Abstract
Surgical tracheostomy is a high aerosol-generating procedure that is an essential aid to the recovery of patients who are critically ill with COVID-19 pneumonia. We present a single-centre case series of 16 patients with COVID-19 pneumonia who underwent tracheostomy. We recommend that the patient selection criteria for achieving a favourable outcome should be based on fraction of inspired oxygen together with prone-position ventilation. As with any challenging situation, the importance of effective communication is paramount. The critical modifications in the surgical steps are clearly explained. Timely tracheostomy also leads to an earlier freeing up of ventilator space during a period of a rapidly escalating pandemic. The outcomes in terms of swallow and speech function were also assessed. The study has also helped to remove the anxiety around open a tracheostomy in patients who are COVID-19 positive.
Keywords: COVID-19, Tracheostomy, Surgical tracheostomy, FiO2 in tracheostomy, Proned ventilation in tracheostomy
Background
COVID-19, the infectious disease caused by the most recently discovered coronavirus, is a pandemic affecting many countries globally and poses an extreme challenge to healthcare systems. The literature suggests that 5% of affected patients are critical, having respiratory failure, septic shock or multi-organ failure.1 In 26–32% of patients who are hospitalised, mechanical ventilation in the intensive care setting is required.2,3 According to the Intensive Care National Audit and Research Centre, 63.2% of the patients admitted to intensive care in UK needed mechanical ventilation within the first 24 hours.4 A subset of these patients needed tracheostomy to help wean them from ventilation.
The primary modes of spread of COVID-19are droplet infection and aerosols. It is suspected that approximately 29% of infected healthcare workers acquired the virus in hospital.2 Tracheostomy is a high-risk procedure in terms of aerosol generation and cross-contamination.5
We present a single-centre case series of patients with COVID-19 pneumonia who underwent tracheostomy. Our primary aim was to look at the timing of the tracheostomy based on the fraction of inspired oxygen (FiO2) and the need for prone ventilation as a marker of favourable outcome. We also highlight the critical modifications made to the procedure to minimise the risk of aerosol generation. The outcomes in terms of swallow and speech function were also assessed. The importance of proper planning and preoperative preparation for the management of these patients was of vital importance. The study helps to fill the gaps in the existing literature on the topic.
Case history
We prospectively analysed data for a cohort of 16 patients with COVID-19 who had tracheostomy, from 1 April 2020 to 20 May 2020. The hospital audit department approved the study. Ethical approval was deemed unnecessary as the study did not involve any new procedure. All patients with COVID-19 pneumonia (positive polymerase chain reaction swab) who were intubated and ventilated and had tracheostomies (n = 16) were included in the study. Patients having tracheostomy for any other reason during the period were excluded.
The decision to perform a tracheostomy should not be taken lightly, as it is a high-risk aerosol-generating procedure. In Luton and Dunstable Hospital, open tracheostomy was agreed by both ear, nose and throat surgeons and intensivists in favour of a percutaneous technique, which the literature suggests leads to more aerosolisation through the bronchoscopic port and repeated dilatations.6 The percutaneous technique also requires repeated opening of the ventilator circuit.7 Additionally, evidence suggests that percutaneous techniques are associated with increased technical difficulties when compared with surgical open tracheostomies.8 Guidelines therefore relate mainly to open techniques, although in some units percutaneous procedures may be preferred. All procedures were performed in the dedicated COVID-19 theatre, which reduced the stress of an overstretched intensive care unit and the risk of cross-contamination. The size of the theatre team was kept to a minimum. To avoid risk of infection through vapour plumes, ties were used to ligate vessels and the thyroid isthmus as required. Only monoploar diathermy with a vacuum extractor device was used, and only where absolutely necessary. Closed inline suction with attached viral filter was used for airway suctioning.
During the procedure, the personal protective equipment (PPE) worn consisted of fit-tested N95 (FFP3) mask, full-sleeve gown, double gloves, face/eye protection and shoe covers following the systematic donning and doffing sequence. No additional protection was used.
The procedure was carried out on the critical care bed to reduce the risk of disconnection in transferring patients attached with multiple tubes and wires. Anaesthetic principles were mainly to minimise disconnections, ensure total paralysis to minimise coughing and spluttering, and stopping ventilation of the patient when the trachea was opened. The patient’s neck was extended using a shoulder bolster without using a head ring. A four-towel drape was used to drape the patient. A clear plastic sheet was taped to the body towel covering the operative site, which protected the surgical team from plumes if monopolar diathermy had to be used. The head and face were kept free from drapes to allow the anaesthetist easy access to the endotracheal tube.
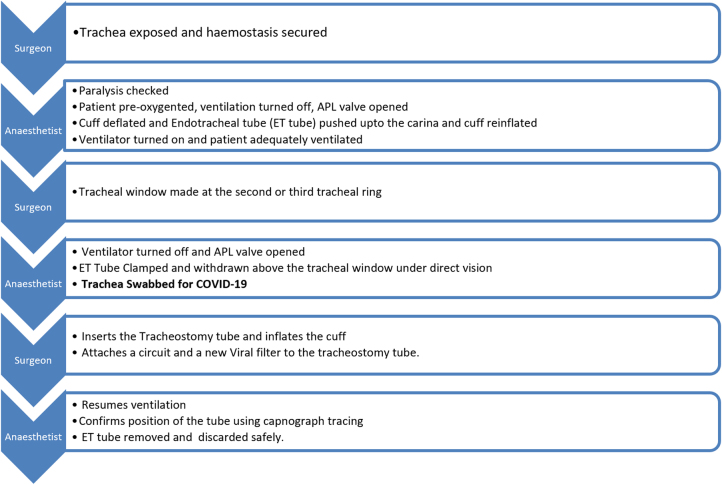
The initial surgical steps of tracheostomy are no different compared with the pre-COVID-19 era. The critical differences are essentially once the trachea is exposed and the surgeon is about to perform the tracheotomy. The critical steps are shown in Figure 1.
Figure 1 .
Surgical steps of tracheostomy (adapted and locally modified from the ENT UK COVID-19 Tracheostomy Framework, 6 April 2020: www.entuk.org).9
Brief periods of apnoea are expected. The lowest oxygen saturation reached in our study was 60%. No patient had an adverse outcome with the drop in saturation. Clear and loud communication among the surgical teams at this point was an essential requirement.
Sixteen patients (male to female ratio 3 : 1) with an age range of 37–70 years (mean 49.12 years) had a tracheostomy. All patients were intubated and ventilated for COVID-19 pneumonia. The average duration of intubation prior tracheostomy was 16.1 days (range 12–32 days). The FiO2 on the day of tracheostomy ranged from 0.3 to 0.65. Inotropic support was minimal for all patients on the day of the procedure. The C-reactive protein trend was taken as a marker of progression of the inflammatory response, and a downward trend was noted in all cases on the day of the procedure. Fourteen patients were successfully decannulated. Unfortunately, three patients died within the same episode of hospital admission, one of whom was successfully decannulated. The average time of step down from intensive care for decannulated patients was 11 days. The swab for COVID-19 taken from the trachea during the procedure was positive for two patients.
In terms of functional patient outcomes, data were collected by speech and language therapy team regarding the ability to safely commence oral intake. Depending on sedation, ventilation, medical status and ability to engage, the mean time between insertion of tracheostomy and first speech and language therapy contact was 7.9 days, indicating that patients were ready for a swallow or communication assessment within this time. Patients were seen by speech and language therapy on average 3.7 times prior to decannulation. Functional oral intake was rated at the time of initial speech and language therapy contact, and at the time of decannulation using the Functional Oral Intake Scale for Dysphagia (FOIS).10 Although no formal outcome measure was used for communication, by the time of decannulation, all patients seen by speech and language therapy had a functional voice, and were communicating effectively in full sentences. Successful outcome in terms of decannulation with a good cough and swallow following tracheostomy was 87.5%.
Discussion
High-risk procedures in patients having highly infectious disease should be balanced between the risks of exposure to healthcare professionals and optimising patient care. The indication for tracheostomy in patients with COVID-19 remains unchanged from normal practice. The consensus among otolaryngologists and intensivists is that tracheostomy should be considered in patients requiring prolonged mechanical ventilation, because of the resulting benefits of reduced effort of breathing and improved weaning and patient communication. Tracheostomy also helps avoid adverse outcomes such as subglottic or tracheal stenosis. Minimal evidence exists for early tracheostomy being performed in patients with COVID-19 who are ventilated for less than 14 days. Additionally, tracheostomy prevents patients from being able to lie in a prone position, which has been shown to improve oxygenation in patients who require mechanical ventilation support for the management of acute respiratory distress syndrome.11,12 There is also evidence that prone positioning could prevent ventilator-induced lung injury.13,14
The British Laryngological Association tracheostomy guidelines for patients with COVID-19 and the ENT UK Framework for open tracheostomy in patients with COVID-19 suggest that tracheostomy is unlikely to be indicated below day 14 of ventilation.9,15 Other organisations suggest only performing tracheostomies in patients with prolonged periods of intubation, defined as more than 21 days.6 Our average time to tracheostomy from intubation was 16.1 days, which is in accordance with the British Laryngological Association guidelines and ENT UK Framework.
The findings from our study suggest that consideration should be given to tracheostomy in patients with COVID-19 who are intubated at the earliest point from day 14. Timing of tracheostomy was based on the used FiO2 on the day of the procedure and the need for prone ventilation. Patients with very high FiO2 (>0.5) are deemed unstable from a respiratory viewpoint, resulting in poor outcomes. In addition, patients who have had tracheostomies cannot be safely placed in the prone position and hence lose the benefit of ventilation in that position. Our average FiO2 prior to tracheostomy was 0.468 (0.3–0.7). Anecdotal data suggest that tracheostomy beyond 14 days leads to increased incidence of critical care myopathy and worsening functional outcome. Two patients who died prior to decannulation had FiO2 greater than 0.6 on the day of the procedure. These procedures were performed at the early stage, as we were still at the learning phase of treating the disease. We submit this as a learning point and revised our selection criteria of patients for tracheostomy is as follows:
-
•
14 days post-intubation
-
•
one failed attempt of extubation of endotracheal tube
-
•
FiO2 less than 0.5
-
•
48 hours since the last deproning.
We found an average time of intensive-care step-down from tracheostomy of 11 days, supporting the indication for tracheostomy in these patients.
PPE is important to protect healthcare workers. With our usage of PPE, no positive cases occurred in our tracheostomy team, which was led by the senior author. The emphatic requirement for using adequate PPE was evident as the tracheal swabs for COVID-19 tested positive for two patients.
Conclusion
In summary, tracheostomy is an essential aid to the recovery of patients with COVID-19 who are critically ill and being mechanically ventilated. Delaying tracheostomy offers no additional benefit and leads to poorer functional outcome as a result of prolonged sedation. Careful patient selection based on FiO2 and need for prone ventilation results in better outcome. Timely tracheostomy helps to quicken the weaning of patients from ventilators, which are freed up sooner than otherwise. Within a small sample size, we show that performing tracheostomy in ventilated patients at around day 16 has had good outcomes. Despite being a high-risk aerosol-generating procedure, using regular PPE and adhering to a systematic donning and doffing sequence resulted in zero healthcare associated transmission. The role of effective communication between the surgeon and anaesthetist during every stage of the procedure is equally important. Further studies are required with larger sample sizes and in multiple centres to establish an optimal timing for tracheostomy.
References
- 1.Wu Z, McGoogan JM. . Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 2.Wang D, Hu B, Hu Cet al. . Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061–1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li Xet al. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Intensive Care National Audit and Research Centre. ICNARC Report on COVID-19 in Critical Care: England, Wales and Northern Ireland, 6 November 2020. London: ICNARC; 2020. [Google Scholar]
- 5.Broderick D, Kyzas P, Sanders Ket al. . Surgical tracheostomies in COVID-19 patients: important considerations and the ‘5Ts’ of safety. Br J Oral Maxillofac Surg 2020; 58: 585–-589. 10.1016/j.bjoms.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chao TN, Braslow BM, Martin NDet al. . Tracheotomy in ventilated patients with COVID-19. Ann Surg 2020; 272: e30–e32. 10.1097/SLA.0000000000003956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tay JK, Khoo ML, Loh WS. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg 2020; 146: 517–518. 10.1001/jamaoto.2020.0764 [DOI] [PubMed] [Google Scholar]
- 8.Putensen C, Theuerkauf N, Guenther Uet al. . Percutaneous and surgical tracheostomy in critically ill adult patients: a meta-analysis. Crit Care 2014; 18: 544. 10.1186/s13054-014-0544-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harrison L, Ramsden J, Winter Set al. . Tracheostomy guidance during the COVID-19 Pandemic ENT UK 19 March 2020. https://www.entuk.org/tracheostomy-guidance-during-covid-19-pandemic (cited November 2020).
- 10.Crary MA, Carnaby-Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005; 86: 1516–1520. 10.1016/j.apmr.2004.11.049 [DOI] [PubMed] [Google Scholar]
- 11.Guérin C. Prone ventilation in acute respiratory distress syndrome. Eur Respir Rev 2014; 23: 249–257. 10.1183/09059180.00001114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valter C, Christensen AM, Tollund C, Schønemann NK. Response to the prone position in spontaneously breathing patients with hypoxemic respiratory failure. Acta Anaesthesiol Scand 2003; 47: 416–418. 10.1034/j.1399-6576.2003.00088.x [DOI] [PubMed] [Google Scholar]
- 13.Broccard A, Shapiro RS, Schmitz LLet al. . Prone positioning attenuates and redistributes ventilator-induced lung injury in dogs. Crit Care Med 2000; 28: 295–303. 10.1097/00003246-200002000-00001 [DOI] [PubMed] [Google Scholar]
- 14.Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome rationale, indications, and limits. Am J Respir Crit Care Med 2013; 188: 1286–1293. 10.1164/rccm.201308-1532CI [DOI] [PubMed] [Google Scholar]
- 15.British Laryngological Association. COVID 19 BLA Tracheostomy Guideline. London: BLA; 2020. https://www.britishlaryngological.org/news/tracheostomy-guideline-covid-19 (cited November 2020). [Google Scholar]