BACKGROUND
Uncomplicated paediatric umbilical hernias are common. The literature reports low postoperative morbidity (2%), recurrence rates (2%) and good patient-reported cosmetic results (90% satisfaction).1 We describe a refined approach to that previously described,2 improving the cosmetic result (Figures 1–4).
Figure 1 .

Uncomplicated paediatric umbilical hernia
Figure 4 .

Postoperative result
TECHNIQUE
The umbilical skin is lifted and the excess umbilical skin excised (Figure 2). Through this opening the defect in the linea alba is identified. The hernia sac is reduced or excised. The defect is closed with interrupted 3-0 absorbable sutures. The skin is closed with two sutures. A suture to anchor the neo-umbilicus to the linea alba is inserted first but not tied: the defect in the skin is closed with a subcuticular purse-string before tying the anchoring suture to create an umbilical depression (Figure 3).
Figure 2 .
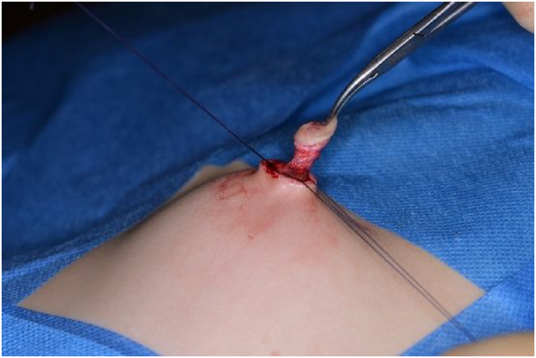
Excess umbilical skin excised, providing better access to the hernia defect
Figure 3 .

Closure of defect
DISCUSSION
In the last 6 years, the senior author has repaired 35 congenital umbilical hernias using this technique. The mean age was 4.4 years (range, 0.3–11.0 years). There have been no postoperative complications or recurrences and good cosmetic outcomes (Figure 4). The average follow up was 122 days (range, 22–180 days), for which 31.4% (n=11) of the patients attended a follow-up clinic appointment. However, long-term results have not been assessed for all patients. With this refined approach, a visible scar is avoided adjacent to the umbilicus and excess and potentially unsightly skin is removed, providing better access to the hernia defect to facilitate the repair and improving the cosmetic result.
References
- 1.Zendeja B, Kuchena A, Onkendi EO, et al. Fifty-three-year experience with pediatric umbilical hernia repairs. J Pediatr Surg 2011; 46: 2151–2156. 10.1016/j.jpedsurg.2011.06.014 [DOI] [PubMed] [Google Scholar]
- 2.Gilleard O, Gee AS. Paediatric umbilical herniplasty. Ann R Coll Surg Engl 2008; 90: 426–427. 10.1308/rcsann.2008.90.5.426 [DOI] [PMC free article] [PubMed] [Google Scholar]


