Abstract
The World Health Organization (WHO) declared monkeypox as a public health emergency of international concern (PHEIC) on July 23, 2022, their highest level of alert. This raised concerns about the management of the global monkeypox outbreak, as well as the scientific analysis and accurate prediction of the future course of the epidemic. This study used EpiSIX (an analysis and prediction system for epidemics based on a general SEIR model) to analyze the monkeypox epidemic and to forecast the major tendencies based on data from the USA CDC (https://www.cdc.gov) and the WHO (https://www.who.int/health-topics/monkeypox). The global outbreak of monkeypox started in the UK on May 2, 2022, which marked the beginning of an epidemic wave. As of October 28, 2022, the cumulative number of reported cases worldwide was 77,115, with 36 deaths. EpiSIX simulations predict that the global monkeypox epidemic will enter a low epidemic status on March 1, 2023 with the cumulative number of confirmed cases ranging from 85,000 to 124,000, and the total number of deaths ranging from 60 to 87. Our analysis revealed that the basic reproduction number (R0) of monkeypox virus (MPXV) is near to 3.1 and the percentage of asymptomatic individuals is 13.1 %–14.5 %, both of which are similar to the data for SARS. The vaccination efficiency against susceptibility (VEs) of individuals who have had monkeypox is ∼ 79 %, and the vaccination efficiency against infectiousness (VEi) of individuals who have had monkeypox is ∼ 76 %–82 %. The mean incubation period for monkeypox is 8 days. In total, 94.7 % of infected individuals develop symptoms within 20 days and recover within 2 weeks after the confirmation of symptoms. Simulation results using EpiSIX showed that ring vaccination was remarkably effective against monkeypox. Our findings confirmed that a 20-day isolation for close contacts is necessary.
Keywords: Monkeypox, Epidemic, Prediction, Tendency
1. Introduction
Monkeypox is a viral zoonosis that causes symptoms similar to those seen in patients with smallpox. Since 1980, smallpox has been eradicated, while monkeypox is still endemic in parts of Africa.
Monkeypox first occurred in monkeys in the rainforest of West-Central Africa and can infect other animals and humans. The clinical symptoms of monkeypox are similar to those of smallpox, but milder. Monkeypox is caused by the monkeypox virus (MPXV), which belongs to a group of viruses that include smallpox virus and vaccinia virus used in smallpox vaccines. However, unlike smallpox and chickenpox viruses, MPXV can be transmitted from animals to humans through direct close contact or from humans to humans, with the main routes of infection including blood and bodily fluids. In addition, monkeypox is far less contagious than smallpox. Clinically, MPXV infection can be divided into three stages.1, 2, 3
The incubation period (5–21 days) is the period between the time an individual is infected and the appearance of symptoms, which usually lasts 6–13 days, but can be up to 21 days.
The onset period (0–5 days)4 is characterized by fever, severe headache, lymphadenopathy, back pain, muscle pain and general weakness (lethargy). Compared with infectious diseases such as chickenpox, measles and smallpox, lymphadenopathy is a distinct feature of monkeypox. Neither smallpox nor chickenpox has this characteristic.
The rash stage (14–21 days) is a period in which the rash that tends to be concentrated on the face and limbs, changes from a maculopapular rash to small blisters and pustules that dry up and crust over, and can vary in number from a few to several thousand. It takes about 3 weeks for the crusts to completely disappear. Monkeypox symptoms usually last from 14 to 21 days.
The first case of this recent monkeypox epidemic was reported by the UK Centers for Disease Control (CDC) on May 7, 2022.5 As of May 20, 2022, the cumulative number of reported cases and suspected cases was over 100. The World Health Organization (WHO) held an emergency meeting in June 2022 in which they considered renaming monkeypox to avoid stigmatization and discrimination; however, a new name is yet to be adopted. The media speculated that the rationale for renaming monkeypox is similar to that of COVID-19. On July 23, 2022, the WHO claimed that the monkeypox outbreak was a public health emergency of international concern (PHEIC), which is the highest level of public health alert issued by the WHO.1 On June 6, 2022, the China CDC published Technical Guidance for Control and Prevention of Monkeypox (2022) for the management of probable monkeypox outbreaks in China. As of October 28, 2022, a total of 109 countries had reported monkeypox cases,1 with 77,115 laboratory-confirmed cases and a further 3,610 probable cases, and 36 deaths, distributed worldwide. By region, there were 50,573 cases in the Americas, 25,297 in Europe, 934 in Africa, 209 in the Western Pacific, 72 in the Eastern Mediterranean and 30 cases in South-East Asia. The monkeypox epidemic in Africa is still a cause for concern, but numbers of cases have declined in other regions following the administration of smallpox vaccine to monkeypox-infected individuals and their close contacts (Table 1 ). The case-fatality rate globally is 0.7005 per 1,000.
Table 1.
Total number of monkeypox cases by region based on data from the WHO, as of October 28, 2022.
| Region | TCC | TPC | TD | CPW1 | 7dCC1 |
|---|---|---|---|---|---|
| The Americas | 50,573 | 3,610 | 16 | 1,016 | −49 % |
| European | 25,297 | 0 | 4 | 100 | −38 % |
| African | 934 | 0 | 14 | 34 | 10 % |
| Western Pacific | 209 | 0 | 0 | 1 | −83 % |
| Eastern Mediterranean | 72 | 0 | 1 | 0 | −100 % |
| South-East Asia | 30 | 0 | 1 | 1 | −83 % |
| Total | 77,115 | 3,610 | 36 | 1,152 | −47 % |
Note:1Using the most recent, complete, international standard week (Monday–Sunday). TCC is the total confirmed cases, TPC is the total probable cases, TD is total deaths, CPW is cases in the past week, 7dCC is the 7-day % change in cases.2
2. Methods
EpiSIX is a prediction system based on a general SEIR epidemic model.7, 8 The functional control efficacy of the SEIR model includes non-pharmaceutical intervention (NPI), vaccination and natural immunity, which describes the increasing (or decreasing) control efficacy when the control strategies are operated strictly (or loosely). Based on data for the monkeypox epidemic from the USA CDC and the WHO,1, 2 we used EpiSIX to estimate the main parameters of this monkeypox epidemic, and to predict its tendencies in the USA, Europe and other global regions.
3. Results
3.1. Parameter settings for EpiSIX simulation
It has been reported1 that the proportion of asymptomatic cases of monkeypox is slightly higher than 13.0 %, which is close to that of SARS.7 In the EpiSIX simulation, the initial proportion of monkeypox asymptomatic cases was set in the range 13.0 %–15.0 %. The efficiency of existing smallpox vaccination in monkeypox patients is estimated to be ∼ 85 % based on data from the US CDC.2 We used a lower, more cautious value of 75 % as a comparison for our EpiSIX simulation. Both vaccine efficacy against susceptibility (VEs) and vaccine efficacy against infectiousness (VEi) were set in the range 75.0 %–85.0 %. Finally, the half-life of antibody was set at 720 days, based on known smallpox vaccine data.
3.2. Estimation of the VEs, VEi and NPI efficacy
During this monkeypox epidemic, the ring vaccination strategy (mainly targeting vaccination of infected individuals and their close contacts) has been applied worldwide. The efficient coverage rate is computed by two values: the number of individuals who received vaccination, and the number of probable susceptible individuals. The number of individuals who received vaccination is easy to check, but estimation of the number of probable susceptible individuals must be performed carefully. For example, as of October 21, 2022, the cumulative number of confirmed cases in the USA was 27,881, with circa 600,000 smallpox vaccines being administered at two doses per individual, giving an estimated number of vaccinated individuals of ∼ 300,000. The percentage of the population constituted by MSM in the USA is about 2.0 % (i.e., circa 6.6 million in total), thus the coverage rate of the smallpox vaccine among the MSM population in the USA is ∼ 4.55 %. However, ring vaccination focuses on infected individuals and their close contacts. It is reasonable to assume that the number of close contacts to each infected individual ranges from 15 to 20. This yields the number of susceptible individuals to be ∼ 432,000–567,000 and the efficient coverage rate of the smallpox vaccine of ∼ 52.9 %–69.4 %. EpiSIX simulations on the monkeypox epidemic of 2022 in the USA and Europe showed that the VEs was in the range 78.7 %–79.1 % and VEi was in the range 76.0 %–81.9 %, with an efficient coverage rate of 63.6 %–65.8 %. This revealed that the efficiency of the smallpox vaccine is similar between the USA and Europe (Table 2 ).
Table 2.
Estimation of the efficiency of the smallpox vaccine and non-pharmaceutical intervention (NPI).
| Region | VEs (%) | VEi (%) | Max. Vaccine coverage rate (%) | Max. NPI (%) |
|---|---|---|---|---|
| USA | 78.7 | 76.0 | 65.8 | 49.5 |
| Europe | 79.1 | 81.9 | 63.6 | 51.8 |
| Global | 79.1 | 77.7 | 53.5 | 52.0 |
The NPI efficiency is derived from the control and management of the total population when the alert level is raised, and the efficient management of close contacts when ring vaccination is underway. EpiSIX estimated that the NPI efficiency started at zero and increased to 49.5 % (in the USA, as of October 21, 2022) and 51.8 % (in Europe, as of October 24, 2022). The NPI efficiency in Europe is therefore ∼ 2 % higher than that in the USA.
3.3. Possible scales of the monkeypox epidemic
We considered the scenario in which vaccination was carried out without NPI (Scenario A) and NPI was carried out without vaccination (Scenario B), to allow for assessment of the management of the epidemic. For Scenario B, the simulations revealed that the possible cumulative number of infected individuals for the USA and Europe were 4.47 million and 3.56 million, respectively, within 200 days. As mentioned above, the NPI efficiency in Europe was ∼ 2 % higher than that of the USA, so the possible number of infected individuals would be lower for Europe under Scenario B (Table 3 ).
Table 3.
Other estimated parameters, and prediction of the possible epidemic scales within 200 days.
| Region | Theoretical number of initial cases | Theoretical number of vaccinated cases among all cases | Awareness delay (day) | Possible infected number with Scenario A (10 k) | Possible infected number with Scenario B (10 k) |
|---|---|---|---|---|---|
| USA | 4 | 9,403 | 15 | 447 | 19 |
| Europe | 67 | 9,811 | 14 | 356 | 279 |
| Global | 77 | 25,362 | 14 | 613 | 891 |
Note: It is assumed that there is a delay during which healthcare professionals and epidemiologists become aware of a new outbreak, which is presented as an awareness delay in this table.9
3.4. Estimation of the R0 and incubation period
The value of the basic reproduction number, R0, and the length of the incubation period were two important parameters for epidemic management. Our study showed that the value of R0 for monkeypox was near to 3.1 (Table 4 ), which is close to that of SARS, and is lower than that of SARS-CoV-2 (with an R0 value in the range 5.6–6.0 for Omicron variants). Our study also showed that 94.7 % of infected individuals completed the incubation period and showed symptoms within 20 days, and 88.5 % of infected individuals showed symptoms within 15 days, which supports the control measure of isolating close contacts for a period of 20 days. Our findings also revealed that 96.9 % of infected individuals recovered within two weeks after the confirmation of symptoms (Table 5 ).
Table 4.
Estimation of the parameters of the monkeypox epidemic.
| Region | Mean incubation period (95 % CI) | Mean infectious period (95 % CI) | Mean generation time (95 % CI) | Asymptomatic (%) | R0 |
|---|---|---|---|---|---|
| USA | 8.13 (4.9, 19.5) | 4.01 (1.6, 11.6) | 10.66 (5.3, 16.0) | 13.1 | 3.167 |
| Europe | 8.08 (4.8, 21.0) | 3.89 (1.6, 12.1) | 10.36 (5.2, 15.5) | 14.5 | 3.126 |
| Global | 8.23 (4.9, 21.4) | 3.77 (1.5, 11.7) | 10.38 (5.2, 16.6) | 14.3 | 3.012 |
| [8] | 9.10 (6.5, 10.9) | 12.50 (7.5, 17.3) | 1.82–3.26 |
Table 5.
Probability of a monkeypox-infected individual completing the incubation period / infectious period within the given number of days.
| Probability (%) | 5d | 10d | 15d | 20d | 25d |
|---|---|---|---|---|---|
| For incubation | 35.0 | 72.7 | 88.5 | 94.7 | 97.3 |
| For infectiveness | 73.4 | 91.5 | 96.9 | 98.7 | 99.5 |
3.5. Tendency of the 2022 monkeypox epidemic
Next, the data sources used in this study and the tendency predictions for the monkeypox epidemic are discussed in detail.
3.5.1. Tendency in the USA
The first monkeypox case was reported by the USA CDC on May 10, 2022. As of October 21, 2022, the cumulative number of reported cases was 27,881. During this monkeypox epidemic, the alert level in the USA was raised to Level 2, which is defined as “transmission within a defined sub-population with high numbers of close contacts”. A total of 600,000 smallpox vaccine doses2 have been administered, with two doses administered per individual. Among these, 550,000 doses were administered to the MSM population. Correspondingly, the number of vaccinated individuals was circa 300,000. EpiSIX simulations revealed that the monkeypox epidemic in the USA would reach low epidemic status in the near future (Fig. 1 ).
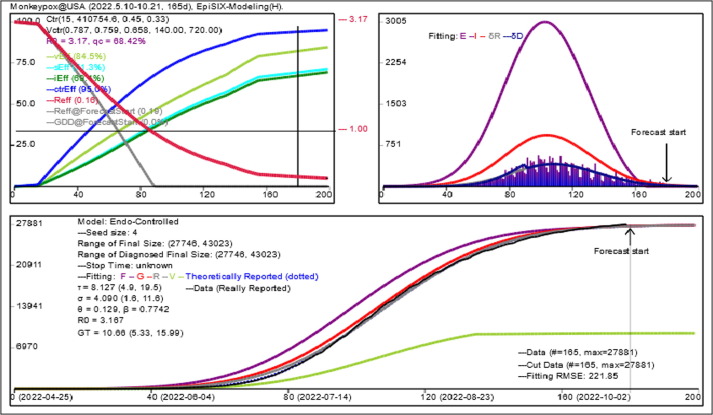
Fig. 1.
EpiSIX simulates the outbreak of monkeypox in the USA based on 165-day data from 2022.5.10 to 2022.10.21. Left top panel: The values for all control efficiencies used in the simulation. vEff is the efficiency of vaccination, iEff is the control efficiency for infectious individuals, sEff is the control efficiency for susceptible individuals, and ctrEff is the comprehensive efficiency for vEff and NPI, where NPI is the comprehensive efficiency generated by sEff and iEff. The red curve is the effective reproduction number, the gray curve is the degree of diagnosis,8 which measures the error between the number of reported cases and theoretical cases decreasing from 100% to 0. Right top panel: The block bars indicate the daily number of new confirmed cases, the purple/red/gray/blue curve is the theoretical daily number of exposed/infectious/recovered or died/confirmed individuals. Bottom panel: The black curve is the cumulative number of reported cases, the other curves are the theoretical numbers of cumulative cases. The green curve is the theoretical cumulative number of vaccinated cases among all cases, the purple/red/gray/blue (dotted) curve is the theoretical cumulative number of exposed/infectious/recovered or died/confirmed individuals. The root mean square error (RMSE) was used to measure the error between theoretical cumulative numbers and the real cumulative numbers for reported cases. Epidemic parameters and NPI efficiency were estimated directly by minimizing RMSE in EpiSIX. τ is the mean incubation period, σ is the mean infectious period, θ is the percentage of asymptomatic cases, β is the mean infection rate, R0 is the basic reproduction number and GT is the generation time.8
3.5.2. Tendency in the European Region
The first monkeypox case was reported by the UK CDC on May 2, 2022. As of October 24, 2022, the cumulative number of reported cases was 25,297. The effective vaccine coverage rate for Europe was close to that of the USA. For example, as of the first half of October 2022, 110,000 vaccine doses had been administered in France6 compared with 600,000 vaccine doses in the USA, giving a vaccine dose ratio of 18.3 % for France compared with the USA, which is similar to the ratio of the total population size between France and the USA (20.27 %, total population size of France is ca. 67.5 million compared with ca. 333.0 million for the USA). In this study, we assumed that the efficient coverage rates for Europe and the USA were within the same range of 52.9 %–69.4 %. The alert level for the monkeypox epidemic in Europe was raised to Level 3, which is defined as “transmission within multiple sub-populations or larger sub-populations”, compared with the lower Level 2 in the USA. EpiSIX simulations revealed that control efficiency in Europe was higher than that in the USA, and that the monkeypox epidemic in Europe would enter low epidemic status in the near future.
3.5.3. Tendency in the global Region
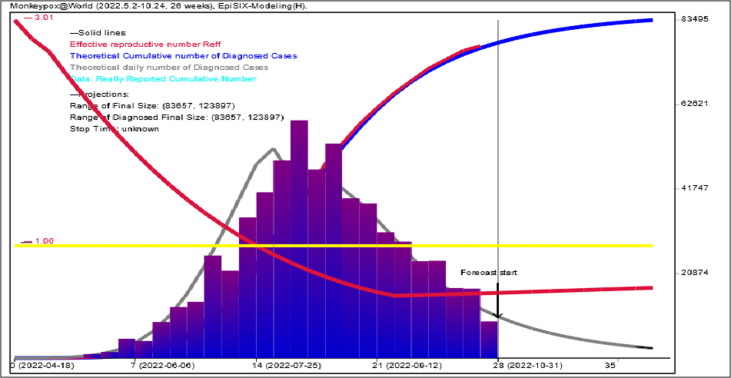
The first monkeypox case of the recent epidemic wave was reported by the UK CDC on May 2, 2022, which was the beginning of the new global outbreak of monkeypox. As of October 28, 2022, the cumulative number of reported cases was 77,115, with a total of 36 deaths. We assumed that the global vaccine coverage rate was the same as that of the USA, i.e., within the range 52.9 %–69.4 %. EpiSIX simulations revealed that, as of March 1, 2023, the global monkeypox epidemic will enter low epidemic status (i.e., the daily number of new confirmed cases will be under 100), and the cumulative number of confirmed cases will range from 85,000 to 124,000 (Fig. 2 ). Moreover, the total number of deaths will range from 60 to 87, under the case-fatality rate of 0.7005 per 1,000.
Fig. 2.
EpiSIX simulates the outbreak of monkeypox for the global region based on 182-day data from 2022.5.2 to 2022.10.24. The time unit is a week. If the effective reproduction number Reff is less than 1.0 (yellow line), then the outbreak is under control; otherwise, the outbreak is out of control. The blue block bars show the daily number of confirmed cases reported by the WHO and the gray curve presents its theoretical values. The blue curve shows the theoretical cumulative number of confirmed cases.
4. Conclusion
The EpiSIX prediction system was established based on the SEIR epidemic model, and was used to estimate the epidemic parameters of monkeypox, yielding the following results: the basic reproduction number R0 of MPXV is near to 3.1, the percentage of asymptomatic individuals is 13.1 %–14.5 %, which is close to that of SARS.7 The vaccination efficiency of the individuals who had monkeypox is ∼ 80 %. The mean incubation period of monkeypox is 8 days. In total, 95 % of infected individuals show symptoms within 20 days, and recover within 2 weeks after the confirmation of symptoms. The simulations revealed that ring vaccination is remarkably effective for controlling the monkeypox epidemic, and the study confirms that a 20-day isolation of close contacts is necessary.
EpiSIX simulations also revealed that, as of March 1, 2023, the global monkeypox epidemic will enter low epidemic status (i.e., a daily number of new confirmed cases of under 100), and the cumulative number of confirmed cases will range from 85,000 to 124,000 (the current cumulative number of confirmed cases is 77,115), with a total of 60 to 87 deaths under the case-fatality rate of 0.7005 per 1,000 (i.e., the empirical estimation is 1.5 times the current case-fatality rate of 0.467 as of October 28, 2022).
CRediT authorship contribution statement
Fengying Wei: Writing – original draft. Zhihang Peng: Conceptualization. Zhen Jin: . Jinjie Wang: Conceptualization. Ximing Xu: Conceptualization. Xinyan Zhang: Conceptualization. Jun Xu: Conceptualization. Zixiong Ren: Conceptualization. Yao Bai: Conceptualization. Xiaoli Wang: Conceptualization. Bulai Lu: Conceptualization. Zhaojun Wang: Supervision, Methodology. Jianguo Xu: Supervision, Methodology. Senzhong Huang: Writing – original draft, Methodology, Software.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was supported by grants from the Consultancy Project by the Chinese Academy of Engineering (CAE, 2022-JB-06), the Natural Science Foundation of Fujian Province (2021 J01621), the National Natural Science Foundation of China (No. 61873154) and the National Key R&D Program of China (2021ZD0114102).
References
- 1.Monkeypox, World Health Organization. https://www.who.int/health-topics/monkeypox. Updated Oct. 28, 2022.
- 2.Monkeypox, Centers for Disease Control and Prevention, USA CDC. https://www.cdc.gov/poxvirus/monkeypox/index.html. Updated Oct.28, 2022.
- 3.Ogoina D. Sexual behaviours and clinical course of human monkeypox in Spain. Lancet. 2022 doi: 10.1016/S0140-6736(22)01497-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Public Health England. https://www.gov.uk/government/organisations/public-health-england.
- 5.Girometti N., Byrne R., Bracchi M., et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis. 2022 Sep;22(9):1321–1328. doi: 10.1016/S1473-3099(22)00411-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministère De La Santć Et De La Prćvention. https://solidarites-sante.gouv.fr.
- 7.Huang S. A new SEIR model with applications to the theory of eradiction and control of diseases, and to the calculation of R0. Math Biosci. 2008;215:84–104. doi: 10.1016/j.mbs.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Huang S., Peng Z., Jin Z. Studies of the strategies for controlling the COVID-19 epidemic in China: Estimation of control efficacy and suggestions for policy makers. Sci Sinica Math. 2020;50(6):885–898. [Google Scholar]
- 9.Huang S., Wei F., Peng Z., et al. Assessment method of coronavirus disease 2019 outbreaks under normal prevention and control. Disease Surveill. 2020;35(08):679–686. [Google Scholar]
- 10.Guzzetta G, Alessia M, Federica F, et al. Early estimates of Monkeypox incubation period, generation time, and reproduction number, Italy, May-June 2022. Emerging Infect Disease. 2022; 28(10). https://wwwnc.cdc.gov/eid/article/28/10/22-1126_article. [DOI] [PMC free article] [PubMed]