Abstract
Objectives
From May-September 2022, 203 cases of monkeypox (MPX) were reported in the Tel Aviv (TA) District, Israel. We aim to report the first ongoing local transmission of MPX in Israel.
Methods
We analyzed the epidemiologic and clinical features of all cases of MPX notified to the TA District. Each case was contacted to verify the source of infection and locate potential contacts.
Results
All cases were men; 195 (96%) were among men having sex with men, and 171 (84%) resided in the city of TA. Median age was 35 years. One case occurred in a healthcare worker. All cases had a self-limiting disease.
Conclusion
A combined public health campaign with vaccination against MPX of high-risk individuals leads to a decrease in disease rates. Enhanced surveillance and prevention among susceptible populations are warranted.
Keywords: Monkeypox, Monkeypox outbreak, Epidemiology
Introduction
Monkeypox (MPX) virus, a DNA Orthopox virus, has evolved from being essentially endemic in central and western African countries to causing a Public Health Emergency of International Concern [1].
In Israel, before 2022, there had only been one reported case of MPX in 2018, attributed to travel in Nigeria [2]. From May-September 13, 2022, 246 cases of MPX were reported in Israel (rate of 2.7 per 100,000 population) [3]; of them, 203 (83%) reside in the Tel Aviv (TA) District (rate of 14 per 100,000 population). In this report, we describe the epidemiologic and clinical features of an outbreak of MPX virus in the TA District, Israel.
Methods
All patients in this study were residents of the TA District, Israel, which have 1.5 million inhabitants (16% of the total Israeli population) [4]. It is comprised of 12 cities on the coastline of Israel, among them, the city of TA, markedly renowned for its annual gay pride week with a mass parade, which occurs during the first week of May and attracts many tourists [5].
MPX was added as a notifiable disease by law in Israel in 2022. A case of MPX was defined as having compatible clinical symptoms (such as the presence of a typical rash) and laboratory evidence of infection by polymerase chain reaction of either cutaneous and/or respiratory and/or rectal samples. All patients were routinely tested for sexually transmitted infections during their visit. Each case was told to self-isolate until the complete resolution of the rash and was contacted by the Ministry of Health (MoH) to undergo an epidemiologic inquiry, which included questions regarding clinical presentation and sources of exposure. Close contacts were defined as having stayed in proximity to a confirmed case for more than 3 hours at a distance of less than 2 meters or as having direct contact with skin lesions or body fluids of a confirmed case, including sexual intercourse, during the infectious period. The infectious period was defined as the period from symptom onset until complete resolution of the rash. Contacts were told to actively track for the appearance of fever or skin lesions in the 3 weeks following contact, to seek medical advice if those were to develop, and to avoid sexual contact during that period. Post-exposure prophylaxis with one dose of the Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine was given to at-risk close contacts, such as children or immune-suppressed individuals.
Results
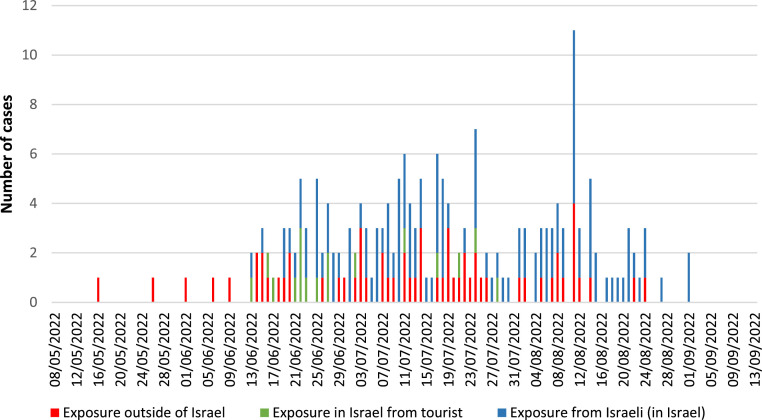
Between May 16 and September 13, 2022, a total of 203 cases of MPX were reported in the TA District (Figure 1 ). Among all cases, 61 (30%) were acquired during trips outside of Israel, mostly in Europe. All cases were men. Median age was 35 years (range 19-62 years). Among all cases, 25 (12%) were HIV positive. Among 178 HIV-negative patients, 89 (50%) patients took HIV pre-exposure prophylaxis. Among all cases, 195 (96%) were among men having sex with men (MSM), all of whom had reported having sexual contact as the source of infection in the 3 weeks before disease onset. Among those cases, 110 (54%) reported having had more than three sexual partners in the 21 days before symptom onset (Table 1 ). One case was a physician working in the emergency service who had provided medical care for patients with MPX and subsequently developed a rash on his left hand. Most cases (171, 84%) were residents of the city of TA (Supplemental Material). All our cases had a self-limiting disease, and 11 (5%) had a co-occurring sexually transmitted infection. Post-exposure prophylaxis with the MVA-BN vaccine was administered to 12 children and three adults, household contacts of MPX cases.
Figure 1.
Monkeypox cases, by date of disease onset and source of exposure, Tel Aviv District, Israel, 2022.
Table 1.
Characteristics of monkeypox cases in the Tel Aviv District, Israel, 2022.
| Number of cases N = 203 |
% | |
|---|---|---|
Gender
|
203 |
100% |
Age category
|
2 40 113 37 4 2 5 |
1% 20% 56% 18% 2% 1% 2% |
| Men having sex with men | 195 | 96% |
Co-occurring sexually transmitted infections:
|
11 6 2 3 |
5% 3% 1% 1% |
Underlying medical conditions:
|
170 25 6 2 |
84% 12% 3% 1% |
SymptomsFeverFlu-like symptomsRash
|
125 140 186 128 48 44 41 35 115 33 14 81 |
84% 69% 92% 63% 24% 22% 21% 17% 57% 16% 7% 40% |
| Median time (day) until complete resolution of symptoms (IQR) | 19.5 (10) | |
Route of transmission
|
197 1 5 |
97% 1% 2% |
Positive laboratory samples
|
141 83 33 42 |
69% 41% 16% 21% |
| > 3 sexual partners in the 3 weeks preceding symptom onset | 110 | 54% |
| Median time (day) from symptom onset to diagnosis (range) | 6 (1-17) |
Discussion
This study describes the first sustained outbreak with local transmission of MPX in the TA District, Israel. This outbreak occurred simultaneously with established worldwide outbreaks of MPX [6,7].
Although 41% of cases in our study tested positive on their respiratory sample, all cases were linked to sexual or close physical contact, and we did not observe respiratory transmission of MPX.
Local spread of MPX cases was evident a few weeks after the TA gay pride parade, and cases peaked approximately 2 months thereafter. Most cases were condensed in the city of TA, which allowed for focused prevention efforts to decrease transmission, including community outreach, case isolation, and contact tracing. Most cases were not willing to provide details of known sexual contacts they had had during the infectious period, and those could not be directly reached by the MoH. However, we found that a large portion of contacts (who subsequently became cases) had been notified by cases and had self-isolated themselves. During the TA gay pride weekend, there were mass gatherings and parties, which included anonymous sexual contacts (including tourists) who could not be reached, and this likely contributed to the spread that ensued.
The MVA-BN vaccine was unavailable at the start of the outbreak, and mitigation measures consisted of self-isolation of cases and a public health online information campaign aimed at raising awareness among high-risk populations (preeminently among MSM). The vast majority of the cases in our study were MSM, which prompted a recommendation by the MoH that at-risk men born after 1980 be vaccinated with one dose of the MVA-BN vaccine as of July 27, 2022, free of charge, with prioritization of men having HIV and a co-occurring sexually transmitted infection and men treated with pre-exposure prophylaxis for HIV [8].
One of our cases was a healthcare worker who developed a rash after attending to patients with MPX. He had worn personal protective equipment (including gloves and a mask) during all his physical examinations of patients with MPX. The incident prompted an inspection by the National Center for Infection Control, which stated that it suspects the transmission might have occurred either by a tear of the glove during lesion sampling (which was done by a scalpel) or during the removal of the personal protective equipment. This stresses the necessity of updating guidelines and training for infectious disease prevention in medical settings.
At the start of the outbreak, most cases in Israel were imported or due to contact with a tourist. However, local transmission quickly followed, with its relative part increasing as the outbreak progressed. MPX cases spiked at the end of August, during vacation season, signaling that practitioners should issue prevention guidelines to at-risk travelers. This also stresses the importance of a combined international effort to vaccinate as many at-risk individuals, to stall the spread of MPX. Ongoing surveillance with quick identification of cases is crucial as community transmission has already been established to assess the scope of transmission and detect new populations affected by MPX.
Declaration of Competing Interest
The authors have no competing interests to declare.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Data on individual patients were available as part of the disease notification mandate. It gives legal authority to analyze the recorded data and to report it. For the purpose of this study, all patients from this existing database were de-identified.
Author contributions
Rivka Sheffer and Matanelle Salama wrote and designed the study; and extracted and analyzed patients' data; Michal Savion, Naama Nuss and Ziva Amitai contributed to dataset design and gave critical input to the study draft.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
References
- 1.World Health Organization. WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern, https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern; 2022 [accessed 08 November 2022].
- 2.Erez N, Achdout H, Milrot E, Schwartz Y, Wiener-Well Y, Paran N, Politi B, Tamir H, Israely T, Weiss S, Beth-Din A, Shifman O, Israeli O, Yitzhaki S, Shapira SC, Melamed S, Schwartz E. Diagnosis of imported monkeypox, Israel, 2018. Emerg Infect Dis. 2019;25:980–983. doi: 10.3201/eid2505.190076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Our world in data. Mpox (Monkeypox) Data explorer, https://ourworldindata.org/explorers/monkeypox?tab=table&facet=none&hideControls=false&Metric=Confirmed%2Bcases&Frequency=Cumulative&Relative%2Bto%2Bpopulation=false&country=~OWID_WRL; 2022 [accessed 08 November 2022].
- 4.Israeli Central Bureau of Statistics, 2022, https://www.cbs.gov.il/EN/Pages/default.aspx; 2022 [accessed 08 November 2022].
- 5.Israeli Ministry of Foreign affairs. Tel Aviv Pride Parade 2022, https://www.gov.il/en/departments/general/tel-aviv-pride-parade-2022-11-may-2022; 2022 [accessed 08 November 2022].
- 6.Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, Harrison LB, Palich R, Nori A, Reeves I, Habibi MS, Apea V, Boesecke C, Vandekerckhove L, Yakubovsky M, Sendagorta E, Blanco JL, Florence E, Moschese D, Maltez FM, Goorhuis A, Pourcher V, Migaud P, Noe S, Pintado C, Maggi F, Hansen AE, Hoffmann C, Lezama JI, Mussini C, Cattelan A, Makofane K, Tan D, Nozza S, Nemeth J, Klein MB. Orkin CM, SHARE-net Clinical Group. Monkeypox virus infection in humans across 16 countries - April–June 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 7.Perez Duque M, Ribeiro S, Martins JV, Casaca P, Leite PP, Tavares M, Mansinho K, Duque LM, Fernandes C, Cordeiro R, Borrego MJ, Pelerito A, de Carvalho IL, Núncio S, Manageiro V, Minetti C, Machado J, Haussig JM, Croci R, Spiteri G, Casal AS, Mendes D, Souto T, Pocinho S, Fernandes T, Firme A, Vasconcelos P, Freitas G. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.22.2200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Israeli Ministry of Health. Monkeypox, https://www.gov.il/he/departments/guides/disease-monkeypox?chapterIndex=2; 2022 (accessed 8 November 2022).