Abstract
Background and Aims
Problematic internet use (PIU) by children and adolescents is a concern for many parents. Several factors, including students’ education level, the method of instruction, the dependence on the internet, and their intended use of the internet, could all be contributing factors to PIU and depression. Disturbed mental health may be attributed to the cancellation of physical education classes because of the COVID‐19 outbreak. This study aimed to assess the association of COVID‐19 pandemic with PIU and depressive symptoms in adolescent students.
Methods
We performed this cross‐sectional study among 491 school‐going adolescents of 10 to 16 years. Self‐administered questionnaires were applied to collect sociodemographic information and the internet usage pattern of the participants. We measured the prevalence of PIU and depressive symptoms using the PIU questionnaire (PIUQ‐SF‐6) and patient health questionnaire‐9 (PHQ‐9).
Results
The estimations of the risk group for PIU and depressive symptoms among school‐going adolescents were 80.04% and 77.80%, respectively. The latent profiling of PIU scores for obsession, neglect, and control sub‐groups were 5.82, 6.12, and 6.35, respectively. Moreover, we observed mild, moderate, and severe depressive symptoms in 48.68%, 27.70%, and 1.43% of cases. Age, education level, medium of education, financial impression, internet connection, the device used, the purpose for internet use, and the living status of respondents were significantly associated with the PIU. Reported mental health issues was associated with education level, medium of education, financial impression, and internet connection.
Conclusion
The present study revealed an association of PIU and depressive symptoms with sociodemographic factors and internet usage patterns. Therefore, these results might have practical implications in clinical psychology, psychiatry, and psychotherapy. The healthcare professional can develop a context‐specific comprehensive clinical intervention plan for children and adolescents.
Keywords: adolescents, COVID‐19, depressive symptoms, mental health, problematic internet use
1. INTRODUCTION
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID‐19) as a pandemic on March 11, 2020, and the world is now in a chaotic state due to the COVID‐19 pandemic. 1 , 2 This pandemic resulted in a ban on all non‐essential outdoor activities to stop the spread of the virus. 3 , 4 Thus, the COVID‐19 pandemic impacted individuals from all backgrounds. 5 The mental health of people across the globe has altered due to several COVID‐19 responses. 6 The consequences of lockdown, such as separating from loved ones, insufficient food, the loss of freedom, ambiguity in household supplies, and so forth, may be responsible for developing mental health‐related issues such as anxiety, and depressive symptoms. 7 , 8 The life of students changed considerably when educational institutions suspended classroom teaching in favor of online learning, and this pandemic catastrophe may have compounded the damage by causing emotional stress. 9 , 10 , 11 Poor mental health is a discomfort for students because of their age. Any disruption during study time can have far‐reaching long‐term consequences in their life. The COVID‐19 pandemic has several implications for students of all ages. It affects sleep patterns, exercise routines, learning mediums, and the effects on weight, social life, and mental health. 12 The psychological and social impact of the COVID‐19 pandemic is already affecting the mental health of school‐going young children and adolescents and will continue to do so in the future. 13
The COVID‐19 pandemic may have more long‐term negative consequences for children and adolescents than adults. The development phase of life, present educational status, special requirements, pre‐existing mental health issues, and economic status of children and adolescents are vulnerable factors for poor mental health. Such factors may be responsible for developing depressive disorder among school‐going adolescents. 14 , 15 Similar to other countries, the Bangladesh government has decided to close all educational institutions to prevent COVID‐19 from spreading during the early stage of the pandemic. 16 , 17 , 18 The authorities promoted online education for several months. 19 Unfortunately, over 90% of students suffered significantly from widespread school and institution closures worldwide. 20 Children and adolescents confined to their homes experience uncertainty and anxiety due to disruptions in their schooling, physical activity, and possibilities for socializing. 21 The absence of a disciplined educational setting for an extended time involves changes in routine, boredom, and a lack of inventive ideas for engaging in different academic and extracurricular activities. Some children have shown reduced levels of effectiveness as a case of not being able to explore outside, meet up with friends, or participate in in‐person academic activities. 20 , 22 , 23 Children who have been in lockdown for a year or more are clingier, attention‐seeking, and reliant on their parents. Restarting academic activities and restricting their freedom of movement would have a long‐term harmful impact on their mental health. The development of negative psychological issues would play a detrimental role here.
On the other hand, lockdown measures implemented during the COVID‐19 pandemic have increased the use of digital devices with internet connection. 24 , 25 Students rely heavily on technology and the internet to pass the time or attend online schools. 26 Students are on the internet for educational, recreational, and social reasons during the pandemic. 27 Though the online world has been a game‐changer for teenagers in many ways, its usage can also become disruptive and troublesome, with severe consequences for their mental health. 28 Adolescents may not be able to limit their internet use, resulting in feelings of discomfort, impairment in everyday tasks, and the development of internet addiction. The term “internet addiction” refers to problematic internet use (PIU). 29 Behavioral difficulties, hyperactivity, and depressive symptoms are associated with PIU. The PIU over a certain level is related to negative impacts on everyday functioning and physical health. 30 Even before the COVID‐19‐related lockdowns, studies had depicted increased internet addiction as an imminent concern. Also, PIU is widespread throughout all domains and platforms (e.g., on smartphones and gaming devices) in most countries. According to current publications, lockdown limitations in India, Taiwan, Indonesia, and Mexico have shown a surge in PIU among young people. 31 Young adults are participating in many online activities such as gambling, video gaming, streaming films, television shows, and social networking sites to cope with their low moods. These potentially addictive activities may aid in reducing stress in daily life. However, avoidance of difficult tasks and trouble thinking will have long‐term consequences. 32 During the lockdown, there was a significant increase in anxiety and depressive symptoms and growing concerns about the internet's influence on mental health. These mental health issues are linked to PIU among teenagers in several nations. 31
In short, The COVID‐19 pandemic is responsible for developing PIU along with significant mental health issues such as depressive symptoms among school‐going adolescents. In our current study, we aimed to investigate PIU and depressive symptoms among school‐going adolescents in Bangladesh. The findings might aid future developmental research and the implementation of scientific proof‐based detailed interventional strategies for vulnerable adolescents both during and after the COVID‐19 pandemic.
2. MATERIALS AND METHODS
2.1. Study design and participants
We conducted this online cross‐sectional survey from October 1, 2021, to December 30, 2021. We considered convenient sampling for this survey. The margin of error, response rate, and confidence level were considered as 5%, 50%, and 95%, respectively. To get 80% statistical power, we needed 384 responses based on the above estimations. Initially, we received responses from a total of 502 persons. After analyzing responses, we decided to exclude 11 responses because of inaccurate or missing information. And then, 491 responses were chosen to include in the final analysis. The study's goal, eligibility conditions, and methodology were well explained to all participants. At the commencement of the study, we received an electronic authorization form from each participant. In addition, all of the respondents were Bangladeshi nationals who lived in Bangladesh at the moment of data collection. We included participants enrolled at a high school in Bangladesh between 10 and 16 years of age. Participants having varied mental diseases identified by a physician as well as a history of addiction were not allowed to participate in this study. The information was provided voluntarily by all participants.
2.2. Estimations
We gathered information on the association of sociodemographic variables and internet usage patterns with depressive symptoms and PIU among school‐going adolescents. We examined depressive symptoms using the PHQ‐9 and assessed PIU by utilizing PIU questionnaires. We used a pre‐structured questionnaire set developed by researchers to acquire the essential sociodemographic data. The questionnaire was initially written in English and then translated into Bangla. We enlisted the support of two Bangla native speakers (a medical graduate and a nonmedical person) fluent in English to translate the questions. An independent author joined the translated versions to generate a single Bangla forward version, and conflicts were addressed with the help of a third author. Professional translators with expertise in medical translation converted this Bangla version into two English questionnaires. An independent researcher combined these back‐translated versions to create a single English version. 33 Then, using a small sample of randomly selected participants, we conducted pilot research to check that the questions were clear and understandable. Finally, we gave the survey questionnaire both in Bangla and English to ensure proper understanding.
2.3. Data collection
To collect all of the responses from our target population, we used the Google survey tool (Google Forms). We sent the survey link to the participants via email, Facebook Messenger, WhatsApp, and other social media platforms. A self‐administered questionnaire was supplied to gather information on mental health, internet usage patterns, and sociodemographic profile. To address any issues or ensure that the questionnaire was fully understood, we offered help via video conferences or phone conversations.
2.4. Sociodemographic and biophysical measures
The most relevant sociodemographic information related to our study was collected from our respondents. Collected data were regarding age, sex, BMI, current education status, family economic impression, smoking habit, etc.
2.5. Patient health questionnaire
The patient health questionnaire‐9 (PHQ‐9) is a widely used questionnaire with nine separate items to assess respondents’ depressed symptoms. 24 The total score for these self‐administered questions is 0–27, with a score of 0–3 assigned to each question (0=not at all; 1=several days; 2=more than a week; 3=nearly every day). The overall score is broken into four individual portions to represent different levels of depressive symptoms: mild symptoms if the score is 9 or less; moderate symptoms if the score is 10–14; moderately severe symptoms if the score is 15–19; and severe symptoms if the score is 20 or above. 34 , 35 , 36
2.6. PIU questionnaire
To assess the PIU, the 6‐item short form of the PIU questionnaire (PIUQ‐SF‐6) was used. This simplified version was created with only six items to examine more impulsive groups in a short time. Three factors of IU such as obsession, neglect, and control disorder, were assessed by using PIUQ‐SF‐6. To determine how much the supplied statements defined the respondents, a 5‐point Likert scale (“never,” “rarely,” “sometimes,” “often,” and “often/almost always”) was employed. The range of values is from 6 to 30, with higher scores suggesting a higher risk of PIU. 37
2.7. Data analysis
The data analysis was performed with the help of Microsoft Excel 2019 and Statistical Packages for Social Sciences (IBM SPSS) V.25.0. Data processing, sorting, coding, classification, and tabulation were all accomplished with Microsoft Excel. The Excel file was then imported into IBM SPSS. To examine the characteristics of study participants, descriptive statistics were used. The chi‐square test was used to look for variations between the group statistics. We performed binary logistic regression analysis to find the risk estimations of independent variables against different dependent variables. We also compared the distribution of responses between groups using bar graphs. We evaluated statistically significant findings from analyses at p < 0.05.
3. RESULTS
3.1. Characteristics of respondents
We presented the demographic profile of participants in Table 1. Among the respondents, males and females were 40.93% and 59.07%, respectively. More than three‐fourths of the respondents (85.54%) were between 14 and 16 years, and 84.13% of respondents had normal BMI. Almost half of the respondents (42.77%) were from class 9, and 62.32% of participants were from the Bangla medium. Moreover, more than half of the respondents (64.96%) belonged to a middle‐class family, and 92.26% lived in urban areas. About two‐thirds of the respondents lived with family (78.2%), and almost all were nonsmokers (94.29%).
Table 1.
Distribution of sociodemographic variables and their association with problematic internet use and depression among school‐going adolescents in Bangladesh
| Sociodemographic parameters | Total (N = 491) | Problematic internet use (N = 393) | Depression (N = 382) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | χ2 | df | p Value | n | % | χ2 | df | p Value | |
| Age in years | ||||||||||||
| 10–13 | 71 | 14.46 | 50 | 12.72 | 4.806 | 1 | 0.028 | 59 | 15.45 | 1.349 | 1 | 0.245 |
| 14–16 | 420 | 85.54 | 343 | 87.28 | 323 | 84.55 | ||||||
| Sex | ||||||||||||
| Female | 290 | 59.07 | 234 | 59.54 | 0.187 | 1 | 0.666 | 228 | 59.69 | 0.276 | 1 | 0.599 |
| Male | 201 | 40.93 | 159 | 40.46 | 154 | 40.31 | ||||||
| BMI (kg/m2) | ||||||||||||
| 18.5–25 (normal) | 413 | 84.13 | 325 | 82.70 | 3.410 | 2 | 0.182 | 319 | 83.51 | 1.455 | 2 | 0.483 |
| Above 25 (obese) | 48 | 9.77 | 43 | 10.94 | 37 | 9.69 | ||||||
| Below 18.5 (CED) | 30 | 6.10 | 25 | 6.36 | 26 | 6.81 | ||||||
| Education level | ||||||||||||
| Six | 6 | 1.23 | 2 | 0.51 | 12.673 | 4 | 0.013 | 3 | 0.79 | 23.197 | 4 | <0.001 |
| Seven | 29 | 5.91 | 26 | 6.62 | 25 | 6.54 | ||||||
| Eight | 111 | 22.60 | 87 | 22.14 | 92 | 24.08 | ||||||
| Nine | 210 | 42.77 | 175 | 44.53 | 175 | 45.81 | ||||||
| Ten | 135 | 27.49 | 103 | 26.21 | 87 | 22.77 | ||||||
| Medium of education | ||||||||||||
| Bangla | 306 | 62.32 | 231 | 58.78 | 10.527 | 1 | 0.001 | 223 | 58.38 | 11.404 | 1 | 0.001 |
| English | 185 | 37.68 | 162 | 41.22 | 159 | 41.62 | ||||||
| Economic impression | ||||||||||||
| High | 161 | 32.79 | 139 | 35.37 | 7.325 | 2 | 0.026 | 139 | 36.39 | 10.762 | 2 | 0.005 |
| Medium | 319 | 64.96 | 244 | 62.09 | 236 | 61.78 | ||||||
| Low | 11 | 2.25 | 10 | 2.54 | 7 | 1.83 | ||||||
| Residence area | ||||||||||||
| Urban | 453 | 92.26 | 363 | 92.37 | 0.031 | 1 | 0.861 | 356 | 93.19 | 2.098 | 1 | 0.148 |
| Rural | 38 | 7.74 | 30 | 7.63 | 26 | 6.81 | ||||||
| Living status | ||||||||||||
| With family | 384 | 78.20 | 300 | 76.34 | 4.048 | 1 | 0.044 | 292 | 76.44 | 3.156 | 1 | 0.076 |
| Without family | 107 | 21.80 | 93 | 23.66 | 90 | 23.56 | ||||||
| Smoking habit | ||||||||||||
| Nonsmoker | 463 | 94.29 | 369 | 93.89 | 0.598 | 1 | 0.439 | 362 | 94.76 | 0.698 | 1 | 0.403 |
| smoker | 28 | 5.71 | 24 | 6.11 | 20 | 5.24 | ||||||
Note: p values are significant at 95% confidence interval (p < 0.05). Significant p values are shown in bold.
Abbreviations: χ2, chi‐square; BMI, body mass index; CED, chronic energy deficiency; df, degree of freedom; N, number.
3.2. Association of PIU with demographic variables and internet use pattern
The risk group was estimated to be 80.04% according to the PIUQ‐SF‐6 scale among school‐going adolescents in Bangladesh. Among them, latent profiling of PIU scores for obsession, neglect, and control sub‐groups were 5.82, 6.12, and 6.35, respectively (Figure 1). We estimated the association of PIU with sociodemographic variables (Table 1). The high prevalence of PIU was observed in (i) respondents aged 14–16 versus respondents aged 10–13 (87.28% vs. 12.72%, p = 0.028), (ii) females versus males (59.54% vs. 40.46%, p = 0.666), (iii) BMI 18.5–25 kg/m2 versus BMI below 18.5 kg/m2 (82.70% vs. 6.36%, p = 0.182), (iv) respondents read in class 9 versus respondents read in class 6 (44.53% vs. 0.51%, p = 0.013), (v) respondents read in Bangla medium versus respondents read in English medium (58.78% vs. 41.22%, p = 0.001), (vi) medium versus low economic background (62.09% vs. 2.54%, p = 0.026), (vii) urban versus rural (92.37% vs. 7.63, p = 0.861), (viii) staying with a family versus staying without family (76.34% vs. 23.66%, p = 0.044), and (ix) nonsmoker versus smoker (93.89% vs. 6.11%, p = 0.439).
Figure 1.
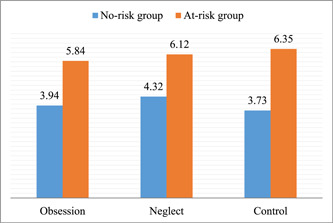
Latent profiling of problematic internet use against PIUQ‐SF‐6 score among school‐going adolescents in Bangladesh. PIUQ‐SF‐6, Problematic Internet Use Questionnaire Short Form.
At the same time, we estimated the association of PIU with the internet use pattern (Table 3). The prevalence of PIU was higher in (i) individuals using Wi‐Fi versus individuals using mobile data (60.31% vs. 39.69%, p = 0.016), (ii) individuals using a smartphone for internet use versus individuals using a desktop for internet use (66.67% vs. 9.41%, p = 0.028), and (iii) individuals using the internet for social media use versus individuals using the internet for a random purpose (41.73% vs. 4.07%, p < 0.001).
Table 3.
Description of internet use and their association with problematic internet use and depression among school‐going adolescents in Bangladesh
| Internet use pattern | Total (N = 491) | Problematic internet use (N = 393) | Depression (N = 382) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | χ2 | df | p Value | n | % | χ2 | df | p Value | |
| Internet connection | ||||||||||||
| WiFi | 309 | 62.93 | 237 | 60.31 | 5.827 | 1 | 0.016 | 228 | 59.69 | 7.777 | 1 | 0.005 |
| Mobile data | 182 | 37.07 | 156 | 39.69 | 154 | 40.31 | ||||||
| Device used for internet | ||||||||||||
| Desktop | 49 | 9.97 | 37 | 9.41 | 9.116 | 3 | 0.028 | 40 | 10.47 | 2.695 | 3 | 0.441 |
| Laptop | 59 | 12.02 | 49 | 12.47 | 47 | 12.30 | ||||||
| Smartphone | 336 | 68.43 | 262 | 66.67 | 255 | 66.75 | ||||||
| TV | 47 | 9.58 | 45 | 11.45 | 40 | 10.47 | ||||||
| Purpose for internet use | ||||||||||||
| Education | 75 | 15.27 | 54 | 13.74 | 28.682 | 4 | <0.001 | 52 | 13.61 | 68.867 | 4 | <0.001 |
| Games | 160 | 32.60 | 137 | 34.86 | 138 | 36.13 | ||||||
| Movie | 25 | 5.09 | 22 | 5.60 | 23 | 6.02 | ||||||
| Social media | 198 | 40.32 | 164 | 41.73 | 161 | 42.15 | ||||||
| Others | 33 | 6.72 | 16 | 4.07 | 8 | 2.09 | ||||||
Note: p values are significant at a 95% confidence interval (p < 0.05). Significant p values are shown in bold.
Abbreviations: χ2, chi‐square; df, degree of freedom; N, number; TV, television.
3.3. Association of depressive symptoms with demographic variables and internet use pattern
The depressive symptoms were estimated to be 77.80% among all respondents. Among them, mild, moderate, and severe depressive symptoms were reported as 48.68%, 27.70%, and 1.43%, respectively (Figure 2). We estimated the prevalence of depressive symptoms associated with sociodemographic variables (Table 1). The frequency of having depressive symptoms was higher in (i) respondents aged 14–16 versus respondents aged 10–13 (84.55% vs. 15.45%, p = 0.245), (ii) females versus males (59.69% vs. 40.31%, p = 0.599), (iii) BMI 18.5–25 kg/m2 versus BMI below 18.5 kg/m2 (83.51% vs. 6.81%, p = 0.483), (iv) respondents read in class 9 versus respondents read in class 6 (45.81% vs. 0.79%, p < 0.001), (v) respondents read in Bangla medium versus respondents read in English medium (58.38% vs. 41.62%, p = 0.001), (vi) medium versus low economic background (61.78% vs. 1.83%, p = 0.005), (vii) urban versus rural (93.19% vs. 6.81, p = 0.148), (viii) staying with a family versus staying without family (76.44% vs. 23.56%, p = 0.076), and (ix) nonsmoker versus smoker (94.76% vs. 5.24%, p = 0.403).
Figure 2.
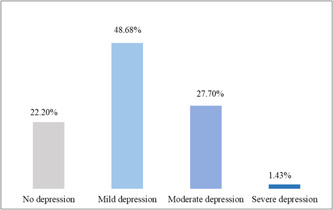
Prevalence of depression and its severity among school‐going adolescents in Bangladesh.
At the same time, we estimated the prevalence of depressive symptoms associated with the internet use pattern (Table 3). More prone to have depressive symptoms was observed in (i) individuals using Wi‐Fi versus individuals using mobile data (59.69% vs. 40.31%, p = 0.005), (ii) individuals using a smartphone for internet use versus individuals using a desktop for internet use (66.75% vs. 10.47%, p = 0.441), and (iii) individuals using the internet for social media use versus individuals using the internet for a random purpose (42.15% vs. 2.09%, p < 0.001).
3.4. Regression analysis
We estimated the correlations between the independent and dependent variables of the demographic profile with the help of binary logistic regression analysis (Table 2). Depressive symptoms were experienced by 7.35 times fewer individuals who studied in class 8 than individuals who studied in class 9 (p = 0.014). Respondents with high economic backgrounds were 0.5 times less likely to have depressive symptoms than respondents with low economic backgrounds (p = 0.014). PIU was found 2.12 times higher in respondents aged between 10 and 13 years than respondents aged 14–16 years (odds ratio [OR] = 2.12, 95% confidence interval [CI] = 1.018–4.453, p = 0.045). Moreover, respondents in the Bangla medium experienced 1.76 times PIU than respondents in the English medium (OR = 1.76, 95% CI = 1.013–3.071, p = 0.045).
Table 2.
Regression analysis of sociodemographic variables by problematic internet use and depression among school‐going adolescents in Bangladesh
| Sociodemographic parameters | Problematic internet use (N = 393) | Depression (N = 382) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | df | 95% CI | p Value | OR | df | 95% CI | p Value | |
| Age in years | ||||||||
| 10–13 | 2.129 | 1 | 1.018–4.453 | 0.045 | 0.762 | 1 | 0.335–1.733 | 0.517 |
| 14–16 | 1 | 1 | ||||||
| Sex | ||||||||
| Female | 0.944 | 1 | 0.576–1.547 | 0.819 | 1.032 | 1 | 0.637–1.670 | 0.899 |
| Male | 1 | 1 | ||||||
| BMI (kg/m2) | ||||||||
| Below 18.5 (CED) | 1.076 | 1 | 0.250–4.636 | 0.922 | 0.388 | 1 | 0.098–1.535 | 0.177 |
| 18.5–25 (normal) | 2.115 | 1 | 0.790–5.660 | 0.136 | 1.154 | 1 | 0.542–2.459 | 0.710 |
| Above 25 (obese) | 1 | 1 | ||||||
| Education level | ||||||||
| Six | 0.701 | 1 | 0.346–1.423 | 0.326 | 0.427 | 1 | 0.217–0.839 | 0.014 |
| Seven | 0.675 | 1 | 0.379–1.201 | 0.181 | 0.414 | 1 | 0.241–0.714 | 0.001 |
| Eight | 0.270 | 1 | 0.068–1.072 | 0.063 | 0.350 | 1 | 0.105–1.160 | 0.086 |
| Nine | 5.063 | 1 | 0.628–40.820 | 0.128 | 2.571 | 1 | 0.374–17.669 | 0.337 |
| Ten | 1 | 1 | ||||||
| Medium of education | ||||||||
| Bangla | 1.763 | 1 | 1.013–3.071 | 0.045 | 1.527 | 1 | 0.896–2.603 | 0.120 |
| English | 1 | 1 | ||||||
| Economic impression | ||||||||
| High | 0.588 | 1 | 0.339–1.021 | 0.059 | 0.505 | 1 | 0.292–0.872 | 0.014 |
| Medium | 0.274 | 1 | 0.028–2.703 | 0.268 | 1.471 | 1 | 0.362–5.981 | 0.590 |
| Low | 1 | 1 | ||||||
| Residence area | ||||||||
| Urban | 1.115 | 1 | 0.451–2.757 | 0.814 | 1.368 | 1 | 0.605–3.098 | 0.452 |
| Rural | 1 | 1 | ||||||
| Living status | ||||||||
| With family | 1.692 | 1 | 0.890–3.217 | 0.108 | 1.506 | 1 | 0.825–2.746 | 0.182 |
| Without family | 1 | 1 | ||||||
| Smoking habit | ||||||||
| Nonsmoker | 1.632 | 1 | 0.513–5.192 | 0.407 | 1.090 | 1 | 0.425–2.796 | 0.858 |
| Smoker | 1 | 1 | ||||||
Note: p values are significant at a 95% confidence interval (p < 0.05). Significant p values are shown in bold.
Abbreviations: BMI, body mass index; CED, chronic energy deficiency; CI, confidence interval; df, degree of freedom; N, number; OR, odds ratio.
Similarly, we estimated the correlations between the independent and dependent variables of internet use patterns with the help of binary regression analysis (Table 4). 0.5 times fewer individuals experienced depressive symptoms when using Wi‐Fi than mobile data (p = 0.028). The probability of having depressive symptoms was 11.70 times higher in persons using the internet for random purposes than persons using the internet for social media (p = 0.032). Respondents who use Wi‐Fi were less likely to experience PIU than the respondents who use mobile data (OR = 0.556, 95% CI = 0.332–0.932, p = 0.026). PIU was experienced 8.46 times higher in individuals while using the desktop for the internet than using the TV for the internet (p = 0.008). The probability of experiencing PIU was 4.19 times higher in persons using the internet for random purposes than in persons using the internet for social media (p = 0.025).
Table 4.
Regression analysis of internet usage pattern by problematic internet use and depression among school‐going adolescents in Bangladesh
| Description of internet use | Problematic internet use (N = 393) | Depression (N = 382) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | df | 95% CI | p Value | OR | df | 95% CI | p Value | |
| Internet connection | ||||||||
| WiFi | 0.556 | 1 | 0.332–0.932 | 0.026 | 0.563 | 1 | 0.337–0.940 | 0.028 |
| Mobile data | 1 | 1 | ||||||
| Device used for internet | ||||||||
| Desktop | 8.469 | 1 | 1.742–41.176 | 0.008 | 1.320 | 1 | 0.428–4.070 | 0.629 |
| Laptop | 3.945 | 1 | 0.803–19.382 | 0.091 | 1.141 | 1 | 0.389–3.342 | 0.810 |
| Smartphone | 7.151 | 1 | 1.659–30.822 | 0.008 | 1.785 | 1 | 0.744–4.285 | 0.194 |
| TV | 1 | 1 | ||||||
| Purpose for internet use | ||||||||
| Education | 2.114 | 1 | 1.099–4.067 | 0.025 | 1.983 | 1 | 1.062–3.702 | 0.032 |
| Games | 0.741 | 1 | 0.413–1.331 | 0.316 | 0.651 | 1 | 0.364–1.163 | 0.147 |
| Movie | 0.824 | 1 | 0.225–3.015 | 0.770 | 0.441 | 1 | 0.098–1.994 | 0.288 |
| Social media | 4.192 | 1 | 1.895–9.271 | <0.001 | 11.704 | 1 | 4.832–28.348 | <0.001 |
| Others | 1 | 1 | ||||||
Note: p values are significant at 95% confidence interval (p < 0.05). Significant p values are shown in bold.
Abbreviations: CI, confidence interval; df, degree of freedom; N, number; OR, odd ratio; TV, television.
4. DISCUSSION
Mental disorders are now widely regarded as one of the most severe public health problems worldwide. The burden of mental disorders is considerable in low‐ and middle‐income nations. 38 , 39 , 40 At the same time, psychiatric diseases in children and adolescents are undeniably common and distressing. About 10%–20% of adolescents are affected by mental health problems worldwide. A large‐scale survey conducted in Bangladesh claimed that 18% of children and adolescents struggled with mental health issues. 41 , 42 The mental health of school‐going children and adolescents was greatly affected during the lockdown due to the COVID‐19 pandemic. The sudden separation from school, social, and outdoor activities had a significant influence on the mental health of children and adolescents. Therefore, they suffer from heightened depressive symptoms. 43 , 44 The widespread closure of schools and institutions may affect more than 90% of the student population worldwide. 20 As a solution, many governments introduced online education, 9 which may act as an influence to increase dependency on digital devices and engage with the online world. 24 The children may be unable to control their engagement with the online world and become addicted to internet usage. These may make them prone to PIU. 29 Several studies conducted among online addicted adolescents revealed a close relationship between the development of depressive symptoms, aggression, and impulsivity with PIU. 45 Thus, the COVID‐19 pandemic worsens depressive disorder among school‐going adolescents and contributes to PIU.
We conducted the present study to investigate problematic internet (PIU) use and depressive symptoms among school‐going adolescents during the COVID‐19 pandemic. According to our analysis, from the perspective of the sociodemographic profile, we concluded that age, sex, BMI, education level, medium of education, financial condition, area of residence, and smoking habit might be responsible for developing mental health issues. Adolescents between the age of 14 and 16 years were supposed to be the more vulnerable group, about 84.55% of them experienced depressive symptoms, and 87.28% of them went through PIU problems. Male students experienced fewer problems than female students during the pandemic. Almost 60% of females dealt with the issue of depressive symptoms (59.69%) and PIU (59.54%). The impact of BMI was clear among our participants. We have discovered that participants with normal BMI (18.5–25 kg/m2) struggled the most with depressive symptoms and PIU. An absolute correlation could have been established between educational level and PIU and depressive symptoms. The respondents in class 9 complained of going through PIU and depressive symptoms more than the other participants. Also, we found that students in Bangla medium were more vulnerable to PIU and depressive symptoms. Financial conditions may have a direct effect on PIU and depressive symptoms. Participants with medium economic impressions were going through such issues more. About 62.09% and 61.78% of participants with medium economic backgrounds suffered from PIU problems and depressive symptoms. According to our findings, students living in an urban area (PIU = 92.37%, depressive symptoms = 93.19%), having no smoking habit (PIU = 93.89%, depressive symptoms = 94.76%) might be more at risk of PIU and depressive symptoms. Most of our respondents lived with their families, and almost more than 76% of them complained of experiencing PIU during the COVID‐19 pandemic. From the perspective of internet use pattern, we concluded that the mode of internet connection, type of device used for the internet, and purpose of internet use might be responsible for emerging PIU and depressive symptoms among our respondents. The participants who used mobile data for the internet experienced less depressive moods and dealt less with PIU than other participants. We found that participants who used the smartphone for internet use reported more depressive symptoms (66.75%) and more struggled with PIU (66.67%) than others. About 41.74% and 42.15% of our participants experienced PIU and depressive symptoms while using the internet for social media.
The lockdown due to COVID‐19 has increased students' engagement with internet use. 46 , 47 , 48 , 49 , 50 , 51 , 52 Students are sometimes unable to participate in face‐to‐face communication since they need to attend an online class. 53 , 54 , 55 This increased involvement of students in the digital world may contribute to the growth of PIU. 56 , 57 A study observed that school‐going adolescents involved more with the internet (e.g., gaming, talking, or streaming videos) are more likely to develop depressive symptoms because they are subjected to unrealistic depictions of others. 57 , 58 Another study concluded that the COVID‐19 pandemic has been responsible for increasing internet use, thus contributing to the development of PIU issue, even before the pandemic same scenario has been observed. 32 , 59 Similar to our study findings, the association of sex, age, living area, and attachment with social sites have been found as contributing factors to PIU. 60 A study has established the association between PIU and depressive symptoms. The study claimed that school closure due to COVID‐19 might cause to develop and increase PIU among students, and PIU may contribute to the development of depressive disorder. 61
As far as our concern, our study is the first approach in Bangladesh to assess the PIU and depressive symptoms among school‐going adolescents during the COVID‐19 pandemic. We found some key factors of the sociodemographic profile, including age, sex, education level, medium of education, economic impression, and smoking, might involve in the development of depressive symptoms and PIU. Nevertheless, we found some critical factors of internet use pattern, including the mode of internet connection, the device used for internet use, and the purpose of internet use that may have contributed to the development of depressive symptoms and PIU. The involvement of demographic factors such as smoking habits, education level, and so forth, and internet usage patterns in the development of PIU. 32 A study claimed that female adolescents between the age of 10 and 12 were vulnerable to the development of depressive symptoms due to the COVID‐19 pandemic. 62 Our study found some sociodemographic factors (e.g., education level, medium of education) and internet use patterns (e.g., internet connection and purpose of internet use) that might be responsible for progressing PIU and depressive symptoms. 63 , 64 Therefore, we recommend longitudinal studies with large sample sizes from different geographical locations for better results.
4.1. Implications for practice
The current study findings have widespread implications. Healthcare professionals can easily differentiate the key sociodemographic factors and internet use patterns that may have contributed to the development of such mental health issues. The healthcare authority should pay attention to developing practical guidelines for the intervention of physical and psychological health of school‐going adolescents. Also, they can improve adolescents' access to mental health support. At the same time, this study's findings can be used in policymaking decisions regarding the mental health of adolescents in countries with similar socioeconomic backgrounds.
4.2. Limitations and strong points
The present study has a few shortcomings. Using Google forms for self‐reporting surveys will induce bias. Furthermore, people who do not have access to the internet were excluded from the study. The inclusion of offline participants or offline surveys or interviews might provide a different picture. Moreover, we are unable to examine these mental health concerns over time in our cross‐sectional investigation, and due to the nature of this investigation. We did not consider how respondents' lifestyles changed throughout the COVID‐19 outbreak. Many of the participants were from the capital city of the Dhaka division, limiting the application of our results to rural locations. All these limitations restrict the scope of our findings. This study contains several noteworthy findings. To begin, the current study assessed the two significant consequences, that is, PIU and depressive symptoms due to the COVID‐19 pandemic among school‐going adolescents. We were able to obtain data from our participants of diverse socioeconomic backgrounds in a timely way because we used Google forms for data collection. Moreover, we employed the mental health assessment scales in Bangla, which ensured that the questions were clearly understood.
5. CONCLUSION
The COVID‐19 pandemic has a significant impact on adolescents' academic performance, mental health, and well‐being. Protecting students' psychological well‐being is a public health concern. Therefore, during and after the ongoing COVID‐19 pandemic, healthcare authorities should pay special attention to preserving these adolescents' mental health. To reduce PIU among adolescents who are vulnerable, specially developed programs should be introduced. Interventions should be implemented by educational institutions to help adolescents with PIU and depressive symptoms.
AUTHOR CONTRIBUTIONS
Md. Rabiul Islam: Conceptualization; formal analysis; writing – review and editing. Md. Ismail Tushar: Formal analysis. Papia Sen Tultul: Conceptualization. Rabeya Akter: Conceptualization. Md. Sohan: Formal analysis. Ramisa Anjum: Writing – original draft. Arpita Roy: Writing – original draft. Md. Jamal Hossain: Writing – original draft. Md. Ashrafur Rahman: Writing – review and editing. Zabun Nahar: Writing – review and editing. Mohammad Shahriar: Supervision. Mohiuddin Ahmed Bhuiyan: Supervision.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
The Research Ethics Committee, University of Asia Pacific, has approved this study protocol (Ref: UAP/Pharm/2021/01003). The entire study was conducted following the Declaration of Helsinki. Before participation, the authors briefed them about the objective and purpose of this study to the legal guardians of participants. Also, the authors took written consent from them.
TRANSPARENCY STATEMENT
The lead author Md. Rabiul Islam affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
All the authors are thankful to the participants for their cooperation to conduct this study.
Islam MR, Tushar MI, Tultul PS, et al. Problematic internet use and depressive symptoms among the school‐going adolescents in Bangladesh during the COVID‐19 pandemic: a cross‐sectional study findings. Health Sci Rep. 2022;6:e1008. 10.1002/hsr2.1008
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article or its Supporting Information.
REFERENCES
- 1. Mohapatra RK, Tiwari R, Sarangi AK, Islam MR, Chakraborty C, Dhama K. Omicron (B.1.1.529) variant of SARS‐CoV‐2: concerns, challenges, and recent updates. J Med Virol. 2022;94(6):2336‐2342. 10.1002/jmv.27633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID‐19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2):e18810. 10.2196/18810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Islam MR, Hossain MJ. Detection of SARS‐CoV‐2 Omicron (B.1.1.529) variant has created panic among the people across the world: what should we do right now? J Med Virol. 2022;94(5):1768‐1769. 10.1002/jmv.27546 [DOI] [PubMed] [Google Scholar]
- 4. Saha J, Barman B, Chouhan P. Lockdown for COVID‐19 and its impact on community mobility in India: an analysis of the COVID‐19 Community Mobility Reports, 2020. Child Youth Serv Rev. 2020;116:105160. 10.1016/j.childyouth.2020.105160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daria S, Islam MR. Increased suicidal behaviors among students during COVID‐19 lockdowns: a concern of student's mental health in Bangladesh. J Affect Disord Rep. 2022;8:100320. 10.1016/j.jadr.2022.100320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Das R, Hasan MR, Daria S, Islam MR. Impact of COVID‐19 pandemic on mental health among general Bangladeshi population: a cross‐sectional study. BMJ Open. 2021;11(4):e045727. 10.1136/bmjopen-2020-045727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID‐19 and severe mental illness: impact on patients and its relation with their awareness about COVID‐19. Psychiatry Res. 2020;291:113265. 10.1016/j.psychres.2020.113265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rahman FI, Islam MR. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Women's Health. 2021;17:174550652110438. 10.1177/17455065211043851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mirhosseini S, Grimwood S, Dadgari A, Basirinezhad MH, Montazeri R, Ebrahimi H. One‐year changes in the prevalence and positive psychological correlates of depressive symptoms during the COVID‐19 pandemic among medical science students in northeast of Iran. Health Sci Rep. 2022;5(1):e490. 10.1002/hsr2.490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ether SA, Emon FA, Roknuzzaman A, Rakibuzzaman M, Rahman FI, Islam MR. A cross‐sectional study of COVID‐19‐related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh. SAGE Open Med. 2022;10:205031212110730. 10.1177/20503121211073014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hossain MJ, Ahmmed F, Sarker MMR, et al. Factors associated with underprivileged E‐Learning, session Jam Phobia, and the subsequent mental distress among students following the extended university closure in Bangladesh. Front Public Health. 2022;9:807474. 10.3389/fpubh.2021.807474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chaturvedi K, Vishwakarma DK, Singh N. COVID‐19 and its impact on education, social life and mental health of students: a survey. Child Youth Serv Rev. 2021;121:105866. 10.1016/j.childyouth.2020.105866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meherali S, Punjani N, Louie‐Poon S, et al. Mental health of children and adolescents amidst COVID‐19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. 2021;18(7):3432. 10.3390/ijerph18073432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shen K, Yang Y, Wang T, et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts' consensus statement. World J Pediatr. 2020;16(3):223‐231. 10.1007/s12519-020-00343-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID‐19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429. 10.1016/j.psychres.2020.113429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Daria S, Bhuiyan MA, Islam MR. Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: associated risk factors and preventive actions. J Med Virol. 2022;94(4):1267‐1268. 10.1002/jmv.27503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Islam MR. The SARS‐CoV‐2 Omicron (B.1.1.529) variant and the re‐emergence of COVID‐19 in Europe: an alarm for Bangladesh. Health Sci Rep. 2022;5(2):e545. 10.1002/hsr2.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Daria S, Asaduzzaman M, Shahriar M, Islam MR. The massive attack of COVID‐19 in India is a big concern for Bangladesh: the key focus should be given on the interconnection between the countries. Int J Health Plann Manage. 2021;36(5):1947‐1949. 10.1002/hpm.3245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mirhosseini S, Bazghaleh M, Basirinezhad MH, Abbasi A, Ebrahimi H. The relationship between depression and academic satisfaction in medical science students. J Ment Health Train Educ Pract. 2021;16(2):99‐111. 10.1108/JMHTEP-03-2020-0017 [DOI] [Google Scholar]
- 20. Lee J. Mental health effects of school closures during COVID‐19. Lancet Child Adolesc Health. 2020;4(6):421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jiao WY, Wang LN, Liu J, et al. Behavioral and emotional disorders in children during the COVID‐19 epidemic. J Pediatr. 2020;221:264‐266. 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID‐19. Lancet Child Adolesc Health. 2020;4(5):347‐349. 10.1016/S2352-4642(20)30096-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhai Y, Du X. Mental health care for international Chinese students affected by the COVID‐19 outbreak. Lancet Psychiatry. 2020;7(4):e22. 10.1016/S2215-0366(20)30089-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wong CW, Tsai A, Jonas JB, et al. Digital screen time during the COVID‐19 pandemic: risk for a further myopia boom? Am J Ophthalmol. 2021;223:333‐337. 10.1016/j.ajo.2020.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Islam MR, Jannath S, Moona AA, Akter S, Hossain MJ, Islam SMA. Association between the use of social networking sites and mental health of young generation in Bangladesh: a cross‐sectional study. J Community Psychol. 2021;49(7):2276‐2297. 10.1002/jcop.22675 [DOI] [PubMed] [Google Scholar]
- 26. Hosen I, Al Mamun F, Mamun MA. The role of sociodemographics, behavioral factors, and internet use behaviors in students' psychological health amid COVID‐19 pandemic in Bangladesh. Health Sci Rep. 2021;4(4):e398. 10.1002/hsr2.398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sedgwick R, Epstein S, Dutta R, Ougrin D. Social media, internet use and suicide attempts in adolescents. Curr Opin Psychiatry. 2019;32(6):534‐541. 10.1097/YCO.0000000000000547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Machimbarrena J, González‐Cabrera J, Ortega‐Barón J, Beranuy‐Fargues M, Álvarez‐Bardón A, Tejero B. Profiles of problematic internet use and its impact on adolescents' health‐related quality of life. Int J Environ Res Public Health. 2019;16(20):3877. 10.3390/ijerph16203877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Islam MA, Hossin MZ. Prevalence and risk factors of problematic internet use and the associated psychological distress among graduate students of Bangladesh. Asian J Gambl Issues Public Health. 2016;6(1):11. 10.1186/s40405-016-0020-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. El Asam A, Samara M, Terry P. Problematic internet use and mental health among British children and adolescents. Addict Behav. 2019;90:428‐436. 10.1016/j.addbeh.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 31. Fernandes B, Uzun B, Aydin C, et al. Internet use during COVID‐19 lockdown among young people in low‐ and middle‐income countries: role of psychological wellbeing. Addict Behav Rep. 2021;14:100379. 10.1016/j.abrep.2021.100379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Islam MS, Sujan MSH, Tasnim R, et al. Problematic internet use among young and adult population in Bangladesh: correlates with lifestyle and online activities during the COVID‐19 pandemic. Addict Behav Rep. 2020;12:100311. 10.1016/j.abrep.2020.100311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross‐cultural adaptation of self‐report measures. Spine. 2000;25(24):3186‐3191. 10.1097/00007632-200012150-00014 [DOI] [PubMed] [Google Scholar]
- 34. Sun Y, Fu Z, Bo Q, Mao Z, Ma X, Wang C. The reliability and validity of PHQ‐9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 2020;20(1):474. 10.1186/s12888-020-02885-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maurer DM, Raymond TJ, Davis BN. Depression: screening and diagnosis. Am Fam Physician. 2018;98(8):508‐515. [PubMed] [Google Scholar]
- 36. Kroenke K, Spitzer RL, Williams JBW. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606‐613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Aivali P, Efthymiou V, Tsitsika AK, et al. Validation of the Greek version of the Problematic Internet Use Questionnaire – Short Form (PIUQ‐SF‐6). EMBnet J. 2021;26:e978. 10.14806/ej.26.1.978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hossain MD, Ahmed HU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry. 2014;14:216. 10.1186/s12888-014-0216-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shalahuddin Qusar MMA, Hossain R, Sohan M, Nazir S, Hossain MJ, Islam MR. Attitudes of mental healthcare professionals and media professionals towards each other in reducing social stigma due to mental illness in Bangladesh. J Community Psychol. 2022;50:3181‐3195. 10.1002/jcop.22823 [DOI] [PubMed] [Google Scholar]
- 40. Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the Covid‐19 has worsened the situation. Chronic Stress. 2021;5:247054702110356. 10.1177/24705470211035602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kieling C, Baker‐Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515‐1525. 10.1016/S0140-6736(11)60827-1 [DOI] [PubMed] [Google Scholar]
- 42. Jesmin A, Mullick M, Zillur Rahman KM, Muntasir MM. Psychiatric disorders in children and adolescents attending pediatric out patient departments of tertiary hospitals. Oman Med J. 2016;31(4):258‐262. 10.5001/omj.2016.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. de Figueiredo CS, Sandre PC, Portugal LCL, et al. COVID‐19 pandemic impact on children and adolescents' mental health: biological, environmental, and social factors. Prog Neuropsychopharmacol Biol Psychiatry. 2021;106:110171. 10.1016/j.pnpbp.2020.110171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Panda PK, Gupta J, Chowdhury SR, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID‐19 pandemic on children, adolescents and caregivers: a systematic review and meta‐analysis. J Trop Pediatr. 2021;67(1):fmaa122. 10.1093/tropej/fmaa122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Haddad C, Malaeb D, Sacre H, et al. Association of problematic internet use with depression, impulsivity, anger, aggression, and social anxiety: results of a national study among Lebanese adolescents. Pediatr Investig. 2021;5(4):255‐264. 10.1002/ped4.12299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Alam S, Emon NU, Hosaain MJ, et al. Social perspectives of COVID‐19 pandemic in Bangladesh: a review. Bangladesh J Infect Dis. 2022;9(9):S28‐S39. 10.3329/bjid.v9i9.62613 [DOI] [Google Scholar]
- 47. Dhama K, Nainu F, Frediansyah A, et al. Global emerging Omicron variant of SARS‐CoV‐2: impacts, challenges and strategies. J Infect Public Health. 2023;16(1):4‐14. 10.1016/j.jiph.2022.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nahar Z, Sohan M, Supti KF, et al. Prevalence and associated risk factors for mental health problems among female university students during COVID‐19 pandemic: a cross‐sectional study findings from Dhaka, Bangladesh. Heliyon. 2022;8(10):e10890. 10.1016/j.heliyon.2022.e10890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Arafat SMY, Hussain F, Zaman MS, et al. Thwarted belongingness, perceived burdensomeness, and acquired capability for suicide among university students of Bangladesh: scales validation and status assessment. Front Psychiatry. 2022;13:1025976. 10.3389/fpsyt.2022.1025976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Al‐Mamun M, Hossain MJ, Alam M, Parvez MS, Dhar BK, Islam MR. Discrimination and social exclusion of third‐gender population (Hijra) in Bangladesh: A brief review. Heliyon. 2022;8(10):e10840. 10.1016/j.heliyon.2022.e10840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Islam R. The COVID‐19 pandemic and suicidal behavior in Bangladesh: social stigma and discrimination are key areas to focus on. Alpha Psychiatry. 2021;22:275‐276. 10.5152/alphapsychiatry.2021.21498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Haque AKMB, Arifuzzaman BM, Siddik SAN, et al. Semantic web in healthcare: a systematic literature review of application, research gap, and future research avenues. Int J Clin Pract. 2022;2022:1‐27. 10.1155/2022/6807484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hossain MJ, Soma MA, Bari MS, Emran TB, Islam MR. COVID‐19 and child marriage in Bangladesh: emergency call to action. BMJ Paediatr Open. 2021;5(1):e001328. 10.1136/bmjpo-2021-001328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hossain MJ, Ahmmed F, Khandokar L, et al. Status of psychological health of students following the extended university closure in Bangladesh: results from a web‐based cross‐sectional study. PloS Global Public Health. 2022;2(3):e0000315. 10.1371/journal.pgph.0000315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jannath S, Sohan M, Rahman MA, Islam MR. Suicides among university students during the COVID‐19 pandemic: Bangladeshi press reports. Open Health. 2022;3:13‐19. 10.1515/openhe-2022-0002. [DOI] [Google Scholar]
- 56. Jahan I, Hosen I, Al Mamun F, Kaggwa MM, Griffiths MD, Mamun MA. How has the COVID‐19 pandemic impacted internet use behaviors and facilitated problematic internet use? A Bangladeshi study. Psychol Res Behav Manag. 2021;14:1127‐1138. 10.2147/PRBM.S323570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Liu S, Zou S, Zhang D, Wang X, Wu X. Problematic Internet use and academic engagement during the COVID‐19 lockdown: the indirect effects of depression, anxiety, and insomnia in early, middle, and late adolescence. J Affect Disord. 2022;309:9‐18. 10.1016/j.jad.2022.04.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Islam MR, Qusar MMAS, Islam MS. Mental health of children amid COVID‐19 pandemic in Bangladesh: an exploratory observation. Asia Pac J Public Health. 2021;33(4):469‐470. 10.1177/10105395211004371 [DOI] [PubMed] [Google Scholar]
- 59. Krishnamurthy S, Chetlapalli S. Internet addiction: prevalence and risk factors: a cross‐sectional study among college students in Bengaluru, the Silicon Valley of India. Indian J Public Health. 2015;59(2):115‐121. [DOI] [PubMed] [Google Scholar]
- 60. Balhara YS, Mahapatra A, Sharma P, Bhargava R. Problematic internet use among students in South‐East Asia: current state of evidence. Indian J Public Health. 2018;62(3):197‐210. [DOI] [PubMed] [Google Scholar]
- 61. Xie X, Zhu K, Xue Q, et al. Problematic internet use was associated with psychological problems among university students during COVID‐19 outbreak in China. Front Public Health. 2021;9:675380. 10.3389/fpubh.2021.675380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kostev K, Weber K, Riedel‐Heller S, von Vultée C, Bohlken J. Increase in depression and anxiety disorder diagnoses during the COVID‐19 pandemic in children and adolescents followed in pediatric practices in Germany. Eur. Child Adolesc Psychiatry. 2021;2021:1‐7. 10.1007/s00787-021-01924-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nahar Z, Sohan Md, Supti KF, Hossain MdJ, Shahriar M, Bhuiyan MA, Islam MdR. Prevalence and associated risk factors for mental health problems among female university students during COVID‐19 pandemic: A cross‐sectional study findings from Dhaka, Bangladesh. Heliyon. 2022;8(10):e10890. 10.1016/j.heliyon.2022.e10890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Islam MR, Tushar MI, Jannath S, Moona AA, Akter S, Islam SMA. Data set concerning the use of social networking sites and mental health problems among the young generation in Bangladesh. Data Brief. 2021;39:107593. 10.1016/j.dib.2021.107593 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article or its Supporting Information.


