Abstract
Purpose:
This study’s purpose was to compare changes in parent-reported pediatric oral health-related quality of life between children with early childhood caries (ECC) and children who were caries-free; the ECC children received surgical dental intervention between baseline and follow-up.
Methods:
A newly developed self-report instrument, the POQL, was administered to 501 parents of 2- to 8-year-old children (caries-free=315; ECC= 186) in hospital dental clinics in Columbus, Ohio, and Washington, D.C.
Results:
At baseline, ECC children were more likely to have fair or poor oral health and were rated as having more pain and trouble with physical, mental, and social functioning due to their teeth or mouth vs caries-free children (P<.001). At 6 and 12 months following dental treatment for ECC, there were significant improvements in parental ratings of their children’s oral health status and a significant reduction in problems reported with physical, mental, and social functioning (all P<.001).
Conclusions:
Compared with caries-free children, early childhood caries children were more likely to have worse questionnaire response scores and to experience greater negative impacts on physical, mental, and social functioning. Dental interventions in ECC children had a significant positive impact on parental ratings of their overall oral health and physical, mental, and social functioning.
Keywords: Infant oral health/early childhood caries, oral health services/access to care, public health/epidemiology
Dental caries continues to plague children in the United States; it is the most common disease of childhood. The National Health and Nutrition Examination Survey showed that, between 1999 and 2002, 41 % of 2- to 11-year-old children had primary tooth caries experience and 21 % had untreated primary tooth caries.1 Children from poor socioeconomic backgrounds and those of some racial and ethnic minorities are more likely to suffer from dental caries.1,2 Limited access to dental care and high treatment costs are serious public health issues that continue to affect these children today.
Early childhood caries (ECC) is a particularly severe dental condition affecting many young children in the United States and around the world. Dental caries is an infectious disease that, when left untreated, may result in systemic consequences. There is conflicting evidence regarding the specific sequelae of this link between dental/oral health with general health and well-being3,4 Clarke et al. found that young children with severe ECC (S-ECC) are more likely to suffer malnourishment problems such as iron deficiency and lower-than-ideal body weight.3 In another study by Thomas et al., however, children with severe caries showed only a slight nonsignificant increase in weight following oral rehabilitation treatment under general anesthesia.4 Parents in this same study reported a significant improvement in their children’s oral health-related quality of life (QOL) following dental treatment in the operating room.4
Several studies have addressed the effects that ECC can have on a child’s and their family’s QOL.4–9 In a recent study by Feitosa et al., more parents of children with severe caries (69%) reported via questionnaire that dental problems adversely affected their child’s QOL vs only 10% of parents of caries-free children.5 QOL factors frequently associated with poor oral health were: toothaches, having trouble eating certain foods, and missing schoo.5 Locker found a difference between high-vs low-income children regarding oral health-related QOL.9 Predictably, lower-income children suffered worse QOL due to problems with their teeth or mouth.9
Research studies also have investigated the potential positive effect of treatment intervention on QOL for children with severe caries.10–14 In a study with follow-up data for 37 ECC subjects, Filstrup et al. found evidence to support the theory that dental intervention may improve the QOL for ECC children10. Low et al. examined the effect of severe caries on the QOL of 77 young children (mean age=44 months), and found that, after dental treatment, there was a significant improvement in several areas such as sleeping, eating, and pain.11
Several additional studies have addressed QOL of children following oral rehabilitation in the operating room.12–14 These studies demonstrate improved oral health-related QOL/dental discomfort following treatment intervention under general anesthesia.12–14 Malden et al. found that, 1 to 4 weeks following treatment under general anesthesia, children were reported to have better perceived QOL.13 Acs et al. found that parents of children undergoing oral rehabilitation under general anesthesia reported improvements in their child’s QOL, including: overall improvement in their child’s health; reduction in pain; improved ability to eat; and improved ability to sleep.12
The purposes of this study were to determine, using a large sample size and a newly constructed assessment instrument, whether parent-reported oral health-related QOL of children with early childhood caries differed from that of caries-free children and if it improved with treatment intervention.
METHODS
This longitudinal study of parent-reported oral health-related QOL in preschool children with and without ECC was conducted at 2 sites, Children’s National Medical Center, Washington, D.C., and Columbus (now Nationwide) Children’s Hospital, Columbus, Ohio. Institutional Review Boards at Boston University Medical Center, Tufts University and at each of the 2 study sites approved the protocol, and written informed consent was obtained from the parents.
SAMPLE
Parents of preschool children who were receiving care at pediatric dental clinics in participating medical centers were invited to participate. There were 2 study groups:
children with S-ECC, defined as a primary dentition with at least 3 smooth surface carious lesions, including at least 1 pulpally involved tooth; and
children who were caries-free at baseline and had no prior caries experience.
OUTCOME MEASURES
A questionnaire instrument (POQL) was developed in order to assess pediatric oral health-related quality of life by measuring the extent to which oral conditions impact the social, psychological, and physical well-being of children, and the QOL of their families (Spetter et al., manuscript under review). The POQL questionnaire was developed in a purposely diverse sample; questions comprising the POQL were developed based on a literature review and parent focus groups. Briefly, the POQL was developed to assess 4 domains of daily functioning believed to be affected by oral health: (1) physical functioning; (2) social functioning; (3) mental functioning, including interpersonal relationships and concern with esthetics; and (4) impairment, including pain and parent-reported symptoms.
For each item, respondents were asked to rate how often the event occurred for their child in the past 3 months due to their child’s teeth or mouth. Answer choices were: all of the time; some of the time; once in a while; and did not happen. For each item, respondents were asked how bothered the child was by the event over the past 3 months. Answer choices were: very bothered; somewhat bothered; bothered a little bit; never bothered; and did not happen.
In addition to the 4 domains, the POQL also yields a summary score, obtained by summing the scores on all 13 items. Parents were also asked to rate their child’s overall oral health (OH1) and several questions assessing demographics (parent or caretaker’s gender, child’s age and gender). Regarding the child’s overall oral health, parents were asked, “In general, how would you describe the health of your child’s teeth and mouth?” The 5 answer choices were: excellent, very good, good, fair, or poor.
Three versions of the POQL (child self-report, parent report on child [PRC], and parent self-report) were developed for 3 age groups of children: preschoolers (2–8 years old), elementary schoolers (8–12 years old), and preteens (12–14 years old). For preschoolers, no self-report measure was developed, due to the children’s inability to accurately report their health.
In the present study, only the PRC was used because of the children’s young ages. In this version of the POQL, the 4 domains were: physical (which included pain and impairment), social, mental, and emotional. We used the 13 POQL items to construct 5 outcome measures: 1 total impact score and 4 domain scores (physical plus pain/impairment, mental, social, emotional). For the 13 POQL items, scores were computed by reverse-scoring all items, so that higher scores indicated greater frequency or bother. We then multiplied the frequency score by the bother score to obtain an “impact” score for the item. Impact scores on all 13 items were summed to form a total score (with a possible range from 0–156 [3×4×13]). The 4 domain scores were computed using 4, 4, 2, and 2 items, respectively (1 item, “did your child cry?” was excluded from the domain scores). We also treated parent-perceptions of the OH1 as an outcome.
Parents completed the questionnaire at 3 timepoints: at baseline and at 6- and 12-month recalls. At baseline, no subjects had received dental treatment other than routine diagnostic and preventive treatment. The data were coded, double-entered, and accuracy verified. All analyses were performed using SAS 9.1 (SAS Institute, Cary, NC).
RESULTS
The baseline questionnaire was administered to 501 parents: 315 reporting on their caries-free children and 186 reporting on their ECC children. At the 6-month recall, parents of 209 caries-free children and 81 ECC children responded; at the 12-month recall, 109 caries-free and 46 ECC parents completed surveys (Table 1).
Table 1.
Sample description
| Baseline | 6 mos | 12 mos | ||||
|---|---|---|---|---|---|---|
| Caries-free n (%) | Early childhood caries n (%) | Caries-free n (%) | Early childhood caries n (%) | Caries-free n (%) | Early childhood caries n (%) | |
| Site | ||||||
| Total | 315 | 186 | 209 | 81 | 109 | 46 |
| Washington D.C. | 143 | 28 | 106 | 13 | 58 | 7 |
| 172 | 158 | 103 | 68 | 51 | 39 | |
| Caries-free mean(SD) | Early childhood mean(SD) | Caries-free mean(SD) | Early childhood mean(SD) | Caries-free mean(SD) | Early childhood mean(SD) | |
| 3.35 (0.96) | 4.09 (1.02) | 3.92 (0.93) | 4.65 (1.18) | 4.68 (1.04) | 5.13 (1.22) | |
| Caries-free n (%) | Early childhood caries n (%) | Caries-free n (%) | Early childhood caries n (%) | Caries-free n (%) | Early childhood caries n (%) | |
| Respondent: Mother | 291 (92) | 166 (90) | 189 (91) | 72(89) | 97 (90) | 39 (85) |
| Child’s sex | ||||||
| Male | 139 (44) | 95 (51) | 86 (42) | 40 (49) | 45 (42) | 20 (43) |
| Female | 176 (56) | 91 (49) | 121 (58) | 41 (51) | 63 (58) | 26 (57) |
| Child’s race | ||||||
| Caucasian | 62 (20) | 98 (53) | 34 (16) | 44 (54) | 18 (17) | 25 (54) |
| African American | 211 (68) | 56 (30) | 146 (70) | 25 (31) | 74 (68) | 16 (35) |
| Other | 38 (12) | 31 (17) | 29 (14) | 12 (15) | 17 (16) | 5 (11) |
| Hispanic | 20 (6) | 16 (9) | 13 (6) | 8 (10) | 6 (6) | 4 (9) |
| Family’s income | ||||||
| <$15,000 | 116 (46) | 78 (46) | 78 (45) | 34 (47) | 33 (39) | 15 (38) |
| $15,000–$24,999 | 35 (14) | 40 (24) | 20 (12) | 14 (19) | 9 (11) | 8 (20) |
| >$25,000 | 102 (40) | 51 (30) | 74 (43) | 25 (34) | 42 (50) | 17 (42) |
| Insurance | ||||||
| Medicaid | 258 (83) | 159 (86) | 173 (83) | 71 (88) | 86 (79) | 39 (85) |
| Private | 50 (16) | 22 (12) | 33 (16) | 7 (9) | 22 (20) | 6 (13) |
| None | 2 (1) | 4 (2) | 2 (1) | 3 (4) | 1 (1) | 1 (2) |
| OH1 group parental response | ||||||
| Excellent, very good, or good | 304 (97) | 24 (13) | 205 (98) | 65 (80) | 105 (97) | 40 (89) |
| Fair or poor | 11 (3) | 162 (87) | 4 (2) | 16 (20) | 3 (3) | 5 (11) |
At baseline, compared with caries-free children, ECC children were rated by their parents as having significantly poorer over-all oral health (P<.001; Table 1, Figure 1). Across all 3 visits, caries-free children were rated by their parents as having better oral health status vs ECC children (P<.001).
Figure 1.
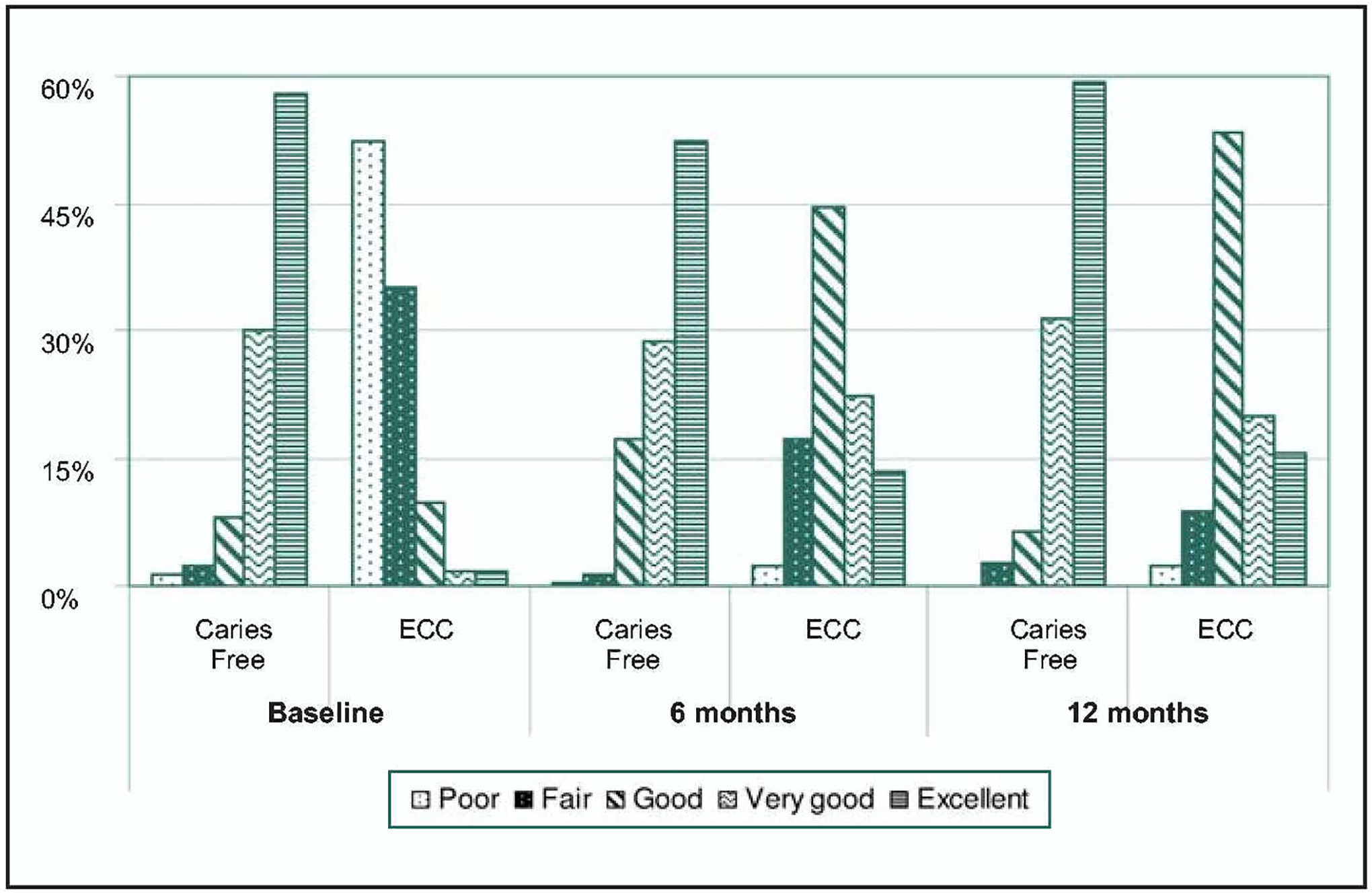
Parental rating of child’s overall oral health (OH1) by group and timepoint.
At baseline, the mean difference in the total impact scores between the ECC and caries-free groups was 12.07 (P<.001).
Impact scores on 4 items (pain, trouble sleeping, trouble eating hard foods, trouble eating hot or cold foods) were summed to provide an index of the impact of dental problems on physical functioning. At baseline, ECC children were rated as having worse physical functioning (a greater negative impact of oral problems on their physical functioning) vs caries-free children (mean difference=7.3, P<.001; Figure 2).
Figure 2.
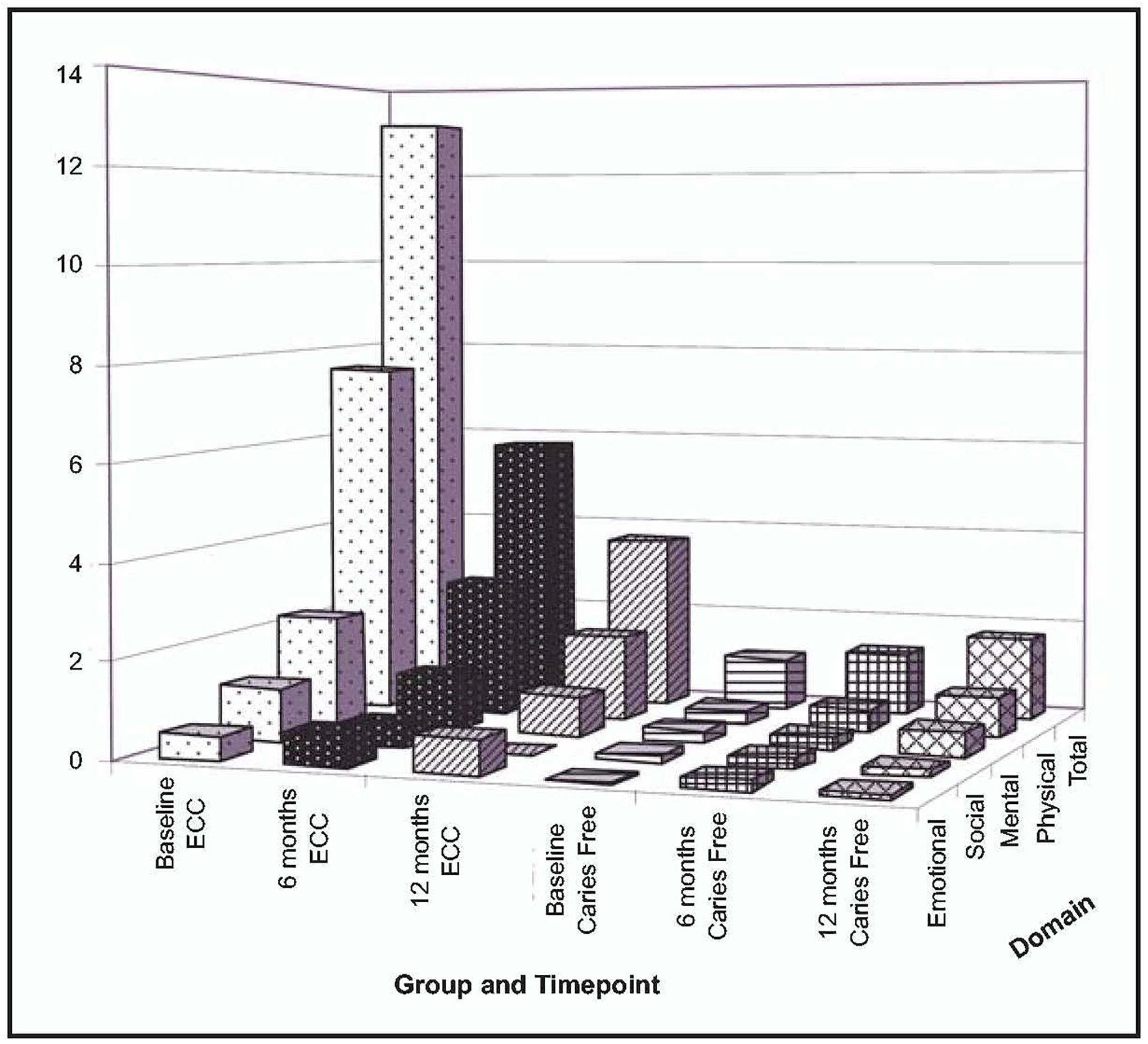
Mean impact scores by group and timepoint.
At baseline, ECC parents reported greater impact on their child’s mental functioning due to their child’s teeth or mouth, compared with caries-free children (mean difference=2.0, P<.001; Figure 2). Mental functioning was defined by summing the impact scores on 2 items: (1) feel angry or upset; and (2) feel worried.
Social functioning was defined by summing impact scores on 4 items: (1) missing preschool or day care; (2) not interested in playing with other friends; (3) missing out on planned activity such as a birthday party or a trip to the zoo; and (4) not joining a family activity. At baseline, ECC children were reported by their parents as having significantly worse social functioning vs caries-free children (mean difference=0.98, P<.001; Figure 2).
Emotional functioning was defined by summed impact scores on 2 items: 1) having trouble saying certain words; and (2) being mocked by others because of the teeth or mouth. ECC and caries-free children were not found to have significantly different emotional functioning at baseline.
We examined differential change between ECC and caries-free children for 6 outcomes: OH1, PRC impact score (sum of the product of frequency times bother for all items), and impact scores for 4 domains: (1) physical functioning/pain; (2) mental functioning; (3) social functioning; and (4) emotional functioning. For each outcome, we fit a mixed model that included terms for group (ECC vs caries-free), timepoint (baseline, 6 months, and 12 months), and a group-time interaction to test whether the ECC group showed more improvement over follow-up visits than caries-free children. Site was also included as a covariate to adjust for possible differences between Columbus and Washington, D.C. Preliminary analyses also included child’s age and gender and relationship of respondent to child, but these effects were not significant, so they were excluded from further consideration.
Prior to conducting the longitudinal analysis, we compared outcomes between children who dropped out of the study. Approximately equal percentages of ECC and caries-free children dropped out from baseline to timepoint 2 and then to timepoint 3. Those who dropped out after the baseline visit: were older (P<.03); had significantly more problems (P<.001); had a greater impact on physical functioning (P=.003) and mental functioning domains (P<.003); and had higher total impact scores (P<.004).
Table 2 shows the mixed model analysis results for all outcomes. Each set of columns in Table 2 (eg, OH1 and PRC Total) refers to an outcome. The fixed effects rows indicate the regression weights to predict scores on the outcomes. In particular, note the rows labeled ECC × Time 1 and ECC × Time 2, which refer to the group (ECC vs caries-free) by time (0, 1, 2) interaction. This indicates whether the 2 groups changed differently over the intervals (0–1, 1–2). For the 6 outcomes, the interaction is significant, indicating that the 2 groups changed differently. In fact, the ECC group improved between baseline and 6-month follow-up (0,1 interval), whereas the caries-free group did not change. The random effects rows in Table 2 indicate that there were differences among children within each group; the Akaike information criterion is a measure of model fit. The estimated means are the predicted means for ECC and caries-free children at the 3 time-points (baseline, 6-month, and 12-month follow-up), based on the afore-mentioned model. As shown in Figure 1, ECC children improved in the OH1 (increased); PRC total, and 3 out of 4 PRC domains also improved (decreased).
Table 2.
Results of mixed model analysis*
| OH1 | PRC total | PRC factor 1: Social | |||||
|---|---|---|---|---|---|---|---|
| Estimate(SE) | P-value | Estimate(SE) | P-value | Estimate(SE) | P-value | ||
| Fixed effects | |||||||
| Intercept | 4.54(0.09) | <.001 | 2.41(1.05) | .02 | 0.25(0.24) | .30 | |
| ECC group | −1.04(0.15) | <.001 | 3.40(1.75) | .05 | 0.34(0.39) | .38 | |
| Exam (timepoint): 1 | −0.01 (0.09) | .93 | −0.43(0.96) | .66 | 0.15(0.20) | .46 | |
| Exam (timepoint): 2 | −0.15(0.09) | .09 | −0.22(1.00) | .83 | 0.20(0.21) | .34 | |
| Site: Columbus | −0.20(0.07) | <.01 | −1.64(0.97) | .08 | −0.48(0.22) | .03 | |
| ECC × Time 1 | −1.65(0.15) | <.001 | 9.17(1.76) | <.001 | 0.79(0.37) | .40 | |
| ECC × Time 2 | 0.09(0.16) | .60 | 1.94(1.84) | .29 | 0.07(0.39) | .87 | |
| Random effects | |||||||
| ID (group) | 0.20(0.04) | <.001 | 49.54(6.38) | <.001 | 3.42(0.31) | <.001 | |
| Residual | 0.52(0.04) | <.001 | 63.55(4.42) | <.001 | 2.72(0.17) | <.001 | |
| Subjects (n) | 501 | 501 | 501 | ||||
| Observations (n) | 936 | 936 | 931 | ||||
| Estimated means | |||||||
| Group time | Mean(SD) | Mean (SD) | Mean(SD) | ||||
| ECC | 1 | 1.66(0.07) | 13.16(0.59) | 1.12(0.17) | |||
| 2 | 3.26(0.08) | 6.16(0.60) | 0.45(0.18) | ||||
| 3 | 3.32(0.07) | 4.42(0.59) | 0.18(0.17) | ||||
| Caries-free | 1 | 4.42(0.10) | 1.09(0.82) | 0.14(0.24) | |||
| 2 | 4.28(0.10) | 1.38(0.82) | 0.21(0.24) | ||||
| PRC factor 2: Physical | PRC factor 3: Mental | PRC factor 4: Emotional | |||||
| Estimate(SE) | P-value | Estimate(SE) | P-value | Estimate(SE) | P-value | ||
| Fixed effects | |||||||
| Intercept | 1.14(0.56) | .04 | 0.61(0.25) | .02 | 0.20(0.15) | .18 | |
| ECC group | 1.16(0.97) | .23 | 0.60(0.41) | .15 | 0.73(0.26) | .01 | |
| Exam (timepoint): 1 | −0.50(0.58) | .39 | −0.25 (0.22) | .26 | 0.17(0.15) | .28 | |
| Exam (timepoint): 2 | −0.38(0.61) | .54 | −0.19(0.22) | .39 | 0.15(0.16) | .36 | |
| Site: Columbus | −0.57(0.42) | .18 | −0.21 (0.24) | .37 | −0.26(0.11) | .02 | |
| ECC × Time 1 | 6.31(1.05) | <.001 | 1.47(0.40) | <.001 | −0.36(0.28) | .19 | |
| ECC × Time 2 | 1.49(1.13) | .19 | 0.50(0.41) | .22 | −0.21 (0.30) | .47 | |
| Random effects | |||||||
| ID (group) | 4.24(1.72) | .01 | 3.74(0.40) | <.001 | 0.35(0.11) | <.001 | |
| Residual | 25.28(1.85) | <.001 | 3.11(0.22) | <.001 | 1.71(0.12) | <.001 | |
| Subjects (n) | 501 | 501 | 501 | ||||
| Observations (n) | 933 | 929 | 909 | ||||
| Estimated means | |||||||
| Group time | Mean(SD) | Mean(SD) | Mean(SD) | ||||
| ECC | 1 | 7.62(0.20) | 2.25(0.08) | 0.51(0.09) | |||
| 2 | 2.92(0.21) | 1.35(0.08) | 0.64(0.10) | ||||
| 3 | 1.82(0.21) | 1.03(0.08) | 0.71(0.09) | ||||
| Caries-free | 1 | 0.32(0.28) | 0.25(0.11) | 0.22(0.13) | |||
| 2 | 0.48(0.29) | 0.32(0.11) | 0.22(0.13) | ||||
| 3 | 0.87(0.29) | 0.52(0.11) | 0.08(0.13) | ||||
OH1=child’s perceived overall oral health as reported by parent (1=poor, 2=fair, 3=good, 4=very good, 5=excellent); PRC=parent’s report on child; ECC × Time 1 and ECC × Time 2=group (ECC vs caries-free) by time (0, 1, 2) interaction.
For all outcomes except emotional functioning, the interaction between group (ECC vs caries-free children) and timepoint was significant, with ECC children showing a significant decrease between baseline and 6-month recall vs caries-free children. At the 12-month recall, ECC children maintained this improvement, but still had worse parent-reported health than did caries-free children. There was a significant site effect, suggesting somewhat lower OH1 in Columbus.
Based on the model, we estimated predicted means for the ECC and caries-free groups at each exam timepoint. Examining these means shows that caries-free children are relatively stable across the 3 time-points, while ECC children move from poor to moderate oral health-related QOL between the first and second visits, and remain relatively stable between visits 2 and 3.
Table 2 shows the results for the social, physical/pain, mental, and emotional PRC domains. For the first 3, the group-exam interaction is significant. Additionally, the estimated means show that ECC children “improved” much more from baseline to 6-month follow-up than did the caries-free children, who remained relatively stable over time. For the social interaction domain, there was a significant group effect, with ECC children having higher scores across all exam timepoints. Columbus children had lower scores on emotional and social interaction domains.
DISCUSSION
Generally, parents of ECC children reported markedly poorer oral health at baseline and worse perceived impact on physical functioning and pain than caries-free children. ECC children were rated by their parents as having worse perceived oral health status across the physical/pain, mental and, to a lesser extent, social functioning domains. At baseline, the overall oral health of ECC children was rated by their parents as significantly less likely to be excellent, very good, or good. Following dental intervention at the 6-month recall, ECC children were rated by their parents as having significantly improved oral health, and physical, mental, and social functioning compared to baseline. By contrast, improvements in emotional functioning were not seen; possible reasons include the fact that children may have difficulty speaking at this age regardless of oral conditions. Also, these children may be too young for teasing to occur to such an extent to bother them significantly. Furthermore, we do not know why social and emotional impacts are different by study site (worse in Washington, D.C.). One possible explanation is that there may be additional burdens in the urban environment not otherwise captured.
Parent-reported oral health QOL was relatively constant for the ECC group between the 6- and 12-month follow-up visits. Surgical dental intervention resulted in significant improvement in oral health-related QOL in the first 6 months following treatment, and oral health-related QOL remained improved after 12 months. Caries-free children were found to enjoy relatively good oral health across all 3 timepoints.
This study’s results were consistent with the findings by previous studies relating oral health to QOL.4–9 Also, similar to Filstrup et al., Low et al., Acs et al., Malden et al., and Versloot et al., we found that, following dental intervention, children with severe caries experienced significant improvement in QOL.10–14 This study’s findings demonstrate that ECC children specifically found improved QOL related to physical functioning and pain. This study highlights the ever-increasing need for US children to have improved access to dental care and to receive preventive dental treatments such as fluoride applications and sealants. This study also supports the validity of items included in the PRC version of our preschool POQL questionnaire.
A major strength of this study was the large number of parents (501) who reported on their children. In addition, this study’s longitudinal design allowed assessment of the impact of dental intervention on changes in QOL parameters for caries-free and ECC children. Major limitations of this study include: it did not examine other barriers to access, including insurance, availability of the provider, and distance to the dentist; and differential loss to follow-up. We only, however, examined changes in children seen over all 3 time points: baseline, 6 months, and 12 months. Future research should examine the impact of dental intervention on generic plus oral-specific measures of children’s health-related QOL.
CONCLUSIONS
Based on this study’s results, the following conclusions can be made:
Children’s oral health significantly impacts their well-being, as assessed by their parents. Children with early childhood caries (ECC) are rated by their parents as having worse oral health-related quality of life (QOL) than are caries-free children.
The positive effects of a dental intervention for ECC children are significant at the 6- and 12-month follow-ups, and enhance QOL in multiple domains.
Despite improvements in parent-reported oral health QOL, differences between ECC and caries-free children persist after dental treatment.
ACKNOWLEDGMENT
The work presented in this original research report is supported by NIDCR Grants # U54 DE014264, K24 DE018211 and K24 DE00419.
REFERENCES
- 1.US Department of Health and Human Services, Center for Disease Control and Prevention. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis—United States, 1988–1994 and 1999–2002. MMWR Surveill Summ 2005;54:1–44. [PubMed] [Google Scholar]
- 2.Albert DA, Park K, Findley S, Mitchell DA, Mc-Manus JM. Dental caries among disadvantaged 3- to 4-year-old children in northern Manhattan. Pediatr Dent 2002;24:229–33. [PubMed] [Google Scholar]
- 3.Clarke M, Locker D, Berall G, Pencharz P, Kenny OJ, Judd P. Malnourishment in a population of young children with severe early childhood caries. Pediatr Dent 2006;28:254–9. [PubMed] [Google Scholar]
- 4.Thomas CW, Primosch RE. Changes in incremental weight and well-being of children with rampant caries following complete dental rehabilitation. Pediatr Dent 2002;24: 109–13. [PubMed] [Google Scholar]
- 5.Feitosa S, Colares V, Pinkham J. The psychosocial effects of severe caries in 4-year-old children in Recife, Pernambuco, Brazil. Cad Saude Publica 2005;21:1550–6. [DOI] [PubMed] [Google Scholar]
- 6.Barbosa TS, Gaviao MBD. Oral health-related quality of life in children: Part II. Effects of clinical oral health status: A systematic review. Int J Dent Hyg 2008;6:100–7. [DOI] [PubMed] [Google Scholar]
- 7.Do LG, Spencer A. Oral health-related quality of life of children by dental caries and fluorosis experience. J Public Health Dent 2007;67: 132–9. [DOI] [PubMed] [Google Scholar]
- 8.Versloot J, Veerkamp JS, Hoogstraten J. Dental discomfort questionnaire: Assessment of dental discomfort and/or pain in very young children. Community Dent Oral Epidemio12006;34:47–52. [DOI] [PubMed] [Google Scholar]
- 9.Locker D. Disparities in oral health-related quality of life in a population of Canadian children. Community Dent Oral Epidemiol 2007;35:348–56. [DOI] [PubMed] [Google Scholar]
- 10.Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: Child and parent perspectives. Pediatr Dent 2003;25:431–40. [PubMed] [Google Scholar]
- 11.Low W, Tan S, Schwartz S. The effect of severe caries on the quality of life in young children. Pediatr Dent 1999;21:325–6. [PubMed] [Google Scholar]
- 12.Acs G, Pretzer S, Foley M, Ng MW Perceived outcomes and parental satisfaction following dental rehabilitation under general anesthesia. Pediatr Dent 2001;23:419–23. [PubMed] [Google Scholar]
- 13.Malden PE, Thomson WM, Jokovic A, Locker D. Changes in parent-assessed oral health-related quality of life among young children following dental treatment under general anesthetic. Community Dent Oral Epidemio12008;36:108–17. [DOI] [PubMed] [Google Scholar]
- 14.Versloot J, Veerkamp JSJ, Hoogstraten J. Dental discomfort questionnaire for young children following full mouth rehabilitation under general anesthesia: A follow-up report. Eur Arch Paediatr Dent 2006;7:126–9. [DOI] [PubMed] [Google Scholar]


