screen both adults and youth, medical settings can be leveraged as valuable points of care in suicide prevention.
Acknowledgements:
The authors would like to acknowledge Annabelle Mournet for all her hard work on this manuscript. In addition, the authors want to thank the following people who were instrumental to the success of the study, including Daniel Powell, Adam Rosenfeld, Jeanne Radcliffe, Eliza Lanzillo, Asher Siegelman, Janet Frazier, Louis French, Mary Tipton, Jared Smith, Keenan Withers, Samantha Chalker, Rumsha Hafeez, Amanda Hayes, Olla Elbasheer, Apoorva Deshpande, Mehreen Kahn, the Leadership of the Directorate of Behavioral Health of WRNMMC, and all the patients, nurses, mental health and medical teams that helped make the study run smoothly. The views expressed in this abstract are those of the author and do not reflect the official policy of the National Institute of Mental Health, National Institute of Health, Department of Health and Human Services or Department of Army/Navy/Air Force, Department of Defense, or U.S. Government.
Funding:
This research was supported in part by the Intramural Research Program of the NIMH (Annual Report Number ZIAMH002922).
Footnotes
Declarations of Interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC National Center for Injury Prevention and Control: Web-based Injury Statistics Query and Reporting System (WISQARS). Available at: cdc.gov/injury/wisqars/index.html. Accessed February 28, 2020.
- 2.Luoma JB, Martin CE, Pearson JL: Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 2002;159:909–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmedani BK, Stewart C, Simon GE, et al. : Racial/Ethnic differences in health care visits made before suicide attempt across the United States. Medical Care 2015;53(5),430–435. doi: 10.1097/MLR.0000000000000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmedani BK, Simon GE, Stewart C, et al. : Health care contacts in the year before suicide death. J Gen Intern Med 2014;29:870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan YJ, Lee MB, Chiang HC, Liao SC: The recognition of diagnosable psychiatric disorders in suicide cases’ last medical contacts. Gen Hosp Psychiatry 2009;31:181–1843. doi: 10.1016/j.genhosppsych.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Fang F, Fall K, Mittleman MA, et al. : Suicide and Cardiovascular Death after a Cancer Diagnosis. The New England Journal of Medicine 2012;366:1310–1318. [DOI] [PubMed] [Google Scholar]
- 7.Furlanetto LM, Stefanello B: Suicidal ideation in medical patients: psychosocial and clinical correlates. General Hospital Psychiatry 2011;33:572–578. [DOI] [PubMed] [Google Scholar]
- 8.Qin P, Webb R, Kapur N, Sorensen HT: Hospitalization for physical illness and risk of subsequent suicide: A population study. Journal of Internal Medicine 2012. doi: 10.1111/j.1365-2796.2012.02572.x. [DOI] [PubMed]
- 9.The Joint Commission: Summary Data of Sentinel Events Reviewed by The Joint Commission. Available at: https://www.jointcommission.org/assets/1/18/Summary_4Q_2017.pdf. Accessed February 11, 2020.
- 10.The Joint Commission: Detecting and treating suicide ideation in all settings. Sentinel Event Alert Issue 56 2016;56:1–7. [PubMed] [Google Scholar]
- 11.Brahmbhatt K, Kurtz BP, Afzal KI, et al. : Suicide risk screening in pediatric hospitals: Clinical pathways to address a global health crisis. Psychosomatics 2019;60(1):1–9. doi: 10.1016/j.psym.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roaten K, Johnson C, Genzel R, Khan F, North C: Development and implementation of a universal suicide risk screening program in a safety-net hospital system. Jt Comm J Qual Patient Saf 2018;44(1):4–11. doi: 10.1016/j.jcjq.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 13.Snyder D, Jordan BA, Aizvera J, et al. : From pilot to practice: Implementation of a suicide risk screening program in hospitalized medical patients. Jt Comm J Qual Patient Saf, in submission. [DOI] [PMC free article] [PubMed]
- 14.Thom R, Hogan C, Hazen E: Suicide risk screening in the hospital setting: A review of brief validated tools. Psychosomatics 2020;61(1);1–7. doi: 10.1016/j.psym.2019.08.009 [DOI] [PubMed] [Google Scholar]
- 15.Horowitz LM, Bridge JA, Teach SJ, et al. : Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med 2012;166(12):1170–1176. doi: 10.1001/archpediatrics.2012.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Devylder JE, Ryan TC, Cwik M, et al. : Screening for suicide risk among youths with a psychotic disorder in a pediatric emergency department. Psychiatric Services 2019. doi: 10.1176/appi.ps.201900290 [DOI] [PubMed]
- 17.Reynolds WM: Psychometric characteristics of the adult suicidal ideation questionnaire in college students. J Pers Assess 1991a;56:289–307. doi: 10.1207/s15327752jpa5602_9 [DOI] [PubMed] [Google Scholar]
- 18.Reynolds WM: Adult suicidal ideation questionnaire: Professional manual. Psychological Assessment Resources 1991b.
- 19.Franklin JC, Riberio JD, Fox KR, et al. : Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull 2016;143(2):187–232. [DOI] [PubMed] [Google Scholar]
- 20.Horowitz LM, Snyder DJ, Ludi E, et al. : Ask suicide-screening questions to everyone in medical settings: The asQ’em Quality Improvement Project. Psychosomatics 2013;54(3):239–247. doi: 10.1016/j.psym.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buderer NMF: Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med 1996;3:895–900. [DOI] [PubMed] [Google Scholar]
- 22.SAS Institute Inc: SAS® 9.4 Statements: Reference. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 23.Cozza SJ, Fisher JE, Zhou J, et al. : Bereaved military dependent spouses and children: Those left behind in a decade of war (2001–2011). Mil Med 2014;182(3–4):e1684–1690. [DOI] [PubMed] [Google Scholar]
- 24.Deming WE: The New Economics for Industry, Government, Education. Cambridge, MA: Massachusetts Institute of Technology, Center for Advanced Engineering Study; 1993. [Google Scholar]
- 25.Miller IW, Camargo CA, Arias SA, et al. : Suicide prevention in an emergency department population: The ED-SAFE study. JAMA Psychiatry 2017;74(6):563–570. doi: 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Office of the Surgeon General (US), National Action Alliance for Suicide Prevention (US): 2012. national strategy for suicide prevention: Goals and objectives for action: A report of the U.S. Surgeon General and of the National Action Alliance for suicide prevention. Washington, DC: US Department of Health & Human Services; 2012. [PubMed] [Google Scholar]
- 27.National Institute of Mental Health: Suicide prevention: Next steps. Director’s Messages. Avaiable at: https://www.nimh.nih.gov/about/director/messages/2017/suicide-prevention-next-steps.shtml. Accessed on February 11, 2020.