Abstract
Introduction
Recent consensus guidelines suggest that the laparoscopic approach may be a useful, safe and feasible approach in emergency general surgery. Despite this, the UK National Emergency Laparotomy Audit (NELA) suggests the rate of laparoscopy is low (9% fully laparoscopic) and slow to increase over time. A European survey found uptake to be variable. This UK survey was therefore undertaken to establish current UK practice and to determine factors affecting implementation.
Materials and methods
A questionnaire survey of currently practising UK consultant general surgeons was carried out by the North West Surgical Research Collaborative, using a secure web-based database maintained by the North West Surgical Trials Centre.
Results
A total of 151 completed questionnaires were returned from 22 UK centres; 18% of respondents were unaware that laparoscopic cases should be reported to NELA. Appendicectomy (97%) and cholecystectomy (87%) were routinely performed laparoscopically. Laparoscopy was infrequently used in perforation, ischaemia or obstructed hernias. There appears to be equipoise regarding laparoscopic compared with open surgery in small-bowel obstruction among all subspecialty emergency general surgeons, in perforated peptic ulcer among upper gastrointestinal surgeons and in Hinchey III diverticulitis among colorectal surgeons.
Conclusion
Uptake of laparoscopy in UK emergency general surgery is influenced by surgeon preference, subspecialty, patient and operative factors. Further research into outcomes may help to identify areas of greatest potential benefit. The rate of laparoscopy reported by NELA may be an underestimate due to the 18% of surgeons unaware that laparoscopic cases should be reported, which may affect the validity of analyses performed from this dataset.
Keywords: Laparoscopy, Laparotomy, Acute abdomen, Attitude of health personnel
Introduction
Laparoscopy has improved surgical outcomes in many areas of abdominal surgery. In elective procedures such as cholecystectomy and anti-reflux surgery, the laparoscopic approach is regarded as the gold standard.1
In emergency general surgery, studies as early as the 1990s suggested that laparoscopy was safe and effective in selected patients.2 Laparoscopy in the emergency setting is suggested to have many benefits: improved views of the abdominal cavity with minimal trauma, permitting simultaneous precise diagnosis and definitive treatment, and reducing postoperative pain, postoperative surgical site infection, incisional hernia rates and inflammatory response resulting from surgical trauma.3–5
Although there are potential benefits, the uptake of laparoscopy in emergency general surgery remains variable, probably because there are limited large-scale high-quality studies to determine these benefits in a controlled setting.
In the UK, the annual National Emergency Laparotomy Audit (NELA) provides large-scale multicentre data on emergency general surgery procedures, excluding appendiceal and biliary pathology. The fourth report, published in November 2018, included 23,929 patients from 183 hospitals in England and Wales. The number of emergency operations started and completed laparoscopically has marginally increased over time: 17% were approached laparoscopically with 9% completed laparoscopically in the 2018 fourth NELA report (previous years: 2017: 15% and 9%; 2016: 14% and 8%; 2015: 13% and 7%).6–9 Although there has been no specific NELA study on the use of laparoscopy in emergency surgery to determine the factors potentially affecting the low uptake of laparoscopy in emergency surgery, other studies suggest that factors may include steep learning curves, uncertainty regarding effectiveness, long operative times and lack of tactile feedback.7–10
The World Journal of Emergency Surgery guidelines for emergency laparoscopy were first introduced in 2006.10 The European Association for Endoscopic Surgery published a consensus status update in 2012 on emergency conditions for which laparoscopy was recommended,11 then similar recommendations were published in 2013 by the World Society of Emergency Surgery on the management of intra-abdominal infections.12 These guidelines support the use of laparoscopy for the management of cholecystitis,13–15 appendicitis,11 perforated duodenal ulcer,16 diverticulitis,17–19 adhesional small bowelobstruction,20–22 non-specific abdominal pain23 and trauma,24–27 provided that patients are appropriately selected and the surgeons have the necessary training skills in undertaking these procedures.
Despite consensus guidelines on the safe use of laparoscopy in the management of the acute abdomen, the uptake is variable, especially in the UK.28 Given the potential benefits to patients, this national survey aims to provide valuable information to assess current UK practice and to determine the factors affecting the variable use of laparoscopy within emergency general surgery in the UK.
Materials and methods
Study design and population
A questionnaire survey of currently practising UK consultant general surgeons who regularly participate in an emergency general surgery on-call rota was undertaken during November and December 2017. The study was coordinated and delivered via a North West Surgical Research Collaborative steering committee. The survey was presented as a new study at the National Research Collaborative Conference 2017 and distributed via the network of surgical trainee research collaboratives, which has a presence in the majority of acute hospital trusts in the UK. It was also publicised through Twitter (@LEGS_Study) to improve enrolment. Each trainee who registered and led the study at their site individually approached each of the consultant general and emergency surgeons at their trust to include them in the study.
An initial survey pilot was trialled by 10 general surgical consultants. Feedback was provided on the questionnaire design and suggestions provided for amendments and supplementary relevant questions. The questionnaire design was then modified according to this feedback.
Questionnaire design
This was a four-part questionnaire, designed to obtain a ‘snapshot’ overview of aspects of current clinical practice in the use of laparoscopy in emergency general surgery. The component parts were: (1) clinical profile questions establishing clinical practice parameters such as laparoscopic case volume, subspecialty interest, number of years since qualification from medical school, completion of a laparoscopic fellowship, awareness and practice of reporting laparoscopic cases to NELA; (2) clinical scenario questions assessing the likelihood of approaching a variety of emergency clinical scenarios and surgical pathologies laparoscopically; (3) and (4) factors influencing decision to use laparoscopy questions assessing the likelihood of a variety of factors influencing the decision to approach an operation laparoscopically, including a patient-specific factors, procedure-specific factors, and external factors.
Survey implementation
Surgical trainees directly approached consultants participating in the general surgery on-call rota within their departments and invited them to complete a paper version of the questionnaire with them in a face-to-face setting. Once the survey was completed, the trainees then uploaded the responses directly into a secure web-based REDCap database maintained by the North West Surgical Trials Centre. All trainees returning five completed questionnaires were acknowledged within the LEGS Study Group contributor list. A total of 152 questionnaires were returned from 22 UK centres in England, Scotland and Wales.
Statistical analysis
Statistical analyses were performed using Jamovi Version 1.0.0.0. Comparisons were made using the Mann–Whitney U test for two groups and one-way analysis of variance for multiple comparisons.
Results
Baseline demographics
A total of 152 completed questionnaires were returned from 21 UK centres located in Northwest England (6), London and the South East (5), East England (3), the Midlands (3), South West England (2) and Scotland (2). One respondent did not fully complete the questionnaire and was excluded from final analysis. The median time as a consultant was 9.0 years (interquartile range, IQR, 4.0–16.0 years) with a median time since the time of primary medical qualification of 23.0 years (IQR 18.0–29.0 years). Surgical training was distributed across 11 different countries with the UK being most common (n = 137). Other countries included Australia, Austria, Belgium, Greece, India, Iraq, Ireland, Malta, Netherlands, Spain and Pakistan; 49.1% undertook a laparoscopic fellowship. The distribution across subspecialties can be seen in Table 1.
Table 1 .
Subspecialty distribution of respondents
| Subspecialty | Respondents |
|
|---|---|---|
| (n) | (%) | |
| Colorectal | 83 | 54.6 |
| Upper gastrointestinal | 36 | 23.7 |
| General/emergency | 19 | 12.5 |
| Hepatopancreatobiliary | 10 | 6.6 |
| Endocrine | 2 | 1.3 |
| Breast | 1 | 0.7 |
| Vascular | 1 | 0.7 |
| Total | 152 | 100 |
Laparoscopic emergency surgery and NELA
Some 18.4% of consultants were unaware that laparoscopic emergency cases (excluding appendicectomy and cholecystectomy) should be entered into the NELA database. Only 70.4% of consultants routinely included laparoscopic emergency cases in NELA data recording. Ten (6.6%) questionnaires were returned from Scotland, where data are not submitted to NELA.
Laparoscopic approach by emergency condition
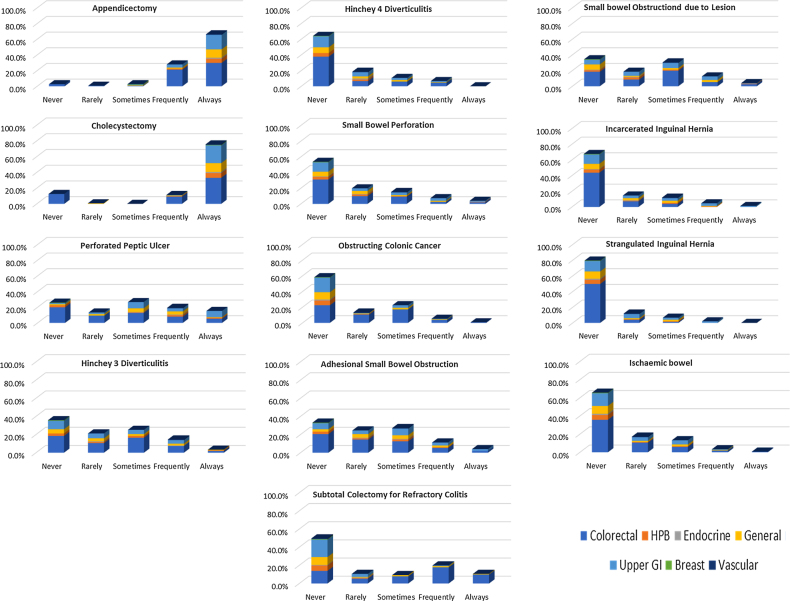
Results are displayed in Figure 1 for all respondents, stratified by subspecialty. Respondents said the laparoscopic approach was used either ‘frequently or always’ for appendicectomy (94%) and cholecystectomy (86.8%); only 2.6% of respondents would never approach appendicectomy laparoscopically.
Figure 1 .
Likert scale responses for the use of laparoscopic approach for each emergency condition stratified by sub-specialty
The majority of the respondents would ‘never’ use the laparoscopic approach in the following situations: Hinchey 4 perforated diverticulitis (64.2%), small-bowel perforation (53.6%), colonic cancer with bowel obstruction (58.3%), incarcerated (67.5%) or strangulated (79.5%) inguinal hernia, ischaemic bowel (65.6%) or subtotal colectomy for refractory colitis (49.7%). The laparoscopic approach was considered sometimes, frequently or always in approaching half of small bowel obstructions due to either adhesions (42.5%) or a lesion (47.1%).
There appeared to be general equipoise for the use of laparoscopy for perforated peptic ulcer, particularly in the upper gastrointestinal subspecialty, where 85.7% of upper gastrointestinal surgeons would approach a perforated peptic ulcer laparoscopically ‘sometimes, frequently or always’. Equipoise is also suggested for Hinchey III diverticular perforation, with 47% of colorectal surgeons using this approach ‘sometimes, frequently or always’.
In the free-text responses, two upper gastrointestinal subspecialty surgeons said that they did not operate on patients with lower gastrointestinal pathology because they have a split specialty on-call rota and colorectal pathology would be operated upon by their colorectal colleagues. One respondent said they ‘always had a look with the laparoscope’, while another said that ‘the laparoscope is the tool of the devil and should not be used in emergency laparotomy cases’.
Patient-specific scenarios
Table 2 looks at the influence of patient and environmental factors on the use of laparoscopy in emergency surgery. The majority of respondents disagreed that higher body mass index (BMI, 60.3%), elderly patients (63.6%), operating between 8pm and 8am (51.6%) or at the weekend (73.5%) would make them less likely to use a laparoscopic approach. Previous abdominal surgery, poorer performance status, high American Society of Anesthesiologists (ASA) grade, frailty or return to theatre for complications appeared to split the responses, with no consensus as to whether these factors would affect their decision to use laparoscopy.
Table 2 .
Factors influencing the use of laparoscopy in emergency surgery
| Factor | Strongly Disagree |
Disagree |
Neither Agree nor Disagree |
Agree |
Strongly Agree |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| I am less likely to perform emergency laparoscopic procedures in patients with a higher body mass index | 29 | 19.2 | 62 | 41.1 | 35 | 23.2 | 19 | 12.6 | 6 | 4.0 |
| I am less likely to perform emergency laparoscopic surgery in the elderly | 21 | 13.9 | 75 | 49.7 | 41 | 27.2 | 12 | 7.9 | 2 | 1.3 |
| I am less likely to perform emergency laparoscopic procedures in patients who have had previous abdominal surgery | 8 | 5.3 | 34 | 22.5 | 46 | 30.5 | 56 | 37.1 | 7 | 4.6 |
| I am less likely to perform emergency laparoscopic procedures in patients who have poorer performance statuses | 7 | 4.6 | 49 | 32.5 | 48 | 31.8 | 43 | 28.5 | 4 | 2.6 |
| I am less likely to perform emergency laparoscopic procedures in patients who have high American Society of Anesthesiologists grades | 6 | 4.0 | 46 | 30.5 | 47 | 31.1 | 44 | 29.1 | 8 | 5.3 |
| I am less likely to perform emergency laparoscopic procedures in frail patients | 9 | 6.0 | 49 | 32.5 | 56 | 37.1 | 32 | 21.2 | 5 | 3.3 |
| I am less likely to perform emergency laparoscopic procedures in patients who are returning to theatre for management of complications from a recent operation | 6 | 4.0 | 33 | 21.9 | 43 | 28.5 | 48 | 31.8 | 21 | 13.9 |
| I am less likely to perform emergency laparoscopic procedures during the hours of 8pm to 8am | 28 | 18.5 | 50 | 33.1 | 35 | 23.2 | 33 | 21.9 | 5 | 3.3 |
| I am less likely to perform emergency laparoscopic procedures at weekends | 37 | 24.5 | 74 | 49.0 | 31 | 20.5 | 9 | 6.0 | 0 | 0.0 |
Procedure-specific scenarios
The respondents were surveyed about seven common surgical scenarios that would present to the emergency surgical team with subsequent patient or environmental factors that may affect their decision to use the laparoscopic approach. In appendicectomy, the laparoscopic approach was favoured ‘frequently or always’ for 12-year-old boys (66.2%), 25-year-old women (97.4%) and 65-year-old men (89.4%). In a six-year-old girl, 49.7% would either ‘never or rarely’ approach laparoscopically, yet 29.8% would always do so.
In the case of a 50-year-old man with computed tomography (CT) diagnosed perforated duodenal ulcer, there appears to equipoise when a patient has no significant comorbidities, with 24.5% ‘never’ using laparoscopy and 21.2% ‘always’ using laparoscopy. The laparoscopic approach becomes less likely to be used with previous open abdominal surgery (never, 39.1%) and evidence of small-bowel dilatation on CT (never, 33.8%).
When presented with a 60-year-old woman with CT diagnosed Hinchey III diverticulitis, respondents would ‘never or rarely’ use laparoscopy if there was previous open abdominal surgery (67.5%) or evidence of small bowel dilatation on CT (75.5%). Furthermore, if the same patient had Hinchey 4 diverticulitis, 81.1% of respondents would ‘never or rarely’ use a laparoscopic approach even if no significant comorbidities. Only three respondents would ‘always’ use a laparoscopic approach in this instance.
A scenario of small-bowel obstruction in a patient with no prior history of abdominal surgery was presented with CT findings of an abrupt transition point in the pelvis. In a patient with no comorbidities, 58.9% of respondents would use a laparoscopic approach ‘sometimes, frequently or always’, but this was again less likely among the respondents if the patient had undergone previous open abdominal surgery (36.4%).
Respondents were asked about two postoperative complications scenarios. The first concerned a decision to reoperate two days following laparoscopic repair of perforated duodenal ulcer who had deteriorated with a CT showing free fluid and pneumoperitoneum; 59.6–70.9% of respondents would ‘never or rarely’ use the laparoscopic approach for the return to theatre, with between 15.2–21.2% ‘frequently or always’ approaching this scenario laparoscopically. This was similar whether the patient had significant comorbidities, ASA 3, BMI 42kg/m2 or age.
The second concerned a decision to operate on a patient who had undergone a laparoscopic anterior resection (primary anastomosis and not defunctioned) where four days later they deteriorated and CT showed a probable leak at the anastomosis; 56.6–64.9% of respondents would ‘never or rarely’ use the laparoscopic approach for the return to theatre, with between 20.5–25.1% ‘frequently or always’ approaching this scenario laparoscopically. This was similar whether the patient had significant comorbidities, ASA 3, BMI 42kg/m2 or age.
Subgroup analysis was performed to compare the practice of colorectal surgeons (n = 82) with upper gastrointestinal surgeons (n = 35). For scenario 2 (perforated duodenal ulcer, Table 3), upper gastrointestinal surgeons are more likely to use a laparoscopic approach than colorectal surgeons for each of the variables (median); no significant comorbidities (frequently vs sometimes, p = 0.002), ASA 3 (sometimes vs rarely, p = 0.007), BMI 42kg/m2 (frequently vs rarely, p < 0.001), previous abdominal surgery (sometimes vs rarely, p = 0.001) and evidence of small bowel dilatation on CT (sometimes vs rarely, p = 0.017). Upper gastrointestinal surgeons are also more likely than colorectal surgeons to use a laparoscopic approach for complication from a perforated duodenal ulcer (p < 0.05).
Table 3 .
Likert scale of the likelihood of the use of the laparoscopic approach for seven common emergency surgical scenarios depending on various patient and environmental factors
| Scenario 1: A patient with suspected appendicitis. They have no significant comorbidities. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Never |
Rarely |
Sometimes |
Frequently |
Always |
|||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) 6-yr-old female | 61 | 40.4 | 14 | 9.3 | 14 | 9.3 | 16 | 10.6 | 45 | 29.8 |
| b) 12-year-old male | 23 | 15.2 | 12 | 7.9 | 15 | 9.9 | 42 | 27.8 | 58 | 38.4 |
| c) 25-year-old female | 3 | 2.0 | 0 | 0.0 | 0 | 0.0 | 14 | 9.3 | 133 | 88.1 |
| d) 65-year-old male | 3 | 2.0 | 4 | 2.6 | 8 | 5.3 | 31 | 20.5 | 104 | 68.9 |
| Scenario 2: A 50-year-old male with a computed tomography diagnosed perforated duodenal ulcer. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 37 | 24.5 | 20 | 13.2 | 31 | 20.5 | 30 | 19.9 | 32 | 21.2 |
| b) ASA grade 3 | 43 | 28.5 | 27 | 17.9 | 28 | 18.5 | 32 | 21.2 | 20 | 13.2 |
| c) Body mass index 42kg/m2 | 42 | 27.8 | 26 | 17.2 | 28 | 18.5 | 32 | 21.2 | 22 | 14.6 |
| d) Previous abdominal surgery | 51 | 33.8 | 34 | 22.5 | 41 | 27.2 | 12 | 7.9 | 12 | 7.9 |
| e) Evidence of small bowel dilatation on CT | 59 | 39.1 | 38 | 25.2 | 33 | 21.9 | 14 | 9.3 | 6 | 4.0 |
| Scenario 3: A 60-year-old female with Hinchey grade 3 diverticulitis diagnosed on computed tomography. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 43 | 28.5 | 26 | 17.2 | 39 | 25.8 | 30 | 19.9 | 12 | 7.9 |
| b) ASA grade 3 | 50 | 33.1 | 29 | 19.2 | 36 | 23.8 | 29 | 19.2 | 6 | 4.0 |
| c) Body mass index 42kg/m2 | 56 | 37.1 | 29 | 19.2 | 34 | 22.5 | 24 | 15.9 | 7 | 4.6 |
| d) Previous abdominal surgery | 66 | 43.7 | 36 | 23.8 | 30 | 19.9 | 16 | 10.6 | 2 | 1.3 |
| e) Evidence of small bowel dilatation on CT | 73 | 48.3 | 41 | 27.2 | 23 | 15.2 | 11 | 7.3 | 2 | 1.3 |
| Scenario 4: 60-year-old female with Hinchey grade 4 diverticulitis diagnosed on computed tomography. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 92 | 60.9 | 29 | 19.2 | 18 | 11.9 | 8 | 5.3 | 3 | 2.0 |
| b) ASA grade 3 | 97 | 64.2 | 29 | 19.2 | 17 | 11.3 | 5 | 3.3 | 2 | 1.3 |
| c) Body mass index 42kg/m2 | 96 | 63.6 | 33 | 21.9 | 15 | 9.9 | 4 | 2.6 | 2 | 1.3 |
| d) Previous abdominal surgery | 104 | 68.9 | 28 | 18.5 | 12 | 7.9 | 4 | 2.6 | 2 | 1.3 |
| e) Evidence of small bowel dilatation on CT | 106 | 70.2 | 29 | 19.2 | 10 | 6.6 | 3 | 2.0 | 2 | 1.3 |
| Scenario 5: You have performed a laparoscopic repair of a perforated duodenal ulcer. Two days later the patient deteriorates on the ward. Computed tomography shows a large amount of free fluid and free air. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 74 | 49.0 | 16 | 10.6 | 27 | 17.9 | 19 | 12.6 | 13 | 8.6 |
| b) ASA grade 3 | 82 | 54.3 | 20 | 13.2 | 24 | 15.9 | 15 | 9.9 | 8 | 5.3 |
| c) Body mass index 42kg/m2 | 81 | 53.6 | 17 | 11.3 | 21 | 13.9 | 21 | 13.9 | 9 | 6.0 |
| d) 50-year-old male | 79 | 52.3 | 15 | 9.9 | 25 | 16.6 | 19 | 12.6 | 11 | 7.3 |
| e) 80-year-old male | 90 | 59.6 | 17 | 11.3 | 19 | 12.6 | 15 | 9.9 | 8 | 5.3 |
| Scenario 6: A patient has had a laparoscopic anterior resection four days ago (primary anastomosis and not defunctioned). Today they have deteriorated and computed tomography shows a probable leak at the anastomosis. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 68 | 45.0 | 19 | 12.6 | 24 | 15.9 | 23 | 15.2 | 15 | 9.9 |
| b) ASA grade 3 | 72 | 47.7 | 22 | 14.6 | 21 | 13.9 | 23 | 15.2 | 11 | 7.3 |
| c) Body mass index 42kg/m2 | 73 | 48.3 | 23 | 15.2 | 21 | 13.9 | 23 | 15.2 | 8 | 5.3 |
| d) 50-year-old male | 71 | 47.0 | 18 | 11.9 | 24 | 15.9 | 21 | 13.9 | 15 | 9.9 |
| e) 80-year-old male | 76 | 50.3 | 22 | 14.6 | 20 | 13.2 | 23 | 15.2 | 8 | 5.3 |
| Scenario 7: A patient presents with small-bowel obstruction confirmed on computed tomography. They have had no previous surgery and the radiologist reports an abrupt transition point in the pelvis. You decide to operate. How likely are you to approach this laparoscopically? | ||||||||||
| Patient | Never | Rarely | Sometimes | Frequently | Always | |||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| a) No significant comorbidities | 39 | 25.8 | 31 | 20.5 | 39 | 25.8 | 30 | 19.9 | 20 | 13.2 |
| b) ASA grade 3 | 42 | 27.8 | 25 | 16.6 | 43 | 28.5 | 28 | 18.5 | 11 | 7.3 |
| c) Body mass index 42kg/m2 | 47 | 31.1 | 28 | 18.5 | 37 | 24.5 | 22 | 14.6 | 15 | 9.9 |
| d) 50-year-old male | 39 | 25.8 | 24 | 15.9 | 39 | 25.8 | 27 | 17.9 | 20 | 13.2 |
| e) 80-year-old male | 47 | 31.1 | 27 | 17.9 | 36 | 23.8 | 23 | 15.2 | 15 | 9.9 |
| f) A patient who has had previous open abdominal surgery | 63 | 41.7 | 31 | 20.5 | 34 | 22.5 | 14 | 9.3 | 7 | 4.6 |
ASA, American Society of Anesthesiologists; CT, computed tomography
For scenario 6 (anastomotic leak after laparoscopic anterior resection, Table 3), colorectal surgeons are more likely to use a laparoscopic approach than upper gastrointestinal surgeons for each of the variables (median); no significant comorbidities (sometimes vs never, p = 0.002), ASA 3 (sometimes vs never, p = 0.002), BMI 42kg/m2 (rarely vs never, p = 0.006), 50-year-old man (sometimes vs never, p = 0.002) and 80-year-old man (rarely vs never, p = 0.003).
The small numbers in the other groups mean that it was not possible to perform subgroup analyses between those groups. There was no difference in responses when comparing those who had completed a laparoscopic fellowship with those who had not (p > 0.005).
Comparison of the use of the laparoscopic approach based on the achievement of Certificate of Completion of Training before or after 2006
The World Journal of Emergency Surgery guidelines for emergency laparoscopy were first introduced in 2006.10 This section looks at their potential impact on the use of laparoscopy in emergency surgery for consultants reaching the Certificate of Completion of Training (CCT) in 2006 or later, compared with those who gained CCT before 2006. Table 4 shows these results. Of the 151 respondents, comparison of the 52 who gained CCT prior to 2006 was made with the 99 gaining CCT during or after 2006. Those that gained CCT after 2006 were more likely to use laparoscopy to approach appendicectomy (p < 0.001), perforated peptic ulcer (p = 0.024), Hinchey III diverticulitis (p = 0.004), obstructing colonic cancer (p = 0.031), obstructing small bowel lesions (p = 0.005) and subtotal colectomy for refractory colitis. No significant difference was seen between the rest of the operations (p > 0.05). There was no difference in responses when comparing those who had completed a laparoscopic fellowship with those who had not (p > 0.005).
Table 4 .
Comparison of the use of laparoscopy by operation for Certificate of Completion of Training before and after 2006
| Operation type | Before or after 2006 | Respondents (n) | Likelihood of laparoscopic approach (median Likert)a | 95% confidence interval |
p-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Appendicectomy | Before | 52 | 4 | –1 | –4.76e−5 | <.001 |
| After | 99 | 5 | ||||
| Cholecystectomy | Before | 52 | 5 | –5.13e−5 | 4.61E–05 | 0.837 |
| After | 99 | 5 | ||||
| Perforated peptic ulcer | Before | 52 | 3 | –1 | –8.88e−6 | 0.024 |
| After | 99 | 3 | ||||
| Hinchey 3 diverticulitis | Before | 52 | 1 | –1 | –6.46e−5 | 0.004 |
| After | 99 | 3 | ||||
| Hinchey 4 diverticulitis | Before | 52 | 1 | –2.37e−5 | 3.05E–05 | 0.301 |
| After | 99 | 1 | ||||
| Small bowel perforation | Before | 52 | 1 | –1.02e−7 | 5.92E–05 | 0.191 |
| After | 99 | 1 | ||||
| Obstructing colonic cancer | Before | 52 | 1 | –4.67e−5 | –2.84e−5 | 0.031 |
| After | 99 | 1 | ||||
| Adhesional small-bowel obstruction | Before | 52 | 2 | –1 | 1.78E–05 | 0.151 |
| After | 99 | 2 | ||||
| Obstructing small-bowel lesion | Before | 52 | 2 | –1 | –9.13e−5 | 0.005 |
| After | 99 | 3 | ||||
| Incarcerated hernia | Before | 52 | 1 | –5.09e−5 | 3.61E–05 | 0.411 |
| After | 99 | 1 | ||||
| Strangulated hernia | Before | 52 | 1 | –4.47e−5 | 4.94E–05 | 0.45 |
| After | 99 | 1 | ||||
| Ischaemic bowel | Before | 52 | 1 | –4.63e−5 | 2.95E–05 | 0.555 |
| After | 99 | 1 | ||||
| Subtotal colectomy for refractory colitis | Before | 52 | 1 | –1 | –4.19e−5 | 0.006 |
| After | 99 | 2 | ||||
a Likert scale: never, 1; rarely, 2; sometimes, 3; frequently, 4; always, 5. Comparison made using the Mann–Whitney U test. Significance level p < 0.05.
Discussion
This national multicentre survey provides novel information on the factors influencing the use of laparoscopy in UK emergency general surgery. The use of the laparoscopic approach in the UK is highly variable and is influenced by surgeon preference, subspecialty, patient and operative factors. Although the laparoscopic approach to emergency appendicectomy and cholecystectomy have become the norm, it is not used frequently in cases of (small and large) bowel perforation, ischaemia or obstructed hernias. Our results may suggest potential clinical equipoise in the approach to small-bowel obstruction, for perforated peptic ulcer and Hinchey III diverticulitis by respective surgeons in upper gastrointestinal and colorectal surgical subspecialties. This variability of the use of laparoscopy has the potential to affect patient outcomes and the provision of surgical training.
We recognise the limitations of a questionnaire-based survey and that our methodology opens the results to an element of selection bias, where consultants who were strongly for or against laparoscopy may be more likely to complete the questionnaire. This is a relatively small sample size and, although it may be difficult to state that it is a reflection of true UK practice, we have attempted to address this issue in our sampling through focusing on individual site recruitment through research-active collaborative trainees, and subsequently including consultants at the individual sites. This reduced the risk of bias seen in email surveys.
We also acknowledge that constructed scenarios have their limitations in that it is not possible to provide all the required information for decision making. We tried to simplify them to allow the study to capture potential caveats that have been highlighted as preclusions to a laparoscopic approach, such as increased age, ASA grade and obesity. Introducing more complex descriptions of comorbidities and prior abdominal surgery was beyond the scope of this study and would have reduced the reliability of the results as an illustration of the potential issue surrounding the decision making.
Nevertheless, with one-fifth of surgeons not knowing that the laparoscopic approach should be entered into the NELA database and 30% not uploading these cases, there are implications for the accuracy and validity of nationally collected data. Data submission to NELA has been implemented in hospitals across England and Wales and provides a means by which clinical teams can assess and benchmark their care against national standards, actively encouraging teams to use their own data to drive local quality improvement.6 Since the introduction of the audit in 2013, there have been improvements in 30-day mortality, longer patient survival, shorter length of stay and increased consultant input and presence in theatre, but improving these standards further should start with improving the data collection.
Additionally, over the course of the four annual NELA reports, there has been only a minimal increase in the use of the laparoscopic approach, either entirely laparoscopically, converted to open or laparoscopically assisted from year one (13%)9 to year four (16.7%).6 Our results suggest a higher use of laparoscopy for the same emergency procedures in the surveyed cohort. This is likely to be due to differences in what individuals say they do compared with what they actually do, as previous research has shown that there can be discordance between self-reported surveys and practical behaviours.29 Alternatively, it may be due to the underreporting to NELA of the use of the laparoscopic approach highlighted above, or even due to selection bias within the respondents in that those who perform laparoscopy more frequently were more likely to complete the survey.
The respondents demonstrated relative equipoise for the approach to small-bowel obstruction across all specialties, with subspecialty equipoise for the management of peptic ulceration (by upper gastrointestinal surgeons) and Hinchey III diverticulitis (colorectal surgeons). This is in keeping with the previously reviewed evidence that the laparoscopic approach can be advantageous in these conditions in appropriately selected patients. Although there are some randomised controlled trials in these settings,18, 19, 30 the findings of these trials have not yet been implemented in widespread clinical practice, for reasons unknown. This may, however, be a reflection of queries over patient selection and longer-term outcomes. Further research aiming to identify which factors permit the identification of patients most likely to benefit from the laparoscopic approach would likely need to focus upon outcomes to aid the decision-making process.
It is known that a surgeon's decision making is affected by five groups of factors: medical condition, information, institutional, patient and surgeon factors.31 However, no specific factors from the scenarios in our survey provided consensus on the use or not of laparoscopy. Factors such as high BMI, elderly patients and out-of-hours operating, which may once have discouraged the use of laparoscopy, seem not to be a barrier to this approach. While there was a tendency for respondents to agree that return to theatre for management of postoperative complications would affect the use of laparoscopy, one-quarter of respondents disagree that this would affect their decision. Ultimately, and as shown in the subgroup analysis of upper gastrointestinal and colorectal surgeons, it would appear that surgeon expertise and technical ability may provide more influence than patient-specific or institutional factors, but more targeted research would be required to determine the effects. Gunaratnam et al found that when guidelines and class 1 evidence are lacking, surgeon factors are the most powerful.31
We found differences in the use of laparoscopy depending on whether CCT was gained before or after 2006, when the World Journal of Emergency Surgery guidelines for emergency laparoscopy were introduced. It is acknowledged that this may be somewhat an arbitrary cut-off point, but it may reflect a change in approach where newly qualified consultants have evidence-based guidelines on which to base their practice. One may also attribute this difference to laparoscopic training programmes such as the National Training Programme for Laparoscopic Colorectal Surgery, which was introduced in 2008,32 or the updating of the National Institute for Health and Care Excellence guidelines for colorectal surgery in 2006.33 It may also be related to the uptake in laparoscopic surgeons based on surgeon experience, with the effect of reduced uptake of laparoscopic surgery (especially resectional surgery) in older surgeons, although the completion of a laparoscopic fellowship did not change the likelihood of the responses. On the other hand, given that these operations include perforated peptic ulcer, Hinchey III diverticulitis, obstructing colonic cancer, obstructing small-bowel lesions and subtotal colectomy for refractory colitis, it may be a consequence of subspecialisation.
Respondents were asked about their use of laparoscopy for procedure-specific emergency scenarios and patient factors that may influence their decision to use this approach. The three most common indications for emergency surgery are small-bowel obstruction, perforation and peritonitis, with laparotomy for ischaemia and acidosis being less common but carrying the highest mortality rates.6 In our cohort, respondents would tend to favour laparoscopic approach for adhesional small-bowel obstruction, but would be discouraged if patients had previous abdominal surgery. When considering perforations and return to theatre for complications, colorectal surgeons are more likely to approach colonic pathology laparoscopically, whereas upper gastrointestinal surgeons are more likely to approach duodenal pathology laparoscopically.
The latest NELA report has demonstrated overall lower mortality with laparoscopy compared with open surgery (three-year mortality 35.5% open surgery vs 23.3% laparoscopic).6 This may suggest an increasing role for laparoscopy; however, there is potential for significant bias given the differences in the populations when considering age and physiological status. Accepting the limitations of incomplete reporting to NELA, further subgroup analysis of the differences in outcomes between laparoscopic and open surgery, adjusting for variables would help to identify the areas in which laparoscopy could produce the greatest potential patient benefit.
The use of laparoscopy in emergency general surgery is variable and its uptake may be increasing, particularly in the group of consultant surgeons who completed their training more recently. This may be driven by guidelines or advancement in surgical techniques, but further work is required to identify differences in outcomes between the two approaches.
Acknowledgements
The authors would like to thank the North West Surgical Trials Unit for their support in providing the REDCap database and to Ellie Badrick for advice on data analysis. There was no funding for this study.
References
- 1.Velanovich V. Laparoscopic vs open surgery: a preliminary comparison of quality-of-life outcomes. Surg Endosc 2000; 14: 16–21. 10.1007/s004649900003 [DOI] [PubMed] [Google Scholar]
- 2.Navez B, Tassetti V, Scohy JJet al. Laparoscopic management of acute peritonitis. Br J Surg 1998; 85: 32–36. 10.1046/j.1365-2168.1998.00531.x [DOI] [PubMed] [Google Scholar]
- 3.Cuschieri A. Cost efficacy of laparoscopic vs open surgery. Hospitals vs community. Surg Endosc 1998; 12: 1197–1198. 10.1007/s004649900819 [DOI] [PubMed] [Google Scholar]
- 4.Larsson PG, Henriksson G, Olsson Met al. Laparoscopy reduces unnecessary appendicectomies and improves diagnosis in fertile women: a randomized study. Surg Endosc 2001; 15: 200–202. 10.1007/s004640000255 [DOI] [PubMed] [Google Scholar]
- 5.Di Saverio S. Emergency laparoscopy: a new emerging discipline for treating abdominal emergencies attempting to minimize costs and invasiveness and maximize outcomes and patients’ comfort. J Trauma Acute Care Surg 2014; 77: 338–350. 10.1097/TA.0000000000000288 [DOI] [PubMed] [Google Scholar]
- 6.NELA Project Team . Fourth Patient Report of the National Emergency Laparotomy Audit. London: Royal College of Anaesthetists; 2018. [Google Scholar]
- 7.NELA Project Team . Third Patient Report of the National Emergency Laparotomy Audit. London: Royal College of Anaesthetists; 2017. [Google Scholar]
- 8.NELA Project Team . Second Patient Report of the National Emergency Laparotomy Audit. London: Royal College of Anaesthetists; 2016. [Google Scholar]
- 9.NELA Project Team . First Patient Report of the National Emergency Laparotomy Audit. London: Royal College of Anaesthetists; 2015. [Google Scholar]
- 10.Neugebauer EA, Sauerland S. Guidelines for emergency laparoscopy. World J Emerg Surg 2006; 1: 31. 10.1186/1749-7922-1-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agresta F, Ansaloni L, Baiocchi GLet al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Societa Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Societa Italiana di Chirurgia (SIC), Societa Italiana di Chirurgia d'Urgenza e del Trauma (SICUT), Societa Italiana di Chirurgia nell'Ospedalita Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc 2012; 26: 2134–2164. doi: 10.1007/s00464-012-2331-3 [DOI] [PubMed] [Google Scholar]
- 12.Sartelli M, Viale P, Catena Fet al. 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 2013; 8: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kiviluoto T, Siren J, Luukkonen Pet al. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet 1998; 351: 321–325. 10.1016/S0140-6736(97)08447-X [DOI] [PubMed] [Google Scholar]
- 14.Johansson M, Thune A, Nelvin Let al. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg 2005; 92: 44–49. 10.1002/bjs.4836 [DOI] [PubMed] [Google Scholar]
- 15.Csikesz N, Ricciardi R, Tseng JFet al. Current status of surgical management of acute cholecystitis in the United States. World J Surg 2008; 32: 2230–2236. 10.1007/s00268-008-9679-5 [DOI] [PubMed] [Google Scholar]
- 16.Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev 2013; 2: CD004778. 10.1097/SLA.0000000000001061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Angenete E, Thornell A, Burcharth Jet al. Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Ann Surg 2016; 263: 117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kohl A, Rosenberg J, Bock Det al. Two-year results of the randomized clinical trial DILALA comparing laparoscopic lavage with resection as treatment for perforated diverticulitis. Br J Surg 2018; 105: 1128–1134. 10.1002/bjs.10839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schultz JK, Wallon C, Blecic Let al. One-year results of the SCANDIV randomized clinical trial of laparoscopic lavage versus primary resection for acute perforated diverticulitis. Br J Surg 2017; 104: 1382–1392. 10.1002/bjs.10567 [DOI] [PubMed] [Google Scholar]
- 20.Byrne J, Saleh F, Ambrosini Let al. Laparoscopic versus open surgical management of adhesive small bowel obstruction: a comparison of outcomes. Surg Endosc 2015; 29: 2525–2532. 10.1007/s00464-014-4015-7 [DOI] [PubMed] [Google Scholar]
- 21.Nordin A, Freedman J. Laparoscopic versus open surgical management of small bowel obstruction: an analysis of clinical outcomes. Surg Endosc 2016; 30: 4454–4463. 10.1007/s00464-016-4776-2 [DOI] [PubMed] [Google Scholar]
- 22.Quah GS, Eslick GD, Cox MR. Laparoscopic versus open surgery for adhesional small bowel obstruction: a systematic review and meta-analysis of case-control studies. Surg Endosc 2019; 33: 3209–3217. 10.1007/s00464-018-6604-3 [DOI] [PubMed] [Google Scholar]
- 23.American College of Emergency Physicians . Clinical policy: critical issues for the initial evaluation and management of patients presenting with a chief complaint of nontraumatic acute abdominal pain. Ann Emerg Med 2000; 36: 406–415. 10.1067/mem.2000.109446 [DOI] [PubMed] [Google Scholar]
- 24.Society of American Gastrointestinal and Endoscopic Surgeons . Guidelines for Diagnostic Laparoscopy. Los Angeles, CA: Society of American Gastrointestinal and Endoscopic Surgeons; 2019. [Google Scholar]
- 25.Chol YB, Lim KS. Therapeutic laparoscopy for abdominal trauma. Surg Endosc 2003; 17: 421–427. 10.1007/s00464-002-8808-8 [DOI] [PubMed] [Google Scholar]
- 26.Zantut LF, Ivatury RR, Smith RSet al. Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma: a multicenter experience. J Trauma 1997; 42: 825–831. 10.1097/00005373-199705000-00012 [DOI] [PubMed] [Google Scholar]
- 27.Mathonnet M, Peyrou P, Gainant Aet al. Role of laparoscopy in blunt perforations of the small bowel. Surg Endosc 2003; 17: 641–645. 10.1007/s00464-002-9049-6 [DOI] [PubMed] [Google Scholar]
- 28.Agresta F, Campanile FC, Podda Met al. Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc 2017; 31: 1785–1795. 10.1007/s00464-016-5175-4 [DOI] [PubMed] [Google Scholar]
- 29.Hartman SL, Nelson, MS.. What we say and what we do: self-reported teaching behavior versus performances in written simulations among medical school faculty. Acad Med 1992; 67: 522–527. 10.1097/00001888-199208000-00010 [DOI] [PubMed] [Google Scholar]
- 30.Sallinen V, Di Saverio S, Haukijarvi Eet al. Laparoscopic versus open adhesiolysis for adhesive small bowel obstruction (LASSO): an international, multicentre, randomised, open-label trial. Lancet Gastroenterol Hepatol 2019; 4: 278–286. 10.1016/S2468-1253(19)30016-0 [DOI] [PubMed] [Google Scholar]
- 31.Gunaratnam C, Bernstein M. Factors affecting surgical decision-making-a qualitative study. Rambam Maimonides Med J 2018; 9: e0003. 10.5041/RMMJ.10324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coleman MG, Hanna GB, Kennedy Ret al. The National Training Programme for Laparoscopic Colorectal Surgery in England: a new training paradigm. Colorectal Dis 2011; 13: 614–616. 10.1111/j.1463-1318.2011.02643.x [DOI] [PubMed] [Google Scholar]
- 33.Green CJ, Maxwell R, Verne Jet al. The influence of NICE guidance on the uptake of laparoscopic surgery for colorectal cancer. J Public Health (Oxf ) 2009; 31: 541–545. 10.1093/pubmed/fdp027 [DOI] [PubMed] [Google Scholar]