Abstract
Aggressive angiomyxoma is a rare mesenchymal tumour, primarily arising in the soft tissue of the pelvis and perineum in women of reproductive age. There is a paucity of evidence on optimal management because of the rarity of these tumours, but the consensus has been for surgical excision. We present the case of a 65-year-old woman who was admitted with left-sided buttock pain and initially diagnosed with a perianal abscess. She underwent examination under anaesthesia rectum with surgical excision of the lesion, subsequent histopathological and immunochemical analysis was suggestive of aggressive angiomyxoma. To complement our case report, we also present a literature review focusing on aggressive angiomyxoma in the ischioanal fossa (also known as the ischiorectal fossa) with only eight cases of primary aggressive angiomyxoma involving the ischioanal fossa documented to date. The primary aims of this case report and literature review are to familiarise clinicians with the clinical, histopathological and immunochemical features of these tumours, and to increase appreciation that despite the rarity of aggressive angiomyxoma, it might be considered in the differential diagnosis of ischioanal lesions.
Keywords: Angiomyxoma, Ischioanal fossa, Mesenchymal tumour
Background
Aggressive angiomyxoma is a rare mesenchymal tumour, primarily arising in the soft tissue of the pelvis and perineum in women of reproductive age, first described by Steeper and Rosai.1 The tumours are usually benign but highly infiltrative with a high predilection for local recurrence.2 To date, just over 400 cases have been reported in the literature and despite being described as an indolent neoplasm, three cases of metastatic disease have been documented.2
The mainstay of treatment is surgical excision and there has been some success with hormonal management.3 Owing to the rarity of these tumours there is a paucity of evidence on optimal management, but the general consensus is for complete surgical excision with tumour-free margins.4
We present a case report of aggressive angiomyxoma in a post-menopausal woman initially diagnosed as a perianal abscess and review the current literature.
Case history
A 65-year-old woman with a background of hypertension, chronic obstructive pulmonary disease and hypothyroidism presented with a three-week history of left-sided buttock pain, radiating to the thigh. There were no gastrointestinal or urinary symptoms and no red flag features. On examination, the abdomen was soft and non-tender. Digital rectal examination revealed an exquisitely tender area perianally but no discharge or overlying cutaneous changes.
Blood tests showed raised inflammatory markers and the patient was commenced on intravenous antibiotics with a provisional diagnosis of a deep-seated perianal abscess. Magnetic resonance imaging (MRI) of the pelvis revealed a large ovoid encapsulated lesion measuring approximately 6.4×5.5×9.4cm (anteroposterior × transverse × craniocaudal) predominantly located in the left inferior aspect of the pelvic cavity with extension into the ischioanal fossa (Figures 1 and 2). The lesion's contents were predominantly of fluid signal, so the initial diagnosis was of an abscess.
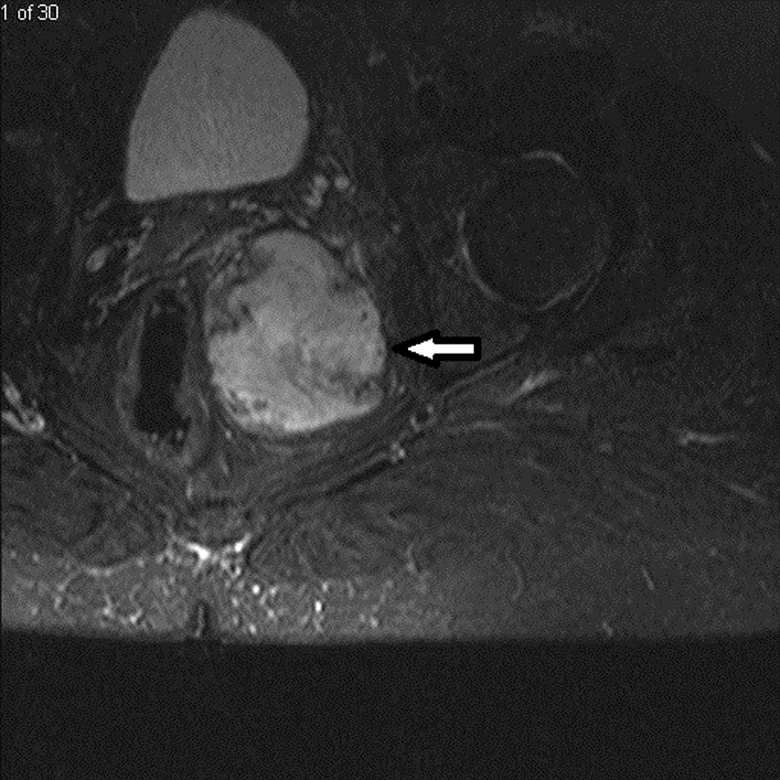
Figure 1 .
Magnetic resonance image of the pelvis; the axial short tau inversion recovery image showing a well-defined soft-tissue signal intensity mass (white arrow). The mass is predominantly located in the left inferior aspect of the pelvic cavity with extension into the ischioanal fossa, medial to the left obturator internus muscle and lateral to the distal rectum.
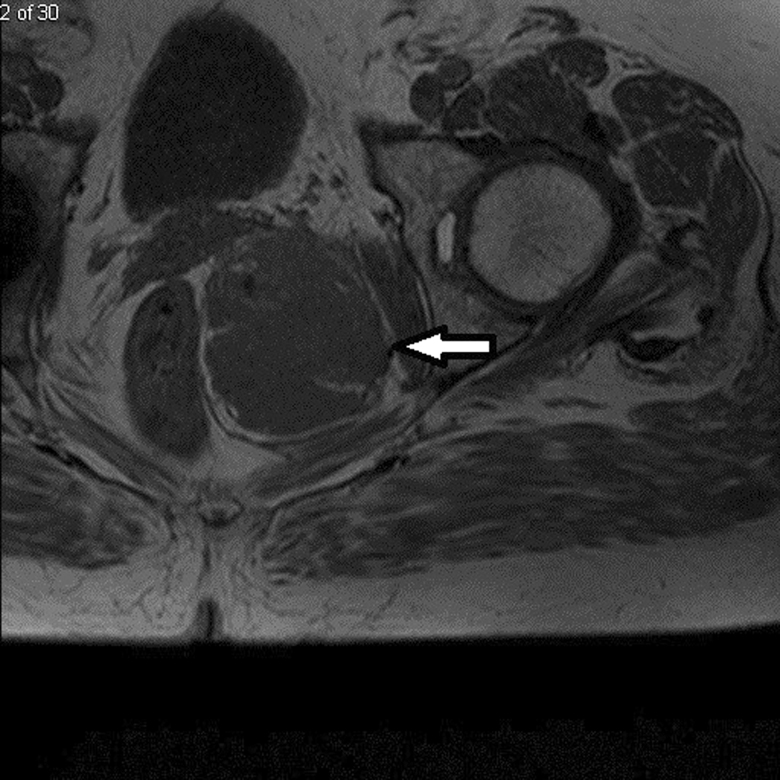
Figure 2 .
Magnetic resonance image of the pelvis (axial T1 view) showing a well-defined soft-tissue signal intensity mass (white arrow). The mass is predominantly located in the left inferior aspect of the pelvic cavity with extension into the ischioanal fossa, medial to the left obturator internus muscle and lateral to the distal rectum.
Based on the MRI findings and the clinical suspicion of a perianal abscess, the patient was taken to theatre for examination under anaesthesia per rectum (with or without incision and drainage of perianal abscess). Intraoperatively, a 3cm incision was made in the left ischioanal fossa and a 6×8cm cystic lump was removed piecemeal and sent for histological analysis. Approximately 500ml blood loss was recorded. The wound was left open and was packed at the end of the procedure. Because of the significant blood loss and the patient experiencing a vasovagal episode, she was kept in hospital overnight for observation. She made an uneventful recovery and was discharged the next day with follow-up arranged both in the community for wound management and in the outpatient department.
Histology of the lump showed hypocellular spindle-shaped cells and collagen-containing stroma with no atypical/mitotic activity and numerous thin- and thick-walled blood vessels in a myxoid background. Immunohistochemically, the cells tested positive for desmin, vimentin, estrogen and progesterone and negative for HMGA2, smooth muscle actin (SMA), H-caldesmon, CD34, AE1/3, CAM5.2, S100, CD117 and ALK1. The histopathological conclusion was of aggressive angiomyxoma.
Computed tomography (CT) of the chest, abdomen and pelvis was arranged five weeks postoperatively to exclude metastatic disease, given the finding of aggressive angiomyxoma rather than a simple abscess. This found soft-tissue swelling consistent with a residual mass, but there was no evidence of metastatic disease (Figure 3). At follow-up in the outpatient department, the patient's symptoms had completely resolved and her wound had healed.
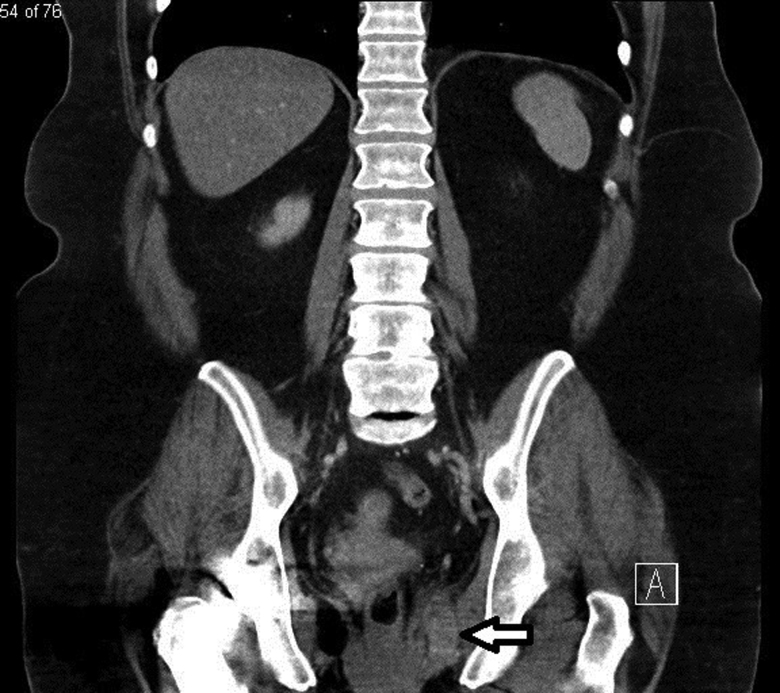
Figure 3 .
Intravenous-enhanced computed tomography of the abdomen and pelvis in portal venous phase. The coronal view shows a fairly well defined residual soft-tissue density mass (white arrow), following surgery.
She was initially referred to the sarcoma multidisciplinary team at the local tertiary centre for further management and was subsequently commenced on letrozole (an aromatase inhibitor and anti-estrogen). She has since been discharged from the sarcoma service (as the lesion is not regarded as a sarcoma) and remains under the care of the regional gynaecological oncology team, who have arranged repeat MRI (three months post-CT) and initial conservative management with surveillance imaging.
Discussion
Aggressive angiomyxoma is a rare but well-described mesenchymal tumour occurring mostly in the pelvic and perineal region of females,1 with over 400 cases documented in the medical literature. Aggressive angiomyxoma is considered a benign tumour with locally invasive properties and a predilection to local recurrence.5 However, three cases of distant metastatic disease have been reported.2 Most cases occur in women, with a female to male ratio of 6.6:1, with peak incidence in the third decade (age range 9 months to 82 years).6 Of significance, a large percentage of tumours are positive for estrogen and progesterone hormone receptors, which suggests a pathogenic association with female sex hormones.5
Although cases typically occur in the pelvic and perineal regions, rarer locations have been described. To date, only eight cases of primary aggressive angiomyxoma involving the rectum/ischioanal fossa have been documented, so the present case, initially diagnosed as a perianal abscess, augments the existing literature and supports the possibility of aggressive angiomyxoma as a differential diagnosis of ischioanal lesions. An initial diagnosis of aggressive angiomyxoma is usually challenging and is frequently misdiagnosed as a gynaecological malignancy, benign vulval lesion or groin hernia.3 Most cases are diagnosed retrospectively after histological analysis post-surgical excision.3 In the present patient, aggressive angiomyxoma was initially misdiagnosed as an ischioanal abscess and she was examined under anaesthesia with subsequent surgical excision.
The characteristic findings of aggressive angiomyxoma on diagnostic imaging include, on ultrasonography, the appearance of a cystic, hypoechoic mass; on CT an attenuated mass is seen and on MRI there is a characteristic ‘swirl’ pattern with high signal intensity on T2-weighted images.7 Imaging also has an essential role in the management of these tumours as the size and extent of deep tissue involvement is often not appreciated on clinical assessment alone.8
Histologically, aggressive angiomyxomas are composed of myxoid stroma with intermixed collagen fibres and dilated, thick-walled vessels.3 Cells are commonly hypocellular with spindled or stellate fibroblasts, and no atypical mitoses.1 Histological analysis in this case and the previous cases of rectal/ischioanal aggressive angiomyxoma demonstrated a spindle cell neoplasm with numerous blood vessels in a myxoid background, highly suggestive of aggressive angiomyxoma.
Immunohistochemical analysis has found aggressive angiomyxoma to be frequently positive for desmin, vimentin, CD 34, estrogen and progesterone receptors, and negative for S100 protein, but this can be variable.9 Table 1 describes the eight cases of rectal/ischioanal aggressive angiomyxoma found during our literature search and relevant immunohistochemical features. In our patient, immunostaining was positive for desmin, vimentin, estrogen and progesterone, and was negative for, SMA, AE1/3 and S100, which supports the diagnosis of aggressive angiomyxoma.
Table 1 .
Previously reported cases of aggressive angiomyxoma in the ischiorectal/ischioanal fossa
| Study | Study design | Age/sex | Clinical presentation | Imaging | Management | Macroscopic findings | Histopathology | Immunohistochemistry | Recurrence |
|---|---|---|---|---|---|---|---|---|---|
| Nakamura et al (2002)4 | Case report | 31/F | Perineal mass and dysmenorrhoea | CT: large soft-tissue mass in the inferior pararectal region. MRI: mass originating in abdominal pelvis and traversing pelvic diaphragm to the right of the anus; high signal intensity on T2-weighted images. Subsequent incisional biopsy. | Surgical excision | 6×5×3cm mass between vagina and rectum originating from rectal wall. Whitish, soft, rubbery. | Stellate and spindle-shaped cells with fibromyxoid stroma. Dilated venules and capillaries | Positive for vimentin, actin, desmin, estrogen and progesterone receptors. Weakly positive for S100 and CD34. Negative for SMA. | No recurrence at 3 years |
| Hastak et al (2008)12 | Case report | 65/M | Left perineal swelling | CT: defined lobulated heterogenous minimally enhancing mass in the left ischiorectal fossa. | Surgical excision | 13×10×9cm unencapsulated mass. Greyish-white with gelatinous cut sections. | Low grade spindle cell lesion comprising of areas of hypocellularity amidst myxoid change. Numerous thick and thin walled vessels. | Positive for SMA. Negative for S100. | Not reported |
| Rawlinson et al (2008)7 | Case report | 72/F | Abdominal pain and perirectal mass; soft mobile mass on PR examination | CT: 3cm mass in left ischiorectal fossa. Subsequent FNA. | Surgical excision and adjuvant radiotherapy | 7×3×1cm mass. Tan-pink, rubbery with gelatinous surface. | Spindle-shaped cells on myxoid background. No mitotic activity. | Positive for estrogen receptor, desmin, HMGA2. Negative for S100, AE1/AE3. FISH analysis: translocation of AML1 gene (21q22) from chromosome 21 to chromosome 12. | Not reported |
| Buchs et al (2015)13 | Case series | 38/F | Lump in the buttock; palpable mass adjacent to rectum on PR examination | MRI: 8cm mass with high signal intensity on T2-weighted images. Subsequent biopsy. | Surgical excision | Not reported | Not reported | Not reported | Recurrence after 4 months. Treated with hormone therapy with no further recurrence at 12 months. |
| Kelley et al (2018)5 | Case report | 39/F | Progressive pelvic discomfort and sensation of left buttock fullness | CT: retrorectal mass. MRI: 8.7×3.5cm complex cystic lesion in the presacral space. | Robotic extralevator excision with Da Vinci® Xi robot system | 17.7×9.7×5.8cm mass. Tan-pink, focally yellow, myxoid. | Hypocellular, small spindled and stellate fibroblasts with no atypia. Myxoid stroma with collagen fibres. Thick-walled vessels. | Positive for desmin, CD34, HMGA2, actin (focal), estrogen and progesterone receptors. Negative for caldesmon, KIT, DOG1, S100 and type IV collagen. | No recurrence at 6 months |
| Kanoa et al (2019)14 | Case report | 46/F | Vulval swelling | MRI: tumour in left ischiorectal fossa | Surgical excision (laparoscopic and open perineal) | Large mass extending from ischiorectal fossa to vulva, perineal region, and pelvic cavity. Exact dimensions not reported. Tan-pink, focally yellow. | Not reported | Not reported | No recurrence at 12 months |
| Dalvi et al (2019)15 | Case report | 60/F | Progressive swelling in the right gluteal region; 5×5cm non-tender swelling in the right pararectal region | Ultrasound: suggestive of ischiorectal abscess. CT: 4.2×5.7×7.9cm ischiorectal abscess. | Surgical excision | Pink, gelatinous mass | Spindle cell tumour | Suggestive of AA (specific markers not reported) | Not reported |
| Cabanilla-Manuntag et al (2020)8 | Case report | 26/F | Severe left-groin pain | Initial CT: 10.4×8.5×5.3cm lobulated mass in the left pelvis extending down to the ischioanal fossa. MRI 12 months later: hyperintense 12×11×6cm mass on T2-weighted signal within ischiorectal fossa causing displacement of cervix, anorectum and urinary bladder. Subsequent CT-guided biopsy. | Bilateral ureteral stenting, exploratory laparotomy with osteotomy of left pubic ramus and excision of ischiorectal fossa tumour | 16×10cm mass, pink | Mesenchymal lesion with no atypical histomorphological features | Positive for SMA, H-caldesmon, MSM2, estrogen and progesterone receptors. No comment on negative markers. | No recurrence at 3 months |
AA, aggressive angiomyxoma; CT, computed tomography; F, female; FISH, fluorescence in situ hybridisation; FNA, fine-needle aspiration; M, male; MRI, magnetic resonance imaging; PR, per rectum; SMA, smooth muscle actin
The current treatment of aggressive angiomyxoma is surgery and the aim is to achieve tumour-negative excision margins.5 However, due to the infiltrative nature of the tumour, partial excision may be acceptable if significant operative morbidity is anticipated or when preservation of fertility is prioritised.10 Unfortunately, in our case the lesion was received fragmented and margin status could not be assessed.
In terms of local recurrence, rates have been reported between 25–83% with most recurrences within three to five years of initial excision.5 Given the paucity of evidence on rectal/ischioanal aggressive angiomyxoma, we are unable to comment on specific recurrence rates for this tumour location.
Alternative or adjuvant therapies for aggressive angiomyxoma remain controversial. Radiotherapy and chemotherapy yield little benefit because the mitotic index of aggressive angiomyxoma is usually low.3 Tumour embolisation has also been used, but its effectiveness remains unclear.11 After review by the regional gynaecological oncology team, our patient was commenced on letrozole in accordance with previous studies suggesting that hormonal therapies (anti-estrogens and gonadotrophin-releasing hormone analogues) may be useful alternative or adjuvant therapies.3
Long-term follow-up and careful monitoring with imaging techniques are essential for detection of recurrence; however, owing to the rarity of aggressive angiomyxoma, there is no clear follow-up strategy. In this case, the patient is awaiting repeat MRI three months post-CT (performed five weeks postoperatively) and she remains under the care of the gynaecological oncology team and probable conservative management with surveillance imaging (interval not yet determined).
Conclusion
Aggressive angiomyxoma is a benign mesenchymal tumour with locally invasive properties and high rates of local recurrence. Surgery is the principle treatment; however, surgical considerations should include patient preference and causing minimal operative morbidity. Adjuvant therapies including hormonal suppression can be considered to reduce tumour size and/or control local recurrence.
This report describes the ninth case of aggressive angiomyxoma involving the rectum/ischioanal fossa, which is an uncommon location for this tumour. Incision and drainage of a cutaneous abscess, including perianal abscess, is a commonly performed procedure and we advocate that aggressive angiomyxoma should be considered as a potential differential diagnosis. Reporting a large series of aggressive angiomyxoma originating from typical and atypical regions may lead to an improved understanding of how these tumours can be optimally diagnosed and managed.
References
- 1.Steeper TA, Rosai J.. Aggressive angiomyxoma of the female pelvis and perineum: report of nine cases of a distinctive type of gynecologic soft-tissue neoplasm. Am J Surg Pathol 1983; 7: 463–476. 10.1097/00000478-198307000-00009 [DOI] [PubMed] [Google Scholar]
- 2.Geng J, Cao B, Wang L.. Aggressive angiomyxoma: an unusual presentation. Korean J Radiol 2012; 13: 90. 10.3348/kjr.2012.13.1.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sozutek A, Irkorucu O, Reyhan Eet al. A giant aggressive angiomyxoma of the pelvis misdiagnosed as incarcerated femoral hernia: a case report and review of the literature. Case Rep Surg 2016; 2016: 1–6. 10.1155/2016/9256749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakamura T, Miura K, Maruo Yet al. Aggressive angiomyxoma of the perineum originating from the rectal wall. J Gastroenterol 2002; 37: 303–308. 10.1007/s005350200040 [DOI] [PubMed] [Google Scholar]
- 5.Kelley SR. Robotic extralevator excision of a retrorectal giant aggressive angiomyxoma. Obstet Gynecol Sci 2018; 61: 693. 10.5468/ogs.2018.61.6.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed MAM, Uehelie MA, Rage AMAet al. Aggressive angiomyxoma of the penis: the first case report in a 9-month-old infant. Urology. 2017; 104: 187–190. 10.1016/j.urology.2016.12.045 [DOI] [PubMed] [Google Scholar]
- 7.Rawlinson NJ, West WW, Nelson M, Bridge JA.. Aggressive angiomyxoma with t(12;21) and HMGA2 rearrangement: report of a case and review of the literature. Cancer Genet Cytogenet 2008; 181: 119–124. 10.1016/j.cancergencyto.2007.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabanilla-Manuntag MCC, Lopez MPJ, Tampo MM, Gaston CL.. Aggressive angiomyxoma presenting as an ischiorectal fossa tumour. BMJ Case Rep 2020; 13: e234093. 10.1136/bcr-2019-234093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiser A, Korach J, Gotlieb WHet al. Importance of accurate preoperative diagnosis in the management of aggressive angiomyxoma: report of three cases and review of the literature. Abdom Imaging 2006; 31: 383–386. 10.1007/s00261-005-0378-5 [DOI] [PubMed] [Google Scholar]
- 10.Sutton BJ, Laudadio J.. Aggressive angiomyxoma. Arch Pathol Lab Med 2012; 136: 217–221. 10.5858/arpa.2011-0056-RS [DOI] [PubMed] [Google Scholar]
- 11.Amezcua CA, Begley SJ, Mata Net al. Aggressive angiomyxoma of the female genital tract: a clinicopathologic and immunohistochemical study of 12 cases. Int J Gynecol Cancer 2005; 15: 140–145. 10.1111/j.1048-891x.2005.15015.x [DOI] [PubMed] [Google Scholar]
- 12.Hastak MS, Raghuvanshi SR, Sahu Set al. Aggressive angiomyxoma in men. J Assoc Physicians India 2008; 56: 373–375. [PubMed] [Google Scholar]
- 13.Buchs NC, Mortensen NJ, Guy RJet al. Management of tumors of the ischiorectal fossa: the role of percutaneous biopsy. Dis Colon Rectum 2015; 58: 938–942. 10.1097/DCR.0000000000000438 [DOI] [PubMed] [Google Scholar]
- 14.Kanao H, Aoki Y, Tanigawa Tet al. En bloc resection of an aggressive angiomyxoma by a novel combination laparoscopic and open perineal approach. J Minim Invasive Gynecol 2019; 26: 598–599. 10.1016/j.jmig.2018.07.008 [DOI] [PubMed] [Google Scholar]
- 15.Dalvi AN, Garale MN, Churiwala JJet al. Pararectal angiomyxoma: a diagnostic dilemma. J Surg Case Rep 2019; 2019: rjz331. 10.1093/jscr/rjz331 [DOI] [PMC free article] [PubMed] [Google Scholar]